Abstract
Peer-provided services exist in many different domains and professions. However, there is a knowledge gap in the existing programs’ descriptions and grouping that hinders creating new high-quality peer support programs. The objectives of this article are two-fold in describing existing peer support programs published in the literature in the medical field and evaluating their descriptive quality. Six electronic databases, grey literature, and reference lists were systematically searched. Studies reporting the existence of a support program delivered by peers and its description or methodology were included. Studies targeting patients and children were excluded. 11 articles were included in the qualitative synthesis and explored in detail. A total of 2155 peers participated in support programs in the fields of medicine, nursing, or both. Programs in other professional fields were not found. Programs were described in five different countries. Three methods of peer support delivery were found: in person, online, and mixed varying in their goals, duration, peer training supervision and participant demographics and number. Program descriptions were rated as good, fair, or poor using a verified rating scale. There are numerous well-described programs varying in their methodology and type of delivery. Thus, the emergence of new programs can be based on such models that have been well-described in the literature.
Abstract
Les services fournis par les pairs existent dans de nombreux domaines et professions. Cependant, les connaissances en matière de description et de regroupement des programmes existants sont lacunaires, entravant ainsi la création de nouveaux programmes de soutien par les pairs de qualité. Le présent article vise d’une part à décrire les programmes actuels de soutien par les pairs dont fait état la littérature médicale et d’autre part à évaluer leur qualité descriptive. Une recherche systématique a été effectuée dans six bases de données électroniques, dans la littérature grise et dans les listes de références. Toutes les études présentant un programme de soutien fourni par des pairs et sa description ou sa méthodologie ont été incluses. Les études ciblant les patients et les enfants ont été exclues. Onze articles ont été inclus dans la synthèse qualitative et explorés en détail. Au total, 2155 pairs ont participé à un programme de soutien en médecine, en sciences infirmières ou dans les deux domaines. Aucun programme n’a été trouvé dans d’autres domaines professionnels. Les programmes décrits proviennent de cinq pays différents. Trois méthodes de soutien par les pairs ont été trouvées : en personne, en ligne et mixte. Les objectifs, la durée, la supervision de la formation par les pairs, les données démographiques des participants et leur nombre varient d’un programme à l’autre. Les descriptions de programmes ont été évaluées selon une échelle d’évaluation validée comme bonnes, acceptables ou médiocres. Il existe de nombreux programmes, bien décrits, qui varient en termes de méthodologie et de type de prestation. Aussi, la création de nouveaux programmes pourra s’appuyer sur les modèles qui sont bien décrits dans la littérature.
Introduction
Peer support is a dynamic socio-emotional relationship between people who share various commonalities such as environment, experiences, or mental health to bring about the desired change.1 The terms peer support, peer-provided services and peer programs are used interchangeably. However, throughout this review, only the term peer support will be consistently used. Although peer support was first developed as an asset for patients with severe psychiatric disorders, peer support has expanded into many different domains and professions.1
The importance of social relationships in maintaining one’s well-being and health has attracted many scientists and health discipline experts to explore its efficacy.2 Particular attention is being made to peer-run services and peer support workers found in clinical environments,2 where healthcare professionals are being immersed in different peer support initiatives and trends.3 Burnout plagues many medical professions and is linked to long work hours, resource constraints, and troublesome documentation. This inevitably beckons the importance of robust support systems, such as peer support, especially amidst the current draining medical culture that healthcare professionals face.4
Peer support is not only prevalent in the medical profession but is also seen in the non-medical workplace. For example, Alberta Health Services has created a peer support program to suit every workplace.5 Additionally, evidence of peer support groups from 1994 shows teachers aiming to support educators in making informed decisions about day-to-day events.6 Peer support may also occur in a more formal manner where the team may host social events or offer wellness activities to benefit all employees.5
Peer support programs are effective in education, psychiatric care, and workplaces. A broad list of programs exists for a diverse type of populations, collectively highlighting many different outcomes. However, current deficiencies in the literature exist featured by the inability to perceive a systematic approach to investigating, categorizing, and describing existing peer support groups, systems, or initiatives for non-patient populations. In addition, the establishment of high-quality peer support programs based on the literature necessitates properly described and replicable published strategies.
Therefore, this study has a double aim. The first intent was to describe the existing peer support programs published in the literature. The second was to evaluate the quality of the program descriptions provided by each published article. As the study was conducted, all descriptions regardless of quality were included to provide a summary of peer support for institutions to develop and implement such programs.
Materials and methods
This systematic search adhered to the Preferred Reporting Items for Systematic reviews and Meta-analyses – PRISMA checklist.7 Our research is exempt from the Research Ethics Board (REB) Review.
Identification of relevant studies
Eligibility criteria: Published articles reporting and describing peer support programs or initiatives around the world were included. The target population was participants of peer support programs at post-secondary, graduate or professional levels. No language or publication date restrictions were set. The following scenarios were considered eligible: peer-support writing groups aiming to increase feelings of self-efficacy and self-esteem and support systems delivered on a social media platform to peers.
Studies were excluded if the peer support programs’ target population pertained to children or to patients and those designed explicitly towards specific mental health conditions. Blogs, websites, editorial and personal statements were not considered.
