Abstract
Background Patients who use patient portals may be more engaged and empowered in their care; however, differences in who accesses patient portals remain. The characteristics of who uses patient portals more frequently and who perceives them as useful may also differ, as well as which functions people use.
Objective We assessed the characteristics of patient portal users to examine who uses them more frequently and who perceives them as useful. In addition, we wanted to see if those who use them more frequently or perceive them to be more useful use different functions or more functions of patient portals.
Methods Pooled cross-sectional data from 2017 to 2018 Health Information National Trends Survey (HINTS) were used. Ordinal regression models were developed to assess frequency of use and perceived usefulness by demographics, and multivariable logistic regression models were used to examine the association between the use of 10 patient portal functions and frequency of use and perceived usefulness of patient portals.
Results The odds of using patient portals more frequently were higher among those with Bachelor's degrees, incomes between $35,000 and $75,000, and those with two or more chronic conditions. Respondents with three or more chronic conditions had higher odds of rating patient portals as useful. Those who used their patient portal 10 or more times in the past year had higher odds of using all functions except for viewing test results compared with those who used their patient portal one to two times per year. Those who rated patient portals as “very useful” had higher odds of using seven of the functions compared with those who rated them “not very”/“not at all useful.”
Conclusion It is important to continue to assess usefulness, frequency of use, and overall patient portal function use to identify opportunities to increase patient engagement with patient portals.
Keywords: patient portals, electronic health record, surveys and questionnaires, public health surveillance
Background and Significance
Digital technology that gives patients access to their medical record information can promote patient engagement and potentially improve healthcare quality. Indeed, the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009, and more recently the 21st Century Cures Act of 2016, recognized that the diffusion of digital technologies, such as patient portals, is necessary to enhance care continuity, encourage patient self-care management, and address broader population health needs. 1 2 Patient portals are internet-enabled personal health record tools that allow patients to manage and share health-related information, schedule appointments and view test results. 3 4 5 6 Patient portals are tethered to an institution's electronic health records, which are tools for providers to manage care. 7 Previous research indicates that patient portals can improve disease self-management and empower patients to engage in their medical care, 8 9 10 11 12 which may also help explain why health care organizations have invested heavily in patient portal infrastructure to support the delivery of patient-centered care. 13
Despite the potential for patient portals to enable patients to actively engage in their care, adoption remains low. 14 A literature review and meta-analysis found that the mean adoption rate of patient-facing patient portals was approximately 52% across 40 studies conducted from 2002 to 2016. Notably, the rate was only 23% on average in real-world studies compared with 71% in controlled experiments. 15 Variability in internet access across sociodemographic characteristics such as gender, race and ethnicity, income, and rurality have also likely contributed to differences and disparities in patient portal adoption and use. 16 17 18 19 20 Studies have identified the lack of infrastructure (e.g., access to broadband internet, smartphones, or computers), limited technical skills, not being offered access to a patient portal, and concerns about data security as factors that limit the adoption and use of these and similar technologies. 7 21 22 For example, El-Toukhy et al 16 found that patients with lower educational attainment, no health insurance, no regular doctor, and lower English proficiency were less likely to access and use specific functions of their patient portals (e.g., refill medications or message a provider). However, the authors also discovered that patient knowledge and use of specific patient portal functions varied (i.e., certain functions were used more than others by those who accessed their patient portal in the previous year), and that few demographic characteristics predicted patients' likelihood of using each function other than older age and lower education levels were associated with using some functions less frequently. 16 Therefore, if many patients are not using most or all available functions, it raises significant concerns that patients are not realizing the full potential of patient portals to help them manage their health.
In the field of user-centered design, a patient's context, defined as the goals of the user and the environmental characteristics of the situation in which a product will be used, 23 can influence how and when they use their patient portal. A patient's context can help explain the circumstances in which they use (or do not use) a patient portal to manage their health. At the same time, a person's experience with a specific technology (e.g., patient portals) is a relevant characteristic that can influence a person's likelihood of using that technology to achieve their health goal(s). According to the Diffusion of Innovation Theory, 24 a patient is more likely to find their patient portal useful if the technology aligns with their preferences for interacting with their health care provider or for managing their health conditions. Also, a patient's prior experience with using a patient portal is likely to shape their subsequent use (or nonuse) of the patient portal such that more positive experiences are likely to influence ongoing use of the technology. 25 In addition, the convenience and ease with which patients can request prescription refills, ask questions, and schedule appointments via the patient portal can also contribute to why patients perceive this specific type of technology to be useful for managing their health, thus helping to explain why patients may choose to use the technology. 13 26
Given our expectation that a patient's context of use—defined as a patient's frequency of patient portal use and perceptions about patient portal usefulness—can provide valuable information about how they use their patient portal—defined as which functions a patient uses—to manage their health needs, we aimed to explore the relationship between patient portal use and perceptions of usefulness. Specifically, we hypothesized that (1) patients who use their patient portal more frequently will be more likely to use each of the patient portal functions compared with patients who used their patient portal less frequently, and (2) patients who perceive the patient portals as useful will be more likely to use each of the patient portal functions compared with patients who perceive the patient portals as not very useful. As existing patient portals continue to evolve, health care managers and patient portal developers may find value in understanding patients' perceptions about and interactions with patient portals to the extent that this information can be used to help make patient portals more patient centered. Improving our understanding of these relationships can help inform health care systems' efforts to support patient use of patient portals.
