Abstract
Background
On March 11, 2020 the World Health Organization declared the novel coronavirus SARS-CoV-2 disease (COVID-19) a global pandemic. We sought to understand impact of COVID-19 on learner wellness at a large tertiary care academic institution to inform the future development of learner wellness interventions during the COVID-19 pandemic.
Methods
A cross-sectional, internet-based survey collected quantitative and qualitative data from learners April-June 2020. Descriptive statistics and univariate analyses were reported for quantitative data. Open-ended, qualitative responses were analyzed deductively using thematic analysis.
Results
Twenty percent of enrolled learners in that faculty of medicine (540/2741) participated including undergraduate [Bachelor’s] students (25.7%), graduate [science] students (27.5%), undergraduate medical students (22.8%), and postgraduate resident physicians (23.5%). We found that learner wellness across all stages of training was negatively impacted and the ways in which learners were impacted varied as a result of their program’s response to the COVID-19 pandemic.
Conclusions
Learners in health sciences and medical education report worsening well-being because of the programs and the systems in which they function with the added burden of the COVID-19 pandemic. Future interventions would benefit from a holistic framework of learner wellness while engaging in systems thinking to understand how individuals, programs and respective systems intersect. The importance of acknowledging equity, diversity and inclusion, fostering psychological safety and engaging learners as active participants in their journey during a pandemic and beyond are key elements in developing wellness interventions.
Abstract
Contexte
Le 11 mars 2020, l’Organisation mondiale de la santé a déclaré que le nouveau coronavirus SRAS-CoV-2 (COVID-19) était pandémique. Nous avons tenté de cerner l’impact de la COVID-19 sur le bien-être des apprenants dans un grand centre universitaire de soins tertiaires afin d’étayer le développement futur d’interventions en faveur du bien-être des apprenants en contexte de pandémie.
Méthodes
Une enquête transversale par sondage en ligne, menée entre les mois d’avril et juin 2020, a permis de recueillir des données quantitatives et qualitatives auprès des apprenants. Des statistiques descriptives et des analyses univariées ont été présentées comme données quantitatives. Les réponses ouvertes, qualitatives, ont été analysées de manière déductive par le biais d’une analyse thématique.
Résultats
Vingt pour cent des étudiants de la faculté de médecine (540/2741) ont participé, dont 25,7 % étaient inscrits au premier cycle (baccalauréat), 27,5 % au deuxième cycle (sciences), 22,8 % au premier cycle en médecine et 23,5 % étaient résidents. Nous avons constaté que la pandémie a négativement affecté le bien-être des apprenants à tous les niveaux de formation et que les effets précis sur les étudiants pouvaient varier en fonction de la réponse de leur programme à la situation sanitaire.
Conclusions
Les étudiants en médecine et en sciences de la santé signalent une détérioration de leur bien-être liée aux programmes et aux systèmes dans lesquels ils évoluent, auxquels s’ajoute le fardeau supplémentaire de la pandémie de la COVID-19. Il conviendrait de définir les interventions futures sur la base d’un cadre holistique du bien-être des apprenants tout en adoptant une réflexion systémique pour appréhender l’entrecroisement entre individus, programmes et systèmes. Reconnaître l’importance de l’équité, de la diversité et de l’inclusion, favoriser la sécurité psychologique et assurer la participation active des apprenants dans leur parcours pendant la pandémie et au-delà, constituent des éléments clés dans l’élaboration d’interventions au profit de leur bien-être.
Introduction
Learners in Canadian medical schools have significantly higher rates of psychological distress, mood disorders, and lifetime suicidal ideation compared to university students in non-medical programs.1 Globally, medical learners experience significantly increased rates of burnout and psychiatric morbidity.2-4 Educators and learners alike cite concerns about the effects of health sciences training and medical education on learner well-being,5-7 as well as the lack of standards for how best to structure and optimize wellness initiatives for learners to thrive in their training.8-13
On March 11, 2020 the World Health Organization (WHO) declared the novel coronavirus SARS-CoV-2 disease (COVID-19) a global pandemic.14 The impact of the COVID-19 pandemic on learners continues to evolve rapidly and impact learners in various ways. Without targeted interventions, consequences for learner wellness may become more prevalent and severe.10, 15
To address this concern, we conducted a needs assessment to understand learner well-being in training environments disrupted by the COVID-19 pandemic. The aim of our study was to inform the development of learner wellness interventions at academic institutions such as medical schools in order to promote wellness and enhance well-being among the next generation of health care scientists and professionals during the COVID-19 pandemic.
Methods
Study design and setting
A cross-sectional survey was designed to collect data from all learners enrolled at the accredited Cumming School of Medicine, University of Calgary, in Calgary, Alberta, Canada (N = 2741). Participants were invited through e-mail correspondence from the Dean of Medicine, Assistant or Associate Deans, program administrators or directors, and student-led organizations. All learners were sent follow-up email invitations at weekly intervals for eight weeks.
Study respondents
Four groups of learners at the Cumming School of Medicine participated in this study: undergraduate students (i.e., Bachelor of Health Sciences [BHSc] and Bachelor of Community Rehabilitation [BCR] students); graduate science students (i.e., MSc and PhD students); undergraduate medical students; and postgraduate resident physicians. Information on program requirements are available at the Cumming School of Medicine webpage.16
Some participants were learners in multiple groups (e.g., students in the combined MD-PhD program). To prevent duplication and to gain as much comprehensive data as possible, these individuals were assigned to the learner group they were enrolled in at the start of the COVID-19 pandemic (on March 11, 2020). Data were collected between April 07, 2020 and June 02, 2020.
Data collection
An online survey was developed based on recommendations from the International Association for Medical Education in order to develop synthetic frameworks to attempt to view medical learners holistically, focusing on real-world activities and performance.17 Survey items were informed by the World Health Organization-Five (WHO-5) Well-Being Index,18 the Wellness Innovation Scholarship for Health Professions Education and Health Sciences (WISHES) framework domains.19 We also explored factors impactful (i.e., individual, program, systematic) to learners’ training based on comprehensive scoping review of interventions for improved wellness of Canadian learners in medical schools (under peer-review). The assessment tools were chosen specifically to inform the development of future wellness interventions for medical learners that could be targeted to subjective learner well-being (i.e, informed from the WHO-5), validation for the wellness domains (i.e., informed from the WISHES wellness domains)1, and factors impactful to learners’ education during the COVID-19 pandemic. See Supplemental Table 1 for descriptors of WISHES wellness domains and impactful factors.
Table 1.
