Abstract
Rationale.
There is a robust link between patients’ expectations and clinical outcomes, as evidenced by the placebo effect. Expectations depend in large part on the context surrounding treatment, including the patient-provider interaction. Prior work indicates that providers’ behavior and characteristics, including warmth and competence, can shape patient outcomes. Yet humans rapidly form trait impressions of others before any in-person interaction. It is unknown whether these first impressions influence subsequent health care choices and expectations.
Objective.
Our goal was to test whether trait impressions of hypothetical medical providers, based exclusively on facial images, influence the choice of medical providers and expectations about pain and analgesia following hypothetical painful medical procedures.
Method.
Across five online experiments, participants (total N=1108) viewed and made judgments about hypothetical healthcare providers. Experiments 1–4 included computer-generated faces that varied in features associated with competence, while experiment 5 included real faces. We measured how apparent competence affected expectations about pain and anticipated analgesic use in all studies. We also measured warmth and similarity.
Results.
Across five online studies, participants selected providers who appeared more competent, based on facial visual information alone. Further, providers’ apparent competence predicted participants’ expectations about post-procedural pain and medication use. Participants’ perception of their similarity to providers also shaped expectations about pain and treatment outcomes.
Conclusions.
Results from our experimental simulations suggest that humans develop expectations about pain and health outcomes before even setting foot in the clinic, based exclusively on first impressions. These findings have strong implications for health care, as individuals increasingly rely on digital services to select healthcare providers and even receive treatment, a trend that is exacerbated as the world embraces telemedicine.
Keywords: Pain, Placebo, Expectations, patient-provider, Trait Impressions, Implicit Evaluation, social cognition
INTRODUCTION
People increasingly use the web to select and interact with healthcare professionals, a trend intensifying during the COVID-19 pandemic (Anthony Jnr, 2020; Claire Elson et al., 2020). Hospitals feature physicians’ headshots prominently on websites, and web-based services allow patients to peruse potential providers and make appointments based on limited information, including a provider’s photo. Images that patients see online may be their first exposure to their healthcare provider and have the potential to shape physician selection and/or bias expectations for care prior to any clinical interaction. Do patients’ trait impressions of healthcare professionals that emerge from these images shape patients’ healthcare choices and expectations about pain and treatment?
Medical providers’ behaviors play a central role in shaping patients’ healthcare expectations (Chen et al., 2019; Daniali and Flaten, 2019; He et al., 2017; Osch et al., 2017), which, in turn, profoundly influence the way that we experience pain (Atlas and Wager, 2012). This is most striking in placebo analgesia, in which the context surrounding treatment (as well as prior experience) influences patient expectations, which in turn reduce pain (Evers et al., 2018; Wager and Atlas, 2015). Placebo effects and responses to active treatments are maximized by supportive patient-provider relationships (Czerniak et al., 2016; Fuentes et al., 2014; Kaptchuk et al., 2008). Placebo effects and responses to clinical outcomes including pain are particularly sensitive to provider competence and warmth (Ashton-James et al., 2019; Howe et al., 2019, 2017), so-called ‘universal dimensions of social cognition’ (Fiske et al., 2006) that explain over three-quarters of the variance in how we characterize others (Fiske et al., 2006; Wojciszke et al., 1998).
Though extant literature focuses on interacting with a physician and on physician’s behaviors, humans form impressions of others within 50 ms before any social interaction based on visual appearance alone (Necka et al., 2016; Todorov, 2005). These impressions shape real-world outcomes (Necka et al., 2016; Todorov, 2005; Wilson and Rule, 2015), our expectations about how people will behave towards us (FeldmanHall et al., 2017), and behavior (Necka et al., 2019, 2018; Over and Cook, 2018), despite weak relationships, if any, between trait impressions and reality (Graham et al., 2017; Christopher Y. Olivola and Todorov, 2010; Stoker et al., 2016; Tedeschi et al., 2015; Wyatt and Silvester, 2018) (c.f. (Little and Perrett, 2007; Slepian and Ames, 2016)). Impressions of competence are particularly important, as individuals who appear more competent based on facial features are more likely to be elected (Todorov, 2005) and receive higher compensation (Graham et al., 2017).
Consistent with these findings, recent work indicates that pain perception is influenced by patients’ perceptions of their providers’ competence, based on the patient-provider interaction, as well as the providers’ appearance of familiarity, as rated by people other than the patient (Ashton-James et al., 2019; Mattarozzi et al., 2020). However, it is unknown whether patients’ own initial impressions influence expectations, as no studies have measured effects of first impressions on subsequent health care choices and expectations. However, it is likely that first impressions do influence health care choices: Qualitative research indicates that consumers spend an average of just over 6 minutes on a physician rating website when selecting a pediatrician, whereas they spend over 9 minutes on average when selecting a hotel from the website TripAdvisor (Rothenfluh et al., 2016). We asked whether trait impressions of potential medical providers based on facial features alone influence selection of health care providers and expectations about pain and analgesic use in clinical simulations.
Across five experiments, participants (total N=1108) viewed and made judgments about hypothetical healthcare providers (Figure 1). We focused on competence in all experiments, as competence is particularly important when someone’s behavior directly influences your pain (Ashton-James et al., 2019; Tedeschi et al., 2015). We hypothesized people would prefer to have hypothetical painful medical procedures conducted by more competent-looking healthcare providers and that provider competence would be positively associated with expectations for less pain and less invasive post-procedural analgesic treatment. We used real and computer-generated faces that were manipulated to correspond to perceived competence in previous studies (Oh et al., 2019; Todorov et al., 2013) (e.g., competent looking faces had angular jaws, higher cheekbones, eyes close to brows (Christopher Y Olivola and Todorov, 2010)), and real faces that were not manipulated (Ma et al., 2015). We also measured warmth and similarity in follow up experiments (see Table 1). People endorse greater intent to adhere to treatment (Street et al., 2008) and experience less pain when they feel the person administering to them is similar to them (Losin et al., 2017), although effects may vary across racial and ethnic groups (Anderson et al., 2020). We hypothesized that individuals would therefore prefer providers they perceived to be more similar to them and that similarity would be associated with expectations for less pain and less invasive treatment. Finally, we explored the role of physician and participant demographic characteristics (sex, race), and assessed via questionnaires general attitudes toward medical providers and past experiences with healthcare.
Fig. 1. Study Tasks.

A) Provider Preference Task. Participants selected which of two providers they would prefer to conduct a painful medical procedure. B) Painful Procedure Expectation Task. Participants imagined that the provider was performing a painful medical procedure on them, and were asked to rate their expectations about various post-procedural outcomes (see C for specific items. C) Differences in study designs. Stimuli varied by study (see Fig. 2), as did the items in the Expectations Task and in the Trait Rating Task (when present; Studies 4–5). All studies included the Provider Preference Task prior to the Painful Procedure Expectations Task, and some also included questionnaires at the end of all of the tasks. Note that in Study 2, half of participants completed a question about expectations for medication use, and half of participants completed a question about their perceptions of the provider’s similarity. For full methods, including descriptions of the item wording and scale anchors, see Supplementary Materials.
Table 1.
Effect of competent appearance on participants’ preference for medical providers.
| Provider Preference | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Difference in Apparent Competence Between Faces | Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||
| Sex | Race | Sex | Race | |||||||||||||||||
| Percent | t | df | p | B | SE | Z | p | t | df | p | t | df | p | t | df | p | t | df | p | |
| Study 1 | 61.63% | 3.39 | 49 | .001 | .05 | .03 | 1.93 | .054 | - | - | - | - | - | - | - | - | - | - | ||
| Study 2 | 68.30% | 12.07 | 136 | 2.97E-23 | .11 | .02 | 6.32 | 2.62E-10 | .11 | 135 | .906 | −1.45 | 41 | .156 | - | - | - | - | - | - |
| Study 3M | 50.91% | .84 | 149 | .402 | .04 | .07 | .61 | .545 | .91 | 93 | .366 | .71 | 21 | .485 | - | - | - | - | - | - |
| Study 3A | 49.39% | −.80 | 288 | .426 | .05 | .07 | .70 | .482 | - | - | - | - | - | - | −2.09 | 287 | .038 | - | - | - |
| Study 4 | 56.39% | 4.69 | 281 | 4.18E-06 | −.32 | .14 | −2.25 | .024 | −.15 | 277 | .883 | 1.94 | 71 | .056 | −2.12 | 261 | .035 | - | - | - |
| Study 5 | 62.20% | 15.56 | 259 | 5.26E-39 | .34 | .03 | 10.89 | 1.23E-27 | .91 | 199 | .362 | 2.03 | 85 | .046 | −1.41 | 243 | .160 | 2.24 | 122 | .027 |
Note. Study 3 analyses were initially conducted on the sample of participants who saw male providers only (Study 3M), to test replication of Studies 1 and 2, and then were conducted on the full sample with moderation by stimulus sex (Study 3A). Moderation by provider sex was evaluated in Studies 3A, 4, and 5, and moderation by provider race was evaluated in Study 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
GENERAL METHODS
Participants
Five studies were conducted in independent samples online through Amazon’s Mechanical Turk (“MTurk”) between November 2018 and October 2019 (see Supplementary Methods for dates for each study). The protocol was approved by the National Institute of Health’s Office of Human Subjects Resesarch Protection (protocol 18-NCCIH-0622), and was determined to be exempt from IRB review based on the Common Rule, as no identifiers were collected and the study only involved surveys and benign behavioral measures. For each study, participants were recruited through TurkPrime (Robinson et al., 2016), a service that interfaces with MTurk, for a study about the choices people make about their healthcare providers and how they feel about medical procedures. To be eligible, participants had to have at least a 90% approval rate on MTurk, have completed at least 100 Mturk HITS, and be in the United States. ‘Suspicious geolocations’ identified by TurkPrime were blocked to mitigate the likelihood of bot responders (Robinson, n.d.). Across five studies, 1108 participants (aged 18–99, 58.9% male, 76.7% White) completed the tasks (see Supplementary Table 1.0 for study-specific demographics). Sample sizes for Studies 2–5 were determined a priori using effect sizes estimated from preceding studies (see Supplementary Materials for more information).