Objectives
In this study, we sought to assess the characteristics of who uses patient portals, who uses them more frequently, and who perceives them as useful. In addition, we wanted to see if those who use them more frequently or perceive them as more useful use different functions or more functions of the patient portals than those who are infrequent users or find them not useful.
Methods
Sample
Data were from 2017 to 2018 Health Information National Trends Survey (HINTS) 5 (cycle 1 and 2), a nationally representative mail survey of adults (≥18 years old) sponsored by the National Cancer Institute. 27 HINTS asks questions about cancer prevention and risk behaviors, health information usage, cancer beliefs, technology use, care received, and demographic information. Data for our final sample were drawn in a two-phase process. In the first phase, adults were sampled from a random selection of residential addresses from the U.S. Postal Service. In the second phase, an adult within the household was selected with the nearest upcoming birthday. 28 Response rates were 32% for HINTS 5 cycle 1 (2017) and 33% for HINTS 5 cycle 2 (2018). We included respondents only if they answered “yes” to the HINTS 5 question: “Have you ever been offered online access to your medical records by your health care provider or health insurer?” and if they provided a response to the question: “How many times did you access your online medical record in the last 12 months?” The respondents could respond with the number of times they accessed their record even if they indicated that they had not been offered access in 2017; they were classified as accessing their record zero times if they had not been offered access in 2018. The inclusion of only those respondents who had been offered access reduced inconsistencies between the data years.
Measures
Frequency of patient portal use was assessed by using responses to the question: “How many times did you access your online medical record in the last 12 months?” (“none,” “1–2 times,” “3–5 times,” “6–9 times,” and “10 or more times”). Perceived usefulness of patient portals was assessed with: “In general, how useful is your online medical record for monitoring your health?” (“very useful,” “somewhat useful,” “not very useful,” and “not at all useful”). This question was only asked if the respondent indicated that they used their patient portal at least once in the previous 12 months. Respondents who had accessed their patient portal at least once in the previous 12 months were asked questions approximately 10 specific patient portal functions: “In the past 12 months, have you used your online medical record to…” (1) add health information to share with your health care provider” (add health info), (2) “download your health information to your computer or mobile device” (download info), (3) “make appointments with a health care provider” (make appointments), (4) “help make you make a decision about how to treat an illness or condition” (make decisions), (5) “securely message health care provider staff” (message providers), (6) “monitor your health” (monitor health), (7) “fill out forms or paperwork related to your healthcare” (complete paperwork), (8) “request a refill of medications” (request refills), (9) “request the correction of inaccurate information” (request corrections), and (10) look up test results” (view test results) (“yes,” “no”).
Additional sociodemographic and clinical characteristic data used in our analyses included gender (male/female), age (18–34/35–49/50–64/65–74/75+ years), race/ethnicity (non-Hispanic White/non-Hispanic Black/Hispanic/Other), education (high school graduate or less/some college/bachelor's degree or more), income (under $35,000/$35,000–$75,000/over $75,000), metropolitan status (metro area/nonmetro area), insurance status (insured/uninsured), number of chronic conditions (0, 1, 2, 3, or more), last routine checkup (within past year/one or more years ago), and survey year (2017/2018).
Analysis
All data were analyzed by using survey weights based on population estimates from the American Community Survey to account for nonresponse and coverage error, making the results more generalizable to the population based on HINTS protocols. 29 As is best practice with the HINTS data, jackknife replicate weights were used to provide bias-corrected variance estimates. 30 We used weighted descriptive statistics to analyze the pooled 2017 and 2018 sample, comparing those who ever used patient portals to those who did not if they said “yes” to having ever been offered a portal. Chi-square tests were used to test for associations between sociodemographic characteristics and patient portal use. Weighted ordinal regression models were developed to assess frequency of use (i.e., 1–2, 3–5, 6–9, and 10 or more times) and perceived usefulness (i.e., not very/not at all useful, somewhat useful, and very useful). For usefulness, only 28 respondents answered “not at all useful” so this was combined with the response “not very useful” for analysis. Brant tests were performed to assess proportional odds across response categories for the ordinal models. We calculated the frequencies and percentages of respondents who answered “yes,” “no,” or had missing data for each of the 10 patient portal functions ( Fig. 1 ).
Fig. 1.
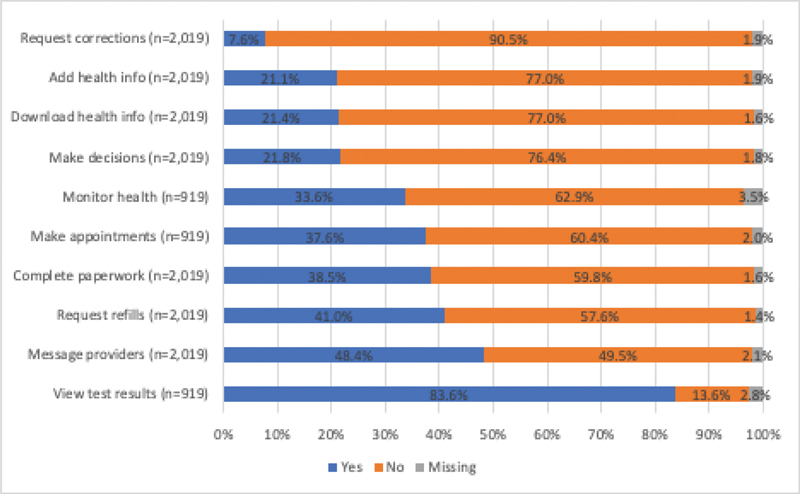
Proportion of respondents using each patient portal function at least once in the past 12 months.
