Abstract
Objective:
Despite evidence supporting the use of measures to track ongoing progress and outcome in treatment, there is a relative absence of measures that are appropriate for this purpose in youth with eating disorders. This study examined the psychometric properties of the Eating Disorder-15 for Youth (ED-15-Y) scale, including its ability to detect short-term change in symptomatology.
Method:
Youth (N = 203) ages 8 to 18 years completed self-report questionnaires and semi-structured diagnostic interviews upon initial presentation for an outpatient eating disorders assessment at an academic medical center.
Results:
The ED-15-Y demonstrated excellent reliability (internal consistency, split-half reliability) and high sensitivity to change early in treatment (change from sessions 1 to 8, adjusting for baseline score). Further, these data demonstrate that the ED-15-Y has excellent convergent validity, being highly correlated with a well-tested, longer measure of eating disorders psychopathology—the Eating Disorders Examination-Questionnaire (EDE-Q). These data also support good discriminant and concurrent validity, differentiating between youth without an eating disorder or with ARFID and youth with eating disorders involving weight and shape concerns (e.g., anorexia nervosa, bulimia nervosa).
Discussion:
The ED-15-Y may be a useful tool to briefly assess eating disorder psychopathology in youth as young as 8 years old. Its sensitivity to change very early in treatment suggests that it has the potential to be used as a routine outcome measure in the context of treatment.
Keywords: assessment, eating disorder psychopathology, psychometrics, routine outcome monitoring, youth, children and adolescents
Introduction
Despite the importance of evidence-based assessment in children and adolescents with eating disorders, there is a paucity of measures designed to assess eating disorder psychopathology in youth. Upon examining the randomized trials for youth with eating disorders cited in Lock’s (2015) literature review and several more recent trials, the Eating Disorders Examination (Fairburn & Cooper, 1993) is the most frequently used measure of outcome. However, the EDE interview is costly and time-intensive, and it is generally not feasible as a measure of outcome in non-research settings. Although not reported in the main outcome publications, over half of the trials for adolescents with AN or BN in the past 15 years (Le Grange, Lock, Agras, Bryson, & Jo, 2015; Le Grange, Crosby, Rathouz, & Leventhal, 2007; Lock, Agras, Bryson, & Kraemer, 2005; Lock et al., 2010; Lock et al., 2015) have also had participants complete the parallel self-report Eating Disorders Examination – Questionnaire (EDE-Q) (Fairburn & Beglin, 1994), which has very strong convergence with the interview (Berg et al., 2011).
There are significant advantages to the EDE-Q as an outcome measure, including perceived anonymity, time efficiency, and geographical flexibility, which makes the EDE-Q more feasible as an outcome measure in clinical practice. However, the EDE-Q was developed for women ages 16 to 35 (Fairburn & Beglin, 1994), and data on its psychometric properties in adolescents is extremely limited. Available studies examined the factor structure of the EDE-Q in adolescents ages 14–18 (White, Haycraft, Goodwin, & Meyer, 2014), demonstrating good internal consistency of the measure, and demonstrated some evidence of validity in adolescent inpatients ages 11–18, given significantly higher global scores for those with binge/purge type AN compared to those with restrictive type AN (Jennings & Phillips, 2017). There are currently two adolescent-specific adaptations of the EDE-Q—the Eating Questionnaire - A (EDE-A; CORC, 2020) and the Youth Eating Disorder Examination-Questionnaire (YEDE-Q; Goldschmidt, Doyle, & Wilfley, 2007). The EDE-A made significant changes to the wording of question and changed the timeframe from 28 days to 14 days. Community norms for youth ages 12–14 are available (Carter, Stewart, & Fairburn, 2001), but psychometric properties of the EDE-A have not been examined. In contrast, the YEDE-Q has been used primarily in overweight populations (Balantekin et al., 2017; Eichen et al., 2019; Kass et al., 2017; Sheinbein et al., 2019; Skjåkødegård et al., 2016). Only one study of eating disorders was identified that used the YEDE-Q, which demonstrated some evidence of convergent validity in adolescent inpatients with AN (Noetel et al., 2016). In summary, the available measures for youth with eating disorders are relatively long (near 30 items), they are limited to youth older than age 11–12 or 14, and their psychometric properties in youth with eating disorders are largely unexamined. Further, the original EDE-Q is more often selected as an outcome measure in youth with eating disorders as young as 12, despite the absence of psychometric data for children and the availability of measures more appropriate for adolescents, albeit with minimal psychometric data.
An additional barrier to assessment of eating disorder psychopathology in youth is the absence of measures that would be appropriate for assessing week-to-week changes. Systematic monitoring of patients’ symptoms throughout the course of treatment, or routine outcome monitoring (ROM), is increasingly important as a facet of evidence-based care. Indeed, mental and physical health outcomes are significantly improved when usual care incorporates measurement feedback systems using ROM (Bickman et al., 2011; Carlier et al., 2012; Shimokawa et al., 2010). However, ROM relies on the availability of brief, psychometrically strong outcome measures. While two measures of session-to-session symptom change have been developed for adults with eating disorders (Tatham et al., 2015; Gideon, Hawkes, Mond, Saunders, Tchanturia, & Serpell, 2016), their application would be inappropriate in younger populations.
Given the lack of measures available to assess eating disorder psychopathology in youth and the absence of measures appropriate to track change over time, this study leveraged an existing brief measure of eating disorder psychopathology in adults (ED-15; Tatham et al., 2015). At the time of initial adaptation, the ED-15 was the only available measure of its kind, demonstrated excellent psychometric properties, and seemed suitable for adaptation. With careful consideration of the developmental and reading level for youth as young as 8 years of age, the ED-15 for youth (ED-15-Y) was adapted from the ED-15. This study examines the psychometric properties of the ED-15-Y, including its reliability (factor structure, internal consistency), sensitivity to change over time, and validity (convergent, discriminant, concurrent).
