Abstract
Chromatin remodeling plays an essential role in regulating transcriptional networks and timing of gene expression. Chromatin remodelers such as SWItch/Sucrose Non-Fermentable (SWI/SNF) harbor many protein components, with the catalytic subunit providing ATPase activity to displace histones along or from the DNA molecules, and associated subunits ensuring tissue specificity and transcriptional or co-transcriptional activities. Mutations in several of the SWI/SNF subunits have been linked to cancer. Here, we describe how SMARCD3/Baf60c expression is associated with hormone positive (ER+) breast cancer. The level SMARCD3, as detected by immunohistochemistry in breast cancer patient samples, is correlated with differential long-term disease-free survival. In contrast, the expression level of SMARCD1/Baf60a and SMARCD2/Baf60b, which are mutually exclusive within the SWI/SNF complex and have a partially redundant function, lacks predictive value in breast cancer patient samples. Lower proliferation rates are observed in SMARCD3 depleted cells, which reflects a failure to fully progress through G2/M, and an increase in endoreplication. In the absence of SMARCD3, p21 accumulates in cells but does not halt the cell cycle, and DNA damage accumulates and remains unrepaired. Taken together, our data begin to explain why ER+ breast cancer patients with low SMARCD3 expressing tumors exhibit reduced survival rates compared to patients expressing normal or higher levels of SMARCD3. SMARCD3 might act as a tumor suppressor role through regulation of cell cycle checkpoints and could be a reliable and specific breast cancer prognostic biomarker.
Keywords: SMARCD3, DNA damage repair, Breast Cancer, Cell cycle
Introduction
The chromatin remodeler SWI/SNF harbors a large number of subunits (12 genes in yeast, 29 in human; see [1] for review; Fig. 1A), whose functions are conserved among eukaryotes [2]. Early work identified SWI/SNF as a transcription activator through histones sliding and alteration of the nucleosome structure [3]. Since then, it has been implicated in DNA replication, damage repair, apoptosis, metabolism, and cell differentiation. Mutations or aberrant expression of SWI/SNF subunits are frequently found in a broad range of cancer subtypes [4], hinting at subtle and tissue-specific regulation of the SWI/SNF subunits. Contribution of individual SWI/SNF subunits to the complex function and its structure stability have been extensively studied in yeast [5, 6] and humans [7]. These studies have provided insights into how mutations in individual subunits or their epigenetic silencing affect gene expression and favor carcinogenesis [5–7].
Figure 1.
SMARCD3 expression is modified in breast cancer (A) Schematic of the BAF complex showing combinations of subunits. (B) RT-qPCR analysis of SMARCD3 expression in BRCT102 relative to 18S and RNAseq analysis of SMARCD3 in TCGA breast invasive carcinoma dataset (unpaired t-test, ** p < 0.01; **** p < 0.0001). (C) SMARCD3 promoter methylation levels are shown for all 92 normal (N) and all 735 tumor (T) samples (drawn to scale) in the TCGA Breast Invasive Carcinoma dataset. The degree of methylation is color-coded; normal samples also shown off scale (N*). (D, E) The SMARCD3 promoter is hypermethylated in TCGA breast cancer samples compared to normal samples. (D) Unpaired analysis (Mann Whitney U test). (E) paired analysis (Wilcoxon signed rank test). (F) Hypermethylated SMARCD3 promoters in tumors correlate with significantly lower SMARCD3 mRNA than in respective matched normal samples, as per unpaired and paired tests (Mann Whitney U test and Wilcoxon signed rank test, respectively). (G) Kaplan Meier curves of overall survival in TCGA dataset, patient stratified using SMARCD3 high, normal or low expression. Log-rank p-value testing for similarity between survival curve. (H) Frequency of patient with gene expression alteration in TCGA Breast Invasive Carcinoma and corresponding log-rank P val. testing for similarity between survival curve
The catalytic subunits, BRG1 or BRM, are essential for enzymatic function and the structural integrity of SWI/SNF, and have been intensely studied. In contrast, tissue-specific subunits (BRG1 associated factors, or BAF) and non-catalytic subunits of SWI/SNF, e.g. SMARCD3, one of three paralogs of SMARCD (SMARCD1/2/3, or Baf60a/b/c respectively), remain poorly characterized. SMARCD1/2/3 are mutually exclusive, tissue-specific, and their function is only partially redundant as they cannot complement each other [8, 9]. They have been identified as recruiter of the SWI/SNF complex to target site on the chromatin through interaction with protein partners [10, 11]. SMARCD1/2 role in the complex have been better characterized ad SMARCD3 precise function remains to be discovered. However, previous work SMARCD3 shed light on SMARCD3 as a potentially essential subunit. For instance, SMARCD3 is critical for cell differentiation via direct interactions with partners such as MYOD, thus coordinating cell differentiation cascades through transcriptional activation of genes, and through epigenetic reprogramming [12, 13]. Recent studies have associated SMARCD3 levels and breast cancer risks: first, the promoter region of SMARCD3 is significantly hypermethylated in triple negative breast cancer (TNBC) [14] compared to matched normal tissues. Second, SMARCD3 was shown to contribute to mesenchymal to epithelial transition (MET) of TNBC [15]. As methylation of regulatory elements often leads to decreased gene expression, we ask here whether SMARCD3 silencing in TNBC contributes to the promotion of breast cancer, which could potentially be a valuable biomarker in predicting patient outcome and/or response to therapy. Using a large, population-based data set we build prognostic models for predicting outcomes of patients with breast cancer based on SMARCD3 expression. We show that expression of SMARCD3 correlates with good patient outcomes, and low SMARCD3 is associated with diminished survival rates. Investigation of SMARCD3 protein levels in breast cancer samples uncovered frequent co-expression of SMARCD3 and ER, and colocalization of the two proteins in the nuclei of luminal cells. Through investigating the link between ER/SMARCD3 expression and localization, and the disease-free survival of patients, we have found that low-SMARCD3 is a marker of recurrence in ER+ patients but no correlation between ER and SMARCD3 expression. In our effort to understand the role of SMARCD3 in cancer suppression, we show that SMARCD3 contributes to proper progression of the cell cycle, through its role as a repressor of p21. SMARCD3 depleted cells exhibit slow proliferation rates, yet higher sensitivity to genotoxic agents such as radiation. Taken together, our data support a novel role of SMARCD3 as a breast tumor suppressor, likely through regulation of ER-mediated cell cycle checkpoints, and indicate that SMARCD3 nuclear expression has predictive value for survival in ER+ breast cancer patients.
