Abstract
Background
The International Diabetes Federation (IDF) estimated that 1.1 million children and adolescents aged 14–19 years are living with diabetes. Diabetes is a chronic, progressive disease characterized by elevated levels of blood glucose. It is also recognized as a complex disease that affects people of different ages due to different causes. The present study aims to estimate the prevalence of pre-diabetes/diabetes at the national level. Additionally, the respective study determines the factors associated with pre-diabetes/diabetes conditions among adolescents at the national level.
Methods
The data for this study was carried out from the Comprehensive National Nutrition Survey (CNNS), the first-ever nationally representative nutrition survey of children and adolescents in India. The study used a sample size of 17,865 adolescent boys and 17,965 adolescent girls for the analysis. Descriptive statistics, bivariate analysis, and logistic regression analysis were done to carve out the results.
Results
The prevalence of pre-diabetes/diabetes was 12.3% and 8.4% among adolescent boys and girls in India, respectively. Body mass index and Subscapular skinfold thickness were the two most important predictors of pre-diabetes/diabetes among adolescents. Further, physical activities show a negative association with pre-diabetes/diabetes. Moreover, interaction models in the present study clearly reveal the fact that adolescent girls were less likely to suffer from pre-diabetes/diabetes than adolescent boys. Additionally, it was found that the prevalence of pre-diabetes/diabetes was high among adolescent girls from lower socio-economic strata.
Conclusion
The high prevalence of pre-diabetes and diabetes among adolescents portrayed serious public health concern in India. As body mass index and Subscapular skinfold thickness were positively associated with pre-diabetes/diabetes conditions among adolescents. Therefore, effective approaches are needed to be taken to tackle these pre-diabetes/diabetes conditions among adolescents and especially among adolescent boys.
Keywords: Pre-diabetes/diabetes, Obesity, Adolescents, India
Background
The International Diabetes Federation (IDF) estimated that 1.1 million children and adolescents aged 14–19 years were living with diabetes [1]. In addition, the increasing prevalence of pre-diabetes and diabetes led by obesity among the young population fuelled metabolic syndrome and obesity-related co-morbidities across the low and middle-income countries [2]. There is a global effort to curb down the rise of diabetes and obesity by 2025; however, a steady rise in the prevalence of diabetes is a matter of concern [3].
India alone contributes a larger proportion to premature deaths from non-communicable diseases (NCDs), including diabetes across all socio-economic groups [4]. Achieving the global agenda of Sustainable Development Goals (SDGs) by 2030, by reducing one-third of premature mortality from NCDs–including diabetes, a universal healthcare access approach is therefore required in most developing countries, including India [3, 4]. India is currently going through the nutritional transition, and it is evident with a rise in the prevalence of overweight and obesity [5]. Also, estimates shows that nearly 166 million adults are overweight/obese in 2016 in India [3]. In the case of adults who are affected by diabetes, the numbers are estimated to be nearly 73 million, the second-largest in the world [1].
Diabetes is a chronic, progressive disease characterized by elevated levels of blood glucose levels. It is also recognized as a complex disease that affects people of different ages due to different causes. There are three main types of diabetes, type-1 diabetes (T1D), type-2 diabetes (T2D), and gestational diabetes mellitus (GDM) [3]. The type-1 diabetes incidence rate is increasing among the younger population, and the contributing factors have remained unclear. However, there are factors that affect the heterogeneity of the respective disease such as genetic factors, behavioural risk factors, food and dietary habits, physical inactivity, lifestyle changes.
Furthermore, the prevalence of pre-diabetes/diabetes among children, adolescents, and even younger adults is increasing at a much higher rate irrespective of socio-economic strata, and it becomes more severe because of the rising levels of obesity among them [6–8], physical inactivity [9, 10], and poor dietary habits [11]. Moreover, increased levels of substance use [12, 13] among adolescent groups have also led to risk for pre-diabetes/diabetes-associated health issues [10, 14]. Further, the high spread of pre-diabetes/diabetes among the population is also witnessed in the light of different socio-economic groups [15], and it is concentrated differently across rural-urban, age-sex, and family history of diabetes [16–18].
However, lack of physical activities and having a sedentary lifestyle among adolescents made responsible for cardiovascular disease and obesity-related risk factors which in turn may cause menace of pre-diabetes/diabetes among them [10, 19, 20]. That has not been well established in the literature in the Indian context among the adolescents population. In this way, there are multiple determinants associated with risk factors for pre-diabetes and diabetes that influence the adolescent population and they are more prone to be affected by them [16, 21]. Moreover, Triglycerides, Cholesterol, High-density lipoprotein (HDL), and Low-density lipoprotein (LDL) levels are found to be significant factors for the prevalence of pre-diabetes/diabetes among adolescents [22, 23].
The present study utilized the different forms of obesity, which may affect the chaos of pre-diabetes/diabetes differently. Previous literature showed different measures of obesity in their studies [11, 24–26]. For instance, obesity measured through body mass index [23], waist circumference [23], waist to hip ratio [27], Subscapular skinfold thickness (SSFT) [28] and Triceps skinfold thickness (TSFT) [28].
There exists a dearth of literature focusing on the association of pre-diabetes/diabetes with obesity levels among adolescents at the national level in India. Therefore, the present study aims to estimate the prevalence of pre-diabetes/diabetes at the national level. Additionally, the study also analyses the factors that are responsible for pre-diabetes/diabetes conditions among adolescents (for both adolescent boys and girls) at the national level. The study hypothesized that there was no association between pre-diabetes/diabetes conditions with obesity levels and physical activity among adolescents in India.
Methods
The data was taken from the Comprehensive National Nutrition Survey (CNNS), the first-ever nationally representative nutrition survey of children and adolescents in India. The survey collected the data on the status of pre-school (0–4 years), school-age children (5–9 years), and adolescents (10–19 years) through interviews, a comprehensive set of anthropometric measures, and biochemical indicators. The CNNS covered all 30 states of India using a multi-stage survey design for the selection of households and individuals aged 0–19 years. The data has been collected with the written consent of the participants. The survey was implemented under the guidance of the MoHFW, UNICEF, a Technical Advisory Group (TAG), and the Center for Disease Control (CDC). Data can be obtained on request from the Population Council (India office) website. The detailed methodology, sampling design, and data collection procedure were published in the survey report [29]. The CNNS collected data from a total of 38,060 children aged 0–4 years, 38,355 children aged 5–9 years, and 35,830 adolescents age 10–19 years. The study used a sample size of 17,865 adolescent boys and 17,965 adolescent girls for the analysis.