Information sources & search protocol
With the assistance and expertise of a health sciences librarian, a search strategy was designed. Appropriate truncation with word combinations was adapted for each electronic database: Ovid MEDLINE, Embase, PubMed, Ovid ERIC. The search was up to July 9, 2020. Two grey literature search engines were used, including Google Scholar and an online university library. Supplemental Data, Table 1 details each database strategy, word truncations, key search terms and Booleans used. All references were managed, and duplicate articles were removed automatically with a revision from two reviewers (L.P. and T.R.). The Covidence Software (Veritas Health Innovation, Melbourne, Australia), an interface-specific for evidence synthesis processes, available at www.covidence.org8 was used in all phases.
Study selection
A two-phase process was followed. In phase one, two reviewers (L.P. and T.R.) independently screened all titles and abstracts of the imported references. Articles meeting the inclusion criteria were included. In phase two, the same reviewers independently applied the inclusion criteria to these article’s full-text form. Supplemental Data, Table 2 shows full texts not meeting the inclusion criteria and the reason for their exclusion. Throughout phases one and two, any conflicts between the reviewers were reconciled by agreeing on a mutual and final decision by discussing with the field expert and project supervisor (K-A.H.). The reference lists of the selected articles were manually screened to identify any relevant references that may have been missed during the search of electronic databases. Articles referenced by the field experts were also considered. The final selection and eligibility decisions were based on the full-text articles.
Charting the data
The “PICOS principle” was followed in the extraction of key features of the included articles.9 Population: Medical, non-medical, post-secondary and professional fields; Intervention: Peer support programs or initiatives; Comparison: Not required; Outcome: Any outcome/existence and description of the program; Study design: No restriction to study design.
The first author (L.P.) extracted all required data from included articles following a standardized form. The second author (T.R.) reviewed all retrieved information. Any conflicts were settled through a discussion between the reviewers and the field expert (K.-A. H.).
Level of evidence
Program description rating - classification and quality ratings: A validated quality rating checklist for peer support programs10 was tailored to our research question. Initially, this checklist was to rate the quality and completeness of the program’s descriptions, for the peer supporters (volunteers) giving support and for the peers (participants) receiving support. For our included studies, the subsection for patient description rating was not applied; see exclusion criteria. The maximum total score for program and peer descriptions was 28 points. The authors assigned each program to one of three categories: ‘poor’, ‘fair’, and ‘good’, based on a scoring system for a program description and peer description.
Synthesis of results
Although the research question focused on the description of peer support programs, a qualitative description of results for evaluations or analyses, if provided, was summarized.
Results
Study selection
A total of 1724 studies were identified through a database search. Another 239 were identified from the grey literature, totalizing 1963 articles included in phase one. After eliminating 1932 articles, 31 articles entered phase two, where full texts are assessed for eligibility. Supplemental Data Table 2 presents the articles deemed ineligible and the reasons for exclusion. A total of 11 articles were included in the content qualitative synthesis and explored in detail. The flow diagram details the selection process, as per Figure 1.
Figure 1.
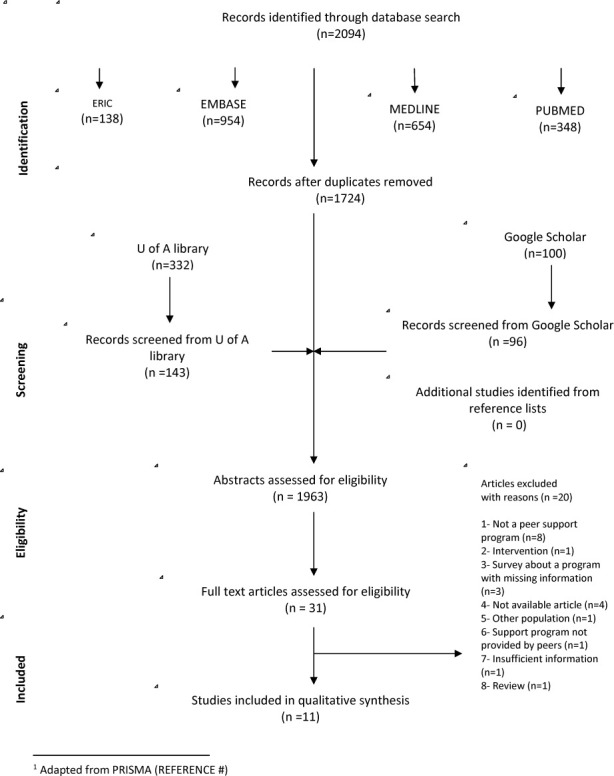
Flow diagram of literature search and selection criteria
Study characteristics
At least 2155 participants benefited from the peer support programs during the reported time. The exact number is difficult to estimate due to the lack of specification of participant numbers for some studies.11–13 Table 1 (Appendix A) summarizes the key program features reported by the included articles. Three models of peer support delivery were identified: in-person (n = 5),11,12,14–16 online (n = 2),13,17 mixed (n = 3),4,18,19 and not specified (n = 1).20 Mixed delivery is defined as including combinations of in-person and online models along with online and over the phone sessions. These programs originated from the United States of America (USA),4,11,14,17,18,20 Hong Kong,13 New Zealand,21 Canada,12 and Australia.15,16 The peer support programs and initiatives described in the included articles were targeted to the fields of medicine4,12–17,20,21 and nursing11 or both.18 Programs were delivered to specific populations: six programs were offered to medical students,13–15,17,19,20 three to graduated physicians (fellows, residents, specialized physicians),4,12,16 one to nurses only,11 and one was offered to both physicians and nurses.18
Results of individual studies: George et al.17 made 55 video-narratives which were viewed a total of 369 times. These videos covered topics such as valuable advice, orientations, and stories of success and failure. The ease of utilizing Facebook, a platform already used by students, was communicated in the feedback as a peer support delivery tool. Also, students preferred the use of Facebook and online group sessions over e-mails and in-person sessions.