Procedures
Each study consisted of the Provider Preference Task, the Painful Procedure Expectation Task, and questionnaires (Figure 1). In the Provider Preference Task (henceforth, the ‘Preference Task’), participants saw two healthcare providers and chose the provider they preferred. Participants had seven seconds to indicate their preference of provider by pressing the left or right arrow on their keyboard (corresponding to the two stimuli; Figure 1A).
In the Painful Procedure Expectation Task (henceforth, the ‘Expectation Task’), participants saw a face from the Preference Task and rated how painful they expected a painful procedure conducted by that provider to be (“Not at all painful” to “Extremely painful”), where higher scores indicated greater pain (Figure 1B). Participants also reported other expectations about the hypothetical procedure, including how long they expected pain following the procedure (Study 1), their likelihood of using over-the-counter or prescription strength pain medication following the procedure (assuming the doctor recommended both; Studies 2–5), and how similar the provider was to them (Studies 2–4). Finally, participants completed a Trait Rating Task in which they rated the faces on various trait qualities (Studies 4–5) and completed questionnaires that measured their attitudes towards various types of medications and towards healthcare providers and the frequency of their previous healthcare visits (Studies 3–5), reported in the Supplementary Materials, as well as loneliness (Studies 3–5), objective social isolation (Studies 3–5), and depression (Studies 4–5), to be reported elsewhere. Studies were created using Psytoolkit (Stoet, 2010) (Studies 1–4) and Psychopy (Peirce et al., 2019) hosted by Pavlovia (Study 5). For study specific procedures, see Figure 1C and Supplementary Materials.
Each choice or rating was required to be recorded within seven seconds. The time limit was incorporated to ensure participants were actively engaged in the task (i.e., had not left their computer) and duration was determined based on piloting. If a participant did not record a response within 7s, the trial was considered as a non-response and omitted from analyses. The average number of missing trials was less than 2 for all studies and tasks (see Supplementary Methods). Participants who made no responses during the Preference Task were excluded from analyses (see Supplement; n ranged from 0 [Study 1] to 36 [Study 4]).
Stimuli
Face stimuli varied across studies, beginning with the most internally but least ecologically valid stimuli and finishing with the most ecologically valid but least experimentally controlled stimuli. More specifically, Studies 1 and 2 used computer-generated male White faces (‘CG faces’) from a previously published and validated stimulus set that were manipulated to vary in competence (Todorov et al., 2013) (Figure 2A). Studies 1 and 2 each included 25 unique facial identities at 7 competence levels each (ranging from −3 SD to +3 SD in competence based on normed ratings (Todorov et al., 2013), for a total of 175 unique stimuli. Studies 3 and 4 used real White faces that were manipulated to vary in competence (‘Manipulated faces’; Figure 2B) from a previously published and validated stimulus set (Oh et al., 2019). For both studies, there were 79 unique facial identities presented at 4 competence levels each (for a total of 175 unique stimuli) and each participant completed 10 trials during the Preference task. Whereas Study 3 presented stimuli from the original stimulus set, Study 4 included modified images that were masked (‘Masked manipulated faces’, Figure 2C) to remove all distinguishing non-facial features (i.e., only the face alone was presented). Both male and female stimuli were used, but all participants saw stimuli of only one sex during the Preference and Expectation tasks. Finally, Study 5 used unaltered neutral faces (‘Natural faces’; Figure 2D) from the Chicago Face Database (Ma et al., 2015). Images consisted of 585 individuals aged 18–40 who self-identified as either Caucasian, Black/African American, Latinx, or East Indian/Asian and as either male or female (Table S5.42). Participants saw hypothetical providers from only one demographic category and, as in Studies 3–4, saw all hypothetical providers of one sex only. There were 25 Preference task trials per participant, drawn from the 585 unique stimuli. Detailed information on stimuli can be found in the Supplementary Materials.
Fig. 2. Medical Provider Stimuli.

A) Computer Generated Faces (Todorov et al., 2013) that varied in competence were used in Studies 1 and 2. All stimuli were generated from male faces. B) Manipulated Faces (Oh et al., 2019) that were made by morphing real faces with computer models of low and high competence at varying levels (−25% and −8.33% morphs with the low competence face; 8.33% and 25% morphs with the high competence faces). These stimuli were used in Study 3. Participants viewed either male or female faces. C) Masked Manipulated Faces were created by stripping manipulated faces (from Study 3) of any distinguishing non-facial features, and were used in Study 4. Participants viewed either male or female faces. D) Naturalistic Faces (Ma et al., 2015) were used in Study 5. Participants saw stimuli from a single race-sex category.
Data Analysis
All analyses were conducted in R v3.61. Mixed-effects models were conducted using the lme4 (Bates et al., 2015) and the lmerTest (Kuznetsova et al., 2015) packages. All within-subjects fixed effects were group-mean centered (i.e., centered within participants), as recommended in (Aguinis et al., 2013; Brauer and Curtin, 2017; Enders and Tofighi, 2007; Nezlek, 2012), to accurately estimate the within-subject effect and ensure unbiased estimation of cross-level interactions (e.g., moderation by participant sex/race). Trials on which individuals failed to respond were included as non-numbers and omitted from analyses, rather than imputing values, which can introduce noise to multilevel linear models (Twisk et al., 2013). Group means were included as covariates in analyses when predictor variables were participants’ ratings (e.g., perceptions of similarity), rather than manipulated factors (e.g., competence level of morphed faces). For tests of moderation by participant race, we recoded data to reflect ‘white’ versus ‘people of color’ to account for small samples within specific racial/ethnic cells (full breakdown of participant demographics in Supplementary Table 1.0).
In mixed-effects models, all fixed effects were also modeled as random slopes within-subjects and stimulus identity; if a model failed to converge, random slopes and correlations between random slopes and intercepts that explained the least variance were removed (as recommended in (Barr et al., 2013)) until the model converged. Only fixed effects are reported in the main text, but full model results are included in the Supplementary Materials.
Following convergence of all models, we standardized models using the effectsize package and conducted a random effects meta-analysis using the meta package (Balduzzi et al., 2019). The meta-analysis was conducted with the Sidik-Jonkman estimator of between-study variance using the Hartung-Knapp correction, which has been found to preserve the nominal type I error rate more accurately (Inthout et al., 2014), or even potentially more conservatively (Röver et al., 2015), especially when the number of studies in the meta-analysis is low (Guolo and Varin, 2017). Given the acceptability of standardized regression coefficients as effect size estimates in meta-analysis (Becker and Wu, 2007; Borenstein et al., 2011; Rosenthal and Dimatteo, 2001), we used standardized betas as our effect size estimates, except for our meta-analysis of the Preference Task. For full details on statistical models and analytical steps, including full model results, see Supplementary Materials.
RESULTS
Study 1
Our first experiment included computer generated (CG) faces morphed with respect to competence, based on previous work (Todorov et al., 2013) (Figure 2A). Participants (N=50) were more likely to choose the more competent looking provider, t(49)=3.39, p=.001, choosing the more competent looking face on 61.63% of trials (Table 1). Participants also expected less pain with more competent-looking providers, B=−.12, t=−2.77, p=.008 (Table 2).
Table 2.
Effect of competent appearance on participants’ expectations for post-procedural pain.
| Expected Pain | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 1 | −.12 | .04 | −2.77 | 47 | .008 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Study 2 | −.16 | .03 | −5.78 | 102 | 8.06E-08 | .03 | .05 | .55 | 135 | .583 | −.09 | .06 | −1.65 | 135 | .102 | - | - | - | - | - | - | - | - |
| Study 3M | −.07 | .05 | −1.48 | 6 | .185 | −.08 | .06 | −1.22 | 1164 | .223 | −.06 | .09 | −.63 | 1164 | .527 | .06 | .06 | .93 | 14 | .368 | - | - | - |
| Study 3A | −.07 | .04 | −1.70 | 13 | .113 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Study 4 | −.27 | .04 | −6.56 | 13 | 2.13E-05 | −.07 | .06 | −1.21 | 235 | .229 | .17 | .08 | 2.22 | 234 | .028 | −.06 | .06 | −1.08 | 240 | .282 | - | - | - |
| Study 5 | −.23 | .02 | −10.59 | 290 | 2.29E-22 | .02 | .04 | .37 | 244 | .713 | .05 | .05 | .94 | 247 | .349 | .03 | .04 | .67 | 290 | .505 | .29 | (3, 287) | .955 |
Note. Study 3 analyses were initially conducted on the sample of participants who saw male providers only (Study 3M), to test replication of Studies 1 and 2, and then were conducted on the full sample with moderation by stimulus sex (Study 3A). Moderation by provider sex was evaluated in Studies 3A, 4, and 5, and moderation by provider race was evaluated in Study 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
Study 2
Study 1 suggested that the providers’ competent appearance was associated with perceivers’ preference for providers and expectations of pain. Using the effect size estimate of the effect of competent appearance on pain in Study 1, we aimed to collect a sample size large enough to test this effect with at least 80% power (total N=140). Further, in light of evidence that perceptions of similarity influence pain experience in a simulated clinical paradigm (Losin et al., 2017) and that healthcare experiences are often influenced by patient’s demographic characteristics (including race and sex) (Chapman et al., 2013; Zestcott et al., 2016), we explored potential race- or sex-based differences in the effect of competent appearance and whether participants’ perceptions of their providers’ similarity to themselves influenced their healthcare expectations. Finally, we explored whether first impressions would influence expectations of post-procedural medication use, which could have implications for patients’ likelihood of turning to prescription opioids. Therefore, we added additional measures of perceptions of provider similarity and expectations for post-procedural analgesic treatment (half of participants rated similarity and half rated expected medication use), and tested whether participant demographics moderated any effects. Participants who were asked to rate similarity were not given instructions about what characteristics to use when rating similarity. They were simply asked “How similar is this person to you?” and provided ratings on a 1–10 Likert Scale (see Supplementary Materials).