Outcome variable
The outcome variable was pre-diabetes/diabetes conditions among adolescents aged 10–19 years. The pre-diabetes/diabetes was diagnosed using glycosylated haemoglobin (HbA1c) [30]. The American Diabetes Association recommended glycated hemoglobin (HbA1c) as a possible substitute to fasting blood glucose for diagnosis of diabetes [31, 32]. Analysis of glycated hemoglobin (HbA1c) in blood provides the evidence about the respondent’s/individual average blood glucose levels during the last 2–3 months, which is the predicted half-life of red blood cells (RBCs) [33]. The cut-off points for pre-diabetes/diabetes among adolescents were as: pre-diabetes (> 5.8% and ≤ 6.4%) and diabetes (> 6.4%) [34]. We merged diabetes and pre-diabetes into one category due to the small sample in the diabetes condition. The outcome variable was divided into two categories as 0 “no pre-diabetes/diabetes” and 1 “pre-diabetes/diabetes”. The type of diabetes studied is Type 2 Diabetes mellitus. The study did not include fasting glucose data as HbA1c reflects average plasma glucose levels over the previous 8 to 12 weeks [28].
Exposure variables
Body mass index was categorized as not overweight/obese (BMI ≤ + 1 SD) and overweight/obese (BMI > + 1 SD) group, abdominal obesity was categorized as no (waist circumference-for-age ≤ + 1 SD) and yes (waist circumference-for-age > + 1 SD), Triceps skinfold thickness (TSFT) was grouped as not overweight (TSFT-for-age ≤ + 1 SD) and overweight (TSFT-for-age > + 1 SD) and Subscapular skinfold thickness (SSFT) was divided into two categories: not overweight (SSFT-for-age ≤ + 1 SD) and overweight (SSFT-for-age > + 1 SD). Body mass index z-scores, also called BMI standard deviation (s.d.) scores, are measures of relative weight adjusted for child age and sex [35]. Given a child’s age, sex, BMI, and an appropriate reference standard, a BMI z-score (or its equivalent BMI-for-age percentile) can be determined [35]. Physical activity was categorized as a low, medium, and high using the principal component analysis approach as 15 questions were used to generate the respective variable [29]. Serum triglycerides (assessed by spectrophotometry and enzymatic endpoint method) was categorized into low (< 130 mg/dl) and high (≥130 mg/dl), cholesterol (assessed by spectrophotometry using cholesterol oxidase esterase peroxidase) was recoded as low (< 200 mg/dl) and high (≥200 mg/dl), low-density lipoprotein (LDL) (assessed by spectrophotometry and direct measure cholesterol oxidase) was categorized as low (< 130 mg/dl) and high (≥130 mg/dl), and high-density lipoprotein (HDL) cholesterol (assessed by spectrophotometry and direct measure polyethylene glycol-modified cholesterol oxidase) was recoded as low (< 40 mg/dl) and high (≥40 mg/dl). Age was categorized into early adolescents (10–14 years) and late adolescents (15–19 years), education was divided into no schooling, dropouts and currently studying, Media exposure was categorized as no “no exposure to television & radio & newspaper & internet” and yes “exposure to television or radio or newspaper or internet), parent education was recoded as (both uneducated, anyone educated and both educated), parent diabetes status was categorized as (no or anyone had), the diet was categorized as vegetarian and non-vegetarian; Junk food consumption was categorized as no, 1–2 days and 3–7 days; substance use was categorized as no and yes. Caste was categorized as Scheduled Caste/Scheduled Tribe (SC/ST) and non- Scheduled Caste/Scheduled Tribe. Among the four categories of castes, people belonging to the Scheduled caste lies at the bottom of the Indian caste system and have been exploited for over centuries. The indigenous groups of India belong to the category of Scheduled tribes and are among the most deprived sections. Therefore SC/ST is the deprived section of the society [36]. Religion was categorized as Hindu, Muslim, Christian, and Others; wealth quintile was categorized as poor, middle and rich; the residence was categorized as urban and rural; and region were divided as north, central, east, north-east, west, and south.
Statistical analysis
Descriptive analysis was used to show the sample profile of the respondents. Further, bivariate analysis was carried out to estimate the prevalence of pre-diabetes/diabetes by selected variables, and a proportion test was applied to test the significant difference between adolescent boys and girls for pre-diabetes/diabetes. Finally, multivariate logistic regression was performed to find out the effects of different predictors on pre-diabetes/diabetes. The results are presented in the form of an odds ratio (OR) with a 95% confidence interval (CI). The model is usually put into a more compact form as follows:
Where β0, …. . , βM are the regression coefficient indicating the relative effect of a particular explanatory variable on the outcome, the study further examined the possible interaction between body mass index, abdominal obesity, triceps skinfold thickness (TSFT), subscapular skinfold thickness (SSFT), and gender in models 2, 3, 4, and 5 respectively.
Results
Anthropometric and socio-demographic profiles of adolescents aged 10–19 years are presented in Table 1. Overall, nearly 5% of adolescent boys and girls (each) were overweight/obese whereas about 2% and 1% of adolescent boys and girls had abdominal obesity, respectively. Moreover, about 5% and 2% of adolescent boys and girls had triceps skinfold thickness, respectively. Seven percent of adolescent boys and 4% of girls had subscapular skinfold thickness. About 14% of boys and 18% of adolescent girls had high serum triglycerides. Moreover, almost the same proportion of adolescents (3% vs. 5%) had high cholesterol and low-density lipoprotein respectively. The proportion of adolescents was higher in the 10–14 years age group irrespective of gender. The majority of adolescents are currently studying and, around 17% of adolescent boys and 21% of girls were school dropouts. More than three-fourth of adolescents had some mass media exposure. One-fourth of the parents had no schooling and a very low proportion of parents (anyone) had diabetes (4%). About 81% of adolescent boys and 73% of girls were non-vegetarian. Seven out of ten adolescents were consumed 1–2 days of junk food. Substance use was higher among adolescent boys (8%) than girls. One-third of adolescents belonged to SC/ST group and the majority of adolescents were Hindu. Two-fifth of adolescents belonged to rich families and one-fourth of adolescents lived in urban areas.