Finally, we estimated weighted multivariable logistic regression models to examine the association between the use of each of the 10 patient portal functions and the two main independent variables (1) frequency of patient portal use and (2) perceived usefulness of patient portal, controlling for sociodemographic characteristics (i.e., gender, age, education, income, metropolitan status, insurance status, number of chronic conditions, and last routine checkup). Survey year was omitted from these analyses because not all 10 functions were asked in both data years: monitor health, make appointments, and view test results were only asked in 2017. Results were considered significant for p -values less than 0.05. All analyses were completed by using Stata version 14.2 (2015, StataCorp LP, College Station, Texas, United States).
Results
Of the 3,466 respondents who said “yes” to being offered a patient portal by their healthcare provider or health insurer, approximately 58.3% indicated that they had used a patient portal at least once in the previous year. Demographic characteristics are summarized in Table 1 . The majority of the sample was female, non-Hispanic White, lived in a metropolitan area, had health insurance, and reported seeing a doctor within the past year. Unadjusted, bivariate analyses indicated that there were significant associations between patient portal use and seven of the weighted factors: age (Χ 2 [4] = 46.7, p = 0.0034), race (Χ 2 [3] = 29.2, p = 0.0036), education (Χ 2 [2] = 178.0, p < 0.0001), income (Χ 2 [2] = 128.0, p < 0.0001), metropolitan status (Χ 2 [1] = 9.6, p = 0.0344), insurance status (Χ 2 [1]= 23.9, p = 0.0311), and last routine checkup (Χ 2 [1]= 24.7, p = 0.0052).
Table 1. Sample population from Health Information National Trends Survey 5 Cycle 1 (2017) and 2 (2018) data.
| Characteristic | Total ( n = 3,466) n |
Did not use patient portal (
n
= 1,447)
n (weighted %) |
Used patient portal one or more times (
n
= 2,019)
n (weighted %) |
p -Value |
|---|---|---|---|---|
| Gender | 0.570 | |||
| Male | 1,227 | 510 (43.0) | 717 (57.0) | |
| Female | 2,194 | 911 (41.4) | 1,283 (58.6) | |
| Age | 0.003 | |||
| 18–34 | 384 | 132 (40.0) | 252 (60.0) | |
| 35–49 | 751 | 270 (37.7) | 481 (62.3) | |
| 50–64 | 1,159 | 461 (40.1) | 698 (59.9) | |
| 65–74 | 752 | 349 (50.5) | 403 (49.5) | |
| 75+ | 339 | 191 (57.8) | 148 (42.2) | |
| Race/ethnicity | 0.004 | |||
| Non-Hispanic White | 2,209 | 875 (41.9) | 1,334 (58.2) | |
| Non-Hispanic Black | 415 | 194 (43.3) | 221 (56.7) | |
| Hispanic | 352 | 166 (45.5) | 186 (54.5) | |
| Non-Hispanic Other | 247 | 82 (25.2) | 165 (74.8) | |
| Education | <0.001 | |||
| High school or less | 617 | 363 (58.8) | 254 (41.2) | |
| Some college | 991 | 456 (44.4) | 535 (55.6) | |
| Bachelor's or more | 1,810 | 602 (30.1) | 1,208 (69.9) | |
| Income | <0.001 | |||
| Less than $35,000 | 729 | 430 (57.1) | 299 (42.9) | |
| $35,000–$75,000 | 1,004 | 435 (46.3) | 569 (53.7) | |
| Greater than $75,000 | 1,421 | 431 (32.3) | 990 (67.7) | |
| Metro status | 0.034 | |||
| Metro area | 3,001 | 1,217 (41.2) | 1,784 (58.8) | |
| Nonmetro area | 465 | 230 (48.8) | 235 (51.2) | |
| Insurance | 0.031 | |||
| Insured | 3,356 | 1,381 (41.2) | 1,975 (58.8) | |
| Not insured | 89 | 53 (62.6) | 36 (37.4) | |
| Number of chronic conditions | 0.194 | |||
| 0 | 971 | 391 (42.7) | 580 (57.3) | |
| 1 | 979 | 392 (41.4) | 587 (58.6) | |
| 2 | 729 | 301 (37.3) | 428 (62.7) | |
| 3 or more | 668 | 302 (46.7) | 366 (53.3) | |
| Last routine checkup | 0.005 | |||
| Within past year | 2,739 | 1,084 (39.3) | 1,655 (60.7) | |
| More than 1 year ago | 675 | 334 (49.1) | 341 (50.9) | |
| Survey year | 0.547 | |||
| 2017 | 1,633 | 714 (43.1) | 919 (56.9) | |
| 2018 | 1,833 | 733 (41.4) | 1,100 (58.6) |
Frequency of Portal Use and Usefulness by Demographics
For respondents who used a patient portal at least once in the past year, the odds of using it more frequently were higher among those with Bachelor's degrees (1.6 [1.1–2.6]), incomes between $35,000 and $75,000 (OR = 1.6 [1.0–2.6]), and those with two (OR = 1.8 [1.2–2.8]) or three or more chronic conditions (OR = 2.6 [1.6–4.3]). Of those who used patient portals, those with 3 or more chronic conditions had higher odds of rating patient portals as useful (OR = 1.7 [1.1–2.7]) compared with those with no chronic conditions, and those who were ages 50 to 64 (OR = 0.6 [0.3–0.9]) or 75 and older (OR = 0.4 [0.2–0.8]), not insured (OR = 0.3 [0.1–0.9]), or had last had a routine checkup over a year ago (OR = 0.7 [0.5–1.0]) had lower odds of considering patient portals useful.