Scales and observational assessments used in the internet-based survey
| Assessment Tool or Questions | Intended Use | Categories or Questions | Score Range or Selections | Rating | Comments |
|---|---|---|---|---|---|
| Impactful Factors | Understand the factors impactful to learners’ education during the COVID-19 pandemic20 | Factors impactful to thrive in education during the COVID-19 pandemic Factors impactful to struggle in education during the COVID-19 pandemic |
Individual factors Program factors System factors Other factors |
N/A | Prompted to select all that apply |
| World Health Organization Well-Being Index (WHO-5) | Measure subjective learner well-being21 | Rate five positively phrased statements considering the last 14 days in the COVID-19 pandemic from 5 (all of the time) to 0 (none of the time) | Raw score translated to percentage; scale range from 0-100 | Lower scores indicate lower well-being while higher scores indicate higher well-being | The WHO-5 has high clinimetric validity and has been applied across a wide range of study fields as a screening tool for depression22-24 |
| Wellness Innovation Scholarship for Health Professions Education and Health Sciences (WISHES) domains | Assess the impact of COVID-19 on wellness domains (i.e., social, mental, physical, intellectual, occupational) | Rate if the COVID-19 pandemic negatively impacted a particular wellness domain in the last 14 days from 5 (strongly disagree) to 1 (strongly agree) | Raw score translated to percentage scale range from 20 (all domains negatively impacted) to 100 (no domains negatively impacted) | Lower scores indicate lower wellness while higher scores indicated higher wellness | No assessment measure of wellness domains is considered “gold standard” and evidence is insufficient to support clinical utility of a single particular wellness instrument25 |
The survey consisted of discrete answer questions (including Likert-scale items) to collect quantitative data and open-ended responses to collect qualitative data. The survey was revised for brevity (i.e., conciseness and exact use of words) and clarity (i.e., to be coherent and intelligible), and based on feedback from pilot testing with three learners enrolled at the Cumming School of Medicine. Given the rapid transition to online learning at our institution and the need to distribute the online survey quickly in order to capture learner well-being status at the start of the pandemic, a full pilot study was not feasible. Responses from pilot testing were not included in final analyses. The final version of the survey contained 21 questions divided into three sections: 1) demographics; 2) factors impactful for learners to thrive or struggle in their training during the COVID-19 pandemic; and 3) assessment of learner well-being and wellness domains with regard to the COVID-19 pandemic. A summary of the measurement scales and validated observational assessments tools used in the survey are provided in Table 1. All questions and possible responses for the online survey are available in Appendix A.
Ethical considerations
This study received ethical approval from the University of Calgary Conjoint Health Research Ethics Board (REB20-0117). Participation in this study was voluntary, and informed consent was obtained from all participants prior to beginning the online survey. Learners did not receive any incentives or compensation for their participation.
Data analysis
We used descriptive statistics to assess learner demographics and questions with discrete answer choices. Independent t tests were used to examine differences between dichotomized variables (e.g., visible ethnic minority, diagnosis of clinical disability). Total scores were calculated for the WHO-Five Well-Being Index and the WISHES domains as well as mean scores with confidence intervals (CI) for each group,18 to allow for direct comparison between assessment tools and because scales measuring subjective wellness outcomes (e.g., health-related quality of life) are conventionally translated to a percentage scale. Table 1 provides information on the possible range and calculation method for how total scores were computed.
To examine group differences (e.g., gender, learner program) we used an Analysis of Variance (ANOVA) with Bonferroni corrections to account for post-hoc analyses. Using Promax rotation, we performed an exploratory factor analysis on the wellness domains assessment tool to examine item loading as a way of assessing construct validity. Reliability analyses were performed for the WHO-Five and WISHES wellness domains by calculating a Cronbach’s alpha. Quantitative data were analyzed using STATA IC 15 (StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
Two independent investigators analyzed open-ended responses in duplicate using a deductive thematic approach to qualitative analysis.26 A deductive approach entailed the application of themes that we expected based on our existing knowledge of a multi-dimensional construct of well-being from a previous scoping review (under review). Furthermore, we applied the WISHES wellness domains, factors impactful (at the levels of individual, program and system) to establish validity evidence for the framework. We also coded the data with respect to the categories of content, format, process and outcome of learner concerns to inform the development of learner wellness interventions. Codes that did not fit within the existing framework and categories were constructed and all coding was reviewed on an ongoing basis to promote consistency between investigators, and peer debriefing was used to ensure adequate sampling and thematic representation.27 Discrepancies were resolved by discussion and negotiated to establish a final coding scheme. Using an engaged scholarship approach;28,29 two learners graduated from or currently representing each of the learner programs (S.C., A.B., R.H., K.M., M.P., S.S., A.K.) coded and analyzed full data independently using NVivo Qualitative Data Analysis Software Version 12 (QSR International). Dyads had an average interrater agreement of 80.4% (dyad-specific agreement provided in Supplemental Table 3) and discrepancies were resolved by in-depth discussion. Insightful excerpts and comments from respondents are provided to highlight potential program-specific targets for wellness interventions during the COVID-19 pandemic.
Table 3.
