Abstract
Context:
Non-urgent emergency department (ED) use contributes to healthcare costs and disrupts continuity of care. Factors influencing patient/guardian decision-making in non-urgent situations are poorly understood.
Objective:
Determine the association of patient/guardian – primary care provider (PCP) relationship with non-urgent ED usage and explore related factors.
Methods:
In an urban practice, we recruited 218 parent-child pairs and administered a survey with the PCP relationship (PDRQ-9), caregiver knowledge of office resources, and care-seeking behavior. We performed a 12-month retrospective chart review to document non-urgent ED visits. We evaluated the association of PDRQ9 and non-urgent ED usage by regression analysis.
Results:
Mean child age was 7.0 ± 5 years, and 32.6% of children had at least one non-urgent ED visit. Mean PDRQ9 score was 39.8 ± 7.3 and was not associated with non-urgent ED use (p=0.46). Lower child age (p<0.001) and shorter time coming to the PCP practice (p<0.001) were both associated with increased non-urgent ED use. Only 36.4% reported usually going to their PCP when they are sick. Knowledge of office resources was limited, and when prompted with acute, non-urgent medical scenarios, in 4 of 5 scenarios, 50% or more of participants chose to go to the ED over communicating with or going to their PCP.
Conclusion(s):
We did not find an association between patient-doctor relationship strength and non-urgent ED usage. Many patients/guardians were unaware of the practice’s resources and selected the ED as first choice for acute, non-urgent medical scenarios. Additional work is needed to determine interventions to reduce non-urgent ED use.
Keywords: Primary care, Non-urgent, Relationship, Emergency Department, Acute visits
Introduction
Emergency department (ED) overutilization is a well-documented concern in the healthcare system, contributing to over-crowding, increased costs, and fragmented patient care.1–5 Reducing non-urgent ED use may help ease this burden. While the factors driving non-urgent ED use have been studied in the ED setting, results are varied and do not show consensus. Moreover, data on pediatric ED use and caregiver decision-making is scarce.
Commonly held beliefs about factors related to non-urgent ED use, such as lack of insurance coverage, poor access to primary care, or physical distance to care sites, have not been consistently verified.1–4 In one study, almost all (95%) of pediatric patients visiting an urban pediatric hospital had health insurance, and most (94%) had a primary care provider (PCP).2 Several studies have pointed to factors driving decision-making that involve the relationship between the patient and their PCP.5–8 Investigators have reviewed caregiver opinions about primary care and emergency settings, opportunities for education and expectations in communication, and overall continuity of care, all with the goal of better understanding how to appropriately guide health care usage.2,3,9–16 Family centeredness and access to health care resources have been shown to be related to reductions non-urgent visits to different degrees.2,13,14 These different aspects together may be unified under the umbrella of the patient-doctor relationship/medical home. The strength of this relationship may improve continuity of care and health literacy as caregivers seek medical care for their children.
Most previous studies in this field have focused on the population of patients in the ED. Understanding which caregivers initially seek help from their child’s PCP rather than the ED may provide a model of behavior that reduces ED over-crowding and increases continuity of care. Therefore, we focused on the population of patients connected to care with a PCP. Measuring the relationship between a patient, or caregiver, and their PCP can be complicated, but validated tools have been developed. The Patient-Doctor Relationship Questionnaire (PDRQ-9), is a tool that was developed to evaluate patient-provider relationship.17 The PDRQ-9 was initially validated as a self-administered survey among participants at three primary care centers and a specialized neurology epilepsy clinic.17 In a comparison of 18 other measures of doctor-patient relationships, the PDRQ-9 was described as “excellent” overall for its internal consistency and brevity, especially for practical applications in the primary care setting.17,18 Therefore, the primary aim of our study was to evaluate whether the strength of this patient-doctor relationship was associated with non-urgent ED use. Additionally, we aimed to identify other patterns of medical decision-making through self-reported preferences and patient characteristics.