Methods
Participants were youth up to 18 years who presented to a specialty eating disorders program at an academic medical center for an initial psychiatric evaluation between November 2015 and April 2020. All youth who provided assent/consent were included, except those younger than 8 years due to their developmental capacity to understand and complete a battery of self-report questionnaires. A subsample received outpatient treatment within the program and provided session-to-session reports of symptoms. The primary treatment modality offered in the program was family-based treatment (Lock & Le Grange, 2013), but adolescent focused therapy (Lock, 2020), cognitive behavior therapy (Fairburn, 2008), and dialectical behavior therapy (Linehan, 2014) were also delivered where appropriate. Written informed consent/assent was obtained from youth and their caregiver(s). All procedures were approved by the Institutional Review Board at the University of California, San Francisco.
Procedures
Demographic and clinical information was collected during the intake interview and via questionnaires. Weight (without shoes in light indoor clothing) was taken on a regularly recalibrated scale, and percent of median body weight was calculated using the 50th Body Mass Index percentile according to Center for Disease Control norms for age and gender (CDC, 2002).
Measures
Eating Disorder-15 for Youth (ED-15-Y).
The original ED-15 (Tatham et al., 2015) was designed as a brief measure of eating disorder psychopathology for adults, with 10 attitudinal items and five behavioral items that inquire about the frequency of binge eating, vomiting, laxative use, restricting, and driven exercise in the past week. The attitudinal items yield a total score and two subscale scores (eating concerns and weight/shape concerns).
In consultation with other experts in child and adolescent eating disorders, the ED-15 was adapted by the first author for use with youth ages 8 to 18 (see ED-15-Y measure in Supporting Information). The scale was modified from a seven-point scale (0–6) to a five-point scale (1–5), and language was modified for age appropriateness. The modified ED-15-Y has a Flesch-Kincaid grade level of 3.7, indicating that the language was appropriate for youth in the third grade (age 8), and a Flesch reading ease of 84.8, indicating excellent readability. These initial adaptations were administered to a group of ten pediatric patients (ages 8 through 17) with eating disorders. None reported any difficulty understanding the items, and their explanation of the instructions and items demonstrated good item clarity. Therefore, this initial adaptation was finalized with minor formatting changes as suggested by one caregiver. The total score is the mean of the first ten items, with scores ranging from 1 to 5. Youth completed the ED-15-Y at the initial assessment and at each session early in treatment if they engaged in treatment between October 2015 and October 2018 for an eating disorder involving weight and shape concerns.
Eating Disorder Examination Questionnaire (EDE-Q).
The EDE-Q (version 6.0; Fairburn & Beglin, 2008) is the leading questionnaire for assessing eating disorder psychopathology (Berg, Peterson, Frazier, & Crow, 2011). Its global score has demonstrated good reliability (Luce & Crowther, 1999) in adolescents with AN (Herzog, Keller, Sacks, Yeh, & Lavori, 1992) and BN (Binford, Le Grange, & Jellar, 2005).
Eating Disorders in Youth-Questionnaire (EDY-Q).
The EDY-Q (Hilbert & van Dyck, 2016) assesses early-onset restrictive eating disturbances characteristic of Avoidant-Restrictive Food Intake Disorder (ARFID) and other less common eating disorders in youth ages 8–13. The total score is comprised of 12 items that focus exclusively on ARFID symptoms. The EDY-Q demonstrated acceptable reliability and adequate convergent and discriminant validity (Kurz, Van Dyck, Dremmel, Munsch, & Hilbert, 2015).
Symptoms and Functioning Severity Scale (SFSS).
The SFSS (Bickman, Athay, et al., 2010) is a 26-item global measure of general psychopathology in youth that demonstrates excellent reliability and validity (Athay, Riemer, & Bickman, 2012).
Multidimensional Anxiety Scale for Children (MASC-10).
The MASC-10 (March et al., 1997) is an abbreviated 10-item global measure of anxiety symptoms in patients ages 8–18. The questionnaire demonstrates good internal and test-retest reliability (March, Sullivan, & Parker, 1999) as well as good discriminative validity (Rynn et al., 2006).
Children’s Depression Inventory-2 (CDI-2).
The CDI-2 Short form (Kovacs & MHS Staff, 2011) is a 12-item measure of global depressive symptoms for ages 7–17 years. The questionnaire demonstrates good reliability and discriminative validity (Kovacs & MHS Staff, 2011).
Mini International Neuropsychiatric Interview Kid (MINI-Kid).
The MINI-Kid is a widely used semi-structured interview that is used to diagnose co-occurring psychiatric disorders with high reliability and validity (Sheehan, Sheehan, et al., 2010). Version 7.0.2 was administered by clinical psychologists or psychology interns who were supervised live by a clinical psychologist to assess Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition co-occurring psychiatric disorders.
Eating Disorder Assessment for DSM-5 (EDA-5).
The EDA-5 is a semi-structured interview used to assist in determining DSM-5 eating disorder diagnosis (Sysko et al., 2015). Clinicians (licensed clinical psychologists and clinical psychology interns who received live clinical supervision by a licensed psychologist) administered this measure in the context of the initial evaluation and further specified the eating disorder diagnosis as clinically indicated.
Data analyses
All analyses were conducted with IBM SPSS Statistics 27.
Reliability.
Factor structure.
Factor structure for the ten attitudinal items was examined using principal axis factoring with an unspecified number of components and an oblique rotation to establish whether the scale represented one global factor or multiple subscales.
Internal consistency.
Internal consistency and split-half reliability (first five items versus last five items) for the ED-15-Y were examined using Cronbach’s alpha and Spearman-Brown coefficients, respectively. Internal consistencies were examined for each of the other self-report measures as well.
Sensitivity to change over time.