Table 1.
Anthropometric and socio-demographic profile of adolescents aged 10–19 years in India, 2016–18
| Variables | Adolescent boys | Adolescent girls | ||
|---|---|---|---|---|
| Sample | Percent | Sample | Percent | |
| Body mass Index (BMI) | ||||
| Not overweight/obese | 15,697 | 95.0 | 14,841 | 95.1 |
| Overweight/obese | 821 | 5.0 | 761 | 4.9 |
| Abdominal obesity | ||||
| No | 17,116 | 97.8 | 16,271 | 98.8 |
| Yes | 381 | 2.2 | 202 | 1.2 |
| Triceps skinfold thickness (TSFT) | ||||
| Not overweight | 16,675 | 94.7 | 16,276 | 98.3 |
| Overweight | 937 | 5.3 | 276 | 1.7 |
| Subscapular skinfold thickness (SSFT) | ||||
| Not overweight | 16,356 | 92.9 | 15,826 | 95.7 |
| Overweight | 1249 | 7.1 | 704 | 4.3 |
| Physical activity | ||||
| Low | 6963 | 37.8 | 12,178 | 70.0 |
| Medium | 4975 | 27.0 | 2544 | 14.6 |
| High | 6486 | 35.2 | 2683 | 15.4 |
| Serum triglycerides | ||||
| Low | 5856 | 85.9 | 5241 | 81.7 |
| High | 963 | 14.1 | 1172 | 18.3 |
| Cholesterol | ||||
| Low | 6582 | 96.6 | 6112 | 95.4 |
| High | 234 | 3.4 | 293 | 4.6 |
| Low-density lipoprotein | ||||
| Low | 6591 | 96.8 | 6121 | 95.5 |
| High | 220 | 3.2 | 289 | 4.5 |
| High-density lipoprotein | ||||
| Low | 2008 | 29.6 | 1533 | 24.0 |
| High | 4780 | 70.4 | 4854 | 76.0 |
| Age (years) | ||||
| Early adolescence (10–14) | 9757 | 53.0 | 8832 | 50.7 |
| Late adolescence (15–19) | 8668 | 47.0 | 8573 | 49.3 |
| Education | ||||
| No schooling | 885 | 4.8 | 1182 | 6.8 |
| Dropout | 3194 | 17.3 | 3721 | 21.4 |
| Currently studying | 14,346 | 77.9 | 12,502 | 71.8 |
| Media exposure | ||||
| No | 2955 | 16.0 | 4080 | 23.4 |
| Yes | 15,470 | 84.0 | 13,325 | 76.6 |
| Parent education | ||||
| Both uneducated | 4487 | 24.4 | 4529 | 26.0 |
| Anyone educated | 5908 | 32.1 | 5782 | 33.2 |
| Both educated | 8030 | 43.6 | 7094 | 40.8 |
| Parents diabetes status | ||||
| No one | 17,675 | 95.9 | 16,769 | 96.4 |
| Anyone had | 750 | 4.1 | 636 | 3.7 |
| Diet | ||||
| Vegetarian | 3519 | 19.1 | 4770 | 27.4 |
| Non-vegetarian | 14,902 | 80.9 | 12,634 | 72.6 |
| Junk food consumption | ||||
| No | 4876 | 26.5 | 4638 | 26.7 |
| 1–2 days | 12,771 | 69.3 | 12,216 | 70.2 |
| 3–7 days | 774 | 4.2 | 549 | 3.2 |
| Substance use | ||||
| No | 16,876 | 91.6 | 17,194 | 98.8 |
| Yes | 1549 | 8.4 | 211 | 1.2 |
| Caste | ||||
| SC/ST | 5769 | 33.2 | 5769 | 33.2 |
| Non-SC/ST | 11,636 | 66.9 | 11,636 | 66.9 |
| Religion | ||||
| Hindu | 14,878 | 80.8 | 13,797 | 79.3 |
| Muslim | 2643 | 14.3 | 2819 | 16.2 |
| Christian | 458 | 2.5 | 381 | 2.2 |
| Others | 446 | 2.4 | 408 | 2.3 |
| Wealth quintile | ||||
| Poor | 7292 | 39.6 | 7036 | 40.4 |
| Middle | 3696 | 20.1 | 3473 | 20.0 |
| Rich | 7437 | 40.4 | 6896 | 39.6 |
| Place of residence | ||||
| Rural | 13,788 | 74.8 | 13,174 | 75.7 |
| Urban | 4637 | 25.2 | 4231 | 24.3 |
| Regions | ||||
| North | 2597 | 14.1 | 2306 | 13.3 |
| Central | 5750 | 31.2 | 5936 | 34.1 |
| East | 4248 | 23.1 | 4148 | 23.8 |
| Northeast | 582 | 3.2 | 507 | 2.9 |
| West | 2327 | 12.6 | 1864 | 10.7 |
| South | 2921 | 15.9 | 2644 | 15.2 |
| Total | 17,865 | 100.0 | 17,965 | 100.0 |
SC/ST Scheduled caste/ Scheduled tribe
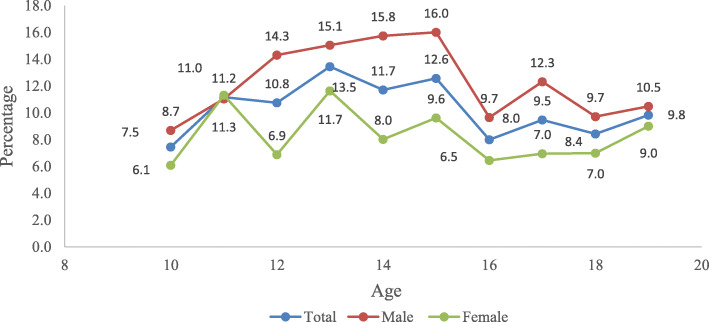
Gender differentials for pre-diabetes/diabetes among adolescents are presented in Fig. 1. Pre-diabetes/diabetes was more prevalent among 15 years of adolescents, and it is lower in 10 years of adolescents. Though, the prevalence of pre-diabetes/diabetes was higher among adolescent boys compared to girls irrespective of their age.