Use of Patient Portal Functions
The percent of respondents that answered “yes” to the use of each patient portal function ranged from 7.6% for correction of inaccurate information to 83.6% for looking up test results, followed by securely messaging providers (48.4%), requesting medication refills (41.0%), completing paperwork (38.5%), and making appointments (37.6%; Fig. 1 ).
Use of Patient Portal Functions by Frequency of Use and Usefulness
Compared with respondents who used their patient portal only one to two times in the past year, those who used their patient portal three to five times had higher odds of adding health information, making appointments, making decisions, messaging providers, completing paperwork, requesting refills, or requesting corrections, controlling for demographics ( Table 2 ). Those who used their patient portal six to nine times had higher odds of using all functions except for downloading health information; those using it 10 or more times in the past year had higher odds of using all functions except for viewing test results compared with those who used their patient portal once or twice per year.
Table 2. Weighted odds of using each of the 10 patient portal functions by frequency of use and perceived usefulness of patient portals to monitor one's health.
| Patient portal function | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Request corrections (
n
= 1,632)
OR (95% CI) |
Add health info (
n
= 1,635)
OR (95% CI) |
Download health info (
n
= 1,640)
OR (95% CI) |
Make decisions (
n
= 1,637)
OR (95% CI) |
Monitor health (
n
= 757)
OR (95% CI) |
Make appointments (
n
= 764)
OR (95% CI) |
Complete paperwork (
n
= 1,638)
OR (95% CI) |
Request refills (
n
= 1,638)
OR (95% CI) |
Message providers (
n
= 1,636)
OR (95% CI) |
View test results (
n
= 845)
OR (95% CI) |
|
| Frequency of use | ||||||||||
| 1–2 ( n = 966) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 3–5 ( n = 646) | 2.4 (1.2–4.8) | 2.5 (1.5–4.1) | 1.3 (0.8–2.1) | 2.1 (1.3–3.3) | 1.5 (0.7–3.2) | 2.6 (1.5–4.6) | 1.8 (1.2–2.9) | 1.6 (1.1–2.3) | 3.3 (2.3–4.7) | 2.6 (1.0–6.8) |
| 6–9 ( n = 204) | 4.8 (1.9–12.3) | 5.4 (3.2–9.1) | 1.7 (0.9–3.2) | 3.8 (2.1–6.7) | 4.6 (1.7–12.3) | 2.9 (1.3–6.7) | 3.0 (1.8–5.0) | 3.2 (1.9–5.3) | 6.6 (3.5–12.5) | 19.7 (7.4–52.2) |
| ≥10 ( n = 203) | 8.0 (3.8–16.8) | 6.0 (3.3–10.8) | 3.8 (2.3–6.5) | 7.1 (4.1–12.5) | 3.8 (1.2–12.0) | 4.7 (1.7–13.0) | 3.1 (1.8–5.4) | 5.5 (3.0–9.9) | 4.6 (2.5–8.5) | 12.4 (0.1–1894.6) |
| Usefulness | ||||||||||
| Not at all/not very useful ( n = 179) | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Somewhat ( n = 831) | 0.6 (0.1–3.1) | 1.7 (0.7–4.1) | 1.7 (0.8–3.6) | 1.4 (0.6–3.4) | 2.4 (0.5–11.3) | 1.3 (0.3–4.9) | 1.3 (0.8–2.3) | 1.9 (0.9–3.9) | 2.1 (1.1–3.8) | 2.5 (0.8–7.6) |
| Very ( n = 833) | 1.4 (0.3–6.9) | 3.8 (1.4–10.0) | 2.1 (0.9–4.8) | 3.2 (1.3–8.1) | 7.6 (1.9–30.1) | 3.3 (0.9–12.8) | 2.1 (1.2–3.6) | 3.1 (1.5–6.6) | 4.5 (2.5–8.0) | 5.3 (1.4–19.7) |
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference category.
Note: All models control for all sociodemographic characteristics (i.e., gender, age, education, income, metropolitan status, insurance status, number of conditions, and last routine checkup).
Those who rated patient portals as “somewhat useful” had significantly higher odds of messaging providers than those who rated patient portals as “not very”/“not at all useful.” Those who rated patient portals as “very useful” had higher odds of using each of the functions except for requesting corrections, downloading health information, or making appointments compared with those who rated them “not very”/“not at all useful.”