The ED-15-Y is designed to be sensitive to change over time and should therefore demonstrate only moderate temporal stability. Greater improvement early in treatment is a robust predictor of outcome at end of treatment and follow-up (Vall & Wade, 2015), so early symptom change was examined to assess sensitivity to change over time. Given that prior studies have examined early change through session eight (Doyle, Le Grange, Loeb, Doyle, & Crosby, 2010; Le Grange, Accurso, Lock, Agras, & Bryson, 2014; Le Grange, Doyle, Crosby, & Chen, 2008) and our expectation that cognitive improvement would not be expected much earlier than this time, multilevel mixed-effects models examined change in the ED-15-Y from sessions 1 to 8. The first eight sessions were generally scheduled within the first two months of treatment. The model included baseline ED-15-Y score and session number, with the expectation that there would be a statistically significant decrease in ED-15-Y score across sessions.
Validity.
Convergent validity.
Eating disorder psychopathology.
Convergent validity for the ED-15-Y was established through Pearson’s correlations with the EDE-Q. Given that the EDE-Q is not well-established for younger populations, separate correlations were provided for youth ages 8 to 13 and adolescents 14 years and older. We also examined the Pearson chi-squared values of the crosstabulations between each of the five behavioral items on the ED-15-Y and their parallel items on the EDE-Q. Agreement on frequency was also measured, using correlations between each pair of behavioral items for youth who endorsed the behavior on both measures.
Other psychopathology.
Pearson’s correlations were examined between the ED-15-Y and measures of overall psychopathology (SFSS), anxiety (MASC-10), and depression (CDI-2). As a comparison, correlations between these measures and the EDE-Q were also examined. We expected moderate to strong correlations between the ED-15-Y and co-occurring psychopathology (general, anxiety, and depression), and expected the correlations to be comparable to those with the EDE-Q.
Discriminant validity.
A Pearson’s correlation was examined between the ED-15-Y and ARFID symptomatology (EDY-Q). As a comparison, the correlation between the EDY-Q and the EDE-Q was also examined. We expected a small correlation between ARFID symptomatology and both the ED-15-Y and EDE-Q, as these measures should measure unique symptom combinations.
Concurrent validity.
Scores on the ED-15-Y were compared by eating disorder diagnosis using a one-way ANOVA. Given the lack of weight and shape concerns in ARFID, we anticipated that ED-15-Y scores in youth with ARFID would be significantly lower than those with eating disorders involving weight and shape concerns (i.e., AN, Atypical AN, BN) and not significantly different than youth without an eating disorder. We further expected that scores would be highest for BN and significantly greater than scores for youth with AN or Atypical AN, given minimization of symptoms in AN-like presentation and research indicating that eating disorders psychopathology in adolescents presenting for treatment appears to be more severe in BN than AN (Binford, Le Grange, & Jellar, 2005; Gorrell et al., 2020). We also expected that youth with Atypical AN would report more severe eating disorder psychopathology compared to those with “typical” AN, given more recent research suggesting a significant difference between these groups (Garber et al., 2019; Noetel et al., 2016; Sawyer et al., 2016).
Results
Of those evaluated (N = 363) in the specialty eating disorders program, 83.3% (n = 252) agreed to participate in this observational study, four of whom were excluded due to age younger than 8 years. The final sample for this study included 203 youth due to missing data on the ED-15-Y or EDE-Q for 44 youth (17.7%). Participants were mostly White (75.9%) girls (75.9%) with a mean age of 15.09 years (SD = 1.99). Most were adolescents ages 14 to 18 (n = 151), with a smaller group of children ages 8 to 13 (n = 52). The most common diagnoses were AN (26.6%) and Atypical AN (27.5%). Additional detail about demographic and clinical characteristics is provided in Table 1.
Table 1.
Demographic and clinical characteristics of sample (N = 203).
| M (SD) or n (%) | [min, max] | |
|---|---|---|
| Race (White) | 154 (75.9%) | |
| American Indian or Alaska Native | 1 (0.5%) | |
| Asian | 17 (8.9%) | |
| Black | 2 (1.0%) | |
| Native Hawaiian or Other Pacific Islander | 1 (0.5%) | |
| Bi/multiracial | 25 (12.3%) | |
| Latino Ethnicity | 33 (16.3%) | |
| Gender (girls) | 154 (75.9%) | |
| Boys | 41 (19.7%) | |
| Transgirls | 3 (1.5%) | |
| Transboys | 6 (3.0%) | |
| Eating disorder diagnosis (any) | 189 (92.6%) | |
| AN | 54 (26.6%) | |
| Atypical AN | 56 (27.5%) | |
| ARFID | 23 (11.3%) | |
| BN | 14 (6.9%) | |
| BED | 4 (2.0%) | |
| Purging Disorder | 3 (1.5%) | |
| Rumination Disorder | 2 (1.0%) | |
| OSFED | ||
| OSFED BED | 2 (1.0%) | |
| OSFED BN | 3 (1.5%) | |
| “Other” OSFED | 27 (13.3%) | |
| Percent of median BMI | 99.32 (18.67) | [66.79, 166.48] |
| Duration of illness (months) | 23.29 (33.58) | [1,201] |
| ED-15-Y total | 3.09 (1.26) | [1.00, 5.00] |
| EDE-Q Global | 2.42 (1.85) | [0.00, 5.75] |
| EDY-Q total | 2.85 (1.08) | [1.00, 5.50] |
| SFSS total | 49.14 (9.05) | [32.74, 73.52] |
| CDI T-score | 70.82 (16.24) | [40, 90] |
| MASC T-score | 54.38 (13.76) | [29, 90] |
| Co-occurring psychiatric disorder (any) | 139 (68.5%) | |
| Mood disorder | 71 (35.0%) | |
| Anxiety disorder | 95 (46.8%) | |
| Previous medical hospitalization | 50 (24.6%) | |
| Previous psychiatric hospitalization | 13 (6.4%) | |
| Previous outpatient therapy | 139 (68.5%) |
Abbreviations: Anorexia nervosa (AN), Avoidant Restrictive Food Intake Disorder (ARFID), Bulimia nervosa (BN), Other Specified Feeding or Eating Disorder (OSFED), Binge Eating Disorder (BED), Eating Disorder-15 for Youth (ED-15-Y), Eating Disorders Examination-Questionnaire (EDE-Q), Eating Disorders in Youth-Questionnaire (EDY-Q), Symptoms and Functioning Severity Scale (SFSS), Child Depression Inventory (CDI), and Multidimensional Anxiety Scale for Children (MASC).