Fig. 1.
Gender differentials for pre-diabetes/diabetes among adolescents in India
Table 2 shows the gender differences in the prevalence of pre-diabetes/diabetes among adolescents aged 10–19 years across different socio-demographic characteristics in India. The prevalence of pre-diabetes/diabetes was higher among adolescent boys across all the selected socio-demographic characteristics and differences were statistically significant. Substantial differences were observed among adolescents who had abdominal obesity (11.7%), overweight (SSFT) (9.8%), belonged to the Northeast region (10.1%), consumed junk food for 3–7 days (8.5%), and belonged to the middle (6.4%) and rich families (5.6%).
Table 2.
Prevalence of pre-diabetes/diabetes among adolescents aged 10–19 years by socio-demographic characteristics in India, 2016–18
| Variables | Adolescent boys | Adolescent girls | Adolescent boys - Adolescent girls | Proportion Test |
|---|---|---|---|---|
| (%) | (%) | (%) | P < 0.05 | |
| Body Mass Index (BMI) | ||||
| Not overweight/obese | 12.1 | 8.2 | 3.9 | |
| Overweight/obese | 17.2 | 11.5 | 5.7 | * |
| Abdominal obesity | ||||
| No | 12.2 | 8.3 | 3.8 | * |
| Yes | 20.8 | 9.1 | 11.7 | |
| Triceps skinfold thickness (TSFT) | ||||
| Not overweight | 12.0 | 8.3 | 3.7 | |
| Overweight | 18.6 | 10.5 | 8.0 | |
| Subscapular skinfold thickness (SSFT) | ||||
| Not overweight | 11.6 | 8.1 | 3.5 | |
| Overweight | 22.6 | 12.8 | 9.8 | * |
| Physical activity | ||||
| Low | 13.6 | 8.3 | 5.4 | * |
| Medium | 12.2 | 9.2 | 3.0 | * |
| High | 11.6 | 7.5 | 4.0 | * |
| Serum triglycerides | ||||
| Low | 12.2 | 9.2 | 3.0 | * |
| High | 10.3 | 5.5 | 4.8 | * |
| Cholesterol | ||||
| Low | 12.0 | 8.5 | 3.5 | * |
| High | 9.1 | 8.5 | 0.6 | * |
| Low-density lipoprotein | ||||
| Low | 11.9 | 8.3 | 3.6 | * |
| High | 13.2 | 13.1 | 0.1 | * |
| High-density lipoprotein | ||||
| Low | 8.7 | 7.9 | 0.8 | * |
| High | 12.3 | 8.7 | 3.7 | * |
| Age (years) | ||||
| Early adolescence (10–14) | 13.0 | 8.7 | 4.3 | * |
| Late adolescence (15–19) | 11.7 | 7.8 | 3.9 | * |
| Education | ||||
| No schooling | 8.2 | 7.7 | 0.5 | |
| Dropout | 12.3 | 9.4 | 2.9 | * |
| Currently studying | 12.6 | 8.1 | 4.6 | * |
| Media exposure | ||||
| No | 11.8 | 7.1 | 4.7 | |
| Yes | 12.6 | 8.6 | 4.0 | * |
| Parent education | ||||
| Both uneducated | 12.5 | 8.0 | 4.5 | * |
| Anyone educated | 12.7 | 9.3 | 3.4 | * |
| Both educated | 12.3 | 7.7 | 4.6 | * |
| Parents diabetes status | ||||
| No one | 12.5 | 8.4 | 4.2 | * |
| Anyone had | 10.2 | 6.7 | 3.5 | |
| Diet | 0.0 | |||
| Vegetarian | 14.1 | 10.3 | 3.9 | * |
| Non-vegetarian | 12.0 | 7.6 | 4.5 | * |
| Junk food consumption | ||||
| No | 12.9 | 10.7 | 2.2 | * |
| 1–2 days | 12.1 | 7.5 | 4.7 | * |
| 3–7 days | 14.1 | 5.7 | 8.5 | * |
| Substance use | ||||
| No | 11.9 | 8.2 | 3.7 | * |
| Yes | 18.9 | 14.1 | 4.8 | * |
| Caste | ||||
| SC/ST | 11.8 | 9.5 | 2.4 | * |
| Non-SC/ST | 12.7 | 7.7 | 5.0 | * |
| Religion | ||||
| Hindu | 12.3 | 8.5 | 3.8 | * |
| Muslim | 11.8 | 6.3 | 5.5 | * |
| Christian | 18.1 | 12.3 | 5.8 | * |
| Others | 15.3 | 10.1 | 5.1 | |
| Wealth quintile | ||||
| Poor | 10.8 | 9.4 | 1.4 | * |
| Middle | 14.0 | 7.6 | 6.4 | * |
| Rich | 13.3 | 7.6 | 5.6 | * |
| Place of residence | ||||
| Rural | 12.4 | 8.4 | 4.0 | * |
| Urban | 12.7 | 8.0 | 4.7 | * |
| Regions | ||||
| North | 16.3 | 10.6 | 5.8 | * |
| Central | 11.1 | 6.9 | 4.2 | * |
| East | 9.3 | 5.5 | 3.7 | * |
| Northeast | 18.4 | 8.3 | 10.1 | * |
| West | 13.7 | 12.9 | 0.9 | |
| South | 14.5 | 10.2 | 4.3 | * |
| Total | 12.4 | 8.3 | 4.1 | * |
*if p < 0.05; SC/ST Scheduled caste/ Scheduled tribe, % Percentage
Binary logistic regression estimates for pre-diabetes/diabetes among adolescents aged 10–19 years are presented in Table 3. Results from model-1 found that overweight/obese adolescents had 41% higher chances [Odd ratio (OR), 1.41; CI: 1.08–1.82] to get pre-diabetes/diabetes compared to adolescents who were not overweight/obese. Moreover, SSFT had a significant effect on pre-diabetes/diabetes among adolescents. Overweight adolescents (SSFT) were significantly more likely (OR, 1.49: CI: 1.15–1.94) to suffer from pre-diabetes/diabetes than those who were not overweight. There was a negative relationship between the physical activity of adolescents and their pre-diabetes/diabetes condition. Adolescents involved in high physical activity were less likely to suffer from pre-diabetes/diabetes compared to those who did low physical activities. However, the result was not significant for physical activities.
