Abstract
Background
The evidence surrounding the impact of COVID-19 on medical learners remains anecdotal and highly speculative despite the anticipated impact and potential consequences of the current pandemic on medical training. The purpose of this study was to explore the extent that COVID-19 initially impacted medical learners around the world and examine global trends and patterns across geographic regions and levels of training.
Methods
A cross-sectional survey of medical learners was conducted between March 25–June 14, 2020, shortly after the World Health Organization declared COVID-19 a pandemic.
Results
6492 learners completed the survey from 140 countries. Most medical schools removed learners from the clinical environment and adopted online learning, but students reported concerns about the quality of their learning, training progression, and milestone fulfillment. Residents reported they could be better utilized and expressed concerns about their career timeline. Trainees generally felt under-utilized and wanted to be engaged clinically in meaningful ways; however, some felt that contributing to healthcare during a pandemic was beyond the scope of a learner. Significant differences were detected between levels of training and geographic regions for satisfaction with organizational responses as well as the impact of COVID-19 learner wellness and state-trait anxiety.
Conclusions
The disruption to the status quo of medical education is perceived by learners across all levels and geographic regions to have negatively affected their training and well-being, particularly amongst postgraduate trainees. These results provide initial empirical insights into the areas that warrant future research as well as consideration for current and future policy planning.
Abstract
Contexte
On s’attendait à ce que la pandémie de la COVID-19 ait des conséquences sur la formation médicale, mais les constats relatifs à son impact sur les étudiants en médecine demeurent anecdotiques et plutôt spéculatifs. L’objectif de cette étude était d’explorer l’étendue des premiers effets de la COVID-19 sur les étudiants en médecine dans le monde et d’examiner les tendances et les schémas qui se dégagent, quels que soient la région géographique ou le niveau d’études.
Méthodes
Une enquête transversale sur les étudiants en médecine a été menée entre le 25 mars et le 14 juin 2020, peu après que l’Organisation mondiale de la santé ait déclaré que la COVID-19 était une pandémie.
Résultats
Le sondage a été réalisé auprès de 6492 étudiants de 140 pays. La plupart des facultés de médecine ont retiré les apprenants de l’environnement clinique et adopté l’apprentissage en ligne, mais les étudiants ont exprimé des préoccupations quant à sa qualité, à la progression de la formation et à l’atteinte de divers jalons. Les résidents jugent qu’ils pourraient être plus utiles et s’inquiètent de l’avancement de leur carrière. Les apprenants se sentent généralement sous-utilisés et souhaitent s’engager cliniquement de manière plus significative; cependant, certains estiment qu’il n’est pas à propos de demander aux étudiants de contribuer aux soins de santé pendant une pandémie. Des écarts importants ont été relevés entre les différents niveaux de formation et les différentes régions géographiques en ce qui concerne la satisfaction face aux réponses organisationnelles, l’impact de la COVID-19 sur leur bien-être et l’anxiété chronique et réactionnelle.
Conclusions
La perturbation du statu quo dans l’éducation médicale est perçue par les étudiants de tous les niveaux et de toutes les régions géographiques, mais davantage encore par les résidents, comme ayant affecté négativement et leur formation et leur bien-être. Ces résultats fournissent des aperçus empiriques préliminaires sur les domaines qui méritent des recherches futures et qui devraient être pris en compte dans la formulation des politiques actuelles et à venir.
Introduction
The coronavirus pandemic (COVID-19) represents the first global interruption to medical education since World War II. This public health emergency has required undergraduate and postgraduate medical training programs around the world to rapidly respond, including re-deploying learners to other clinical spaces or removing them entirely, and moving education online to promote physical distancing.1–3 The current COVID-19 pandemic has changed the status quo of medical training as we know it – whether for better or for worse remains unclear and may have profound implications.
Prior localized disruptions to medical training have negatively affected trainees, such as pandemics and climate emergencies. The severe acute respiratory syndrome (SARS) pandemic in 2003 revealed the tension between embracing learning opportunities that a public health emergency offers and protecting the needs and well-being of learners.4–6The SARS pandemic adversely affected the mental health of learners and healthcare professionals, and heightened anxiety amongst learners was associated with a perceived negative educational experience.4,7–9 In 2005, the rapid restructuring of the medical school curriculum in response to Hurricane Katrina resulted in a decline in academic performance.10 Lessons from both SARS and Hurricane Katrina highlighted the importance of support networks and attention to learner wellness, recognizing the additional stressors that these disruptions can place on medical trainees.4,7,10,11 These emergencies led to significant and rapid innovation in curriculum structure and content.11 While disruptions to medical education can provide an impetus to reconsider ethical and practical implications of training during emergencies, training models may remain stagnant.7,11Despite a heightened awareness fifteen years ago of the potential implications of interruptions to medical education, many organizations and systems entered the current pandemic relatively unprepared.
Medical education’s understanding of the impact of global emergencies and disruptions to medical training remained limited to SARS and localized emergencies, yet the current pandemic remains the single most substantial disruption to contemporary medical training with global impact. Critical decisions made during the pandemic may lead to long-term consequences.12
The extent to which COVID-19 has impacted medical training remained speculative and anecdotal, despite the potential implications to not only the future generations of physicians, but to patient care. Understanding how medical learners were initially impacted by the pandemic and the medical school and health system responses is an important first step in our broader understanding of how COVID-19 has impacted medical training. The research question for this exploratory study was: How have medical learners been impacted by the COVID-19 pandemic around the world?
Methods
Data collection
We administered a cross-sectional survey between March 25 and June 14, 2020, shortly after the World Health Organization declared COVID-19 a pandemic. Criterion and snowball sampling techniques were used to collect data from undergraduate (e.g., medical students) and postgraduate (e.g., interns, house staff, resident physicians) medical learners at any medical school around the world. This study explicitly focused on medical learners given that they provide a significant proportion of patient care yet are still considered learners.
Our decision to use a survey was based on the ability of this method to efficiently collect empirical data from a large population.13 The survey instrument was designed to include both quantitative and qualitative questions in order to later compare variables across groups, allow participants to provide insight into how they have been impacted using their own words, and use the qualitative data to potentially expand upon the results of the quantitative data. All participants completed demographic questions followed by questions specific to their level of training. Next, shared questions explored the effect of the pandemic on learner wellbeing and their communications with others. Open-ended questions collected qualitative data surrounding the impacts of the pandemic on training, utilization of residents, and strategies used in response to the pandemic. Items were constructed by a member of our research team (AB) a PhD-trained medical education scientist with formal training in psychometrics and survey development. All items were newly developed based on best practices for scale development14 and designed to capture key information specific to the research question with the exception of the 6-item State-Trait Anxiety Inventory (STAI-6) which is an established instrument.15 One 5-item scale exploring the impact of the pandemic on five domains of wellness was informed by a holistic framework for learner wellness.16
An initial survey underwent pilot testing with seven individuals (two medical students, four residents, and one graduate student) to examine item comprehension and survey functionality, leading to refinements to both the content and usability of the survey. The final survey (Supplemental File A) was translated to 19 additional languages (based on the availability of volunteer translators) to increase the inclusion of learners from around the world. The survey was administered online using Qualtrics software by distributing an anonymous, re-usable link over social media (e.g., Twitter, Facebook, Reddit), emailing key contacts, and through snowball sampling. Each time the study was promoted, we encouraged others to pass along information about the study through their social networks (e.g., re-tweeting). The final page of the survey thanked learners for their participation and asked them to forward the study to their colleagues and peers to help diversify responses.