Methods
Primary Care Engagement and Acute Care Election (PEACE) was a cohort study with a retrospective chart review consisting of 218 parent-child pairs (436 individuals. English-speaking families receiving care at this urban, hospital-based practice during the summer of 2018 were eligible for inclusion. Non-English-speaking patients were excluded because the PDRQ-9 has not been validated in non-English languages and our practice serves very few non-English speaking families. Of note, no families ultimately were excluded for language. We also excluded children under the age of 12 months to permit a 12-month retrospective chart review on all participants without censoring of data. The IRB reviewed and approved this protocol. We obtained written informed consent and HIPAA release from all parents and guardians, or patients who were 18 years or older, as well as assent when appropriate. Data collection occurred in two parts – first we conducted an in-person PEACE survey (available by request from the author), then we conducted the 12-month retrospective chart review (available by request from the author).
PEACE Survey
Parents or guardians, or patients 18 years or older, completed the PEACE survey in the waiting room prior to being seen. This was a convenience sampled based the individuals who presented to the primary care practice during the study period and gave written, informed consent. The survey was self-completed by the caregiver and returned to study team member to ensure the survey was answered completely and was kept secure and confidential. The study team member was not related to the patient’s clinical care process and identified herself as such prior to obtaining consent. The PEACE survey included questions to assess demographics, typical health behaviors, knowledge of PCP practice resources, illness situational responses, and patient-doctor relationship via the PDRQ-9 (Appendix A). Some examples of questions include preferred location to receive acute care, home proximity to different acute care centers, and knowledge of available walk-in visits and overnight phone service. The illness situational response scenarios focused on three common acute complaints in the pediatric population: ear pain, fever of 103 F, and difficulty breathing and coughing – during daytime and nighttime. Caregivers were asked to select their preferred next step in seeking medical care: contacting or going to their child’s doctor’s office, going to an urgent care center or emergency room, or waiting until morning if appropriate.
The PDRQ-9 formatting was kept consistent with its previous validation studies, including wording of the Likert scale and use of the acronym “PCP.” Clarification of this term was provided at the beginning of the survey and immediately prior to the PDRQ-9. Participants were asked to circle a number 1 to 5 to represent which best represents their child’s regular doctor (PCP) – 1 indicating “not at all appropriate” and 5 indicating “totally appropriate.” Statements include: (1) My PCP helps me (2) My PCP has enough time for me (3) I trust my PCP (4) My PCP understands me (5) My PCP is dedicated to help me (6) My PCP and I agree on the nature of my medical symptoms (7) I can talk to my PCP (8) I feel content with my PCP’s treatment (9) I find my PCP easily accessible.17 The PDRQ-9 was scored by totaling the results of the 9 questions scored on a 5 point Likert scale - a final score of 9 indicates the weakest relationship and 45 indicates the strongest.17
Chart Review
A retrospective chart review was conducted over the 12 months prior to the survey date to evaluate typical behaviors across a year. Our institution utilizes an Electronic Medical Record (EMR) system that is congruent with other institutions in the area and includes features of data sharing across institutions; therefore, our review included data from ED visits from most major institutions in our catchment area. Data abstraction was performed to collect other potential confounding factors, such as the child’s age, insurance type, and presence of chronic disease. We also recorded other indicators of patient use of PCP resources, including number of well and sick visits in 12 months, missed appointment percentage, and the last time the patient saw their PCP. This data was extracted by one study team member (S.K., a medical student). The chart review was performed after survey data collection by a blinded study team. The whole study team reviewed the EMR together on an initial sample to develop the extraction plan and any participant with discordant EMR data was reviewed as a team. After chart extraction, A.S. audited 5% of the chart extractions and concurred with >95% of the findings.