Table 3.
Logistic regression estimates for pre-diabetes/diabetes among adolescents aged 10–19 by socio-demographic characteristics in India, 2016–18
| Variables | Model-1 | Model-2 | Model-3 | Model-4 | Model-5 |
|---|---|---|---|---|---|
| OR(95% CI) | OR(95% CI) | OR(95% CI) | OR(95% CI) | OR(95% CI) | |
| Body mass index (BMI) | |||||
| Not overweight/obese | Ref. | Ref. | Ref. | Ref. | |
| Overweight/obese | 1.41*(1.08,1.82) | 1.4*(1.08,1.82) | 1.39*(1.07,1.81) | 1.39*(1.07,1.81) | |
| Abdominal obesity | |||||
| No | Ref. | Ref. | Ref. | Ref. | |
| Yes | 1.06 (0.73,1.54) | 1.09 (0.75,1.59) | 1.07 (0.73,1.55) | 1.07 (0.74,1.56) | |
| Triceps skinfold thickness (TSFT) | |||||
| Not overweight | Ref. | Ref. | Ref. | Ref. | |
| Overweight | 0.89 (0.64,1.24) | 0.92 (0.66,1.27) | 0.9 (0.65,1.25) | 0.92 (0.66,1.28) | |
| Subscapular skinfold thickness (SSFT) | |||||
| Not overweight | Ref. | Ref. | Ref. | Ref. | |
| Overweight | 1.49*(1.15,1.94) | 1.49*(1.15,1.94) | 1.5*(1.15,1.95) | 1.5*(1.15,1.95) | |
| Physical activity | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| Medium | 0.90 (0.76,1.06) | 0.90 (0.76,1.06) | 0.90 (0.76,1.06) | 0.90 (0.76,1.06) | 0.90 (0.76,1.06) |
| High | 0.80 (0.85,1.14) | 0.80 (0.85,1.14) | 0.80 (0.85,1.14) | 0.80 (0.84,1.14) | 0.80 (0.85,1.14) |
| Serum triglycerides | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 0.90 (0.75,1.07) | 0.90 (0.75,1.07) | 0.90 (0.75,1.07) | 0.90 (0.76,1.07) | 0.90 (0.75,1.07) |
| Cholesterol | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 1.02 (0.69,1.52) | 1.03 (0.69,1.53) | 1.03 (0.69,1.52) | 1.03 (0.69,1.53) | 1.03 (0.69,1.53) |
| Low-density lipoprotein | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 1.33 (0.93,1.9) | 1.32 (0.92,1.9) | 1.33 (0.93,1.9) | 1.33 (0.93,1.91) | 1.33 (0.92,1.9) |
| High-density lipoprotein | |||||
| Low | Ref. | Ref. | Ref. | Ref. | Ref. |
| High | 0.93 (0.8,1.07) | 0.93 (0.8,1.07) | 0.93 (0.8,1.07) | 0.93 (0.8,1.07) | 0.93 (0.8,1.07) |
| Body mass index (BMI)*Gender | |||||
| Adolescent boysa Not overweight/obese | Ref. | ||||
| Adolescent boysa Overweight/obese | 1.18 (0.78,1.79) | ||||
| Adolescent girls a Not overweight/obese | 0.72*(0.62,0.83) | ||||
| Adolescent girls a Overweight/obese | 0.74 (0.48,1.15) | ||||
| Abdominal obesity*Gender | |||||
| Adolescent boys a No | Ref. | ||||
| Adolescent boysa Yes | 1.26 (0.74,2.17) | ||||
| Adolescent girls a No | 0.73*(0.63,0.84) | ||||
| Adolescent girls a Yes | 0.41 (0.16,1.07) | ||||
| Triceps skinfold thickness (TSFT)*Gender | |||||
| Adolescent boysa Not overweight | Ref. | ||||
| Adolescent boysa Overweight | 0.96 (0.63,1.45) | ||||
| Adolescent girls a Not overweight | 0.72*(0.62,0.83) | ||||
| Adolescent girls a Overweight | 0.48 (0.21,1.1) | ||||
| Subscapular skinfold thickness (SSFT)*Gender | |||||
| Adolescent boysa Not overweight | Ref. | ||||
| Adolescent boysa Overweight | 2.23*(1.53,3.23) | ||||
| Adolescent girls a Not overweight | 0.72*(0.62,0.84) | ||||
| Adolescent girls a Overweight | 1.38 (0.9,2.11) | ||||
a Interaction; OR: Odds Ratio; CI: Confidence Interval; Ref: Reference; *if p < 0.05
Note: All the models have been run after controlling the other socio-demographic factors
Model 2 represents the interaction between body mass index and gender for pre-diabetes/diabetes. Interestingly, adolescent girls with not overweight/obese category were significantly less likely to suffer (OR, 0.72; CI: 0.62–0.83) from pre-diabetes/diabetes compared to adolescent boys who belonged to the not overweight/obese category. Interaction between gender and abdominal obesity for pre-diabetes/diabetes condition is presented in Model 3. Adolescent boys having abdominal obesity were more likely (OR, 1.26; CI: 0.74–2.17) to suffer from pre-diabetes/diabetes than adolescent boys with no abdominal obesity. Moreover, adolescent girls with abdominal obesity were significantly less likely (OR, 0.73; CI: 0.63–0.84) to suffer from pre-diabetes/diabetes compared to adolescent boys with no abdominal obesity. Results from Model 4 revealed the interaction between gender and triceps skinfold thickness (TSFT) for pre-diabetes/diabetes among adolescents. The likelihood of pre-diabetes/diabetes among overweight (TSFT) adolescent boys was lower (OR, 0.96; CI: 0.63–1.45) than a not overweight adolescent boys. However, the chances of pre-diabetes/diabetes among girls with not overweight category were significantly lower (OR, 0.72; CI: 0.62–0.83) compared to boys with no overweight category. Model 5 shows the interaction between gender and subscapular skinfold thickness (SSFT) for pre-diabetes/diabetes among adolescents. SSFT had a significant effect on diabetes among both adolescent boys and girls. The probability of getting diabetes was significantly higher (OR, 2.23; CI: 1.53–3.23) among overweight (SSFT) adolescent boys than those who were not overweight. Moreover, adolescent girls from the not overweight category were significantly less likely (OR, 0.72; CI: 0.62–0.84) to suffer from pre-diabetes/diabetes compared to boys from the not overweight category.
