Abstract
Graphic cigarette warnings increase quit attempts. Perceived message effectiveness and message avoidance are predictive of later quit attempts. We sought to examine whether randomized exposure to warning messages would inadvertently increase intentions to use alternate tobacco products (ATPs) while enhancing attempts to quit cigarettes. An online survey of 1,392 adult smokers in the US asked participants to rate six randomly selected tobacco warnings (from a set of 319) on perceived effectiveness and avoidance intentions. These two indicators of message effectiveness were calculated at the message-level and then at the individual campaign-level to facilitate causal inference. After viewing a message campaign of six warning messages, participants indicated their intentions to use ATPs. 68% of participants reported some intention to use e-cigarettes and intentions to use other ATPs ranged from 31% to 40%. Campaigns of messages eliciting higher avoidance increased the odds of intending to use hookah (aOR:4.32), smokeless tobacco (aOR:4.88), and snus (aOR:8.06), but not the intention to use electronic cigarettes. These relationships are mediated by intentions to quit smoking (all p<.05). Viewing campaigns with higher campaign-level perceived effectiveness increased the intentions to quit, which in turn increased intentions to try alternate tobacco products. Our findings increase the tobacco control community’s understanding of unintended consequences of graphic tobacco warnings.
Introduction
Tobacco communication
Worldwide, tobacco use causes nearly 8 million deaths per year (World Health Organization, 2019). In the US, 16 million Americans are living with smoking-related disease (U.S. Department of Health and Human Services, 2020). The World Health Organization proposed the Framework Convention on Tobacco Control (FCTC) in 2003 with the goal of decreasing the number of smokers worldwide (World Health Organization, 2003). The FCTC encourages use of graphic warnings on tobacco packs to increase the effectiveness of tobacco prevention campaigns. Cigarette packs have proven to be an effective communication device for tobacco companies (Slade, 1997; Wakefield et al., 2002), and research has shown they can be effective tools to communicate about the health risks of smoking (Hammond, 2011).
Communication and media campaigns designed to encourage healthy behaviors and deter unhealthy ones are commonly used to improve the health of the public. The WHO FCTC recommends large pictorial warnings appear on cigarette packages because of evidence that, compared to text only warnings, graphic warnings communicate health risks more effectively (World Health Organization, 2003). Research has shown that graphic warning messages, including labels on cigarette packs, or mass media campaigns like The Real Cost, or Tips from a Former Smoker are effective at preventing smoking initiation (Farrelly et al., 2017), increasing population level quit intentions (Brewer et al., 2016; Davis et al., 2018; Duke et al., 2015; Noar, Francis, et al., 2016), quit attempts (Brewer et al., 2016; Davis et al., 2018; Murphy-Hoefer et al., 2018; Noar, Francis, et al., 2016), and sustained quits (Murphy-Hoefer et al., 2018). Perceived effectiveness and intentions to avoid the warnings are intermediate outcomes of graphic warnings that are associated with quit attempts (Brewer et al., 2018; Hall et al., 2017; Hammond & White, 2012). These campaigns require substantial amounts of time, money, and effort to promote health; however even successful communication campaigns can have unintended effects (Byrne & Niederdeppe, 2012; Cho & Salmon, 2007).
Unintended consequences of heath communication
Despite the undeniable overall effectiveness of communication campaigns to reduce tobacco consumption, there are examples of new policies or media campaigns having unintended and undesirable consequences. Some campaigns even produce boomerang effects, increasing smoking (Rogers & Mewborn, 1976), drinking (Kleinot & Rogers, 1982), and drug initiation (Hornik et al., 2008) -- the very behaviors the campaigns were designed to deter. According to (Glantz, 1996), the campaign to stop underage smoking enabled the tobacco industry and was associated with increased cigarette sales, as the message “we don’t want kids to smoke” implied that smoking is an “illicit pleasure,” a “declaration of independence,” and a “self-identity.”
Iatrogenic effects are different from boomerang effects in that they yield effects that are undesirable and unexpected but not necessarily opposite to the intended effect. For example, breast cancer prevention messages emphasizing the need for women with a family history of breast cancer to have regular mammography created a false sense of security among women who did not have a family history of breast cancer (Lerman et al., 1990). Guttman and Zimmerman (2000) found that in the face of health education messages promoting breast-feeding and society’s disapproval of breast-feeding in public, infant-raising women felt guilty, deprived, and frustrated.
Nicotine and alternate tobacco products
The nicotine in tobacco products is an addictive substance, but it is also a powerfully reinforcing drug. While it does not produce a euphoric high the way marijuana or opioids do, it has been shown to enhance the enjoyment of pleasurable activities (Perkins et al., 2017), and prolong the enjoyment of other activities (Karelitz & Perkins, 2018). Given the authorization of modified risk tobacco products and rise in popularity of e-cigarettes and other alternate tobacco products that provide users with nicotine, but with purportedly less health risk, it is crucial to understand how successful anti-smoking campaigns may have unintended impact on interest in alternate tobacco products.
We examine such an effect with cigarette warnings and their impact on intended use of alternative tobacco products, ones not directly implicated by the campaign. Would cigarette warning messages effective in reducing cigarette smoking also reduce interest in alternate tobacco products? Or, alternately, if the messages successfully reduced the intention to smoke, would smokers instead seek alternate nicotine sources?
Theoretical motivation for alternate tobacco use
Some theories of motivation suggest the responses to the range of tobacco products will be compensatory (seeking alternate sources of nicotine) rather than consistent (avoidance of all tobacco) (Higgins, 1998). People must balance competing desires of pleasure seeking and pain avoidance all the time. In the case of smoking, when barriers arise preventing engagement in a pleasure producing behavior, or information makes clear an increased risk for pain or disease, safety concerns and the avoidance of pain become dominant motivations leading to a need to reduce the behavior to avoid pain. However, this reduction simultaneously results in losing the reward provided by smoking and nicotine consumption. The balance is thrown off as the individual is motivated to reduce tobacco consumption but simultaneously motivated to find a way to reinstate similar rewards while maintaining safety (Higgins, 1998).
The core idea is that the behavior change required to increase safety by avoiding pain and cost intensifies the drive to replace the rewards lost with another potentially rewarding behavior. The person losing rewards from a behavior change is likely to seek alternative compensatory rewards that are equally satisfying. With the proliferation of alternative tobacco products about which the individual may know very little, the person may either categorize them with other combustible tobacco products (i.e. cigarettes) as equally unsafe and dangerous or, in a more hopeful and self-serving turn, see well-known combustible tobacco products as fundamentally different from alternate tobacco products that might be safer substitutes for the rewards lost. In the latter case, one is motivated to explore alternative products while reducing interest in standard combustible tobacco and turning away from it.