Results
SMARCD3 is downregulated in breast cancer
Subunits of the SWI/SNF complex, as well as other chromatin remodeling complexes, are inactivated or mutated in many solid tumors [4, 16, 17]. Consistent with this, others and our group identified SMARCD3 as a potential tumor suppressor candidate gene in breast cancer [14]. We investigated the possible link between expression of SMARCD3 and breast cancer using real-time quantitative PCR in primary mammary carcinomas in normal (n=5) and tumor samples (n=40). The expression of SMARCD3 varied greatly across control samples, and we detected a 3.8-fold decrease in SMARCD3 expression in tumor samples as compared with control samples (Fig. 1B). This panel contains limited number of normal samples, and to verify our observation, we next analyzed SMARCD3 expression in primary breast cancer and normal breast tissues using gene expression profile datasets from the TCGA breast invasive carcinoma cohort. Of 114 normal breast tissue samples and 1097 breast tumor samples, SMARCD3 transcript level in tumors is significantly reduced compared with normal breast tissues (Fig. 1B). Normal matched samples were used as control to account for genetic diversity amongst patients. Tumor sample were found to have a decreased expression of SMARCD3 when compared to healthy adjacent tissue (Fig. 1B; Fig.S1A & B).
To investigate the causes of SMARCD3 lowered expression in breast cancer, we interrogated methylation status of the SMARCD3 promoter. SMARCD3 promoter methylation levels were found significantly higher in tumor (T) than normal (N) in the TCGA Breast Invasive Carcinoma dataset (Fig. 1C, D). Paired analysis indicated frequent hypermethylation of the SMARCD3 promoter in tumor compared to matched normal tissue, and significantly lower SMARCD3 expression. Although the decrease in expression of SMARCD3 is observed across breast cancer datasets (Fig 1B, 1F; Fig. S1C) and can be explained by frequent allelic copy number loss (Fig. S1B), a majority of silencing events might occur through methylation of the SMARCD3 promoter (Fig. 1 C–F).
Members of the SMARCD family have been found mutually exclusive within the SWI/SNF complex and depletion of individual SWI/SNF subunits can destabilize the residual complex [18]. SMARCD1/2/3 family of proteins occupy the same position in the BAF complex and we sought to investigate possible function overlap. We examined transcript levels and found that SMARCD2, but not SMARCD1, was significantly up-regulated in tumor samples (Fig. S1A). We next investigated possible correlation between SMARCD1/2/3 expression. Using Spearman test, we found SMARCD1 and SMARCD2 are positively correlated in the TCGA primary tumor dataset (Fig. S1D(i)). Conversely, SMARCD1 and SMARCD3 are negatively correlated (Fig. S1D(ii)). Both correlations, although statistically significant, are weak and more work would be necessary to establish any biologically relevant interaction with the three SMARCD1/2/3 isoforms. No direct correlation was observed between SMARCD2 and SMARCD3, indicating that even though both genes show inverse expression in tumor vs matched normal, their expression is not associated by monotonic relationship (Fig. S1D(iii), Spearman ρ = 0.005, p=0.881).
SMARCD3, but not SMARCD1 or 2, has good prognostic value in breast cancer
Based on emerging evidence that SWI/SNF has tumor suppressor properties, we next investigated whether changes in SMARCD3 expression are associated with specific patient survival probabilities. To explore this, we first performed survival analysis using Kaplan-Meier (KM) estimates on the TCGA Breast Invasive Carcinoma dataset. Cancer samples were categorized based on significant z-score deviation from the normal. Amongst the three genes, SMARCD3 expression was found to be the most frequently altered (37.6%) compared to SMARCD1 (23.6%) or SMARCD2 (17.3%) (Fig. 1H).
KM estimates showed a significant difference in survival between patients based on their expression of SMARCD3 (Fig. 1G). In particular, the median survival of patients with unaltered SMARCD3 is 10.8 years (3945 days, n=566) compared to 8.9 years (3262 days, n=309) in tumors that had a low level of SMARCD3, suggesting that decreased SMARCD3 expression is associated with decreased survival. Survival was not affected by SMARCD1 or SMARCD2 gene expression alterations (Fig. S1E). Association analysis of SMARCD3 levels and clinicopathological variables revealed a strong association between SMARCD3 expression and molecular subtypes and hormone receptors (Table 1). There was no significant association between SMARCD3 expression with age, TNM Stage, T stage and N stage (Table 1). Tumors of the luminal A subtype mostly express normal levels of SMARCD3, while low SMARCD3 expression is more frequent in the primary tumor of patients with ER and PR negative breast cancers and with invasive ductal carcinoma (Table 1). ER- tumors with copy number loss express significantly lower SMARCD3 when compared to normal, all tumor types, ER+ or total ER- tumors (Fig. S1B). We then broadened our analysis of SMARCD3 prognostic value using Cox regression modelling. As a single continuous variable, SMARCD3 expression, but not that of SMARCD1 or SMARCD2, was significantly predictive of survival for patients with TCGA primary tumors (Table 1). Hazard ratio calculation correlates each unit of increase in SMARCD3 expression with a predicted 21% decrease in fatalities (Table 1, HR=0.79 95% CI: 0.67–0.92, p=0.003).
Table 1.
Single variable Cox regression analysis.
| SMARCD3 expression | ||||
|---|---|---|---|---|
| Variable | Low | Normal | High | p-value |
| Age (years) | 0.292 | |||
| < 45 | 55 (6.1) | 79 (8.7) | 6 (0.7) | |
| ≥ 45 | 254 (28.0) | 487 (53.6) | 27 (3.0) | |
| PAM50 | < 0.001 | |||
| Lum A | 115 (12.7) | 333 (36.7) | 13 (1.4) | |
| Lum B | 80 (8.8) | 109 (12.0) | 4 (0.4) | |
| Her2 | 47 (5.2) | 21 (2.3) | 1 (0.1) | |
| Basal | 64 (7.0) | 80 (8.8) | 13 (1.4) | |
| Normal | 3 (0.3) | 23 (2.5) | 2 (0.2) | |
| ER status | < 0.001 | |||
| Positive | 195 (22.5) | 455 (52.4) | 17 (2.0) | |
| Negative | 96 (11.1) | 92 (10.6) | 13 (1.5) | |
| PR status | < 0.001 | |||
| Positive | 167 (19.3) | 396 (45.8) | 15 (1.7) | |
| Negative | 123 (14.2) | 149 (17.2) | 15 (1.7) | |
| HER2 | 0.00142 | |||
| Negative | 157 (25.6) | 301 (49.0) | 18 (2.9) | |
| Positive | 67 (10.9) | 70 (11.4) | 1 (0.2) | |
| Pathological Stage | 0.914 | |||
| Stage I | 48 (5.3) | 104 (11.5) | 6 (0.7) | |
| Stage II | 184 (20.3) | 323 (35.6) | 19 (2.1) | |
| Stage III | 71 (7.8) | 131 (14.4) | 8 (0.9) | |
| Stage IV | 6 (0.7) | 8 (0.9) | 0 (0.0) | |
| Tumor stage | 0.0648 | |||
| T1 | 74 (8.1) | 157 (17.3) | 7 (0.8) | |
| T2 | 194 (21.4) | 319 (35.1) | 18 (2.0) | |
| T3 | 27 (3.0) | 77 (8.5) | 6 (0.7) | |
| T4 | 14 (1.5) | 13 (1.4) | 2 (0.2) | |
| Node status | 0.528 | |||
| N0 | 144 (15.9) | 270 (29.7) | 17 (1.9) | |
| N1 | 102 (11.2) | 194 (21.4) | 11 (1.2) | |
| N2 | 42 (4.6) | 58 (6.4) | 3 (0.3) | |
| N3 | 17 (1.9) | 41 (4.5) | 1 (0.1) | |
| NX | 4 (0.4) | 3 (0.3) | 1 (0.1) | |
| Histological type | < 0.001 | |||
| IDC | 261 (28.8) | 388 (42.8) | 24 (2.6) | |
| ILC | 22 (2.4) | 125 (13.8) | 5 (0.6) | |
| Other | 25 (2.8) | 53 (5.8) | 4 (0.4) | |
Clinicopathological factors influencing overall survival of patients in the TCGA Breast invasive carcinoma dataset. CI: confidence Interval; HR: hazard ratio. P value derived from Wald statistical test
Immunohistochemistry (IHC) staining of patient samples reveals strong and specific nuclear localization of SMARCD3 in luminal cells.