Discussion
The overall prevalence of pre-diabetes/diabetes was 12.3% and 8.4% among adolescent boys and girls in India respectively. Moreover, it was found that body mass index (BMI) and subscapular skinfold thickness (SSFT) was significantly associated with pre-diabetes/diabetes among adolescents in India. Additionally, it was revealed that adolescent girls were less likely to suffer from pre-diabetes/diabetes than adolescent boys in every category of obesity measure.
Earlier studies found that no accessibility of proper care such as early diagnosis, diabetes care management, and blood glucose testing available in primary healthcare settings in the early phases of life for children and adolescents [16, 37]. Early diagnosis of pre-diabetes/diabetes can have lesser risk in the long-term than remaining undiagnosed.
The current study reveals the fact that there was a positive association between BMI, SSFT, and low physical activity status with pre-diabetes/diabetes conditions among adolescents in India. The results were consistent with previous findings that increased BMI was positively associated with pre-diabetes/diabetes conditions among adolescents [20]. Moreover, SSFT was also a significant risk factor of pre-diabetes/diabetes conditions among adolescents, as argued by previous literature [38–40]. Apart from obesity, genetic and metabolic factors, there are other significant risk factors, but in the present study, those were not taken into account due to data limitations [2, 26, 37]. Additionally, low physical activity status was found to be a substantial risk factor for pre-diabetes/diabetes conditions among adolescents, as found in previous studies [41]. It was too argued that even a moderate level of physical activity could help in the prevention of pre-diabetes conditions by reducing obesity levels among adolescents [41].
Dietary practices with unhealthy food such as high intake of junk foods and sugar-sweetened beverages are associated with a high prevalence of obesity/overweight that may lead to pre-diabetes/diabetes conditions among adolescents [42, 43]. This finding is consistent with findings of the present that adolescents with junk food consumption frequency of 3–7 days a week had a high prevalence of pre-diabetes/diabetes condition. Additionally, the menace of substance use among adolescents was a staunch factor for pre-diabetes/diabetes conditions. The finding was paralleled with the previous study that abnormal alcohol and drug use among adolescents increases the risk of pre-diabetes/diabetes conditions [44].
Although it was earlier argued that diabetes is an affluent disease and it occurs among the population from higher socio-economic strata [16], however, the present study revealed that the disease pattern is now shifting towards lower affluent population, for instance, pre-diabetes/diabetes condition was more among SC/ST, poor and adolescents from rural areas especially in case of adolescent girls. Further research is needed to look into the highly prevailing pre-diabetes/diabetes among adolescents irrespective of caste, class, gender and geographical locations.
The results showed that pre-diabetes/diabetes vary across gender; for instance, gender differential was over 4%, i.e., adolescent boys are more prone to pre-diabetes/diabetes than adolescent girls. Moreover, for most of the background factors, adolescent boys were at high risk than adolescent girls. Even previous literature argued that adolescent girls do have a lower probability to suffer from pre-diabetes/diabetes [45]. The plausible reasons can be derived through descriptive statistics in the present study where it was clearly visible that obesity levels and substance use were low among adolescent girls and which may further protect them from the burden of pre-diabetes and diabetes condition in comparison to their counterpart. Additionally, interaction models revealed that adolescent girls were less likely to suffer from pre-diabetes/diabetes in comparison to adolescent boys for the obesity measure. The findings are found to be consistent with the previous one as it was argued that adolescent girls are less likely to be overweight or obese [46].
Limitation
The study has potential limitations. This study used cross-sectional data that does not allow establishing a causal relationship between variables. Additionally, Type 1 Diabetes mellitus, which is more common in adolescents, is not taken into account which is also a major limitation of this article. Glucose Tolerance Test, Fasting Blood Sugar (FBS) test and Post Prandial Blood Sugar (PPBS) test were not performed. Despite the limitation, the study also has its own strength. This study used large scale survey data of adolescents which is the first-ever survey on nutrition and gives reliable estimates on diabetes at the national level.
Conclusion
Our study found that pre-diabetes/diabetes was highly prevalent among adolescents especially among adolescent boys in India. Interaction models in the present study clearly reveal the fact that adolescent girls are less likely to suffer from pre-diabetes/diabetes than adolescent boys. BMI and SSFT are the two most important predictors of pre-diabetes/diabetes among adolescents in India. The high prevalence of pre-diabetes/diabetes among adolescent girls from lower socio-economic strata poses a high concern in the Indian scenario. The emerging type 1 diabetes (T1D) among children and adolescents cannot be prevented with existing knowledge [3]. However, type 2 diabetes can be prevented with effective approaches available, and premature deaths can be curtailed off [3]. To avoid diabetes and related risk factors, regular exercise, maintaining a healthy diet, avoiding substance use, and controlling blood pressure and lipids as recommended by WHO guidelines [3]. The present study also suggests that to prevent pre-diabetes/diabetes conditions among adolescents certain health interventions are required. Utilization of knowledge, awareness, and programme (KAP) re-intervention to control obese/overweight among adolescents on the one hand and the regular health check-ups among adolescents, on the other hand, will surely help to curtail pre-diabetes/diabetes conditions among adolescents in India. Adolescent sub-populations are out of the coverage of the special programme that addresses the crucial public health issues of diabetes and related various risk factors.
Acknowledgments
The authors are thankful to the Population Council (India) for providing the data for this study. The authors are also thankful to Aditya and Megha Mittal for providing financial support to carry out the CNNS. Their generous support enabled us to utilize the highest quality and innovative methods for conducting the world’s largest comprehensive nutrition survey. The authors also thankful to Dr. Sahana Nagaraj for her insightful comments and suggestions to improve the quality of the paper.