Results
Participants were more likely to choose the more competent-looking provider, p<.001, choosing the more competent looking face on 68.30% of trials, an effect that became more pronounced the larger the difference in competence between the two faces, t(136)=12.07, p<.001 (Table 1). Participants expected less pain with more competent-looking providers, B=−.16, t(102)=−5.78, p<.001 (Table 2).
In exploratory analyses, we tested whether perceptions of provider similarity influenced expectations of pain. Participants expected less pain following procedures performed by providers perceived to be more similar to themselves, B=−.23, t(59)=−3.78, p<.001 (Table 3). This was independent of competent appearance (Table S2.5), and there was no significant association between competent appearance and similarity, p>.615 (Table S2.12). There was no difference in similarity as a function of participant race/ethnicity, gender, or their interaction (all p’s > 0.1).
Table 3.
Effect of perceived similarity on participants’ expectations for post-procedural pain.
| Expected Pain | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 2 | −.23 | .06 | −3.78 | 59 | 3.71E-04 | .05 | .12 | .39 | 52 | .695 | −.15 | .14 | −1.06 | 48 | .293 | - | - | - | - | - | - | - | - |
| Study 3M | −.41 | .05 | −7.50 | 19 | 4.48E-07 | −.22 | .09 | −2.48 | 109 | .015 | −.04 | .13 | −.31 | 123 | .757 | - | - | - | - | - | - | - | - |
| Study 3A | −.41 | .05 | −7.67 | 45 | 1.05E-09 | - | - | - | - | - | - | - | - | - | - | .09 | .08 | 1.15 | 47 | .254 | - | - | - |
| Study 4 | −.39 | .03 | −13.36 | 242 | 6.99E-31 | −.03 | .06 | −.48 | 239 | .633 | .13 | .08 | 1.66 | 231 | .097 | .10 | .06 | 1.76 | 2.42 | .079 | - | - | - |
| Study 5 | −.19 | .02 | −9.14 | 249 | 2.21E-17 | .02 | .04 | .55 | 209 | .582 | .12 | .04 | 2.61 | 206 | .010 | −.03 | .04 | −.69 | 248 | .489 | .77 | (3, 246) | .513 |
Note. Study 3 analyses were initially conducted on the sample of participants who saw male providers only (Study 3M), to test replication of Studies 1 and 2, and then were conducted on the full sample with moderation by stimulus sex (Study 3A). Moderation by provider sex was evaluated in Studies 3A, 4, and 5, and moderation by provider race was evaluated in Study 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
We also measured whether the providers’ apparent competence influenced participants’ expectations about analgesic treatment. Apparent competence influenced medication use expectations, B=−.13, t(66)=−3.86, p<.001, such that participants expected to be less likely to use prescription-strength pain medication following procedures with more competent looking providers (Table 4). There were no systematic differences in expectations about pain or medication as a function of participant race, t(35)=1.40, p=.172 and t(23)=−.47, p=.640 respectively, or sex, t(135)=1.34, p=.181 and t(75)=1.68, p=.098 respectively. Neither race nor sex moderated the effects of competent appearance on expectations of pain, ps>.148 (Tables S2.6–2.7), or medication use, ps>.465 (Tables S2.8–2.9), or of similarity on expectations of pain, ps>.293 (Tables S.2.10–2.11).
Table 4.
Effect of competent appearance on participants’ expectations for post-procedural analgesic treatment.
| Expected Analgesic Treatment | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 2 | −.13 | .03 | −3.86 | 66 | 2.61E-04 | .05 | .07 | .73 | 77 | .465 | −.01 | .08 | −.08 | 79 | .935 | - | - | - | - | - | - | - | - |
| Study 3M | −.08 | .03 | −2.80 | 1062 | .005 | −.05 | .06 | −.78 | 1169 | .437 | −.04 | .09 | −.46 | 1172 | .648 | - | - | - | - | - | - | - | - |
| Study 3A | −.05 | .02 | −2.56 | 28 | .016 | - | - | - | - | - | - | - | - | - | - | .14 | .04 | 3.38 | 1916 | .001 | - | - | - |
| Study 4 | −.13 | .05 | −2.59 | 12 | .023 | −.09 | .06 | −1.42 | 241 | .156 | .14 | .08 | 1.80 | 242 | .073 | −.04 | .06 | −0.61 | 242 | .541 | - | - | - |
| Study 5 | −.18 | .03 | −6.39 | 276 | 6.97E-10 | −.01 | .06 | −.16 | 242 | .875 | .07 | .06 | 1.10 | 246 | .272 | −.01 | .06 | −0.32 | 256 | .749 | .28 | (3,273) | .838 |
Note. Study 3 analyses were initially conducted on the sample of participants who saw male providers only (Study 3M), to test replication of Studies 1 and 2, and then were conducted on the full sample with moderation by stimulus sex (Study 3A). Moderation by provider sex was evaluated in Studies 3A, 4, and 5, and moderation by provider race was evaluated in Study 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
Study 3
Studies 1 and 2 revealed providers’ facial appearance influenced participants’ choice of providers and expectations about pain and treatment. However, both studies used CG, White male faces as stimuli. To test external validity, we used real faces that were manipulated to vary in levels of perceived competence(Oh et al., 2019) (Figure 2B). By using stimuli from a stimulus set that included female faces, we could also test whether effects observed in male providers generalized to female providers. All participants saw faces of only one sex (N=164 male; N=158 female). All stimuli depicted White faces.
Results
We initially conducted all analyses on the subset of participants who saw male providers (N=150 after excluding participants who did not indicate preference for either provider on any trial), to test whether effects observed in CG stimuli generalized to real faces. Contrary to Studies 1 and 2, participants were no more likely to choose the more competent looking provider in the pair, p=.402. Participants chose the provider morphed higher in competence only 50.91% of the time (Table 1). Preference also did not differ as a function of the difference in competence between the two faces, p=.545 (Table 1).
We then turned to measuring the effects of provider apparent competence and perceived provider similarity on healthcare expectations. Contrary to Studies 1 and 2, there was no effect of apparent competence on expectations of pain, p=.185 (Table 2), though it continued to significantly predict expectations for analgesic medication, B=−.08, t(1062)=−2.80, p=.005 (Table 4), such that participants expected to be more likely to require post-procedural prescription-strength pain medication with less competent looking providers.
Participants expected less pain following procedures conducted by providers they perceived as more similar to themselves, B=−.41, t(19)=−7.50, p<.001 (Table 3), and to be more likely to use prescription-strength pain medication following procedures with providers perceived to be more different from them, B=−.24, t(42)=−4.30, p<.001 (Table 5), replicating Study 2. The effect of similarity differed as a function of participant sex for both expectations for post-procedure pain, B=−.22, t(109)=−2.48, p=.015 (Table 3), and medication use, B=−.27, t(129)=−2.56, p=.012 (Table 5), such that both effects were stronger for females (B=−.52, 95% CI=[−.69, −.34] for pain and B=−.38, 95% CI=[−.55, −.22] for medication use) than males (B=−.32, 95% CI=[−.47, −.17] for pain and B=−.13, 95% CI=[−.26, −.001] for medication use). Follow-up analyses indicated that similarity ratings differed by participant sex (B=−.61, t(145)= −3.74, p<.001), such that male participants reported higher similarity than female participants. There were no influences of race/ethnicity or interactions between sex and race/ethnicity. In light of these sex differences, we examined questionnaire data to determine whether there were group differences in average perceptions of healthcare providers or general attitudes towards analgesic treatments. Questionnaires revealed no sex differences in the extent to which participants in general perceive their providers to be similar to them, p=.711, nor in their attitudes towards prescription-strength relative to over-the-counter pain medication, p=.487 (Table S3.23). Neither participant race nor sex moderated any other effects, ps>.223 (Table S3.8–3.13).
Table 5.
Effect of perceived similarity on participants’ expectations for post-procedural analgesic treatment.
| Expected Analgesic Treatment | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 3M | −.24 | .06 | −4.30 | 42 | 1.02E-04 | −.27 | .10 | −2.56 | 129 | .012 | .02 | .15 | .15 | 140 | .885 | - | - | - | - | - | - | - | - |
| Study 3A | −.24 | .05 | −4.43 | 73 | 3.28E-05 | - | - | - | - | - | - | - | - | - | - | .01 | .08 | .14 | 76 | .886 | - | - | - |
| Study 4 | −.26 | .03 | −7.84 | 47 | 4.58E-10 | −.08 | .06 | −1.25 | 252 | .213 | .09 | .08 | 1.16 | 247 | .247 | −.08 | .06 | −1.30 | 256 | .195 | - | - | - |
| Study 5 | −.16 | .03 | −6.04 | 238 | 5.92E-09 | .02 | .05 | .29 | 219 | .775 | .13 | .06 | 2.15 | 217 | .032 | −.04 | .05 | −.78 | 237 | .438 | 0.86 | (3, 236) | .462 |
Note. Study 3 analyses were initially conducted on the sample of participants who saw male providers only (Study 3M), to test replication of Studies 1 and 2, and then were conducted on the full sample with moderation by stimulus sex (Study 3A). Moderation by provider sex was evaluated in Studies 3A, 4, and 5, and moderation by provider race was evaluated in Study 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
We next conducted analyses on the full sample and tested for moderation by provider sex. The effect of providers’ apparent competence on participant’s preference for providers differed as a function of provider sex, t(287)= −2.09, p=.038 (Table 1). Whereas there was no effect of provider’s competent appearance on preference for male providers (50.9%, 95% CI=[.49, .53]), participants chose the more competent looking female provider only 47.8% of the time (95% CI=[.45, .50]) – in other words, they were more likely to choose the less competent looking female provider. Provider sex also moderated the effect of the difference in competence levels between the two providers on participant’s choice, B=−.26, 95% CI=[−.39, −.13], p=.010 (Table S3.14): as the apparent competence difference between the two faces was more pronounced, participants preferred the less competent looking female provider, B=−.21, 95% CI=[−.35, −.07], whereas there was no effect of the difference in apparent competence for male providers, B=.05, 95% CI=[−.09, .19].
