Abstract
Objective:
To investigate the joint associations of amounts of alcohol consumed and drinking habits with risks of all-cause mortality and cause-specific mortality.
Patient and methods:
A total of 316,627 healthy current drinkers, with baseline measurements between March 13, 2006, and October 1, 2010, were included in this study. We newly created a drinking habit score (DHS) according to regular drinking (frequency of alcohol intake ≥ 3 days/week) and whether consuming alcohol intake with meals (yes).
Results:
During a median follow-up of 8.9 years, we documented 8652 incident cases of all-cause death, including 1,702 cases of cardiovascular diseases (CVD) death, 4,960 cases of caner (CA) death and 1,990 cases of other-causes death. After adjustment confounders and amount of alcohol consumed, higher DHS was significantly associated with a lower risk of all-cause mortality, CVD mortality, CA mortality or other-causes mortality (P-trend<.001, P-trend=.03, P-trend<.001, P-trend<.001, respectively). We observed that amount of alcohol consumed have different relationships with risks of all-cause mortality and cause-specific mortality among participants with distinct drinking habits, grouped by DHS. For example, in the joint analyses, a J-shaped association between amount of alcohol consumed and all-cause mortality was observed in participants with unfavorable DHS (P-quadratic trend=.02); while the association appeared to be U-shaped in participants with favorable DHS (P-quadratic trend=.003), with lower risks among those consuming more than 50 g/week and less than 300g/week.
Conclusions:
Our results indicate that alcohol consumption levels have different relationships with risk of mortality among current drinkers depending on their drinking habits.
Keywords: Drinking habits, alcohol intake, mortality
INTRODUCTION
The associations between excessive alcohol consumption and higher risks of all-cause mortality and cause-specific mortality have been well established1–3. However, the relationship between moderate alcohol consumption and mortality is controversial. A wealth of previous epidemiological studies have shown that moderate-drinkers have lower risks of all-cause mortality and CVD mortality as compared with non-drinkers1–4, but not all5–7.
Of note, such previous studies only analyzed the amount of alcohol consumed, without considering drinking habits that may modify the associations of amount of alcohol consumed with health outcomes8–15. Several previous studies showed that more frequent episodes of drinking were associated with lower risks of diabetes, coronary heart disease, and all-cause mortality independent of the amount of alcohol consumed8–11,15. In addition, alcohol drinking with meals may in the short term slow the absorption of alcohol and reduce the overall hyperglycemic properties of alcohol or a mixed meal and, in the long term, lower risk of cardiovascular disease or all-cause mortality compared to drinking alcohol outside of meals12–14. However, these drinking habits are usually studied individually, no study has evaluated the combined impact of these drinking habits factors on the risk of mortality outcomes in a large prospective cohort.
Notably, debates are growing regarding the inverse association of moderate alcohol consumption with risk of mortality due to several methodological limitations16–20. For example, using non-drinkers as reference group may introduce selection bias to the associations, and augment potential confounding due to systematic differences in lifestyle, socioeconomic status or unmeasured factors between drinkers and non-drinkers. Therefore, analysis of the alcohol-mortality relation across the intake spectrum among drinkers may minimize such bias5.
Therefore, we studied these associations in a prospective study of 316,627 current alcohol drinkers from the UK Biobank. To capture overall drinking habits, we characterized drinking habits by considering both frequency of alcohol intake and whether alcohol was consumed with meals. We evaluated the association of overall drinking habits with risk of all-cause mortality and cause-specific mortality. We also analyzed the joint associations of alcohol consumption (actual and genetically determined) and drinking habits with risks of all-cause mortality and cause-specific mortality.
METHODS
Study population
The study design of the UK Biobank has been previously described elsewhere21. In brief, more than 500,000 participants aged 37–73 years were recruited from 22 assessment centers across the United Kingdom in 2006–2010. In this study, the inclusion criteria were as follows: (1) current alcohol drinkers (current alcohol drinkers were defined by who indicated they drink alcohol based on alcohol intake frequency questionnaire and alcohol consumed >0g/week), (2) participants without cardiovascular disease or cancer at baseline, (3) participants who have complete data on drinking habits, (4) participants who did not reduce their alcohol consumption due to illness or doctor’s advice, and (5) women included were non-pregnant. A total of 316,627 participants were included in the final analysis.
Assessment of drinking habits and amount of alcohol consumed
Participants were asked “How often do you drink alcohol?” through a touch-screen questionnaire (answers: “prefer not to answer”, “never”, “special occasions only”, “one to three times a month”, “once or twice a week”, “three or four times a week”, “daily or almost daily”). Current drinkers were further asked to report their usual average weekly consumption (or average monthly consumption for participants who indicated they drink alcohol on special occasions or one to three times a month.). Alcohol intake (g/week) was calculated by the quantity of each type of drink (red wine, white wine, beer/cider, fortified wine, and spirits) multiplied by its standard drink size and reference alcohol content (1 unit-equivalent described as containing 8g of pure alcohol; 125ml wine=1.6 units-equivalents, 1 pint beer =2.6 units-equivalents, 25ml spirits=1 unit-equivalent, 62.5ml fortified wine=1 unit-equivalent). In the main analysis, we categorized weekly alcohol intake in grams into five categories: >0–<50 (reference), ≥50–<100, ≥100–<200, ≥200– <300 and ≥300 g per week.
Other information about alcohol intake was obtained with the following questions. First, current drinkers were asked “When you drink alcohol is it usually with meals?” (“yes”, “no”, “it varies”, “do not know”, “prefer not to answer”); second, participants were asked “Compared to 10 years ago, do you drink?” Participants selected an the option from, “More nowadays”, “about the same”, “less nowadays”, “do not know”, “prefer not to answer”, if participants indicated they drank less nowadays than 10 years ago, they were asked the reason for reducing amount of alcohol drunk (“illness or ill health”, “doctor’s advice”, “health precaution”, “financial reasons”, “other reasons”, “do not know”, “prefer not to answer”).