Keeping in mind the potential prognostic value of SMARCD3, we interrogated whether protein and mRNA levels correlate. First, we used a commercial breast cancer TMA which contains 192 samples from exclusively female breast cancer cases distributed across all hormonal receptor status (ER, PR and HER2) as assessed by IHC (Fig. 2). SMARCD3 expression was evaluated using IHC with anti-SMARCD3 antibody, after optimization (Fig. S2A). Strong nuclear staining was observed in luminal cells of normal acini (Fig. 2A), reminiscent of ER staining. These data are consistent with our previous observation that normal SMARCD3 expression was associated with hormonal receptors and luminal A molecular subtype in the TCGA dataset. In tumor cells, nuclear intensity of SMARCD3 staining was found variable across patient samples, and scored negative (−), weak (+), moderate (++) or strong (+++) (Fig. 2B). Most samples were found reasonably homogeneous. Of the 144 cores in which SMARCD3 levels could be measured, 87 cases (60.4%) were scored negative, 24 cases (16.7%) weak, 25 cases (17.3%) moderate and 8 cases (5.6%) strong for SMARCD3 staining.
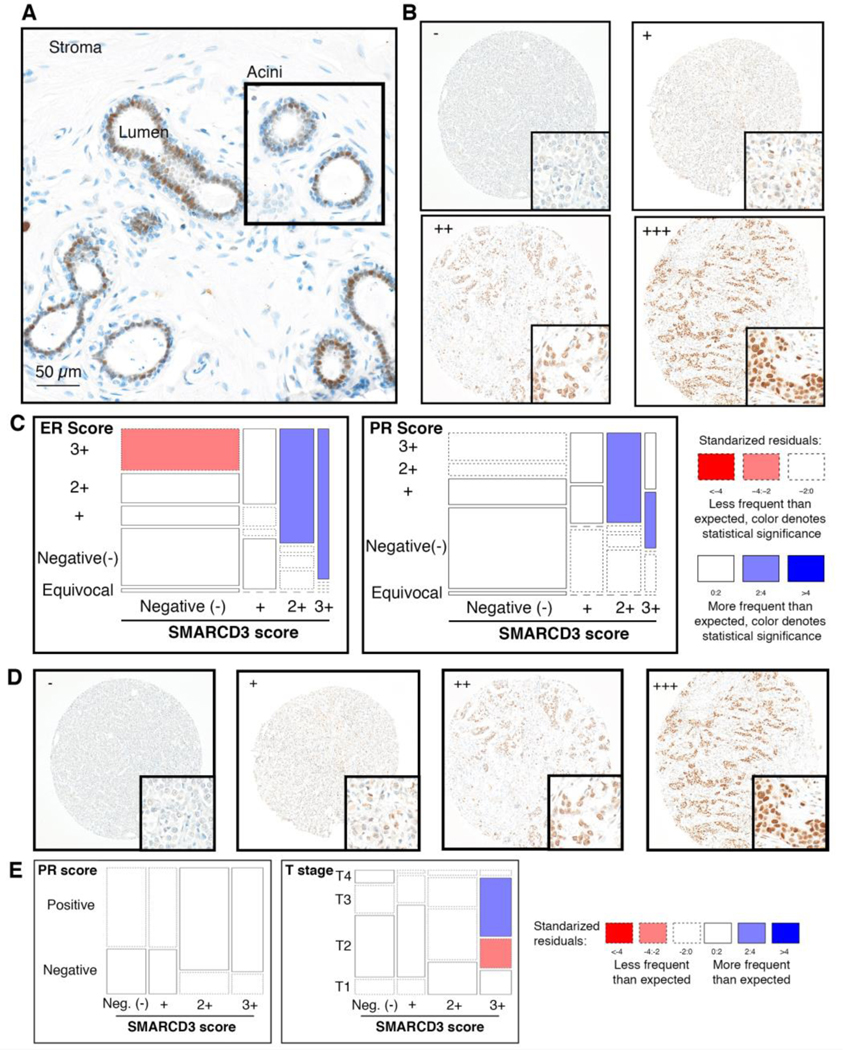
Figure 2: Expression of SMARCD3 in breast cancer is reminiscent of ER IHC staining.
(A),(B) Representative images of SMARCD3 IHC staining tumor sections show (A) colocalization with ER (B,D) variable nuclear staining across samplesnegative, (+) weak, (++) moderate and (+++) strong. (C,E) Mosaic plot of ER, PR, or stage in association with SMARCD3 expression. (A-C) performed on ER+ cohort (18), (D,E) on US Biomax1921b
Contingency tables were built to investigate the relationships between SMARCD3 nuclear scores and clinicopathological variables and mosaic plots were used to investigate the direction of significant deviation (Fig. 2C). SMARCD3 protein levels were significantly associated with the IHC status of ER and PR (Table S1, p<0.001). A correlation was observed between the level of SMARCD3 and ER (Fig. 2B–C), and between moderate/strong SMARCD3 level and strong PR signal (Fig. 2C). Interestingly, the correlation between SMARCD3 expression and ER level of expression is not complete, as negative SMARCD3 tumors expressed the full range of ER expression (Table S1).
As IHC validated our previous mRNA analyses, we wondered whether SMARCD3 protein level could be used to predict patient outcome. To answer this query, we made use of a cohort recently published [19], which contains 229 ER+, HER2- breast cancer patients with axillary nodal metastatic disease, with median follow-up time of 4.9 years. Relapse was used as a surrogate for breast cancer survival and occurred in 46 patients (20.1%; see [19]) with a median relapse-free time of 7.7 years (SD 3.8 years).
