Abstract
Penetrating abdominopelvic trauma usually results from abdominal cavity violation from a firearm injury or a stab wound and is a leading cause of morbidity and mortality from traumatic injuries. Penetrating trauma can have subtle or complex imaging findings, posing a diagnostic challenge for radiologists. Contrast-enhanced CT is the modality of choice for evaluating penetrating injuries, with good sensitivity and specificity for solid-organ and hollow viscus injuries. Familiarity with the projectile kinetics of penetrating injuries is an important skill set for radiologists and aids in the diagnosis of both overt and subtle injuries. CT trajectography is a useful tool in CT interpretation that allows the identification of subtle injuries from the transfer of kinetic injury from the projectile to surrounding tissue. In CT trajectography, after the entry and exit wounds are delineated, the two points can be connected by placing cross-cursors and swiveling the cut planes obliquely in orthogonal planes to obtain a double-oblique orientation to visualize the wound track in profile. The path of the projectile and its ensuing damage is not always straight, and the imaging characteristics of free fluid of different attenuation in the abdomen (including hemoperitoneum) can support the diagnosis of visceral and vascular injuries. In addition, CT is increasingly used for evaluation of patients after damage control surgery and helps guide the management of injuries that were overlooked at surgery.
An invited commentary by Paes and Munera is available online.
Online supplemental material is available for this article.
©RSNA, 2021
SA-CME LEARNING OBJECTIVES
After completing this journal-based SA-CME activity, participants will be able to:
■ Discuss the importance of ballistic kinematics and its role in image interpretation.
■ Explain the importance of CT trajectography in trauma CT image interpretation.
■ Identify imaging signs in peritoneal violation and hollow and solid visceral and vascular injuries.
Introduction
Trauma is an ongoing public health concern and is broadly categorized as blunt or penetrating. Both categories have predictable epidemiologic patterns with associated morbidity and mortality. Penetrating abdominopelvic trauma usually results from abdominal cavity violation from a firearm injury or a stab wound and is a leading cause of morbidity and mortality. Any object that can impale the body can result in penetrating trauma, but most of these injuries are caused by gunshots or firearms (1).
According to the Centers for Disease Control and Prevention, gun-related violence in the United States is associated with seven deaths every hour (2). This results in 645 deaths and 1565 emergency department (ED) visits per week in the United States. These firearm injuries are highly lethal, accounting for 7% of premature deaths before the age of 65 years (3). Penetrating abdominal trauma affects approximately 35% of patients admitted to urban trauma centers and 1%–12% of those admitted to suburban or rural centers (4).
Before the advent of antibiotics and aseptic techniques, penetrating abdominal injuries were managed expectantly with poor outcomes. Improvements in aseptic technique during World War II increased survival in patients with penetrating abdominal trauma. Today, hemodynamic instability along with evisceration and peritonitis are indications for urgent surgical exploration. However, with progress in trauma management and the availability of minimally invasive and noninvasive tools, nonoperative treatment is increasingly being pursued in hemodynamically stable patients (5). Currently, the imaging modality of choice for evaluation of hemodynamically stable patients with penetrating trauma is contrast-enhanced CT.
High-pitch CT scanners with improved z-axis and temporal resolution provide useful anatomic information and a reduced scan time, which are excellent for guiding initial patient treatment and for following patients who are treated nonoperatively (6,7). In this review, we explore the kinetics of penetrating objects, an approach to penetrating trauma, and patterns of hollow viscus and solid-organ penetrating injuries. In addition, we discuss special considerations for performing imaging of pregnant patients with penetrating trauma and patients assessed after damage control surgery.
Basics of Ballistics
Overview of Ballistics
Ballistics is the science of projectiles, and a comprehensive understanding of penetrating trauma relies on a basic understanding of ballistics. Variables that determine initial projectile speed, flight characteristics, and the effects on a target are divided into different subfields (7). Internal and external ballistics are subfields concerned with events that occur before a projectile reaches a target. Terminal ballistics describes the effects of projectiles on a target, the sequelae of which are identified by radiologists at imaging. Here we describe features of internal, external, and terminal ballistics in further detail.
Internal Ballistics
Internal ballistics describes the events before a projectile leaves a weapon (8). This subfield is concerned with the initial generation of projectile kinetic energy, which is highly dependent on weaponry design and components. For a projectile to generate velocity, reach a target, and inflict damage, it requires adequate initial kinetic energy transfer. Central to projectile kinetic energy is the following mechanistic equation: kinetic energy = (1/2) × (mass) × (velocity)2. The kinetic energy is proportional to the velocity squared, highlighting the importance of velocity for an effective projectile (9). Different projectiles use different mechanisms to generate initial velocity. Injuries related to firearms are commonly encountered in clinical practice (2).
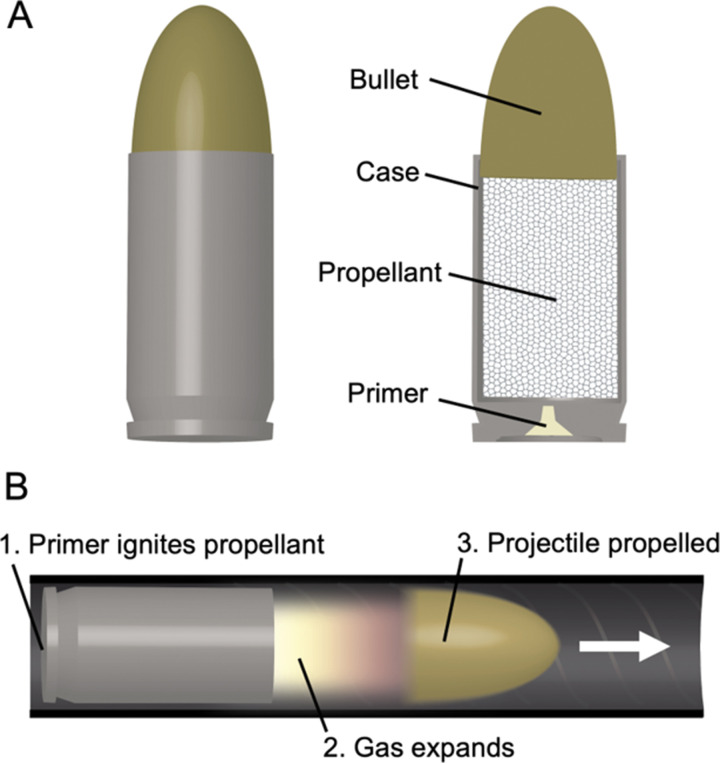
Firearms, including handguns, rifles, and shotguns, are barreled range weapons that propel projectiles with the action of expanding gas, and they are designed to be transported and operated by a single individual. A cartridge or round is the fundamental unit of firearm ammunition and contains a projectile, a propellant (eg, gunpowder), and a primer responsible for ignition, and these components are held together by a case (Fig 1, A) (10).
Figure 1.
The cartridge or round, A, is the fundamental ammunition for firearms and is composed of a projectile (bullet), a propellant, and primer held together with a case. Firing a projectile, B, requires a barrel to effectively transfer kinetic energy.
Handguns and rifles typically eject a single projectile: a bullet. Shotguns, on the other hand, can fire either a slug, which is a single projectile, or multiple projectiles known as pellets or shot. Barrels provide a means for directional transfer of kinetic energy to projectiles. Barrels are rigid structures, typically made of alloy steel, with an opening on one end that facilitates kinetic energy transfer to projectiles (Fig 1, B). To further maximize energy transmitted to pellets or shot, wadding is positioned between the propellant and the multiple small projectiles.
On ignition, the propellent combusts, and gas expansion transfers kinetic energy to the projectiles. Ultimately, weapon positioning and the initial velocity are core elements in determining a projectile’s path. Rifling, or helical grooves machined into the inner surface of a barrel, facilitates the generation of rotational kinetic energy, which is important for stabilizing projectiles during the flight (11).
External Ballistics
External ballistics is the science of projectiles in flight (9,11). Air resistance (or drag) is complex and can greatly affect a projectile from reaching the intended target. A critical component of air resistance is the projectile surface area. Features to stabilize the projectiles in flight are ultimately aimed at reducing surface area directed toward a flight path (9).
The deviation of the long axis of a projectile from the direction of flight is termed yaw, which in extreme cases, can result in tumbling during flight. This deviation of the long axis increases surface area and, in turn, drags. For firearms, as previously mentioned, rifling can impart rotational kinetic energy to bullets that can have a gyroscopic effect, maintaining a bullet’s long-axis orientation in the direction of flight. In addition, rotating bullets can exhibit precession and nutation. Precession is a change in the orientation of the rotational axis akin to the slow sweeping rotations seen in a spinning top. Contrast this with nutation, which is smaller nodding or swaging changes in the axis of rotation (9). These kinematic characteristics also play an important part in mechanisms of pathologic conditions in trauma.
Terminal Ballistics
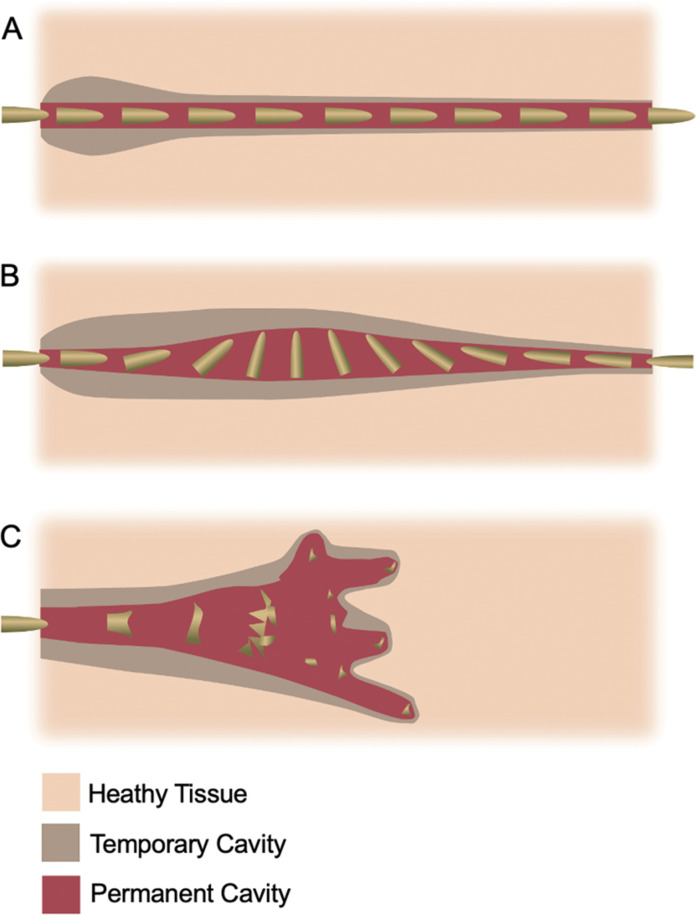
Terminal ballistics is the subfield concerned with the effects of the projectiles on targets (8,10). Terminal ballistics may be referred to as wound ballistics if the target is a person (8). In many cases, the specifics regarding the type of weapon or ammunition, which can affect the degree of injury, are unavailable to clinicians. Nonetheless, pathologic conditions in trauma are the result of kinetic energy transfer from projectiles to human tissue and depend on the projectile mass and impact velocity, the tissue encountered, projectile composition and construction, the path of travel, and if the projectile continues after traversing tissue (Fig 2).
Figure 2.
Wound ballistics refers to terminal ballistics in tissues. Penetrating injuries, A, can generate temporary and permanent cavities. Trajectory and kinetics, including yaw or tumbling, B, and projectile deformation and fragmentation,C, within tissues can affect cavity dimensions.
The deposition of a projectile’s energy can have varying effects in different tissues. For example, bone may fracture or result in a ricochet after being struck by a bullet. This may result in additional wound tracks due to the fragmentation of the projectile itself. Soft tissues lacerate if elastic limits are surpassed. A projectile can generate a permanent local cavity, but hydrostatic forces can cause more distant damage, including temporary cavities. These features can be identified at CT (12).
Like projectiles traveling outside the body, projectiles traveling inside the body can experience yaw, which increases the surface area directed toward the path of travel. Thus, more energy can be transferred to the target for a given length, and the wound cavity is widened. This concept of increased surface area to maximize the deposition of kinetic energy is the basis for projectile configurations that deform, expand, or fragment (Fig 2). For example, full metal jacket (FMJ) bullets exhibit minimal expansion compared with jacketed hollow point (JHP) bullets, which deform and fragment, thus imparting more kinetic energy in tissues (13). Radiologists should be mindful that ammunition for law enforcement and home defense is often JHP, with the aim of maximal kinetic energy deposition; thus, bullet fragmentation can commonly be seen at imaging.
Being mindful of a projectile’s path is important because that is where most kinetic energy deposits and subsequent damage occur. The described basics of ballistics play a role in the imaging approach to and sequelae of penetrating abdominal trauma as discussed in the subsequent sections.
Preimaging and CT Protocol Considerations
Prehospital stabilization and expedient patient transfer are paramount for managing critical injuries in patients with penetrating trauma. Prehospital mortality in abdominopelvic penetrating trauma is frequently secondary to exsanguination, and impaling objects should be left in place before cross-sectional imaging to rule out major vascular involvement (5,6). An impaling object involving a large artery may have a tamponade effect when left in place. Removing such an object may cause brisk hemorrhage that cannot be addressed outside of an operating room.
On arrival at the hospital, patients with penetrating abdominopelvic trauma are primarily surveyed by using the ABCDE algorithm (airway, breathing, circulation, disability, and exposure). This includes a rapid evaluation of vital signs, level of consciousness (Glasgow Coma Scale), and wound location and documentation of all entry and exit wounds.
After the primary survey, the secondary survey is performed according to the Advanced Trauma Life Support (ATLS) protocol (14). In the trauma bay, a focused assessment with sonography in trauma (FAST) examination is often performed to assess for free fluid and blood to direct patients to surgery when their condition is too unstable for CT evaluation (15). All hemodynamically stable patients then undergo imaging according to the respective institutional protocol for CT.