Drinking Habit Score
According to previous studies, a healthy drinking habits score was defined by regular drinking (frequency of alcohol intake ≥ 3 days/week)22,23 and consuming alcohol intake with meals (participant who indicated they drink alcohol with meals). One point was given for each favorable drinking habits (range, 0–2).
Ascertainment of all-cause mortality and cause-specific mortality
Information on death and death date were provided by the National Health Service (NHS) Information Centre (England and Wales) and NHS Central Register Scotland (Scotland). End of follow-up for the main study for each participant was recorded as or the date of end of follow-up or the date of lose to follow-up or the date of death for the assessment center attended, whichever came first. The underlying cause of death was determined according to the ICD-10 (International Classification of Disease, 10th revised edition). Causes of deaths were classified as CVD with ICD-10 code of I00-I99 and cancer (CA) with code of C00-D48. Details of the assessment of mortality have been described previously (https://biobank.ctsu.ox.ac.uk/showcase/field.cgi?id=40000).
Statistical Analysis
Chi-square test for categorical variables and general linear models for continuous variables (except for amounts of alcohol consumed) were applied to compare proportions or means of characteristics between participants with different drinking habits (with vs. without meal, and regular vs. non-regular drinkers). Mann–Whitney U test was used to compared to median of amounts of alcohol intake between participants with different drinking habits. The associations between drinking habits and mortality were explored using Cox-proportional hazard models. We adjusted for several potential confounders including age (years), sex (women or men), assessment centres, race (White European, Mixed, Asian, Black, Others), Townsend deprivation index (quintiles), BMI (kg/m2), smoking status (current, past, never), physical activity (MET minutes/week), healthy diet (yes or no), diabetes (yes or no), hypertension (yes or no), and high cholesterol (yes or no). Details of the assessment of covariates are described in Supplemental Materials. We created a genetic risk score (GRS) for amount of alcohol consumed using 90 single nucleotide polymorphisms (SNPs),which passed quality control, based on previous studies24 (Supplementary Table 1). Details of the genotyping and calculation of genetic risk score are also described in Supplemental Materials. For analyses about genetic data, we also adjusted for the first 10 genetic principal components, genotyping array (106 batches) and the third-degree relatedness. If covariate information was missing (all covariates <1% missing in the current study), missing data were coded as a missing indicator category for categorical variables and with mean values for continuous variables. The modifying effect of healthy drinking habit score on the association between alcohol consumption and risk of death was tested by including a cross-product term of the healthy drinking habit score with levels of amount of alcohol consumed (categorical variable). The proportional hazards assumption was tested by Kaplan-Meier method and Schoenfeld residuals method. We conducted tests of linear trend by assigning the median of amount of alcohol consumed within each group and modeling this variable continuously. To test departure from linearity, a linear and a quadratic term were included in the model.
To validate our results, we performed a 10-fold cross-validation analysis. The cohort was randomly divided into 10 batches. In each run, one of the 10 samples was used as the testing data. The Cox regression was applied to the testing data to evaluate associations between DHS and mortality. The process was repeated 10 times, with each of the 10 samples used once as the testing data. A fixed‐ effects meta‐ analysis was conducted to obtain the comprehensive HR of these 10 groups.
All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc) and SPSS (22.0). All statistical tests were two sided, and we considered P<.05 to be statistically significant.
Results
Baseline characteristics of the study participants
Baseline characteristics of participants according to drinking habits are shown in Table 1. Compared with participants who consumed alcohol outside of meals and those who had varying patterns (with answer as “It varied” in the questionnaire), participants who consumed alcohol with meals drank less alcohol overall, were more likely to be women; be non-current smokers; have a healthy diet; have lower BMI, Townsend deprivation index, physical activity levels; and have lower prevalence of diabetes, hypertension and high cholesterol. Compared with non-regular drinkers (< 3 times/week), regular drinkers (≧3 times/week) consumed more alcohol overall; more likely to be men and current smokers; and tended to have lower BMI, Townsend deprivation index, physical activity, and prevalence of diabetes, but higher prevalence of hypertension and high cholesterol.
Table 1.
Baseline characteristics according to drinking habit factor.
