Abstract
We launched a survey in April 2020 to assess the number and proportion of hospital workers infected during the first wave of the COVID-19 pandemic in France, and to assess the attributable mortality. All French hospital settings (HS) were invited to declare new cases and attributable deaths by occupation category each week. Between March 1 and June 28, 2020, participating HS accounted for 69.5% of the total number of HS workers in France, and declared 31,088 infected workers; 16 died from the infection. We estimated that 3.43% (95% CI: 3.42–3.45) of French workers in HS, and 3.97% (95% CI: 3.95–3.99) of healthcare workers were infected during the first wave. Workers in regions with a cumulative rate of hospitalized COVID-19 patients equal or above the national rate, HS other than tertiary hospitals, or occupations with frequent patient contacts were particularly impacted. Targeted prevention campaigns should be elaborated.
Keywords: COVID-19, Healthcare workers, Hospital settings
Much like the rest of Europe, France has been deeply affected by the COVID-19 pandemic [1]. A general population lockdown was initiated on March 17, 2020, in the face of a rapid increase in the number of cases, and was lifted on May 11, 2020. During this first wave, the scarcity of personnel protective equipment and difficulty to diagnose COVID-19 cases put professionals in hospital settings (HS) at high risk of being exposed to SARS-CoV-2 [2], [3], [4]. As French surveillance systems were not designed to estimate the impact of the pandemic on hospital workers, we launched a nationwide survey in April 2020 to estimate the number of infections and attributable deaths among salaried employees of HS, including healthcare workers (HCW) and non-HCW.
Here, we report on the burden of COVID-19 among workers in HS during the first wave of the pandemic. To our knowledge, only few regional assessments of the number of infected HCW have been reported and no estimation is available at the national level [5], [6].
All French HS, either public or private, were invited to participate. In each HS, a dedicated person has been prospectively declaring new cases, the occupation of cases, and attributable deaths on a weekly basis since April 13, 2020. Cases and deaths were retrospectively reported between March 1 and April 12, 2020. Reported deaths were individually confirmed by communication with the reporting site to be attributable to COVID-19.
Considering the lack of diagnostic tests during the first wave of the pandemic and heterogeneity in testing practices between settings, a case was either defined by a positive RT-PCR, a positive serological test following clinical symptoms, or by an assessment of the local COVID-19 investigation team based on clinical and epidemiological data.
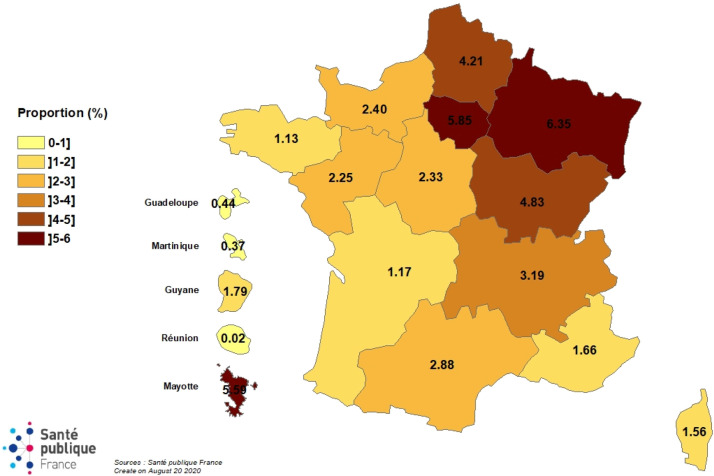
We classified French regions according to their cumulative rate of hospitalized COVID-19 patients during the study period, which was obtained from national surveillance: six “highly-affected regions” with a rate equal or above the national rate, and 12 “less-affected regions” with a rate below the national rate (Grand-Est, Haut de France, Île-de-France, and Bourgogne-Franche-Comté for mainland regions and Guyana and Mayotte for overseas regions, were classified as “highly-affected regions”. The 12 remaining regions were classified as “less-affected regions”) [1]. We defined teaching hospitals or military hospitals as tertiary hospitals; local hospitals as secondary hospitals; local private clinics as primary hospitals; psychiatric hospitals or oncology centers as specialized hospitals; long-term HS providing rehabilitation care as rehabilitation care centers; and dialysis centers or day hospitals as “other”.