Demographic and clinical factors were examined in relation to missing ED-15-Y/EDE-Q data, revealing that missingness was not associated with any measured factors, including age, gender identity, race, ethnicity, eating disorder diagnosis, duration of illness, weight, treatment history, or co-occurring diagnosis (ps > .06).
Reliability
Factor structure.
The unrotated factor analysis revealed one factor (eigenvalue = 6.791), consisting of all ten items, with loadings from 0.702 to 0.936. All other unrotated factors had Eigenvalues of .794 and lower. The direct oblimin rotation did not result in a multifactor solution because only one factor could be extracted, and therefore the solution was not rotated. ED-15-Y items had the following loadings on the single, general factor: worry about losing control over eating (.702), avoid people/places due to appearance (.738), think about food and eating constantly (.751), compare body negatively to others (.889), avoid looking at body (.726), uptight or nervous about weight (.915), body checking (.833), strict rules about eating (.610), uptight or nervous about shape (.936), and worry others will judge shape (.881).
Internal consistency.
The ED-15-Y demonstrated excellent internal consistency (Cronbach’s alphas = .946) and split-half reliability (Spearman-Brown coefficients = .945). Internal consistencies (Cronbach’s alphas) were .973 for the EDE-Q, .719 for the EDY-Q, .863 for the CDI-2, .799 for the MASC-10, and .925 for the SFSS.
Sensitivity to change over time
Youth with eating disorders involving weight and shape concerns (n = 57) completed the ED-15-Y an average of 4.04 times (SD = 2.41) in the first eight sessions. The majority of these youth were engaging in family-based treatment (n = 48, 87.7%) for AN or Atypical AN (n = 42, 76.3%). Completed ED-15-Ys (n = 230) were relatively evenly distributed across sessions (i.e., ED-15-Ys per session represented 10.0% and 15.2% of all available data). There was a significant effect of time on ED-15-Y scores, such that scores decreased by 0.118 (SE = 0.017, F = 50.895, p < .001) per session in the early phase of treatment (i.e., total reduction of .823 between sessions 1 and 8), after adjusting for baseline ED-15-Y score (B = 0.532, SE = 0.110, F = 23.284, p < .001).
Validity
Convergent validity.
Eating disorder psychopathology.
The ED-15-Y demonstrated high convergence with the longer self-report measure of eating disorder psychopathology (EDE-Q) in adolescents 14 years and older (r = .892, p <.001) and youth ages 8 to 13 (r = .935, p <.001). The five behavioral items on the ED-15-Y were compared to their matching items on the EDE-Q (i.e., dietary restraint, binge eating, vomiting, laxative misuse, and driven exercise). Given the different timeframes of the measures, not all of the youth who endorsed behaviors on the EDE-Q (past month) would be expected to endorse those behaviors on the ED-15-Y (past week), but all of the youth endorsing behaviors on the ED-15-Y would be expected to endorse those behaviors on the EDE-Q. There was statistically significant convergence across all five behaviors (dietary restraint: χ2 = 83.670, binge eating: χ2 = 69.691, vomiting: χ2 = 91.054, laxative misuse: χ2 = 63.096, driven exercise: χ2 = 80.482, ps < .001). Table 2 provides data on alignment in presence/absence of each of the five behaviors on the ED-15-Y and EDE-Q. Of note, 22% (n = 11) of the 51 individuals who endorsed binge eating in the past week had not endorsed binge eating in the past month, suggesting that the ED-15-Y item may be more sensitive to detecting binge episodes than the EDE-Q. For those who endorsed behaviors on both the ED-15-Y (days or episodes in past week) and EDE-Q (days in past month rated on a Likert scale), the correlation coefficients for behavior frequencies were as follows: restraint (days in past month v. past week: r = .618), objective bingeing (days in past month v. episodes in past week: r = .687); vomiting (days in past month v. episodes in past week: r = .684); and driven exercise (days in past month v. past week: r = .819) (ps < .01). The correlation for laxative misuse was not calculated due to low frequency of this behavior (n = 5). Missing data (skipped questions) occurred more frequently on the EDE-Q than the ED-15-Y for binge eating (6.4% v. 0.5%), vomiting (6.4% v. 1.0%), laxatives (6.9 v. 0.0%), and driven exercise (6.4% v. 0.0%), with no differences in restraint (0% overall).
Table 2.
Convergence on five behavioral items (i.e., dietary restraint, binge eating, vomiting, laxative misuse, and driven exercise) between the ED-15-Y and EDE-Q.
| Past month (EDE-Q) | Total Endorsed (n, %) | ||||
|---|---|---|---|---|---|
| No (n, %) | Yes (n, %) | ||||
| Dietary Restraint | Past week (ED-15-Y) | No | 67 (33.2%) | 41 (20.3%) | |
| Yes | 1 (0.5%) | 93 (46.0%) | 135 (66.2%) | ||
| Binge Eating | Past week (ED-15-Y) | No | 117 (62.2%) | 20 (10.6%) | |
| Yes | 11 (5.9%) | 40 (21.3%) | 71 (34.8%) | ||
| Vomiting | Past week (ED-15-Y) | No | 149 (79.7%) | 13 (7.0%) | |
| Yes | 3 (1.6%) | 22 (11.8%) | 38 (18.6%) | ||
| Laxative Misuse | Past week (ED-15-Y) | No | 176 (93.6%) | 5 (2.7%) | |
| Yes | 2 (1.1%) | 5 (2.7%) | 12 (5.9%) | ||
| Driven Exercise | Past week (ED-15-Y) | No | 98 (51.9%) | 26 (13.8%) | |
| Yes | 7 (3.7%) | 58 (30.7%) | 91 (44.6%) | ||
Co-occurring psychopathology.