SMARCD3 expression using IHC could be assessed in 207 tumor cores and SMARCD3 nuclear staining intensity (Fig. 2D) was recorded as negative in 55 cases (26.6%), weak in 39 cases (18.8%), moderate in 69 cores (33.3%) and strong in 44 samples (21.3%). Chi-square analysis indicated a significant direct relationship between SMARCD3 level and PR expression (Table S2, p=0.018). Mosaic plots did not indicate significant correlation between categories, however negative and weak SMARCD3 associates with negative PR expression, whereas moderate and strong SMARCD3 expression tend to associate with positive PR expression and with higher stage (Fig. 2E). Significant differences in relapse were observed with patients grouped by low (−/+) SMARCD3 (n=94) vs high SMARCD3 (++/+++; n=113), (Fig. 2D). KM plots (Fig. 2D) and hazard ratio calculation (Table S3) indicated that high-SMARCD3 expression (as defined by IHC: ++/+++) halves the risks of relapse compared to low-SMARCD3 (as defined by IHC: - or +) patients (HR=2.11 95% CI: 1.10–4.06, p=0.024).
Cells depleted for SMARCD3 are deficient for DNA damage repair
The DNA damage response, comprising an intricate network of DNA damage checkpoints and damage repair mechanisms, allow cells to maintain their genomic integrity. For this reason, many DNA repair proteins are suppressors of breast tumors [20]. In eukaryotes, the organization of DNA into chromatin regulates the access of genetic material to biological processes such as DNA repair and imposes chromatin remodelling as a prerequisite for proteins of the repair machinery to access the genetic material (Goodarzi AA, Jeggo P, Lobrich M. 2010). Catalytic and non-catalytic subunits of the SWI-SNF complex have been directly implicated in DNA repair function, in link with putative tumor suppressor activities (Watanabe 2014, Qi, W. 2015, Velez-Cruz, R. 2016, Chen, Y. 2019). Given the potential protective role of SMARCD3 in ER+ breast cancer, we wondered whether this tumor suppression activity could be attributed to a DNA damage repair role. We monitored γH2AX immunofluorescence as a surrogate for DNA double-strand breaks (DSBs), and used X-ray irradiation as the DSB inducing agent, we observed an accumulation of γH2AX foci in cells depleted for SMARCD3 when compared to control cells. Interestingly, γH2AX foci form in SMARCD3 depleted cells even in the absence of genotoxic stress (t=0, Figure 3A (i) and (ii)). In addition, following irradiation, the resolution of γH2AX foci is delayed in the absence of SMARCD3 when compared to control cells (Fig. 3A–B). To confirm that SMARCD3 depleted cells are impaired for DNA damage repair pathways, we examined survival using colony formation upon irradiation (Fig. 3C). SMARCD3 depletion led to radiation hypersensitivity, noticeable even at low dose (2Gy), indicating that cells with low SMARCD3 expression are indeed impaired for DNA damage repair. A minor reduction of EdU incorporation was also observed following 6Gy irradiation, in cells depleted for SMARCD3 compared to the control (Fig. 3C). Interestingly, investigation of SMARCD3 expression level the Homology Directed Repair (HDR) signature (e.g. expression of other genes whose expression decreases in response to DNA damages) indicated a direct correlation between SMARCD3 and the (HDR) signature (Fig. 3D) [21]. For each cohort (low-expressing and high-expressing SMARCD3), we investigated the following markers: Number of telomeric allelic imbalances (NtAI); Large-scale state transitions (LST); Number of genomic segments with Loss Of Heterozygozity (HRD-LOH) and finally the total HRD score, which is the sum of each individual marker.
Figure 3. SMARCD3 is a DNA repair protein.
(A) γH2AX foci were quantified (i) or visualized (ii) in control and SMARCD3 depleted cells (HeLa) 8 h post 2 Gy irradiation. (B) Western analysis of γH2AX in of control and SMARCD3-depleted cells post irradiation (10 Gy). β-actin is the loading control. (C) (i) Colony forming assay in response to γ-radiation. (ii) Survival (%) of control and SMARCD3-knockdown cells is plotted. Data are shown as mean +/ SD of three independent experiments. (iii) Percentage of EdU positive cells 24 h post-treatment (2 Gy). Results were analyzed by one-way ANOVA with Dunnett’s multiple comparisons test correction. ** adjusted P-value < 0.01; *** adjusted P-value< 0.001. (D) HDR score analysis of TCGA ER+ breast cancer patients. Median SMARCD3 expression level was split at the median into SMARCD3-low and SMARCD3-high cohorts. The following markers of homologous recombination deficiency (HRD) are plotted for each cohort: NtAI: Number of telomeric allelic imbalances; LST: Large-scale state transitions; HRD-LOH: Number of genomic segments with LOH; HRD score: The sum of each aforementioned score. Statistics: Mann-Whitney U test.
This analysis shows that the number of each type of homologous recombination deficiency (HRD) and the total HRD score is significantly higher in SMARCD3-low than in SMARCD3-high ER+ samples.
Depletion of SMARCD3 perturbs cell cycle progression and overall proliferation
Uncontrolled proliferation is a key characteristic of cancer cells and catalytic subunits of the SWI/SNF complex are known to impact upon proliferation and senescence [22, 23]. Many DNA repair pathways are subject to cell cycle control. We investigated whether the DNA damage repair deficiency in and reduced survival of SMARCD3 depleted cells might have stemmed from perturbations in cell cycle progression. Stable knockdowns were generated in HeLa, as well as in triple negative breast cancer cells MDA-MB-231 and MDA-MB-468 (Fig. 4 and S3), which all have high baseline expression of SMARCD3, using two independent short-hairpin RNAs or an empty lentiviral vector (EV) as control (Fig. 4 and S3).
Figure 4. Knockdown of SMARCD3 promote genome instability.
(A), (B) The following were investigated in MDA-MB-231 (A) and HeLa (B): (i) Cell cycle distribution by PI staining. Percentage of cells in G0/G1, S or G2/M is plotted as mean +/− SD for three independent technical replicates. Significance assessed using t-test. (ii) Western blot of SMARCD3 and p21 proteins in SMARCD3 depleted cells and controls (iii) Percentage of EdU positive cells depleted for SMARCD3 or controls following 1h EdU incorporation. (C) Representative single-cell time series tracks of mKO2-hCdt1 and mAG-hGeminin arbitrary relative fluorescence units (RFU) percentages over time in HeLa-FUCCI cells transduced with EV control, or SMARCD3 shRNAs. (ii) Average duration of individual cell cycle phases is plotted (mean ± SD for 30 individual cell tracks). Significance determined using unpaired t-test. (D) Violin plot comparing SMARCD3 gene expression distribution across breast cancer samples that have undergone none (green), single (red) or double whole-genome doubling (purple). Significance determined by Mann Whitney U tests, blue line denotes significant inverse correlation between SMARCD3 expression and genome doubling (Spearman’s rank correlation P value). In all panels * p<0.05, ** p<0.01, *** p<0.001, **** p<0.0001, ns = non- significant.