Data analysis
Quantitative data were imported into SPSS Version 26 (IBM Corp., New York) for analysis. Countries were coded to the geographic regions defined by the World Bank to explore geographic differences.17 Descriptive statistics were calculated for each item. Total scores were computed for scaled questions, with positively worded items reverse coded in the calculation. Independent t-tests were used to compare total scores between medical students and residents, and an Analysis of Variance test was used to compare data across geographic regions using a post-hoc correction to account for multiple comparisons. To examine the psychometric properties of the survey, Cronbach’s alpha was computed for scaled items to assess reliability evidence and an exploratory factor analysis was used to examine construct validity.
Qualitative data were manually back-translated to English by fluent translators (i.e., not through automated software) to ensure accuracy. Data were then analyzed in NVivo Version 12 (QSR International, Melbourne). Three investigators read through the data to identify preliminary themes, which were then organized into a coding framework for deductive thematic and content analysis to similarly examine patterns in the data between levels and across geographic regions.18 Using content analytic techniques, two investigators (KB, MM) independently coded 100 responses to refine the initial coding framework and assess the degree of coding consistency using the Kappa statistic, a measure of inter-coder agreement between 0 (no agreement) and 1 (perfect agreement), where K > .40 is considered to reflect moderate agreement and K > .60 is considered to reflect substantial inter-coder agreement (19). After an additional 400 responses were double coded and the Kappa statistics for each code continued to suggest acceptable inter-coder agreement (K > .60) and confidence that the framework could be applied consistently, a decision was made to divide the codes between investigators to improve the efficiency of coding given the volume of data. Upon completion of the coding for all responses, thematic analytic techniques were used to further analyze the data. Themes in the coding framework were divided amongst the research team, and each member analyzed the data coded to their assigned themes and summarized the patterns in the data. Theme summaries were compiled for interpretation by the study team, who then compared and contrasted the results of the qualitative data with the quantitative data to examine how these findings converge or diverge from, and ultimately expand upon, the quantitative results.
The University of Calgary Conjoint Health Research Ethics Board reviewed and approved this study (File #20-0484). Participation in this study was voluntary. Implied consent was obtained from all participants. Participants had the option to either skip individual questions or select “prefer not to answer.”
Results
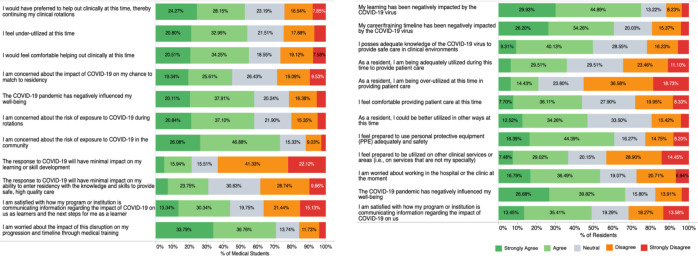
A total of 6492 learners from 140 countries completed the survey (N = 5260 medical students, N = 1007 residents, N = 225 did not specify level; see Appendix A, Table 1 for demographics). The majority of participants were from the World Bank regions of Europe and Central Asia (43.4%, N = 2819). Over half (53.4%, N = 3465) completed the survey in English. The results for both medical student-specific and resident-specific questions are summarized in Appendix A, Table 2. Figure 1 visualizes the responses to the scaled questions for both levels (see Supplemental Data, File B for additional visualizations of the data by level of training and geographic region).
Figure 1.
Scaled questions exploring the impact of COVID on learners
Undergraduate medical learners
The majority (84.3%, N = 2044/2426) of clinical-level medical students were excused from clinical duties; however, some worked clinically in some capacity (9.0%, N = 473/5260). Most spent their time in online learning coordinated by their medical school (68.2%, N = 3587/5260), pursuing self-directed learning (44.1%, 2322/5260), resting (36.4%, N = 1913/5260), and engaging in more wellness activities than normal (31.4%, 1654/5260). Most (80.9%, N = 3997/4938) had online learning coordinated by their school but 66.5% (N = 2608/3919) felt their education would be of lower quality as a result. Some had difficulties learning from home (21.3%, N = 835/3919) and accessing the internet (11.0%, N = 431/3919).
Students reported that their core electives (23.5%, N = 1235/5260) and visiting electives (19.5%, N = 1027/5260) were cancelled or postponed. The qualitative data highlighted how reduced clinical exposure limited opportunities to explore specialties, decreased career interests, and created anxiety about implications for future milestones (e.g., examinations, residency match). While the majority of medical students did not report the pandemic influenced their career interests, 11.4% (N = 600/5260) of medical students reported increased interests in both Public Health and Infectious Disease as a result of the pandemic, as well as Family Medicine (N = 314/5260), other clinical specialties (e.g., Emergency Medicine, Critical Care, Internal Medicine), and new interests in incorporating epidemiology into their future careers. Decreased interest in clinical careers and concerns about the impact of the pandemic on job prospects in their country were noted qualitatively.
Over half of medical students reported feeling under-utilized (53.8%, N = 2119/3942); 52.4% (N = 1797/3428) wanted to assist clinically and felt comfortable doing so (54.8%, N = 2117/3866). While 57.9% (N = 1963/3388) worried about the risk of exposure to the virus during rotations, 73.0% (N = 3217/4409) worried about the risk of exposure in the community. Over two-thirds (70.6%, N = 2942/4170) reported feeling worried about the disruption to their progression through medical training, with 45.0% (N = 1420/3159) worrying about their chances to match to residency. Only 21.0% (N = 933/4435) thought the pandemic would have a minimal impact on their learning or skill development, and only 31.0% (N = 1193/3852) felt that it would have a minimal impact on their ability to enter residency with sufficient knowledge and skill to provide safe, high-quality care. The majority of students (58.0%, N = 2571/4431) felt that the pandemic negatively affected their wellbeing.