Trauma CT Protocol
Regardless of institutional CT protocol variation, measures to optimize injury identification can begin before the examination. At our institution, the trauma team typically marks the entry and exit wounds with an adhesive metallic BB. Contrast-enhanced CT of the chest, abdomen, and pelvis is performed with the patient’s arms positioned above the head, if possible. We perform our standard trauma CT by administering 100 mL of nonionic iodinated contrast material at a rate of 3–4 mL/sec with a fixed 70-second delay.
The axial images are reconstructed with 3-mm–thick sections and 2-mm overlap, with the option to reconstruct thinner sections as needed. Multiplanar reconstructions are generated in the sagittal and coronal planes by a technologist. Dedicated thoracolumbar spine reconstructions may be obtained from the body CT images to be reviewed separately. The images are reviewed in real time by a radiologist at the scanner in the presence of the trauma team. Additional delayed imaging may be performed, depending on abnormalities on the initial images, such as excretory phase images to evaluate for collecting system injury in renal trauma. Rectal contrast material and CT cystography are used only if indicated by the trauma mechanism or imaging findings.
Use of Enteric Contrast Material
The use of enteric contrast material in patients with trauma has garnered debate. Triple-contrast CT (combined intravenous, oral, and rectal contrast material) reportedly carries the advantage of high specificity for helping diagnose bowel perforation as identified with enteric contrast material leak. Early research and practice centered on triple-contrast CT describe sensitivity and specificity of 97% and 98%, respectively, and it is considered 98% accurate for evaluation of peritoneal violation (16).
However, there are variable reference standards reported when characterizing triple-contrast CT, and to our knowledge, there are no randomized studies (17). Disadvantages of triple-contrast CT are that it can significantly delay care, may result in aspiration, and can obscure important findings such as vascular contrast material extravasation. In addition, it increases the scan time in hemodynamically unstable patients or those who are transiently responsive to resuscitation. This may account for the decreased use of triple-contrast CT over time (18).
In our practice, we use enteric contrast material as a problem-solving tool, typically after performing single-phase CT with intravenous contrast material and imaging in the portal venous phase (17). A recent meta-analysis demonstrated that the use of enteric contrast material at CT does not provide diagnostic benefits. The researchers reported a pooled sensitivity of 83.8% and specificity of 93.8% among the enteric contrast material group, compared to a sensitivity of 93% and specificity of 90.3% in the non–enteric contrast material group (19). The use of enteric contrast material in penetrating abdominopelvic trauma is still controversial and varies on the basis of institutional preferences. Multi-institutional prospective studies may be needed to elucidate the value of enteric contrast material in imaging hemodynamically stable patients.
CT trajectography has excellent sensitivity for penetrating rectal trauma, which can be further confirmed by administering rectal contrast material. Although the leakage of rectal contrast material is specific for rectal injury, it is insensitive for ruling out rectal injury, and therefore both CT trajectography and rectal contrast material can be used as problem-solving tools (20).
Limitations exist in the use of rectal contrast material without bowel preparation that may alter the distensibility and opacification of more proximal colonic segments. The rectum and sigmoid usually have the best distensibility and opacification, and injuries in these segments are well delineated with rectal contrast material. Progressing proximally, the proportion of distensibility and opacification decreases by a greater percentage (20).
Trajectory and Its Interpretation
Suspicion for penetrating abdominopelvic trauma should be raised when encountering any skin wound within craniocaudal boundaries outlined anteriorly by the nipples to the groin crease and posteriorly from the scapulae tips to the gluteal skin crease (21). Using this approach, the diaphragm should be included in the search pattern. Diaphragmatic injury is more commonly seen with adjacent organ injuries such as stomach and spleen injuries in left-sided wounds and liver injuries in right-sided wounds. However, this article does not discuss diaphragmatic injuries in detail.
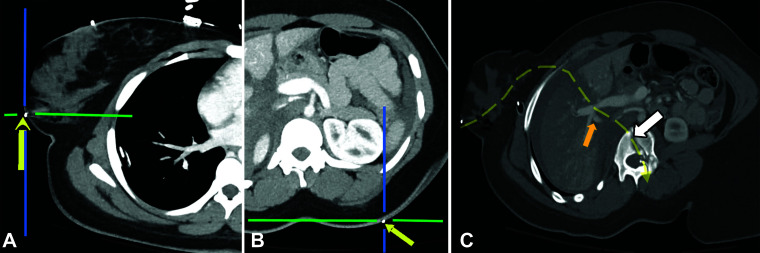
Following the path of penetrating objects is a fundamental principle of penetrating trauma CT interpretation and is termed CT trajectography, also known as CT trajectogram (22,23). In the surgical literature, trajectography is mostly described on the basis of axial CT, but there are advantages for evaluation with multiplanar oblique reconstructions (21). With the introduction of 64-section CT scanners in 2004, the acquisition of near-isotropic datasets resulted in the acquisition of the coronal and sagittal reformations, which allowed rapid evaluation of the retroperitoneal vascular column along its long axis as well as diaphragm and spinal injuries. These multiplanar reformations also helped in the trajectory evaluation in the nonstandard planes such as wound tracks with oblique orientations (22).
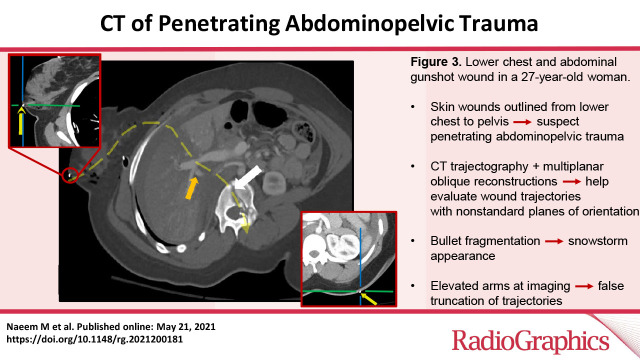
Evaluation should start at the skin surface with careful inspection of the subcutaneous fat for the bullet tract (Fig 3). Evaluation ends at the termination of the penetrating injury tract. Stranding in subcutaneous fat, bullet fragments, or beveling of the bone (inward for entry wounds and outward for the exit wounds) can sometimes be helpful if the sites are not marked with a metallic marker (23). Fragmentation of bullets can occasionally create a “snowstorm” appearance at imaging, where the area over which the fragments are deposited widens as the distance from the entry site increases, and can sometimes be used to mark the entry wound (23).
Figure 3.
Lower chest and abdominal gunshot wound in a 27-year-old woman. A, B, Axial CT trajectograms depict the external BBs marking the entry wound in the right breast (arrow in A) and the exit wound in the dorsal left midback (arrow in B). After localizing the entry and exit wounds, the cut planes are swiveled obliquely in orthogonal planes to obtain a double-oblique orientation in which the wound track is visualized in profile. These points are used to create a curved multiplanar reconstruction. C, Curved multiplanar reconstruction from CT that was created along the pathway of the ballistic injury (dashed yellow arrow) demonstrates soft-tissue gas in the right breast (there was no intrathoracic or diaphragmatic violation), portal vein confluence extravasation centered in the grade V liver injury (orange arrow), and an L1 burst fracture (white arrow). The exit wound metallic marker (not shown) was located one section above that shown in C.
After the entry and exit wounds are delineated, the two points can be connected by placing cross-cursors and rotating the cut planes obliquely in orthogonal planes to obtain a double-oblique orientation to visualize the wound track in profile (23). Commercially available software packages can help perform the multiplanar reformations in oblique and curved trajectories. Using a Cartesian coordinate system, it has shown strong interreader agreement in trauma-related findings (24–26).
Trajectography is specific but not sensitive, and trajectories should not be strictly extrapolated on the basis of surface wounds, as trajectography is subject to various pitfalls. Bullets often exhibit yaw and can ricochet, which can greatly alter trajectories (21,23). In addition, positioning the patient on the scanner with arms elevated can falsely truncate the trajectories and does not mimic the position of the patient when the trauma occurred (23). Breathing can alter the trajectories of the bullet, and breathing motion can induce artifact at CT, which may further change the trajectory interpretation (22,23).
Profiling the trajectory can help identify organs in the vicinity that may be subject to blast injury secondary to shock waves, which may not be readily apparent at imaging (21). In addition, patients with trauma from firearms may have been shot multiple times, and interpreting physicians should be on alert for possible multiple tracts. After assessing the projectile tract or tracts, the radiologist can then resume a normal CT search pattern for other injuries and incidental findings (21).
Imaging Signs of Peritoneal Violation: Depiction of Free Fluid
Depiction of free fluid or blood is the basis of the FAST examination and usually prompts surgical exploration or further imaging (15). Accurate characterization of free fluid is vital for trauma CT interpretation, as imaging features can help differentiate blood from less ominous findings.
Free fluid can be either simple, with attenuation values ranging between –10 and 10 HU, or it can be hyperattenuating blood with attenuation values ranging between 30 and 70 HU (clotted blood ranging between 45 and 70 HU and unclotted blood ranging between 30 and 45 HU). However, in coagulopathic acute trauma in patients who are being aggressively resuscitated, these absolute values may pose a dilemma and therefore should be used with caution.
The simple fluid has characteristic locations in certain circumstances, usually seen in small volumes layering in the dependent portions such as the cul-de-sac, paracolic gutters, or Morison pouch (Fig 4). Trace free fluid in premenopausal women is often physiologic (21,27). However, trace free fluid in men can pose a diagnostic dilemma and in most cases warrants surgical exploration when there is additional evidence of the peritoneal violation. Trace free fluid in males with attenuation values less than 10 HU below the S3 level has been shown to not be associated with mesenteric or bowel injury, according to studies of patients with blunt trauma (27). However, in the presence of peritoneal violation and a trajectory including the bowel or bladder, simple free fluid can be representative of extraluminal urine or bowel contents. Simple free fluid may also be difficult to interpret in patients with underlying heart, kidney, or liver disease leading to third spacing.
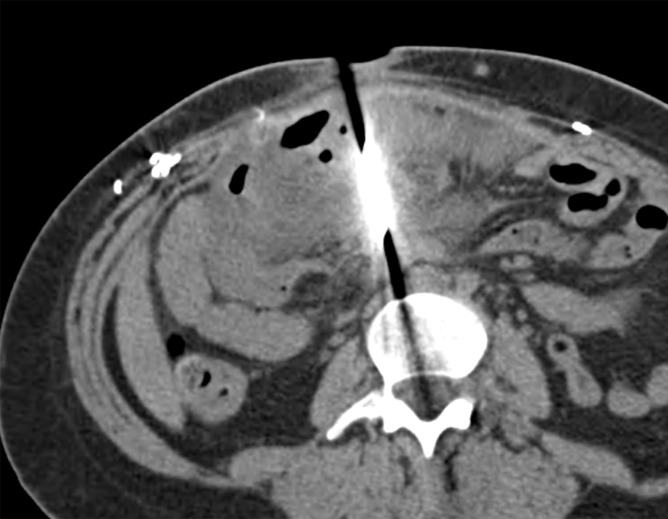
Figure 4a.
Axial contrast-enhanced CT images of the abdomen and pelvis in a 56-year-old man with gunshot trauma to the abdomen show simple attenuating free fluid (arrow) in the dependent portions, which are the cul-de-sac (a) and Morison pouch (b).
Figure 4b.
Axial contrast-enhanced CT images of the abdomen and pelvis in a 56-year-old man with gunshot trauma to the abdomen show simple attenuating free fluid (arrow) in the dependent portions, which are the cul-de-sac (a) and Morison pouch (b).
Hemoperitoneum is a more specific finding for ballistic injury in the peritoneal cavity. This may manifest with a sentinel clot sign or hematocrit effect. The sentinel clot sign implies that the anatomic site of hemorrhage lies nearest the highest-attenuation portion of the clot (Fig 5a). Hematocrit effect refers to clotted blood layering dependently within the hemoperitoneum (blood-clot level) (Fig 5b) (28). Hemoperitoneum may be missed in patients with anemia, who can have lower attenuation values of blood. Even in individuals without anemia, approximately 24% of patients can have regions of hemoperitoneum where attenuation values can measure below 30 HU. Preexisting ascites (for example, in renal failure) can also enhance at delayed imaging because of transperitoneal excretion of iodine and can lead to high-attenuation ascites, leading to a misdiagnosis of hemoperitoneum (28).
Figure 5a.
Axial CT images of the abdomen and pelvis in a 38-year-old man with penetrating trauma to the chest and abdomen demonstrate two manifestations of hemoperitoneum with the sentinel clot sign (arrow in a) and the hematocrit effect (arrow in b).
Figure 5b.

Axial CT images of the abdomen and pelvis in a 38-year-old man with penetrating trauma to the chest and abdomen demonstrate two manifestations of hemoperitoneum with the sentinel clot sign (arrow in a) and the hematocrit effect (arrow in b).
The utility of pneumoperitoneum as an imaging sign in penetrating trauma is imperfect, as air can gain access into the peritoneal cavity through the penetrating object’s tract. It is surprisingly uncommon in patients with peritoneal injury and is seen in only one-third of patients with documented intraperitoneal injury (but is not specific for visceral injury when present) (21).
Regional Injuries
Deposition of kinetic energy by penetrating objects, projectiles or otherwise, generates indirect or direct imaging findings. Direct signs are more specific and diagnostic for an injury, whereas indirect signs are more sensitive. In the subsequent sections, we provide examples of how different direct or indirect imaging findings for different abdominopelvic organ systems can aid in diagnosis. In any case, the most critical task when evaluating for injury in patients with penetrating trauma is determining the wound trajectory.
Hollow Viscera Injury
Injuries to hollow viscera are common in penetrating trauma, occurring in 63% of patients (17). Identifying these injuries at CT can be challenging. Therefore, a high index of suspicion and familiarity with direct and indirect signs of bowel injury are critical.