Gilliland et al.11 described the earliest peer support program in our included articles. Many key factors leading to the successful implementation of a peer support group were listed. Among those factors were a population in need of peer support, administrative advocacy, a convenient time and location, a broad scope of program content, a motivated organizational committee, and an on-going evaluation.
Lane et al.18 described various necessary steps towards creating a successful peer support program for physicians. They noted a rate of 4.8 referrals of clinicians to peer supporters per month, with 16 clinicians out of 165 demanding higher levels of support.
Lau et al.13 explored student engagement in their program. Two-thirds of the respondents (n~200) stated having heard of the support group, while 20 of these students had entered the peer support forum. Only one student had reached out to the program through e-mail.
In the study conducted by Moir et al.,19 mental health improvements were compared between a peer support group and a mindfulness group. While 25% (n = 17) of the participants used the program’s face-to-face component, more than half attended a peer social event or a mindfulness program. The authors found improvements in the mental health of the peer supported group although not statistically significant (p>0.05).
Redwood et al.14 described a 16-year-long program as part of the medical school curriculum. The mean annual participation rate for first-year students in the program was 94%. The program was a valuable learning experience and worth attending even without the grade incentive, according to 72% (n = 94) of the survey respondents. Most respondents (n = 46) reported being able to manage their stress better. Only 3% (n = 4) felt uncomfortable in participating in the group. Most students deemed the relaxation response and empathetic listening as useful components of the program, 74% (n = 97) and 71% (n = 93) respectively.
Robledo et al.20 outlined the rate of program use within medical students. Many students (n = 39) reported seeking out peer support from a senior peer. In contrast, 19 of them reported getting support from a peer in their own year. Many participants indicated they used both types of support. Also, 56% of participants (n = 31) received support for themselves, while 38% (n = 21) sought it for their peers. The various reasons to pursue peer support include problems with relationships, mental health concerns, and academic issues. Less than 10% (n = 3) of respondents reported not wanting support from the program.
In the study by Calder-Sprackman et al.12 targeting emergency medicine residents, 58.8% of survey respondents (n = 20) perceived that they had gained awareness of the challenges within their residency program, as well as of coping strategies to tackle them. Half of the residents (n = 34) felt that the “Ice Cream Rounds,” which are regular peer support wellness rounds, helped them reflect on their clinical practice. Participants also reported a decreased sensation of burnout and less stress and anxiety.
Shapiro et al.4 reported a stepwise programmatic approach to peer support initiatives. Useful peer support conversation requires outreach calls, invitations, listening, reflecting, reframing, sense-making, coping, closing, and resources/referrals, with all steps being comprehensively described.
Sugumar et al.15 put a mental health program in place for medical students. All survey respondents agreed that the program helped reduce the stigma associated with mental health in medicine. The program also assisted in improving peer support and self-care practices. The reported key success of this program was that it is peer-led.
Wilson et al.16 used a Likert scale to report survey results and participant feedback for their peer support group targeted to general practitioners treating mental health problems. Participants generally stated that practical sessions were helpful and that they would attend them again. However, participants disliked the role-play session reporting that it led to confusion and discomfort.
Synthesis of results
Our goal was to describe the type of peer support program delivery and the quality of the program descriptions.
Type of program delivery
In-person groups: Five of the included articles provided a peer support program to in-person groups.11,12,14–16 Only two of these authors cited a specific number of attendees for each session15,16 while the other three provided an estimated range of attendees for each event.11,12,14 One of the articles15 provided detailed participant feedback about the benefits.
Online delivery: Two articles described peer support exclusively online, through various communication tools.13,17 One program17 strictly used the online social media platform Facebook and specifically targeted students’ feelings to reduce anxiety and enhance academic confidence. The other13 used a non-specified online forum, as well as e-mails to reach out to participants. Their goal was to offer resources to students by increasing students’ mental health awareness and creating effective channels for seeking help. Both programs13,17 targeted medical students, aimed to facilitate social connectedness. The type of support delivered was unscheduled, spontaneous, and always available through the platforms mentioned.
Mixed delivery: Three of the included articles adopted a mixed method of peer support delivery.4,18,19 These authors provided combinations of phone or e-mail communication, in groups, and/or individualized programs. Except for one,18 all programs in this type of delivery recorded attendance for their programs.