Abbreviations
- MoHFW
Ministry of Health and Family Welfare
- UNICEF
United Nations Children Funds
- CNNS
Comprehensive National Nutrition Survey
- BMI
Body Mass Index
- HbA1c
Glycosylated haemoglobin
- T1D
Type-1 diabetes
- T2D
Type-2 diabetes
- GDM
Gestational diabetes mellitus
- TSFT
Triceps skinfold thickness
- SSFT
Subscapular skinfold thickness
- LDL
Low-density lipoprotein
- HDL
High-density lipoprotein
- SC/ST
Scheduled Tribe/Scheduled Caste
Authors’ contributions
The concept was drafted by SS; PK and SS contributed to the analysis design; PSM and SS advised on the paper and assisted in paper conceptualization; PSM, PK, and SS contributed to the comprehensive writing of the article. All authors read and approved the final manuscript.
Funding
Authors did not receive any funding to carry out this research.
Availability of data and materials
We have provided details of the data in the methodology section. The CNNS data can be obtained on request from the Population Council, Delhi (India). The report and the survey tools are also available on the website: https://www.popcouncil.org/uploads/pdfs/2019RH_CNNSreport.pdf and cnns.pc@gmail.com respectively.
Declarations
Ethics approval and consent to participate
The study is based on secondary data which is publically available on request from cnns.pc@gmail.com. Therefore ethical approval and consent to participate are not required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pradeep Kumar, Email: pradeepiips@yahoo.com.
Shobhit Srivastava, Email: shobhitsrivastava889@gmail.com.
Prem Shankar Mishra, Email: psmishrabhu@gmail.com.
E. T. Krishnan Mooss, Email: dretkmooss@gmail.com.
References
- 1.IDF . IDF DIABETES ATLAS Eighth edition 2017. 2017. [Google Scholar]
- 2.Tester J, Sharma S, Bradner C, et al. Diabetes & Metabolic Syndrome : Clinical Research & Reviews Gender differences in prediabetes and insulin resistance among 1356 obese children in northern California. Diabetes Metab Syndr Clin Res Rev. 2013;7(3):161–165. doi: 10.1016/j.dsx.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 3.WHO . Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity Report of the Ad hoc Working Group on Science and Evidence for Ending Childhood Obesity. Geneva: World Health Organization; 2016. pp. 1–218. [Google Scholar]
- 4.Dandona L, India State-Level Disease Burden Initiative Collaborators (167 authors) Nations within a nation : variations in epidemiological transition across the states of India , 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IIPS and ICF . National Family Health Survey (NFHS-4), 2015–16. Mumbai, India. 2017. [Google Scholar]
- 6.Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;6736:1–13. doi: 10.1016/S0140-6736(17)30058-2. [DOI] [PubMed] [Google Scholar]
- 7.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, Rao PV, Yajnik CS, Prasanna Kumar KM, Nair JD, Diabetes Epidemiology Study Group in India (DESI) High prevalence of diabetes and impaired glucose tolerance in India : National Urban Diabetes Survey. Diabetologia. 2001;44(9):1094–1101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 8.Hills PAP, Arena PR, Kamlesh P, et al. Series type 2 diabetes in South Asia 1 epidemiology and determinants of type 2 diabetes in. Lancet Diabetes Endocrinol. 2018;8587:1–13. doi: 10.1016/S2213-8587(18)30204-3. [DOI] [PubMed] [Google Scholar]
- 9.Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. 2011. pp. 866–870. [DOI] [PubMed] [Google Scholar]
- 10.Kumar B, Robinson R, Till S. Physical activity and health in adolescence. Clin Med. 2015;15:267–272. doi: 10.7861/clinmedicine.15-3-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lahiri A, Chakraborty A, Dasgupta U, Roy AKS, Bhattacharyya K. Effect of dietary habit and physical activity on Overnutrition of Schoolgoing adolescents : a longitudinal assessment in a rural block of West Bengal. Indian J Public Health. 2019;63(3):171–177. doi: 10.4103/ijph.IJPH_159_19. [DOI] [PubMed] [Google Scholar]
- 12.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance ( IDPP-1 ) Diabetologia. 2006;49:289–297. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 13.Ujuanbi SA, Mezie-Okoye MM. Prevalence of overaweight and obeisty among adolescents in secondary schools in an urban city in Niger Delta region, Nigeria. Nig Del Med J. 2019;3(4):22–30.
- 14.Ojo O, Wang X, Ojo OO, et al. The effects of substance abuse on blood glucose parameters in patients with diabetes : a systematic review and Meta-analysis. Int J Environ Res Public Heal. 2018;15:1–16. doi: 10.3390/ijerph15122691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vennu V, Abdulrahman TA, Bindawas SM. The prevalence of overweight, obesity , hypertension , and diabetes in India: analysis of the 2015–2016 national family health survey. Int J Environ Res Public Heal. 2019;16:1–22. doi: 10.3390/ijerph16203987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anjana RM, Deepa M, Pradeepa R, et al. Prevalence of diabetes and prediabetes in 15 states of India : results from the ICMR – INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–596. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 17.Gupta N, Shah P, Nayyar S, Misra A. Childhood obesity and the metabolic syndrome in developing countries. Indian J Pediatr. 2013;80(S1):28–37. doi: 10.1007/s12098-012-0923-5. [DOI] [PubMed] [Google Scholar]
- 18.Patterson CC, Dahlquist GG, Gyürüs E, et al. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20 : a multicentre prospective registration study. Lancet. 2005;373:2027–2033. doi: 10.1016/S0140-6736(09)60568-7. [DOI] [PubMed] [Google Scholar]
- 19.Srinivasan M. Sudha, Pescatello S. Linda BNA. Current perspectives on physical activity and exercise recommendations for children Spectrum disorders. Am Phys Ther Assoc. 2014;94(6):875–889. doi: 10.2522/ptj.20130157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farah BQ, Andrade-Lima A, Germano-Soares AH, Christofaro DGD, Virgı’lio Gomes de Barros M, do Prado WL, Ritti-Dias RM. Physical activity and heart rate variability in adolescents with abdominal obesity. Pediatr Cardiol. 2018;39(3):466–472. doi: 10.1007/s00246-017-1775-6. [DOI] [PubMed] [Google Scholar]