Postgraduate resident learners
Residents were from a variety of specialties, mostly in urban settings (66.7%, N = 766/1148). Three-quarters of residents agreed their learning was negatively impacted by COVID-19 and 60.5% (N = 480/794) felt it disrupted their career progression and timeline. Only 16.0% (N = 184/1148) reported working more than normal during the pandemic and 36.7% (N = 421/1148) working less than normal. Some residents felt adequately utilized (35.9%, N = 285/793) or over-utilized (20.9%, N = 165/790); however, 46.8% (N = 370/791) reported they could be better utilized. Over one-third (43.8%, N = 347/792) felt comfortable providing patient care at this time, and 60.8% (N = 482/793) felt prepared to use personal protective equipment (PPE). Half of residents (49.4%, N = 393/795) reported adequate knowledge of COVID-19 to provide care, 36.5% (N = 288/789) were prepared to be redeployed to other clinical services, and 53.3% (N = 422/792) were worried about working in the hospital. 66.5% (N = 526/791) agreed that COVID-19 had negatively impacted their wellbeing. The qualitative data provided further evidence that residents felt under-utilized – but highlighted how they saw their re-deployment in a clinical setting as conflicting with their educational goals.
Shared questions
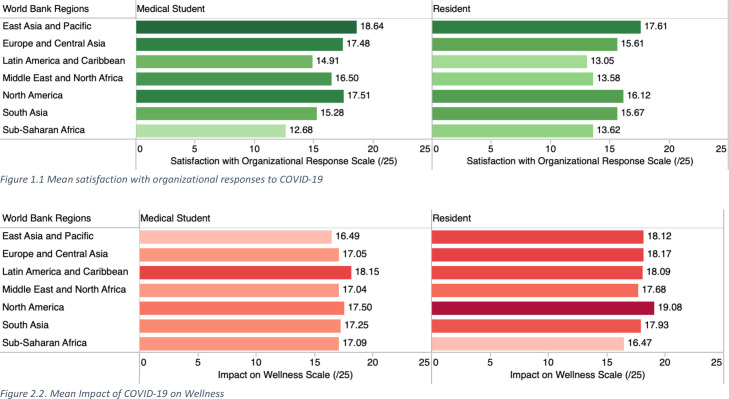
All scaled items had acceptable internal consistency (α > .7) and factor loadings, suggesting reliability and validity evidence. Statistically significant differences were detected between undergraduate (i.e., medical student) and postgraduate (i.e., resident) levels of training (p <.05) and geographic regions (p <.007) for the items examining satisfaction with organizational responses [t = 7.517, p <.000; [F(6,5258) = 73.85, p <.007]], the impact of COVID-19 on wellness [t = –7.774, p <.000 [F(6,5165) = 11.81, p <.007]], and state-trait anxiety [t = –4.710, p <.000; [F(6, 5131) = 10.48, p <.007]] (Supplemental File C). In general, residents reported lower satisfaction with organizational responses than medical students (x̄ = 15.67, 95% CI = 15.36––159.98) as well as a greater negative impact on their wellbeing (x̄ = 18.52, 95% CI 18.24––18.80) and anxiety (x̄ = 15.13, 95% CI 14.83––15.42). Learners from the East Asia and Pacific region were most satisfied with organizational responses compared to other geographic regions, and learners from Sub-Saharan Africa and Latin America and Caribbean were least satisfied (Figure 2.1). Medical students from the Latin America and Caribbean region as well as residents from North America reported the largest negative impact of COVID-19 on their wellness (Figure 2.2). Residents from South Asia, Latin America and Caribbean reported the highest state-trait anxiety (Figure 2.3)
Figure 2.
Comparison of shared scaled items between levels and geographic regions
Seventy-four percent of residents and 57% of medical students reported being more anxious than usual (Appendix A, Table 3; Figure B.4). Common concerns were the health and wellbeing of family members, the impact of the pandemic on their learning, the health of the public, their personal health, the financial situation of others, and their personal financial situation (Figure B.3). One-quarter of participants identifying as Asian reported an increase in racist comments or behaviours in the clinical setting during COVID-19. Over half (54.7%) of learners living with a disability felt their school’s response to the pandemic would further disadvantage them due to their disability.
14.8% (N = 775) of learners reported having to be in quarantine or isolation at the time of the survey. Nearly all learners were practicing physical and social distancing.
The qualitative data highlighted how normal education and training processes were severely disrupted by the pandemic across ten themes, including: communication, training, utilization of learners, future concerns and implications, and silver linings (see Supplemental File D for a summary of themes). Learners identified a need for institutions to adapt and innovate in order to mitigate these impacts and continue education. Learners also desired to have input into their institutions’ pandemic response. Strategies such as town halls, surveys, and learner representation on decision-making committees helped ensure their circumstances were accurately understood and enabled them to raise concerns overlooked by decision-makers.
Clear and effective communication during the pandemic was essential for learners, while poor or absent communication left learners uncertain of what was happening and contributed to their anxiety. Effective communication provided clarity and reassurance about the pandemic’s impacts and the institutional response. Learners wished to be informed about impacts on their programs, details of the pandemic response, their role (including how to help), and resources they could access. Effective communications about these topics were clear, specific, decisive, concise, and reassuring. Irregular (sporadic) communication created an “information vacuum” that was filled with speculation, rumours, and misinformation. Overly frequent communication was overwhelming and led students to ignore institutional communications.
Numerous interventions were implemented in response to COVID-19, including virtual teaching strategies (e.g., Zoom, Microsoft Teams), office hours and town halls, and clinical strategies (e.g., patient handover via teleconference, alternating call schedules to minimize exposure). When done effectively, online learning maintained educational momentum and provided learners with motivation, a routine, and a sense of purpose. Self-directed learning was frequently used to augment online learning, and when provided with support and guidance, this motivated learners and provided them with a sense of progress. Programs with too much content overwhelmed them, whereas programs that provided minimal guidance left learners feeling aimless. Some participants stated that their program or school had done nothing in response to the pandemic and that either their education had continued as usual or, in some instances, students were told to stay at home and self-direct their learning without any guidance from their program.
Discussion
This study provides empirical data about the impact of COVID-19 on medical education around the world, notably the effects on learning and wellbeing. Taken together, our findings highlight how learners have been impacted regardless of their program’s response to the pandemic and whether or not they were removed from the clinical environment. However, the extent that COVID-19 has impacted learners differs significantly between levels of training and geographic regions.
COVID-19 has disrupted the traditional format and process of medical training for the vast majority of medical students and residents around the world. The rapid adoption of online learning by most schools may raise concerns about the quality of education, particularly at the pre-clinical stage of training where the vast majority of learning typically occurs in the classroom.20 Despite these concerns, equivalent educational outcomes between online and offline methods have been reported in the literature.21 It can also be argued that the uptake and refinement of technology to allow for online learning – which has been long resisted at some schools – may represent a key innovation in medical training as it has increased accessibility for many medical students who can now learn remotely, and, if recorded, revisit materials that were previously inaccessible outside of the lecture theatre. In considering the broad range of strategies that medical training programs have adapted during the pandemic, this may be an opportunity to reconceptualize, innovate, and improve the current models of medical training, and ultimately catalyze broader educational transformation.22,23
The removal of learners from the clinical setting may diminish training (particularly for residents in time-based models of training), influencing clinical competence acquisition and career-decision making – all of which may affect patient care and health system outcomes.22 For instance, medical students in our study reported that the loss of clinical experiences, such as clinical electives, impacted their decision-making regarding which specialties to apply to. In this way, one could argue that the removal of medical students from the clinical environment has consequences for their professional identity and career-decision making. On the other hand, the consequences of removing resident physicians from the clinical environment may have a lesser influence on their professional identity formation, and a greater influence on their clinical competence acquisition depending on the extent their clinical rotations were influenced. While it was common in Canada and the US for clerkship rotations and electives to be cancelled, thus removing nearly all medical students from the clinical environment during the initial wave, most resident physicians continued to provide clinical care.