During the 17-week period between March 1 and June 28, 2020, 1132 HS participated at least once in the survey. These settings account for 69.5% of the total number of HS workers in France, 98% of workers of French tertiary hospitals, and 68% of secondary hospitals [7]. No difference was observed between coverage in “highly-affected regions” and “less-affected regions” (69.8% vs. 69.3%). Regarding occupation, coverage of the survey was almost the same between HCW (69.1%) and non-HCW (70.6%). The coverage was above 58% for every occupation sub-category.
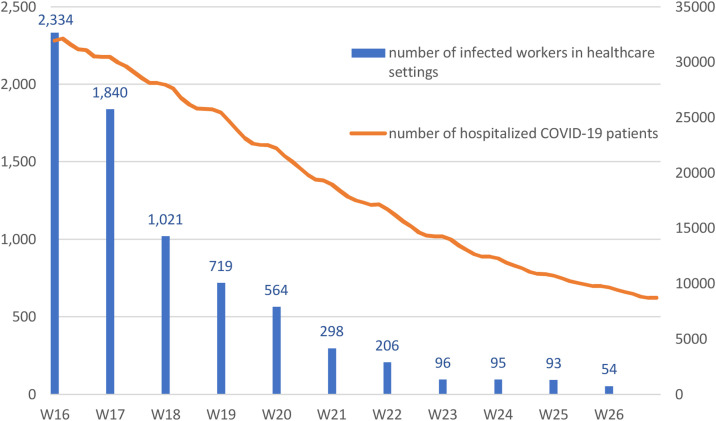
A total of 31,088 infections and 16 deaths among workers were reported by 829 HS (with a median of 10 cases per HS) while 303 HS reported no case. Based on the hypothesis that non-participating HS were less impacted by the outbreak, we estimated that the vast majority of HS workers infected during the first wave were reported in this survey. We note that reporting of infections in workers dropped faster than the number of patients hospitalized with COVID-19 in France (Fig. 1 ).
Fig. 1.
Weekly number of hospital setting workers (n = 7320) infected with COVID-19 and number of hospitalized COVID-19 patients, France (April 13 to June 28, 2020). Between March 1 and April 12, 2020, 23,768 cases occurred and were retrospectively reported aggregated, as prospective data collection started on April 13, 2020.
The vast majority (n = 25,337; 82%) of infections occurred in HCW, especially in nurses (29%) and healthcare assistants (25%). Among the 16 deaths reported, 10 were reported in HCW. Various proportions of HCW among the total number of COVID-19 cases during the first wave have been reported in different countries. HCW accounted for 3% of all COVID-19 cases in the United States [8], 5% in China [9], and much more in Italy (10%) [10] and Spain (20%) [11]. In France, the 25,337 cases reported in our survey represent 15% of the 164,801 confirmed cases reported during the same period [1]. However, as testing policies at the start of the pandemic were not homogenous and targeted in priority professionals and patients in hospitals, this proportion is probably overestimated.
We estimate that the 31,088 infected workers account for 3.43% (95% CI: 3.42–3.45) of French workers in HS (Table 1 ). Among HCW, this proportion is 3.97% (95% CI: 3.95–3.99). Five regions had a higher proportion of infected workers than the national proportion (Fig. 2 ). After adjustment, “highly-impacted regions” had significantly more infected workers than “less-impacted regions”.
Table 1.
Number and proportion of infected COVID-19 workers (n = 30,248a) by type of hospital setting, geographic area, and occupation, France (March 1 to June 28, 2020).