Small Bowel and Colonic Injuries.—Direct signs of bowel injury include discontinuity of the bowel wall and mural hematoma. Focal discontinuity of the bowel wall is a highly specific (99%) sign of bowel injury but may be seen in only approximately 43% of patients with bowel injury (29). Often the focus of discontinuity is accompanied by adjacent pneumoperitoneum or mesenteric stranding, further emphasizing the injury (Fig 6). Focal wall thickening representing a mural hematoma is reported to be the most accurate sign of bowel injury in the setting of penetrating trauma (sensitivity 74%, specificity 95%) (29). A focal bowel wall hematoma is often associated with adjacent mesenteric stranding or hematoma (Fig 7). More diffuse bowel wall thickening is likely secondary to systemic volume overload from resuscitation or shock bowel from hypoperfusion rather than traumatic injury (30).
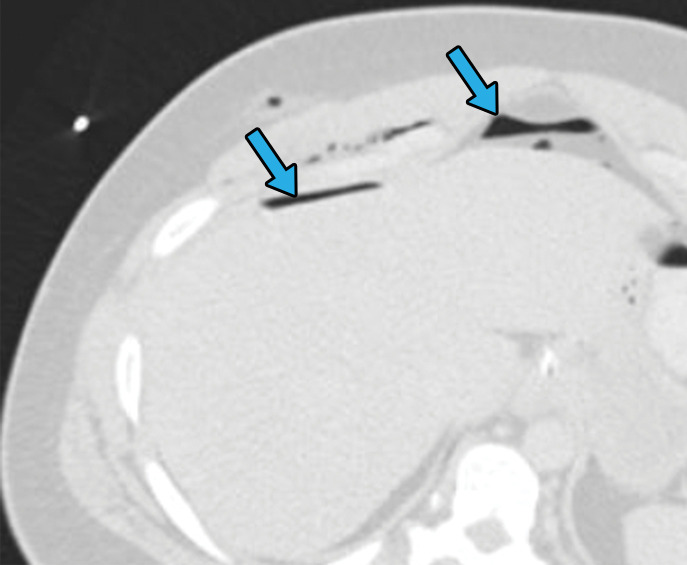
Figure 6a.
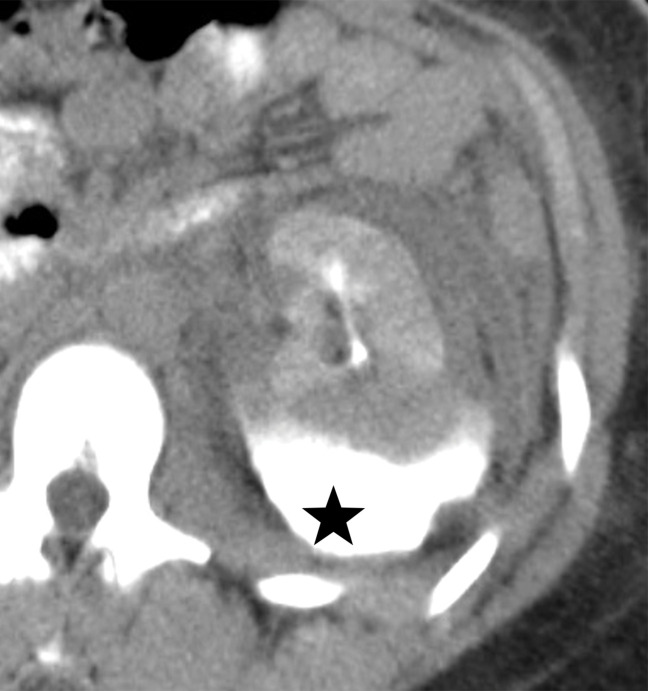
Axial CT images of the abdomen and pelvis with lung window (a) and soft-tissue window (b) in a 24-year-old man who presented with a penetrating gunshot injury demonstrate pneumoperitoneum (blue arrows in a) secondary to cecal injury, as demonstrated by focal bowel wall discontinuity (yellow arrow in b) with adjacent free air (☆ in b).
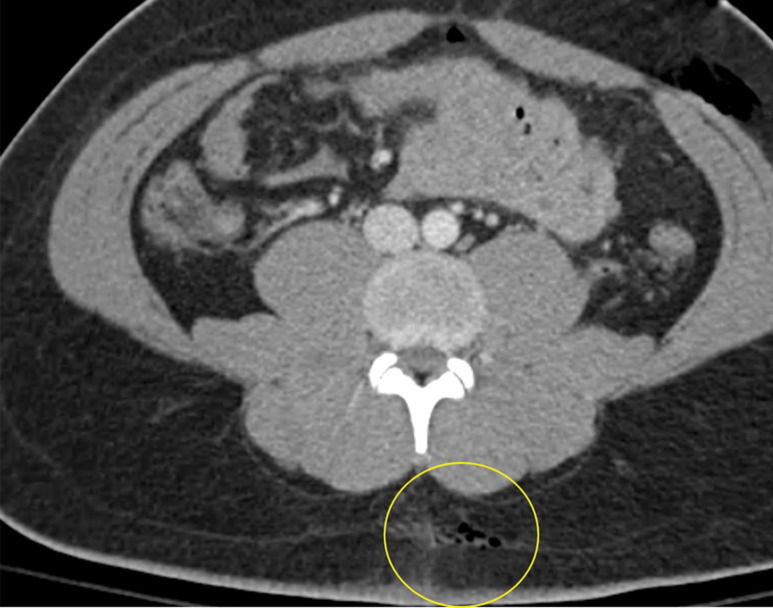
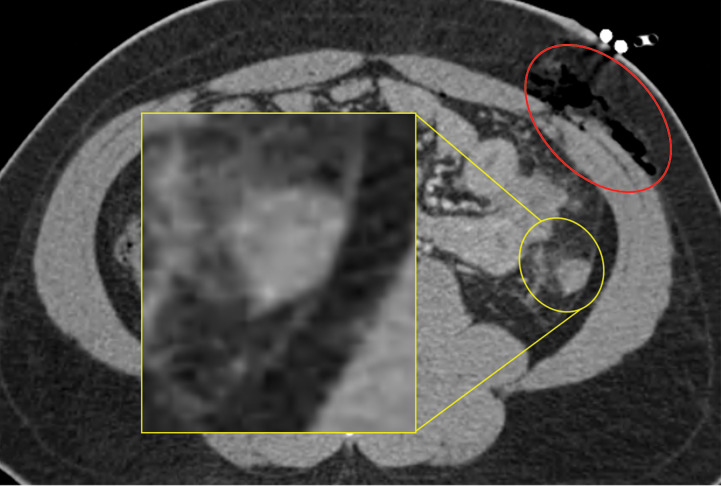
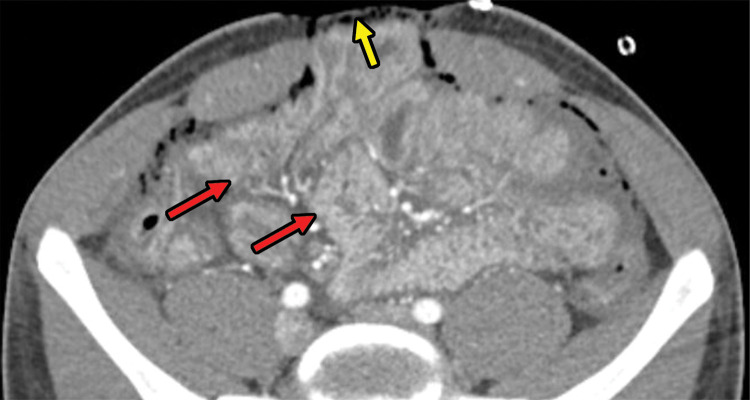
Figure 7a.
Gunshot injury in a 21-year-old man. Axial contrast-enhanced CT images of the abdomen and pelvis demonstrate foci of gas within the subcutaneous fat, indicating the entry wound (yellow circle in a) and exit wound (red oval in b). In the path of the bullet trajectory (not double oblique orientation), there is evidence of bowel injury, as indicated by focal bowel wall thickening and surrounding stranding (yellow circle in b), which is magnified for clarity (inset in b).
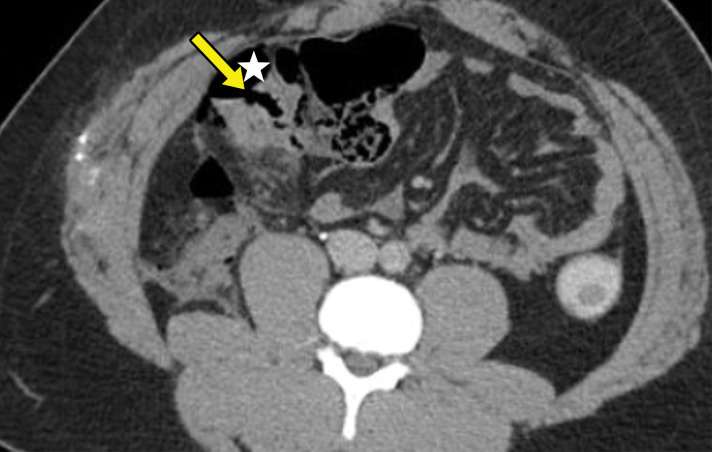
Figure 6b.
Axial CT images of the abdomen and pelvis with lung window (a) and soft-tissue window (b) in a 24-year-old man who presented with a penetrating gunshot injury demonstrate pneumoperitoneum (blue arrows in a) secondary to cecal injury, as demonstrated by focal bowel wall discontinuity (yellow arrow in b) with adjacent free air (☆ in b).
Figure 7b.
Gunshot injury in a 21-year-old man. Axial contrast-enhanced CT images of the abdomen and pelvis demonstrate foci of gas within the subcutaneous fat, indicating the entry wound (yellow circle in a) and exit wound (red oval in b). In the path of the bullet trajectory (not double oblique orientation), there is evidence of bowel injury, as indicated by focal bowel wall thickening and surrounding stranding (yellow circle in b), which is magnified for clarity (inset in b).
Extraluminal leakage of oral or rectal contrast material is a highly specific but uncommon finding of bowel injury in penetrating trauma, occurring in only 14%–29% of bowel injuries (16,18,31,32). In addition to the low sensitivity of extraluminal contrast material leakage, administration of oral contrast material can lead to a potential delay in diagnosis, as it takes at least 30 minutes to opacify the small bowel after the administration of oral contrast material. To a lesser degree, the administration of rectal contrast material also delays imaging because of the time it takes to prepare and instill the contrast agent. Pneumoperitoneum is not a reliable sign of bowel injury in penetrating trauma, as intraperitoneal air is almost always introduced during peritoneal violation and limits specificity (16,31).
One of the most sensitive indirect signs of bowel injury is a wound tract extending adjacent to a segment of bowel, which is seen in 69%–94% of patients with a bowel injury (Fig 8) (16,18,31). A wound tract that approaches close to a loop of bowel can also result in bowel injury secondary to a shock wave or a temporary cavity created by medium- and high-energy projectiles (21,33). This may result in a contusion or serosal injury without luminal perforation but still warrants surgical exploration and potential repair.
Figure 8a.
Bowel perforation in a 29-year-old man with a penetrating stab wound by a knife. Axial CT image of the abdomen and pelvis (a) and sagittal reconstruction from CT (b) demonstrate the knife penetrating the mesentery and bowel. There is no question whether bowel or mesenteric trauma exists, even in the absence of free air. The bowel perforation was confirmed at laparotomy.
Figure 8b.

Bowel perforation in a 29-year-old man with a penetrating stab wound by a knife. Axial CT image of the abdomen and pelvis (a) and sagittal reconstruction from CT (b) demonstrate the knife penetrating the mesentery and bowel. There is no question whether bowel or mesenteric trauma exists, even in the absence of free air. The bowel perforation was confirmed at laparotomy.
Anorectal Injury.—The indirect and direct signs of rectal injury are identical to those discussed for small bowel and colonic injury. As in other segments of the gastrointestinal tract, a projectile path through or adjacent to the rectum is the most sensitive direct sign of bowel injury (24). A focal wall defect is a highly specific but uncommon sign of rectal injury, while mural hematoma is a highly accurate sign of injury (Fig 9) (29,34). Indirect signs include perirectal fat stranding and hematoma (34).
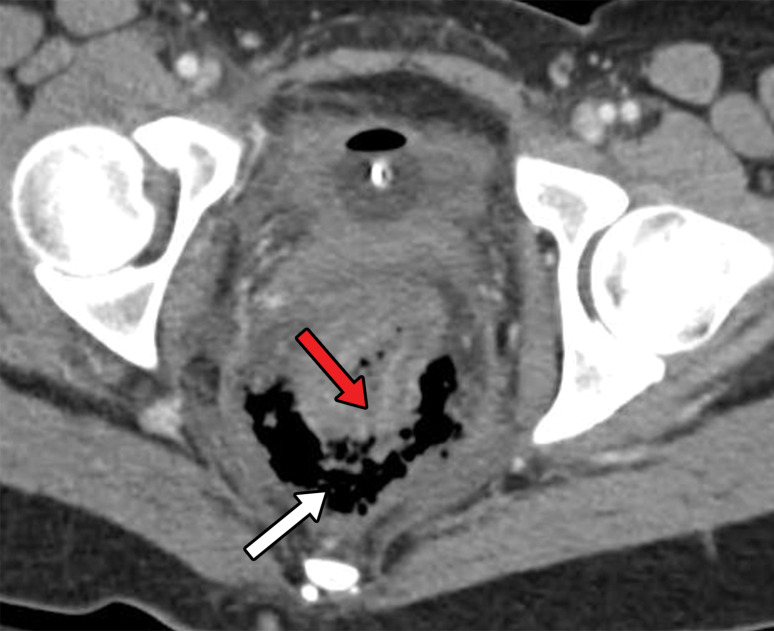
Figure 9a.
Axial CT images with intravenous contrast material obtained before (a) and after (b) the administration of rectal contrast material in a 27-year-old man with penetrating rectal trauma from a foreign body show a transmural defect (red arrow) with a focal collection of free air (white arrow in a) that was confirmed with rectal contrast material, demonstrating extraluminal leakage through the defect in b.
Figure 9b.
Axial CT images with intravenous contrast material obtained before (a) and after (b) the administration of rectal contrast material in a 27-year-old man with penetrating rectal trauma from a foreign body show a transmural defect (red arrow) with a focal collection of free air (white arrow in a) that was confirmed with rectal contrast material, demonstrating extraluminal leakage through the defect in b.