- 21.Pradeepa R, Anjana RM, Joshi SR, et al. Prevalence of generalized & abdominal obesity in urban & rural. Indian J Med Res. 2015;14:139–150. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khaodhiar L, Cummings S, Apovian CM. Treating diabetes and prediabetes by focusing on obesity management. Curr Diab Rep. 2009;9(5):348–354. doi: 10.1007/s11892-009-0055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al Amiri E, Abdullatif M, Abdulle A, et al. The prevalence, risk factors, and screening measure for prediabetes and diabetes among Emirati overweight/obese children and adolescents. BMC Public Health. 2015. 10.1186/s12889-015-2649-6. [DOI] [PMC free article] [PubMed]
- 24.Kelishadi R, Growth C. Childhood overweight , obesity , and the metabolic syndrome in developing countries. 2014. [DOI] [PubMed] [Google Scholar]
- 25.Alam DS, Talukder SH, Chowdhury MAH, et al. Overweight and abdominal obesity as determinants of undiagnosed diabetes and pre-diabetes in Bangladesh. BMC Obes. 2016;3:1–2. doi: 10.1186/s40608-016-0099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, et al. Prevalence of diabetes and prediabetes ( impaired fasting glucose and / or impaired glucose tolerance ) in urban and rural India : Phase I results of the Indian Council of Medical Research – INdia DIABetes ( ICMR – INDIAB ) study. Diabetologia. 2011;54(12):3022–3027. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 27.Alam DS, Talukder SH, Chowdhury MAH, Siddiquee AT, Ahmed S, Pervin S, Khan S, Hasan K, Koehlmoos TLP, Niessen LW. Overweight and abdominal obesity as determinants of undiagnosed diabetes and pre-diabetes in Bangladesh. BMC Obes. 2016;3(1):19. doi: 10.1186/S40608-016-0099-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ganvir RH, Bhalla AK, Dayal D. Growth attainments of Indian children with type 1 diabetes: a mixed longitudinal study. Indian J Pediatr. 2015. 10.1007/s12098-014-1466-8. [DOI] [PubMed]
- 29.Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF and Population Council. Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi. 2019;1–290.
- 30.WHO . Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus Abbreviated Report of a WHO Consultation. 2011. [PubMed] [Google Scholar]
- 31.Sherwani SI, Khan HA, Ekhzaimy A, et al. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights. 2016. 10.4137/Bmi.s38440. [DOI] [PMC free article] [PubMed]
- 32.Rani JS. Significance of HbA1c test is a stable indicator of triglycerides in diagnosis and prognosis of diabetic patients. Int J Res Med Sci. 2020. 10.18203/2320-6012.ijrms20204894.
- 33.McPherson RA, Pincus MR. Chapter 16: Carbohydrates. In: Henry’s clinical diagnosis and management by laboratory methods. 22. 2011. pp. 210–225. [Google Scholar]
- 34.International Diabetes Federation . Globall IDF/IPAD Guideline for Diabetes in childhood and adolescence. 2011. [Google Scholar]
- 35.Must A, Anderson SE. Body mass index in children and adolescents: Considerations for population-based applications. Int J Obes. 2006;30(4):590–594. doi: 10.1038/sj.ijo.0803300. [DOI] [PubMed] [Google Scholar]
- 36.Kumar P, Dhillon P. Length of stay after childbirth in India : a comparative study of public and private health institutions. BMC Pregnancy Childbirth. 2020;20:1–13. doi: 10.1186/s12884-020-2839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mohan B, Verma A, Singh K, et al. Prevalence of sustained hypertension and obesity among urban and rural adolescents : a school-based , cross- sectional study in North India. BMJ Open. 2019;9:1–9. doi: 10.1136/bmjopen-2019-030833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim HM, Park J, Kim H, et al. Prevalence of the metabolic syndrome in Korean adolescents aged 12–19 years from the Korean National Health and Nutrition Examination Survey 1998 and 2001. Diabetes Res Clin Pract. 2007;75(1):111–114. doi: 10.1016/j.diabres.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 39.Lambert M, Paradis G, Loughlin JO, et al. PEDIATRIC HIGHLIGHT Insulin resistance syndrome in a representative sample of children and adolescents from Quebec, Canada. 2004. [DOI] [PubMed] [Google Scholar]
- 40.Cruz ML, Weigensberg MJ, Huang TT, et al. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrinol Metab. 2004;89(1):108–113. doi: 10.1210/jc.2003-031188. [DOI] [PubMed] [Google Scholar]
- 41.Thomas AS, Greene LF, Ard JD, Oster RA, Darnell BE, Gower BA. Physical activity may facilitate diabetes prevention in adolescents. Diabetes Care. 2009;32(1):9–13. doi: 10.2337/dc08-0780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee YS. Consequences of childhood obesity. Ann Acad Med Singap. 2009;38:75–81. [PubMed] [Google Scholar]
- 43.Daniels SR. Complications of obesity in children and adolescents. Int J Obes. 2009;33:S60–S65. doi: 10.1038/ijo.2009.20. [DOI] [PubMed] [Google Scholar]
- 44.Gold MA, Gladstein J. Substance use among adolescents with diabetes mellitus: preliminary findings. J Adolesc Heal. 1993;14(2):80–84. doi: 10.1016/1054-139X(93)90089-8. [DOI] [PubMed] [Google Scholar]
- 45.Zamora-Kapoor A, Fyfe-Johnson A, Omidpanah A, et al. Risk factors for pre-diabetes and diabetes in adolescence and their variability by race and ethnicity. Prev Med (Baltim). 2018. 10.1016/j.ypmed.2018.08.015. [DOI] [PMC free article] [PubMed]
- 46.Khan MMA, Karim M, Islam AZ, Islam MR, Khan HTA, Khalilullah MI. Prevalence of overweight and obesity among adolescents in Bangladesh: do eating habits and physical activity have a gender differential effect? J Biosoc Sci. 2019;51(6):843–856. doi: 10.1017/S0021932019000142. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
We have provided details of the data in the methodology section. The CNNS data can be obtained on request from the Population Council, Delhi (India). The report and the survey tools are also available on the website: https://www.popcouncil.org/uploads/pdfs/2019RH_CNNSreport.pdf and cnns.pc@gmail.com respectively.