The primary outcome of non-urgent ED visit was collected during our chart review. We assessed the outcome using the Emergency Severity Index (ESI) Triage algorithm. The ESI Version 4 is a reliable and consistent tool for assessment of urgency of visits used by U.S. centered studies and is widely utilized in existing literature.2,3,10,15,16,19–22 To use the ESI, patients are assigned a numerical score from 1–5 upon arrival to an acute care center, with 1 representing the most severe medical situation and 5 the least severe.23 Examples of triage scores of 4 or 5 include superficial lacerations, medication refills, or poison ivy on extremities, which can be evaluated at most primary care practices.23 Triage scores assigned at patient presentation were not available for all EMR-recorded ED visits. To maintain consistency in assessment of non-urgency, each visit was assigned a retrospective triage score using the official ESI handbook with information such as presenting vital signs, resources utilized in the ED, and clinical severity by a single study member at the time of chart review.23 We reviewed 10% of these retrospective classifications against those ED visits that did have an assigned triage score, and the concordance rate was >90%. The study member was a medical student who was blinded to the PDRQ-9 and other survey results. Any participant with an ESI that was not straightforward was discussed as a study team (blinded to survey data). Those visits that were assigned a score of 4 or 5, and did not have a referral from a physician to go to the ED, were coded as a non-urgent ED visit.
Data Management
We collected and managed study data using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at University of Maryland.24,25
Data Analysis
We conducted a univariate analysis of our primary independent/exposure and dependent/outcome variables. The primary independent/exposure variable was the score of the PDRQ-9 and the primary dependent/outcome variable was the number of non-urgent ED visits within the past 12 months. Other potential predictors in our study included responses to individual questions in the PEACE survey (knowledge of practice resources and self-reported situational responses), individual components of the PDRQ-9, child age, chronic conditions, and insurance status, length of time with the primary care practice, length of time since last visit at the practice, number of phone calls, and number of well visits.
We performed bivariate analysis using Kruskal-Wallis testing for an ordinal variables and categorical variables with 3 or more groups, and Mann Whitney U testing for an ordinal or categorical variable with 2 groups. We utilized Spearman’s rank-order analysis for correlation of non-urgent ED visits with our continuous independent variables.
In conducting bivariate analyses of associations of our PDRQ-9 and other potential predictors with the primary outcome, we utilized a Poisson regression because the number of non-urgent ED visits is a count variable. In sensitivity analyses we repeated the testing with logistic regression (ANY non-urgent ED visit) to confirm results of the Poisson regression. We also repeated the analysis excluding individuals with missing data for any PDRQ-9 questions (n=10). We performed adjusted analysis controlling variables with p < 0.2 in bivariate analyses. Additionally, in secondary analyses we stratified for type of visit on date of survey to determine if there was a difference in associations based on the patients visit type (acute, well, or follow up). All statistical testing was two-sided with a significance level of p < 0.05. This analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Demographics
The mean age of the pediatric patients in this study was 7.0 years, with a range of 1 to 21 years. Most patients were covered by public insurance (86.6%) and had at least one chronic medical condition (78.5%) (Table 1). When asked where they usually choose to seek care when their child is sick, 36.7% of caregivers reported that they prefer their doctor’s office whereas 29.4% preferred the ED (Table 1).
Table 1:
Overall Sample Characteristics (N=220)
| Characteristic | Mean ± SD (range) | N |
|---|---|---|
| Age (years) | 7.0 ± 5.0 (1–21) | 218 |
| Years at the practice | 5.7 ± 4.5 (0–18) | 209 |
| Frequency (%) | ||
| Insurance Type | 216 | |
| Public | 86.6 | |
| Private | 11.6 | |
| None | 1.8 | |
| Chronic Medical Condition | 214 | |
| Yes | 78.5 | |
| No | 21.5 | |
| Visit Type on Survey Day | 209 | |
| Well Visit | 58.9 | |
| Sick/follow up | 41.1 | |
| Does child have regular PCP | 217 | |
| Yes | 86.2 | |
| No | 13.8 | |
| Is home closer to ED or PC | 220 | |
| ED | 66.4 | |
| PCP | 16.4 | |
| No difference | 17.2 | |
| Usual choice for sick child care | 218 | |
| PCP | 36.7 | |
| Urgent Care | 12.8 | |
| ED | 29.4 | |
| Other (all of above & combinations) | 21.1 | |
Knowledge of PCP Practice Resources
Between 19.6% and 57.0% of participants were unable to accurately identify each of the resources offered by the PCP practice (Figure 1). The only service the PCP practice does not have is nighttime hours.