Assessments of learner well-being and wellness domains negatively impacted
|
WHO-Five Well-Being Indexa Cronbach α=0.86 Bartlett test of sphericity p-value<0.001 Kaiser-Meyer-Olkin Sample Adequacy=0.84 |
Wellness Domains Negatively Impactb,c,d Cronbach’s α=0.74 Bartlett test of sphericity p-value<0.001 Kaiser-Meyer-Olkin Sample Adequacy=0.76 |
||||||
|---|---|---|---|---|---|---|---|
| N (%) | Mean (SD) | 95% CI | p-valuee | Mean | 95% CI | p-valuee | |
|
Gender Man Woman Non-Binary |
381/540 88 (23.10%) 285 (74.80%) 8 (2.10%) |
54.45 (20.91) 47.72 (19.66) 40.5 (21.75) |
50.07-58.84 45.43-50.01 25.38-55.62 |
0.01* |
49.41 (19.46) 48.60 (16.41) 31.00 (13.82) |
45.33-53.49 46.69-50.51 21.40-40.60 |
0.01* |
|
Visible Minorityf Yes No |
379/540 113 (29.82%) 266 (70.18%) |
50.41 (20.86) 48.45 (19.92) |
46.55-54.27 46.05-50.85 |
0.39 |
47.22 (18.52) 48.96 (16.76) |
43.80-50.65 46.94-50.93 |
0.37 |
|
Clinically diagnosed conditiong Yes No |
380/540 197 (51.84%) 183 (48.16%) |
45.54 (19.37) 52.90 (20.42) |
42.83-48.26 49.93-55.86 |
<0.01 |
46.94 (11.31) 50.05 (16.22) |
44.69-49.23 47.40-50.70 |
0.08 |
|
Program of training Undergraduate Education Graduate Science Educationh Undergraduate Medical Education Postgraduate Medical Education |
381/540 97 (25.46) 110 (28.87) 79 (20.73) 94 (24.67) |
47.42 (16.98) 46.32 (21.86) 57.27 (18.53) 47.36 (21.14) |
44.00-50.84 42.19-50.45 53.12-61.42 43.03-51.69 |
<0.01* |
46. 14 (14.34) 47.85 (17.57) 52.30 (18.41) 48.21 (18.46) |
43.25-49.03 44.53-51.17 48.18-56.42 44.43-51.99 |
0.12 |
Range from 0 (absence of well-being) to 100 (maximal well-being)
Range from 20 (all domains negatively impacted) to 100 (no domains negatively impacted)
Pearson correlation coefficient with WHO-Five indicates strong correlation between well-being and impacted domains of wellness (r=0.61)
Exploratory factor analysis using Promax rotation (i.e., construct validity) showed 1-factor solution accounting for 50% of variance with factor loadings greater than 0.6 for each of the five questions
t-test, visible minority and clinically diagnosed condition; analysis of variance, gender and program
Non-Caucasian in race or non-white in colour
Pain, flexibility, mobility, mental health, seeing, hearing, dexterity, learning or memory
Master of Science or Doctor of Philosophy
CI, confidence interval; N, number of respondents; SD, standard deviation; %, proportion of respondents; *, statistically significant after Bonferonni correction
Results
To inform the development learner wellness interventions, results are separated according to learner program.
A total of 540 learners completed the survey between April 07, 2020 (i.e., 27 days after the start of the pandemic) and June 02, 2020 (i.e., 83 days after the start of the pandemic), representing 19.7% of all learners in the medical school. Our sample was comprised of 137 (25.4%) undergraduate (bachelor’s) students [101 BHSc students, 36 BCR students]; 149 (27.6%) graduate science education students; 122 (22.6%) medical students; and 125 (23.1%) resident physicians. Seven medical learners did not indicate program and were excluded from analyses. We obtained 70.9% (383/540) complete data, which was deemed satisfactory given timing of survey distribution with regard to the “peak” of the pandemic in our geographic location30 and the number of substantial alterations in learners’ personal and professional lives at that time. Precaution should be exercised when interpreting the data given respondents provided data at a single point in time (i.e., completed the survey once).
The majority of respondents were women (72.6%) and not a visible minority (i.e., Caucasian/white in color) (69.2%) (Table 2). Nearly half of learners (48.5%) were diagnosed clinically with a condition relating to pain, flexibility, mobility, mental health, seeing, hearing, dexterity, learning or memory. Overall, learners most frequently (95.8%) reported individual (self) factors as impactful for them to thrive in their training, whereas, both individual (58.8%) and program factors (55.5%) were frequently reported as impactful to lead learners to struggle.
Table 2.
Learner demographics
| Group | All Programs N (%) |
Undergraduate Bachelor Education N (%) |
Graduate Science Education N (%) |
Undergraduate Medical Education N (%) |
Postgraduate Medical Education N (%) |
|---|---|---|---|---|---|
|
Enrolled learners Respondents (%)a |
2741 540 (100%) |
669 137 (25.70%) |
719 149 (27.49%) |
487 122 (22.89%) |
866 125 (23.45%) |
|
Gender Man Woman Non-Binary |
540/540 133 (24.63%) 392 (72.59%) 15 (2.78%) |
137/137 16 (11.68%) 117 (85.40%) 4 (2.92%) |
149/149 42 (28.19%) 99 (66.44%) 8 (5.37%) |
122/122 33 (27.05%) 88 (72.13%) 1 (0.82%) |
125/125 40 (32.00%) 83 (66.40%) 2 (1.60%) |
|
Visible Minorityb Yes No |
536/540 165 (30.78%) 371 (69.22%) |
137/137 52 (37.96%) 85 (62.04%) |
148/149 39 (26.35%) 109 (73.65%) |
121/122 35 (28.93%) 86 (71.07%) |
124/125 39 (31.45%) 85 (68.55%) |
|
Clinically diagnosed conditionc Yes No |
537/540 260 (48.51%) 276 (51.49%) |
137/137 73 (53.28%) 64 (46.72%) |
148/149 74 (50.00%) 74 (50.00%) |
120/122 62 (51.67%) 58 (48.33%) |
125/125 48 (38.40%) 77 (61.60%) |
Seven respondents did not indicate enrolled program
Non-Caucasian in race or non-white in colour
Pain, flexibility, mobility, mental health, seeing, hearing, dexterity, learning or memory
N, number of respondents; %, proportion of respondents
In terms of validity evidence, reliability of the WHO-Five Well-Being Index and WISHES wellness domains assessment tools were 0.86 and 0.74, respectively, indicating a satisfactory level of internal consistency (Table 3). Our assessment of construct validity for the WHO-Five Well-Being Index and WISHES wellness domains was also satisfactory. The exploratory factor analysis using Promax rotation (i.e., construct validity) showed 1-factor solution accounting for 50% of variance with factor loadings greater than 0.6 for each of the five questions.
Significant group differences in WHO-Five Well-Being Index Scores were detected between genders (p-value=0.01), learners with clinically diagnosed conditions (p-value<0.01) and training programs (p-value<0.01). Wellness domains negatively impacted by the COVID-19 pandemic differed only between groups based on gender (p-value=0.01). The distribution of responses for wellness domains negatively impacted is provided in Supplemental Table 2.
The qualitative results provided additional insight as themes between learner concerns (content, format, processes, outcomes) impactful factors (individual, program, system), and their subjective assessment of wellness domains during the pandemic. Themes from the seven open-ended responses are summarized in Supplemental Table 3.