| With meal | Without meal or it varies | Regular drinkers | Non-regular drinkers | |
|---|---|---|---|---|
| N | 138,862 (43.9) | 177,765 (56.1) | 183,898 (58.1) | 132,729 (41.9) |
| Age, years (SD) | 57.1 (7.8) | 55.0 (8.1)a | 56.4 (7.9) | 55.2 (8.2)b |
| Women | 82,455 (59.4) | 78,800 (44.3)a | 85,782 (46.6) | 75,473 (56.9)b |
| Whites | 133,109 (95.9) | 171,222 (96.3)a | 179,332 (97.5) | 124,999 (94.2)b |
| BMI, kg/m2 (SD) | 26.6 (4.3) | 27.4 (4.5)a | 26.7 (4.1) | 27.5 (4.7)b |
| Physical activity, MET, minutes/week (SD) | 2677.5 (3279.4) | 2928.0 (3919.9)a | 2768.0 (3575.8) | 2887.6 (3760.7) |
| Current smoker | 8,469 (6.1) | 23,684 (13.3)a | 19,906 (10.8) | 12,247 (9.2)b |
| Healthy diet | 105,634 (76.1) | 119,600 (67.3)a | 129,701 (70.5) | 95,533 (72.0)b |
| TDI | −1.9 (2.7) | −1.4 (3.0)a | −1.7 (2.8) | −1.4 (3.0)b |
| Total alcohol intake, g/week, median (5th–95th Percentiles) | 89.6 (12.8–318.4) | 129.6a (16.0–499.2) | 166.4 (59.2–518.4) | 51.2b (6.4–195.2) |
| Disease status | ||||
| Diabetes | 4,284 (3.1) | 5,981 (3.4)a | 5,181 (2.8) | 5,084 (3.8)b |
| Hypertension | 72,389 (52.1) | 96,496 (54.3)a | 101,598 (55.2) | 67,287 (50.7)b |
| High cholesterol | 18,389 (13.2) | 24,249 (13.6)a | 25,245 (13.7) | 17,393 (13.1)b |
Data are n (%) unless otherwise indicated
compared with “with meal” group, the P-value<.05;
compared with “regular drinker” group, the P-value<.05;
The associations between drinking habits and all-cause mortality and cause-specific mortality
During a median follow-up of 8.9 years, we documented 8652 incident cases of all-cause death, including 1,702 cases of CVD death, 4,960 cases of CA death and 1,990 cases of other-causes death. After adjustment for potential confounders and amounts of alcohol consumed, regular drinking (frequency of alcohol intake≧3 times/week) were significantly associated with a 7% lower risk of all-cause mortality (HR, 95 % CI, 0.93, 0.88–0.99) and 8% lower risk of CA mortality (HR, 95 % CI, 0.92, 0.85–0.99) as compared with non-regular drinking (frequency of alcohol intake<3 times/week) (Table 2). Similarly, compared with participants who consumed alcohol outside of meals and those who had varying patterns, participants who consumed alcohol with meals have a significantly 12 % lower risk of all-cause mortality (HR, 95 % CI, 0.88, 0.84–0.93), 13% lower risk of CVD mortality (HR, 95 % CI, 0.87, 0.78–0.97), 10% lower risk of CA mortality (HR, 95 % CI, 0.90, 0.85–0.95) and 14% lower risk of other-causes mortality (HR, 95 % CI, 0.86, 0.78–0.94) (Table 2).
Table 2.
The association between individual drinking habits and all-cause mortality and cause specific mortality.
| Frequency of alcohol intake | Whether consumed alcohol with meal | |||
|---|---|---|---|---|
| All-cause mortality | Non-regular | Regular | No or it varied | Yes |
| No, death | 3,245 | 5,407 | 5,331 | 3,321 |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.00 (0.96–1.05) | 1 (reference) | 0.86 (0.84–0.90) |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.93 (0.88–0.99) | 1 (reference) | 0.88 (0.84–0.93) |
| CVD mortality | Non-regular | Regular | No or it varied | Yes |
| No, death | 660 | 1,042 | 1.092 | 610 |
| Model 1 (HR, 95%, CI) | 1 (reference) | 0.95 (0.86–1.05) | 1 (reference) | 0.87 (0.79–0.97) |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.99 (0.87–1.13) | 1 (reference) | 0.87 (0.78–0.97) |
| CA mortality | Non-regular | Regular | No or it varied | Yes |
| No, death | 1,820 | 3,140 | 2,983 | 1,977 |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.04 (0.98–1.11) | 1 (reference) | 0.87 (0.82–0.92) |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.92 (0.85–0.99) | 1 (reference) | 0.90 (0.85–0.95) |
| Other reason | Non-regular | Regular | No or it varied | Yes |
| No, death | 765 | 1,225 | 1.256 | 734 |
| Model 1 (HR, 95%, CI) | 1 (reference) | 0.95 (0.87–1.04) | 1 (reference) | 0.83 (0.76–0.92) |
| Model 1+ alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.91 (0.81–1.03) | 1 (reference) | 0.86 (0.78–0.94) |
Model 1 adjusted for age, sex, race, assessment centres, BMI, physical activity, smoking (never, past, current), healthy diet, Townsend deprivation index, diabetes, hypertension, high cholesterol, whether consumed alcohol with meal or regular drinking.
To better capture the overall drinking habits, we developed a DHS that combined frequency of alcohol intake (regular drinking, ≧3 times/week) and whether alcohol was consumed with meals (with meals). The DHS showed significantly and consistently inverse associations with risks of all-cause mortality (P-trend<.001), CVD mortality (P-trend=.03), CA mortality (P-trend<.001) and other-causes mortality (P-trend<.001). For example, compared with participants with a low DHS (DHS=0, unhealthy drinking habits), the multivariable adjusted HRs for all-cause mortality were 0.96 (95% CI, 0.90–1.01) for participants with an intermediate DHS (DHS=1), and 0.82 (95% CI, 0.76–0.88) for participants with a high DHS (DHS=2, healthy drinking habits). (Table 3).
Table 3.
The association between drinking habits score (DHS) and all-cause mortality and cause specific mortality.