Discussion
Patient portals represent an important tool to help patients engage in their health care. However, our analysis of a U.S. based survey showed that, overall, patient portals are accessed infrequently, and a majority of patient portal functions go unused by the general population. Our findings about the association of age, race, and socioeconomic status with accessing a patient portal at all are consistent with the results of previous research. 16 31 Despite the use of patient portals at all being associated with several sociodemographic characteristics, many of these characteristics were not associated with frequency of patient portal use; only having a Bachelor's degree or more education, reporting an income of $35,000 to $75,000 compared with <$35,000 and having two or more chronic conditions were significant predictors of frequency. This finding that those with more health conditions use the portal more frequently than respondents without health conditions is consistent with other research that has found a relationship between having a chronic condition and increased frequency of patient portal use in the outpatient setting. 32 Having more health concerns may lead to more frequent patient portal use partly due to increased appointment load, managing more medications, and communicating with a greater number of providers.
Our results showing no use frequency differences by race contrast with literature about the digital divide, which has shown lower health information technology usage among non-Hispanic Blacks. 16 17 18 33 Our findings suggest that addressing initial barriers to access, such as physicians not offering patients access to their patient portal, 16 may be an important step to increasing patients' use of patient portals. There is evidence that there are disparities in who is offered portal access, with non-White respondents being less likely to report being offered access. 17 Our findings may indicate that though there may be initial barriers to being offered and accessing patient portals, once people use them, patient portals are used with similar frequency and considered similarly useful across sociodemographic groups. Nonetheless, it may be important for providers to help people in disadvantaged groups complete the initial steps needed to access patient portals.
We also found that individuals who used patient portals three or more times in the past 12 months had higher odds of using most of the patient portal functions compared with respondents who reported using their patient portal one to two times. These findings suggest that those who use their patient portal infrequently may only use patient portals to view test results or to monitor their health information, functions that require little patient-provider communication. On the one hand, infrequent users may not be aware of all of the functions their patient portal has to offer, 34 35 36 37 suggesting that opportunities may exist to support increased patient portal engagement among infrequent users. On the other hand, frequent patient portal users were perhaps more likely to use a greater number of patient portal functions partly because they became familiar with their patient portal, or because they had a higher level of technological or health literacy which allowed them to become proficient patient portal users. 38 39 40 41 Future studies could help ascertain whether technological literacy and patient portal use frequency are associated with increased patient engagement and perhaps better patient self-management.
Our results regarding the relationship between perceptions of usefulness of the patient portal and the functions used suggests that finding patient portals very useful contributes to use of more functions. However, as our model does not assess causality, it may be possible that those who use more functions then find patient portals more useful, or that those who find patient portals more useful are actually more comfortable using a variety of functions. There were three functions not associated with usefulness: making appointments, requesting corrections, and downloading health information. However, only communicating with health providers had higher odds among those who reported portals were only “somewhat useful.” This aligns with the diffusion of innovation theory, which predicts that ratings of usefulness are associated with having technology aligned with preferences for interacting with healthcare providers. 24 Those who rate usefulness higher may, in practice, be more likely to use the more communication-oriented and interactive features.
As health care systems continue to implement patient portals, our findings highlight the importance of needing to assess patients' perceptions about and interactions with their patient portals (i.e., context of use) to ensure use disparities do not widen. 42 Studying patient portal implementation may help to identify both patients' contextual needs and barriers that may hinder their use of patient portals as well as improving understanding of how to optimize patient portals, so they can be used by all patients, including those with poor technological or health literacy. 38 39 40 In this vein, future studies should consider examining the range of tasks patients engage in when using their patient portal to understand how patients use similar or different functions to manage their health, and how these functions affect the overall usability of patient portals. Given that previous research has found that nonuse of patient portal functions has been associated with lack of awareness of the functions, 34 36 increasing awareness of and training around the available functions might impact perceptions of patient portal usefulness. 43 44
Overall, our findings also emphasize the need to consider patients' context of use when examining the suitability of patient portals for different patient populations. 42 45 We found that the nature of the tasks patients perform when using a patient portal varies depending on how frequently they use their patient portals. Improving our understanding of patients' context of use with respect to various patient portal functions is important to ensure that such tools are both usable and perceived as useful for those patients, because patient portal use may improve patient outcomes including medication adherence, appointment attendance, and patient-provider communication. 12 46 47 48 Furthermore, identifying strategies to effectively facilitate patient portal use, including tailored patient portal education or trainings, 49 50 may be particularly important in efforts to reduce patient portal use disparities and increase the use of this important health information technology.
Limitations
Our study should be interpreted with several limitations in mind. First, HINTS data are based on self-report and subject to recall bias; respondents could have used more functions or used their patient portal more or less frequently than they reported. Second, HINTS data are cross-sectional, precluding any analysis of change over time, or inference about causation. Third, our analyses of perceived usefulness and frequency of use was limited to patient portal users, reducing our sample size. Additionally, sample size was limited for three functions (i.e., monitor health, make appointments, and view test results) because they these questions were asked in 2017 and not 2018. Some differences in use may be partially due to differences in the characteristics of who is offered use of a patient portal, and those offered use may not be demographically the same as the general population. Given our aim of assessing the characteristics of patients who reported using a patient portal, we believe that by using a national sample our findings are generalizable to the general population of patient portal users. Also, we acknowledge that when subsequent years of HINTS data become available, new trends may emerge, and existing trends may be strengthened by the addition of these data. Finally, our study did not examine the relationship between perceived usefulness or frequency of use with satisfaction with interactions in medical care. Understanding this impact of the technology is an important area for future research.