Undergraduate students
Undergraduate students reported individual factors primarily impacted their ability to thrive (93.6%) or led them to struggle (64.9%) in their training during the COVID-19 pandemic. When asked to rate their well-being within the last 14 days, respondents reported neutral well-being (WHO-5 mean score 47.42, 95% CI 44.00-50.84). Respondents reported their social, mental, physical, and intellectual wellness had been negatively impacted because of the COVID-19 pandemic. When asked about their greatest concerns, undergraduate learners regarded mental wellness, intellectual wellness (individual outcomes, program processes, program outcomes) and a new theme surrounding financial wellness (funding of individuals, programs and systems) emerged that did not fit within the deductive coding framework. These learner’s comments summed up the group’s ideas:
The [University of Calgary] offered a pass/fail option this semester… As helpful as this option may seem, I am worried that if I do take the “credit received” option, it will not look good to medical schools when I apply in later years… will negatively impact my chances of getting accepted into medical school. Participant 237
With the ongoing pandemic, I will not be able to interact and learn onsite skills through practicum placements and complete my degree to its fullest potential at this point in time. I also really value the location of the learning facilities on campus such as the library and study spaces which are currently unavailable. Participant 128
Graduate students
Learners in master’s or doctoral programs related to health and medical sciences described nearly exclusively individual factors as impactful to thrive in their training (96.4%), while both individual (65.4%) and program related factors (50.5%) led them to struggle during the COVID-19 pandemic. Respondents subjective well-being over the last 14 days appeared to be waning (WHO-5 mean score 46.32, 95% CI 42.19-50.45). Three major themes emerged when participants were asked to list greatest wellness concerns related to the COVID-19 pandemic:
1) Program processes with respect to intellectual wellness (how programs delivered learning); and 2) Systems outcomes with respect to occupational wellness (career outcomes mandated by the higher education/healthcare systems or intersections of both). Again, a third theme of financial wellness (funding of individuals, programs and systems) emerged that did not fit within the deductive coding framework.
I fear that I will be unable to meet current program, and production deadlines… Though a leave of absence is possible, that would also entail pausing my stipend which would not be financially responsible… Cancellation of school and daycare has eliminated much of my working time and I am prioritizing my children's health and wellness over my learning, but this does come at the cost of my learning capabilities. Participant 53
Time lost in research. External scholarships not being extended… Pressure to maintain productivity. PPE when coming into work by the university. Better campus network connection… Participant 123
Medical students
There was nearly universal agreement among medical students that individual factors were most impactful for them to thrive during the COVID-19 pandemic (98.7%).
I find the following strategies helpful: (1) drawing on resilience from facing previous challenges, (2) engaging classmates/friends with whom I can learn material, (3) sharing struggles with family and friends, (4) feeling confident I will be supported by sharing honestly with researchers my concerns, believing that this will help the school/program/educational system to be more proactive, (5) openness to new types of learning formats offered by my program and academic institution, (6) setting individual realistic goals. Participant 342
Medical students acknowledged their recent well-being to be stable (WHO-5 mean score 57.27, 95% CI 53.12-61.42), despite commenting that their general well-being, in addition to their social, mental, physical and intellectual wellness had been negatively impacted as a result of the COVID-19 pandemic.
We really don't know what the repercussions for our already condensed medical [education] program are going to be regarding pre-clerkship electives time, clerkship itself and even residency. Participant 51
Missing out on the last bit of clinical rotation, which is relevant to my residency program... Even though this time is a break, it's not the usual post medical school break. There is some concern about starting residency without really feeling rested since all normal activities and celebrations are cancelled. Participant 270
Resident physicians
The majority (97.8%) of resident physicians reported individual factors as impactful to thrive in their training. Resident physicians frequently indicated program (53.2%) and system (69.6%) factors negatively impacted them. The WHO-5 mean score for resident physicians was 47.36 (95% CI 43.05-51.69). The greatest concerns among resident physicians related to their physical wellness (i.e., dying), intellectual wellness (program outcomes and system outcomes) and occupational wellness (program processes and system processes). Residents were substantially impacted by the COVID-19 pandemic in several, diverse ways for example, they reported concerns at the systemic level.
We will be called to serve and not treated equally with our staff counter parts. I have also seen programs who have been unkind to their residents, which gives me a great deal of stress. Watching my colleagues be drafted to the front lines from educational electives to mandatory rotations and lose their vacation but also be told they are no longer able to do extenders shows that they are not respected. The loss of autonomy has been acutely felt and removing additional freedoms is insult to injury. Participant 270
Learner coping and need for additional wellness supports
When asked to describe tools or strategies helpful to coping with the COVID-19 pandemic, respondents from all programs described these major themes: social wellness, mental wellness, and physical wellness, Individual strategies were most commonly discussed.
It’s a long journey to wellness. You would have had to have started this [wellness] journey before the pandemic hit in order to fully cope with it… So, what do we need to be doing if we have had tunnel vision on our career/education and have invested no time in anything else? I think this is a perfect opportunity to get in touch with other parts of yourself. Listen to the side of yourself that has been ignored for so long. Participant 111
Most learners appreciated the goodwill and timely efforts of their program and the academic institution but felt inadequately prepared to continue their program to meet national standards and training requirements. Despite a decline in May 2020 of new COVID-19 cases in Alberta, Canada (Figure 1), learners persist to report their well-being as below the 50th percentile, indicating that without targeted interventions poor learner well-being is unlikely to improve over time. A dominant theme was the lack of control over individual well-being which led them to struggle in their training during the COVID-19 pandemic. Recommendations for additional wellness support included mental support (for individuals), intellectual support (for programs), financial support (from the system).
Figure 1.
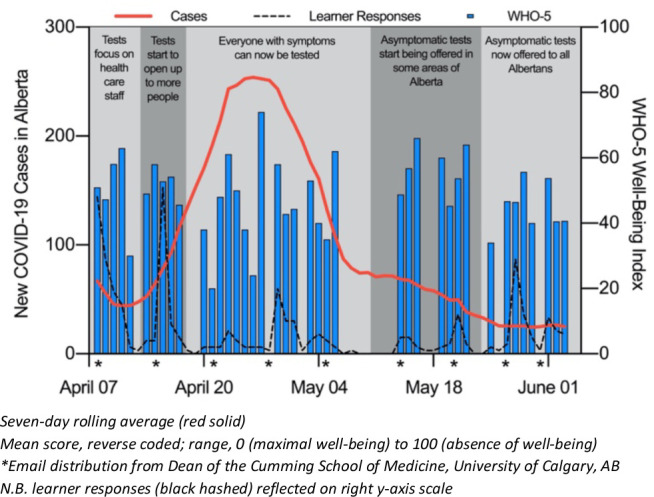
New COVID-19 cases in Alberta, Canada1 with WHO-Five Well-Being Index2
I would like to have professors offer us time to process the changes before assigning new deadlines. I would like to be offered financial assistance or support… as many students have received no deductions from our tuition payments. I have had to rely on self-learning which should not cost the same amount of money… Participant 237
The university should have a specific townhall for each of its [medical education] programs to clearly communicate what expectations are for graduate students at this time. Participant 109
Life balance! We are trapped in a career that, if the previous generation had to suffer through inhumane work-conditions, justifies the next generation not having to. There has to be a line drawn in the sand where we must say that physician lives have value above the needs of their patients. Participant 98
Discussion
The results of this study explore the impact of the COVID-19 pandemic on learners at a single academic medical institution in Canada using a holistic framework for wellness. We found the ways in which learners were impacted varied as a result of their program’s response to the COVID-19 pandemic. We found neutral well-being scores for learners overall, and as such, we must interpret these results with caution taking-into-account that our response rate was 20%.