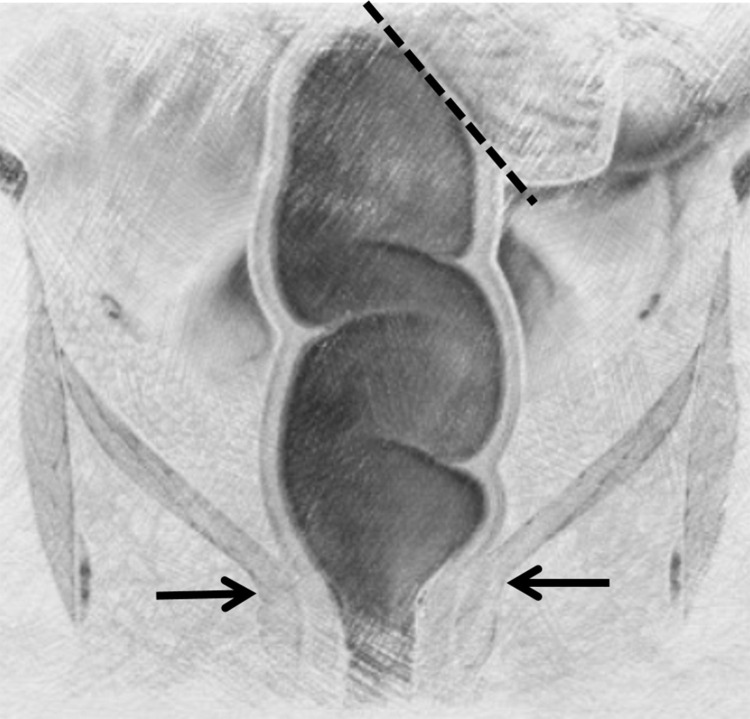
When evaluating anorectal trauma, there are important anatomic considerations that guide surgical management (Fig 10). The rectosigmoid junction is defined by the confluence of the tenia coli muscles, which are located approximately at the level of the sacral promontory. The anorectal junction is defined as the dentate line that is located approximately at the level of the levator ani at CT. The distal third of the rectum is extraperitoneal. The posterior portion of the upper two-thirds of the rectum is extraperitoneal, while the anterior portion is intraperitoneal (34).
Figure 10.
Diagram of anorectal anatomy demonstrates the proximal aspect of the rectum, which is defined by the confluence of the tenia coli muscles along the serosal aspect of the sigmoid colon (dashed line). The anorectal junction is at the dentate line (arrows), which is roughly inferred by the position of the levator ani muscle. Rectal anatomy is pertinent when interpreting CT images, as the level of injury may change management.
It is important to make the distinction of whether a rectal injury is intraperitoneal or extraperitoneal. Intraperitoneal injuries are commonly treated with primary surgical repair and fecal diversion. On the other hand, extraperitoneal rectal injuries are often treated with fecal diversion only (24,25). Extraperitoneal rectal injuries are far more common, representing 93% of penetrating rectal injuries, with most occurring in the lower one-third of the rectum (24).
Mesenteric Injury.—Direct signs of mesenteric injury include narrowing or occlusion of mesenteric vessels, beading of the vessels, and active extravasation from mesenteric vessels. A pseudoaneurysm may be suggested by the beading or irregularity of the mesenteric vessels, which is seen in 39% of patients with mesenteric injury (35). Active extravasation from the mesentery has specificity approaching 100%, but sensitivity is limited to less than 20% for mesenteric injury (35). Active extravasation from the mesentery is an indication for emergent laparotomy. Active extravasation is often accentuated with delayed contrast phases by pooling of contrast material within a mesenteric hematoma (30).
Indirect signs of mesenteric injury include intramesenteric free fluid or blood. Intramesenteric free fluid often appears in a triangular or polygonal configuration as it interdigitates between the mesenteric leaves. Other indirect signs of mesenteric injury include fat stranding or mesenteric mistiness (35).
Urinary Bladder Injury.—Urinary bladder injury is relatively uncommon in penetrating trauma. Bladder injuries occur in approximately 4% of abdominal gunshot wounds (36). When there is a concern for urinary bladder injury in penetrating trauma, the patient should be further evaluated with CT cystography (sensitivity and specificity of 95% and 100%, respectively, for depicting bladder rupture, similar to those for conventional cystography) (37–40). Findings at single-contrast CT that should prompt evaluation with CT cystography include a wound track coursing near or through the bladder (direct sign) and unexplained free fluid in the pelvis, hemorrhage in the space of Retzius, and gross or microscopic hematuria (>25 red blood cells per high-power field), which are indirect signs (40,41).
At our institution, the protocol for CT cystography is as follows. First, the patient is evaluated for urethral injury. Signs of urethral injury include blood at the urethral meatus, suprapubic fullness, urinary retention, and high-riding prostate. If there is any concern for urethral injury, a urologic consult is obtained, and the patient is evaluated with retrograde urethrography. Any attempt to pass a Foley catheter could worsen the urethral injury when present (39). Once a urethral injury has been excluded, a Foley catheter is inserted, and the urinary bladder is drained.
Next, 350 mL of iodinated water-soluble contrast material that is diluted to 3%–5% with normal saline is instilled into the urinary bladder under gravity. The infusion continues until the patient reports severe discomfort due to bladder distention or the infusion stops dripping with gravity. Passive filling of the bladder (through antegrade excretion of contrast material that was intravenously administered during CT) is not adequate to depict bladder rupture because of inadequate bladder distention. Axial CT is then performed from the level of the iliac crests to the level of the femoral lesser trochanters, utilizing 0.5–1-mm-thick sections. Reformatted coronal and sagittal reconstructions are made. CT cystography is always performed after single-contrast CT to help avoid diagnostic uncertainty as to the source of intraperitoneal gas or contrast material (30).
At CT, bladder injuries are classified into five types (40). A type 1 injury is a bladder contusion that is characterized by the thickening of the urinary bladder wall. A type 2 injury is an intraperitoneal bladder rupture where extraluminal contrast material from the urinary bladder can be seen outlining loops of the bowel as well as in the paracolic gutters and the cul-de-sac (38,40). A type 3 injury is an interstitial bladder injury characterized by bladder wall thickening with intraluminal contrast material dissecting into the bladder wall without extension into the extraperitoneal or intraperitoneal spaces. A type 4 injury is an extraperitoneal bladder rupture that can be further classified as simple or complex. In a simple extraperitoneal rupture, extraluminal contrast material is confined to the space of Retzius (Fig 11). In a complex rupture, the fascia is violated, and contrast material may extend into the anterior abdominal wall, penis, scrotum, perineum, or thighs (38,40). A type 5 injury is a combined intraperitoneal and extraperitoneal rupture (40).
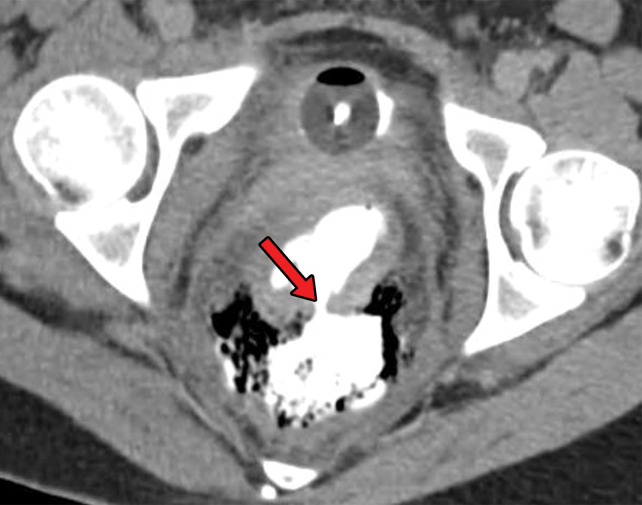
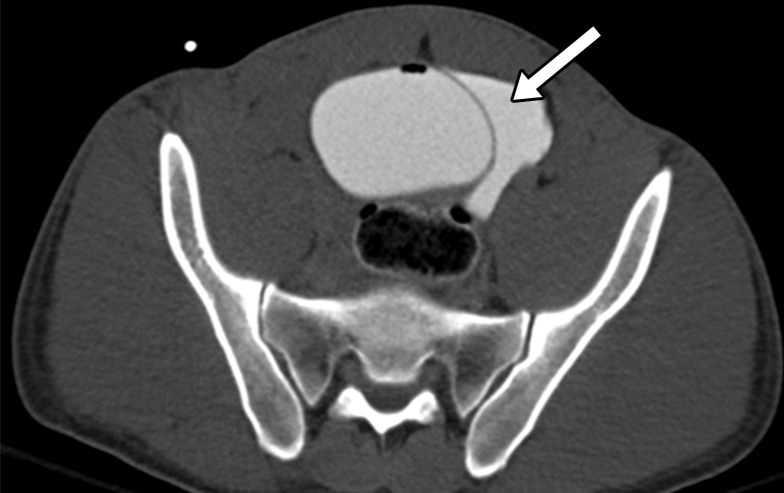
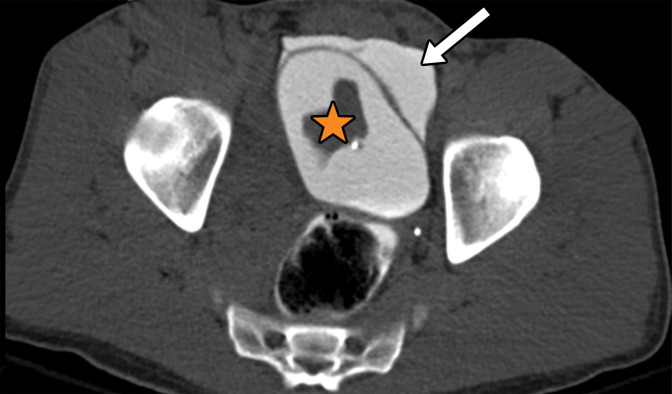
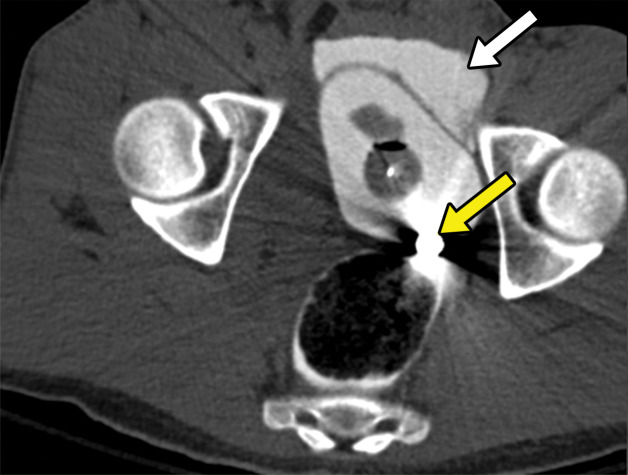
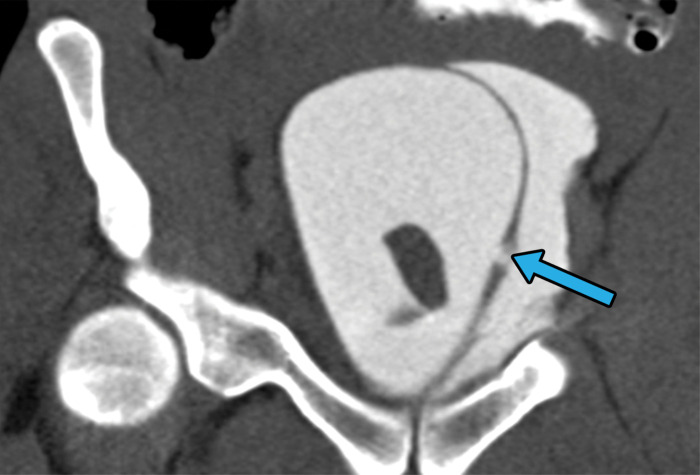
Figure 11a.
Extraperitoneal bladder injury in a 27-year-old man with a gunshot wound to the right buttock. Axial CT cystograms of the pelvis demonstrate a single bullet within the bladder lumen (yellow arrow in c). There is extraperitoneal extravasation of contrast material from the bladder into the space of Retzius (white arrow in a–c). An extraperitoneal rupture can be seen in the left lateral wall of the bladder (blue arrow in d). The extraluminal contrast material is confined to the pelvic space, which is consistent with a type 4b injury. An intraluminal hematoma can be seen (☆ in b). The patient underwent surgical repair for this extraperitoneal bladder injury during a laparotomy for small bowel injury.
Figure 11b.
Extraperitoneal bladder injury in a 27-year-old man with a gunshot wound to the right buttock. Axial CT cystograms of the pelvis demonstrate a single bullet within the bladder lumen (yellow arrow in c). There is extraperitoneal extravasation of contrast material from the bladder into the space of Retzius (white arrow in a–c). An extraperitoneal rupture can be seen in the left lateral wall of the bladder (blue arrow in d). The extraluminal contrast material is confined to the pelvic space, which is consistent with a type 4b injury. An intraluminal hematoma can be seen (☆ in b). The patient underwent surgical repair for this extraperitoneal bladder injury during a laparotomy for small bowel injury.
Figure 11c.
Extraperitoneal bladder injury in a 27-year-old man with a gunshot wound to the right buttock. Axial CT cystograms of the pelvis demonstrate a single bullet within the bladder lumen (yellow arrow in c). There is extraperitoneal extravasation of contrast material from the bladder into the space of Retzius (white arrow in a–c). An extraperitoneal rupture can be seen in the left lateral wall of the bladder (blue arrow in d). The extraluminal contrast material is confined to the pelvic space, which is consistent with a type 4b injury. An intraluminal hematoma can be seen (☆ in b). The patient underwent surgical repair for this extraperitoneal bladder injury during a laparotomy for small bowel injury.
Figure 11d.