Conclusion
Across patients who used a patient portal at least once in the past year, those with Bachelor's degrees, incomes between $35,000 and $75,000, and those with multiple chronic conditions had higher odds of being frequent patient portal users. In addition, those with three or more chronic conditions had higher odds of perceiving the patient portal was useful, older adults, uninsured patients, and those who had last seen a doctor more than a year prior to the survey had lower odds of perceiving the patient portal was useful. As patient portal use may improve patient and care outcomes, it is important to continue to assess usefulness, frequency of use, and overall patient portal function use to identify opportunities to increase patient engagement with patient portals. Providing information and training about both patient portal use and the variety of functions available may also be important, particularly for patient groups for whom patient portal use and access have been low.
Clinical Relevance Statement
Encouraging the use of patient portal may improve patient's engagement with care, appointment attendance, communication with providers, and adherence. The frequency of use and perceptions of usefulness are associated with use of many functions, and training may be important to improve perceptions and comprehensiveness of patient portal use.
Multiple Choice Questions
-
Which group had higher odds of rating patient portals as “very useful”?
Those with incomes greater than $75,000
Those aged 75 or older
Those with three or more chronic conditions
Those who do not have health insurance
Correct Answer: The correct answer is option is c, those with 3 or more chronic conditions ( Table 3 ).
-
Which group had higher odds of using every patient portal function other than viewing test results?
Those who rated patient portals as “somewhat” useful
Those who rated patient portals as “very” useful
Those who used patient portals six to nine times per year
Those who used patient portals 10 or more times per year
Correct Answer: The correct answer is option d, those who used patient portals 10 or more times per year ( Table 2 ).
Table 3. Weighted odds of using patient portals, using them more times, and finding them useful, by demographic characteristic.
|
Frequency of use
a
(
n
= 1,684)
OR (95% CI) |
Usefulness
a
( n = 1,544) OR (95% CI) |
|
|---|---|---|
| Gender | ||
| Male | 1.0 | 1.0 |
| Female | 1.0 (0.8–1.4) | 1.0 (0.7–1.4) |
| Age | ||
| 18–34 | 1.0 | 1.0 |
| 35–49 | 0.8 (0.5–1.3) | 0.9 (0.6–1.5) |
| 50–64 | 0.7 (0.4–1.1) | 0.6 (0.3–0.9) |
| 65–74 | 0.7 (0.4–1.2) | 0.7 (0.4–1.4) |
| 75+ | 0.9 (0.5–1.6) | 0.4 (0.2–0.8) |
| Race/ethnicity | ||
| Non-Hispanic White | 1.0 | 1.0 |
| Non-Hispanic Black | 0.9 (0.6–1.5) | 1.6 (0.9–2.6) |
| Hispanic | 0.8 (0.5–1.2) | 1.5 (0.9–2.4) |
| Non-Hispanic Other | 1.0 (0.6–1.6) | 1.8 (1.0–3.2) |
| Education | ||
| High school or less | 1.0 | 1.0 |
| Some college | 1.4 (0.9–2.2) | 0.8 (0.5–1.4) |
| Bachelor's or more | 1.6 (1.1–2.6) | 0.8 (0.5–1.3) |
| Income | ||
| Less than $35,000 | 1.0 | 1.0 |
| $35,000–$75,000 | 1.6 (1.0–2.6) | 1.0 (0.6–1.9) |
| Greater than $75,000 | 1.3 (0.8–2.2) | 1.1 (0.6–2.0) |
| Metro status | ||
| Metro area | 1.0 | 1.0 |
| Nonmetro area | 0.7 (0.4–1.2) | 0.7 (0.5–1.0) |
| Insurance | ||
| Insured | 1.0 | 1.0 |
| Not insured | 0.4 (0.1–2.1) | 0.3 (0.1–0.9) |
| Number of chronic conditions | ||
| 0 | 1.0 | 1.0 |
| 1 | 1.3 (0.8–2.0) | 1.2 (0.7–1.8) |
| 2 | 1.8 (1.2–2.8) | 1.3 (0.8–2.0) |
| 3 or more | 2.6 (1.6–4.3) | 1.7 (1.1–2.7) |
| Last routine checkup | ||
| Within past year | 1.0 | 1.0 |
| > 1 year ago | 1.1 (0.7–1.7) | 0.7 (0.5–1.0) |
| Survey year | ||
| 2017 | 1.0 | 1.0 |
| 2018 | 1.2 (0.9–1.5) | 1.0 (0.7–1.3) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Modeled using ordinal logit (frequency categories = 1–2, 3–5, 6–9, 10 or more; usefulness categories = not at all/not very useful, somewhat useful, very useful).
Conflict of Interest None declared.
Protection of Human and Animal Subjects
This study uses publicly available deidentified data from a national survey. No human or animal subjects were included in this project.