Changing an addictive behavior is especially challenging as it makes coping with the loss of pleasure from tobacco use very difficult. In these cases, the behaviors that reduce pleasure or increase pain are then changed but the need for pleasure or pain avoidance may well be satisfied by other behaviors whose status as highly risky is not yet settled. The tobacco industry currently offers tobacco products that are alternatives to smoking cigarettes, and FDA documents suggest that different tobacco products may fall on a continuum of differing levels of risk (Food and Drug Administration, 2012). General Snus and IQOS have been authorized to market their products as with MRTP claims, however whether other alternative tobacco products qualify as MRTPs is still being reviewed in the US. Some research has suggested that combustible tobacco (e.g. cigarettes and hookah) represents the most harmful type of product to individual health, while noncombustible (e.g. smokeless, snus, and dissolvable) and nontobacco products (e.g. e-cigarettes or vapes) represent less harmful products on the spectrum of risk to individual health (Fiore et al., 2014; Zeller, 2013; Zeller et al., 2009). While some of these products may be less harmful than combustible cigarettes (Abrams et al., 2018; Foulds et al., 2003), the tobacco control community is currently divided on whether use of these products is a good harm reduction strategy. While the science hasn’t reached any conclusions about the actual harm reduction value of these products, consumers perceptions are already being shaped by the limited information they have. In general, the public, especially young adults, view alternate tobacco products as less risky than combustible cigarettes (Getachew et al., 2018; Kong et al., 2019; Majeed et al., 2017).
Study rationale
The goal of graphic warnings is to encourage people to quit tobacco use in order to improve their health. However, if graphic warnings were to inadvertently increase people’s motivations to explore alternative tobacco products rather than quit tobacco use altogether, they would not be able to achieve maximal health impacts otherwise expected, especially for products known to be harmful or for products whose harm is uncertain. Although tobacco industry lawsuits have delayed implementation of graphic warnings in the US, the Food and Drug Administration (FDA) has proposed a revised set of warnings that have addressed concerns raised in the lawsuit (Re: R.J. Reynolds v. Food & Drug Administration, No. 11–5332 (D.C. Cir. 2013), 2013). Understanding possible unintended consequences of graphic warnings and associated message campaigns may provide important information as designs for new warnings are considered. This paper examines potential unintended consequences of graphic warnings on intentions to use alternative tobacco products.
Methods
Participants
We recruited 1,392 current smokers ages 18 or older through Survey Sampling International (SSI). Participants were considered smokers if they had smoked at least 100 cigarettes in their lifetime and currently smoke every day or some days (Jamal, 2016). Additionally, participants could not have participated in more than two online surveys about cigarette smoking or other tobacco products in the last three months. Participants included 589 men and 803 women, with a mean age of 43.7 years. Participants were diverse in race, education, and income (Table 1) but were not a representative sample of US adult smokers.
Table 1.
Participant Characteristics (n=1,392)
| M (SD) | |
| Age | 43.72 (12.57) |
| Contemplation ladder | 5.98 (2.91) |
| Fagerstrom score | 4.72 (2.39) |
| % (n) | |
| Gender | |
| Male | 42 (589) |
| Female | 58 (803) |
| College education or higher | 42 (584) |
| Hispanic | 9 (120) |
| White | 87 (1,203) |
| Income <$50K | 55 (768) |
Note: Missing data ranged from 0-.001%.
Procedures
Participants completed an eligibility survey, answered demographic survey questions, and information about their current smoking including the Fagerstrom scale (Heatherton et al., 1991), and the contemplation ladder (Biener & Abrams, 1991). Each participant viewed six warnings out of a pool of 319 previously developed and deployed pictorial tobacco warnings. The six tobacco warnings were randomly selected for each participant and presented in random order to that respondent. Participants viewed each warning for at least eight seconds. After each warning, participants assessed perceived effectiveness, emotional engagement, negative emotions, defensive processing, and intentions to avoid the warning. After viewing the campaign of six static warnings, we assessed intentions to quit smoking, and intentions to use e-cigarettes, hookah, smokeless tobacco, snus, and dissolvable tobacco.
The 319 possible warnings included all available implemented pictorial warnings labels from Australia, Canada, New Zealand and the UK (n=103) and the nine labels proposed by the FDA. Tobacco warning messages from local and national anti-tobacco communication campaigns (n=187), anti-smoking messages produced by tobacco companies (n=15), and 5 testimonial graphic warnings designed for and used in an experimental study by Brennan et al. (2016) were included in the stimuli to facilitate our understanding of the full range of print-form smoking cessation messages, and to insure variance in the stimulus set. Additional details about the inclusion of the warning messages can be found in earlier papers (Sutton et al., 2019). The University of Pennsylvania institutional review board approved the procedures.
Measures
Message effectiveness- perceived effectiveness
The survey assessed perceived effectiveness of each warning with 13 items, including the degree to which the image was convincing, important to them, motivated them to try to quit, made them stop and think, told them something new, made them feel concerned about their smoking, was over all effective, made them feel like staying away from smoking, and was relevant (Bigsby et al., 2013). The 5-point response scale ranged from strongly disagree (coded as 1) to strongly agree (coded as 5). Two items on thoughts about (a) quitting smoking and (b) wanting to continue smoking were rescaled by subtracting the two from each other, dividing by two, and then adding three to fit a five-point scale. A similar procedure was used to rescale items on whether the image was easy to understand or ambiguous. An 11-item scale was created with these items (M=3.39, SD=.38), Cronbach’s α=.94. These specific scales and approach have exhibited predictive validity and reliability in prior work (Kim et al., 2016; Zhao et al., 2011). Further detail on this procedure, the scale, and its validity is available in Bigsby et al. (2013).
Message effectiveness- intention to avoid the warning
The survey measured the extent to which the graphic warning messages resulted in intentions to avoid the warning with items from Borland et al. (2009). After each image, participants were asked if they would perform three possible behaviors if the image appeared on a usual cigarette pack: (1) “cover it up” (2) “keep the pack out of sight” and (3) “transfer the cigarettes to a different container.” Participants rated each item on a 5-point scale ranging from strongly disagree (coded as 1) to strongly agree (coded as 5). Like the analysis perform by Borland et al. (2009) and Gibson et al. (2015), we averaged these together to create an intention to avoid scale, Cronbach’s α=.93 (M= 2.75, SD=1.24).
Alternative measures of message evaluation
Participants rated the warnings on three other measures. Defensive processing (e.g., the image exaggerated negative effects of tobacco cigarettes/was manipulative) measures reactance to the warnings (Brehm, 1966; Hall et al., 2016), which has been shown to weaken the effects of warnings (Hall et al., 2017) and therefore was not included as a measure of message effectiveness. Messages that induce a sense of defensiveness can undermine message persuasion. In our analysis, defensive processing was not highly correlated with perceived effectiveness (r=−.06, p<.05) or avoidance intentions (r=.29, p<.01), but the correlations were significant. We controlled for it in analysis to ensure that the effects of perceived effectiveness and avoidance on intentions to try alternate tobacco products were statistically free of the covariation with defensive processing. While emotional reactions are measures of message effectiveness, emotional engagement (identification with and empathy for characters in the images) and negative emotional reactions (worried, guilty, disgusted, sad, regretful, anxious, uncomfortable, scared, and angry) showed strong collinearity with perceived effectiveness (r= .88, and .89, p>.01), and were hence dropped from further analysis.
Calculating indicators of campaign-level effectiveness
Rationale.
The goal for the current research was to examine whether viewing effective warnings warning messages could unexpectedly increase current smokers’ intention to use alternative tobacco products while reducing smoking cigarettes. This paper used individual ratings of perceived effectiveness and avoidance intentions to derive objective message-level effectiveness (O’Keefe, 2019), which have been shown to be associated with more effective graphic warning messages (Borland et al., 2009; Evans et al., 2015; Gibson et al., 2015). We then used these objective message-level scores for perceived effectiveness and avoidance intentions to determine the effectiveness of the mini-message campaign to which participants were randomly assigned. By averaging responses from everyone who viewed to message to a create a message-level score, the measure can be treated as a feature of the message rather than as a personal rating score. This method avoids confounding the message-level effectiveness with individual dispositions such as stage of change and allows us to make causal claims just as in typical message effects experiments.