The removal of medical students from the classroom and clinical environment meant that many learners experienced significant disruption to their routine. Consistent with early reports, medical students felt under-utilized and have a strong desire to help out clinically during times of need.24–28 However, not all learners may share these views. In addition to concerns about physical safety, numerous resident participants in our study believed a primary role of trainees is to be educated and that any deviation from that role is inappropriate. Other learners felt personally invested in contributing to care and viewed it as their personal calling and professional obligation. The optimal role of trainees during pandemics is complicated given their dual role as learners and healthcare providers – particularly with respect to resident physicians, who can provide patient care with minimal supervision and function with increasing autonomy throughout their training. The extent to which each role is prioritized during emergencies remains debated. On one hand, it has been argued that medical students specifically, as an unpaid workforce, are not essential workers, and may increase disease transmission and waste scarce supplies of PPE.29 In contrast, it can also be argued that medical students are a semi-skilled workforce that can alleviate the burden on residents and staff and should gain experience in preparation for future pandemics when they will no longer be trainees. In one study, hospital leaders viewed medical students who graduated early to help during COVID-19 as “game-changers.”30 It has also been argued that medical education is equally important to patient care during a pandemic.31 This may be a unique opportunity to cultivate leadership skills if learners are well-supported.32 For learners in the clinical environment, supervision, feedback, and evaluation as well as access to adequate wellness supports remain crucial.31,32 The ethical and practical considerations of utilizing medical learners during a pandemic remains an ongoing point of discussion and needs to be weighed against potential benefits of learning and implications to patient care.33,34
COVID-19 is anticipated to affect the mental health of the public35 as well as that of healthcare professionals.36 Previous health emergencies and disruptions to training, such as SARS and Hurricane Katrina, have been shown to diminish the mental health of trainees and healthcare professionals.37 Our study provides similar evidence but from a global perspective that the wellbeing of medical learners has been negatively impacted by COVID-19 across all levels of training and geographic regions. This is concerning given the existing evidence on the alarming prevalence of burnout and psychiatric morbidities in learners, as COVID-19 may amplify these pre-existing issues.38–41 Pandemic responses have superimposed new stressors while exacerbating existing stressors for learners. The “anticipatory loss” associated with the disruption of traditional processes and milestones –– the loss of clerkship rotations and electives for medical students, disruption to the residency match processes and timelines, and the cancellation of licensing exams for residents – appear associated with heightened anxiety and decreased wellness. Similarly, front-line learners (e.g., residents) may be particularly prone to wellness stressors at this time given the occupational hazards associated with providing clinical care during a pandemic.24,27 Postgraduate participants in our study often commented on the numerous challenges they faced working in clinical environments at this time, including their lack of PPE, resources, infrastructure, support, and advocacy during this time. Suggestions for mitigating the psychological consequences of COVID-19 on front-line care providers include providing clear communication, education, and psychological support, among others.37 Tailored strategies to support medical learners during a pandemic in various contexts to mitigate their situational stressors may be a key area for educators to share their innovations and lessons learned in order to better support learners.
This pandemic remains an ongoing challenge for medical education. At the moment of this publication, many countries are challenged with an even more critical challenge during the second wave of the pandemic – when multiple vaccines have been approved and countries are adopting diverse vaccination strategies. While the uncertainty of the initial COVID-19 wave required organizations to adopt a “worst-case scenario” approach, medical schools not only continue to react to the current needs of health systems, but proactively plan for the future. While some participants in this study applauded their program’s response, it is important to learn from this experience and improve planning and policies for current and future emergencies that may disrupt medical education.42Recommendations are increasingly being discussed in the literature.31,42–45As this is a critical opportunity to learn from the COVID-19 pandemic, a synthesis of key considerations for medical educators synthesized from our results and existing recommendations are summarized in Appendix A Table 4, spanning five key areas: teaching and learning (e.g., online learning), utilization of learners (e.g., using medical students during emergencies in clinical and non-clinical roles), supporting learner well-being, communicating with learners, and planning and decision-making. The COVID-19 pandemic may transform medical education for the better –– if newly embraced innovations that are working well are sustained rather than returning to the status quo.46,47 This represents a pivotal moment in our field to consider sustaining innovations that have been long resisted, such as online learning. We must continue to evaluate and share innovations and lessons learned from the pandemic amongst the global medical education community.12,46,48,49
Limitations
We acknowledge that this study has several limitations, including the response and selection bias. The use of snowball sampling techniques may have inevitably introduced bias into the sample and results. Further, we cannot calculate a response rate as we do not know the number of learners who declined to participate in this study. The response rates from residents are low, potentially because they continued working clinically and the disruptions to their training were less extreme than for medical students who were completely removed from their training environments. Further, this study excluded participants who did not speak any of the 20 languages of the survey and there may be inconsistencies across the survey translations despite our best attempts to ensure questions and constructs translated accurately. Due to the public circulation of the survey, participants could not be validated as medical learners. A small fraction (3.5%) of participants did not specify their level of training and were excluded from the comparisons across levels of training. The geographic comparisons remain limited, as other classification systems (e.g., the World Health Organization regions) may have generated different results and there may be more pronounced differences between countries within similar regions (e.g., the United States vs. Canada). Finally, the variable responses to COVID-19 across countries and time is worth noting. Numerous qualitative comments highlighted how national responses informed the responses of professional organizations and training programs. Future research could examine potential associations between temporality and the political and health system responses to examine how these factors may influence medical learners.50 Future research is also warranted to understand the long-term impact and potential consequences of the COVID-19 pandemic on education, patient care, and health system outcomes.
Conclusions
This global study provides empirical data surrounding the profound impact that COVID-19 has had on medical learners, which can inform responses to the current pandemic, future disruptions to training, and future research. Despite the global shift toward online education, all education may not be created or perceived equally, as the results of this study suggest medical students fear their education will be of lower quality at this time. Both medical students and residents report their under-utilization, yet the role of the medical learner during a pandemic remains controversial. A delicate balance remains between medical training and the acute needs of the health system to ensure that both education and patient care remain safe. Finally, this study highlights how the COVID-19 pandemic has negatively impacted the wellbeing of medical learners globally, particularly those at the postgraduate level of training, which may be associated with their anxiety relating to the anticipatory losses of their educational experience. While the goal of this study was to broadly examine the impacts of COVID-19 on medical education, it highlights several areas for further exploration. Future research is warranted to better understand the implications of COVID-19 on learner outcomes and to generate evidence-based strategies surrounding how best to teach, engage, and support medical learners during similar events.