| Categories | Number of infected workers | Proportion (%) of infected workers [95% CI] | Adjusted odds ratio [95% CI] | P-value |
|---|---|---|---|---|
| Type of HS | ||||
| Tertiary hospital | 9963 | 2.83 [2.78–2.89] | Reference | |
| Secondary hospital | 13,526 | 4.02 [4.00–4.04] | 1.52 [1.48–1.56] | < 0.001 |
| Primary hospital | 3214 | 4.51 [4.46–4.57] | 1.66 [1.60–1.73] | < 0.001 |
| Specialized hospital | 2152 | 2.54 [2.50–2.59] | 1.05 [1.00–1.10] | 0.057 |
| Rehabilitation care | 1125 | 3.72 [3.67–3.76] | 1.37 [1.28–1.46] | < 0.001 |
| Other | 253 | 12.69 [12.12–13.25] | 1.63 [1.40–1.90] | < 0.001 |
| Unknown | 15 | [NA] | [NA] | [NA] |
| Geographic area | ||||
| Less-impacted regions | 19,377 | 5.34 [5.27–5.41] | Reference | |
| Highly-impacted regionsb | 10,871 | 2.10 [2.09–2.11] | 2.48 [2.42–2.54] | < 0.001 |
| Occupation | ||||
| HCW | 25,337 | 3.97 [3.95–3.99] | ||
| Nurses | 8922 | 3.79 [3.77–3.81] | Reference | |
| Healthcare assistants | 7561 | 4.91 [4.88–4.94] | 1.30 [1.26–1.34] | < 0.001 |
| Physicians | 3015 | 3.59 [3.57–3.61] | 0.92 [0.89–0.96] | < 0.001 |
| Residents | 1074 | 3.55 [3.53–3.57] | 1.00 [0.94–1.07] | 0.961 |
| Physiotherapists | 315 | 4.65 [4.62–4.68] | 1.23 [1.09–1.38] | 0.001 |
| Midwives | 195 | 1.62 [1.61–1.63] | 0.39 [0.34–0.45] | < 0.001 |
| Other HCW | 4255 | 3.66 [3.64–3.68] | 0.94 [0.91–0.98] | 0.001 |
| Non-HCW | 3208 | 1.32 [1.32–1.33] | 0.34 [0.33–0.35] | < 0.001 |
| Unknown | 1703 | [NA] | [NA] | [NA] |
| Totala | 30,248 | 3.43 [3.42–3.45] | [NA] | [NA] |
HCW: healthcare workers; HS: hospital setting; NA: not applicable.
Teaching hospitals or military hospitals were defined as tertiary hospitals; local hospitals as secondary hospitals; local private clinics as primary hospitals; psychiatric hospitals or oncology centers as specialized hospitals; long-term HS providing rehabilitation care as rehabilitation care centers; and dialysis centers or day hospitals as “other”.
Students (n = 840) were excluded from this analysis, as no published denominator was available.
Grand-Est, Haut de France, Île-de-France, and Bourgogne-Franche-Comté for mainland regions and Guyana and Mayotte for overseas regions, were classified as “highly-affected regions”. The remaining 12 regions were classified as “less-affected regions”.
Fig. 2.
Proportion of SARS-CoV-2-infected workers in hospital settings by region, France (March 1 to June 28, 2020).
Again, the proportions of infected HCW reported by studies in other countries vary greatly. A living review [12] reported this proportion ranging from 0.4% to 49.6% and when based on serological testing from 1.6% to 31.6%. This variability is linked to differences in study design, selection criteria, and sample sizes. Overall, most early studies were small and single centered. Our large coverage of both existing employees and hospital settings in France could explain why our proportion of infected HCW lies within the lower part of the range of estimates.
Interestingly, we found that infections were significantly more frequent among workers from secondary and primary hospitals than from tertiary hospitals. Tertiary settings were identified as referral hospitals at the start of the pandemic. We hypothesize that staff from these hospitals were more aware and better trained to apply preventive measures against the risk of SARS-CoV-2 infection, and may also have had better access to personal protective equipment. On the contrary, workers in secondary and primary hospitals may have received patients with fewer or atypical symptoms, especially at the start of the pandemic, and been unconsciously exposed to COVID-19.
Healthcare assistants and physiotherapists, followed by nurses and residents were the most affected workers (Table 1). Those categories have already been reported to be especially at risk in the literature [2], [13], as they have frequent and prolonged contacts with patients. This highlights the need for prevention strategies targeting these specific occupational categories.