First, we followed MDA-MB-231 and MDA-MB-468 growth rates by live-cell imaging for over 96 hours. MDA-MB-231 (Fig. S3A) and MDA-MB-468 (Fig. S3B) cells depleted for SMARCD3 exhibited lower proliferation rates than control cells. PI staining of the DNA and flow cytometry in HeLa and MDA-MB-231 showed that SMARCD3 decrease (shRNA1) leads to a modest accumulation in G1 when compared to controls, and a slight decrease in the numbers of cells entering S phase (Fig. 4A–B); raw data in Fig. S3C). To investigate G1/S transition, we measured the level of cyclin-dependent kinase inhibitor p21 by Western blotting. This revealed a strong accumulation of p21 in response to SMARCD3 depletion (Fig. 4A–B). Intriguingly, the level of p21 does not correlate with the cell proliferation rate, indicating that cells depleted for SMARCD3 might not respond to activated checkpoints. Consistently, incorporation of EdU indicated no noticeable difference between cells depleted for SMARCD3 and controls (Fig. 4A–B), which hints at normal DNA synthesis. Subtle variations in the cell cycle can be overlooked when using populations of cells. We used the FUCCI system [24] and live-cell imaging to investigate single cells behavior. While the ratio of cells in each phase of the cell cycle does not change, individual phases of the cell cycle are longer in cells depleted for SMARCD3 than in control cells (Fig. 4C). In addition to a longer S-phase, the S/G2 transition is compromised in cells depleted for SMARCD3, and we observed cells undergoing endoreplication, where cells initiate a new cycle of DNA synthesis instead of entering mitosis. This results in whole-genome doubling, a phenomenon estimated to occur in 45% of breast cancers [25]. Consistent with our in vitro data, we find that SMARCD3 expression is significantly lower in breast tumors that had undergone one or two whole-genome doublings (Fig. 4D).
Discussion
Here, we provide evidence that SMARCD3 is downregulated in malignant breast tissue, which may indicate a tumor suppressor function of SMARCD3 in breast cancer. We used three cohorts of breast cancer patients with various clinicopathological features to reach this conclusion. In all three, we observed significant downregulation of SMARCD3 in breast cancer relative to normal breast tissue. This indicates that besides mutations and copy number loss targeting the SMARCD3 gene locus, transcriptional inactivation of SMARCD3 gene, such as by promoter methylation, might contribute to the cancer phenotype. SMARCD1, 2 and 3 are three isoforms that can each be incorporated into the BAF chromatin remodeling complex. However, we have demonstrated that the expression of the three isoforms is not correlated either positively or negatively, indicating that they probably do not compensate for each other in cells when one is absent or downregulated. Interestingly, SMARCD3 was the only subunit that exhibited a strong link with breast cancer with prognosis value, with low SMARCD3 correlating with worse patient outcome. On average, the survival of patients with unaltered SMARCD3 is 673 additional days (1.9 years) when compared to patients with low SMARCD3, indicating a dramatic difference in outcome between these two patient groups. Thorough analysis of confounding factor is warranted to validate the predictive value of SMARCD3. In that regard, our histological investigation of SMARCD3 indicated a possible link between SMARCD3 and hormone receptors.
In breast cancer, estrogen can be a major driver of cell proliferation, as well as an efficient means for therapeutic intervention. Interestingly, we found that in normal breast tissue, SMARCD3 localizes in the nuclei of luminal cells, which is the same localization pattern as the estrogen receptor (ER). Similarly, the staining of SMARCD3 in ER+ breast cancer is reminiscent of that of ER, although expression of SMARCD3 and ER do not fully correlate. While high SMARCD3 is only found in strong ER+ samples, where both proteins could contribute to increased proliferation of the tumor, low SMARCD3 was observed across the full range of tumors, irrespective of ER expression level.
Conversely, both high- and low-SMARCD3 expression correlated with the expression of Progesterone Receptor (PR). Although more studies are required to fully understand the link between SMARCD3 and both ER and PR hormone receptors, the inclusion of SMARCD3 as a prognostic marker, together with PR and HER2 status, may help stratify ER positive breast cancer patients and aid in treatment decision making.
While SMARCD3 depleted cells appear to exhibit slower division rates as measured by live-cell imaging and accumulate high levels of G1/S checkpoint proteins, further investigation by live-cell imaging and the FUCCI system demonstrated that cells depleted for SMARCD3 might undergo DNA synthesis and cell cycle progression like the WT counterpart, only failing in the G2/M transition and undergoing endoreplication as a result. This finding is consistent with our observation that breast tumors that have undergone whole-genome doubling express significantly lower levels of SMARCD3 than tumors that have not. It also suggests that high risks of genomic instability do not always correlate with increased mitotic index. While we expected that SMARCD3 depletion would impair the normal progression of the cell cycle by limiting DNA replication through its role in chromatin remodeling, we found that replication is proficient. However, termination of replication and then mitosis are compromised. Although more work will be needed to fully understand SMARCD3 function, we cannot exclude that the role played by SMARCD3 in DNA repair and cell cycle regulation, is mediated through transcriptional regulation of genes involved in these mechanisms.
Interestingly, the phenotype observed in the absence of SMARCD3 is reminiscent of the BRG1 knock- down. Studies in mice revealed that BRG1 null heterozygosity increased the frequency of mammary tumors [26]. Delays in cell cycle progression were also previously reported in BRG1 knockout cells and attributed to interaction of the SWI/SNF complex and TOPIIα during decatenation of newly synthesized sister chromatid[27]. While ARID1A was ultimately identified as the non-catalytic subunit recruiting TOPIIα to the complex, SMARCD1/Baf60a was the most frequently immunoprecipitated subunit with TOPIIα. However, the role of SMARCD1/Baf60a during decatenation has yet to be elucidated. Given the mutually exclusiveness of this family of subunit, it is possible that SMARCD3 excess this function in tissue where SMARCD1 is absent. We know that BRG1 levels are intact in SMARCD3 depleted cells, which indicates that the phenotype of SMARCD3 depleted cells cannot be explained by concomitant BRG1 depletion. Our findings that SMARCD3 levels directly impact cell cycle progression by regulating p21 provides an additional clue to explain the role of SMARCD3 in carcinogenesis. Although the absence of SMARCD3 correlates with a low mitotic index, tumors expressing low levels of SMARCD3 could be considered aggressive given a heightened risk of recurrence and lack of response of these cells to p21. Our work provides evidence that low-SMARCD3 expression in ER+ tumors predicts poor response to the current standard of care, and patients with such tumors might benefit more from aggressive or personalized treatments. As a subpopulation of SMARCD3 cells accumulates in G0, it is easy to speculate that cells expressing low SMARCD3 levels might stay dormant and delay their re-entry into the cell cycle, accounting for some of the recurrence observed in poor-prognosis ER+ patients. In the future, it will be interesting to test whether SMARCD3 inactivation could provide a means to sensitize ER+ cells to genotoxic chemotherapy or radiotherapies.
Materials and Methods
Cell lines culture.
MDA-MB-231, MDA-MB-468 and HeLa were obtained from ATCC and cultured in DMEM supplemented with 10% fetal bovine serum (FBS).
Lentiviral particles production and cell infection.