Acknowledgments
Acknowledgements: The authors wish to acknowledge the O’Brien Institute for Public Health for funding this research, members of the University of Calgary medical education community for their support in conducting this study, as well as the Conjoint Health Research Ethics Board (Ashley Krecsy) for reviewing this study in a timely manner. Thanks to Kayla Atchison, Kyle Lafrenière, Suhair Bandeali, Krista Reich, Matthew Mancusco, Tefani Perera, and Nadiya Goswami for pilot testing the initial survey and providing feedback to help improve the survey items and functionality. We also wish to acknowledge Erika Tan and the Immigration Services Centre of Calgary and the assistance of numerous individuals who helped with the translation of the survey into additional languages: Philippe Pepin and Kyle Lafrenière (French), Yusuf Yilmaz (Turkish), Dinesh Chavda (Hindi), Tayebah Chaudhry (Urdu), Giuliana and Salvatore Guarna (Italian), Michael Ji (Korean), Joska Eelsingh (Dutch), Laura Massignani (Spanish), Shenghao Huang (Chinese), Elzbieta Raniszewska (Polish), Florentino Guerra Filho (Portuguese), Tomoka Tsuhara and Lea Mezger (German), Hengameh Kheirkhah (Farsi), Atipong Pathanasethpong (Thai), Thi Hong An Do (Vietnamese), Vesta Seibel (Ukrainian), Alena Yakimenka (Russian), and Aito Ueno (Japanese). Next, our study team wishes to acknowledge all who amplified this study over social media or other forms of snowball sampling, including the Association for Medical Education in Europe (AMEE), AMOpportunities. Finally, our study team wishes to acknowledge the patient partners who reviewed the results of this research and the draft manuscript.
Appendix A.
Table 1.
Demographic characteristics of participants
| N (%) | |||
|---|---|---|---|
| Level of Training | |||
| Medical Student | 5260 (81.0%) | ||
| Resident | 1007 (15.5%) | ||
| Prefer not to answer | 225 (3.5%) | ||
| World Bank Geographic Region | |||
| East Africa and Pacific | 445 (6.9%) | ||
| Europe and Central Asia | 2819 (43.4%) | ||
| Latin America and Caribbean | 944 (14.5%) | ||
| Middle East and North Africa | 191 (2.9%) | ||
| North America | 1607 (24.8%) | ||
| South Asia | 170 (2.6%) | ||
| Sub-Saharan Africa | 316 (4.9%) | ||
| Gender Identity | |||
| Woman | 4195 (64.7%) | ||
| Man | 2138 (32.9%) | ||
| Non-Binary | 25 (0.4%) | ||
| Woman + Non-Binary | 3 (0.05%) | ||
| Prefer to self-describe | 21 (0.3%) | ||
| Prefer not to answer | 110 (1.7%) | ||
| Race | Participants who selected East Asian, South Asian, and/or West Asian: Have you noticed or experienced an increase in racist comments or behaviors towards you or other Asian individuals in the clinical setting since the emergence of COVID-19? N = 944 | ||
| Black | 320 (4.9%) | Yes | 231 (24.5%) |
| East Asian | 315 (4.9) | No | 631 (66.8%) |
| Hispanic/Latinx | 779 (12.0%) | Prefer not to answer | 82 (8.69%) |
| South Asian | 430 (6.6%) | ||
| Southeast Asian | 181 (2.8%) | ||
| West Asian | 222 (3.4%) | ||
| White | 3540 (54.5%) | ||
| Multi-racial | 276 (4.25%) | ||
| Prefer to self-describe | 191 (2.9%) | ||
| Prefer not to answer | 238 (3.7) | ||
| Do you have a physical disability? | |||
| Yes | 157 (2.4%) | ||
| No | 6138 (94.6%) | ||
| Prefer not to answer | 197 (3.0%) | ||
| Do you have a learning disability? | If yes to either physical or learning disability: Has the response to COVID-19 from your school or program resulted in any concern(s) about how you may be disadvantaged at this time as a result of your physical or learning disability? | ||
| Yes | 256 (3.9%) | Yes | 188 (54.7%) |
| No | 5994 (92.3%) | No | 147 (42.7%) |
| Prefer not to answer | 242 (3.73%) | Prefer not to answer | 9 (2.6%) |
| Do you have children? | If yes: Do you feel that you have adequate childcare during this time? | ||
| Yes | 286 (4.4%) | Yes, I have adequate childcare at this time | 117 (43.5%) |
| No | 6036 (93.0%) | No, I do not have adequate childcare at this time | 104 (38.7%) |
| Prefer not to answer | 170 (2.6%) | Not applicable, my children do not require supervised childcare at this time | 41 (15.2%) |
| Prefer not to answer | 7 (2.6%) | ||
| Are you currently a caregiver to others? | If yes: Are you able to continue to maintain your caregiver responsibilities at this time? | ||
| Yes | 548 (8.4%) | Yes | 410 (77.7%) |
| No | 5640 (86.9%) | No | 103 (19.5%) |
| Prefer not to answer | 304 (4.7%) | Prefer not to answer | 15 (2.8%) |
Table 2.