The proportion of infected workers was higher in all types of HCW compared with non-HCW, except for midwives. Several articles reported a higher infection rate among HCW compared with non-HCW or the general population [2], [3], [14], suggesting the strong contribution of occupational exposure to the infection of HCW. In this study, we found a parallel trend between the weekly number of infected workers and the number of hospitalized COVID-19 patients. But notably, we observed a faster decline of COVID-19 cases in workers than in COVID-19 cases admitted to hospitals. This reveals that the risk of infection in professionals was particularly increased at the beginning of the pandemic, probably due to the shortage of personal protective equipment and to a general lack of precaution before transmission from asymptomatic individuals was recognized.
In addition, community exposure remains a common underlying factor of infection, as suggested by the temporal and spatial similarities between the proportion of infected workers and the general dynamics of the outbreak in France. Those similarities, also described in other studies [15], show that in addition to work exposure, community and family exposure is also a driver of infection among hospital workers, as reported elsewhere [2], [16]. Determining whether workers’ infections are linked to in-hospital or out-of-hospital exposure is difficult and our survey does not allow to disentangle occupational from community transmission.
Some additional limitations must be considered in our survey. First, as the survey was launched mid-April, two weeks past the epidemic peak in France, data corresponding to the very first phase of the outbreak were collected retrospectively; we therefore lack the temporal distribution of these cases. Second, as testing strategies during this first part of the pandemic differed for HCW and the general public, the proportion of infected HCW among the total cases may be overestimated. Third, the proportion of HS defined as “other” was low (11.8%), and we hypothesize that participating HS in this category were the most impacted by the pandemic, leading to an over-estimation of the proportion of infected workers. Lastly, because of the limited questionnaire length, no additional question was asked about infection control practices and protective equipment use in the workplace or about household or other community exposure to SARS-COV-2. Therefore, this survey cannot distinguish occupational from community transmission.
This survey highlights the high burden of COVID-19 in HS workers in France, with more than 1 in 30 hospital workers infected over the first four months of the pandemic. Workers in regions with a cumulative rate of hospitalized COVID-19 patients equal or above the national rate, HS other than tertiary hospitals, or occupations with frequent and prolonged patient contacts were particularly impacted. In light of these findings, targeted prevention campaigns should be organized, and protecting HCW to reduce the risk of SARS-CoV-2 transmission and to preserve the healthcare workforce in the face of an outbreak must remain a priority [17], [18].
This survey is still ongoing. Since July 1, 2020, the case definition includes asymptomatic cases diagnosed with serological tests and since November 2020 cases diagnosed with antigenic tests.
Funding statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. This survey was undertaken as part of the national surveillance functions of Santé publique France.
Disclosure of interest
The authors declare that they have no competing interest.
Ethical approval
All procedures performed in studies involving human partic-pants were in accordance with the 1964 Helsinki declaration and its later amendments.
Contribution of authors
All authors were involved in the conception and design of the study.
MCC contributed to implementing the survey, data curation, conducting data analysis, interpreting the results and writing the article.
IP contributed to implementing the survey, data management and interpreting the results.
SM contributed to data management, data analysis, and interpreting the results.
ABC and SV contributed to interpreting the results and writing the article.
SLV contributed to writing the second draft of the article.
CO, NF, FG, GP, EDA, EB, ER, DA were members of the coordination team, contributed to promoting survey and to result interpretation.
Acknowledgments
The authors gratefully thank participating hospitals for their involvement in this survey and data collection during this busy epidemic period. We also acknowledge all our regional partners (Centers for the Prevention of Healthcare-Associated Infections, and regional units of Santé publique France) for their involvement in the study promotion, in particular the AP–HP infection control team and the Mayotte regional unit. We thank Jean-Michel Thiolet (French Minister of Health) for his advice in designing the survey. Our thanks also to Cécile Sommen and Côme Daniau (Santé publique France) for their help and advice concerning the analysis, and to Victoria Grace for the English revision of the article.