We did find significant differences in well-being scores with respect to program, gender identity and a clinical diagnosis. Learners who identified as women or non-binary had lower scores than men and those with a clinically diagnosed condition had lower well-being scores than those learners that did not. Further exploration of the impact of program, gender identity as well as the presence of a clinically diagnosed condition on learner well-being is needed.
The themes identified across learner programs are consistent with what is known currently on learner well-being—medical schools are called to help their progressively diverse student cohorts to effectively enhance self-actualization and professional development both during training and as future health care professionals.5,12, 15, 31,32,33
From our needs assessment we uncovered three potential targets within two wellness domains for program-specific wellness interventions during the COVID-19 pandemic. These targets include: (1) the processes (e.g., learning methodologies, learning responsibilities) and (2) outcomes (e.g., educational deliverables, career trajectories) related to intellectual and occupational wellness domains respectively, as well as (3) the processes (e.g., informal check-ins, coffee chat hours) for maintaining social wellness.
In designing new wellness interventions to respond to the COVID-19 pandemic and learner well-being in general, we suggest that six main recommendations that future wellness interventions consider. First, a holistic approach to wellness that acknowledges a “one-size fits all” approach may not work for all learners is important to consider given that each learner has their own lived experience. Second, individual, program and system factors must be accounted when designing wellness interventions. The onus cannot fall on individual learners often subjected to dysfunctional program and system factors that may influence well-being. For example, mindfulness meditation and yoga as individual level interventions can only go so far in maintaining learner wellness; program and system-level interventions also have a role in modelling and supporting learner wellness. Third, during the COVID-19 pandemic and beyond, consider maintaining social wellness among learners equally as important as teaching and training since learning can occur through social interaction. Fourth, ensure safe learning environments by fostering psychological safety so that learners can share their lived experiences, which can help normalize disclosure and help seeking. Fifth, consider equity diversity and inclusion principles such as intersectionality in relation to well-being. For example, gender identity, clinical diagnoses, financial status and other socio-demographic variables warrant further consideration. Last, engage learners as active participants in their learning process. As key stakeholders, learners may have innovative solutions that will inform each other as well as program and system level interventions thereby creating a community of practice.
Challenges to implementation
In order to address these needs among learners, new wellness interventions34 will need to be developed while acknowledging the program and systems in which the learner functions (higher education, healthcare or an intersection of both).
The quantitative and qualitative data converged showing many learners are experiencing hardships in several wellness domains. Thus, given that most existing opportunities are optional35 and do not acknowledge a holistic framework for learner wellness,36 it is unlikely simply changing existing wellness initiatives to be mandatory would be sufficient to meet the increased wellness demands from learners due to the COVID-19 pandemic.37
The COVID-19 pandemic continues to evolve rapidly and continues to impact learners in various ways. Our data was collected from each learner at a single point in time at the start of the first wave of the pandemic. Sequential phases of surveillance to determine the wellness trajectories among learners may require targeted interventions at different time points.38 What works at one stage of medical education may not be helpful at the next stage of training.38 For learners, the impact of the COVID-19 pandemic on medical education is not to be challenged with a gallant sprint; adversities on learners will continue to persist long after the current pandemic is no longer the prime concern.19
Finally, an additional challenge to note is regarding the feasibility and acceptability of online wellness interventions. Based on our data we posit that online wellness interventions might be more successful if interventions include a socially-distanced in-person component, in addition to components aimed to enhance intellectual and occupational wellness. Still, many questions remain unanswered and much work is required to fully understand the utility and long-term impact of online wellness interventions, especially in most at-risk learners. Questions for future inquiry include identifying the synchronicity of online wellness interventions, determining best modalities to promote online wellness and most effective methodologies to implement online interventions. We suggest that developing an operational definition for wellness associated with a core outcomes set of well-being measures related to specific learner programs might help to develop and implement future program-specific, online interventions.
Limitations
The experiences and lessons learned from the COVID-19 pandemic can serve as a foundation to design wellness interventions for medical learners during a pandemic and beyond. Nonetheless, there are numerous limitations to consider surrounding the applicability and generalizability of the conclusions drawn from this research. External validation of the WISHES wellness domains in other learner cohorts would contribute validity evidence to the WISHES framework and assessment tool. However, well-being among learners is universal to all medical schools10 and the responses gathered herein may be relevant to learners in other contexts. Due to the timing of the “peak” of the first wave of the pandemic in our geographic location and the number of substantial alterations in learners’ personal and professional lives at that time, our low response rate indicates that input may be missing from an important cohort of learners—learners most impacted with poorest well-being. Another limitation is regarding the use of an internet-based survey, as limitations with this format can result in misinterpretation and missed perspectives, failing to capture critical information. We did not assess academic performance and achievement prior to the COVID-19 pandemic, which may have confounded student status. Finally, through impacts on wellness may differ according to learner disabilities and commitments outside of school (e.g., parents, caregivers), our study was not powered to examine differences between visible and non-visible minorities and perspectives from visible minorities were under-represented generally. This may be relevant as differences in cultural values such as family responsibilities and social support networks may influence learners’ well-being.
Conclusions
Learners in health sciences and medical education report worsening well-being because of the programs and the systems in which they function with the added burden of the COVID-19 pandemic. Future interventions would benefit from a holistic framework of learner wellness while engaging in systems thinking to understand how individuals, programs and respective systems intersect. The importance of acknowledging equity, diversity and inclusion, fostering psychological safety and engaging learners as active participants in their journey during a pandemic and beyond are key elements in developing wellness interventions.
Acknowledgments
Acknowledgments: We would like to thank all participants at the Cumming School of Medicine.
Appendix A.
Questions from the online survey “Learner Wellness Needs Assessment During the COVID-19 Pandemic”
Learner Wellness Need Assessment During COVID-19
Start of Block: PREAMBLE & CONSENT
Q1 The Wellness Innovation Scholarship for Health Professions Education Scholarship (WISHES) initiative is conducting a needs assessment for all learners across all programs at the Cumming School of Medicine regarding the impact of COVID-19 on learner wellness. This survey will take 15 minutes of your time and is completely anonymized. Your participation is voluntary. You may decline to answer any question and may withdraw from the survey at any time.