Medical student and resident specific questions
| Medical Studentsa (N = 5260) | N (%)* |
|---|---|
| Clinical level students only: Did your medical school formally excuse you from clinical duties (i.e., clerkship rotations, other clinical rotations or experiences) as a result of the COVID-19 pandemic?* (N = 2426 clinical level students) | |
| Yes | 2044 (84.3%) |
| No | 231 (9.5%) |
| Prefer not to answer | 151 (6.22%) |
| Are you currently working clinically? | |
| Yes, I am currently working in my planned clinical rotations as a medical student | 246 (4.7%) |
| Yes, I am currently working clinically but in other ways at this time | 227 (4.3%) |
| No, I am not working clinically | 2033 (38.7%) |
| No, I am not working clinically because I am in the pre-clinical stage of training | 2483 (47.2%) |
| Prefer not to answer | 271 (5.1%) |
| If your medical school has excused you from clinical duties or moved your scheduled curriculum to online learning modalities, did you leave or depart from your primary residence (i.e., where you live during the school year) to go to another location during this time?** | |
| Parent(s) or family member’s house | 2028 (38.6%) |
| Friend’s house | 58 (1.1%) |
| Somewhere else | 132 (2.5%) |
| Did not leave | 2624 (49.9%) |
| Prefer not to answer | 135 (2.6%) |
| How are you spending your time at the moment?** | |
| My learning/training has not been disrupted so I am spending my time as I typically would during the medical school year | 757 (14.4%) |
| My learning is now online as coordinated by the medical school | 3587 (68.2%) |
| I am engaging in self-directed learning | 2322 (44.1%) |
| I am studying for licensing examinations | 838 (15.9%) |
| I am working on research or scholarly projects | 887 (16.9%) |
| I am volunteering | 622 (11.8%) |
| I am helping with contact tracing | 140 (2.7%) |
| I am taking this time to relax or rest | 1913 (36.4%) |
| I am taking care of someone who is ill | 123 (2.3%) |
| I am personally unwell and need to self-isolate | 121 (2.3%) |
| I am spending this time taking care of my children/family | 437 (8.3%) |
| I am taking this time to engage in more wellness activities than I usually would | 1654 (31.4%) |
| Other | 267 (5.1%) |
| Prefer not to answer | 26 (0.5%) |
| If Yes to volunteering: How are you currently volunteering?** | |
| Contact tracing | 102 (1.9%) |
| Call centres | 122 (2.3%) |
| Screening centres | 64 (1.2%) |
| Providing child care to healthcare professionals | 79 (1.5%) |
| Providing child care to others | 27 (0.5%) |
| Other | 357 (6.8%) |
| Prefer not to answer | 19 (0.4%) |
| Have you participated in any online learning during this time that was coordinated or organized by your medical school for aspects of your core curriculum (e.g., lectures or clerkship teaching sessions on Zoom)? (N = 4938 valid responses) | |
| Yes | 3997 (80.9%) |
| No | 914 (18.5%) |
| Prefer not to answer | 27 (0.5%) |
|
If yes to Online learning: Do you feel that the quality of your medical education will be lower as a result of any online learning your school is coordinating at this time? (N=3919 valid responses) | |
| Yes | 2608 (66.5%) |
| No | 1225 (31.3%) |
| Prefer not to answer | 86 (2.2%) |
| If yes to Online learning: Do you have any challenges accessing online learning modalities (e.g., Zoom, online lectures)? (N=3919 valid responses)** | |
| I have difficulties accessing a computer | 89 (2.27%) |
| I have difficulties accessing the internet | 431 (11.0%) |
| I have difficulties learning from home | 835 (21.3%) |
| I have other difficulties | 202 (5.15%) |
| No, I do not have any difficulties accessing online learning | 2743 (70.0%) |
| Prefer not to answer | 31 (0.79%) |
| How has the COVID-19 pandemic directly impacted your clinical electives? | |
| My visiting electives at other institutions have been cancelled or postponed at this time | 1027 (19.5%) |
| My core electives at my own medical school have been cancelled or postponed at this time | 1235 (23.5%) |
| My electives have not yet been influenced at this time | 203 (3.9%) |
| Not applicable, as all of my electives have been completed | 213 (4.0%) |
| Prefer not to answer | 110 (2.1%) |
| How has the COVID-19 pandemic influenced your career decision-making (e.g., residency interests, career planning)?** | |
| It has influenced the residency program(s) I wish to apply to | 564 (10.7%) |
| It has increased my interest in Public Health as a specialty | 600 (11.4%) |
| It has increased my interest in Infectious Diseases as a specialty | 600 (11.4%) |
| It has increased my interest in Family Medicine as a specialty | 314 (6.0%) |
| It has increased my interest in other programs (open-ended) | 268 (5.1%) |
| It has not influenced my career decision making or interests | 2944 (56.0%) |
| Prefer not to answer | 130 (2.5%) |
| Residentsb (N = 1148) | N (%) |
| Setting | |
| Urban | 766 (66.7%) |
| Rural | 121 (10.5%) |
| Other | 23 (2.0%) |
| Prefer not to answer | 238 (20.7%) |
| Program | |
| Anesthesiology | 50 (4.4%) |
| Emergency Medicine | 30 (2.6%) |
| Family Medicine | 142 (12.3%) |
| Internal Medicine (core) | 147 (12.8%) |
| Medical Subspecialty | 38 (3.3%) |
| Neurology | 11 (1.0%) |
| Obstetrics and Gynecology | 45 (3.9%) |
| Pediatrics | 42 (3.6%) |
| Public Health | 28 (2.4%) |
| Psychiatry | 42 (3.6%) |
| Radiology | 19 (1.6%) |
| Surgery | 113 (9.8%) |
| Other | 290 (25.3%) |
| Prefer not to answer | |
| Are you working more than usual during the COVID-19 pandemic? | |
| Yes, I am working more than usual | 184 (16.0%) |
| No, I am working the same amount | 254 (22.1%) |
| No, I am working less than usual | 421 (36.7%) |
| Prefer not to answer | 289 (25.1%) |
| FM or Psychiatry Residents: Do you think residents in these programs could potentially be utilized at this time to provide peer-to-peer mental health support and/or counseling to other residents or healthcare professionals at this time over videoconferencing modalities (N=184) | |
| Yes, I think we could be useful to provide mental health supports at this time to any and all other residents at this time | 89 (48.4%) |
| Yes, I think we could be useful to provide mental health supports at this time to residents who are working at the front lines of care, or who may be additionally stressed or burnt out as a result of the pandemic | 66 (35.9%) |
| Yes, I think we could be useful to provide mental health supports at this time to other healthcare professionals (e.g., nursing) at this time | 50 (27.2%) |
| No, I do not think we could be useful at this time in providing mental health supports to other residents | 51 (27.7%) |
N=5260 respondents for medical student-specific items; bN=1148 respondents for resident-specific items – participants who did not specify their level of training could complete the resident-specific items; *N= % = of all respondents for at that level for each item; **participants could select all options that applied;
Table 3.