Consistent with effects in participants who saw only male stimuli, a model that included all stimuli and moderation by provider sex revealed no significant main effect of competent appearance on pain expectations, p=.092 (Table 2). We observed no moderation of the association between competent appearance and expected pain by provider sex, p=.317 (Table 2). Provider sex did, however, moderate the effect of competent appearance on expected use of pain medicine, B=.14, t(1916)=3.38, p=.001 (Table 4), such that greater apparent competence was associated with greater expectations of using over-the-counter medication following procedures by male providers, B=−.05, 95% CI=[−.09, −.01], whereas greater apparent competence was associated with enhanced expectations of using prescription-strength medication following procedures by female providers, although this effect was not significant when restricted to female providers, B=.03, 95% CI=[−.01, 07]. Using the full sample and including provider sex as a moderator, the main effects of greater perceived similarity on expectations of less pain, B=−.41, t(19)=−7.50, p<.001, and of over-the-counter post-procedural medication use, B=−.41, t(45)=−7.67, p<.001, persisted, but these effects were not moderated by the provider’s sex, ps>.254 (Tables 3 and 5). On average, there were no differences in expectations of pain, t(13)=−1.26, p=.228, or medication use, t(13)=−1.56, p=.144, as a function of provider sex.
Consistent with findings limited to male stimuli, similarity ratings differed by participant sex (B=−.60, t(280)= −3.49, p<.001), such that male participants reported higher similarity than female participants. There was no interaction between perceiver gender and provider sex (p > 0.1), nor were there any interactions with perceiver race/ethnicity. Thus male perceivers reported higher similarity to provider stimuli regardless of provider gender.
Study 4
In Study 3, providers’ manipulated facial features of competence did not predict participants’ choices or expectations of post-procedural pain. However, Study 3 stimuli differed substantially from those in Studies 1 and 2: they were these real (albeit manipulated) faces and also included additional information such as hair and clothing. This non-facial information might obscure the effect of facial appearance of competence on pain expectations. Thus, in Study 4, we again used real faces, but stripped them of any non-facial cues that might obfuscate perceptions of competence (Figure 2C). As with Study 3, participants (N=322) saw only either male (N=141 after excluding participants who expressed no preference on any trial) or female (N=142 after excluding participants who expressed no preference on any trial) providers, selected preferred providers, and rated expectations of post-procedural pain and analgesic use.
To validate the stripped stimuli, participants provided trait ratings of stimuli competence at the end of the experiment. We also measured participants’ perceptions of stimuli warmth, among other dimensions (Supplemental Materials). Participants provided ratings for both the masked faces that they saw when they rated their healthcare expectations and non-masked faces of the opposite sex. Inclusion of these trait ratings for different types of stimuli allowed us to verify that stripping the images of non-facial information did not influence ratings of competence, and permitted validation of whether the manipulated competence levels correspond with participants’ perceptions of competence.
Results
Stripping the stimuli of non-facial information did not affect perceptions of competence, p=.886 (Table S4.1). Thus, any effects that we observe in Study 4 with the masked manipulated stimuli that differed from those observed with the full stimuli in Study 3 are unlikely to be due to different perceptions of competence among the masked (relative to full-faced) stimuli. Interestingly, we observed no significant association between manipulated competence levels and perceived competence, p=.169 (Table S4.2), suggesting that morphed competence within stimuli did not align well with participants’ perceptions of competence between stimuli. In supplementary analyses, we therefore tested whether aggregate perceptions of competence for each stimulus (i.e., the average perceived competence for each stimulus across all Study 4 participants, collapsing across masked and unmasked stimuli) predicted Study 3 outcomes; results were largely unchanged (Tables S3.21–22). Thus, in all subsequent analyses, we focus only on participants’ ratings of perceived competence, rather than on manipulated levels (for analyses using manipulated competence, see Supplementary Materials). Participants’ own ratings of competence were used in analyses predicting their healthcare expectations. However, due to a coding error, providers whom participants saw when rating their healthcare expectations and perceptions of competence differed from those they saw when making a choice between providers. Thus, aggregate perceived competence (i.e., the averaged competence rating across all subjects for each stimulus) was used as a predictor in analyses predicting participants’ choice of provider. As observed previously (Oh et al., 2019), female faces were rated more competent on average than male faces, t(13)=3.01, p=.010.
Participants preferred providers who were on average rated more competent, choosing the provider higher in perceived competence 56.39% of the time, t(281)=4.69, p<.001, and this effect was exacerbated the larger the difference in perceived competence between providers, B=−.32, 95% CI = [−.46, −.18], p=.024 (Table 1). Provider sex again moderated participants’ preference for more competent looking providers, t(261)= −2.32, p=.035, such that competence was more associated with selection of male providers than female providers: Participants chose the more competent looking female provider 53.5% of the time (95% CI=[.49, .58]) and chose the more competent looking male provider 59.2% of the time (95% CI=[.56, .62]). Participants also expected less pain, B=−.27, t(13)=−6.56, p<.001 (Table 2), and to be less likely to use prescription-strength pain medication, B=−.13, t(12)=−2.59, p=.023 (Table 4), following procedures conducted by providers that participants perceived to be more competent (based on each participants’ post-task ratings). The effect of perceived competence on expected pain was moderated by participant race, p=.028 (Table 2): effects were significant only for White participants, B=−.30, 95% CI=[−.40, −.21], and not for participants of color, B=−.13, 95% CI=[−.28, .02]. Participant race showed a similar trend toward moderating the effect of perceived competence on expected medication use, however this effect was not statistically significant, p=.073 (Table 4). There were no differences in average expected pain or expected medication use as a function of participant race, nor were there any differences in self-reported frequency of healthcare encounters or healthcare attitudes as a function of participant race (all ps>.2; Table S4.36). Neither participant nor provider sex moderated any effects of perceived competence on healthcare expectations and there were no differences in average expected pain or analgesic use as function of provider sex (all ps>.1).
Participants’ perceptions of similarity again predicted both pain expectations, B=−.39, t(242)=−13.36, p<.001 (Table 3), and medication expectations, B=−.26, t(47)=−7.84, p<.001 (Table 5), such that participants expected less pain and to be more likely to use over-the-counter, relative to prescription-strength, medication following procedures conducted by providers they perceived to be similar to themselves. Perceived similarity predicted pain independently of perceived competence, though inclusion of similarity in the model predicting expectations of medication use led competence to drop to non-significance, p=.144 (Table S4.13). Neither participant nor provider demographic characteristics moderated the effect of perceived similarity on healthcare expectations, though we may have been underpowered to detect interactions, as moderation of the effect of similarity on pain expectations by both participant race and provider sex were not statistically significant, p=.097 and p=.079, respectively (Tables 3 and 5). Consistent with study 3, there was a main effect of perceiver gender (B = −.24, t(275) = −2.28, p = .023), such that male participants reported higher similarity than female participants (male: M = 3.83, SD = .71; female: M = 3.60, SD = .92). There was no interaction with provider sex (all p’s > 0.1), nor were there any effects of perceiver race/ethnicity (all p’s > 0.2).
We also tested whether perceived warmth predicted healthcare expectations, and whether it did so independently of perceived competence and similarity. Perceived warmth predicted expectations of both pain, B=−.33, t(14)=−11.72, p<.001 (Table 6), and medication use, B=−.15, t(15)=−4.20, p=.001 (Table 7), such that participants expected less pain and more over-the-counter (relative to prescription-strength) medication for procedures conducted by providers they perceived to be warmer. Neither provider nor participant demographic characteristics moderated any effects, ps>.169. Perceived warmth exerted an effect on expectations of pain and medication use independently of both competence and similarity (Tables S4.29–4.30).
Table 6.
Effect of perceived warmth on participants’ expectations for post-procedural pain.
| Expected Pain | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 4 | −.33 | .03 | −11.72 | 14 | 9.84E-09 | −.04 | .04 | −.91 | 238 | .363 | .07 | .06 | 1.14 | 271 | .256 | .06 | .05 | 1.38 | 259 | .169 | - | - | - |
| Study 5 | −.22 | .02 | −12.47 | 302 | 4.39E-29 | −.02 | .03 | −.61 | 246 | .543 | .09 | .04 | 2.37 | 246 | .018 | .01 | .04 | .26 | 301 | .794 | 1.21 | (3, 265) | .307 |
Note. Warmth was measured and assessed only in Studies 4 and 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
Table 7.
Effect of perceived warmth on participants’ expectations for post-procedural analgesic treatment.
| Expected Analgesic Treatment | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderation by Participant Demographics | Moderation by Provider Demographics | ||||||||||||||||||||||
| Sex | Race | Sex | Race | ||||||||||||||||||||
| B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | B | SE | t | df | p | F | df | p | |
| Study 4 | −.15 | .03 | −4.20 | 15 | .001 | −.05 | .05 | −1.02 | 253 | .31 | .00 | .07 | .04 | 283 | .969 | .01 | .05 | .14 | 265 | .892 | - | - | - |
| Study 5 | −.17 | .02 | −7.62 | 279 | 4.06E-13 | −.05 | .04 | −1.04 | 254 | .297 | .09 | .05 | 1.80 | 254 | .073 | −.03 | .04 | −.77 | 278 | .440 | 1.33 | (3, 276) | .265 |
Note. Warmth was measured and assessed in only Studies 4 and 5. We report statistics when p-values were below 0.1. See text for post-hoc results separate by sex or race, and supplementary tables for full statistics for p-values greater than 0.1.