Q2 UNIVERSITY OF CALGARY
IMPLIED CONSENT TO PARTICIPATE IN SURVEY RESEARCH
TITLE: Exploring a Multi-Faceted Approach to Wellness in Learners during the COVID-19 Pandemic
SPONSOR: Office of the Senior Associate Dean, Cumming School of Medicine
INVESTIGATORS: Principal Investigator: Dr. Aliya Kassam Co-Investigators: Dr. Rahim Kachra, Ms. Allison Brown, Ms. Stephana Cherak Dr. Aliya Kassam; Phone: (403) 210-7526; Email: kassam@ucalgary.ca
INTRODUCTION This consent form is only part of the process of informed consent. It should give you the basic idea of what the research is about and what your participation will involve. If you would like more detail about something mentioned here, or information not included here, please ask. Take the time to read this carefully and to understand any accompanying information. You were identified as a possible participant in this study because you are a learner currently enrolled in the University of Calgary’s Cumming School of Medicine as an undergraduate student, medical student, graduate student or resident physician. Your participation in this research study is voluntary.
WHY IS THIS STUDY BEING DONE?
Wellness programs need to be effective, evidenced-based yet personalized and tailored to meet individual needs and circumstances. In response to the “epidemic of burnout in medicine” a number of wellness initiatives are growing at our institution and the gaze of our leadership is shifting towards early prevention and intervention through engagement, advocacy and scholarship. The Wellness Innovation Scholarship for Health Professions Education Scholarship (WISHES) is designed to be an education laboratory focused on the wellness scholarship of learners across Cumming School of Medicine from the pre-medical school health sciences bachelors program, graduate science programs in medicine, undergraduate medical education and postgraduate medical education. The WISHES framework is a holistic framework which focusses on areas of wellness such as mental, physical, occupational, social and intellectual domains stratified by the levels of individual learners, the training programs and the intersection of the higher education system with the health care system. The current coronavirus (COVID-19) pandemic has impacted learners at the Cumming School of Medicine. Learners are being impacted by the pandemic with regard to their personal well-being. We wish to explore this impact using a multi-faceted approach to wellness in learners, recognizing: 1) wellness can be impacted in different domains specifically mental health, physical health social health, occupational health and intellectual health and 2) that wellness initiatives can occur at the individual (learner), program (postgraduate medical education and resident program) and system (higher education system and health care systems) levels.
Specifically, we aim to investigate the following two objectives:
1. To determine the extent and nature of learner wellness initiatives to facilitate wellness in domains of mental health, physical health, occupational health, social health and intellectual health at the individual, program and system levels during the COVID-19 pandemic.
2. To explore how learners, describe their own wellness with respect to five domains of wellness at the individual, program and system levels during the COVID-19 pandemic.
HOW MANY PEOPLE WILL TAKE PART IN THIS STUDY?
We are aiming to recruit at least 50% of learners from each of the groups at the Cumming School of Medicine which may include up to 1,450 participants across all of the programs.
WHAT WILL HAPPEN IF I TAKE PART IN THIS STUDY?
This study is comprised of two parts. This is the survey part of the study. If you would like to participate in an interview, you may include your contact information in the survey if you wish. Your participation in both parts of this study is completely voluntary.
HOW LONG WILL I BE IN THIS STUDY?
Data will be collected over the next 4-6 weeks. All data will be analyzed in aggregate. We will retain the data for 5 years.
ARE THERE ANY POTENTIAL RISKS OR DISCOMFORTS THAT I CAN EXPECT FROM THIS STUDY?
We do not anticipate any kind of physical, psychological, or social risks associated with this study. The questions are not sensitive of nature. If at any point, you do not want to answer a question, you may skip the question or withdraw from the study by closing the survey window.
ARE THERE ANY POTENTIAL BENEFITS IF I PARTICIPATE?
The proposed research responds to a critical need to enhance learner wellness at our institution during the COVID-19 pandemic. Our study aims to have a large impact to the medical education programs at the University of Calgary. Through the context of the COVID-19 pandemic, the findings gathered from your interview will help us to better understand various mental, physical, social, occupational and intellectual processes that allow learners to thrive and promote wellness during impactful disruptions to medical education. Gathering insights into the challenges and successes of these wellness initiatives will allow for end-of-study knowledge translation that include dissemination to the Cumming School of Medicine, conference and workshop presentations, and journal publications.
WHAT OTHER CHOICES DO I HAVE IF I CHOOSE NOT TO PARTICIPATE?
You are free to choose not to participate in the study. If you decide not to take part in this study, there will be no penalty to you. Your decision will not affect your education or employment.
CAN I STOP BEING IN THE STUDY?
Yes. You can decide to stop at any time by not completing the survey or closing the survey window. Please be assured that any study data obtained from the survey is anonymized and will be analyzed in aggregate.
WILL I BE PAID FOR PARTICIPATING, OR DO I HAVE TO PAY FOR ANYTHING?
You will not be paid for your participation in this research study.
WILL INFORMATION ABOUT ME AND MY PARTICIPATION BE KEPT CONFIDENTIAL?
Qualtrics is an online survey platform with servers in the University of Calgary. All data are encrypted and stored directly on its servers at the University of Calgary. Researcher access to the survey data is password-protected and the transmission is encrypted. Survey responses cannot be linked to your computer. All survey responses will be anonymized.
HOW LONG WILL INFORMATION FROM THE STUDY BE KEPT?
The researchers intend to keep the research data and records for approximately 5 years. After which time, all data will be destroyed. Any future use of this research data is required to undergo review by a Research Ethics Board.
RESEARCHER CONFLICTS OF INTERESTS
The researchers for this study have no conflicts of interest to declare.
USE OF DATA FOR FUTURE RESEARCH
We will also be conducting interviews as part of this research. If you would like to be contacted to participate in an interview, please add your contact information in the space provided after completing the survey.
HOW CAN I FIND OUT ABOUT THE STUDY RESULTS?
Study results will be made publicly available through scholarly publications and a Cumming School of Medicine report.
WHAT ARE MY RIGHTS IF I TAKE PART IN THIS STUDY?
Taking part in this study is completely voluntary. You can choose whether or not you want to participate. Whatever decision you make, there will be no penalty to you.
WHOM MAY I CONTACT IF I HAVE QUESTIONS ABOUT THIS STUDY?