Shared questions
| Which of the following are concerns or stressors for you at this time?** | Medical Student | Resident | Did not specify level | Total |
|---|---|---|---|---|
| My personal health and well-being | 2281 (43.4%) | 440 (43.7%) | 58 (25.8%) | 2779 (42.8%) |
| The health and well-being of my family members | 3518 (66.9%) | 605 (60.1%) | 87 (38.7%) | 4210 (64.9%) |
| The health and wellbeing of the public | 2761 (52.49%) | 509 (50.6%) | 72 (32.0%) | 3342 (51.5%) |
| My personal financial situation | 1391 (26.5) | 200 (19.9%) | 51 (22.7%) | 1642 (25.3%) |
| The financial situation of others | 2089 (39.7%) | 339 (33.7%) | 57 (25.3%) | 2485 (38.3%) |
| The impact of this pandemic on my learning | 3046 (57.9%) | 468 (46.5%) | 71 (31.6%) | 3585 (55.2%) |
| Other | 253 (4.81%) | 83 (8.24%) | 9 (4.00%) | 345 (5.31%) |
| Would you consider yourself more anxious during this time than you typically are during the year? | Medical Student (N = 4361) | Resident (N = 737) | Did not specify level (N = 131) | Total (N = 5229) |
| Yes | 2505 (57.4%) | 547 (74.2%) | 65 (49.6%) | 3117 (59.6%) |
| No | 1779 (40.8%) | 181 (24.6%) | 51 (38.9%) | 2011 (38.5%) |
| Prefer not to answer | 77 (1.8%) | 9 (1.22%) | 15 (11.5%) | 101 (1.93%) |
| Are you practicing social or physical distancing? | Medical Student (N = 4367) | Resident (N = 742) | Did not specify level (N = 132) | Total (N = 5241) |
| Almost always | 3206 (73.4%) | 430 (58.0%) | 72 (54.5%) | 3708 (70.7%) |
| As much as I can | 1099 (25.2%) | 293 (39.5%) | 51 (38.6%) | 1443 (27.5%) |
| Not at all | 49 (1.1%) | 13 (1.75%) | 4 (3.03%) | 66 (1.26%) |
| Prefer not to answer | 13 (0.3%) | 6 (0.81%) | 5 (3.79%) | 24 (0.46%) |
| Have you had to quarantine or self-isolate? | Medical Student (N = 4360) | Resident (N = 741) | Did not specify level (N = 130) | Total (N = 5231) |
| Yes | 596 (13.7%) | 160 (21.6%) | 19 (14.6%) | 775 (14.8%) |
| No | 3749 (86.0%) | 574 (77.5%) | 103 (79.2%) | 4426 (84.6%) |
| Prefer not to answer | 15 (0.34%) | 7 (0.94%) | 8 (6.15%) | 30 (0.57%) |
| Are you being asked by others to provide medical expertise or information regarding the COVID-19 pandemic?** | Medical Student | Resident | Did not specify level | Total |
| Yes – Family | 2477 (38.2%) | 529 (52.5%) | 71 (31.6%) | 3077 (47.4%) |
| Yes – Friends | 1965 (30.3%) | 452 (44.9%) | 60 (26.7%) | 2477 (38.2%) |
| Yes – Others | 591 (9.10%) | 180 (17.9%) | 23 (10.2%) | 794 (12.3%) |
| No | 1392 (21.4%) | 111 (11.0%) | 38 (16.9%) | 1541 (23.7%) |
| Prefer not to answer | 46 (0.71%) | 10 (0.99%) | 5 (2.22%) | 61 (0.94%) |
| Are you using social media to communicate to others about COVID-19? | Medical Student | Resident | Did not specify level | Total |
| Yes – Twitter | 506 (7.79%) | 123 (12.2%) | 25 (11.1) | 654 (10.1%) |
| Yes – Instagram | 1065 (16.40%) | 135 (13.4%) | 37 (16.4%) | 1237 (19.1%) |
| Yes – Facebook | 1208 (18.6%) | 247 (24.5%) | 38 (16.9%) | 1493 (23.0%) |
| Yes - Other | 352 (5.42%) | 78 (7.75%) | 25 (11.1%) | 455 (7.01%) |
| No | 2220 (34.2%) | 347 (34.5%) | 45 (20.0%) | 2612 (40.2%) |
| Prefer not to answer | 58 (0.89%) | 9 (0.89%) | 11 (4.89%) | 78 (1.20%) |
N=respondents for each question; questions were not mandatory so total number of responses per question does not equal the total number of participants throughout the study; **“select all that apply” question percentages calculated using sample size for each level of training (N = 5260 for medical students, N = 1007 for residents, N = 225 for participants who did not specify) or the total sample size (N = 6492) if not specified
Table 4.
Considerations for medical education during COVID-19
| Area | Considerations for Medical Schools and Residency Programs |
|---|---|
| Teaching and Learning |
|
| Utilizing Learners |
|
| Supporting Learners |
|
| Communicating with Learners |
|
| Policy, Planning, and Decision Making |
|
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
Funding: This study was funded by the O’Brien Institute for Public Health through a Catalyst Grant to support the timely back-translation and analysis of the qualitative data to English. O’Brien Institute for Public Health did not influence the design, conduct, collection, analysis, or interpretation of data, or the writing of the manuscript for publication.
References
- 1.Association of American Medical Colleges . Important guidance for medical students on clinical rotations during the Coronavirus (COVID-19) outbreak | AAMC, 2020. Available from: https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak [Accessed Jul 14 2020]
- 2.Rose S. medical student education in the time of COVID-19. J Am Med Assoc. 2020;323(21):2131-2. 10.1001/jama.2020.5227 [DOI] [PubMed] [Google Scholar]
- 3.Harvey A. Covid-19: medical students and FY1 doctors to be given early registration to help combat covid-19. BMJ 2020;368(March):m1268. Available from: 10.1136/bmj.m1268 [DOI] [PubMed] [Google Scholar]
- 4.Rambaldini G, Wilson K, Rath D, et al. The impact of severe acute respiratory syndrome on medical house staff: a qualitative study. J Gen Intern Med. 2005. May 20(5):381-5. 10.1111/j.1525-1497.2005.0099.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sherbino J, Atzema C. "SARS-Ed": Severe acute respiratory syndrome and the impact on medical education. Ann Emerg Med. 2004;44(3):229-31. 10.1016/j.annemergmed.2004.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rieder MJ, Salvadori M, Bannister S, Kenyon C. Collateral damage: the effect of SARS on medical education. Clin Teach. 2004;1(2):85-9. 10.1111/j.1743-498X.2004.00026.x [DOI] [Google Scholar]
- 7.Landis MS, Bradley JW. The Impact of the 2003 SARS outbreak on medical students at the University of Toronto. Univ Toronto Med. 2005;0-6. Available from: https://pdfs.semanticscholar.org/c574/8067e223ea25670788e0a4ca13d0771dccd3.pdf [Google Scholar]
- 8.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Can Med Assoc J. 2003;168(10):1245-51. [PMC free article] [PubMed] [Google Scholar]
- 9.Bai YM, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55(9):1055-7. 10.1176/appi.ps.55.9.1055 [DOI] [PubMed] [Google Scholar]
- 10.Crawford BE, Kahn MJ, Gibson JW, Daniel AJ, Krane NK. Impact of Hurricane Katrina on medical student academic performance: the tulane experience. Am J Med Sci. 2008;336(2):142-6. 10.1097/MAJ.0b013e318180f1b7 [DOI] [PubMed] [Google Scholar]
- 11.DiCarlo RP, Hilton CW, Chauvin SW, et al. Survival and recovery: Maintaining the educational mission of the Louisiana State University School of Medicine in the aftermath of Hurricane Katrina. Acad Med. 2007;82(8):745-56. 10.1097/ACM.0b013e3180cc279b [DOI] [PubMed] [Google Scholar]
- 12.Tolsgaard MG, Cleland J, Wilkinson T, Ellaway RH. How we make choices and sacrifices in medical education during the COVID-19 pandemic. Med Teach. 2020;42(7):741-3. 10.1080/0142159X.2020.1767769 [DOI] [PubMed] [Google Scholar]
- 13.Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Heal Care. 2003;15(3):261-6. 10.1093/intqhc/mzg03 [DOI] [PubMed] [Google Scholar]
- 14.Streiner DL, Norman GR, Cairney J. Health measurement scales : a practical guide to their development and use. 399 p. [Google Scholar]
- 15.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992. September 12;31(3):301-6. 10.1111/j.2044-8260.1992.tb00997.x [DOI] [PubMed] [Google Scholar]
- 16.Kassam A, Ellaway R. Acknowledging a holistic framework for learner wellness. Acad Med. 2020. January;95(1):9-10. 10.1097/ACM.0000000000003026 [DOI] [PubMed] [Google Scholar]
- 17.World Bank . How does the World Bank classify countries? Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries [Accessed Jul 13 2020].