Procedure to calculate campaign effectiveness scores: Step 1- message-level.
Because each participant received their own randomly assigned mini-message campaign of six warnings, these unique campaigns varied in their overall effectiveness indicated by perceived effectiveness and intention to avoid the warning. To calculate the average campaign scores for these variables, we first calculated the mean scores for perceived effectiveness, and intention to avoid the warning for each of the 319 warning messages (Figure 1). Each warning was rated by between 14 and 42 participants (mean=26.2).
Figure 1.
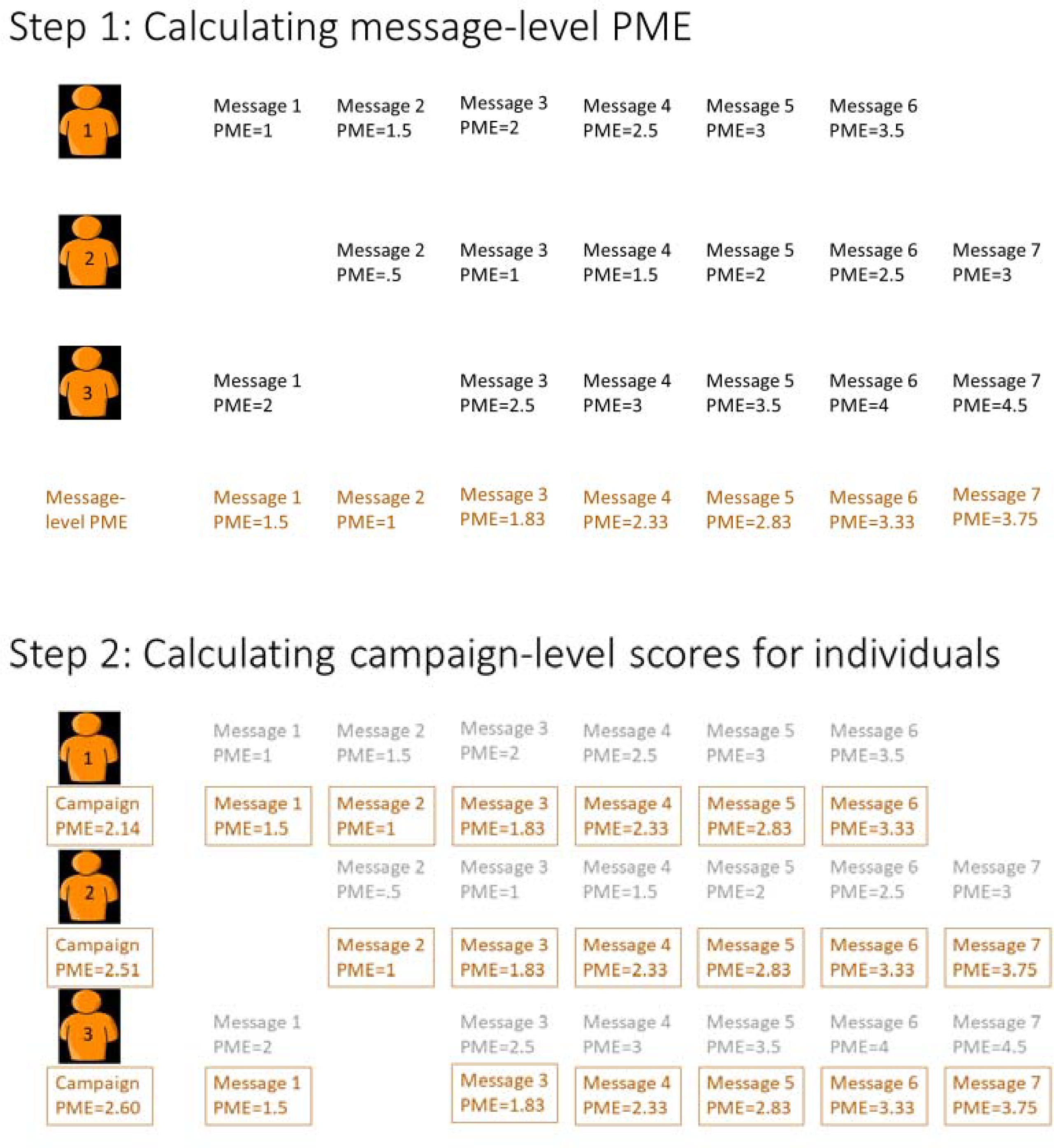
Calculating individual campaign-level scores. The example below uses hypothetical values for three participants’ ratings of perceived message effectiveness (PME) on messages #1 - #7. Step 1 demonstrates how to calculate the message-level PME for each of the messages. Step 2 demonstrates how to the calculate the individual campaign-level scores, or “how much” PME each participant was exposed to with their individual mini-message campaign.
Procedure to calculate campaign effectiveness scores: Step 2- individual campaign-level.
Next, we calculated the average campaign perceived effectiveness and intention to avoid the warning score for each individual mini-message campaign viewed using the message-level scores calculated in step 1; then, we mean centered each score for analysis. For example, someone who viewed a campaign that consisted of graphic warnings #1-#6 which had mean perceived effectiveness scores calculated in step 1 of 1.5, 1, 1.83, 2.33, 2.83, and 3.33 respectively would receive an average individual campaign-level perceived effectiveness score of 2.14 (Figure 1). Across the sample, average campaign-level perceived effectiveness ranged from 2.85 to 3.80, with a mean of 3.38 (SD=.16). Average campaign-level avoidance intentions ranged from 2.37 to 3.19, with a mean of 2.80 (SD=.13). Analyses used an individual’s campaign-level scores, which are not to be confused with the person’s rating of the specific message.
Intention to quit
After viewing the randomly assigned message campaigns, the survey measured intentions to quit smoking with six items about the participants’ quit intentions (Gibson et al., 2015). Participants rated each item on a scale from definitely will not (coded as 1) to definitely will (coded as 4). We averaged these items together to create an intentions to quit scale, Cronbach’s α=.92 (M= 2.50, SD=.83).
Intention to use alternative tobacco products
The survey assessed intentions to use alternative tobacco products with 1 item for each of 5 different tobacco products. Each item provided a short definition of hookah, e-cigarettes, smokeless tobacco, snus, and dissolvable tobacco, and asked if the participant thought they would use the product in the next year. The definitions for hookah specified smoking tobacco in a hookah, and the definition for e-cigarette included that they often contain nicotine. The 4-point response scale ranged from definitely no (coded as 1) to definitely yes (coded as 4).
Statistical analysis
The research questions motivating the analysis were:
Would campaign-level effectiveness affect intentions to use alternate tobacco products?;
Would cigarette quit intentions mediate the relationship between campaign-level effectiveness and interest in alternate tobacco products?
Intention to use alternative tobacco products was dichotomized in order to compare responses of ‘definitely no’ (coded as 0), to other responses (coded as 1). We specified multiple logistic regression models in Stata version 14 to assess the intention to use each of the alternative tobacco products (StataCorp, 2015). Each model includes scores for the level of campaign-level perceived effectiveness and intentions to avoid the warnings for each individual. Each model also controlled for the campaign-level defensive processing and individual-level covariates including contemplation ladder score, Fagerstrom score and sociodemographic characteristics: sex, education, ethnicity, race, and income.