Quality of program within studies
For all articles included, a checklist (Appendix B) adapted from Hoey et al.10 was created to evaluate the quality of each peer support program’s description. Programs were given points for descriptions that were documented, complete, detailed, and explicitly clear. The checklist rated the program descriptions and peer description (both for the peer providing and receiving the services) for all the articles. The total score was out of 28, with a higher score being reflective of a more complete description of programs and peers.
Table 2 (Appendix A) describes the quality assessment scores for each article. A total of eight4,11–13,15,16,18,20 articles fairly described their programs and the minority14,17,19 had a good description of their program. No articles were rated as poor.
Discussion
This narrative review firstly attempted to portray and describe the existing peer support programs published in the literature. Although the inclusion criteria did not limit the search to medical fields, none of the included articles found a population outside the area of healthcare. For this reason, the title of this article specifies the fields (medicine and nursing) to which it pertains. Similar to systematic reviews exploring programs targeting different populations,10,22,23 this review identified various types of peer support interventions and programs, delivering such support in different ways. This heterogeneity led to the classification of peer support delivery type based on existing work.10
To fulfil the second goal of this paper, this research additionally evaluated the quality of the descriptions provided by each included article. To establish the foundation of a new peer support program based on existing literature, the currently available published articles must be thoroughly descriptive of their target populations, interventions, and methodologies. Accordingly, the quality of program description was assessed using a checklist (Appendix B) adapted from Hoey et al.10 Although the population targeted by Hoey et al. is different from the one targeted by this systematic search, the goals are similar such that the checklist was adapted for this purpose.
An important design feature of this paper was its double goal of first describing, then evaluating peer support programs. This specific order of objectives was preferred because of utmost importance, programs must be described and published. This allows for institutions, workplaces and support groups to understand the existence and nature of peer support. Second, program descriptions must be evaluated, such that organizers wishing to start such programs may have a reference of how a program can be excellent and successful.
Generally, a common weakness for many programs4,11–16,18–20 is the lack of clear descriptions of the peers. These studies lacked a direct and explicit description of one-point-worth-each characteristics such as age, sex, and marital status for both the peer providing and receiving support. This can be interpreted as an attempt to maintain participant confidentiality or that this information was deemed insignificant. However, without a clear description of the individuals who successfully delivered the support, it is challenging to reproduce peer-support groups elsewhere. Additionally, a second obstacle in obtaining higher scores was the absence of a guide to develop peer training. Only two programs14,19 utilized objective guidance such as training manuals, to build their program and train the participants. Again, clear protocols and methods of delivery in these published programs would facilitate the ability of creating new peer-support groups based on literature. The only three articles14,17,19 rated as having overall good quality descriptions fully describe the peers participating in the support program. These descriptions are of utmost importance in defining the interventions due to their importance for increasing replicability and maximizing future programs’ success.
The first author of one of the included studies4 launched a program named Center for Professionalism and Peer Support at Brigham and Women’s Hospital (BWH) in 2008.24 Since then, many articles have been published,4,25 which have all been cited by four of the included studies.14,17–19 The program at BWH has influenced others, as it portrays peers as leaders of initiatives targeted towards fellow same-levelled individuals (peer-to-peer interventions)14,18 and it effectively reduces distress, depression and anxiety through early intervention.17,19 Interestingly, two of the four mentioned papers describing certain programs partly inspired by the Peer Support Program at BWM4 have received program rating described as good.17,19 This is the highest rating possible for a specific paper. It is important to note that the program described by Shapiro et al.4 received a rating of “fair.” Perhaps Shapiro et al. could of have enriched their program’s description by adding more details regarding their program implementation, methodology and/or content.
George et al.17 described an online program of peer support that is similar to those reported in papers13,17 previously mentioned. However, this program was staff-led and perhaps could have been improved if led by like-minded peers. To this point, a previous study reports that clinicians rarely access available support from mental health providers after adverse or stressful events, but they might seek help from colleagues or peers.4
The concept of a “second victim” is not new in medicine and has been addressed in previous studies.26–28 It is defined by a situation in which a healthcare provider becomes a victim of the adverse event brought onto the patient due to medical errors, or other causes. These incidents have repercussions on the mental health of doctors and other healthcare providers. Lane et al.18 commented on this notion in their study and described peer support groups as a necessity for these professionals. The benefits include increased communication, sharing of experiences, as well as providing an opportunity to reach out for help and support from peers. Similarly, another included article17 reports an intervention targeting and offering support to a population potentially suffering from feelings of failure. By providing videos of stories pertaining to real experiences among fellow students and professionals, failure became normalized. Consequently, it allowed students to understand that many individuals feel an immense feeling of failure. With this exposure, students were better prepared for potential hardships, and were taught to reframe their reactions to such events.
A common theme among all the articles was the importance of confidentiality, and how it affects participation rates and efficacy of programs. As reported by Lane et al.,18 a common barrier for physicians in participation in peer support services is confidentiality. According to one study,17 participants preferred online group support delivery methods, rather than e-mails and in-person sessions due to privacy. With their identity hidden, participants felt comfortable and encouraged to fully benefit from the support services available. Similarly, one peer support program in Hong Kong13 reported that only three participants opted for e-mail communication. The authors speculated that this minimal endorsement of such identity-revealing modalities illustrates, in part, reluctance to share their distress for fear of being identified and stigmatized.