You may contact Dr. Aliya Kassam at (403) 210-7526 with any questions or concerns about the research or your participation in this study. If you have any questions concerning your rights as a possible participant in this research, please contact the Chair, Conjoint Health Research Ethics Board, University of Calgary at 403-220-7990. This study has been approved by the Conjoint Health Research Ethics Board, University of Calgary (REB: 20-117).
Q3 I understand the above information and consent to my voluntary participation in this research study. Your decision to select this option and participate in the survey will be interpreted as an indication of your agreement to participate. In no way does this waive your legal rights nor release the investigators or involved institutions from their legal and professional responsibilities. Should you wish to not participate in this study, please exit the survey now.
○ I understand and consent to voluntary participation in this research study. (1)
End of Block: PREAMBLE & CONSENT
Start of Block: DEMOGRAPHIC QUESTIONS
Q4 Which of the following best describes your gender identity? (Check all that apply)
□ I identify as a woman (1)
□ I identify as a man (2)
□ I identify as non-binary (3)
□ I prefer to self describe, please specify below: (4) ________________________________________________
□ I prefer to not answer this question (5)
Q5 Do you identify as a visible minority (non-Caucasian in race or non-white in colour)?
○ Yes (1)
○ No (2)
Q6 Have you ever been clinically diagnosed or received professional treatment for pain, flexibility, mobility, mental health, seeing, hearing, dexterity, learning or memory?
○ Yes (1)
○ No (2)
Q7 What program are you currently enrolled in?
○ BHSc Student (1)
○ BCR Student (5)
○ Graduate Student (MSc or PhD) (3)
○ Undergraduate Medical Student (UME) (2)
○ Resident Physician (PGME) (4)
End of Block: DEMOGRAPHIC QUESTIONS
Start of Block: WELLNESS QUESTIONS
Q8 Wellness Questions
The next 14 questions will ask about your wellness characteristics as a learner during the COVID-19 pandemic.
Q9 Do you feel comfortable disclosing the current state of your wellness to your training program?
○ Yes (1)
○ No (2)
Q10 Do you think the Cumming School of Medicine is offering adequate support to you to maintain your wellness during the COVID-19 pandemic?
○ Yes (1)
○ No (2)
○ Other, please specify below: (3) ________________________________________________
Q11 In your own words, please describe what wellness in general means to you?
________________________________________________________________
________________________________________________________________
Q12 In your own words, please describe your own wellness as a result of the current COVID-19 pandemic?
________________________________________________________________
________________________________________________________________
Q13 As an individual, what do you think allows you to thrive in your training during the COVID-19 pandemic? Please select all that apply.
□ Individual factors (i.e., your own economic circumstances, religious norms, stress management and coping strategies) (1)
□ Program factors (i.e., Bachelor of Health Sciences, Undergraduate Medical Education, Graduate Science Education, or Postgraduate Medical Education) (2)
□ System factors (i.e., higher education system or health care system factors, such as University of Calgary or Alberta Health Services) (3)
□ Other factors, please specify below: (4) ________________________________________________
Q14 As an individual, what do you think may lead you to struggle in your training during the COVID-19 pandemic? Please select all that apply.
□ Individual factors (i.e., your own economic circumstances, religious norms, stress management and coping strategies) (1)
□ Program factors (i.e., Bachelor of Health Sciences, Undergraduate Medical Education, Graduate Science Education, or Postgraduate Medical Education) (2)
□ System factors (i.e., higher education system or health care system factors, such as University of Calgary or Alberta Health Services) (3)
□ Other factors, please specify below: (4) ________________________________________________
Q15 Please indicate for each of the five statements which is closest to how you have been feeling over the past two weeks. Over the past two weeks...
| All of the time (1) | Most of the time (2) | More than half of the time (3) | Less than half of the time (4) | Some of the time (5) | At no time (6) | |
|---|---|---|---|---|---|---|
| ...I have felt cheerful and in good spirits (1) | ||||||
| ...I have felt calm and relaxed (2) | ||||||
| ...I have felt active and vigorous (3) | ||||||
| ...I woke up feeling fresh and rested (4) | ||||||
| ...my daily life has been filled with things that interest me (5) |
Q16 The COVID-19 pandemic has negatively influenced the following aspects of my well-being (select one per row):
| Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly Agree (5) | I prefer not to respond (6) | |
|---|---|---|---|---|---|---|
| Physical wellness (e.g., physical activity, nutrition, your own disease management) (1) | ||||||
| Mental wellness (e.g., mood, anxiety, stress management, emotional well-being) (2) | ||||||
| Social wellness (e.g., sense of inclusion, equity) (3) | ||||||
| Intellectual wellness (e.g., ability to learn or fulfill educational goals) (4) | ||||||
| Occupational wellness (e.g., safety in learning and working environments) (5) |
End of Block: WELLNESS QUESTIONS
Start of Block: Block 3
Q17 As a learner what concerns you the most about the COVID-19 pandemic?
________________________________________________________________
Q18 As a learner what concerns you the least about the COVID-19 pandemic?
________________________________________________________________
Q19 Please describe any wellness tools or strategies that you find helpful in coping with the COVID-19 pandemic (these can be personal or delivered by the Cumming School of Medicine).
________________________________________________________________
Q20 What additional wellness supports would you like to see offered to you as a learner during the COVID-19 pandemic?
________________________________________________________________
Q21 Is there anything you would like to add about wellness initiatives for learners during the COVID-19 pandemic?
________________________________________________________________
End of Block: Block 3
Footnotes
Conflicts of Interest: None
Funding/Support: This study was funded by the Office of Postgraduate Medical Education and supported by the Office of the Senior Associate Dean of Education at the Cumming School of Medicine.
Data availability: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
The WISHES wellness domains (1 item for each domain) has a Cronbach’s alpha of 0.74 and a one-factor solution as a holistic definition of learner wellbeing that accounts for 50% of the variance based on a separate global sample of 6,492 medical learners.