We examined quit intentions as a mediator of the relationship between individual campaign-level perceived effectiveness and intentions to avoid the warnings and intention to use alternative tobacco products using structural equation modeling in MPLUS version 9.3 (Muthén & Muthén, 2015). Because the intention to use alternative tobacco products outcome is binary, we used the WLSMV estimator with theta parameterization (Muthén & Muthén, 2009), and report standardized beta coefficients for ease of interpretation. We used bootstrapped 95% confidence intervals with 1,000 repetitions for mediational analysis, as this approach does not assume that indirect effects are normally distributed (Hayes, 2009).
Results
After viewing the graphic warnings about cigarette smoking, 68% of participants reported some intention to use e-cigarettes while intentions to use hookah, smokeless tobacco, snus and dissolvable tobacco ranged from 31% to 40% (Table 2).
Table 2.
Intentions to use individual alternate tobacco products (n=1,392)
| % (n) | |
|---|---|
| E-cigarettes | 68 (945) |
| Hookah | 40 (551) |
| Smokeless | 31 (437) |
| Snus | 33 (457) |
| Dissolvable | 35 (490) |
In the multiple logistic regression models, viewing mini-message campaigns with higher campaign-level ratings of avoidance intentions were associated with greater odds of intending to use hookah (aOR:4.32 [95% CI 1.28 to 14.55]), smokeless tobacco (aOR:4.88 [95% CI 1.23 to 19.37]), snus (aOR:8.06 [95% CI 2.08 to 31.25]), and dissolvable tobacco (aOR:4.83 [95% CI 1.33 to 17.53]), but not of intending to use e-cigarettes (aOR:3.2 [95% CI .94 to 10.83], Table 3). Individual campaign-level perceived effectiveness did not increase intentions to use alternate tobacco products significantly (Table 3).
Table 3.
Multiple logistic regression adjusted odds ratio of any intention to use different tobacco products, n=1388.
| E-cigs aOR [95% CI] |
Hookah aOR [95% CI] |
Smokeless aOR [95% CI] |
Snus aOR [95% CI] |
Dissolvable aOR [95% CI] |
|
|---|---|---|---|---|---|
| Campaign perceived Effectiveness | 0.82 [0.32 to 2.07] |
0.75 [0.30 to 1.89] |
1.00 [0.35 to 2.85] |
0.82 [0.29 to 2.27] |
1.00 [0.38 to 2.65] |
| Campaign intentions to avoid | 3.2 [.94 to 10.83] |
4.32* [1.28 to 14.55] |
4.88* [1.23 to 19.37] |
8.06* [2.08 to 31.25] |
4.83* [1.33 to 17.53] |
| Campaign defensive processing | 3.37 [0.99 to 11.55] |
2.84 [0.84 to 9.56] |
2.72 [0.69 to 10.73] |
2.03 [0.53 to 7.77] |
3.03 [0.84 to 10.96] |
| Male | 1.71* [1.33 to 2.19] |
2.01* [1.59 to 2.54] |
4.06* [3.13 to 5.28] |
3.77* [2.92 to 4.87] |
3.06* [2.40 to 3.92] |
| College education | 1.52* [1.17 to 1.98] |
2.01* [1.57 to 2.58] |
1.73* [1.30 to 2.29] |
1.88* [1.43 to 2.48] |
1.73* [1.33 to 2.26] |
| Contemplation ladder | 1.03 [0.99 to 1.07] |
0.99 [0.95 to 1.03] |
1.01 [0.96 to 1.05] |
1 [0.96 to 1.05] |
0.99 [0.95 to 1.03] |
| Fagerstrom scale | 1.10* [1.04 to 1.15] |
1.03 [0.98 to 1.08] |
1.13* [1.06 to 1.19] |
1.12* [1.06 to 1.18] |
1.11* [1.05 to 1.17] |
| Hispanic | 1.42 [0.90 to 2.24] |
1.94* [1.29 to 2.91] |
2.66* [1.73 to 4.09] |
2.53* [1.65 to 3.88] |
1.76* [1.16 to 2.66] |
| White | 1.15 [0.82 to 1.62] |
0.84 [0.60 to 1.17] |
0.68* [0.47 to 0.98] |
0.68* [0.48 to 0.97] |
0.74 [0.52 to 1.05] |
| Income $50K or more | 1.13 [0.87 to 1.46] |
1.46* [1.13 to 1.87] |
2.26* [1.71 to 3.00] |
1.94* [1.47 to 2.55] |
1.79* [1.37 to 2.33] |
| Constant | 0.46* [0.23 to 0.92] |
0.15* [0.08 to 0.29] |
0.03* [0.01 to 0.06] |
0.04* [0.02 to 0.08] |
0.08* [0.04 to 0.16] |
| Pseudo R2 | 0.05 | 0.09 | 0.19 | 0.17 | 0.14 |
Note: Outcome was any intention to use the tobacco product. Adjusted models control for all variables in the table. Each warning message received a message-level score for each perceived effectiveness, intentions to avoid the warning, and defensive processing averaged from everyone who viewed the label. Each individual received a campaign-level score for each variable based on the 6 warnings they saw, and those variables were mean centered. aOR= adjusted odds ratio. CI= 95% confidence interval.
p<.05.
Mediational analyses examined whether intentions to quit smoking combustible cigarettes mediated effects of tobacco warnings on interest in trying other tobacco products (Table 4). Viewing mini-message campaigns with higher campaign-level ratings on perceived effectiveness increased quit intentions (βa =.12, p<.001), which was associated with greater intentions to use alternative tobacco products (βb ranged from .15 to .46, all p<.001). The mediated effect of quit intentions was largest for smokeless (βa*βb=.05 [95% CI .02 to .08]), snus (βa*βb=.05 [95% CI .02 to .08]), and dissolvable tobacco (βa*βb=.05 [95% CI .02 to .07]) but was also statistically significant for e-cigarettes and hookah. Without intentions to quit as a mediator, the total effect of campaign-level perceived effectiveness on intentions to use alternative tobacco products (the “c path”) ranged from −.02 to .00 (n.s.). When accounting for the mediating effect of quit intentions, the effect of viewing a campaign with higher perceived effectiveness on intentions to use alternative tobacco products was reduced and remained non-significant, (−.07 to −.04, n.s.).
Table 4.
Quit intentions as a mediator of the association between pictorial warning attribute exposure and intentions to use alternative tobacco products (n=1,390).
| Mediation pathways | |||||||
|---|---|---|---|---|---|---|---|
| a path βa |
b path βb |
Mediated effect βa*βb (95% CI) |
Direct effect Βc’ |
Total effect Βc |
|||
| Perceived effectiveness → | .12** | Quit intentions → | .15** | Intentions to use e-cigs | .02* (.00–.03) | −.04 | −.02 |
| Intentions to avoid → | .11* | .02* ( .00–.03) | .08 | .10* | |||
| Perceived effectiveness → | .12** | Quit intentions → | .26** | Intentions to use hookah | .03* ( .01–.05) | −.05 | −.02 |
| Intentions to avoid → | .11* | .03* (.01–.05) | .09* | .12* | |||
| Perceived effectiveness → | .12** | Quit intentions → | .46** | Intentions to use smokeless | .05** (.02–.08) | −.05 | .00 |
| Intentions to avoid → | .11* | .05* (.02–.08) | .08 | .13* | |||
| Perceived effectiveness → | .12** | Quit intentions → | .44** | Intentions to use snus | .05** (.02–.08) | −.07 | −.01 |
| Intentions to avoid → | .11* | .05* (.02–.07) | .11* | .16** | |||
| Perceived effectiveness → | .12** | Quit intentions → | .40** | Intentions to use dissolvable | .05** (.02–.07) | −.05 | .00 |
| Intentions to avoid → | .11* | .04* (.02–.07) | .08* | .13* | |||
Note. Table reports standardized path coefficients (β’s) for a multiple IV model. The ‘a-path’ represents the path from campaign exposure to the warning’s attribute to quit intentions. The ‘b-path’ represents the path between the quit intentions and intentions to use the alternative tobacco product. The model controls for participant’s individual campaign exposure to defensive processing, and individual scores on the contemplation ladder and Fagerstrom scales.
p<.05
p<.001.