The lack of time as a barrier to seeking peer support was also mentioned.18 However, a common trend within programs presented in Table 1 is that overall, those offering online or mixed support delivery types have more participants. It may be that in-person programs constitute a challenge due to time commitment issues, the inconvenience of commuting, or that participants value confidentiality, as proposed by others.17,18 In contrast, mixed and online types of peer support programs reached 34.8% (n = 749) of all participants reported in this review. In addition, over 16 years, 51.6% (n = 1111) of all participants attended in-person sessions. Another weakness that arose from programs is the lack of proper reporting of participation. As stated in the results section, only two15,16 of the in-person support groups11,12,14 were able to provide the number of participants. Also, one support program16 counted a total of eight participants in the first two workshops, and seven participants in the third. However, whether these are consistent attendees, new participants in each workshop, or a mix of new and previous participants is not specified. No authors provided explanations for the lack of reporting of participation rates. Multiple factors, such as unstructured attendance taking, unreported exact attendee numbers, or finally, lack of assurance of confidentiality, could explain those limitations.
On another note, a simple benefit of in-person programs is that program organizers may get direct and immediate feedback from participants. One manuscript16 reported overt participant feedback received during the session, which can enhance program quality. Overall, in-person programs were very well received, and offered users valuable learning experiences and increasing interest in future involvement of similar peer support systems. These programs also helped decrease stress levels among participants.
Interestingly, a gender divide seems to exist in terms of who participates in these programs. Lau et al.13 reported that significantly more women than men wanted to learn about mental health. Similarly, George et al.17 and Moir et al.19 reported that 57% and 53% of their participants were female, respectively. Only one study20 reported a relatively higher number of male (50.5%) participants. The divide is congruent with a study reviewing gender differences in support-seeking behaviour, which found that females reported a significantly higher likelihood of seeking social support (both emotional and instrumental). According to the World Health Organization,29 in all parts of the world except China and Myanmar, the reported rates of suicide are higher for men than for women. In the United States and Canada, males are more than three times as likely to attempt suicide as females. This emphasizes the importance of gender differences in seeking support. These statistics suggest that peer-support programs would significantly enhance their value by increasing male participant population to address this gender gap.
Unsurprisingly, there are multiple downsides or weaknesses to offering peer-support. According to data obtained in London, United Kingdom,30 peer workers found that sharing experiences was an off-putting and challenging task at times. Additionally, previously published studies report that some peer support group participants typically assume the role of “team leader”, and are uncomfortable sharing their own emotional distress.4 This could counterintuitively hinder the mental health of such leaders, who are not receiving the benefits of participating in such groups. Moreover, it is important to consider that a peer support group does not replace professional therapy or treatment. Some articles refer support group participants who need further mental health services to higher-level psychological therapy.4,18,19 This is a strong argument for offering adequate training and some degree of supervision to peers, to minimize instances where severe mental health conditions might be overlooked. In fact, Moir et al.19 reported that their study did not elucidate significant differences between mindfulness programs and peer support programs. Also, it was found that more extended peer training periods and population targeted interventions would be more valuable.19
This review is limited by the data reported. It is difficult to report adequately on the creation of an ideal peer-support program. Although the main goal of this paper was accomplished by providing a detailed outlook on what is currently available in the literature, the authors are unable to deliver an exemplary model for peer support program nor was this a goal of our study. Any attempt at creating a one-size-fits-all model would undermine program specific characteristics such as population, desired outcome, and available resources. Instead, this review elicited common and valuable attributes of published descriptions that might account for the success of the programs. Mainly, confidentiality is an abiding standard that should be highlighted as a foundation of any program. Furthermore, peer support programs should be a fully peer-led initiative. At last, programs should provide in-person as well as online sessions, and be adapted to their target audience to accommodate various different schedules and interests. In addition, the key aspect of confidentiality in peer support programs to protect the identity of the participants prevents the reporting on participants’ identity. As previously stated, included articles are more descriptive of their program than of its participants, and since this is very environment-specific, replicability becomes limited. Finally, there is significant inconsistency in these descriptions, as each individual author reports data differently.
For the future, both authors and readers would benefit if complete descriptions of each program’s goals and methodology were published. To increase knowledge translation, it would be beneficial for undergraduate programs or workplaces outside of healthcare to publish their peer support works, programs, and initiatives. The need for peer support is likely universal and should not be restricted to healthcare workers. In the end, peer support programs should address the reported gender gap in participation, perhaps by training more male peer supporters.
Conclusion
Peer support programs have been instituted for many types of populations and in multiple settings, as described by our article.
One crucial finding was the diversity of programs, varying drastically in their methodology and delivery. Moreover, there are some key aspects that should be included in future peer-support initiatives: explicit confidentiality, purely peer-delivered services, and a variety of delivery methods to fit the needs of all participants. In addition, research and program evaluations, when combined with participant feedback, can lead to adjustments and enhancements to current initiatives. Perhaps current and future innovative programs would benefit from reporting program efficiency, participant satisfaction, pre- and post-intervention scores of targeted variables, such as stress levels or feelings of belonging. A model that englobes efficient methodologies can be created, shared, and shaped to different populations and interventions.