Extraperitoneal bladder injury in a 27-year-old man with a gunshot wound to the right buttock. Axial CT cystograms of the pelvis demonstrate a single bullet within the bladder lumen (yellow arrow in c). There is extraperitoneal extravasation of contrast material from the bladder into the space of Retzius (white arrow in a–c). An extraperitoneal rupture can be seen in the left lateral wall of the bladder (blue arrow in d). The extraluminal contrast material is confined to the pelvic space, which is consistent with a type 4b injury. An intraluminal hematoma can be seen (☆ in b). The patient underwent surgical repair for this extraperitoneal bladder injury during a laparotomy for small bowel injury.
Appropriate classification of bladder injuries is important in directing management. Types 1 and 3 injuries are managed conservatively, often with urinary drainage through a Foley catheter until the injury has healed. Type 4 injuries are initially managed conservatively with urinary drainage. If the injury fails to heal with conservative management, surgical repair may be indicated. Indications for immediate surgical repair of a type 4 injury include concomitant bladder neck injury, rectal or vaginal injury, open pelvic fracture, or fragments of bone projecting into the bladder. Types 2 and 5 bladder injuries require immediate surgical primary bladder repair (39,40).
Solid-Organ Injuries
Many patients with penetrating solid-organ injuries (such as liver, spleen, kidneys, and pancreas) are in an unstable condition and can have other indications for laparotomy. However, with the improved care in resuscitation and immediate availability of interventional vascular management, a subset of these solid-organ injuries can be managed nonoperatively. Injuries to solid viscera are graded on the basis of the American Association for the Surgery of Trauma (AAST) injury scoring scale that was most recently revised in 2018 for spleen, liver, and kidney injuries (42) (Figs E1–E4). While this grading scale relies on surgical evaluation, CT estimates for the surgical grade are concordant with these scales and therefore help in determining when nonsurgical management can be pursued (21,42).
Because of the increasing utilization of nonsurgical management of solid-organ injuries, correct characterization in the CT report is of vital importance (42). For example, in liver trauma, radiologists should describe hepatic hematoma size as an approximate percentage of the surface area as well as its location (either intraparenchymal or subcapsular); laceration (usually seen as an ill-defined, linear, round, or ovoid region of hypoattenuation at CT) measured in centimeters; number of involved liver segments; and relationship to major central veins (juxtavenous injury) (Fig 12).
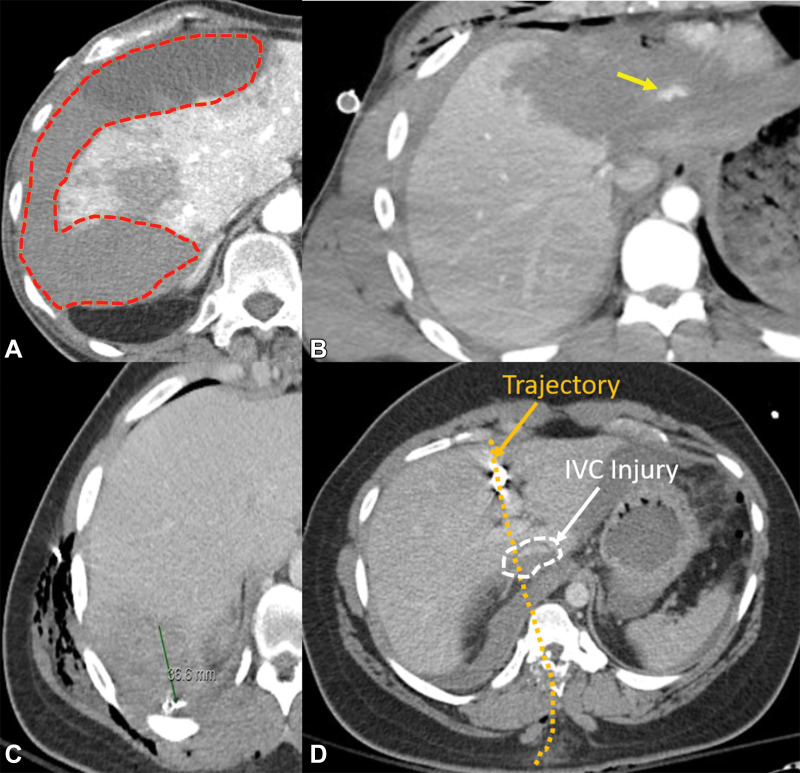
Figure 12.
Description of various imaging features that may help in grading liver injury. Axial CT images depict hematoma (orange outline in A), active extravasation (arrow in B), laceration (green line indicating ruler in C), and juxtavenous injury (white arrow and dashed circle in D). The trajectory is superimposed (orange arrow and orange dotted line in D). IVC = inferior vena cava.
The 2018 addition of vascular injuries to the AAST grading of liver, spleen, and kidney injuries now allows a radiologist to more confidently apply an injury grade. Vascular injuries include pseudoaneurysm, active bleeding, and arteriovenous fistula (42,43). In addition to these descriptors, description in splenic trauma should state whether the trajectory approaches the splenic hilum and report any signs of vascular injury or shattered spleen (Fig 13). For liver and spleen injuries, advance one grade for multiple injuries up to grade III, and for renal injuries advance one grade for bilateral injuries up to grade III (42,43). For renal injuries, a laceration that approaches the collecting system should always be imaged in the delayed phase to assess for urine leak, as it can upgrade an AAST grade to grade IV if a collecting system injury is present and may change the patient’s treatment (Fig 14). Any renal injury in the presence of vascular injury or active bleeding contained within the Gerota fascia is considered a grade III injury (42,43).
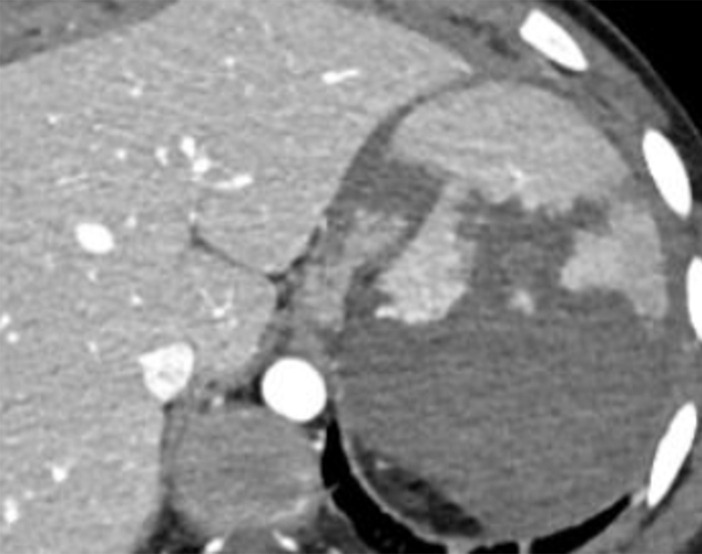
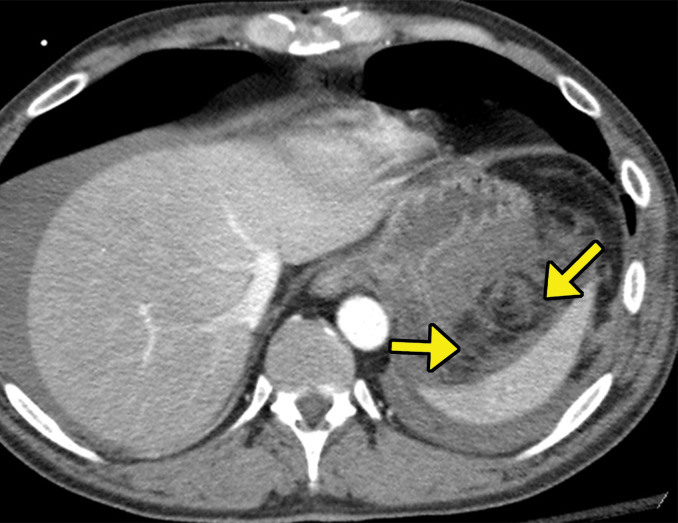
Figure 13a.
Descriptors of imaging features of splenic injury that may help in grading the splenic trauma, in addition to what has been described with liver injury patterns. Axial CT images demonstrate a shattered spleen (a) and a traumatic pseudoaneurysm (arrow in b).
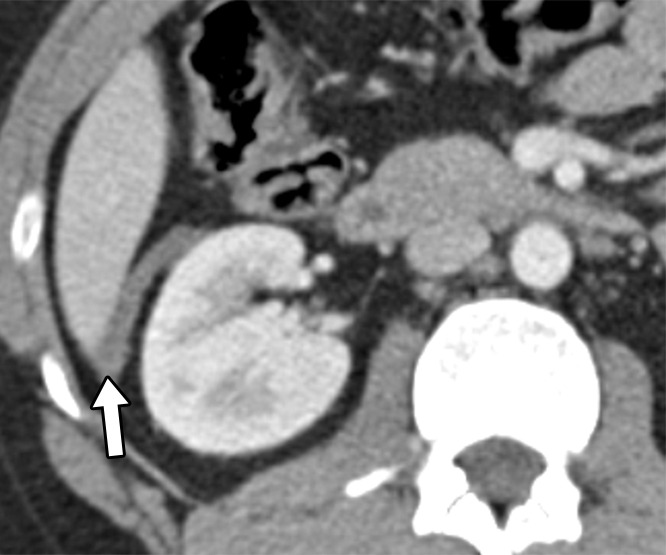
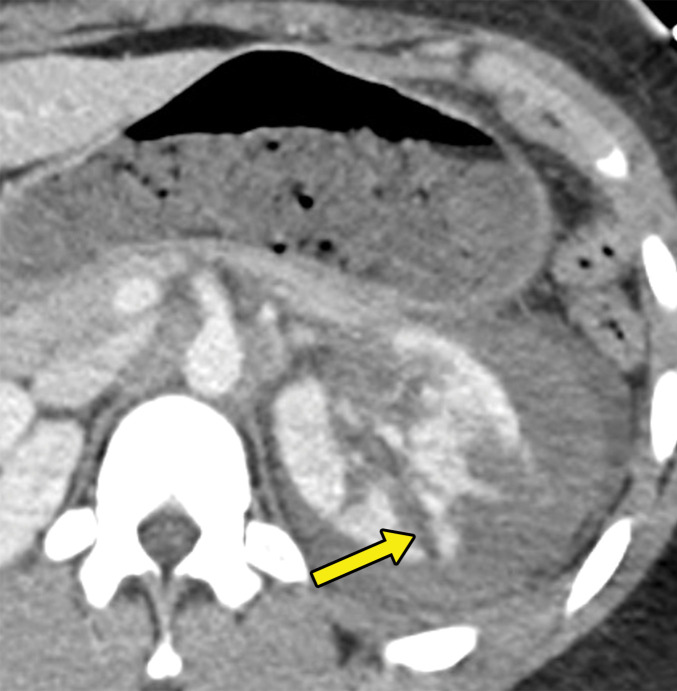
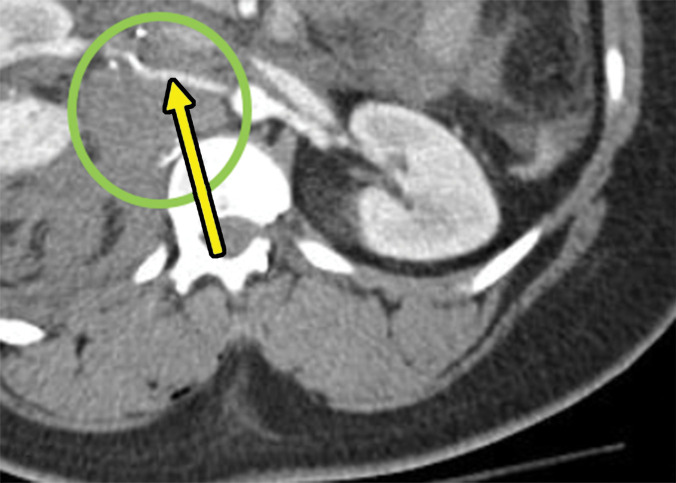
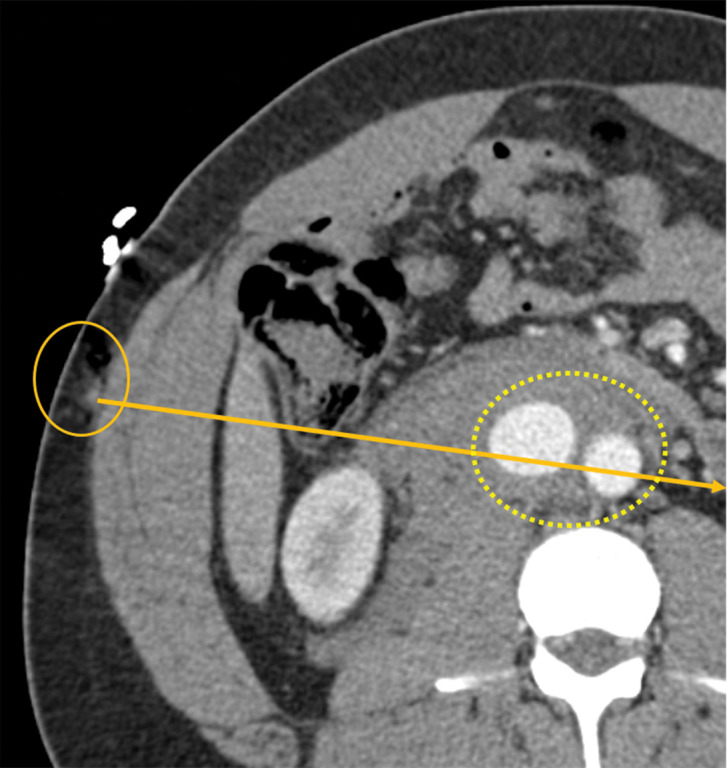
Figure 14a.
Collecting system injury in a 26-year-old woman with a penetrating injury to the left flank. (a) Axial contrast-enhanced CT image of the abdomen demonstrates multiple left renal lacerations with perinephric hematoma. One of these lacerations approaches the collecting system (arrow), which raises the concern for a collecting system injury. (b) Axial contrast-enhanced delayed phase CT image that was obtained for confirmation demonstrates excretion of the contrast material into the perinephric space (⋆), which is a finding consistent with collecting system renal injury.
Figure 13b.