Viewing a campaign with higher campaign-level intention to avoid the warning increased quit intentions (βa =.11, p<.05), which was associated with greater intentions to use alternative tobacco products (βb ranged from .15 to .46, all p<.001). The mediated effect of quit intentions was largest for smokeless (βa*βb=.05 [95% CI .02 to .07] and snus (βa*βb=.05 [95% CI .02 to .08], but was also statistically significant for dissolvable tobacco, e-cigarettes and hookah. The total effect of higher campaign-level avoidance messages on intentions to use alternative tobacco products ranged from .10 to .13 (all p<.05). When accounting for the mediating effect of quit intentions, viewing a campaign with higher campaign-level avoidance on intentions to use alternative tobacco products was reduced but remained significant for hookah (.09, p<.05), snus, (.11, p<.05), and dissolvable (.08, p<.05), indicating partial mediation. The direct effect was reduced and non-significant for e-cigarettes (.08, n.s) and smokeless (.08, n.s), statistically indicating full statistical mediation.
Combustible tobacco (e.g. cigarettes and hookah) poses a higher risk to individual health compared to noncombustible products (e.g. smokeless, snus, and dissolvable) (Fiore et al., 2014; Zeller, 2013; Zeller et al., 2009). To examine whether exposure to tobacco warnings varying in impact was more likely to enhance (hookah) or reduce (smokeless, snus, and dissolvables) risky choices, we employed multilevel mixed effects linear regressions, with respondents as random effects. We used the original 4-point responses for intentions to use alternative tobacco-products. There was a main effect of both product risk and intentions to avoid the label on intentions to use the risker product (hookah). Intentions to use hookah were higher (β=.09 SE=.02, p<.01) compared to intentions to try the less risky products, and exposure to warning messages that elicited avoidance increased intentions to try alternate tobacco products (β=.65 SE=.23, p<.01). However, the interaction between product risk and avoidance was not significant (β=.06 SE=.19, n.s.).
Conclusions
In an environment filled with risky choices, the impact of alerting people to one kind of risk may activate other choices. Understanding the potential unintended consequences of graphic warnings and other educational campaigns with specific foci is an important line of inquiry. In multiple logistic regression analysis, viewing pictorial warning messages that evoke intentions to avoid them were associated with greater intentions to use several alternate tobacco products. While some of these products may be less harmful than combustible cigarettes (Abrams et al., 2018; Foulds et al., 2003), the public health goal of graphic warnings is to encourage tobacco cessation completely in order to improve health. Some previous research has found that people are more likely to switch from alternative tobacco products to smoking cigarettes (Glover et al., 1989), though in Sweden there has been a shift from smoking to using snus (Foulds et al., 2003).
Our work suggests that people may be deterred from smoking cigarettes after viewing effective graphic warnings (as has much other research) (Brewer et al., 2016; Noar, Francis, et al., 2016; Noar, Hall, et al., 2016), but not from tobacco use all together. Quitting smoking improves health outcomes dramatically. However, reductions in the amount of cigarette smoking appear to have few or minor benefits unless the reductions are both substantial (reducing consumption by 50%) and sustained over time (Begh et al., 2015; Pisinger & Godtfredsen, 2007). Therefore, starting or increasing alternate tobacco product use, even if accompanied by some reduction in cigarette smoking, is less likely to lead to improved health outcomes. Dual use of cigarettes and alternate tobacco products may maintain an addiction to nicotine, which hinders tobacco cessation (Schroeder & Hoffman, 2014).
Almost one-third of the participants reported some intention to use hookah, smokeless, snus, or dissolvable tobacco after viewing graphic warnings, and over two-thirds of the participants indicated some intention to use e-cigarettes, which is an increase compared to current use of alternate tobacco products (Kasza et al., 2017). Advertising claims that e-cigarette produce only “harmless water vapor” or contain “no carcinogens” (Grana & Ling, 2014) coupled with positive social interactions from e-cigarette enthusiasts (Pepper et al., 2014) could be encouraging use of e-cigarettes.
Another possible explanation for increased interest in alternate tobacco products is the desire to switch to a less stigmatized product. Smoking cigarettes is a highly stigmatized behavior in the United States (Stuber et al., 2009), and graphic warning labels could be serving as a reminder of the stigma (Riley et al., 2017), especially the warnings that point out the harms to others. This could lead smokers to be interested in a less stigmatized product that still allows them to maintain their nicotine consumption. Indeed one study found that higher perceived stigma was associated with both quit attempts and also alternative tobacco product use (Brown-Johnson & Popova, 2015). As a result of stigma, smokers may turn to alternate tobacco products as a quit aid, rather than seeking help from a medical professional, despite these products not increasing successful quitting rates (Grana et al., 2014).
Consistent with much other research, our study shows that graphic warnings increase quit intentions. However, we also show that increasing quit intentions is in turn associated with greater intentions to use alternative tobacco products. The mediating effects of enhanced quit intentions strengthened our interpretation that the desire to seek alternative tobacco products was partially motivated by the loss of pleasure from smoking combustible cigarettes. The tobacco control community is divided on whether some alternate tobacco products are promising harm reduction strategies (National Academies of Sciences and Medicine, 2018). This study’s findings are particularly important within the US’s current tobacco control landscape where the FDA has authorized two modified risk tobacco products, and is considering others (“Family Smoking Prevention and Tobacco Control Act,” 2009). Graphic warnings are effective, but some of the intermediate outcomes that make them effective (eliciting avoidance) can also increase intentions to use alternative tobacco products. Additionally, our sample was more likely to report intentions to try riskier alternate tobacco products, though viewing more impactful warnings did not exacerbate this effect.
This leads to two important considerations: can campaign designers create effective warnings that do not increase intentions to use alternative tobacco products, and if not, can we encourage people to try the least harmful alternate tobacco products? These may be especially important considerations outside the US since graphic tobacco warnings are currently on cigarette packs in over 100 countries, (Canadian Cancer Society, 2016) and these countries vary in the regulation, acceptance, and availability of alternate tobacco products. Making campaign designers aware of these possible unintended consequences, can prompt them to make campaigns that are more general or that attribute the health or physical outcomes not only to combustible tobacco use, but to tobacco use more generally.
Given the recent release of the new proposed graphic warning labels in the US, it is important to consider the unintended consequences of the new warnings. With the stark increase in rates of youth using e-cigarettes, it is crucial that these warnings do not increase interest in alternate tobacco products. Surveys of youth and young adults show that they perceive some ATPs, especially e-cigarettes, or vaping devices as much less harmful. While the science is still divided on the long-term health effects of e-cigarette consumption, e-cigarettes can harm the adolescent brain (Department of Health and Human Services et al., 2016; Fraga, 2019; Wang et al., 2019). The research using the extended parallel process model suggests that pairing warnings that evoke strong emotions, such as fear, with messages that boost a person’s perceived efficacy to change the behavior can minimize the possible unintended consequences (Cho & Salmon, 2006).