| Drinking habits score (DHS) | ||||
|---|---|---|---|---|
| All-cause mortality | 0 | 1 | 2 | P-trend |
| No, death | 1,927 | 4,722 | 2003 | |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.03 (0.97–1.09) | 0.87 (0.81–0.92) | <0.001 |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.96 (0.90–1.01) | 0.82 (0.76–0.88) | <0.001 |
| CVD mortality | 0 | 1 | 2 | P-trend |
| No, death | 403 | 946 | 353 | |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.01 (0.90–1.14) | 0.82 (0.71–0.95) | 0.010 |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 1.00 (0.88–1.14) | 0.84 (0.72–0.99) | 0.032 |
| CA mortality | 0 | 1 | 2 | P-trend |
| No, death | 1,079 | 2,645 | 1,236 | |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.02 (0.95–1.09) | 0.91 (0.84–0.99) | 0.021 |
| Model 1+alcohol intake level (HR, 95%, CI) | 1 (reference) | 0.92 (0.85–0.99) | 0.82 (0.75–0.90) | <0.001 |
| Other reason | 0 | 1 | 2 | P-trend |
| No, death | 445 | 1131 | 414 | |
| Model 1 (HR, 95%, CI) | 1 (reference) | 1.07 (0.96–1.20) | 0.79 (0.69–0.90) | <0.001 |
| Model 1+ alcohol intake level (HR, 95%, CI) | 1 (reference) | 1.01 (0.90–1.14) | 0.77 (0.67–0.90) | <0.001 |
Model 1 adjusted for age, sex, race, assessment centres, BMI, physical activity, smoking (never, past, current), healthy diet, Townsend deprivation index, diabetes, hypertension and high cholesterol.
Model 2 further adjusted alcohol intake level on the basis of model 1.
In stratified analyses by the potential confounders including sex, age, socioeconomic level (Townsend deprivation index), healthy lifestyle score and predominantly wine drinkers (predominantly wine drinkers was defined as the maximum baseline consumption grams/week for each alcohol type)5 (Supplementary Figure 1A–D). We observed significantly and consistently interactions between healthy drinking habits (unfavorable vs. favorable) and TDI (a greater TDI implies a lower levels of socioeconomic) on the risks of all-cause mortality, CVD mortality and CA mortality (P-interaction<.001, P-interaction=.01, and P-interaction=.01, respectively), and the inverse associations between healthy drinking habits and risk of mortality appeared to be more stronger in participants with low socioeconomic level as compared with participants with high socioeconomic level. We did not find significant interactions between healthy drinking habits and other risk factors on risk of all-cause mortality or cause-specific mortality.