Study 5
Study 4 demonstrated that perceived competence, rather than manipulated competence, predicted provider preference and pain expectations. In Study 5, we used real, unmanipulated faces and analyzed whether participants’ own perceptions of competence, similarity, and warmth predicted their choice of medical provider and healthcare expectations. Using a naturalistic stimulus set allowed us to include stimuli of both sexes and of many races, so we also tested the effect of provider sex and race on healthcare expectations, and whether concordance between participant and provider race and sex influenced any observed effects (as has been observed previously(Street et al., 2008)). Each participant saw providers of only one race and sex.
Results
Participants chose the provider they perceived to be more competent 62.20% of the time, p<.001 (Table 1). This did not vary by provider or participant sex, ps>.160, but did vary by both participant race, p=.046, and provider race, p=.027 (Table 1), such that the effect of perceived competence on preference was strongest for White providers (65.1%, 95% CI=[.62, .68]) and White participants (57.6%, 95% CI=[.55, .61]), relative to providers and participants of color, (61.1%, 95% CI=[.59, .63]) and (50.8%, 95% CI=[.44, .57]), respectively. The effect of perceived competence on preference was larger when the difference in perceived competence between the two providers was greater, p<.001 (Table 1).
Participants again expected less pain, p<.001 (Table 2), and to be less likely to use prescription strength pain medications, p<.001 (Table 4), following procedures conducted by providers they perceived to be more competent. Neither participant nor provider demographic characteristics moderated the effect of perceived competence on expectations of pain or medication use, ps>.272 (Tables 2 and 4).
Participants also expected less pain, p<.001 (Table 3), and more use of over-the-counter (relative to prescription-strength) medication, p<.001 (Table 5), following procedures conducted by providers judged to be similar to themselves. Both effects were moderated by participant race (Tables 3 and 5), such that they were weaker for participants of color (B=−.06, 95% CI=[−.16, −.04] for pain and B=−.06, 95% CI=[−.16, −.04] for medication use), relative to White participants (B=−.19, 95% CI=[−.25, −.13] for pain and B=−.19, 95% CI=[−.25, −.13] for medication use). However, neither participant nor provider demographics nor the concordance of participant and provider demographics moderated any other effects, ps>.349.
Similar effects were observed for perceived warmth: participants expected less pain, p<.001 (Table 6), and more use of over-the-counter medication, p<.001 (Table 7), following procedures conducted by providers judged to be warm. Participant race moderated the effect of warmth on expectations of pain, p=.018 (Table 7), such that effects were weaker among participants of color, B=−.15, 95% CI=[−.22, −.08], compared to White participants, B=−.24, 95% CI=[−.28, −.20], and also showed a similar trend toward moderating the effect of perceived warmth on expectations of analgesic treatment, although this effect was not statistically significant (p=.073). No demographic characteristics of either provider or participant, nor concordance between participant and provider demographics, moderated any other effects of warmth, ps>.265. Perceived similarity, competence, and warmth significantly predicted expectations of pain and medication use independently, ps≤.001 (Tables S5.38–39).
Consistent with studies 2–4, we tested whether perceiver and provider demographics influenced perceived similarity. Because study 5 stimuli varied in race/ethnicity, we also tested for interactions with stimulus race. In contrast to studies 2 and 3, there were no effects of perceiver gender on similarity (all p’s > 0.1). However, there was a significant effect of stimulus race/ethnicity (B = −0.63, t(221) = −2.13, p = .034), such that similarity ratings were lower for non-White providers (MWhiteProvider = 3.40, SD = 0.91; MNon-whiteProvider = 3.13, SD = 1.19). We note that the majority of participants were also White (see Supplementary Table 1.0). While the Participant Race x Provider Race interaction was not significant (p = .08), White participants rated White providers as more similar to them than non-White providers (B = .45, SE = .18, t(233) = 2.53, p = .012; MWhiteProvider = 3.43, SD = 0.77; MNon-whiteProvider = 2.98, SD = 1.13), whereas there was no difference within non-White participants (p > 0.4; MWhiteProvider = 3.29, SD = 1.39; MNon-whiteProvider = 3.54, SD = 1.24).
On average, there was a main effect of provider race on expectations of pain, F(3, 581)=11.67, p=1.96e-7, and medication use, F(3,581)=44.06, p=1.16e-25, and of provider sex on expectations of medication use, F(1, 583)=27.02, p=2.79e-7, such that the mean level of post-surgical pain expected was lowest with Asian providers and the likelihood of using prescription-strength medication was lowest with Asian and White providers and with female providers. Questionnaires revealed no differences in healthcare experiences or attitudes as a function of participant demographics (Tables S5.40–5.41).
Meta-Analysis
We sought to quantify the overall effect of competent appearance in medical providers on participants’ healthcare choices and expectations across all five studies, as well as the effect of perceptions of provider similarity on participants’ healthcare expectations and the moderation effect of participant and provider demographic characteristics. We therefore used meta-analyses to test whether participant sex and race moderated the relationship between provider appearance and participants’ healthcare expectations, and whether provider sex moderated the effect of provider appearance on participant choice or expectations. Because provider race was only manipulated in Study 5, a meta-analysis was not conducted on the moderating effect of provider race on decisions and expectations.
Across all five studies, participants were more likely to choose a more competent looking provider (Figure 3A), choosing the more competent-looking provider an average of 59.45% of the time (95% CI=[50.50%, 68.40%], t(4)=2.93, p=.043). Participants expected less pain during painful medical procedures conducted by providers who appeared more competent, B=−.13, 95% CI=[−.20, −.07], t(4)=−5.48, p=.005 (Figure 3B), and to be more likely to use over-the-counter, relative to prescription-strength, pain medication following procedures conducted by more competent looking providers, B=−.09, 95% CI=[−.13, −.05], t(3)=−6.92, p=.006 (Figure 3C). Participants’ perceptions of similarity to providers also influenced expectations of pain, B=−.23, 95% CI=[−.39, −.07], t(3)=−4.60, p=.020 (Figure 4A), and medication use, B=−.16, 95% CI=[−.31, −.001], t(2)=−4.33, p=.049 (Figure 4B).
Fig. 3. Meta-analytic Effects of Competent Appearance.

A) Meta-analytic effect of apparent competence on patient choice of provider. Across 5 studies, participants chose the more competent looking provider 59.45% of the time. B) Meta-analytic effect of apparent competence on expectations of post-procedural pain. Across 5 studies, participants expected less pain following procedures conducted by more competent looking providers, B = −.13, p = .005. C) Meta-analytic effect of apparent competence on expectations of post-procedural medication use. Across 4 studies, participants expected to be less likely to use prescription-strength pain medication following procedures conducted by more competent looking providers, B = −.09, p =.006.
Fig. 4. Meta-analytic Effects of Perceived Similarity.
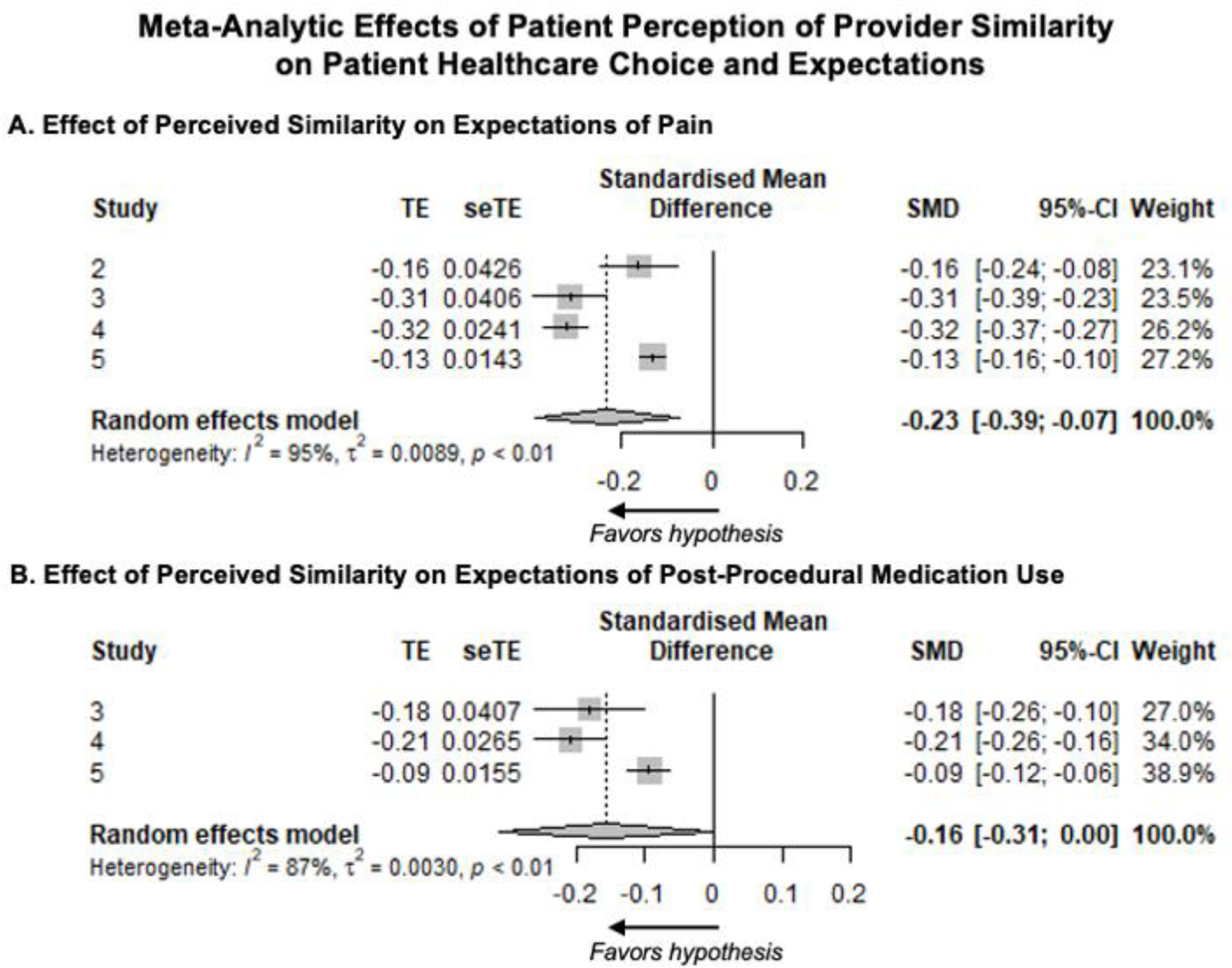
A) Meta-analytic effect of perceived similarity on expectations of pain. Across 4 studies, participants expected less pain following procedures conducted by providers they perceived to be more similar to themselves, B = −.23, p = .019. B) Meta-analytic effect of perceived similarity on expectations of post-procedural medication use. Across 3 studies, participants expected to be less likely to use prescription strength pain medication following procedures conducted by providers they perceived to be more similar to themselves, B = −.16, p = .049.