ED-15-Y correlations with overall psychopathology (SFSS total score: r = .671), anxiety (MASC-10 T-score: r = .482), and depression (CDI-2 T-score: r = .734) were moderate to strong and comparable to correlations between the EDE-Q and these measures (SFSS: r = .605, CDI: r = .697, and MASC: r = .402) (all ps < .001), as expected given the overlap between these domains and eating disorder psychopathology. Consistent with expectations, these correlations were smaller than the direct correlation between the ED-15-Y and EDE-Q.
Discriminant validity.
As expected, the association between the ED-15-Y and ARFID symptomatology was weak (EDY-Q: r = .347, p < .001) and comparable to the EDE-Q’s association with the EDY-Q (r = .356, p < .001).
Concurrent validity.
Diagnosis (comparing scores of individuals with AN, Atypical AN, and BN to those with ARFID and also no eating disorder) was significantly associated with ED-15-Y scores (F = 21.575, p < .001) (see Figure 1). Post-hoc comparisons indicated that ED-15-Y scores were not significantly different between youth with no eating disorder and those with ARFID (p = 0.13). For youth with an eating disorder involving weight and shape concerns (i.e., AN, atypical AN, and BN), their scores were higher than for youth without an eating disorder (ps ≤ .005) or youth with ARFID (ps < .001). Consistent with expectations, youth with BN had significantly higher scores than those with AN or atypical AN (ps < .01), and youth with atypical AN had higher scores than those with AN (p = .018).
Figure 1.
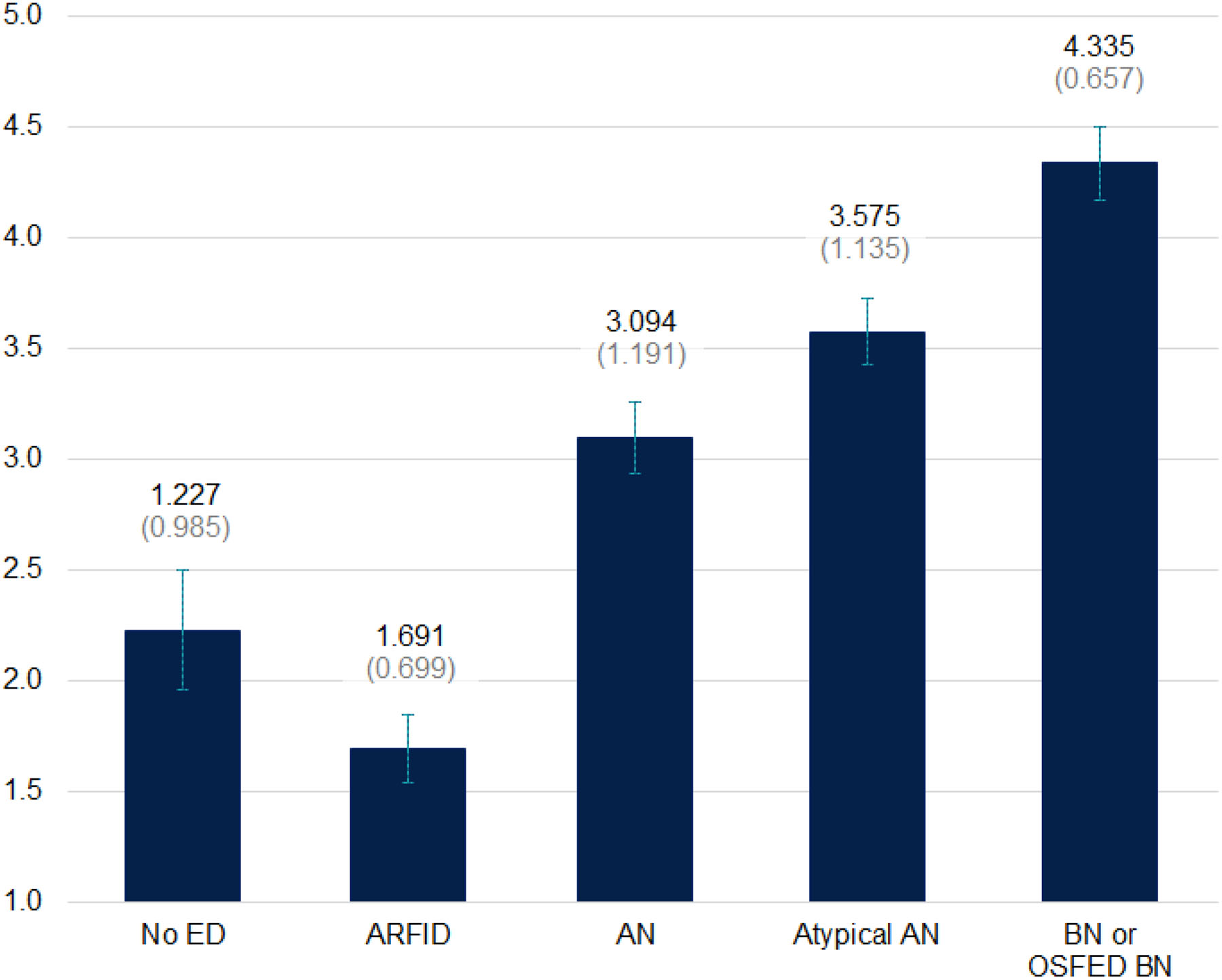
ED-15-Y scores across eating disorder diagnoses with mean (SD).
Abbreviations: Eating disorder (ED), Avoidant Restrictive Food Intake Disorder (ARFID), Anorexia nervosa (AN), Bulimia nervosa (BN), Other Specified Feeding or Eating Disorder (OSFED).