We further conducted cross-validation analysis to evaluate the robustness of our findings. The results of the association between DHS and the risks of all-cause mortality and cause-specific mortality in the cross-validation analysis are shown in the Supplementary Table 2. The validation tests showed consistently significant results as in the current analysis.
The joint association of actual amount of alcohol intake and overall drinking habits with risk of mortality
We observed a positive and curvilinear association between the amount of alcohol consumed and all-cause mortality (P-quadratic trend=.001), as compared with the lowest level of alcohol amount (>0-<50g/week), “moderate alcohol intake” (50g-200g/week) was not associated with all-cause mortality, while high intake (≥300g/week) was associated with a significantly higher risk of all-cause mortality (1.33, 95% CI, 1.23–1.45). (Figure 1A). Because the intermediate DHS (DHS=1) group had similar risk of mortality to the unhealthy DHS (DHS=0) group, we combined these two groups to maximize statistical power. The joint analysis of amount of alcohol consumed and drinking habits score indicated that amount of alcohol consumed was related to risk of all-cause mortality differently based on drinking habits (p-interaction=.009) (Figure 2A). A J-shaped association between amount of alcohol consumed and mortality was observed in participants with unfavorable DHS (DHS≦1) (P-quadratic trend =.02), while the association appeared to be U-shaped (P-quadratic trend=.003) in participant with favorable DHS (DHS=2), with consistently and significantly lower risks among those consuming more than 50 g/week and less than 300g/week (Hazard ratios was 0.90, 95% CI, 0.81–0.995 for category of ≥50-<100g/week; 0.85, 95% CI, 0.78–0.93 for category of ≥100-<200g/week; 0.84, 95% CI, 0.75–0.95 for category of ≥200-<300g/week) as compared with participants who had the lowest amount of alcohol consumed and unfavorable DHS.
Figure 1.
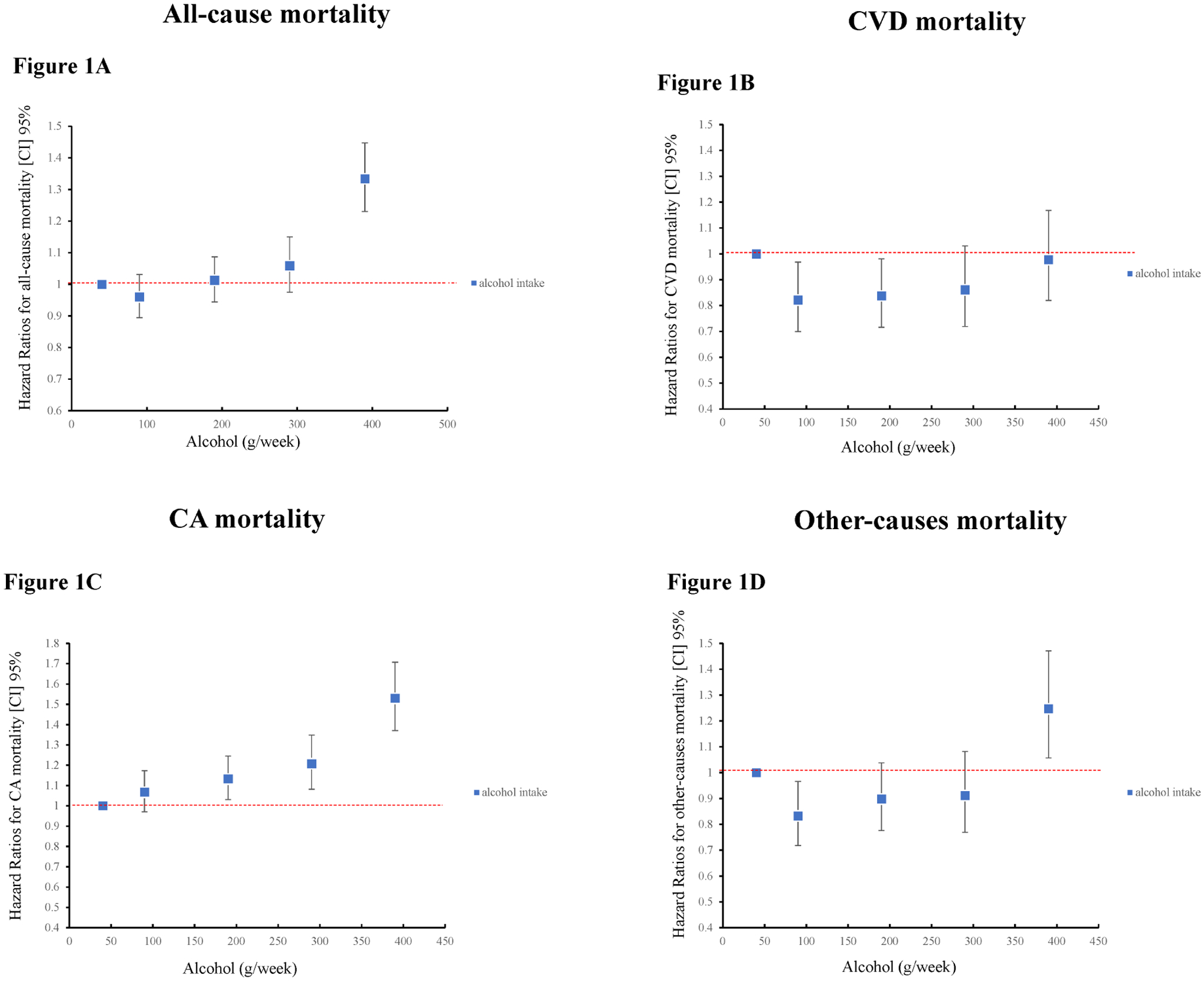
The association of amount of alcohol intake with risks of all-cause mortality and cause-specific mortality.
Results were adjusted age, sex, race, assessment centres, BMI, physical activity, smoking (never, past, current), healthy diet, Townsend deprivation index, diabetes, hypertension, high cholesterol and DHS.
Figure 2.
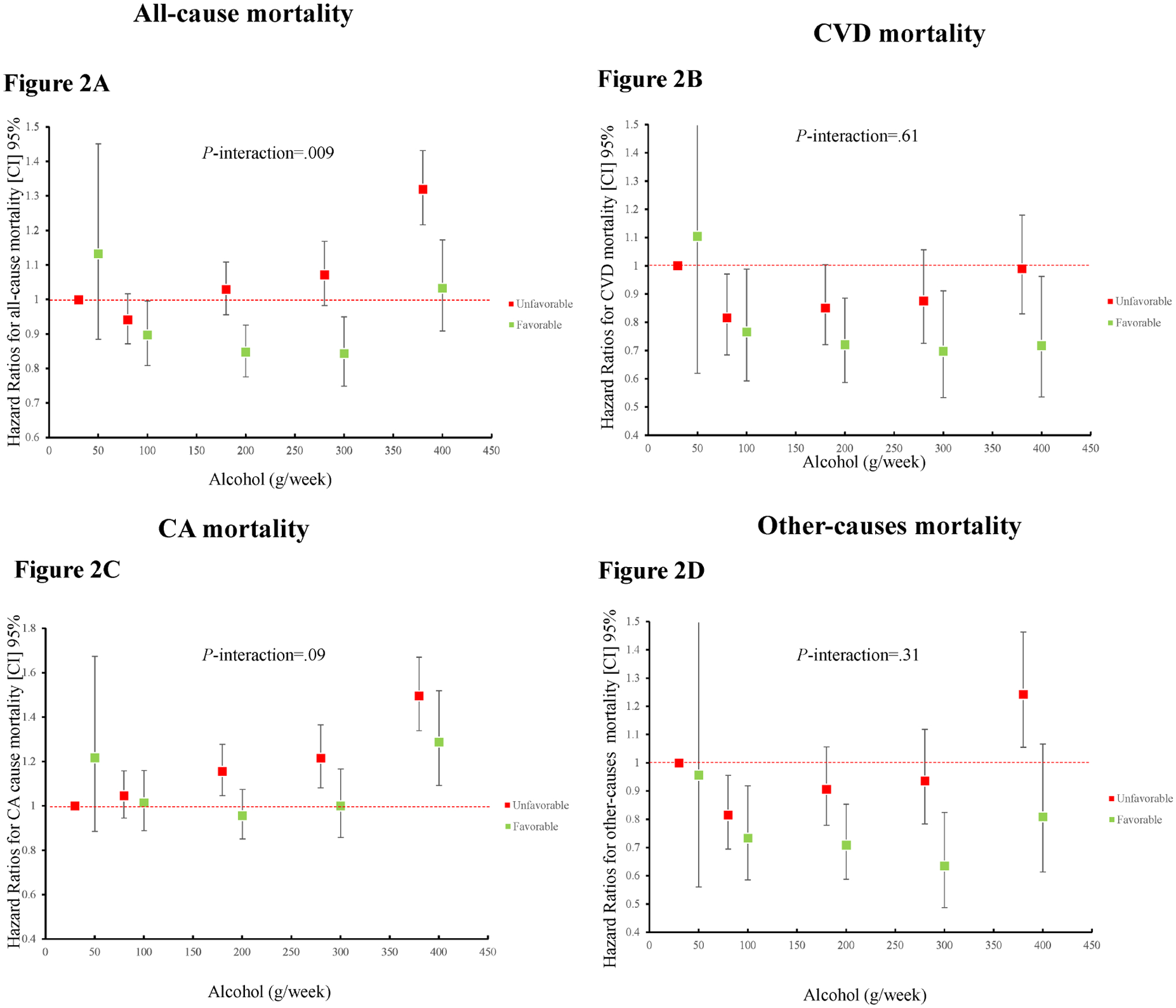
The joint association of amount of alcohol intake and drinking habits score in relation to risks of all-cause mortality and cause-specific mortality.