Our findings suggest that intentions to avoid the warnings are a stronger predictor than perceived message effectiveness (PME). There has been a lot of attention in the literature about PME and its value as a predictor of actual message effectiveness (Cappella, 2018; Noar et al., 2018; O’Keefe, 2019). Our findings indicate that avoidance is an alternative self-report measure. Alternative self-report measures of message effectiveness have not been pitted against one another often enough to know what the best predictors of actual effectiveness might be empirically. Avoidance has been studied more in message research in Australian contexts and these data suggest that avoidance style measures need further deeper exploration as measures of message effectiveness both within the tobacco context and in other persuasive domains.
Limitations and future research
This study provides insights into potential unintended consequences of graphic warnings, but there are some limitations worth noting. First, the sample of current smokers was not a representative sample of US adult smokers and differed from the population on factors such as race and ethnicity, though it is somewhat similar to the demographic makeup of current smokers on factors such as education and income level nationally (Jamal, 2016). Additionally, this study was conducted in an online setting. While the results provide information about initial responses to images of tobacco warning messages, responses to these tobacco warnings on actual cigarette packs or campaigns may differ. Furthermore, we did not assess prior use of other tobacco products. About 30% of adult smokers use cigarettes and another tobacco product. Dual use of cigarettes and e-cigarettes is 23% among US adults smokers, for hookah it is 6%, 4% for smokeless. Dual use of snus and dissolvable is less than 1% (Kasza et al., 2017). Due to randomization of participants to message campaigns, dual use status should not be correlated with the predictor variables, though it does makes us unable to tell whether the effects of exposure to the message campaigns would differ by prior dual use status.
Our study shows that exposure to multiple graphic warnings that increase intentions to avoid the warnings could increase intentions to use alternate tobacco products. The best outcome for public health is smoking cessation, not switching to a potentially less harmful substance. However, modified risk tobacco products may play an important role in harm reduction among highly committed smokers (Abrams et al., 2018). It may benefit countries planning to implement these graphic warnings to pair their release with campaigns encouraging cessation and providing information about evidenced-based modified risk tobacco products. Simply ignoring the possible iatrogenic effects of tobacco control campaigns on the uptake of other tobacco-based or tobacco-substitute products is unwise. Companion messaging or broader-based inoculation against alternative products may also be necessary.
Figure 2.
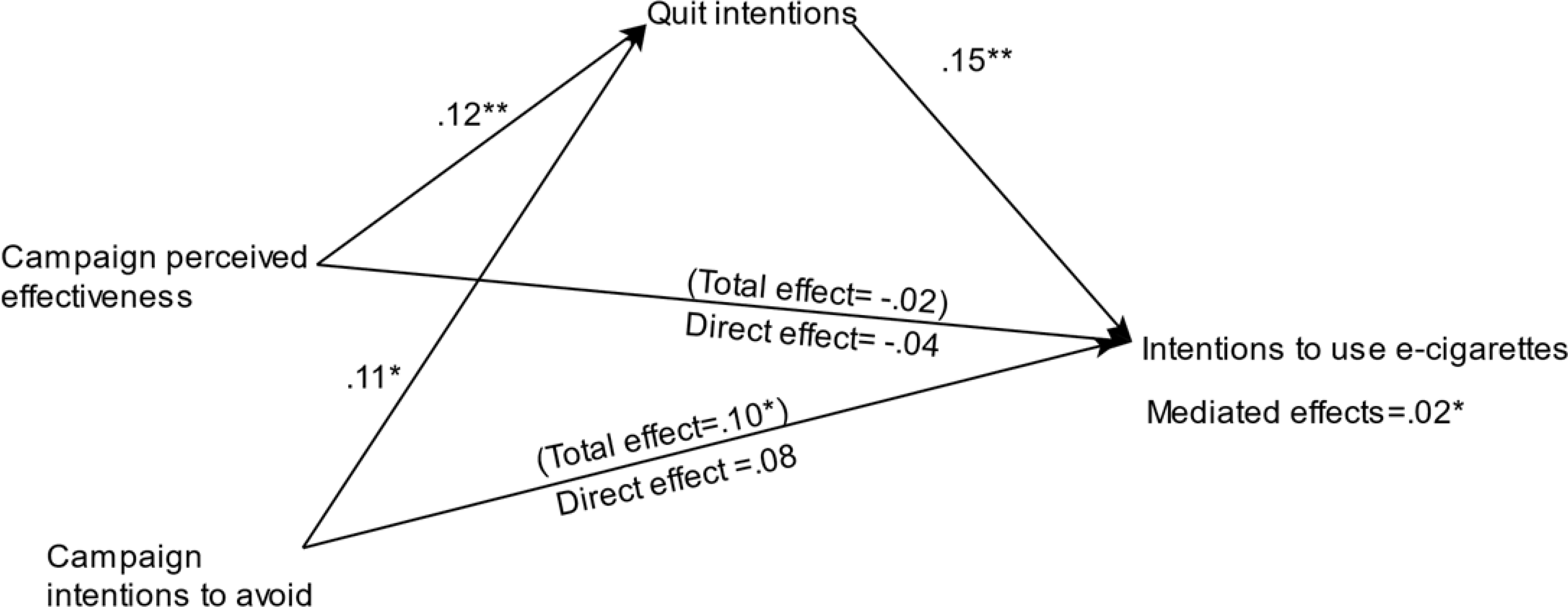
Mediation model for the effects of the campaign’s perceived effectiveness and intentions to avoid the warning message on intentions to use e-cigarettes.
Acknowledgments
The research reported in this publication was supported by grant number P50CA179546 from the National Cancer Institute and FDA Center for Tobacco Products (CTP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
The authors declare no conflicts of interest.