Meta-analytic examination of the effect of participant demographic characteristics on healthcare expectations revealed that participant race moderated the effect of perceived similarity on expectations for post-procedural medication use, B=.07, 95% CI=[.03, .12], t(2)=6.79, p=.021, such that the effect was stronger for White participants relative to participants of color. Male participants reported higher similarity to providers than female participants, B=−.44, 95% CI=[−.76, −.12], t(4)=−3.79, p=.019. No other moderation by participant demographic characteristics was statistically significant in the meta-analyses (Table S.6.1).
DISCUSSION
In a world where our digital presence ever-increasingly precedes face-to-face interactions, many patients rely on the convenience of web services to select healthcare providers (Zhao et al., 2017). Our results suggest that healthcare decisions may be influenced by headshots featured on such services, which have the potential to fundamentally alter patients’ expectations with downstream consequences for their experience in the clinic. Across five studies of simulated clinical decisions, impressions of hypothetical healthcare providers, judged based on providers’ physical appearance alone, influenced participants’ choice of provider and expectations about pain and medication following a hypothetical painful medical procedure. Participants preferred to have painful procedures conducted by providers who appeared more competent (see Table 1 and Figure 3), and expected less pain and to be less likely to use prescription-strength pain medication following procedures conducted by providers they judged to be more competent, warm, and similar to themselves (see Figures 3 and 4). Our findings reveal that first impressions directly influence choices about healthcare (e.g., which physician to see), suggesting they may have real clinical implications before patients even enter the clinic. We also identify one mechanism for how they do so: Trait impressions impact people’s explicit expectations about their own experiences, which can in turn modulate pain. This indicates that the type of expectations that directly influence clinical outcomes in the form of placebo effects may be formed even before patients set foot in a clinic.
Our results link perceived competence with pain expectations and build on prior clinical work that demonstrated that perceptions of physician competence following a clinical interaction influenced patient pain (Mattarozzi et al., 2020). Notably, perceptions of competence based on visual appearance did not impact pain in previous work (Mattarozzi et al., 2020); yet, impressions were measured not in patients themselves but in a unique sample from a similar population. We replicated this finding in Study 3 when we found that competence ratings provided by other participants did not predict pain expectations. This is consistent with evidence that the effects of trait impressions may be perceiver- or context-specific (Hehman et al., 2017). Though we ultimately demonstrated that other observers’ perceptions of targets’ competence (when targets were evaluated in context – i.e., as healthcare providers) did predict participants’ healthcare expectations (Study 4), a particular strength of our study is that, by using hypothetical vignettes, we were able to measure initial trait impressions based exclusively on visual appearance within perceivers themselves (because there was no subsequent clinical experience). Research conducted in actual clinics (e.g., (Ashton-James et al., 2019; Mattarozzi et al., 2020)) cannot so easily disentangle the impact of initial impressions and clinical interactions in the same individuals.
Of course, though first impressions persist into and may shape subsequent social encounters, they are not irreversible. Indeed, the actual patient-provider interactions in the clinic could engender expectations that conflict with and potentially override expectations the patient had upon entering the clinic. Updating our implicit evaluations of others, however, is cognitively taxing (Mann and Ferguson, 2017, 2015). Further, our evidence suggests that initial impressions of healthcare providers’ competence may prevent people from ever even scheduling an appointment with providers they deem to be incompetent, thus limiting their opportunities to revise their initial impressions. Of course, there are many situations in which one’s provider is not chosen by oneself (e.g., emergency room visits, rescheduled appointments), and many healthcare providers that patients interact with throughout the course of their visit to the clinic may not be the primary provider whose image they selected (e.g., nursing staff). Yet our results suggest that initial impressions of even these healthcare providers would have robust effects on patients’ expectations for their pain and analgesia use.
Effects were largely consistent across participant and provider demographic characteristics. Yet meta-analysis suggested that participant race moderated the association between perceived provider similarity and expectations for post-procedural analgesic treatment, such that it was stronger for White participants than for participants of color. Notably, in all but one study, providers were White. Thus, to the extent that individuals show privileged memory for and holistic processing of same-race faces (Meissner and Brigham, 2001; Michel et al., 2006), this could be an artifact of experimental design. Consistent with this, when provider race varied in Study 5, participants (the majority of whom were White) reported being less similar to non-White providers relative to White providers. White individuals also tend to have greater trust in the medical establishment (Halbert et al., 2006), which may make them prone to developing positive expectations about treatments, particularly if they perceive providers to be competent or similar to themselves. Using questionnaire data, we explored whether White participants might, in general, have more positive attitudes towards analgesic treatments or perceive greater similarity to their healthcare providers. Further, in post-hoc analyses (Supplemental Materials), we tested whether there were systematic differences by participant race in how heterogenous expectations of post-procedural analgesic use were across different medical providers. Differences in heterogeneity would be expected, for example, if White participants had invariantly positive expectations for analgesic treatment or if participants from historically underserved groups had invariantly negative expectations for analgesic treatment. However, we did not observe any race-based differences. Future work should continue to examine whether past healthcare experiences, which have been shown to vary based on race and can influence pain (Anderson et al., 2009; Hoffman et al., 2016; Losin et al., 2020; Mossey, 2011), influence patients’ perceptions of their providers and the impact of those perceptions on healthcare expectations. We also note that our study was not powered to detect interactions, and that we observed trends toward interactions with participant race in Studies 4 and 5. Future studies with larger samples and a more diverse population might be better able to determine the extent to which demographic or sociocultural concordance between patient and provider moderates expectations and choices in experimental simulations, as a substantial body of work indicates that concordance can mitigate racial disparities in medical treatment (Dovidio et al., 2008; Shen et al., 2018).
Limitations
Our study provides the first evidence that the selection of hypothetical healthcare providers can influence expectations about pain and analgesia based on first impressions alone. This work has important implications but is not without limitations. As mentioned earlier, our study was conducted entirely online, which provides the benefit of allowing us greater experimental control over stimulus attributes and separating first impressions from impressions that would be due to interactions in the actual clinical context. However, our use of an online venue for these studies required us to limit trial duration, limit the number of potential doctors, and require participants to make repeated decisions. Participants also made judgments about providers without additional information that might influence decisions, such as where the provider completed their degree or their average patient satisfaction rating, which are often as readily available online as are headshots. We also did not instruct participants to use specific characteristics when rating similarity (e.g., physical appearance versus inferred personality), and therefore cannot determine what features guided similarity judgments, which in turn predicted pain expectations. We infer that participants used a mixture of external features (e.g., provider race in Study 5) and personal decisions (e.g., male participants feeling more similar to providers in Studies 3 and 4, regardless of the provider’s sex). Finally, we asked participants about general painful procedures rather than specific medical procedures, which allowed us to avoid the possibility that participants would differ in expectations based on prior experience (i.e., whether they had undergone that procedure). We chose not to specify a procedure to capture the pure influence of trait impressions and expectations on pain and analgesia in general, rather than accounting for variations in patients’ knowledge of and experience with different medical procedures. Our participants were not actual patients, but a diverse group of online participants, and therefore we had to rely on self-report to measure participants’ prior experience and feelings about clinical care in general.
These limitations can be addressed in future work that tests these associations in an ecologically valid clinical context or paired with actual web-based apps and telemedicine. In particular, future work in this area should measure expectations about actual clinicians based on facial images, and examine whether patients’ initial expectations persist throughout actual clinic experience and shape subsequent clinical outcomes, such as pain. Future work should also evaluate how patients weight judgments based on visual appearance relative to more explicit metrics (e.g., degree, patient satisfaction rating), and testing for associations with different aspects of perceived similarity (e.g., similarity based on age, gender, race/ethnicity, or inferred personality). Finally, future studies should evaluate expectations relative to specific painful procedures, as different interventions may be differentially sensitive to social influences and expectations, as well as desired provider traits and characteristics (Dusch et al., 2014).
CONCLUSION
In sum, converging evidence across five studies demonstrates that participants’ expectations about hypothetical healthcare treatment are fundamentally shaped by their trait impressions of potential providers, made based on providers’ physical appearance alone. These findings have profound implications for the future of patient care, especially as the world navigates crises like the COVID-19 pandemic that push patients towards telemedicine, where non-visual cues may be stilted (Emerick et al., 2020), and that demand greater reliance on masks, which may degrade nonverbal cues during face-to-face clinical visits. In such circumstances, patients may come to rely even more on judgments made before an actual interaction in the clinic, judgments made based on whatever information patients can gather about their provider – perhaps most saliently, their provider’s visual appearance.
Supplementary Material
Fig. 5. Effect of Provider Demographic Characteristics on Participant Healthcare Expectations in Study 5.