Discussion
This study provides support for the use of the ED-15-Y to assess eating disorder psychopathology in youth ages 8 to 18 years. It had a robust single-factor solution and can therefore be scored as a single scale. The ED-15-Y eating disorders psychopathology score (first ten items) and the behavioral items (last five items) demonstrated excellent reliability, convergent validity, discriminant validity, and concurrent validity in this study. The ED-15-Y demonstrated high sensitivity to change over time for youth with eating disorders involving weight and shape concerns, establishing its utility in measuring session-to-session change in symptomatology. The statistically and clinically significant change (reduction of .82 on a five-point scale) is particularly notable because most youth were receiving family-based treatment for AN or Atypical AN and might not have been expected to demonstrate cognitive change within the first eight sessions of treatment.
Convergent validity was established with the ED-15-Y’s strong association with the EDE-Q (rs = .89 and .94 for adolescents and youth, respectively). The strength of the correlation is somewhat surprising given the different timeframes of the measures (seven versus 28 days), but it is similar to that between the EDE-Q and the “short” version of the EDE-Q that refers to the past seven days in a previous study of adults with eating disorders (r = .82, Gideon et al., 2016). It is possible that attitudinal symptoms are relatively stable in the month prior to presentation. Alternatively, youth may be more highly influenced by recent attitudinal symptoms because recent history is more salient and/or easier to recall, or because youth have difficulty differentiating between the past week and the past month timeframes. Measures of general psychopathology, depression, and anxiety also helped to establish discriminant validity, with correlations that were moderate and comparable to those between the same measures and the EDE-Q. Concurrent validity was demonstrated through expected mean differences by diagnosis, where youth with BN had the highest scores, followed by youth with Atypical AN, then AN, all of whom had higher scores than youth with ARFID or no eating disorder.
This is the first study to our knowledge examining a brief measure of eating disorder symptoms for youth. Strengths of this study include the use of a cross-diagnostic sample of youth with eating disorders, including children as young as eight years old, and its examination of psychometric properties, including factor structure, reliability, sensitivity to change over time, and multiple types of validity. Limitations of this study include the relatively modest sample size, missing data, and the lack of a community sample with which to establish community norms and examine factor structure equivalence across age groups. In addition, the use of the EDE-Q in this young sample is inappropriate given the lack of psychometric data on the EDE-Q in children. Nevertheless, the high correlation between the ED-15-Y and the EDE-Q in the younger sample demonstrates some convergence, and this represents just one of several types of validity examined in this study.
Since early treatment response is a potent predictor of outcome at the end of treatment for youth with AN (Doyle, Le Grange, Loeb, Doyle, & Crosby, 2010; Le Grange, Accurso, Lock, Agras, & Bryson, 2014) and BN (Le Grange, Doyle, Crosby, & Chen, 2008), measures with high reliability, validity, and sensitivity to detect change (or lack thereof) early in therapy are essential. Even when empirically-supported treatments are implemented in the context of trials, only about half of youth respond well (Le Grange, Lock, Agras, Bryson, & Jo, 2015; Lock, Le Grange, Agras, Moye, Bryson, & Jo, 2010). Further, treatment effects may be diluted in “real world” practice due to implementation drift (Accurso, Fitzsimmons-Craft, Ciao, & Le Grange, 2015; Accurso, Le Grange, & Graham, 2020; Kosmerly, Waller, & Robinson, 2014), highlighting the importance of other potential avenues to improve treatment outcomes in youth with eating disorders. To this aim, ROM may be an important potential avenue to pursue.
The ED-15-Y is a free, rapidly administered, easily scored measure of eating disorder psychopathology for youth that is sensitive to change over time, allowing clinicians to objectively track youth outcome in the context of treatment. However, future efforts are needed to determine whether the ED-15-Y would be an appropriate measure for ROM. Future research with the ED-15-Y might allow for session-by-session examination of how psychotherapy process (e.g., common factors such as therapeutic alliance, or use of particular treatment techniques) predicts patterns of symptom change. Such research is needed to inform our understanding of how cognitive symptoms respond to changes in weight and/or binge/purge behaviors, as well as the relation between eating disorders psychopathology and co-occurring psychopathology over time. In combination, this knowledge can advance the refinement and optimization of existing treatments for youth with eating disorders.
Supplementary Material
Acknowledgments
We would like to acknowledge Madeleine Tatham, Hannah Turner, Victoria A. Mountford, Ashley Tritt, and Rebecca Dyas for their contributions in the development of the original ED-15 measure, which was adapted with their permission. The first author is supported by the National Institute of Mental Health (K23 MH120347).
Footnotes
Data Sharing
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy and ethical restrictions.
Conflict of Interest Statement
The authors have no conflict to declare.
This is the peer reviewed version of the following article: Accurso, E. C., & Waller, G. (2021). A brief session-by-session measure of eating disorder psychopathology for children and adolescents: Development and psychometric properties of the Eating Disorder-15 for Youth (ED-15-Y). International Journal of Eating Disorders, 54, 569–577, which has been published in final form at https://onlinelibrary.wiley.com/doi/10.1002/eat.23449.