Descriptors of imaging features of splenic injury that may help in grading the splenic trauma, in addition to what has been described with liver injury patterns. Axial CT images demonstrate a shattered spleen (a) and a traumatic pseudoaneurysm (arrow in b).
Figure 14b.
Collecting system injury in a 26-year-old woman with a penetrating injury to the left flank. (a) Axial contrast-enhanced CT image of the abdomen demonstrates multiple left renal lacerations with perinephric hematoma. One of these lacerations approaches the collecting system (arrow), which raises the concern for a collecting system injury. (b) Axial contrast-enhanced delayed phase CT image that was obtained for confirmation demonstrates excretion of the contrast material into the perinephric space (⋆), which is a finding consistent with collecting system renal injury.
Pancreatic injuries are difficult to delineate, and trajectography helps determine the presence of pancreatic injury. Any trajectory leading up to or traversing the pancreas is the most sensitive CT finding and requires exploration preoperatively even when other major surgical injuries are absent because of serious consequences associated with missed injuries. Observing linear lacerations through the pancreatic parenchyma, peripancreatic stranding or fluid, and the presence of duct disruption are more specific signs of pancreatic trauma (Fig 15) (21,42). Lacerations involving more than 50% of the pancreatic parenchyma are considered major lacerations, which suggest an underlying pancreatic duct injury and are higher grade. Pancreatitis, contusions, and lacerations involving less than 50% of the parenchyma are considered lower-grade injuries (44).
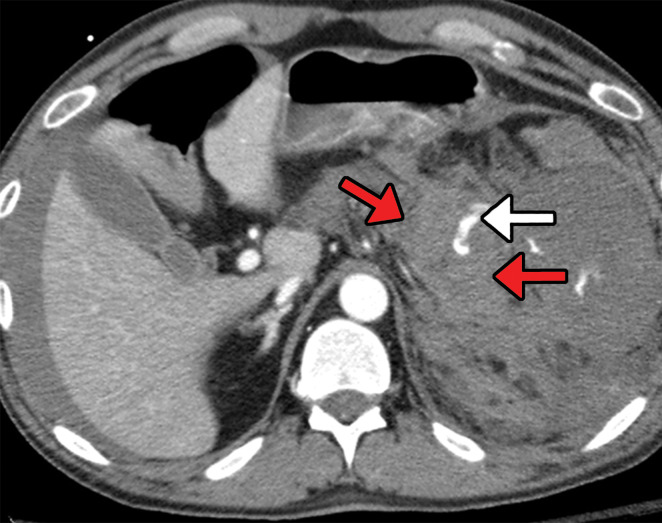
Figure 15a.
Multiple gunshot wounds with pancreatic transection in a 40-year-old man. (a) Axial contrast-enhanced CT image of the abdomen and pelvis demonstrates pancreatic laceration (red arrows) with active extravasation (white arrow), indicating direct signs of pancreatic injury. (b) Axial contrast-enhanced CT image shows extensive peripancreatic stranding extending toward the splenic hilum (yellow arrows), which is an indirect sign of pancreatic injury.
Figure 15b.
Multiple gunshot wounds with pancreatic transection in a 40-year-old man. (a) Axial contrast-enhanced CT image of the abdomen and pelvis demonstrates pancreatic laceration (red arrows) with active extravasation (white arrow), indicating direct signs of pancreatic injury. (b) Axial contrast-enhanced CT image shows extensive peripancreatic stranding extending toward the splenic hilum (yellow arrows), which is an indirect sign of pancreatic injury.
Vascular Injuries
Abdominopelvic vascular trauma is life threatening and, in the majority of cases, is associated with penetrating injuries. The mortality rate for these injuries is high, ranging between 20% and 60%, with early deaths that are secondary to massive hemorrhage and late deaths that are attributed to multisystem organ failure and shock (45–47). In contrast to blunt trauma, where vascular injuries are seen 5%–10% of the time, penetrating trauma due to stab and gunshot wounds results in vascular injuries in 10% and 20%–25% of the cases, respectively (48). The most common vascular injuries related to penetrating abdominal trauma involve the abdominal aorta, superior mesenteric artery, iliac arteries and veins, inferior vena cava, and portal veins (45).
Most penetrating vascular injuries occur because of laceration by the impaling object. In gunshot wounds, additional damage may occur because of the blast effect. The majority of abdominal vascular injuries manifest with either a through-and-through transection of the vessel or partial-thickness wall defects, which can result in either nonpulsatile (venous) hematomas or pulsatile and expanding (arterial) hematomas when explored surgically (48,49). Vascular transection is rarely seen at imaging, as most patients exsanguinate before they arrive at the trauma bay. Those that do arrive at the hospital are often too hemodynamically unstable to undergo imaging and go straight to the operating room. In addition to hemorrhage, penetrating vascular trauma can result in arterial occlusion and end-organ damage, which may be remote from the site of trauma (48,49).
The imaging findings related to a vascular injury at CT may be classified as direct or indirect (Fig 16). Indirect signs, which are sensitive but less specific, include abnormalities of the perivascular tissues or end organs and include the presence of a perivascular hematoma or fat stranding and varying degrees of end-organ ischemia (50). Direct signs, which are more specific but less sensitive in the depiction of vascular trauma, include laceration with active hemorrhage, an intraluminal flap of tissue, thrombosis, pseudoaneurysm, caliber narrowing, presence of arteriovenous fistulas, and bullet embolism (50). Depiction of active extravasation at CT is an important prognostic indicator, necessitating life-saving emergent surgery or interventional vascular treatment (51) (Fig 17).
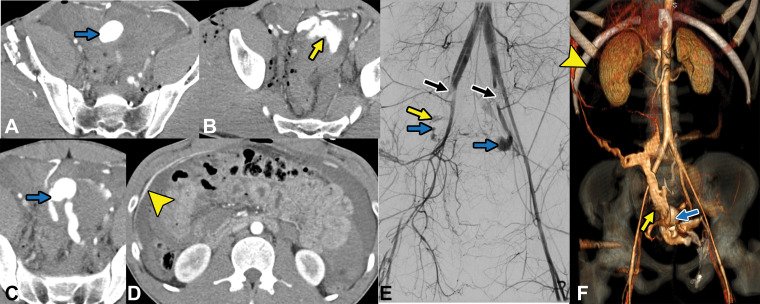
Figure 16a.
Direct and indirect signs of vascular injury in four patients. (a) Axial contrast-enhanced CT image of the abdomen and pelvis in a 34-year-old woman with a gunshot injury to the right flank demonstrates hematoma (circle) abutting the right renal artery (arrow) with vasospasm, which is suggestive of low-grade injury. (b) Axial contrast-enhanced CT image of the abdomen and pelvis in a 25-year-old man with a stab wound to the posterior flank from a long knife demonstrates right renal laceration with perinephric hematoma and a focal outpouching from the right renal artery (arrow), which are consistent with pseudoaneurysm. (c, d) Axial contrast-enhanced CT images of the abdomen and pelvis in a 19-year-old patient with a gunshot injury to the left back demonstrate hematoma in the retroperitoneum with vascular injuries to the aorta and inferior vena cava (obscured by streak from bullets) with active extravasation (arrow in d), suggesting vascular injury. (e) Axial CT image in a 27-year-old man with a gunshot injury to the right lateral abdomen (entry wound shown with solid orange oval) depicts a trajectory superimposed on the image (arrow) that traverses through the aorta and inferior vena cava, causing an arteriovenous fistula (dashed yellow oval).
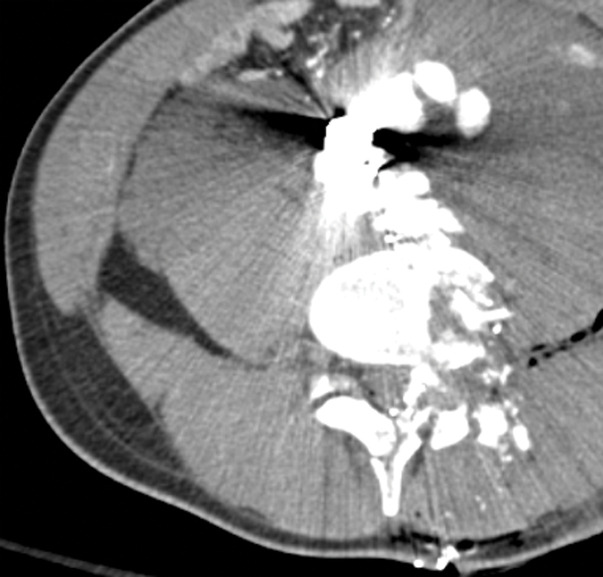
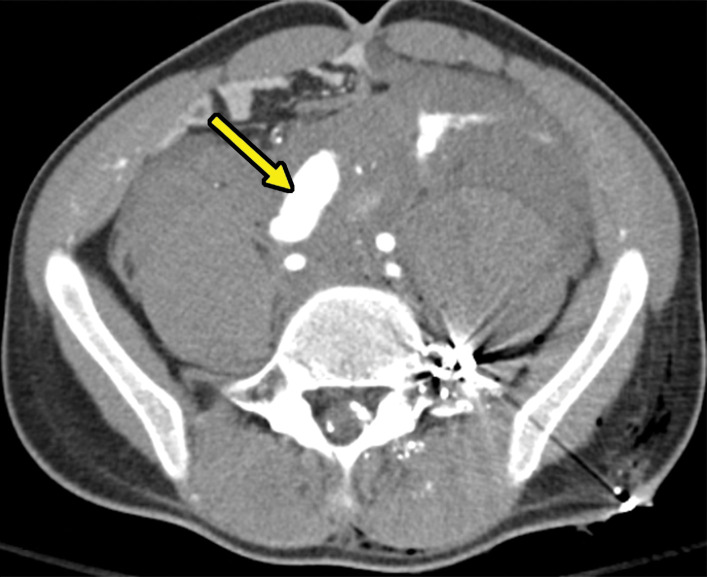
Figure 17.
Gunshot trauma in a 20-year-old patient. A–D, Axial CT images demonstrate multiple gunshot pelvic fractures with resultant large pseudoaneurysm (blue arrows) and active extravasation (yellow arrow) with blood extending into the right upper quadrant (arrowhead in D). E, Catheter angiogram demonstrates pseudoaneurysms (blue arrows) with areas of active extravasation (yellow arrow). Also note arterial spasm due to ongoing active bleeding (black arrows). F, Coronal three-dimensional volume-rendered image demonstrates pseudoaneurysm (blue arrow) and active extravasation (yellow arrow) with blood extending into the right upper quadrant (arrowhead).
Figure 16b.

Direct and indirect signs of vascular injury in four patients. (a) Axial contrast-enhanced CT image of the abdomen and pelvis in a 34-year-old woman with a gunshot injury to the right flank demonstrates hematoma (circle) abutting the right renal artery (arrow) with vasospasm, which is suggestive of low-grade injury. (b) Axial contrast-enhanced CT image of the abdomen and pelvis in a 25-year-old man with a stab wound to the posterior flank from a long knife demonstrates right renal laceration with perinephric hematoma and a focal outpouching from the right renal artery (arrow), which are consistent with pseudoaneurysm. (c, d) Axial contrast-enhanced CT images of the abdomen and pelvis in a 19-year-old patient with a gunshot injury to the left back demonstrate hematoma in the retroperitoneum with vascular injuries to the aorta and inferior vena cava (obscured by streak from bullets) with active extravasation (arrow in d), suggesting vascular injury. (e) Axial CT image in a 27-year-old man with a gunshot injury to the right lateral abdomen (entry wound shown with solid orange oval) depicts a trajectory superimposed on the image (arrow) that traverses through the aorta and inferior vena cava, causing an arteriovenous fistula (dashed yellow oval).
Figure 16c.
Direct and indirect signs of vascular injury in four patients. (a) Axial contrast-enhanced CT image of the abdomen and pelvis in a 34-year-old woman with a gunshot injury to the right flank demonstrates hematoma (circle) abutting the right renal artery (arrow) with vasospasm, which is suggestive of low-grade injury. (b) Axial contrast-enhanced CT image of the abdomen and pelvis in a 25-year-old man with a stab wound to the posterior flank from a long knife demonstrates right renal laceration with perinephric hematoma and a focal outpouching from the right renal artery (arrow), which are consistent with pseudoaneurysm. (c, d) Axial contrast-enhanced CT images of the abdomen and pelvis in a 19-year-old patient with a gunshot injury to the left back demonstrate hematoma in the retroperitoneum with vascular injuries to the aorta and inferior vena cava (obscured by streak from bullets) with active extravasation (arrow in d), suggesting vascular injury. (e) Axial CT image in a 27-year-old man with a gunshot injury to the right lateral abdomen (entry wound shown with solid orange oval) depicts a trajectory superimposed on the image (arrow) that traverses through the aorta and inferior vena cava, causing an arteriovenous fistula (dashed yellow oval).
Figure 16d.
Direct and indirect signs of vascular injury in four patients. (a) Axial contrast-enhanced CT image of the abdomen and pelvis in a 34-year-old woman with a gunshot injury to the right flank demonstrates hematoma (circle) abutting the right renal artery (arrow) with vasospasm, which is suggestive of low-grade injury. (b) Axial contrast-enhanced CT image of the abdomen and pelvis in a 25-year-old man with a stab wound to the posterior flank from a long knife demonstrates right renal laceration with perinephric hematoma and a focal outpouching from the right renal artery (arrow), which are consistent with pseudoaneurysm. (c, d) Axial contrast-enhanced CT images of the abdomen and pelvis in a 19-year-old patient with a gunshot injury to the left back demonstrate hematoma in the retroperitoneum with vascular injuries to the aorta and inferior vena cava (obscured by streak from bullets) with active extravasation (arrow in d), suggesting vascular injury. (e) Axial CT image in a 27-year-old man with a gunshot injury to the right lateral abdomen (entry wound shown with solid orange oval) depicts a trajectory superimposed on the image (arrow) that traverses through the aorta and inferior vena cava, causing an arteriovenous fistula (dashed yellow oval).
Figure 16e.