Results were adjusted age, sex, race, assessment centres, BMI, physical activity, smoking (never, past, current), healthy diet, Townsend deprivation index, diabetes, hypertension, high cholesterol.
We observed that amount of alcohol consumed showed distinct associations with risks of different types of cause-specific mortality [a U-shaped for CVD mortality (P-quadratic trend=.01); a positive linear association for CA mortality (P-linear trend<.001); a J-shaped association for other-causes mortality (P-quadratic trend=.001), Figure 1B, 1C and 1D]. Next, the joint analyses indicated that such associations were differently based on drinking habits (Figure 2B, 2C and 2D), though the interactions did not reach significant level. For CVD mortality, a U-shaped association was observed in participants with unfavorable DHS, while a reverse J-shaped association was observed in participants with favorable DHS. For CA mortality, a positive linear association was as observed in participants with unfavorable DHS, while a U-shaped association was observed in participants with favorable DHS. Of note, “moderate alcohol intake” (50g–200g/week) was not associated with CA mortality in participants with favorable DHS. For other-causes mortality, a J-shaped association was observed in participants with unfavorable DHS, while a U-shaped association was observed in participants with favorable DHS.
We also repeated the joint analyses in women and men, respectively (Supplementary Figure 2 and 3), and the results were similar to the results in the total population. Similar results were also observed after including never drinkers and past drinkers and using never drinkers as the reference group (Supplementary Figure 4).
The joint association of genetically determined alcohol intake levels (ALC-GRS) and overall drinking habits with risk of mortality
Genetic data were available for 296,072 participants of European descent in this study. After adjustment for potential confounders, the first 10 genetic principal components, the third-degree relatedness and genotyping array, higher ALC-GRS was marginally associated with an increased risk of all-cause mortality (p-trend=.048), but not associated with CVD mortality, CA mortality and other-causes mortality (Supplementary Figure 5). In the joint analysis, higher DHS was significantly associated with lower risk all-cause mortality and each cause-specific mortality independent of ALC-GRS. We did not find significant interaction between DHS and ALC-GRS on all-cause mortality or cause-specific mortality (Supplementary Figure 5).
Discussion
In this prospective cohort study of 316,627 current drinkers from the UK Biobank, we found that healthy drinking habits (regular drinking and drinking with meal), as estimated by DHS, were associated with lower risks of all-cause mortality and cause-specific mortality independent of amount of alcohol consumed. Reporting for the first time, we found that drinking habits significantly modified the relations between the actual amounts of alcohol intake and risk of all-cause mortality, while no interaction was observed between drinking habits and genetically determined alcohol intake levels. Similar interaction patterns were observed for cause-specific mortality.
Our findings that regular drinking and drinking with meals were associated with a lower risk of mortality are consistent with previous studies. A body of data have shown that drinking habits were related to the risk of mortality or diseases including cardiovascular disease, diabetes and liver cirrhosis, independent of amount of alcohol consumed8–14,25–28. In the Health Professionals Follow-up Study, regular drinking (consumed alcohol intake at least 3–4 days per week) was associated with lower risks of coronary heart disease and type 2 diabetes9,15. In a cohort of 26,909 men and 29,626 women from Denmark, mortality rate was higher among non-frequent drinkers compared with regular and frequent drinkers at similar level of alcohol intake10. In the Million Women Study, habitually consuming alcohol with meals was associated with a 31% lower risk of liver cirrhosis after adjustment for amount consumed28. In the Risk Factors and Life Expectancy Study, participants who usually consumed alcohol with meals had lower mortality than those consumed alcohol outside of meals after adjustment for amount of alcohol consumed13. Of note, drinking habits, though often correlated because people follow common drinking patterns, were studied individually in previous studies29. Our study for the first time evaluated the association between a combination of multiple drinking habits, assessed as DHS, and risk of all-cause mortality and cause-specific mortality.
In this study, we observed that amount of alcohol consumed showed a J-shaped association with all-cause mortality, a U-shaped association with CVD mortality and a positive linear association with CA mortality. These results are consistent with several previous studies1–4, but not all5–7. However, it should be noted that none of these previous studies have considered the potential impact of overall drinking habits on the association between amount of alcohol consumed and risk of mortality. Our results showed that amount of alcohol consumed was related to risks of all-cause mortality or cause-specific mortality differently based on drinking habits. For example, for all-cause mortality, a J-shaped association was observed in participants with unfavorable DHS, while a U-shaped association was observed in participants with favorable DHS. From another perspective, within the same categories of amount of alcohol consumed, participants with favorable DHS generally had lower risk of mortality than those with unfavorable DHS. Mechanisms hypothesized to explain such results include the healthy drinking habits (regular drinking or alcohol consumed with meals) might improve levels of high-density lipoproteins, blood pressure, glucose, oxidative stress markers and pro-inflammatory cytokines, despite similar amounts of alcohol intake29–38. Other mechanisms may be also involved, and future studies are warranted to explore the functional roles of drinking habits in the health.