References
- Abrams DB, Glasser AM, Pearson JL, Villanti AC, Collins LK, & Niaura RS (2018). Harm Minimization and Tobacco Control: Reframing Societal Views of Nicotine Use to Rapidly Save Lives. Annual Review of Public Health, 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begh R, Lindson-Hawley N, & Aveyard P (2015). Does reduced smoking if you can’t stop make any difference? BMC Medicine, 13(1), 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, & Abrams DB (1991). The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology, 10(5), 360. [DOI] [PubMed] [Google Scholar]
- Bigsby E, Cappella JN, & Seitz HH (2013). Efficiently and Effectively Evaluating Public Service Announcements: Additional Evidence for the Utility of Perceived Effectiveness. Communication Monographs, 80(1), 1–23. 10.1080/03637751.2012.739706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Yong H-H, Wilson N, Fong GT, Hammond D, Cummings KM, Hosking W, & McNeill A (2009). How reactions to cigarette packet health warnings influence quitting: Findings from the ITC Four-Country survey. Addiction, 104(4), 669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehm JW (1966). A theory of psychological reactance. Academic Press. [Google Scholar]
- Brennan E, Maloney EK, Ophir Y, & Cappella JN (2016). Potential effectiveness of pictorial warning labels that feature the images and personal details of real people. Nicotine & Tobacco Research, 19(10), 1138–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Hall MG, Noar SM, Parada H, Stein-Seroussi A, Bach LE, Hanley S, & Ribisl KM (2016). Effect of Pictorial Cigarette Pack Warnings on Changes in Smoking Behavior. JAMA Internal Medicine, 176(7), 905. 10.1001/jamainternmed.2016.2621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer NT, Parada H, Hall MG, Boynton MH, Noar SM, & Ribisl KM (2018). Understanding Why Pictorial Cigarette Pack Warnings Increase Quit Attempts. Annals of Behavioral Medicine. 10.1093/abm/kay032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown-Johnson CG, & Popova L (2015). Exploring Smoking Stigma, Alternative Tobacco Product Use, and Quit Attempts. Health Behavior and Policy Review, 3(1), 13–20. 10.14485/hbpr.3.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne S, & Niederdeppe J (2012). Unintended Consequences of Obesity Prevention Messages. In The Oxford Handbook of the Social Science of Obesity. Oxford University Press. 10.1093/oxfordhb/9780199736362.013.0043 [DOI] [Google Scholar]
- Canadian Cancer Society. (2016). Cigarette Package Health Warnings: International Status Report. [Google Scholar]
- Cappella JN (2018). Perceived Message Effectiveness Meets the Requirements of a Reliable, Valid, and Efficient Measure of Persuasiveness. Journal of Communication, 68(5), 994–997. 10.1093/joc/jqy044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H, & Salmon CT (2006). Fear appeals for individuals in different stages of change: Intended and unintended effects and implications on public health campaigns. Health Communication, 20(1), 91–99. 10.1207/s15327027hc2001_9 [DOI] [PubMed] [Google Scholar]
- Cho H, & Salmon CT (2007). Unintended Effects of Health Communication Campaigns. Journal of Communication, 57(2), 293–317. 10.1111/j.1460-2466.2007.00344.x [DOI] [Google Scholar]
- Davis KC, Patel D, Shafer P, Duke J, Glover-Kudon R, Ridgeway W, & Cox S (2018). Association Between Media Doses of the Tips From Former Smokers Campaign and Cessation Behaviors and Intentions to Quit Among Cigarette Smokers, 2012–2015. Health Education & Behavior : The Official Publication of the Society for Public Health Education, 45(1), 52–60. 10.1177/1090198117709316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention, & CDC’s Office on Smoking and Health. (2016). E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. [PubMed] [Google Scholar]
- Duke JC, Alexander TN, Zhao X, Delahanty JC, Allen JA, MacMonegle AJ, & Farrelly MC (2015). Youth’s awareness of and reactions to the real cost national tobacco public education campaign. PLoS ONE, 10(12). 10.1371/journal.pone.0144827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans AT, Peters E, Strasser AA, Emery LF, Sheerin KM, & Romer D (2015). Graphic warning labels elicit affective and thoughtful responses from smokers: Results of a randomized clinical trial. PLoS ONE. 10.1371/journal.pone.0142879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Family Smoking Prevention and Tobacco Control Act. (2009). Public Law, 111(22). [Google Scholar]
- Farrelly MC, Duke JC, Nonnemaker J, MacMonegle AJ, Alexander TN, Zhao X, Delahanty JC, Rao P, & Allen JA (2017). Association between the real cost media campaign and smoking initiation among youths—United States, 2014–2016. In Morbidity and Mortality Weekly Report (Vol. 66, Issue 2, pp. 47–50). Department of Health and Human Services. 10.15585/mmwr.mm6602a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Schroeder SA, & Baker TB (2014). Smoke, the Chief Killer—Strategies for Targeting Combustible Tobacco Use. New England Journal of Medicine, 370(4), 297–299. 10.1056/NEJMp1314942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Drug Administration. (2012). Modified Risk Tobacco Product Applications. Center for Tobacco Products. [Google Scholar]
- Foulds J, Ramstrom L, Burke M, & Fagerström K (2003). Effect of smokeless tobacco (snus) on smoking and public health in Sweden. Tobacco Control, 12(4), 349–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraga J-A (2019). The Dangers of Juuling | National Center for Health Research. In National Center for Health Research. [Google Scholar]
- Getachew B, Payne JB, Vu M, Pillai D, Shah J, Levine H, & Berg CJ (2018). Perceptions of alternative tobacco products, anti-tobacco media, and tobacco regulation among young adults: A qualitative study. American Journal of Health Behavior, 42(4), 118–130. 10.5993/AJHB.42.4.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson L, Brennan E, Momjian A, Shapiro-Luft D, Seitz HH, & Cappella JN (2015). Assessing the consequences of implementing graphic warning labels on cigarette packs for tobacco-related health disparities. Nicotine & Tobacco Research, 17(8), 898–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glantz SA (1996). Preventing Tobacco Use-The Youth Access Trap. 86(2), 156–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover ED, Laflin M, & Edwards SW (1989). Age of initiation and switching patterns between smokeless tobacco and cigarettes among college students in the United States. American Journal of Public Health, 79(2), 207–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana RA, Benowitz N, & Glantz SA (2014). E-cigarettes: A scientific review. Circulation, 129(19), 1972–1986. 10.1161/CIRCULATIONAHA.114.007667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana RA, & Ling PM (2014). “Smoking revolution”: A content analysis of electronic cigarette retail websites. American Journal of Preventive Medicine, 46(4), 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttman N, & Zimmerman DR (2000). Low-income mothers’ views on breastfeeding. Social Science and Medicine, 50(10), 1457–1473. 10.1016/S0277-9536(99)00387-1 [DOI] [PubMed] [Google Scholar]
- Hall MG, Sheeran P, Noar SM, Boynton MH, Ribisl KM, Parada H, Johnson TO, & Brewer NT (2017). Negative affect, message reactance and perceived risk: How do pictorial cigarette pack warnings change quit intentions? Tobacco Control, tobaccocontrol-2017–053972. 10.1136/tobaccocontrol-2017-053972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MG, Sheeran P, Noar SM, Ribisl KM, Bach LE, & Brewer NT (2016). Reactance to Health Warnings Scale: Development and Validation. Annals of Behavioral Medicine, 50(5), 736–750. 10.1007/s12160-016-9799-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D (2011). Health warning messages on tobacco products: A review. Tobacco Control, 20(5), 327–337. 10.1136/tc.2010.037630 [DOI] [PubMed] [Google Scholar]
- Hammond D, & White CM (2012). Improper disclosure: Tobacco packaging and emission labelling regulations. Public Health, 126(7), 613–619. 10.1016/j.puhe.2012.03.012 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Communication Monographs, 76(4), 408–420. 10.1080/03637750903310360 [DOI] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, & Fagerström K (1991). The Fagerström test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. Addiction, 86(9), 1119–1127. [DOI] [PubMed] [Google Scholar]
- Higgins ET (1998). Promotion and Prevention: Regulatory Focus as A Motivational Principle (M. P. B. T.-A. in Zanna ESP, Ed.; Vol. 30, pp. 1–46). Academic Press. 10.1016/S0065-2601(08)60381-0 [DOI] [Google Scholar]
- Re: Reynolds v. RJ Food & Drug Administration, No. 11–5332 (D.C. Cir. 2013), (2013).