Replication incompetent lentivirus were produced in HEK 293T cells co-transfected by mixing 5 μg of either pLKO.1 Empty Vector or pLKO.1 shRNA targeting SMARCD3 with 6 μg Lenti-vpak packaging kit components (OriGene) and 33 μL of transfection reagent (OriGene) in 1.5 mL OptiMEM, incubated for 20 min at RT. This transfection mixture was added onto 10 mL of HEK 293T cells at 2×105 cell/mL in fresh culture medium was transferred. Culture medium was replaced 24h post-transfection and viral supernatants were harvested twice at 48 and 72h and combined. Viral supernatants were clarified by centrifugation at 500 g, filtered through a 0.45 μm PES and stored at −80°C. Lentiviral transduction was performed with 5×105 cells seeded into a T25 flask in media supplemented with μg/mL polybrene. Viral supernatant (500 μL) was added onto the cells and they were then incubated for 24h. 72h post-transduction, cells were selected with Puromycin (for pLKO) at 1 μg/mL. After two weeks of Puromycin treatment cells were considered selected. Knockdown efficiency of SMARCD3 was determined by Western Blotting and/or qRT-PCR as described below. Cells transduced with FUCCI plasmids were sorted by FACS to select homogenous positive cells populations.
RNA extraction and cDNA preparation.
Total RNA was extracted from cells in exponential growth on 10 cm dishes. Cells were washed twice with PBS and 2 mL of TRIzol (Invitrogen™) was added on each plate. 500 μL of cell extracts were transferred into microfuge, chloroform extracted and nucleic acid was precipitated with isopropanol/ethanol. RNA was dissolved in RNase-free water and stored at −80°C. RNA yield and purity were evaluated on a NanoDrop and agarose gel electrophoresis. The reaction mixture for reverse transcription was prepared as previously described [28]. Briefly, 800 ng total RNA resuspended in RNase-free water was combined with 2.5 μM random hexamer and 500 μM RNase-free dNTPs (both Invitrogen™), heated at 65°C for 5 min, cooled on ice for at least one minute while adding 4 μl SuperScript™ III reaction buffer, 5 mM dithiothreitol, 40 U RNase out RNase inhibitor and 200 U SuperScript™ II RT (all from Invitrogen™) to each sample, except “no RT” control tubes. The mixture was incubated at 25°C for 5 min, at 50°C for 60 min and finally at 70°C for 15 min in a thermal cycler (Eppendorf). cDNA used to generate Figure 1B were sourced from OriGene (BRCT102).
Real-time quantitative PCR (RT-qPCR).
RT-qPCR was performed using Taqman® technology in 10 μL reaction volume. The reaction mixture was prepared as follow: 2 μL of cDNA, 5 μl Taqman® Universal Master Mix (Invitrogen™), 2.5 μL of water and 0.5 μL of Taqman® probe: human SMARCD3 (Invitrogen™ Cat. # 4331182) and human 18s (Invitrogen™ Cat. # 4331182) was used as the reference endogenous control. Taqman® probes were carefully picked to span exon-exon junction and thus, specifically target cDNA. The RT-qPCR assays were completed using the ABI ViiA™ 7 sequence detection system (Applied Biosystems®) with the following parameters: initial denaturation 50°C for 2 min then 95°C for 10 min followed by 40 cycles of 95°C for 15 seconds and 60°C extension for 1 min. Fluorescence was quantified at the end of each cycle. The real-time PCR data was analyzed using the ΔΔCt method.
Western blot analysis.
Cells were pelleted and lysed using RIPA buffer (10 mM Tris-Cl (pH 8.0), 1 mM EDTA, 1% Triton X-100, 0.1% sodium deoxycholate, 0.1% SDS, 140 mM NaCl, 1 mM PMSF). Lysates were sonicated and protein concentration was determined using BCA protein assay (Sigma). 30 μg of total proteins were loaded on 12% SDS–PAGE gel and separated by electrophoresis. Protein were transferred on PVDF membrane, dried and blotted overnight in 5% BSA TBS-T at 4 °C using primary antibodies (Abcam anti-SMARCD3: ab171075; Santa Cruz anti-beta-Actin (C-4): sc-47778; Millipore anti-γH2AX (Ser139): 05–636; Cell Signaling anti- p21WAF1/CIP1 (12D1): 2947). Afterwards, membranes were incubated with secondary antibodies for one hour at room temperature and developed using Clarity ECL Detection Kit (Bio-Rad).
Bioinformatics.
All available TCGA RNA-seq V2 data and clinical annotations were downloaded from the UCSC Xena browser. Data from the METABRIC dataset was obtained from cBioPortal and Oncomine. Both TCGA and METABRIC research data are publicly available and all patient information is de-identified. For Kaplan-Meier analysis, gene expression was converted into discrete variable to categorize patient based on SMARCD3 expression. SMARCD3 expression mean and standard deviation from the normal sample distribution were used to score sample as a z-score. Each sample with a SMARCD3 expression included within 2 standard deviation from the mean was score as unaltered, while samples with 2 standard deviation away from the mean were score as either low or high (i.e. p < 0.05). The number of whole-genome doublings in each TCGA breast cancer sample was determined using ABSOLUTE [29].
Statistical analysis.
Statistical analysis of gene expression in cancer sample was carried out in GraphPad Prism. Survival analysis was carried out in R version 3.4.2 (R Development Core Team; www.r-project.org) Kaplan-Meier estimate, log-rank test and curves were built with Survival and surviminer package (v. 2.41–3 and v. 0.4.1.99, respectively). Cox proportional hazard models were built with the rms-package (v. 4.3–1). Single Cox’s proportional-hazards regression were fitted on gene expression and clinical variables. The hazard ratio and its 95% CI were derived from these models and significance of the results were determined by Wald Statistical test. For the HDR score analysis, TCGA ER+ breast cancer patients were split by median SMARCD3 expression level, referred to as SMARCD3_low and SMARCD3_high cohorts. Then the following measures for homologous recombination deficiency (HRD) are compared in the cohorts (i) NtAI: The number of telomeric allelic imbalances, (as per [30]); (ii) LST: Large-scale state transitions, (as per [31]); (iii)HRD-LOH: Number of genomic segments with LOH, (as per [32]) (iv) HRD score: The sum of each of the above, (as also per [33]). Statistics: Mann-Whitney U test.
Immunohistochemistry (IHC).
Antigen retrieval was performed with the Ventana Discovery ULTRA Staining module, using Discovery CC1 for 32 min, on TMA from US Biomax (1921b) or Mater patient cohort [19]. Primary immunostaining was performed using antibodies against SMARCD3 (Abcam ab1711075) and Ventana antibody dilution buffer for 36 min at 36°C. Secondary immunostaining used an anti-rabbit horseradish peroxidase conjugated antibody and immune complexes were visualized using diaminobenzidine tetrahydrochloride, followed by counter-stain with hematoxylin II for 8 min. The scoring of the immunostained TMAs was performed by two independent investigators based on the SMARCD3 nuclear intensity level, under the guidance of a pathologist.
Cell proliferation assays.