Intriguingly, we found consistent interactions between DHS and socioeconomic level on risks of all-cause mortality, CVD mortality and CA mortality, and the inverse associations appeared to be stronger in participants with low socioeconomic level as compared with those with high socioeconomic level, and these interactions were independent of amount of alcohol consumed. These results have two great implications, first, these results indicate that the observed inverse association of DHS with risks of mortality were unlikely due to its correlation with the higher socioeconomic level; Second, previous studies have shown that participants with low socioeconomic level have higher risk of alcohol-related mortality than those with high socioeconomic level at similar amount of alcohol consumed39,40. Therefore, our results also highlight a special importance of improving drinking habits in the participants with low socioeconomic level. Further studies are needed to explore the reasons for the such observed interaction between DHS and socioeconomic level on the risk of mortality.
In addition, because the amounts of alcohol consumed may change over time41. A genetic predisposition to alcohol consumption (ALC-GRS) might better capture lifetime alcohol consumption exposure42, thus we also included ALC-GRS in our analysis. A higher ALC-GRS indicating a higher levels of alcohol preference. Our results showed that higher ALC-GRS was marginally associated with higher risk of all-cause mortality but not associated with cause-specific mortality, whereas drinking habits did not modify such associations.
The major strengths of this study include the large sample size, the wealth of information of covariates and the wide range of amount of alcohol consumed. Notably, we carefully considered the methodological issues that might introduce bias into the alcohol-mortality relationship. To minimize the selection bias and reverse causality, we limited our study participants to the current drinkers and further excluded participants who reduced their alcohol intake due to health-related problems. We acknowledge that our study may still have several potential limitations. Firstly, self-reported alcohol consumption might be subject to measurement error. Secondly, our study analyzed only all-cause mortality and cause-specific mortality, future studies are needed to assess the associations of drinking habits with various diseases. Thirdly, our study population included only middle-aged adults from UK, it is unknown whether our findings could be generalized to other populations with different drinking cultures. Fourthly, we could not exclude the possibility that a favorable DHS is a marker for a healthier lifestyle. However, we did not find significant interactions between DHS and healthy lifestyle on the risks of mortality. Lastly, the current ALC-GRS only accounts for a small proportion of the variance of alcohol intake, thus caution should be taken in interpreting the results on the genetic risk score for alcohol intake.
Conclusion
Our study indicates that overall drinking habits are related to the risk of all-cause mortality and cause-specific mortality. The association between amount of alcohol consumed and risk of all-cause mortality varies according to overall drinking habits. Our findings emphasize the importance of considering drinking habits in the relation between amount of alcohol consumed and human health.
Supplementary Material
Funding/Support:
The study was supported by grants from the National Heart, Lung, and Blood Institute (HL071981, HL034594, HL126024), the National Institute of Diabetes and Digestive and Kidney Diseases (DK115679, DK091718, DK100383, DK078616)
Role of the Funder/Sponsor:
The funding sources and sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations used:
- BMI
body mass index
- CA
cancer
- CVD
cardiovascular disease
- MET
Metabolic Equivalent Task
- DHS
drinking habit score
- GRS
genetic risk score
- TDI
Townsend deprivation index
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data source:
This research has been conducted using the UK Biobank Resource under Application Number 29256
Declaration of Interests:
The authors declare no conflicts of interest.
Transparency statement:
LQ affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
References
- 1.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, De Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166(22):2437–2445. [DOI] [PubMed] [Google Scholar]
- 2.Jayasekara H, English DR, Room R, MacInnis RJ. Alcohol consumption over time and risk of death: a systematic review and meta-analysis. Am J Epidemiol. 2014;179(9):1049. [DOI] [PubMed] [Google Scholar]
- 3.Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in US adults. J Am Coll Cardiol. 2017;70(8):913. [DOI] [PubMed] [Google Scholar]
- 4.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wood AM, Kaptoge S, Butterworth AS, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. The Lancet. 2018;391(10129):1513–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang L, Zhou M, Sherliker P, et al. Alcohol drinking and overall and cause-specific mortality in China: nationally representative prospective study of 220 000 men with 15 years of follow-up. Int J Epidemiol. 2012;41(4):1101. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari P, Licaj I, Muller DC, et al. Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. BMJ Open. 2014;4(7):e005245–005245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holst C, Becker U, Jørgensen ME, Grønbæk M, Tolstrup JS. Alcohol drinking patterns and risk of diabetes: a cohort study of 70,551 men and women from the general Danish population. Diabetologia. 2017;60(10):1941–1950. [DOI] [PubMed] [Google Scholar]
- 9.Mukamal KJ, Conigrave KM, Mittleman MA, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348(2):109–118. [DOI] [PubMed] [Google Scholar]
- 10.Tolstrup JS, Jensen MK, Tjønneland A, Overvad K, Grønbæk M. Drinking pattern and mortality in middle‐ aged men and women. Addiction. 2004;99(3):323–330. [DOI] [PubMed] [Google Scholar]
- 11.Baglietto L, English DR, Hopper JL, Powles J, Giles GG. Average volume of alcohol consumed, type of beverage, drinking pattern and the risk of death from all causes. Alcohol Alcohol. 2006;41(6):664–671. [DOI] [PubMed] [Google Scholar]
- 12.Hendriks HFJ, Veenstra J, Velthuis-te Wierik EJM, Shaafsma G, Kluft C. Effect of moderate dose of alcohol with evening meal on fibrinolytic factors. BMJ. 1994;308(6935):1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trevisan M, Schisterman E, Mennotti A, Farchi G, Conti S. Drinking Pattern and Mortality:: The Italian Risk Factor and Life Expectancy Pooling Project. Ann Epidemiol. 2001;11(5):312–319. [DOI] [PubMed] [Google Scholar]
- 14.Augustin LSA, Gallus S, Tavani A, Bosetti C, Negri E, La Vecchia C. Alcohol consumption and acute myocardial infarction: a benefit of alcohol consumed with meals. Epidemiology. 2004:767–769. [DOI] [PubMed] [Google Scholar]
- 15.Conigrave KM, Hu BF, Camargo CA, Stampfer MJ, Willett WC, Rimm EB. A prospective study of drinking patterns in relation to risk of type 2 diabetes among men. Diabetes. 2001;50(10):2390. [DOI] [PubMed] [Google Scholar]
- 16.Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. The Lancet. 1988;332(8623):1267–1273. [DOI] [PubMed] [Google Scholar]
- 17.Fat LN, Cable N, Marmot MG, Shelton N. Persistent long-standing illness and non-drinking over time, implications for the use of lifetime abstainers as a control group. J Epidemiol Community Health. 2014;68(1):71–77. [DOI] [PubMed] [Google Scholar]
- 18.Jackson R, Broad J, Connor J, Wells S. Alcohol and ischaemic heart disease: probably no free lunch. The Lancet. 2005;366(9501):1911. [DOI] [PubMed] [Google Scholar]
- 19.Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ. 2015;350:h384–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naimi TS, Stockwell T, Zhao J, et al. Selection biases in observational studies affect associations between ‘moderate’alcohol consumption and mortality. Addiction. 2017;112(2):207. [DOI] [PubMed] [Google Scholar]
- 21.Sudlow C, Gallacher J, Allen N, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3):e1001779–1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health Do. Alcohol Guidelines Review–Report from the Guidelines development group to the UK Chief Medical Officers ,2016.