Direct and indirect signs of vascular injury in four patients. (a) Axial contrast-enhanced CT image of the abdomen and pelvis in a 34-year-old woman with a gunshot injury to the right flank demonstrates hematoma (circle) abutting the right renal artery (arrow) with vasospasm, which is suggestive of low-grade injury. (b) Axial contrast-enhanced CT image of the abdomen and pelvis in a 25-year-old man with a stab wound to the posterior flank from a long knife demonstrates right renal laceration with perinephric hematoma and a focal outpouching from the right renal artery (arrow), which are consistent with pseudoaneurysm. (c, d) Axial contrast-enhanced CT images of the abdomen and pelvis in a 19-year-old patient with a gunshot injury to the left back demonstrate hematoma in the retroperitoneum with vascular injuries to the aorta and inferior vena cava (obscured by streak from bullets) with active extravasation (arrow in d), suggesting vascular injury. (e) Axial CT image in a 27-year-old man with a gunshot injury to the right lateral abdomen (entry wound shown with solid orange oval) depicts a trajectory superimposed on the image (arrow) that traverses through the aorta and inferior vena cava, causing an arteriovenous fistula (dashed yellow oval).
Bullet embolism is also an important direct sign of vascular trauma, the true incidence of which is unknown in the civilian population (Fig 18). During the Vietnam and Afghanistan-Iraq wars, the reported incidence of bullet embolism was 0.3% and 1.1%, respectively (52). Whenever one encounters a penetrating gunshot trauma case, the entry and exit wounds should match. If not, plain radiography can delineate any retained bullets and possible bullet embolization. One should suspect a bullet embolization phenomenon when the bullet is identified remotely from the trajectory. Various factors dictate the pathway of bullet embolization, including anatomy as well as the structure and physics of the projectile. Bullets entering the descending aorta tend to embolize into the lower extremities, causing peripheral vascular ischemia. Bullets entering the systemic veins usually end up in the heart or pulmonary circulation and can rarely embolize into the systemic circulation if a patent foramen ovale exists, a phenomenon known as paradoxical embolism. Very rarely, there may be retrograde embolism of the bullet in the venous tributaries (53).
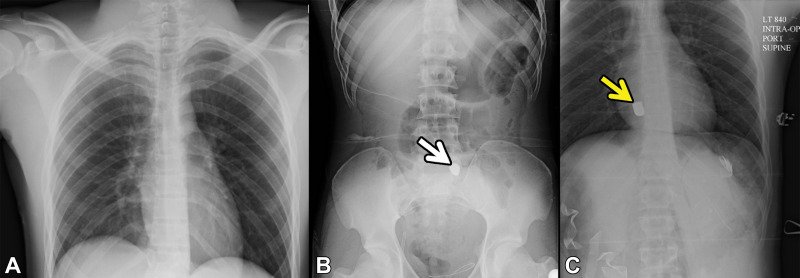
Figure 18.
Bullet embolism in a 19-year-old patient who presented to the ED with gunshot trauma and hemodynamic instability. A, B, Anteroposterior radiographic survey images obtained in the trauma bay before exploratory laparotomy demonstrate a bullet projecting over the sacrum (arrow in B ). C, Supine radiograph that was acquired intraoperatively to reveal the position of the bullet after it could not be found in the pelvis shows that the bullet is embolized to the right ventricle (arrow). This imaging finding is direct evidence of vascular injury.
In addition, the blast effect or shock wave from gunshot trauma can cause vascular injuries similar to those incurred by blunt mechanisms (50). For grading of traumatic abdominal aortic injury, a specific classification scheme is proposed by the Society of Vascular Surgery, in which less severe injuries may manifest with a flap (grade I) or intramural hematoma (grade II), and more severe injuries are characterized by a pseudoaneurysm (grade III) and rupture (grade IV) (54). Grades I and II injuries are often managed with serial follow-up CT to document resolution within 48–72 hours, whereas grades III and IV injuries often require endovascular or open surgical management (54).
The major lifesaving strategy in any vascular trauma is bleeding control by using direct pressure applied over or proximal to the site of injury. However, in abdominal vascular trauma, this is typically not possible. Therefore, timely management of these vascular injuries is crucial, as any delay could have catastrophic consequences, including death. Since the advent of tools such as resuscitative endovascular balloon occlusion of the aorta (REBOA), the management of hemorrhagic shock and cardiac arrest in the prehospital setting has undergone a paradigm shift, as aortic control can now be achieved fairly quickly before the onset of arrest or irreversible shock (48).
In the REBOA technique, the aortic balloon is placed via the femoral artery and inflated inside the aorta to control a distal site of bleeding as well as to raise the blood pressure until definitive surgical hemostasis is achieved. This can be done either fluoroscopically in an angiography suite or, with newer models, in the field or trauma bay of the ED without radiography.
The absolute indication for REBOA is either suspected or confirmed bleeding below the level of the diaphragm in an adult who is in shock or has had a pulseless electrical activity cardiac arrest for less than 10 minutes. Radiologists should be familiar with these catheters, as related complications are relatively uncommon, and once such patients are in a transiently hemodynamically stable condition, imaging is frequently performed to depict internal injuries. Access site complications such as pseudoaneurysms, vascular injury to the aorta with resultant thrombus formation, and distal embolization and ischemia can be seen (55–58).
Special Considerations
Penetrating Trauma in Pregnant Patients
Penetrating trauma affects an estimated 3.27 per 100 000 pregnancies and is less common than blunt trauma (59). Fetal mortality is substantially higher in penetrating trauma compared with in blunt trauma (59,60). The primary goal of treating pregnant patients with trauma is ensuring the health of the mother, as her maintained health is directly linked to the health of the child. CT is the modality of choice owing to its availability and acquisition speed (61,62). Unless there is a compelling contraindication, intravenous contrast material should be used. In the vast majority of penetrating trauma scenarios, the benefits of radiation exposure in performing a whole-body or abdomen and pelvis CT outweigh the risks. While CT of the abdomen and pelvis can result in a high estimated fetal dose (up to 25 mGy), this value is still well below the recommended fetal exposure dose limit of 50 mGy (61,62). Radiologists’ knowledge of radiation exposure may be helpful for ED physicians providing care to these patients.
Imaging after Damage Control Surgery
Patients with penetrating thoracic, abdominal, or other types of trauma and hemodynamic instability often undergo immediate surgical exploration without imaging. Trauma surgeons may perform a limited exploratory laparotomy or a damage control surgery with the goal of stabilizing the patient, leaving the laparotomy incision open with the plan to reexplore after CT (63–65).
Treating these patients can be particularly challenging because of postlaparotomy changes and packing material. CT often delineates injuries that were missed at laparotomy, especially those involving the retroperitoneum. Imaging with intravenous contrast material is ideal unless there are compelling contraindications (64,65). When the radiologist protocols these CT examinations, knowledge of the surgical findings is helpful, as some injury patterns may warrant an arterial examination and potentially excretory phase imaging as well if a renal injury is present.
At imaging, the laparotomy incision is often open with an overlying negative pressure dressing. There may be abundant hyperattenuating packing material, and the bowel may be left in discontinuity (Fig 19). The open abdomen along with the space-occupying packing may cause increased difficulty in diagnosing mesenteric or bowel injuries with a high level of confidence. This is particularly the case with extraluminal gas, fluid, and blood that may be present postoperatively. Although these patients often undergo second-look surgeries, the search for surgically occult injuries is crucial, particularly in the retroperitoneum, for missed foci of active bleeding.
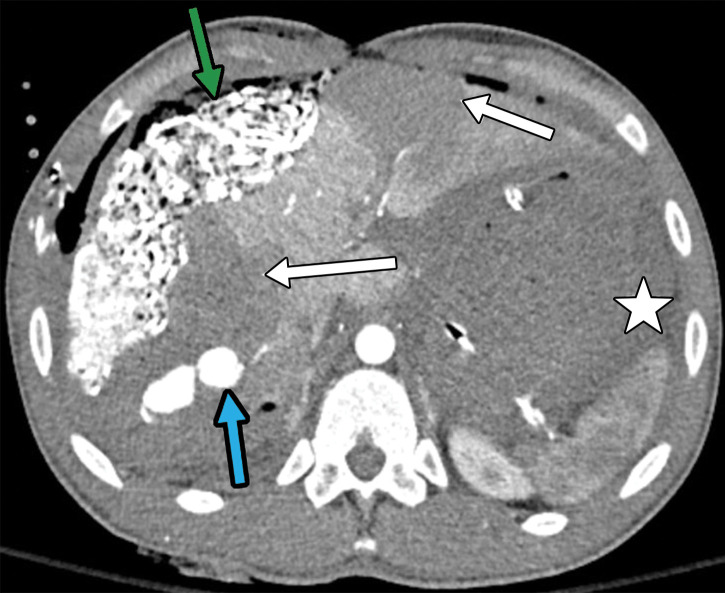
Figure 19a.
Multiple gunshot-related injuries in a 21-year-old patient who was taken to the operating room for initial exploratory laparotomy. Axial CT images reveal packing material (green arrow in a) with an open abdomen (yellow arrow in b). The image obtained after surgical exploration (b) demonstrates thickened bowel walls with hyperenhancement (red arrows), which are likely secondary to hypoperfusion. A bleeding pseudoaneurysm (blue arrow in a) in hepatic segment 7 is demonstrated, which was subsequently coil embolized (not shown). Also note segmental liver infarctions (white arrows in a) and large-volume hematoma (☆ in a). This finding (bleeding pseudoaneurysm) was not appreciated at exploratory laparotomy.
Figure 19b.
Multiple gunshot-related injuries in a 21-year-old patient who was taken to the operating room for initial exploratory laparotomy. Axial CT images reveal packing material (green arrow in a) with an open abdomen (yellow arrow in b). The image obtained after surgical exploration (b) demonstrates thickened bowel walls with hyperenhancement (red arrows), which are likely secondary to hypoperfusion. A bleeding pseudoaneurysm (blue arrow in a) in hepatic segment 7 is demonstrated, which was subsequently coil embolized (not shown). Also note segmental liver infarctions (white arrows in a) and large-volume hematoma (☆ in a). This finding (bleeding pseudoaneurysm) was not appreciated at exploratory laparotomy.
Imaging manifestations related to the CT hypoperfusion complex may also manifest in these patients (64,65). Reported CT findings and definitions of hypoperfusion complex have varied throughout the years (63–65). When defining CT hypoperfusion complex as either a collapsed inferior vena cava or having two or more vascular or visceral enhancement abnormalities present, the most frequent findings are shock bowel (thickening with submucosal edema and hyperenhancement) (41%–66%); renal cortical hyperenhancement (56%–58%); diminished abdominal aortic diameter (35%–48%); gallbladder hyperenhancement (33%–46%); peripancreatic fluid (35%–44%); splenic hypoenhancement (30%–35%); heterogeneous hepatic enhancement (11%–29%); and other less frequent findings (66,67) (Fig 19).
Conclusion
Timely identification of injuries secondary to penetrating abdominopelvic trauma can prevent poor patient outcomes. Familiarity with projectile kinetics aids in understanding injury mechanisms, and following the tracks of penetrating objects can reveal the site of energy deposition and subsequent injury. Knowledge of the imaging features of the injuries acquired in penetrating trauma, including direct and indirect signs, aids in correct injury characterization, which is vital to clinical decision making.
Recipient of a Certificate of Merit award for an education exhibit at the 2019 RSNA Annual Meeting.
For this journal-based SA-CME activity, the authors D.H.B. and M.N.P. have provided disclosures (see end of article); all other authors, the editor, and the reviewers have disclosed no relevant relationships.
D.H.B. supported by the National Institutes of Health (TOP-TIER grant T32-EB021955).
Disclosures of Conflicts of Interest.— : D.H.B. Activities related to the present article: editorial board member of RadioGraphics (not involved in the handling of this article). Activities not related to the present article: disclosed no relevant relationships. Other activities: disclosed no relevant relationships. M.N.P. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: honorarium from Springer Publishing. Other activities: disclosed no relevant relationships.
Abbreviations:
- AAST
- American Association for the Surgery of Trauma
- ED
- emergency department
- FAST
- focused assessment with sonography in trauma
References
- 1.NVDRS Infographic|Violence Prevention|Violence Prevention|Injury Center|CDC . https://www.cdc.gov/violenceprevention/communicationresources/infographics/nvdrs-infographic.html. Published 2020. Accessed May 21, 2020.
- 2.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med 2015;79(5):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Butt MU, Zacharias N, Velmahos GC. Penetrating abdominal injuries: management controversies. Scand J Trauma Resusc Emerg Med 2009;17(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leading Causes of Death and Injury - PDFs|Injury Center|CDC . https://www.cdc.gov/injury/wisqars/LeadingCauses.html. Published 2020. Accessed October 21, 2020.