References
- 1.Santé publique France . Santé publique France; Saint-Maurice: 2020. COVID-19 : point épidémiologique du 25 juin 2020. [cited 13 October 2020. Available from: https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-25-juin-2020] [Google Scholar]
- 2.Akinbami L.J., Vuong N., Petersen L.R., Sami S., Patel A., Lukacs S.L., et al. SARS-CoV-2 seroprevalence among healthcare, first response, and public safety personnel, Detroit Metropolitan Area, Michigan, USA, May–June 2020. Emerg Infect Dis. 2020;26(12):2863–2871. doi: 10.3201/eid2612.203764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.G., Ma W., et al. Risk of COVID-19 among front-line healthcare workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shah A.S.V., Wood R., Gribben C., Caldwell D., Bishop J., Weir A., et al. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: nationwide linkage cohort study. BMJ. 2020;371:m3582. doi: 10.1136/bmj.m3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Contejean A., Leporrier J., Canoui E., Alby-Laurent F., Lafont E., Beaudeau L., et al. Comparing dynamics and determinants of SARS-CoV-2 transmissions among healthcare workers of adult and pediatric settings in central Paris. Clin Infect Dis. 2020;72:257–264. doi: 10.1093/cid/ciaa977. [PMID: 33501952; PMCID: PMC7454459] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Assistance publique–Hôpitaux de Paris . 2020. Professionnels atteints de COVID-19 à l’AP–HP : baisse significative du nombre de nouveaux cas [Internet] [updated; cited 13 October 2020. Available from: https://www.aphp.fr/actualite/professionnels-atteints-de-covid-19-lap-hp-baisse-significative-du-nombre-de-nouveaux-cas] [Google Scholar]
- 7.Ministère de la Santé, Direction de la recherche, des études, de l’évaluation et des statistique . 2018. Statistique annuelle des établissements de santé. [cited 13 October 2020. Available from: https://www.sae-diffusion.sante.gouv.fr/sae-diffusion/accueil.htm] [Google Scholar]
- 8.US Center for disease control and prevention . 2020. Update: characteristics of healthcare personnel with COVID-19 — United States, February 12–July 16. [cited 13 October 2020. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6938a3.htm] [Google Scholar]
- 9.China CDC weekly . 2020. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China. [cited 13 October 2020. Available from: http://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2020.032] [PMC free article] [PubMed] [Google Scholar]
- 10.Epicentro. COVID-19 integrated surveillance data in Italy [Internet]. [updated; cited 13 October 2020. Available from: https://www.epicentro.iss.it/en/coronavirus/sars-cov-2-dashboard].
- 11.Instituto de Salud Carlos III. Informe COVID-19 no 23. [cited 13 October 2020. Available from: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx].
- 12.Chou R., Dana T., Buckley D.I., Selph S., Fu R., Totten A.M. Update Alert 4: epidemiology of and risk factors for Coronavirus infection in healthcare workers. Ann Intern Med. 2020;173:143–144. doi: 10.7326/L20-1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eyre D.W., Lumley S.F., O’Donnell D., Campbell M., Sims E., Lawson E., et al. Differential occupational risks to healthcare workers from SARS-CoV-2 observed during a prospective observational study. Elife. 2020;9:e60675. doi: 10.7554/eLife.60675. [PMID: 32820721; PMCID: PMC7486122] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ran L., Chen X., Wang Y., Wu W., Zhang L., Tan X. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Consonni D., Bordini L., Nava C., Todaro A., Lunghi G., Lombardi A., et al. COVID-19: what happened to the healthcare workers of a research and teaching hospital in Milan, Italy? Acta Biomed. 2020;91(3):e2020016. doi: 10.23750/abm.v91i3.10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steensels D., Oris E., Coninx L., Nuyens D., Delforge M.L., Vermeersch P., et al. Hospital-wide SARS-CoV-2 antibody screening in 3056 staff in a tertiary center in Belgium. JAMA. 2020;324(2):195–197. doi: 10.1001/jama.2020.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.European Centre for Disease Prevention and Control. Infection prevention and control and preparedness for COVID-19 in healthcare settings – sixth update. ECDC: Stockholm. [Available from: https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings].
- 18.WHO . WHO; Geneva: 2020. Interim guidance: infection prevention and control during healthcare when coronavirus disease (COVID-19) is suspected or confirmed. [cited 13 October 2020. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC-2020.4] [Google Scholar]