References
- Accurso EC, Fitzsimmons-Craft EE, Ciao AC, & Le Grange D (2015). From efficacy to effectiveness: Comparing outcomes for youth with anorexia nervosa treated in research trials versus clinical care. Behaviour Research and Therapy, 65, 36–41. 10.1016/j.brat.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accurso EC, Le Grange D, & Graham AK (2020). Attitudes towards family-based treatment impact therapists’ intent to change their therapeutic practice for adolescent anorexia nervosa. Frontiers in Psychiatry, 11, 305. 10.3389/fpsyt.2020.00305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athay MM, Riemer M, & Bickman L (2012). The Symptoms and Functioning Severity Scale (SFSS): Psychometric evaluation and discrepancies among youth, caregiver, and clinician ratings over time. Administration and Policy in Mental Health and Mental Health Services Research, 39, 13–29. 10.1007/s10488-012-0403-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balantekin KN, Hayes JF, Sheinbein DH, Kolko RP, Stein RI, Saelens BE, … & Epstein LH (2017). Patterns of eating disorder pathology are associated with weight change in family-based behavioral obesity treatment. Obesity, 25, 2115–2122. 10.1002/oby.22028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, & Crow SJ (2011). Convergence of scores on the interview and questionnaire versions of the Eating Disorder Examination: A meta-analytic review. Psychological Assessment, 23, 714–724. https://doi/10.1037/a0023246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickman L, Athay MM, Riemer M, Lambert EW, Kelley SD, Breda C, … & Vides de Andrade AR (Eds.). (2010). Manual of the Peabody Treatment Progress Battery, 2nd ed. [Electronic version]. Nashville, TN: Vanderbilt University. http://peabody.vanderbilt.edu/ptpb [Google Scholar]
- Bickman L, Kelley SD, Breda C, de Andrade AR, & Riemer M (2011). Effects of routine feedback to clinicians on mental health outcomes of youths: Results of a randomized trial. Psychiatric Services, 62, 1423–1429. 10.1176/appi.ps.002052011 [DOI] [PubMed] [Google Scholar]
- Binford RB, Le Grange D, & Jellar CC (2005). Eating disorder examination versus eating disorder examination-questionnaire in adolescents with full and partial-syndrome bulimia nervosa and anorexia nervosa. International Journal of Eating Disorders, 37, 44–49. 10.1002/eat.20062 [DOI] [PubMed] [Google Scholar]
- Carlier IV, Meuldijk D, Van Vliet IM, Van Fenema E, Van der Wee NJ, & Zitman FG (2012). Routine outcome monitoring and feedback on physical or mental health status: evidence and theory. Journal of Evaluation in Clinical Practice, 18, 104–110. 10.1111/j.1365-2753.2010.01543.x [DOI] [PubMed] [Google Scholar]
- Carter JC, Stewart DA, & Fairburn CG (2001). Eating Disorder Examination Questionnaire: Norms for young adolescent girls. Behaviour Research and Therapy, 39(5), 625–632. 10.1016/S0005-7967(00)00033-4 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Growth Charts. (2002). Advanced Pediatric Assessment. https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/tool_for_schools.html
- Child Outcomes Research Consortium. (2020, November 13). Eating Disorder Examination. https://www.corc.uk.net/outcome-experience-measures/eating-disorder-examination
- Doyle PM, Le Grange D, Loeb K, Doyle AC, & Crosby RD (2010). Early response to family-based treatment for adolescent anorexia nervosa. International Journal of Eating Disorders, 43, 659–662. 10.1002/eat.20764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichen DM, Strong DR, Rhee KE, Rock CL, Crow SJ, Epstein LH, … & Boutelle KN (2019). Change in eating disorder symptoms following pediatric obesity treatment. International Journal of Eating Disorders, 52, 299–303. 10.1002/eat.23015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders. The Guilford Press. [Google Scholar]
- Fairburn CG, & Beglin S (2008). Eating Disorder Examination Questionnaire (6.0). In Fairburn CG (Ed.), Cognitive behavior therapy and eating disorders. (pp. 309–313). Guilford Press. [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: interview or self-report questionnaire? International Journal of Eating Disorders, 16, 363–370. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper I The eating disorder examination. In: Fairburn CG CG & Wilson GT (Eds.) Binge Eating: Nature, Assessment, and Treatment. 12th ed. New York, NY: Guilford Press; 1993. [Google Scholar]
- Garber AK, Cheng J, Accurso EC, Adams SH, Buckelew SM, Kapphahn CJ, Kreiter A, Le Grange D, Machen VI, Moscicki A, Saffran K, Sy A, Wilson L, & Golden NH (2019). Weight loss and illness severity in adolescents with atypical anorexia nervosa. Pediatrics, 144, 1–11. 10.1542/peds.2019-2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, & Serpell L (2016). Development and psychometric validation of the EDE-QS, a 12 item short form of the Eating Disorder Examination Questionnaire (EDE-Q). PLoS One, 11(5), e0152744. 10.1371/journal.pone.0152744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Doyle AC, & Wilfley DE (2007). Assessment of binge eating in overweight youth using a questionnaire version of the child eating disorder examination with instructions. International Journal of Eating Disorders, 40(5), 460–467. 10.1002/eat.20387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorrell S, Lebow J, Kinasz K, Mitchell JE, Goldschmidt AB, Le Grange D, & Accurso EC (2020). Psychotropic medication use in treatment-seeking youth with eating disorders. European Eating Disorders Review, 28, 739–749. 10.1002/erv.2788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog DB, Keller MB, Sacks NR, Yeh CJ, & Lavori PW (1992). Psychiatric comorbidity in treatment-seeking anorexics and bulimics. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 810–818. 10.1097/00004583-199209000-00006 [DOI] [PubMed] [Google Scholar]
- Hilbert A, & van Dyck Z (2016). Eating Disorders in Youth-Questionnaire: English version. University of Leipsig. http://nbn-resolving.de/um:nbn:de:bsz:15-qucosa-197246 [Google Scholar]
- Jennings KM, & Phillips KE (2017). Eating Disorder Examination–Questionnaire (EDE–Q): norms for clinical sample of female adolescents with anorexia nervosa. Archives of Psychiatric Nursing, 31(6), 578. 10.1016/j.apnu.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kass AE, Theim Hurst K, Kolko RP, Ruzicka EB, Stein RI, Saelens BE, … & Wilfley DE (2017). Psychometric evaluation of the youth eating disorder examination questionnaire in children with overweight or obesity. International Journal of Eating Disorders, 50(7), 776–780. 10.1002/eat.22693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmerly S, Waller G and Robinson AL (2014). Clinician adherence to guidelines in the delivery of family-based therapy for eating disorders. International Journal of Eating Disorders, 48(2), 223–229. 10.1002/eat.22276 [DOI] [PubMed] [Google Scholar]