References
- 1.Burde H. Health Law the hitech act-an overview. Virtual Mentor. 2011;13(03):172–175. doi: 10.1001/virtualmentor.2011.13.3.hlaw1-1103. [DOI] [PubMed] [Google Scholar]
- 2.Lye C T, Forman H P, Daniel J G, Krumholz H M. The 21st Century Cures Act and electronic health records one year later: will patients see the benefits? J Am Med Inform Assoc. 2018;25(09):1218–1220. doi: 10.1093/jamia/ocy065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burke R P, Rossi A F, Wilner B R, Hannan R L, Zabinsky J A, White J A. Transforming patient and family access to medical information: utilisation patterns of a patient-accessible electronic health record. Cardiol Young. 2010;20(05):477–484. doi: 10.1017/S1047951110000363. [DOI] [PubMed] [Google Scholar]
- 4.Huerta T, Fareed N, Hefner J L. Patient engagement as measured by inpatient portal use: methodology for log file analysis. J Med Internet Res. 2019;21(03):e10957. doi: 10.2196/10957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford E W, Hesse B W, Huerta T R. Personal health record use in the united states: Forecasting future adoption levels. J Med Internet Res. 2016;18(03):e73. doi: 10.2196/jmir.4973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones J B, Weiner J P, Shah N R, Stewart W F. The wired patient: patterns of electronic patient portal use among patients with cardiac disease or diabetes. J Med Internet Res. 2015;17(02):e42. doi: 10.2196/jmir.3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irizarry T, DeVito Dabbs A, Curran C R. Patient portals and patient engagement: A state of the science review. J Med Internet Res. 2015;17(06):e148. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Assadi V, Hassanein K. Consumer adoption of personal health record systems: a self-determination theory perspective. J Med Internet Res. 2017;19(07):e270. doi: 10.2196/jmir.7721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimada S L, Allison J J, Rosen A K, Feng H, Houston T K. Sustained use of patient portal features and improvements in diabetes physiological measures. J Med Internet Res. 2016;18(07):e179. doi: 10.2196/jmir.5663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mold F, Raleigh M, Alharbi N S, de Lusignan S. The impact of patient online access to computerized medical records and services on type 2 diabetes: systematic review. J Med Internet Res. 2018;20(07):e235. doi: 10.2196/jmir.7858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tulu B, Trudel J, Strong D M, Johnson S A, Sundaresan D, Garber L. Patient portals: an underused resource for improving patient engagement. Chest. 2016;149(01):272–277. doi: 10.1378/chest.14-2559. [DOI] [PubMed] [Google Scholar]
- 12.Kelly M M, Hoonakker P L, Dean S M. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2017;24(01):153–161. doi: 10.1093/jamia/ocw070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otte-Trojel T, Rundall T G, de Bont A, van de Klundert J, Reed M E. The organizational dynamics enabling patient portal impacts upon organizational performance and patient health: a qualitative study of Kaiser Permanente. BMC Health Serv Res. 2015;15:559. doi: 10.1186/s12913-015-1208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.United States Government Accountability Office Health information technology: Hhs should assess the effectiveness of its efforts to enhance patient access to and use of electronic health information GAO-17–305 https://www.gao.gov/products/gao-17-305Accessed March 15, 2017
- 15.Fraccaro P, Vigo M, Balatsoukas P, Buchan I E, Peek N, van der Veer S N. Patient portal adoption rates: a systematic literature review and meta-analysis. Stud Health Technol Inform. 2017;245:79–83. [PubMed] [Google Scholar]
- 16.El-Toukhy S, Méndez A, Collins S, Pérez-Stable E J. Barriers to patient portal access and use: evidence from the health information national trends survey. J Am Board Fam Med. 2020;33(06):953–968. doi: 10.3122/jabfm.2020.06.190402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anthony D L, Campos-Castillo C, Lim P S. Who isn't using patient portals and why? Evidence and implications from a national sample of us adults. Health Aff (Millwood) 2018;37(12):1948–1954. doi: 10.1377/hlthaff.2018.05117. [DOI] [PubMed] [Google Scholar]
- 18.Walker D M, Hefner J L, Fareed N, Huerta T R, McAlearney A S. Exploring the digital divide: age and race disparities in use of an inpatient portal. Telemed J E Health. 2020;26(05):603–613. doi: 10.1089/tmj.2019.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai R, Bell E J, III, Woo H, Baldwin K, Pfeffer M A. How patients use a patient portal: an institutional case study of demographics and usage patterns. Appl Clin Inform. 2019;10(01):96–102. doi: 10.1055/s-0038-1677528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bush R A, Vemulakonda V M, Richardson A C, Deakyne Davies S J, Chiang G J. Providing access: differences in pediatric portal activation begin at patient check-in. Appl Clin Inform. 2019;10(04):670–678. doi: 10.1055/s-0039-1695792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tieu L, Sarkar U, Schillinger D. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res. 2015;17(12):e275. doi: 10.2196/jmir.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin S C, Lyles C R, Sarkar U, Adler-Milstein J. Are patients electronically accessing their medical records? Evidence from national hospital data. Health Aff (Millwood) 2019;38(11):1850–1857. doi: 10.1377/hlthaff.2018.05437. [DOI] [PubMed] [Google Scholar]
- 23.Maguire M. Context of use within usability activities. Int J Hum Comput Stud. 2001;55(04):453–483. [Google Scholar]
- 24.Rogers E M. 5th edition. New York: Free Press; 2003. Diffusion of Innovations. [Google Scholar]