References
- 1.Maser B, Danilewitz M, Guerin E, Findlay L, Frank E. Medical student psychological distress and mental illness relative to the general population: a Canadian cross-sectional survey. Acad Med. 2019;94(11):1781-91. 10.1097/ACM.0000000000002958 [DOI] [PubMed] [Google Scholar]
- 2.Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: a systematic review and meta-analysis. Eur Psychiatry. 2019;55:36-42. 10.1016/j.eurpsy.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 3.Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456-68. 10.1111/medu.12962 [DOI] [PubMed] [Google Scholar]
- 4.Quek TT, Tam WW, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16(15). 10.3390/ijerph16152735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kemp S, Hu W, Bishop J, et al. Medical student wellbeing-a consensus statement from Australia and New Zealand. BMC Med Educ. 2019;19(1):69. 10.1186/s12909-019-1505-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopkins L, Morgan H, Buery-Joyner SD, et al. To the point: a prescription for well-being in medical education. Am J Obstet Gynecol. 2019;221(6):542-8. 10.1016/j.ajog.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 7.Nordquist J, Hall J, Caverzagie K, et al. The clinical learning environment. Med Teach. 2019;41(4):366-72. 10.1080/0142159X.2019.1566601 [DOI] [PubMed] [Google Scholar]
- 8.Jennings ML, Slavin SJ. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad med. 2015;90(9):1246-50. 10.1097/ACM.0000000000000842 [DOI] [PubMed] [Google Scholar]
- 9.Ripp JA, Privitera MR, West CP, et al. Well-being in graduate medical education: a call for action. Acad Med. 2017;92(7):914-7. 10.1097/ACM.0000000000001735 [DOI] [PubMed] [Google Scholar]
- 10.Slavin SJ, Chibnall JT. Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med. 2016;91(9):1194-6. 10.1097/ACM.0000000000001226 [DOI] [PubMed] [Google Scholar]
- 11.Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clinic proceedings. 2018;93(11):1571-80. 10.1016/j.mayocp.2018.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vogel L. Physician health charter calls on health systems, organizations to share responsibility for burnout. CMAJ 2018;190(26):E812-e3. 10.1503/cmaj.109-5623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogel L. Medical education needs reform to improve student well-being and reduce burnout, say experts. CMAJ. 2018;190(48):E1426-E7. 10.1503/cmaj.109-5685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO Timeline - COVID-19: World Health Organization; 2020. Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- 15.Slavin SJ, Schindler DL, Chibnall JT. Medical student mental health 3.0: improving student wellness through curricular changes. Acad Med. 2014;89(4):573-7. 10.1097/ACM.0000000000000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cumming School of Medicine ; Future Students; Education 2020. Available from: https://cumming.ucalgary.ca
- 17.Pangaro L, ten Cate O. Frameworks for learner assessment in medicine: AMEE Guide No. 78. Med Teach. 2013;35(6):e1197-210. 10.3109/0142159X.2013.788789 [DOI] [PubMed] [Google Scholar]
- 18.Topp CW, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167-76. 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 19.Kassam A, Ellaway R. acknowledging a holistic framework for learner wellness: the human capabilities approach. Acad Med. 2020;95(1):9-10. 10.1097/ACM.0000000000003026 [DOI] [PubMed] [Google Scholar]
- 20.Slavin SJ, Schindler DL, Chibnall JT. Medical student mental health 3.0: improving student wellness through curricular changes. Acad Med. 2014;89(4):573-577. 10.1097/ACM.0000000000000166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Topp CW, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167-176. 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 22.Henkel V, Mergl R, Coyne JC, et al. Depression with atypical features in a sample of primary care outpatients: prevalence, specific characteristics and consequences. J Affect Disord. 2004;83(2-3):237-242. 10.1016/j.jad.2004.07.003 [DOI] [PubMed] [Google Scholar]
- 23.Henkel V, Mergl R, Coyne JC, Kohnen R, Moller HJ, Hegerl U. Screening for depression in primary care: will one or two items suffice? Eur Arch Psychiatry Clin Neurosci. 2004;254(4):215-223. 10.1007/s00406-004-0476-3 [DOI] [PubMed] [Google Scholar]
- 24.Henkel V, Mergl R, Kohnen R, Allgaier AK, Moller HJ, Hegerl U. Use of brief depression screening tools in primary care: consideration of heterogeneity in performance in different patient groups. Gen Hosp Psychiatry. 2004;26(3):190-198. 10.1016/j.genhosppsych.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 25.Bart R, Ishak WW, Ganjian S, et al. The Assessment and Measurement of Wellness in the Clinical Medical Setting: A Systematic Review. Innov Clin Neurosci. 2018;15(9-10):14-23. [PMC free article] [PubMed] [Google Scholar]
- 26.Roberts K, Dowell A, Nie JB. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med Res Methodol. 2019;19(1):66. 10.1186/s12874-019-0707-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Research in Sport, Exercise and Health. 2019:1-16. 10.1080/2159676X.2019.1704846 [DOI] [Google Scholar]
- 28.Beaulieu M, Breton M, Brousselle A. Conceptualizing 20 years of engaged scholarship: a scoping review. PLoS One. 2018;13(2):e193201. 10.1371/journal.pone.0193201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gagliardi AR, Berta W, Kothari A, Boyko J, Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implement Sci. 2016;11:38. 10.1186/s13012-016-0399-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.COVID-19 Alberta Statistics . Interactive aggregate data on COVID-19 cases in Alberta 2020. Available from: https://www.alberta.ca/stats/covid-19-alberta-statistics.htm
- 31.Thomas L, Harry E, Quirk R, et al. Evidence-based interventions for medical student, trainee and practicing physician wellbeing: a charm annotated bibliography 2017. [Google Scholar]
- 32.Wasson LT, Cusmano A, Meli L, et al. association between learning environment interventions and medical student well-being: a systematic review. JAMA. 2016;316(21):2237-52. 10.1001/jama.2016.17573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gengoux GW, Roberts LW. Ethical use of student profiles to predict and prevent development of depression symptoms during medical school. Acad Med. 2019;94(2):162-5. 10.1097/ACM.0000000000002436 [DOI] [PubMed] [Google Scholar]
- 34.Walsh AL, Lehmann S, Zabinski J, et al. Interventions to prevent and reduce burnout among undergraduate and graduate medical education trainees: a systematic review. Acad Psychiatry. 2019;43(4):386-95. 10.1007/s40596-019-01023-z [DOI] [PubMed] [Google Scholar]
- 35.Gaw CE. Becoming a member of the team. Med Teach. 2017;39(1):105-6. 10.1080/0142159X.2016.1209474 [DOI] [PubMed] [Google Scholar]
- 36.Wilkes C, Lewis T, Brager N, et al. Wellbeing and mental health amongst medical students in Canada. Int Rev Psychiatry. 2019;31(7-8):584-7. 10.1080/09540261.2019.1675927 [DOI] [PubMed] [Google Scholar]
- 37.Wang JH, Tan S, Raubenheimer K. Rethinking the role of senior medical students in the COVID-19 response. Med J Aust. 2020;212(10):490-e1. 10.5694/mja2.50601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Swanwick T, Forrest K, O'Brien BC. Understanding medical education: evidence, theory, and practice. Third ed. Hoboken, NJ: John Wiley & Sons, Inc; 2019. 10.1002/9781119373780 [DOI] [Google Scholar]