- Kovacs M, & MHS Staff. (2011). Children’s Depression Inventory 2 (CDI 2), 2nd ed. Multi-Health Systems. [Google Scholar]
- Kurz S, Van Dyck Z, Dremmel D, Munsch S, & Hilbert A (2015). Early-onset restrictive eating disturbances in primary school boys and girls. European Child & Adolescent Psychiatry, 24(7), 779–785. 10.1007/s00787-014-0622-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Accurso EC, Lock J, Agras S, & Bryson SW (2014). Early weight gain predicts outcome in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders, 47, 124–129. 10.1002/eat.22221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Crosby RD, Rathouz PJ, & Leventhal BL (2007). A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Archives of General Psychiatry, 64(9), 1049–1056. 10.1001/archpsyc.64.9.1049 [DOI] [PubMed] [Google Scholar]
- Le Grange D, Doyle P, Crosby RD, & Chen E (2008). Early response to treatment in adolescent bulimia nervosa. International Journal of Eating Disorders, 41, 755–757. 10.1002/eat.20566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Agras WS, Bryson SW, & Jo B (2015). Randomized clinical trial of family-based treatment and cognitive-behavioral therapy for adolescent bulimia nervosa. Journal of the American Academy of Child & Adolescent Psychiatry, 54(11), 886–894. 10.1016/j.jaac.2015.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M,M, (2015). DBT skills training manual (2nd ed). The Guilford Press. [Google Scholar]
- Lock J (2020). Adolescent-focused therapy for anorexia nervosa: A developmental approach. The Guilford Press. [Google Scholar]
- Lock J (2015). An update on evidence-based psychosocial treatments for eating disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology, 44(5), 707–721. 10.1080/15374416.2014.971458 [DOI] [PubMed] [Google Scholar]
- Lock J, Agras WS, Bryson S, & Kraemer HC (2005). A comparison of short- and long-term family therapy for adolescent anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 632–639. 10.1097/01.chi.0000161647.82775.0a [DOI] [PubMed] [Google Scholar]
- Lock J, & Le Grange D (2013). Treatment manual for anorexia nervosa: A family-based approach (2nd ed). The Guilford Press. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Fitzpatrick KK, Jo B, Accurso E, … & Stainer M (2015). Can adaptive treatment improve outcomes in family-based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi-site treatment study. Behaviour Research and Therapy, 73, 90–95. 10.1016/j.brat.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, & Jo B (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry, 67, 1025–1032. 10.1001/archgenpsychiatry.2010.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luce KH, Crowther JH (1999). The reliability of the Eating Disorder Examination-Self-Report Questionnaire (EDE-Q). International Journal of Eating Disorders, 25, 349–51. [DOI] [PubMed] [Google Scholar]
- March JS (1997). Multidimensional anxiety scale for children short version (MASC-10). Multi-Health Systems. [Google Scholar]
- March JS, Sullivan K, & Parker J (1999). Test-retest reliability of the Multidimensional Anxiety Scale for Children. Journal of Anxiety Disorders, 13, 349–358. 10.1016/S0887-6185(99)00009-2 [DOI] [PubMed] [Google Scholar]
- Noetel M, Miskovic-Wheatley J, Crosby RD, Hay P, Madden S, & Touyz S (2016). A clinical profile of compulsive exercise in adolescent inpatients with anorexia nervosa. Journal of Eating Disorders, 4, 1. 10.1186/s40337-016-0090-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rynn MA, Barber JP, Khalid-Khan S, Siqueland L, Dembiski M, McCarthy KS, & Gallop R (2006). The psychometric properties of the MASC in a pediatric psychiatric sample. Journal of Anxiety Disorders, 20, 139–157. 10.1016/j.janxdis.2005.01.004 [DOI] [PubMed] [Google Scholar]
- Sawyer SM, Whitelaw M, Le Grange D, Yeo M, & Hughes EK (2016). Physical and psychological morbidity in adolescents with atypical anorexia nervosa. Pediatrics, 137(4), e20154080. 10.1542/peds.2015-4080 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … & Wilkinson B (2010). Reliability and validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). The Journal of Clinical Psychiatry, 71(3), 313–326. 10.4088/JCP.09m05305whi [DOI] [PubMed] [Google Scholar]
- Sheinbein DH, Stein RI, Hayes JF, Brown ML, Balantekin KN, Conlon RPK, … & Epstein LH (2019). Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: A social-ecological approach. Pediatric Obesity, 14(8), e12518. 10.1111/ijpo.12518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimokawa K, Lambert MJ, & Smart DW (2010). Enhancing treatment outcome of patients at risk of treatment failure: Meta-analytic and mega-analytic review of a psychotherapy quality assurance system. Journal of Consulting and Clinical Psychology, 78, 298–311. 10.1037/a0019247 [DOI] [PubMed] [Google Scholar]
- Skjåkødegård HF, Danielsen YS, Morken M, Linde SRF, Kolko RP, Balantekin KN, … & Júlíusson PB (2016). Study Protocol: A randomized controlled trial evaluating the effect of family-based behavioral treatment of childhood and adolescent obesity–The FABO-study. BMC Public Health, 16(1), 1106. 10.1186/s12889-016-3755-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sysko R, Glasofer DR, Hildebrandt T, Klimek P, Mitchell JE, Berg KC, … & Walsh BT (2015). The Eating Disorder Assessment for DSM-5 (EDA-5): Development and validation of a structured interview for feeding and eating disorders. International Journal of Eating Disorders, 48(5), 452–463. 10.1002/eat.22388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatham M, Turner H, Mountford VA, Tritt A, Dyas R, & Waller G (2015). Development, psychometric properties and preliminary clinical validation of a brief, session-by-session measure of eating disorder cognitions and behaviors: The ED-15. International Journal of Eating Disorders, 48, 1005–1015. 10.1002/eat.22430 [DOI] [PubMed] [Google Scholar]
- Vall E, & Wade TD (2015). Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders, 48(7), 946–971. 10.1002/eat.22411 [DOI] [PubMed] [Google Scholar]
- White HJ, Haycraft E, Goodwin H, & Meyer C (2014). Eating disorder examination questionnaire: Factor structure for adolescent girls and boys. International Journal of Eating Disorders, 47(1), 99–104. 10.1002/eat.22199 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