- 23.Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB. Key findings on alcohol consumption and a variety of health outcomes from the Nurses’ Health Study. Am J Public Health. 2016;106(9):1586–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu M, Jiang Y, Wedow R, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet. 2019;51(2):237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carlsson S, Hammar N, Grill V, Kaprio J. Alcohol consumption and the incidence of type 2 diabetes: a 20-year follow-up of the Finnish twin cohort study. Diabetes Care. 2003;26(10):2785. [DOI] [PubMed] [Google Scholar]
- 26.Murray RP, Connett JE, Tyas SL, et al. Alcohol volume, drinking pattern, and cardiovascular disease morbidity and mortality: is there a U-shaped function. Am J Epidemiol. 2002;155(3):242. [DOI] [PubMed] [Google Scholar]
- 27.Kauhanen J, Kaplan GA, Goldberg DE, Salonen JT. Beer binging and mortality: results from the Kuopio ischaemic heart disease risk factor study, a prospective population based study. BMJ. 1997;315(7112):846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simpson RF, Hermon C, Liu B, et al. Alcohol drinking patterns and liver cirrhosis risk: analysis of the prospective UK Million Women Study. The Lancet Public Health. 2019;4(1):e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heath DB. Cultural variations among drinking patterns. Drinking patterns and their consequences. 1998:103. [Google Scholar]
- 30.Shai I, Wainstein J, Harman-Boehm I, et al. Glycemic effects of moderate alcohol intake among patients with type 2 diabetes: A Multi-center, randomized clinical intervention trial. Diabetes Care. 2007. [DOI] [PubMed] [Google Scholar]
- 31.Davies MJ, Baer DJ, Judd JT, Brown ED, Campbell WS, Taylor PR. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women: a randomized controlled trial. JAMA. 2002;287(19):2559. [DOI] [PubMed] [Google Scholar]
- 32.Greenfield JR, Samaras K, Hayward CS, Chisholm DJ, Campbell LV. Beneficial postprandial effect of a small amount of alcohol on diabetes and cardiovascular risk factors: modification by insulin resistance. The Journal of Clinical Endocrinology & Metabolism. 2005;90(2):661–672. [DOI] [PubMed] [Google Scholar]
- 33.Hätönen KA, Virtamo J, Eriksson JG, et al. Modifying effects of alcohol on the postprandial glucose and insulin responses in healthy subjects–. Am J Clin Nutr. 2012;96(1):44–49. [DOI] [PubMed] [Google Scholar]
- 34.Taskinen M, Välimäki M, Nikkilä EA, Kuusi T, Ylikahri R. Sequence of alcohol-induced initial changes in plasma lipoproteins (VLDL and HDL) and lipolytic enzymes in humans. Metabolism. 1985;34(2):112–119. [DOI] [PubMed] [Google Scholar]
- 35.Rakic V, Puddey IB, Dimmitt SB, Burke V, Beilin LJ. A controlled trial of the effects of pattern of alcohol intake on serum lipid levels in regular drinkers. Atherosclerosis. 1998;137(2):243–252. [DOI] [PubMed] [Google Scholar]
- 36.Abe H, Kawano Y, Kojima S, et al. Biphasic effects of repeated alcohol intake on 24-hour blood pressure in hypertensive patients. Circulation. 1994;89(6):2626–2633. [DOI] [PubMed] [Google Scholar]
- 37.Rakic V, Puddey IB, Burke V, Dimmitt SB, Beilin LJ. Influence of pattern of alcohol intake on blood pressure in regular drinkers: a controlled trial. J Hypertens. 1998;16(2):165–174. [DOI] [PubMed] [Google Scholar]
- 38.Marfella R, Cacciapuoti F, Siniscalchi M, et al. Effect of moderate red wine intake on cardiac prognosis after recent acute myocardial infarction of subjects with Type 2 diabetes mellitus. Diabet Med. 2006;23(9):974. [DOI] [PubMed] [Google Scholar]
- 39.Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(4):1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. The Lancet Public Health. 2017;2(6):e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Britton A, Ben-Shlomo Y, Benzeval M, Kuh D, Bell S. Life course trajectories of alcohol consumption in the United Kingdom using longitudinal data from nine cohort studies. BMC Med. 2015;13(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Millwood IY, Walters RG, Mei XW, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. The Lancet. 2019;393(10183):1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