- 18.Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: a methods sourcebook. 2014. 381 p. [Google Scholar]
- 19.O'Connor C, Joffe H. Intercoder Reliability in Qualitative Research: Debates and Practical Guidelines. Int J Qual Methods. 2020;19:1-13. 10.1177/1609406919899220 [DOI] [Google Scholar]
- 20.Mian A, Khan S. Medical education during pandemics: a UK perspective. BMC Med. 2020;18(1):18-9. 10.1186/s12916-020-01577-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019; 10.1080/10872981.2019.1666538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldhamer MEJ, Pusic M V, Co JPT, Weinstein DF. Can Covid catalyze and educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;1-3. [DOI] [PubMed] [Google Scholar]
- 23.Sklar DP. COVID-19: lessons from the disaster that can improve health professions education. Acad Med 2020; 10.1097/ACM.0000000000003547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallagher TH, Schleyer AM. "We signed up for this!"-Student and trainee responses to the Covid-19 pandemic. N Engl J Med. 2020;382(25):e96( 1-3). 10.1056/NEJMp2005234 [DOI] [PubMed] [Google Scholar]
- 25.Kalet al, Jotterand F, Muntz M, Thapa B, Campbell B. Hearing the call of duty: what we must do to allow medical students to respond to the COVID-19 pandemic. Wis Med J. 2020; [PubMed] [Google Scholar]
- 26.Herman B, Rosychuk RJ, Bailey T, Lake R, Yonge O, Marrie TJ. Medical students and pandemic influenza. Emerg Infect Dis. 2007;13(11):1781-3. 10.3201/eid1311.070279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li HO-Y, Bailey AMJ. Medical education amid the COVID-19 pandemic. Acad Med. 2020; Published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Long N, Wolpaw DR, Boothe D, et al. Contributions of health professions students to health system needs during the COVID-19 pandemic: potential strategies and process for US medical schools. Acad Med. 2020, 95(11). 10.1097/ACM.0000000000003611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menon A, Klein EJ, Kollars K, Kleinhenz ALW. Medical students are not essential workers: examining institutional responsibility during the COVID-19 pandemic. Acad Med. 2020; 10.1097/ACM.0000000000003478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flotte TR, Larkin AC, Fischer MA, et al. Accelerated graduation and the deployment of new physicians during the COVID-19 pandemic. Acad Med. 2020; Publish Ah. 10.1097/ACM.0000000000003540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klasen JM, Vithyapathy A, Zante B, Burm S. "The storm has arrived": the impact of SARS-CoV-2 on medical students. Perspect Med Educ. 2020;9(3):181-5. 10.1007/s40037-020-00592-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brand PLP. COVID-19: a unique learning opportunity if the well-being of learners and frontline workers is adequately supported. Perspect Med Educ. 2020;9(3):129-31. 10.1007/s40037-020-00596-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Simonds AK, Sokol DK. Lives on the line? Ethics and practicalities of duty of care in pandemics and disasters. Eur Respir J. 2008;34(2):303-9. 10.1183/09031936.00041609 [DOI] [PubMed] [Google Scholar]
- 34.Bauchner H, Sharfstein J. A bold response to the COVID-19 pandemic: medical students, national service, and public health. JAMA. 2020;323(18):1790-1. 10.1001/jama.2020.6166 [DOI] [PubMed] [Google Scholar]
- 35.Venkatesh A, Edirappuli S. Social distancing in covid-19: What are the mental health implications? Br Med. 2020;369(April):2020. 10.1136/bmj.m1379 [DOI] [PubMed] [Google Scholar]
- 36.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw open. 2020;3(3):e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: A systematic review and meta-analysis. Vol. 55, European Psychiatry. 2019. 10.1016/j.eurpsy.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 39.Puthran R, Zhang MWB, Tam WW, Ho RC. Prevalence of depression amongst medical students: A meta-analysis. Med Educ. 2016;50(4). 10.1111/medu.12962 [DOI] [PubMed] [Google Scholar]
- 40.Quek TTC, Tam WWS, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Vol. 16, Int. J. Environ. Res. Public Health. 2019. 10.3390/ijerph16152735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med. 2020;1-2. 10.1056/NEJMp2003149 [DOI] [PubMed] [Google Scholar]
- 42.O'Byrne L. Medical students and COVID-19: the need for pandemic preparedness. J Med Ethics. 2020; 10.1136/medethics-2020-106353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kachra R, Brown A. The new normal: medical education during and beyond the COVID-19 pandemic. Can Med Educ J. 2020;4-6. 10.36834/cmej.70317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The Association of Faculties of Medicine of Canada . Ten Guiding Principles for Medical Education [Internet]. 2020. Available from: https://afmc.ca/sites/default/files/pdf/2020-Ten_Guiding_Principles_for_Medical_Education_COVID_Era_en.pdf [Accessed Jul 14 2020].
- 45.The Coalition for Physician's Accountability Work Group on Medical Students in the Class of 2021 . Final report and recommendations for medical education institutions of LCME-Accredited, U.S. Osteopathic, and Non-U.S. medical school applicants. Available from: https://www.aamc.org/system/files/2020-05/covid19_Final_Recommendations_Executive_Summary_Final_05112020.pdf [Accessed Jul 14 2020].
- 46.Cleland J, McKimm J, Fuller R, Taylor D, Janczukowicz J, Gibbs T. Adapting to the impact of COVID-19: sharing stories, sharing practice. Med Teach. 2020;42(7):772-5. 10.1080/0142159X.2020.1757635 [DOI] [PubMed] [Google Scholar]
- 47.Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-2. 10.1097/ACM.0000000000003402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dawe R. A plea for program evaluation in a pandemic. Can Med Educ J. 2020;11(6):170-1. 10.36834/cmej.70331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mehta N, Sayed C, Sharma R, Do V. Medical education advances and innovations: a silver lining during the COVID-19 pandemic. Can Med Educ J. 2020;11(6):141-4. 10.36834/cmej.70926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pablos-Méndez A, Vega J, Aranguren FP, Tabish H, Raviglione MC. Covid-19 in Latin America. BMJ. 2020. July 27; 370. 10.1136/bmj.m2939 [DOI] [PubMed] [Google Scholar]