Automated live cell imaging was conducted using an IncuCyte Zoom (Essen BioScience, Ann Arbor, MA, USA) live-cell imaging system. HeLa cells were seeded onto a 96- well plate at 3×103 cells per well. Phase contrast images of cells were acquired every two hours and proliferation was measured as a percentage of confluency obtained from the IncuCyte cell proliferation analysis module. The proliferation data was analysed in GraphPad Prism v7.0. A non-linear exponential curve was fitted and the population doubling time and R2 goodness-of-fit constant were extracted from the non-linear exponential growth curve analysis module in GraphPad Prism v7.0.
Clonogenic assay.
Cell death in response to irradiations was assayed by measuring colony formation with and without increasing doses of gamma irradiation (0, 2, 4 and 6 Gy) treatment using a Gammacell® 40 Exactor (Best Theratronics Ltd, Kanata, ON, CA). 300 cells per well were seeded on a 6-well plate and incubated for 8 h before being treated with increasing dose of gamma radiation (2, 4 and 6 Gy) using a Gammacell® 40 Exactor (Best Theratronics Ltd, Kanata, ON, CA). Culture medium was replaced every three days, and cells were incubated for 10–11 days or until surviving individual cells at T0 had divided sufficiently to form a visible colony (estimated to be 60 cells). Cells were fixed with methanol-acetic acid (3:1) and stained with 0.4% crystal violet. Excess dye was removed by immersing the plate in clean water twice. The 6-well plates were imaged using a chemidoc (Bio-Rad, Hercules, CA, USA) and the number of colonies was counted in CellProfiler using an automated analysis pipeline. Relative colony formation (%) as measured by the number of colonies from treated well divided by the number of colonies in the untreated control and plotted.
Indirect immunofluorescence.
Stable HeLa cells expressing shRNA or control plasmid were grown on coverslips for 24h and treated with 4 Gy γ-rays. Cell nuclei were pre-extracted with nuclear extraction buffer (10 mM PIPES (pH 6.8), 100 mM NaCl, 300 mM sucrose, 3 mM MgCl2, 1 mM EGTA (pH 8.0), 0.5% Triton X-100) for 2 min at RT and fixed with 4% paraformaldehyde (PFA) for 10 min at 4°C. Nuclei were blocked in 5% BSA/0.3% Triton X-100 for 2h at RT, immunoblotted with a primary antibody (Millipore anti-γH2AX (Ser139): 05–636) in 1% BSA/0.3% Triton X-100 for 2h at RT, followed by secondary antibody for 2h at RT. DNA was stained with ProLong Gold/Diamond Antifade Mountant with DAPI. Number of cells with nuclear foci were quantified using CellProfiler.
Cell cycle progression (flow cytometry).
Cells (asynchronized population) were collected and fixed with 70% ethanol at −20°C for at least 24h. DNA was stained with 100 μg/mL RNase A (QIAGEN) and 150 μg/mL propidium iodide (PI) for one hour at RT. Data were collected using a CytoFLEX Flow Cytometer (Beckman Coulter) and results were analyzed with FlowJo. 10,000 events were collected and aggregated cells were gated out.
Click-iT™ EdU.
Control and knockdown cells (HeLa; 4.0 × 104 cells/well) were seeded in 12-well plates with glass coverslips for 24h. To label the cells (according to manufactureŕs protocol), 5-ethynyl-2´-deoxyuridine (EdU) (Life Technologies) was added to a final concentration of 10 μM and incubated for 90 min at 37°C. Cells were fixed with 4% (PFA) for 10 min at RT, followed by permeabilization with 0.3% Triton X-100 for 20 min at RT. Click-iT™ Reaction Cocktail with Alexa Fluor® 488 (Life Technologies) was added to fixed cells and incubated for one hour at RT. Nuclei were stained with ProLong® Diamond Antifade Mountant with DAPI (Invitrogen™). EdU-stained cells were quantified using CellProfiler.
Supplementary Material
Acknowledgments
Funding
ED and PHGD are recipient of National Breast Cancer Fellowships. RT and BDLP are recipient of the Princess Alexandra Research Foundation. This work was funded by ECR13–04 (NBCF) and Cancer Council Queensland (CCQ). The Mays cancer center is supported by a NCI Cancer Center Support Core Grant P30 CA054174
Footnotes
Supplementary information
This article contains 4 supplementary figures and 3 supplementary tables that can be found online.
Compliance with ethical standards
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
All procedures performed in studies involving human samples were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with human participants or animals performed by any of the authors. Samples acquired from US Biomax guarantees informed consent was obtained from all individual participants included in the study. Subsequent staining experimental protocols were approved by the QUT ethics committee. Samples included in the Mater TMA were cleared for use by the Mater hospital ethics committee.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Tang L, Nogales E, Ciferri C: Structure and function of SWI/SNF chromatin remodeling complexes and mechanistic implications for transcription. Prog Biophys Mol Biol 2010, 102(2–3):122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winston F, Carlson M: Yeast SNF/SWI transcriptional activators and the SPT/SIN chromatin connection. Trends Genet 1992, 8(11):387–391. [DOI] [PubMed] [Google Scholar]
- 3.Clapier CR, Cairns BR: The biology of chromatin remodeling complexes. Annu Rev Biochem 2009, 78:273–304. [DOI] [PubMed] [Google Scholar]
- 4.Kadoch C, Crabtree GR: Mammalian SWI/SNF chromatin remodeling complexes and cancer: Mechanistic insights gained from human genomics. Sci Adv 2015, 1(5):e1500447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dutta A, Sardiu M, Gogol M, Gilmore J, Zhang D, Florens L, Abmayr SM, Washburn MP, Workman JL: Composition and Function of Mutant Swi/Snf Complexes. Cell Rep 2017, 18(9):2124–2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sen P, Luo J, Hada A, Hailu SG, Dechassa ML, Persinger J, Brahma S, Paul S, Ranish J, Bartholomew B: Loss of Snf5 Induces Formation of an Aberrant SWI/SNF Complex. Cell Rep 2017, 18(9):2135–2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang X, Lee RS, Alver BH, Haswell JR, Wang S, Mieczkowski J, Drier Y, Gillespie SM, Archer TC, Wu JN et al. : SMARCB1-mediated SWI/SNF complex function is essential for enhancer regulation. Nat Genet 2017, 49(2):289–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goljanek-Whysall K, Mok GF, Fahad Alrefaei A, Kennerley N, Wheeler GN, Munsterberg A: myomiR-dependent switching of BAF60 variant incorporation into Brg1 chromatin remodeling complexes during embryo myogenesis. Development 2014, 141(17):3378–3387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Witzel M, Petersheim D, Fan Y, Bahrami E, Racek T, Rohlfs M, Puchalka J, Mertes C, Gagneur J, Ziegenhain C et al. : Chromatin-remodeling factor SMARCD2 regulates transcriptional networks controlling differentiation of neutrophil granulocytes. Nat Genet 2017, 49(5):742–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Debril MB, Gelman L, Fayard E, Annicotte JS, Rocchi S, Auwerx J: Transcription factors and nuclear receptors interact with the SWI/SNF complex through the BAF60c subunit. J Biol Chem 2004, 279(16):16677–16686. [DOI] [PubMed] [Google Scholar]