In summary, within our targeted population, interventions such as peer support programs are prevalent and well described. Published articles provide a solid base for aspiring institutions to implement such support systems and could be further enhanced by making the steps towards the development of their program available to the public, as well as by providing specific but anonymous participant population information.
Acknowledgments
Acknowledgements: We thank Amanda Hodgson for her assistance and expertise on the databases search and Dr. Camila Pacheco-Pereira for the methodological guidance.
Appendix A.
Table 1.
Program description
| Author and year, Country |
Name of program Main goals |
Model of peer support | Program timeline/duration Organisers* Location* |
Participant demographics* | Peer training Supervision* | Support program attendees (n) | |
|---|---|---|---|---|---|---|---|
| In-Person | Calder-Sprackman et al, 201712 Canada |
Ice cream rounds – Improve resident wellbeing by create an environment for debriefing, to create resilience and protect from emotional burnout | Groups, in person | Since 2014, 1h sessions 3 or 4 times a year – Department of Medicine – University of Ottawa | Emergency residents | N/A | 40%-60% of residents (n= N/A) |
| Gilliland et al, 199011 USA |
Specialty Nursing Council - 1) networking and role development 2) increase visibility of nurses 3) provide continue education 4) provide community service | Groups, in person | 24 monthly meetings total - Organized by the Steering Committee | Specialty nurses | N/A | 30 to 75 | |
| Redwood et al, 200714 USA |
Stress Management Program – Facilitating adjustment of juniors medical students, aid in developing personal stress management skills, facilitate development of peer support program, identify 2nd year students as resource persons, provide training to medical students about behavioural sciences and health promotion | Group, in person | Yearly 1h/week program for 7 consecutive weeks, for the past 16 years – Department of Behavioural Sciences - Oklahoma State University Center for Health Sciences |
First year medical students with 2nd year students coleaders | Training and supervision provided by the department of behavioural sciences. Two psychologist faculty members serve as program coordinators | 1111, averaging 69.5 participants per year | |
| Sugumar et al, 201915 Australia |
Reduce stigma associated with mental health, improve self-care, increase confidence | Groups, in person | 5-session workshop – University of Tasmania | 4th year medical students | N/A | 20 out of 32 students of the cohort | |
| Wilson et al, 200416 Australia |
N/A – Meet needs of general practitioners for support, sharing of knowledge and skills, ongoing education and skills development, fostering of self-care. | Groups, in person | 3 workshops – the SA Division of General Practice – University of Adelaide | General practitioners | Training program and manual | 8 in workshops 1 and 2, 7 in workshop 3 | |
| Online | George et al 201317 USA |
Facebook Stress Management Group (not official name) – Reduce anxiety, enhance academic confidence, facilitate social connectedness | Online in groups, through Facebook (and also one in person but it was not documented) | No schedules, program available online at all times – program managed by faculty - Facebook | Anonymous medical students – mean 23 years old – 27 females (57%), 20 males (43%) n=47 |
N/A – Supervision by experts in counselling and information technology and monitoring by mental health professional | 47 online, 48 in person |
| Lau et al, 200713 Hong Kong |
Mental Health Support Group (MSG) – 1) Increase students’ mental health awareness 2) provide peer support network 3) create effective channels for help seeking | Online, group forum and email counseling | Group of 2nd and 4th year medical students – Online forum and e-mail | Medical students from years 1 to 4 | 15h training by qualified trainer and mental health promotion project – Supervision by senior teacher in clinical psychology | ~ 602 | |
| Mixed | Lane et al, 201818 USA |
The Washington University School of Medicine Clinician Peer Support Program (PCP) – Providing support to clinicians after adverse events and medical errors | Individualized, email or phone | 3 years program One meeting, or more if necessary - Washington University School of Medicine, WUSM Faculty Practice Plan – Barnes-Jewish Hospital |
6 (3.6%) Nurse practitioners/physician assistants, 4 (2.4%) certified registered nurse anesthetists, specialized physicians, 17 (10.3%) medical fellows, 68 (41.2%) medical residents, 70 (42.4%) faculty members | 2h small group live training sessions – Support of the Washington University School of Medicine, WUSM Faculty Practice Plan, and respective risk management and general counsel departments |
165 |
| Moir et al, 201619 New Zealand |
N/A – Reduce anxiety and depression scores and improve quality of life and resilience among medical students |
Groups, in person, or individualized upon request | 6 months University of Auckland | 2nd and 3rd year medical students Female=53% 20.9 average age (n = 77) |
24h of training over 8 weeks given by facilitators | 68 Intervention group (n = 68) Control (n = 77) |
|
| Shapiro et al, 20164 USA |
Center for Professionalism and Peer support – Encourage a culture that values and promotes mutual respect, trust, and teamwork | Groups, in person and individualized, online over e-mail | Since 2008, program consistently reaches out to peers and holds group sessions – Physicians – Brigham and Women’s Hospital | Physicians, core group of peer supporters | Training with key strategy of simulating scenarios | Over 220 outreach calls and over 240 physicians in group peer support sessions | |
| Not Specified | Robledo et al,20 2018 USA |
Peer Advocate (PA) program – Provide medical students with accessible non-threatening trained peer listeners | N/A | Throughout academic year – Medical students and Associate Dean for Student Affairs – Yale School of Medicine | Medical student Males=50.5% |
Existing PA and professional experts train new PA | 56 |
If provided. Legend: Legend: N/A=not available; USA= United States of America
Table 2.