A) Participant expectations of post-procedural pain varied as a function of provider race. Participants expected less pain with Asian providers, relative to providers of all races (all ps ≤ .001), and marginally greater pain with Black, relative to White, providers, p = .086. Higher scores indicate greater pain. B) Participant expectations of post-procedural medication use varied as a function of provider race. Participants expected to be more likely to use over-the-counter pain medication, relative to prescription strength pain medication, following procedures conducted by Asian relative to Black and Latinx providers, ps < .001, by White relative to Black and Latinx providers, ps < .001, and by Latinx relative to Black providers, ps < .001. Lower scores indicate participants expected to be more likely to use over-the-counter pain medications, whereas higher sores indicate participants expected to be more likely to use prescription strength pain medication. A score of 5 represents equal likelihood of using over-the-counter and prescription strength pain medication. On average, participants expected to be more likely to use over-the-counter pain medication (all means < 5). C) Participant expectations of post-procedural medication use varied as a function of provider sex. Participants expected to be more likely to use over-the-counter pain medication, relative to prescription strength pain medication, following procedures conducted by female, relative to male, providers, ps < .001. See B for description of the scale used to assess expectations of pain medication use. + < .10, * < .05, ** ≤ .01, *** ≤ .001, after Tukey’s post-hoc comparison method.
Highlights.
Participants chose medical providers based on facial features in 5 online studies.
More competent-looking providers were preferred in all experiments.
Competence linked to expectations for less pain and less potent analgesics.
Pain expectations were also independently shaped by perceived similarity and warmth.
First impressions can impact decisions and expectations even outside the clinic.
Acknowledgements.
This work was supported by the Intramural Research Program of the National Center for Complementary and Integrative Health at the National Institutes of Health (ZIA-AT000035). The authors thank Margaret Rose-McCandlish, DongWon Oh, and Alex Todorov for their helpful comments on experimental design considerations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work has been posted as a preprint at https://psyarxiv.com/a5cuh/
The authors report no conflicts of interest.
Identifiable information for Materials and Methods: The project was approved by NIH’s Office of Human Subjects Research Protection (18-NCCIH-0622).
The datasets generated and analysed in the current studies will be available in the Open Science Framework repository at https://osf.io/eshk8/ upon publication.
REFERENCES
- Aguinis H, Gottfredson RK, Culpepper SA, 2013. Best-Practice Recommendations for Estimating Cross-Level Interaction Effects Using Multilevel Modeling. J. Manage 39, 1490–1528. 10.1177/0149206313478188 [DOI] [Google Scholar]
- Anderson KO, Green CR, Payne R, 2009. Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care. J. Pain 10, 1187–1204. 10.1016/j.jpain.2009.10.002 [DOI] [PubMed] [Google Scholar]
- Anderson SR, Gianola M, Perry JM, Losin EAR, 2020. Clinician – Patient Racial / Ethnic Concordance Influences Racial / Ethnic Minority Pain : Evidence from Simulated Clinical Interactions 00, 1–17. 10.1093/pm/pnaa258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthony Jnr B, 2020. Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic. J. Med. Syst 44, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton-James CE, Forouzanfar T, Costa D, 2019. The contribution of patients’ presurgery perceptions of surgeon attributes to the experience of trust and pain during third molar surgery. PAIN Reports 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atlas LY, Wager TD, 2012. How expectations shape pain. Neurosci. Lett 520, 140–148. 10.1016/j.neulet.2012.03.039 [DOI] [PubMed] [Google Scholar]
- Balduzzi S, Rücker G, Schwarzer G, 2019. How to perform a meta-analysis with R: A practical tutorial. Evid. Based. Ment. Health 22, 153–160. 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr DJ, Levy R, Scheepers C, Tily HJ, 2013. Random effects structure for confirmatory hypothesis testing: Keep it maximal. J. Mem. Lang 68, 255–278. 10.1016/j.jml.2012.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker BM, Walker SC, 2015. Fitting Linear Mixed-Effects Models Using {lme4}. J. Stat. Softw 67, 1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Becker BJ, Wu M, 2007. The Synthesis of Regression Slopes in meta-analysis. Stat. Sci 22, 414–429. 10.1214/07-STS243 [DOI] [Google Scholar]
- Borenstein M, Hedges LV, Rothstein HRR, 2011. Introduction to meta-analysis John Wiley {&} Sons. [Google Scholar]
- Brauer M, Curtin JJ, 2017. Linear Mixed-Effects Models and the Analysis of Nonindependent Data: A Unified Framework to Analyze Categorical and Continuous Independent Variables that Vary Within-Subjects and/or Within-Items. Psychol. Methods 23, 389–411. [DOI] [PubMed] [Google Scholar]
- Chapman EN, Kaatz A, Carnes M, 2013. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J. Gen. Intern. Med 28, 1504–1510. 10.1007/s11606-013-2441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen PA, Cheong JH, Jolly E, Elhence H, Wager TD, Chang LJ, 2019. Socially transmitted placebo effects. Nat. Hum. Behav 3, 1295–1305. 10.1038/s41562-019-0749-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claire Elson E, Oermann C, Duehlmeyer S, Bledsoe S, 2020. Use of telemedicine to provide clinical pharmacy services during the SARS-CoV-2 pandemic. Am. J. Heal. Pharm 77, 1005–1006. 10.1093/ajhp/zxaa112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czerniak E, Biegon A, Ziv A, Karnieli-Miller O, Weiser M, Alon U, Citron A, 2016. Manipulating the placebo response in experimental pain by altering doctor’s performance style. Front. Psychol 7, 1–10. 10.3389/fpsyg.2016.00874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniali H, Flaten MA, 2019. A Qualitative Systematic Review of Effects of Provider Characteristics and Nonverbal Behavior on Pain, and Placebo and Nocebo Effects. Front. Psychiatry 10. 10.3389/fpsyt.2019.00242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton J/L.. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care, Social Science & Medicine, 67 (3), 478–486. 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Dusch MN, O’Sullivan PS, Ascher NL, 2014. Patient perceptions of female surgeons: How surgeon demeanor and type of surgery affect patient preference. J. Surg. Res 187, 59–64. 10.1016/j.jss.2013.10.020 [DOI] [PubMed] [Google Scholar]
- Emerick T, Alter B, Jarquin S, Brancolini S, Bernstein C, Luong K, Morrisseyand S and Wasan A, 2020. Telemedicine for Chronic Pain in the COVID-19 Era and Beyond. Pain Medicine, 21(9), pp.1743–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Tofighi D, 2007. Centering Predictor Variables in Cross-Sectional Multilevel Models: A New Look at an Old Issue. Psychol. Methods 12, 121–138. 10.1037/1082-989X.12.2.121 [DOI] [PubMed] [Google Scholar]
- Evers AWM, Blease C, Atlas LY, 2018. Implications of Placebo and Nocebo Effects for Clinical Practice : Expert Consensus 10.1159/000490354 [DOI] [PMC free article] [PubMed]
- FeldmanHall O, Dunsmoor JE, Kroes MCW, Lackovic S, Phelps EA, 2017. Associative Learning of Social Value in Dynamic Groups. Psychol. Sci 28, 1160–1170. 10.1177/0956797617706394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske ST, Cuddy AJC, Glick P, 2006. Universal dimensions of social cognition: Warmth and competence. Trends Cog. Sci 11, 77–83. 10.1016/j.tics.2006.11.005 [DOI] [PubMed] [Google Scholar]
- Fuentes J, Armijo-Olivo S, Funabashi M, Miciak M, Dick B, Warren S, Rashiq S, Magee DJ, Gross DP, 2014. Enhanced Therapeutic Alliance Modulates Pain Intensity and Muscle Pain Sensitivity in Patients With Chronic Low Back Pain: An Experimental Controlled Study. Phys. Ther 94, 477–489. 10.2522/ptj.20130118 [DOI] [PubMed] [Google Scholar]
- Graham JR, Harvey CR, Puri M, 2017. A Corporate Beauty Contest. Manage. Sci 63, 3044–3056. [Google Scholar]
- Guolo A, Varin C, 2017. The number of studies matters. Stat. Methods Med. Res 26, 1500–1518. 10.1177/0962280215583568 [DOI] [PubMed] [Google Scholar]
- Halbert CH, Armstrong K, Gandy OH, Shaker L, 2006. Racial differences in trust in health care providers. Arch. Intern. Med 166, 896–901. 10.1001/archinte.166.8.896 [DOI] [PubMed] [Google Scholar]
- He X, Sun Q, Stetler C, 2017. Warm Communication Style Strengthens Expectations and Increases Perceived Improvement. Health Commun 33, 939–945. 10.1080/10410236.2017.1322482 [DOI] [PubMed] [Google Scholar]
- Hehman E, Sutherland CAM, Flake JK, Slepian ML, 2017. The unique contributions of perceiver and target characteristics in person perception. J. Pers. Soc. Psychol 113, 513–529. 10.1037/pspa0000090 [DOI] [PubMed] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, Oliver MN, 2016. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc. Natl. Acad. Sci 113, 4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe LC, Goyer JP, Crum AJ, 2017. Harnessing the Placebo Effect: Exploring the Influence of Physician Characteristics on Placebo Response. Heal. Psychol [DOI] [PMC free article] [PubMed]