- 25.Emani S, Peters E, Desai S. Who adopts a patient portal?: an application of the diffusion of innovation model. J Innov Health Inform. 2018;25(03):149–157. doi: 10.14236/jhi.v25i3.991. [DOI] [PubMed] [Google Scholar]
- 26.Lin C T, Wittevrongel L, Moore L, Beaty B L, Ross S E. An Internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res. 2005;7(04):e47. doi: 10.2196/jmir.7.4.e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Cancer Institute Hints survey instrumentsAccessed February 27, 2020 at:http://hints.cancer.gov/instrument.aspx
- 28.National Cancer Institute Frequently asked questions about hintsAccessed February 12, 2020 at:http://hints.cancer.gov/faq.aspx
- 29.Davis W, Moser R P.Discussion of statistical weights and their use 2004. Accessed 2004 at:https://hints.cancer.gov/docs/Using-Survey-Weights12-13-05.pdf
- 30.Moser R P, Naveed S, Cantor D.Integrative analytic methods using population-level cross-sectional dataIn:National Cancer Institute; 2013 [Google Scholar]
- 31.Goel M S, Brown T L, Williams A, Hasnain-Wynia R, Thompson J A, Baker D W. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med. 2011;26(10):1112–1116. doi: 10.1007/s11606-011-1728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wallace L S, Angier H, Huguet N. Patterns of electronic portal use among vulnerable patients in a nationwide practice-based research network: From the ochin practice-based research network (pbrn) J Am Board Fam Med. 2016;29(05):592–603. doi: 10.3122/jabfm.2016.05.160046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elston Lafata J, Miller C A, Shires D A, Dyer K, Ratliff S M, Schreiber M. Patients' adoption of and feature access within electronic patient portals. Am J Manag Care. 2018;24(11):e352–e357. [PMC free article] [PubMed] [Google Scholar]
- 34.Turvey C, Klein D, Fix G. Blue Button use by patients to access and share health record information using the Department of Veterans Affairs' online patient portal. J Am Med Inform Assoc. 2014;21(04):657–663. doi: 10.1136/amiajnl-2014-002723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turner A M, Osterhage K, Hartzler A. Use of patient portals for personal health information management: the older adult perspective. AMIA Annu Symp Proc. 2015;2015:1234–1241. [PMC free article] [PubMed] [Google Scholar]
- 36.Powell K, Myers C.Electronic patient portals: Patient and provider perceptionsOnline J Nurs Inform 2018;22(01):
- 37.Irizarry T, Shoemake J, Nilsen M L, Czaja S, Beach S, DeVito Dabbs A. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res. 2017;19(03):e99. doi: 10.2196/jmir.7099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woods S S, Forsberg C W, Schwartz E C. The association of patient factors, digital access, and online behavior on sustained patient portal use: a prospective cohort of enrolled users. J Med Internet Res. 2017;19(10):e345. doi: 10.2196/jmir.7895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoogenbosch B, Postma J, de Man-van Ginkel J M, Tiemessen N A, van Delden J J, van Os-Medendorp H. Use and the users of a patient portal: cross-sectional study. J Med Internet Res. 2018;20(09):e262. doi: 10.2196/jmir.9418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mackert M, Mabry-Flynn A, Champlin S, Donovan E E, Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18(10):e264. doi: 10.2196/jmir.6349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sulieman L, Steitz B, Rosenbloom S T. Analysis of employee patient portal use and electronic health record access at an academic medical center. Appl Clin Inform. 2020;11(03):433–441. doi: 10.1055/s-0040-1713412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Antonio M G, Petrovskaya O, Lau F.Is research on patient portals attuned to health equity? A scoping review J Am Med Inform Assoc 201926(8-9):871–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kornacker D, Fitzgerald K, Elder S. A patient portal push toward acceptance and utilization of the technology. Patient Exp J. 2019;6(02):20–27. [Google Scholar]
- 44.McAlearney A S, Gaughan A, MacEwan S R, Fareed N, Huerta T R. Improving acceptance of inpatient portals: patients' and care team members' perspectives. Telemed J E Health. 2020;26(03):310–326. doi: 10.1089/tmj.2019.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Czaja S J, Zarcadoolas C, Vaughon W L, Lee C C, Rockoff M L, Levy J. The usability of electronic personal health record systems for an underserved adult population. Hum Factors. 2015;57(03):491–506. doi: 10.1177/0018720814549238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarkar U, Lyles C R, Parker M M. Use of the refill function through an online patient portal is associated with improved adherence to statins in an integrated health system. Med Care. 2014;52(03):194–201. doi: 10.1097/MLR.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Graham T AD, Ali S, Avdagovska M, Ballermann M. Effects of a web-based patient portal on patient satisfaction and missed appointment rates: Survey study. J Med Internet Res. 2020;22(05):e17955. doi: 10.2196/17955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dendere R, Slade C, Burton-Jones A, Sullivan C, Staib A, Janda M. Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res. 2019;21(04):e12779. doi: 10.2196/12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Casey I. The effect of education on portal personal health record use. Online J Nurs Inform. 2016;20(02):9. [Google Scholar]
- 50.Lyles C R, Tieu L, Sarkar U. A randomized trial to train vulnerable primary care patients to use a patient portal. J Am Board Fam Med. 2019;32(02):248–258. doi: 10.3122/jabfm.2019.02.180263. [DOI] [PMC free article] [PubMed] [Google Scholar]