Quality assessment for programs as per Appendix B.
| Author | Description Score (out of 28) | Program Description rating |
|---|---|---|
| Calder-Sprackman et al, 201712 | 11 | Fair |
| George et al, 201317 | 24 | Good |
| Gilliland et al, 199011 | 11 | Fair |
| Lau et al, 200713 | 14 | Fair |
| Lane et al, 201818 | 13 | Fair |
| Moir et al, 201619 | 24 | Good |
| Redwood et al, 200814 | 20 | Good |
| Robledo et al, 201820 | 12 | Fair |
| Shapiro et al, 20164 | 14 | Fair |
| Sugumar et al, 201915 | 12 | Fair |
| Wilson et al, 200416 | 10 | Fair |
Legend: N/A= Not available
Appendix B. Quality rating checklist
Program description rating:
Type of support………………………………………………………………………. □
Mode of support (f2f individual, f2f group, online)…………………………………. □
Duration/frequency of support……………………………………………………….. □
Manual used………………………………………………………………………….. □
Manual described…………………………………………………………………….. □
Clear description of how peer support is delivered………………………………….. □
Contact documented………………………………………………………………….. □
Documentation described…………………………………………………………….. □
Peers are trained……………………………………………………………………… □
Description of training……………………………………………………………….. □
Peers are supervised …………………………………………………………………. □
-
Description of supervision…………………………………………………………….. □
Subtotal (max 12) ………………………………………………………………………..
Circle one: Poor (0-4) Fair (5-8) Good (9-12)
Peer (providing support) description rating:
Peer recruitment………………………………………………………………………. □
Number of peers …………………………………..…………………………………. □
Who are the peers …………...……………………………………………………….. □
Age ……….………………………………………………………………………….. □
Sex ……………..…………………………………………………………………….. □
Marital status ……………………………………..………………………………….. □
Education …………………………………………………………………………….. □
-
Occupation ..…………....…………………………………………………………….. □
Subtotal (max 8) ………………………………………………………………………….
Circle one: Poor (0-2) Fair (3-5) Good (6-8)
Peer (receiving support) description rating:
Peer recruitment………………………………………………………………………. □
Number of peers …………………………………..…………………………………. □
Who are the peers …………...……………………………………………………….. □
Age ……….………………………………………………………………………….. □
Sex ……………..…………………………………………………………………….. □
Marital status ……………………………………..………………………………….. □
Education …………………………………………………………………………….. □
-
Occupation ..…………....…………………………………………………………….. □
Subtotal (max 8) …………………………………………………...…………………….
Circle one: Poor (0-2) Fair (3-5) Good (6-8)
Score for program description (max 12)………………………………………………….
Score for peer (giving support) description (max 8) ……………………………………..
Score for peer (receiving support) description (max 8) ………………………………….
Total (max 28)…………………………………………………………………………….
Circle one: Poor (0-7) Fair (8-14) Good (15-28)
Adapted from Hoey et al.10
Footnotes
Conflicts of Interest: All authors disclose the absence of any financial and personal relationships with other people or organizations that could inappropriately influence or bias their work or the results of this study.
Funding: This work was funded by Introduction to Research in Medical Pedagogy Student Bursary, by the Francophone Affairs at the University of Ottawa Faculty of Medicine (https://med.uottawa.ca/affaires-francophones/appui-recherche/bourses-recherche-pedagogie-medicale). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Solomon P. Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr Rehabil J. Published online 2004. 10.2975/27.2004.392.401 [DOI] [PubMed] [Google Scholar]
- 2.Dennis CL. Peer support within a health care context: A concept analysis. Int J Nurs Stud. Published online 2003. 10.1016/S0020-7489(02)00092-5 [DOI] [PubMed] [Google Scholar]
- 3.Van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. BMJ Qual Saf. 2008;17(4 PG-249-252):249-252. 10.1136/qshc.2007.025536. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9 PG-1200-1204):1200-1204. 10.1097/ACM.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 5.Services AH. It’s Our BusIness.; 2020.
- 6.Chisholm B. Promoting peer support among teachers. Published online 1994:174-184. 10.4324/9781315003658-15 [DOI] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J AD. PRISMA 2009 Checklist PRISMA 2009 checklist. PLoS Med. Published online 2009. 10.1371/journal.pmed1000097 [DOI] [Google Scholar]
- 8.Veritas Health Innovation . Covidence systematic review sofware. Covidence.