- Hornik RC, Jacobsohn L, Orwin R, Piesse A, & Kalton G (2008). Effects of the National Youth Anti-Drug Media Campaign on Youths. American Journal of Public Health, 98(12), 2229–2236. 10.2105/AJPH.2007.125849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A (2016). Current cigarette smoking among adults—United States, 2005–2015. MMWR. Morbidity and Mortality Weekly Report, 65. [DOI] [PubMed] [Google Scholar]
- Karelitz JL, & Perkins KA (2018). Tobacco smoking may delay habituation of reinforcer effectiveness in humans. Psychopharmacology, 235(8), 2315–2321. 10.1007/s00213-018-4927-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasza KA, Ambrose BK, Conway KP, Borek N, Taylor K, Goniewicz ML, Cummings KM, Sharma E, Pearson JL, Green VR, Kaufman AR, Bansal-Travers M, Travers MJ, Kwan J, Tworek C, Cheng Y-C, Yang L, Pharris-Ciurej N, van Bemmel DM, … Hyland AJ (2017). Tobacco-Product Use by Adults and Youths in the United States in 2013 and 2014. New England Journal of Medicine, 376(4), 342–353. 10.1056/NEJMsa1607538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M, Shi R, & Cappella JN (2016). Effect of character–audience similarity on the perceived effectiveness of antismoking PSAs via engagement. Health Communication, 31(10), 1193–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinot MC, & Rogers RW (1982). Identifying effective components of alcohol misuse prevention programs. Journal of Studies on Alcohol, 43(7), 802–811. [DOI] [PubMed] [Google Scholar]
- Kong G, Simon P, Mayer ME, Barrington-Trimis JL, Pacek LR, Cooper M, Guy MC, & Stanton CA (2019). Harm Perceptions of Alternative Tobacco Products among US Adolescents. Tobacco Regulatory Science, 5(3), 242–252. 10.18001/trs.5.3.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman C, Rimer B, Trock B, Balshem A, & Engstrom PF (1990). Factors associated with repeat adherence to breast cancer screening. Preventive Medicine, 19(3), 279–290. 10.1016/0091-7435(90)90028-i [DOI] [PubMed] [Google Scholar]
- Majeed BA, Sterling KL, Weaver SR, Pechacek TF, & Eriksen MP (2017). Prevalence and harm perceptions of hookah smoking among U.S. adults, 2014–2015. Addictive Behaviors, 69, 78–86. 10.1016/j.addbeh.2017.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy-Hoefer R, Davis KC, Beistle D, King BA, Duke J, Rodes R, & Graffunder C (2018). Impact of the Tips From Former Smokers Campaign on Population-Level Smoking Cessation, 2012–2015. Preventing Chronic Disease, 15, E71. 10.5888/pcd15.180051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2009). Statistical Analysis with Latent Variables. Wiley. [Google Scholar]
- Muthén LK, & Muthén BO (2015). Mplus. Seventh edition. In Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Academies of Sciences and Medicine, E. (2018). Public health consequences of e-cigarettes. Washington, DC: The National Academies Press. Doi, 10, 24952. [PubMed] [Google Scholar]
- Noar SM, Barker J, & Yzer M (2018). Measurement and Design Heterogeneity in Perceived Message Effectiveness Studies: A Call for Research. Journal of Communication, 68(5), 990–993. 10.1093/joc/jqy047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, & Brewer NT (2016). The impact of strengthening cigarette pack warnings: Systematic review of longitudinal observational studies. In Social Science & Medicine (Vol. 164, pp. 118–129). 10.1016/j.socscimed.2016.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, & Brewer NT (2016). Pictorial cigarette pack warnings: A meta-analysis of experimental studies. In Tobacco Control (Vol. 25, Issue 3, pp. 341–354). 10.1136/tobaccocontrol-2014-051978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Keefe DJ (2019). Message Pretesting Using Perceived Persuasiveness Measures: Reconsidering the Correlational Evidence. Communication Methods and Measures. 10.1080/19312458.2019.1620711 [DOI] [Google Scholar]
- Pepper JK, Emery SL, Ribisl KM, & Brewer NT (2014). How US adults find out about electronic cigarettes: Implications for public health messages. Nicotine & Tobacco Research, 16(8), 1140–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, & Boldry MC (2017). Nicotine acutely enhances reinforcement from non-drug rewards in humans. In Frontiers in Psychiatry (Vol. 8, Issue MAY). Frontiers Media S.A. 10.3389/fpsyt.2017.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisinger C, & Godtfredsen NS (2007). Is there a health benefit of reduced tobacco consumption? A systematic review. Nicotine & Tobacco Research, 9(6), 631–646. [DOI] [PubMed] [Google Scholar]
- Riley KE, Ulrich MR, Hamann HA, & Ostroff JS (2017). Decreasing Smoking but Increasing Stigma? Anti-tobacco Campaigns, Public Health, and Cancer Care. AMA Journal of Ethics, 19(5), 475–485. 10.1001/journalofethics.2017.19.5.msoc1-1705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RW, & Mewborn CR (1976). Fear appeals and attitude change: Effects of a threat’s noxiousness, probability of occurrence, and the efficacy of coping responses. Journal of Personality and Social Psychology, 34(1), 54. [DOI] [PubMed] [Google Scholar]
- Schroeder MJ, & Hoffman AC (2014). Electronic cigarettes and nicotine clinical pharmacology. Tobacco Control, 23(suppl 2), ii30–ii35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade J (1997). Cover essay: The pack as advertisement. Tobacco Control, 6(3), 169–170. 10.1136/tc.6.3.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14. StataCorp LP. [Google Scholar]
- Stuber J, Galea S, & Link BG (2009). Stigma and Smoking: The Consequences of Our Good Intentions. Social Service Review, 83(4), 585–609. 10.1086/650349 [DOI] [Google Scholar]
- Sutton JA, Yang S, & Cappella JN (2019). Perceived effectiveness of objective features of pictorial warning messages. Tobacco Control, 28(e1), e24–e30. 10.1136/tobaccocontrol-2018-054488 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2020). Smoking Cessation: A Report of the Surgeon General. [Google Scholar]
- Wakefield MA, Morley C, Horan JK, & Cummings KM (2002). The cigarette pack as image: New evidence from tobacco industry documents. Tobacco Control, 11(Supplement 1), i73–i80. 10.1136/tc.11.suppl_1.i73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TW, Gentzke AS, Creamer MR, Cullen KA, Holder-Hayes E, Sawdey MD, Anic GM, Portnoy DB, Hu S, Homa DM, Jamal A, & Neff LJ (2019). Tobacco Product Use and Associated Factors Among Middle and High School Students—United States, 2019. MMWR. Surveillance Summaries, 68(12), 1–22. 10.15585/mmwr.ss6812a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2003). WHO framework convention on tobacco control. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. (2019). WHO Report on the Global Tobacco Epidemic, 2019. 10.5455/aces.2012022 [DOI] [Google Scholar]
- Zeller M (2013). Reflections on the “endgame” for tobacco control. Tobacco Control, 22 Suppl 1(suppl 1), i40–1. 10.1136/tobaccocontrol-2012-050789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller M, Hatsukami D, & Strategic Dialogue on Tobacco Harm Reduction Group. (2009). The Strategic Dialogue on Tobacco Harm Reduction: A vision and blueprint for action in the US. Tobacco Control, 18(4), 324–332. 10.1136/tc.2008.027318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Strasser AA, Cappella JN, Lerman C, & Fishbein M (2011). A measure of perceived argument strength: Reliability and validity. Communication Methods and Measures, 5(1), 48–75. [DOI] [PMC free article] [PubMed] [Google Scholar]