- Howe LC, Leibowitz KA, Crum AJ, 2019. When Your Doctor “Gets It” and “Gets You”: The Critical Role of Competence and Warmth in the Patient–Provider Interaction. Front. Psychiatry 10. 10.3389/fpsyt.2019.00475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inthout J, Ioannidis JPA, Borm GF, 2014. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol 14, 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, Kirsch I, Schyner RN, Nam BH, Nguyen LT, Park M, Rivers AL, McManus C, Kokkotou E, Drossman DA, Goldman P, Lembo AJ, 2008. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 336, 999–1003. 10.1136/bmj.39524.439618.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuznetsova A, Brockhoff PB, Christensen RHB, 2015. Package “lmerTest.” R Packag. version 2
- Little AC, Perrett DI, 2007. Using composite images to assess accuracy in personality attribution to faces. Br. J. Psychol 98, 111–126. 10.1348/000712606X109648 [DOI] [PubMed] [Google Scholar]
- Losin EAR, Anderson SR, Wager TD, 2017. Feelings of Clinician-Patient Similarity and Trust Influence Pain: Evidence From Simulated Clinical Interactions. J. Pain 18, 787–799. 10.1016/j.jpain.2017.02.428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losin EAR, Woo C, Medina NA, Andrews-hanna JR, Eisenbarth H, Wager TD, 2020. Neural and sociocultural mediators of ethnic differences in pain. Nat. Hum. Behav 4, 517–530. 10.1038/s41562-020-0819-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma DS, Correll J, Wittenbrink B, 2015. The Chicago face database: A free stimulus set of faces and norming data. Behav. Res. Methods 47, 1122–1135. 10.3758/s13428-014-0532-5 [DOI] [PubMed] [Google Scholar]
- Mann TC, Ferguson MJ, 2017. Reversing implicit first impressions through reinterpretation after a two-day delay. J. Exp. Soc. Psychol 68, 122–127. 10.1016/j.jesp.2016.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann TC, Ferguson MJ, 2015. Can We Undo Our First Impressions? The Role of Reinterpretation in Reversing Implicit Evaluations. J. Pers. Soc. Psychol 108, 823–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattarozzi K, Caponera E, Russo PM, Colonnello V, Bassetti M, Farolfi E, Todorov A, 2020. Pain and satisfaction: healthcare providers’ facial appearance matters. Psychol. Res 10.1007/s00426-020-01330-3 [DOI] [PubMed]
- Meissner CA, Brigham JC, 2001. Thirty Years of Investigating the Own-Race Bias in Memory for Faces: A Meta-Analytic Review. Psychol. Public Policy, Law 7, 3–35. 10.1037/1076-8971.7.1.3 [DOI] [Google Scholar]
- Michel C, Rossion B, Han J, Chung CS, Caldara R, 2006. Holistic processing is finely tuned for faces of one’s own race. Psychol. Sci 17, 608–615. 10.1111/j.1467-9280.2006.01752.x [DOI] [PubMed] [Google Scholar]
- Mossey JM, 2011. Defining racial and ethnic disparities in pain management, in: Clinical Orthopaedics and Related Research pp. 1859–1870. 10.1007/s11999-011-1770-9 [DOI] [PMC free article] [PubMed]
- Necka EA, Faig KE, van Hedger K, Lyons IM, Dimitroff SJ, Luhmann M, Puts DA, Norman GJ, 2018. Women’s Attention to and Memory for Fertile- and Non-Fertile Phase Women Across the Menstrual Cycle. Adapt. Hum. Behav. Physiol 10.1007/s40750-018-0093-4 [DOI]
- Necka EA, Kardan O, Puts DA, Faig KE, Berman MG, Norman GJ, 2019. Visual cues to fertility are in the eye (movements) of the beholder. Horm. Behav 115, 104562. 10.1016/j.yhbeh.2019.104562 [DOI] [PubMed] [Google Scholar]
- Necka EA, Puts DA, Dimitroff SJ, Norman GJ, 2016. Other women’s fertility moderates female resource distribution across the menstrual cycle. Evol. Hum. Behav 37. 10.1016/j.evolhumbehav.2016.03.003 [DOI] [Google Scholar]
- Nezlek JB, 2012. Multilevel Modeling for Psychologists, in: Cooper H, Camic PM, Long DL, Pander AT, Rindskopf D, Sher KJ (Eds.), APA Handbook of Research Methods in Psychology Vol 3 Data Analysis and Research Publication American Psychological Association, pp. 219–241. 10.1037/13621-011 [DOI] [Google Scholar]
- Oh D, Buck EA, Todorov A, 2019. Revealing Hidden Gender Biases in Competence Impressions of Faces. Psychol. Sci 30, 65–79. 10.1177/0956797618813092 [DOI] [PubMed] [Google Scholar]
- Olivola CY, Todorov A, 2010. Fooled by first impressions? Reexamining the diagnostic value of appearance-based inferences. J. Exp. Soc. Psychol 46, 315–324. 10.1016/j.jesp.2009.12.002 [DOI] [Google Scholar]
- Olivola CY, Todorov A, 2010. Elected in 100 milliseconds : Appearance-Based Trait Inferences and Voting. J. Nonverbal Behav 34, 83–110. 10.1007/s10919-009-0082-1 [DOI] [Google Scholar]
- Osch M. Van, Dulmen S. Van, Vliet L. Van, Bensing J, 2017. Specifying the effects of physician’s communication on patients’ outcomes: A randomised controlled trial. Patient Educ. Couns 100, 1482–1489. 10.1016/j.pec.2017.03.009 [DOI] [PubMed] [Google Scholar]
- Over H, Cook R, 2018. Where do spontaneous first impressions of faces come from? Cognition 170, 190–200. 10.1016/j.cognition.2017.10.002 [DOI] [PubMed] [Google Scholar]
- Peirce J, Gray JR, Simpson S, Macaskill M, Höchenberger R, Sogo H, Kastman E, Lindeløv JK, Peirce J, 2019. PsychoPy2: Experiments in behavior made easy. Behav. Res. Methods 51, 195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J, n.d. CloudResearch Tools to Help Combat Responses from Suspicious Geolocations [WWW Document]. Cloud Res. Blog
- Robinson J, Litman L, Robinson J, Abberbock T, 2016. TurkPrime.com : A versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav. Res. Methods 49, 433–442. 10.3758/s13428-016-0727-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R, Dimatteo MR, 2001. Meta-analysis: Recent Developments in Quantitative Methods for Literature Reviews. Annu. Rev. Psychol 52, 59–82. [DOI] [PubMed] [Google Scholar]
- Rothenfluh F, Germeni E, Schulz PJ, 2016. Consumer Decision-Making Based on Review Websites: Are There Differences Between Choosing a Hotel and Choosing a Physician? J Med Internet Res 2016;18(6):e129. doi: 10.2196/jmir.5580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Röver C, Knapp G, Friede T, 2015. Hartung-Knapp-Sidik-Jonkman approach and its modification for random-effects meta-analysis with few studies. BMC Med. Res. Methodol 15, 99. 10.1186/s12874-015-0091-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen MJ, Peterson EB, Costas-Muñiz R et al. The Effects of Race and Racial Concordance on Patient-Physician Communication: A Systematic Review of the Literature. J. Racial and Ethnic Health Disparities 5, 117–140 (2018). 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slepian ML, Ames DR, 2016. Internalized Impressions: The Link Between Apparent Facial Trustworthiness and Deceptive Behavior Is Mediated by Targets’ Expectations of How They Will Be Judged. Psychol. Sci 27, 282–288. 10.1177/0956797615594897 [DOI] [PubMed] [Google Scholar]
- Stoet G, 2010. PsyToolkit: A software package for programming psychological experiments using Linux. Behav. Res. Methods 42, 1096–1104. 10.3758/BRM.42.4.1096 [DOI] [PubMed] [Google Scholar]
- Stoker JI, Garretsen H, Spreeuwers LJ, 2016. The Facial Appearance of CEOs: Faces Signal Selection but Not Performance. PLoS One 11, e0159950. 10.1371/journal.pone.0159950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street RL, O’Malley KJ, Cooper LA, Haidet P, 2008. Understanding Concordance in Patient-Physician Relationships : Personal and Ethnic. Ann. Fam. Med 6, 198–205. 10.1370/afm.821.Department [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi E, Weber J, Prevost C, Mischel W, Mobbs D, 2015. Inference of Others’ Competence Reduces Anticipation of Pain When Under Threat. J. Cogn. Neurosci 27, 2071–2078. 10.1162/jocn [DOI] [PubMed] [Google Scholar]
- Todorov A, 2005. Inferences of Competence from Faces Predict Election Outcomes. Science (80-. ) 308, 1623–1626. 10.1126/science.1110589 [DOI] [PubMed] [Google Scholar]
- Todorov A, Dotsch R, Porter JM, Oosterhof NN, Falvello VB, 2013. Validation of data-driven computational models of social perception of faces. Emotion 13, 724–738. 10.1037/a0032335 [DOI] [PubMed] [Google Scholar]
- Twisk J, De Boer M, De Vente W, Heymans M, 2013. Multiple imputation of missing values was not necessary before performing a longitudinal mixed-model analysis. J. Clin. Epidemiol 66, 1022–1028. 10.1016/j.jclinepi.2013.03.017 [DOI] [PubMed] [Google Scholar]
- Wager TD, Atlas LY, 2015. The neuroscience of placebo effects: Connecting context, learning and health. Nat. Rev. Neurosci 16. 10.1038/nrn3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson JP, Rule NO, 2015. Facial Trustworthiness Predicts Extreme Criminal-Sentencing Outcomes. Psychol. Sci 26, 1325–1331. 10.1177/0956797615590992 [DOI] [PubMed] [Google Scholar]
- Wojciszke B, Bazinska R, Jaworski M, 1998. On the dominance of moral categories in impression formation. Personal. Soc. Psychol. Bull 24, 1251–1263. [Google Scholar]
- Wyatt M, Silvester J, 2018. Do voters get it right? A test of the ascription-actuality trait theory of leadership with political elites. Leadersh. Q 29, 609–621. 10.1016/j.leaqua.2018.02.001 [DOI] [Google Scholar]
- Zestcott CA, Blair IV, Stone J, 2016. Examining the Presence, Consequences, and Reduction of Implicit Bias in Health Care: A Narrative Review. Group Process. Intergroup Relat 19, 528–542. 10.1177/1368430216642029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao P, Yoo I, Lavoie J, Lavoie BJ, Simoes E, 2017. Web-based medical appointment systems: A systematic review. J. Med. Internet Res 19, 1–9. 10.2196/jmir.6747 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