- 5.Martins Filho EL, Mazepa MM, Guetter CR, Pimentel SK. The role of computerized tomography in penetrating abdominal trauma. Rev Col Bras Cir 2018;45(1):e1348. [DOI] [PubMed] [Google Scholar]
- 6.Ghumman Z, Monteiro S, Mellnick V, Coates A, Engels P, Patlas M. Accuracy of Preoperative MDCT in Patients With Penetrating Abdominal and Pelvic Trauma. Can Assoc Radiol J 2020;71(2):231–237. [DOI] [PubMed] [Google Scholar]
- 7.Jandial R, Reichwage B, Levy M, Duenas V, Sturdivan L. Ballistics for the neurosurgeon. Neurosurgery 2008;62(2):472–480; discussion 480. [DOI] [PubMed] [Google Scholar]
- 8.Humphrey C, Kumaratilake J. Ballistics and anatomical modelling: a review. Leg Med (Tokyo) 2016;23(21):29. [DOI] [PubMed] [Google Scholar]
- 9.Powers DB, Delo RI. Characteristics of ballistic and blast injuries. Atlas Oral Maxillofac Surg Clin North Am 2013;21(1):15–24. [DOI] [PubMed] [Google Scholar]
- 10.Hanna TN, Shuaib W, Han T, Mehta A, Khosa F. Firearms, bullets, and wound ballistics: an imaging primer. Injury 2015;46(7):1186–1196. [DOI] [PubMed] [Google Scholar]
- 11.Rhee PM, Moore EE, Joseph B, Tang A, Pandit V, Vercruysse G. Gunshot wounds: a review of ballistics, bullets, weapons, and myths. J Trauma Acute Care Surg 2016;80(6):853–867. [DOI] [PubMed] [Google Scholar]
- 12.Rutty GN, Boyce P, Robinson CE, Jeffery AJ, Morgan B. The role of computed tomography in terminal ballistic analysis. Int J Legal Med 2008;122(1):1–5. [DOI] [PubMed] [Google Scholar]
- 13.Bolliger SA, Thali MJ, Bolliger MJ, Kneubuehl BP. Gunshot energy transfer profile in ballistic gelatine, determined with computed tomography using the total crack length method. Int J Legal Med 2010;124(6):613–616. [DOI] [PubMed] [Google Scholar]
- 14.Galvagno SM Jr, Nahmias JT, Young DA. Advanced Trauma Life Support® Update 2019: Management and Applications for Adults and Special Populations. Anesthesiol Clin 2019;37(1):13–32. [DOI] [PubMed] [Google Scholar]
- 15.American Institute of Ultrasound in Medicine; American College of Emergency Physicians . AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med 2014;33(11):2047–2056. [DOI] [PubMed] [Google Scholar]
- 16.Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Hogan GJF, Scalea TM. Penetrating torso trauma: triple-contrast helical CT in peritoneal violation and organ injury: a prospective study in 200 patients. Radiology 2004;231(3):775–784. [DOI] [PubMed] [Google Scholar]
- 17.Jawad H, Raptis C, Mintz A, Schuerer D, Mellnick V. Single-Contrast CT for Detecting Bowel Injuries in Penetrating Abdominopelvic Trauma. AJR Am J Roentgenol 2018;210(4):761–765. [DOI] [PubMed] [Google Scholar]
- 18.Ozimok CJ, Mellnick VM, Patlas MN. An international survey to assess use of oral and rectal contrast in CT protocols for penetrating torso trauma. Emerg Radiol 2019;26(2):117–121. [DOI] [PubMed] [Google Scholar]
- 19.Alabousi M, Zha N, Patlas MN. Use of Enteric Contrast for Abdominopelvic CT in Penetrating Traumatic Injury in Adults: Comparison of Diagnostic Accuracy Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 10.2214/AJR.20.24636. Published online September 30, 2020. [DOI] [PubMed]
- 20.Dreizin D, Boscak AR, Anstadt MJ, et al. Penetrating Colorectal Injuries: Diagnostic Performance of Multidetector CT with Trajectography. Radiology 2016;281(3):749–762. [DOI] [PubMed] [Google Scholar]
- 21.Dreizin D, Munera F. Multidetector CT for Penetrating Torso Trauma: State of the Art. Radiology 2015;277(2):338–355. [DOI] [PubMed] [Google Scholar]
- 22.Dreizin D, Borja MJ, Danton GH, et al. Penetrating diaphragmatic injury: accuracy of 64-section multidetector CT with trajectography. Radiology 2013;268(3):729–737. [DOI] [PubMed] [Google Scholar]
- 23.Brook OR, Eran A, Engel A. CT multiplanar reconstructions (MPR) for shrapnel injury trajectory. Emerg Radiol 2012;19(1):43–51. [DOI] [PubMed] [Google Scholar]
- 24.Folio L, Fischer T, Shogan PJ, Frew M, Bunger R, Provenzale JM. Cartesian positioning system for localization of blast and ballistic fragments: a phantom-based pilot study. Mil Med 2011;176(11):1300–1305. [DOI] [PubMed] [Google Scholar]
- 25.Folio LR, Fischer TV, Shogan PJ, et al. CT-based ballistic wound path identification and trajectory analysis in anatomic ballistic phantoms. Radiology 2011;258(3):923–929. [DOI] [PubMed] [Google Scholar]
- 26.Folio LR, Fischer T, Shogan P, Frew M, Dwyer A, Provenzale JM. Blast and ballistic trajectories in combat casualties: a preliminary analysis using a cartesian positioning system with MDCT. AJR Am J Roentgenol 2011;197(2):W233–W240. [DOI] [PubMed] [Google Scholar]
- 27.Yu J, Fulcher AS, Wang DB, et al. Frequency and importance of small amount of isolated pelvic free fluid detected with multidetector CT in male patients with blunt trauma. Radiology 2010;256(3):799–805. [DOI] [PubMed] [Google Scholar]
- 28.Lubner M, Menias C, Rucker C, et al. Blood in the belly: CT findings of hemoperitoneum. RadioGraphics 2007;27(1):109–125. [DOI] [PubMed] [Google Scholar]
- 29.Saksobhavivat N, Shanmuganathan K, Boscak AR, et al. Diagnostic accuracy of triple-contrast multi-detector computed tomography for detection of penetrating gastrointestinal injury: a prospective study. Eur Radiol 2016;26(11):4107–4120. [DOI] [PubMed] [Google Scholar]
- 30.Stuhlfaut JW, Soto JA, Lucey BC, et al. Blunt abdominal trauma: performance of CT without oral contrast material. Radiology 2004;233(3):689–694. [DOI] [PubMed] [Google Scholar]
- 31.Shanmuganathan K, Mirvis SE, Chiu WC, Killeen KL, Scalea TM. Triple-contrast helical CT in penetrating torso trauma: a prospective study to determine peritoneal violation and the need for laparotomy. AJR Am J Roentgenol 2001;177(6):1247–1256. [DOI] [PubMed] [Google Scholar]
- 32.Butela ST, Federle MP, Chang PJ, et al. Performance of CT in detection of bowel injury. AJR Am J Roentgenol 2001;176(1):129–135. [DOI] [PubMed] [Google Scholar]
- 33.Lozano JD, Munera F, Anderson SW, Soto JA, Menias CO, Caban KM. Penetrating wounds to the torso: evaluation with triple-contrast multidetector CT. RadioGraphics 2013;33(2):341–359. [DOI] [PubMed] [Google Scholar]
- 34.Anderson SW, Soto JA. Anorectal trauma: the use of computed tomography scan in diagnosis. Semin Ultrasound CT MR 2008;29(6):472–482. [DOI] [PubMed] [Google Scholar]
- 35.Brofman N, Atri M, Hanson JM, Grinblat L, Chughtai T, Brenneman F. Evaluation of bowel and mesenteric blunt trauma with multidetector CT. RadioGraphics 2006;26(4):1119–1131. [DOI] [PubMed] [Google Scholar]
- 36.McGeady JB, Breyer BN. Current epidemiology of genitourinary trauma. Urol Clin North Am 2013;40(3):323–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quagliano PV, Delair SM, Malhotra AK. Diagnosis of blunt bladder injury: a prospective comparative study of computed tomography cystography and conventional retrograde cystography. J Trauma 2006;61(2):410–421; discussion 421–422. [DOI] [PubMed] [Google Scholar]
- 38.Ramchandani P, Buckler PM. Imaging of genitourinary trauma. AJR Am J Roentgenol 2009;192(6):1514–1523. [DOI] [PubMed] [Google Scholar]
- 39.Zaid UB, Bayne DB, Harris CR, Alwaal A, McAninch JW, Breyer BN. Penetrating Trauma to the Ureter, Bladder, and Urethra. Curr Trauma Rep 2015;1(2):119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joshi G, Kim EY, Hanna TN, Siegel CL, Menias CO. CT Cystography for Suspicion of Traumatic Urinary Bladder Injury: Indications, Technique, Findings, and Pitfalls in Diagnosis. RadioGraphics 2018;38(1):92–93. [DOI] [PubMed] [Google Scholar]
- 41.Morgan DE, Nallamala LK, Kenney PJ, Mayo MS, Rue LW 3rd. CT cystography: radiographic and clinical predictors of bladder rupture. AJR Am J Roentgenol 2000;174(1):89–95. [DOI] [PubMed] [Google Scholar]
- 42.Kozar RA, Crandall M, Shanmuganathan K, et al. Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg 2018;85(6):1119–1122 [Published correction appears in J Trauma Acute Care Surg 2019;87(2):512.] [DOI] [PubMed] [Google Scholar]
- 43.O’Neill SB, Hamid S, Nicolaou S, Qamar SR. Changes in Approach to Solid Organ Injury: What the Radiologist Needs to Know. Can Assoc Radiol J 2020;71(3):352–361. [DOI] [PubMed] [Google Scholar]
- 44.Dreizin D, Bordegaray M, Tirada N, Raman SP, Kadakia K, Munera F. Evaluating blunt pancreatic trauma at whole body CT: current practices and future directions. Emerg Radiol 2013;20(6):517–527. [DOI] [PubMed] [Google Scholar]
- 45.Kobayashi LM, Costantini TW, Hamel MG, Dierksheide JE, Coimbra R. Abdominal vascular trauma. Trauma Surg Acute Care Open 2016;1(1):e000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davis TP, Feliciano DV, Rozycki GS, et al. Results with abdominal vascular trauma in the modern era. Am Surg 2001;67(6):565–570; discussion 570–571. [PubMed] [Google Scholar]
- 47.Asensio JA, Chahwan S, Hanpeter D, et al. Operative management and outcome of 302 abdominal vascular injuries. Am J Surg 2000;180(6):528–533; discussion 533–534. [DOI] [PubMed] [Google Scholar]
- 48.Asensio JA, Feliciano DV. Abdominal Vascular Injury. In: Moore EE, Feliciano DV, Mattox KL, eds.Trauma. 8th ed. New York, NY: McGraw-Hill Education, 2017. [Google Scholar]
- 49.Pereira BMT, Chiara O, Ramponi F, et al. WSES position paper on vascular emergency surgery. World J Emerg Surg 2015;10(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baghdanian AH, Armetta AS, Baghdanian AA, LeBedis CA, Anderson SW, Soto JA. CT of Major Vascular Injury in Blunt Abdominopelvic Trauma. RadioGraphics 2016;36(3):872–890. [DOI] [PubMed] [Google Scholar]
- 51.Willmann JK, Roos JE, Platz A, et al. Multidetector CT: detection of active hemorrhage in patients with blunt abdominal trauma. AJR Am J Roentgenol 2002;179(2):437–444. [DOI] [PubMed] [Google Scholar]
- 52.Yoon B, Grasso S, Hofmann LJ. Management of Bullet Emboli to the Heart and Great Vessels. Mil Med 2018;183(9-10):e307–e313. [DOI] [PubMed] [Google Scholar]
- 53.Gunn ML, Clark RT, Sadro CT, Linnau KF, Sandstrom CK. Current concepts in imaging evaluation of penetrating transmediastinal injury. RadioGraphics 2014;34(7):1824–1841. [DOI] [PubMed] [Google Scholar]
- 54.Tsai R, Raptis D, Raptis C, Mellnick VM. Traumatic abdominal aortic injury: clinical considerations for the diagnostic radiologist. Abdom Radiol (NY) 2018;43(5):1084–1093. [DOI] [PubMed] [Google Scholar]
- 55.Gamberini E, Coccolini F, Tamagnini B, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta in trauma: a systematic review of the literature. World J Emerg Surg 2017;12(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brenner M, Bulger EM, Perina DG, et al. Joint statement from the American College of Surgeons Committee on Trauma (ACS COT) and the American College of Emergency Physicians (ACEP) regarding the clinical use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). Trauma Surg Acute Care Open 2018;3(1):e000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Manzano-Nunez R, Orlas CP, Herrera-Escobar JP, et al. A meta-analysis of the incidence of complications associated with groin access after the use of resuscitative endovascular balloon occlusion of the aorta in trauma patients. J Trauma Acute Care Surg 2018;85(3):626–634. [DOI] [PubMed] [Google Scholar]
- 58.DuBose JJ, Scalea TM, Brenner M, et al. The AAST prospective Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery (AORTA) registry: data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg 2016;81(3):409–419. [DOI] [PubMed] [Google Scholar]
- 59.Mendez-Figueroa H, Dahlke JD, Vrees RA, Rouse DJ. Trauma in pregnancy: an updated systematic review. Am J Obstet Gynecol 2013;209(1):1–10. [DOI] [PubMed] [Google Scholar]
- 60.Petrone P, Talving P, Browder T, et al. Abdominal injuries in pregnancy: a 155-month study at two level 1 trauma centers. Injury 2011;42(1):47–49. [DOI] [PubMed] [Google Scholar]
- 61.Raptis CA, Mellnick VM, Raptis DA, et al. Imaging of trauma in the pregnant patient. RadioGraphics 2014;34(3):748–763. [DOI] [PubMed] [Google Scholar]
- 62.Sadro C, Bernstein MP, Kanal KM. Imaging of trauma: Part 2, Abdominal trauma and pregnancy--a radiologist’s guide to doing what is best for the mother and baby. AJR Am J Roentgenol 2012;199(6):1207–1219. [DOI] [PubMed] [Google Scholar]
- 63.Lamb CM, MacGoey P, Navarro AP, Brooks AJ. Damage control surgery in the era of damage control resuscitation. Br J Anaesth 2014;113(2):242–249. [DOI] [PubMed] [Google Scholar]
- 64.Alexander LF, Hanna TN, LeGout JD, et al. Multidetector CT Findings in the Abdomen and Pelvis after Damage Control Surgery for Acute Traumatic Injuries. RadioGraphics 2019;39(4):1183–1202. [DOI] [PubMed] [Google Scholar]
- 65.Baghdanian AA, Baghdanian AH, Khalid M, et al. Damage control surgery: use of diagnostic CT after life-saving laparotomy. Emerg Radiol 2016;23(5):483–495. [DOI] [PubMed] [Google Scholar]
- 66.Ryan MF, Hamilton PA, Sarrazin J, Chu P, Benjaminov O, Lam K. The halo sign and peripancreatic fluid: useful CT signs of hypovolaemic shock complex in adults. Clin Radiol 2005;60(5):599–607. [DOI] [PubMed] [Google Scholar]
- 67.Enslow MS, Preece SR, Wildman-Tobriner B, Enslow RA, Mazurowski M, Nelson RC. Splenic contraction: a new member of the hypovolemic shock complex. Abdom Radiol (NY) 2018;43(9):2375–2383. [DOI] [PubMed] [Google Scholar]