- 9.Davies KS. Formulating the evidence based practice question: A review of the frameworks. Evid Based Libr Inf Pract. Published online 2011. 10.18438/B8WS5N [DOI] [Google Scholar]
- 10.Hoey LM, Ieropoli SC, White VM, Jefford M. Systematic review of peer-support programs for people with cancer. Patient Educ Couns. Published online 2008. 10.1016/j.pec.2007.11.016 [DOI] [PubMed] [Google Scholar]
- 11.Gilliland K, Tosch P, Hussey L, et al. Specialty nursing council: a peer support group for nurses in independent roles. Clin Nurse Spec. 1990;4(1 PG-38-42):38-42. NS- [PubMed] [Google Scholar]
- 12.Calder-Sprackman SM, Kumar T, Sampsel K. Ice Cream Rounds: the adaptation and implementation of a peer-support wellness rounds in an emergency medicine residency training program. Can J Emerg Med. 2017;19(Supplement 1 PG-S42):S42. 10.1017/cem.2017.104 [DOI] [PubMed] [Google Scholar]
- 13.Lau KS, Siong KH, Tang HY, et al. An innovative web-based peer support system for medical students in Hong Kong. Med Teach. 2007;29(9-10 PG-984-986):984-986. 10.1080/01421590701551748 [DOI] [PubMed] [Google Scholar]
- 14.Redwood SK, Pollak MH. Student-led stress management program for first-year medical students. Teach Learn Med. 2007;19(1 PG-42-6):42-46. 10.1080/10401330709336622. [DOI] [PubMed] [Google Scholar]
- 15.Sugumar D, Fleming O, Ogden K. A mental health programme for medical students. Clin Teach. 2019;16(4 PG-352-355):352-355. 10.1111/tct.13052 [DOI] [PubMed] [Google Scholar]
- 16.Wilson I, Howell C. Small group peer support for GPs treating mental health problems. 2004;(PG-). NS - [PubMed]
- 17.George DR, Dellasega C, Whitehead MM, Bordon A. Facebook-based stress management resources for first-year medical students: A multi-method evaluation. Comput Human Behav. 2013;29(3 PG-559-562):559-562. 10.1016/j.chb.2012.12.008 [DOI] [Google Scholar]
- 18.Lane MA, Newman BM, Taylor MZ, et al. Supporting clinicians after adverse events: development of a clinician peer support program. J Patient Saf. 2018;14(3 PG-e56):e56. 10.1097/PTS.0000000000000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moir F, Henning M, Hassed C, Moyes SA, Elley CR. A peer-support and mindfulness program to improve the mental health of medical students. Teach Learn Med. 2016;28(3 PG-293-302):293-302. 10.1080/10401334.2016.1153475. [DOI] [PubMed] [Google Scholar]
- 20.Robledo-Gil T, XM G, Horien C, MA H, Encandela J, NR A. Utilization and Effectiveness of a Peer Advocate Program for Medical Students. Acad Psychiatry. 2018;42(1 PG-168-170):168-170. 10.1007/s40596-017-0790-5 [DOI] [PubMed] [Google Scholar]
- 21.Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: current insights. Adv Med Educ Pr. 2018;9(PG-323-333):323-333. 10.2147/AMEP.S137384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stubbs B, Williams J, Shannon J, Gaughran F, Craig T. Peer support interventions seeking to improve physical health and lifestyle behaviours among people with serious mental illness: a systematic review. Int J Ment Health Nurs. Published online 2016. 10.1111/inm.12256 [DOI] [PubMed] [Google Scholar]
- 23.Hu J, Wang X, Guo S, et al. Peer support interventions for breast cancer patients: a systematic review. Breast Cancer Res Treat. Published online 2019. 10.1007/s10549-018-5033-2 [DOI] [PubMed] [Google Scholar]
- 24.Shapiro, Jo. Harvard Medical School Department of Otolaryngology. https://oto.hms.harvard.edu/people/jo-shapiro [Accessed Aug 16, 2020].
- 25.Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual patient Saf. 2014;40(4 PG-168-77):168-177. 10.1016/s1553-7250(14)40022-9. [DOI] [PubMed] [Google Scholar]
- 26.Panella M, Rinaldi C, Leigheb F, et al. The determinants of defensive medicine in Italian hospitals: The impact of being a second victim. Rev Calid Asist. Published online 2016. 10.1016/j.cali.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 27.Wu AW. Medical error: The second victim. Br Med J. Published online 2000. 10.1136/bmj.320.7237.726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta K, Lisker S, Rivadeneira NA, Mangurian C, Linos E, Sarkar U. Decisions and repercussions of second victim experiences for mothers in medicine (SAVE DR MoM). BMJ Qual Saf. Published online 2019. 10.1136/bmjqs-2018-008372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO | Suicide rates (per 100 000 population) . WHO. Published online 2018. http://www.who.int/gho/mental_health/suicide_rates_male_female/en/ [Accessed Aug 16, 2020].
- 30.Gillard SG, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. 2013;13(1):188. 10.1186/1472-6963-13-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu Y, Fix ML, Hevelone ND, et al. Physicians' Needs in coping with emotional stressors: the case for peer support. Arch Surg. 2012;147(3):212–217. 10.1001/archsurg.2011.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chan AO, Chan YH, Kee JP. Improving resistance and resiliency through crisis intervention training. Int J Emerg Ment Health. 2012;14(2 PG-77-86):77-86. NS- [PubMed] [Google Scholar]