- 11.Flajollet S, Lefebvre B, Cudejko C, Staels B, Lefebvre P: The core component of the mammalian SWI/SNF complex SMARCD3/BAF60c is a coactivator for the nuclear retinoic acid receptor. Mol Cell Endocrinol 2007, 270(1–2):23–32. [DOI] [PubMed] [Google Scholar]
- 12.Acevedo N, Reinius LE, Vitezic M, Fortino V, Soderhall C, Honkanen H, Veijola R, Simell O, Toppari J, Ilonen J et al. : Age-associated DNA methylation changes in immune genes, histone modifiers and chromatin remodeling factors within 5 years after birth in human blood leukocytes. Clin Epigenetics 2015, 7:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sohni A, Mulas F, Ferrazzi F, Luttun A, Bellazzi R, Huylebroeck D, Ekker SC, Verfaillie CM: TGFbeta1-induced Baf60c regulates both smooth muscle cell commitment and quiescence. PLoS One 2012, 7(10):e47629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stirzaker C, Zotenko E, Song JZ, Qu W, Nair SS, Locke WJ, Stone A, Armstong NJ, Robinson MD, Dobrovic A et al. : Methylome sequencing in triple-negative breast cancer reveals distinct methylation clusters with prognostic value. Nat Commun 2015, 6:5899. [DOI] [PubMed] [Google Scholar]
- 15.Gregoire JM, Fleury L, Salazar-Cardozo C, Alby F, Masson V, Arimondo PB, Ausseil F: Identification of epigenetic factors regulating the mesenchyme to epithelium transition by RNA interference screening in breast cancer cells. BMC Cancer 2016, 16:700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee RS, Roberts CW: Linking the SWI/SNF complex to prostate cancer. Nat Genet 2013, 45(11):1268–1269. [DOI] [PubMed] [Google Scholar]
- 17.Wu Q, Madany P, Akech J, Dobson JR, Douthwright S, Browne G, Colby JL, Winter GE, Bradner JE, Pratap J et al. : The SWI/SNF ATPases Are Required for Triple Negative Breast Cancer Cell Proliferation. J Cell Physiol 2015, 230(11):2683–2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helming KC, Wang X, Wilson BG, Vazquez F, Haswell JR, Manchester HE, Kim Y, Kryukov GV, Ghandi M, Aguirre AJ et al. : ARID1B is a specific vulnerability in ARID1A-mutant cancers. Nat Med 2014, 20(3):251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Snell CE, Gough M, Middleton K, Hsieh M, Furnas L, Seidl B, Gibbons K, Pyke C, Shannon C, Woodward N et al. : Absent progesterone receptor expression in the lymph node metastases of ER-positive, HER2-negative breast cancer is associated with relapse on tamoxifen. J Clin Pathol 2017, 70(11):954–960. [DOI] [PubMed] [Google Scholar]
- 20.Sung P, Klein H: Mechanism of homologous recombination: mediators and helicases take on regulatory functions. Nature reviews Molecular cell biology 2006, 7(10):739–750. [DOI] [PubMed] [Google Scholar]
- 21.Peng G, Chun-Jen Lin C, Mo W, Dai H, Park YY, Kim SM, Peng Y, Mo Q, Siwko S, Hu R et al. : Genome-wide transcriptome profiling of homologous recombination DNA repair. Nat Commun 2014, 5:3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He L, Chen Y, Feng J, Sun W, Li S, Ou M, Tang L: Cellular senescence regulated by SWI/SNF complex subunits through p53/p21 and p16/pRB pathway. Int J Biochem Cell Biol 2017, 90:29–37. [DOI] [PubMed] [Google Scholar]
- 23.Hendricks KB, Shanahan F, Lees E: Role for BRG1 in cell cycle control and tumor suppression. Mol Cell Biol 2004, 24(1):362–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newman RH, Zhang J: Fucci: street lights on the road to mitosis. Chem Biol 2008, 15(2):97–98. [DOI] [PubMed] [Google Scholar]
- 25.Zack TI, Schumacher SE, Carter SL, Cherniack AD, Saksena G, Tabak B, Lawrence MS, Zhsng CZ, Wala J, Mermel CH et al. : Pan-cancer patterns of somatic copy number alteration. Nat Genet 2013, 45(10):1134–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bultman SJ, Herschkowitz JI, Godfrey V, Gebuhr TC, Yaniv M, Perou CM, Magnuson T: Characterization of mammary tumors from Brg1 heterozygous mice. Oncogene 2008, 27(4):460–468. [DOI] [PubMed] [Google Scholar]
- 27.Dykhuizen EC, Hargreaves DC, Miller EL, Cui K, Korshunov A, Kool M, Pfister S, Cho YJ, Zhao K, Crabtree GR: BAF complexes facilitate decatenation of DNA by topoisomerase IIalpha. Nature 2013, 497(7451):624–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Betts JA, Moradi Marjaneh M, Al-Ejeh F, Lim YC, Shi W, Sivakumaran H, Tropee R, Patch AM, Clark MB, Bartonicek N et al. : Long Noncoding RNAs CUPID1 and CUPID2 Mediate Breast Cancer Risk at 11q13 by Modulating the Response to DNA Damage. Am J Hum Genet 2017, 101(2):255–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carter SL, Cibulskis K, Helman E, McKenna A, Shen H, Zack T, Laird PW, Onofrio RC, Winckler W, Weir BA et al. : Absolute quantification of somatic DNA alterations in human cancer. Nat Biotechnol 2012, 30(5):413–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Birkbak NJ, Wang ZC, Kim JY, Eklund AC, Li Q, Tian R, Bowman-Colin C, Li Y, Greene-Colozzi A, Iglehart JD et al. : Telomeric allelic imbalance indicates defective DNA repair and sensitivity to DNA-damaging agents. Cancer Discov 2012, 2(4):366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Popova T, Manie E, Rieunier G, Caux-Moncoutier V, Tirapo C, Dubois T, Delattre O, Sigal-Zafrani B, Bollet M, Longy M et al. : Ploidy and large-scale genomic instability consistently identify basal-like breast carcinomas with BRCA1/2 inactivation. Cancer Res 2012, 72(21):5454–5462. [DOI] [PubMed] [Google Scholar]
- 32.Abkevich V, Timms KM, Hennessy BT, Potter J, Carey MS, Meyer LA, Smith-McCune K, Broaddus R, Lu KH, Chen J et al. : Patterns of genomic loss of heterozygosity predict homologous recombination repair defects in epithelial ovarian cancer. Br J Cancer 2012, 107(10):1776–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marquard AM, Eklund AC, Joshi T, Krzystanek M, Favero F, Wang ZC, Richardson AL, Silver DP, Szallasi Z, Birkbak NJ: Pan-cancer analysis of genomic scar signatures associated with homologous recombination deficiency suggests novel indications for existing cancer drugs. Biomark Res 2015, 3:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.