Figure 1:
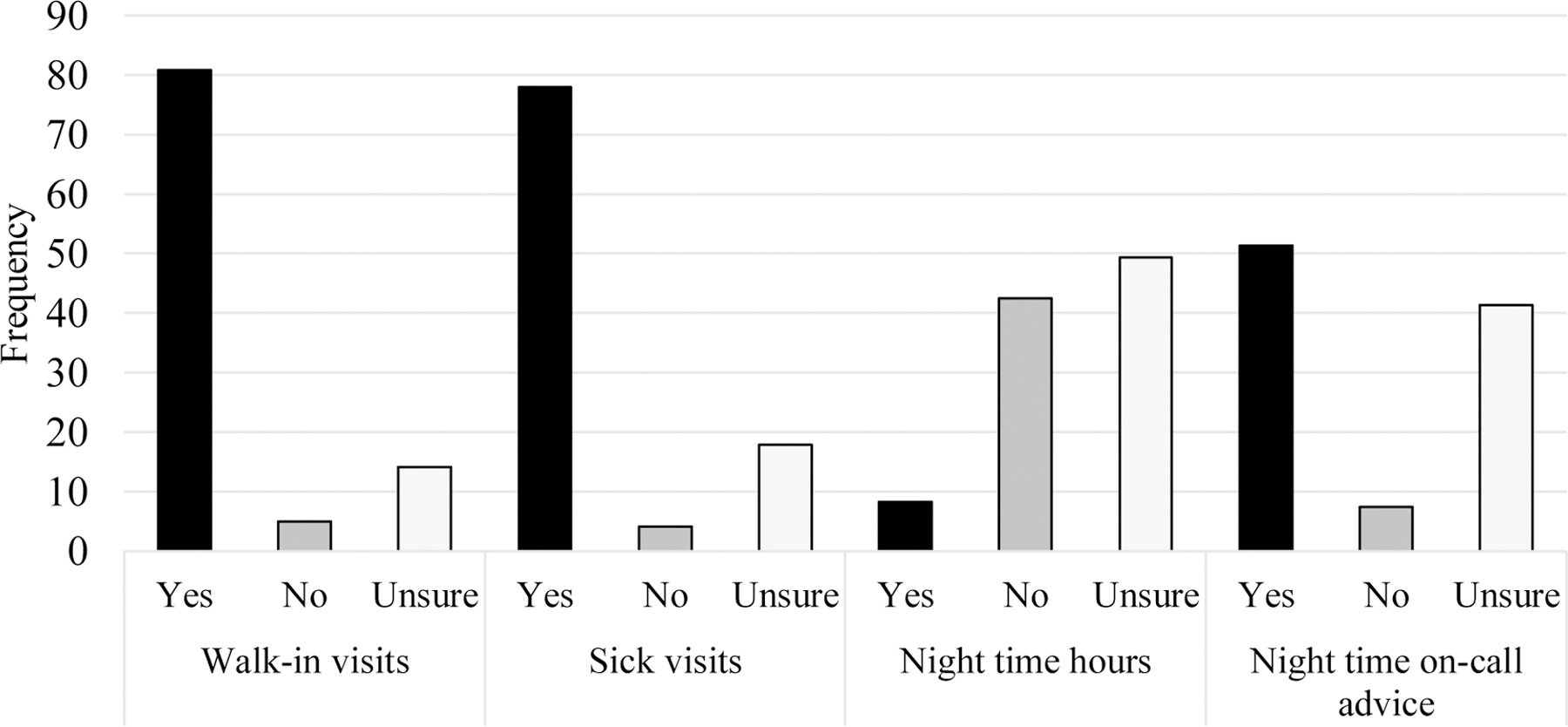
Knowledge of PCP Practice Resources.
The frequency of participants who answered the presence or absence of practice resources by resource line is presented. Walk-in visits, sick visits, and night call services are offered at this practice, night visits are not.
Situational Responses and Illness Scenarios
The survey assessed caregiver response to common pediatric acute care situations during the day and night. All of these situations should be addressed by a visit or call to the PCP. In four of the five scenarios presented, caregivers chose to visit the Emergency Room more frequently than their PCP office (Figure 2).
Figure 2:
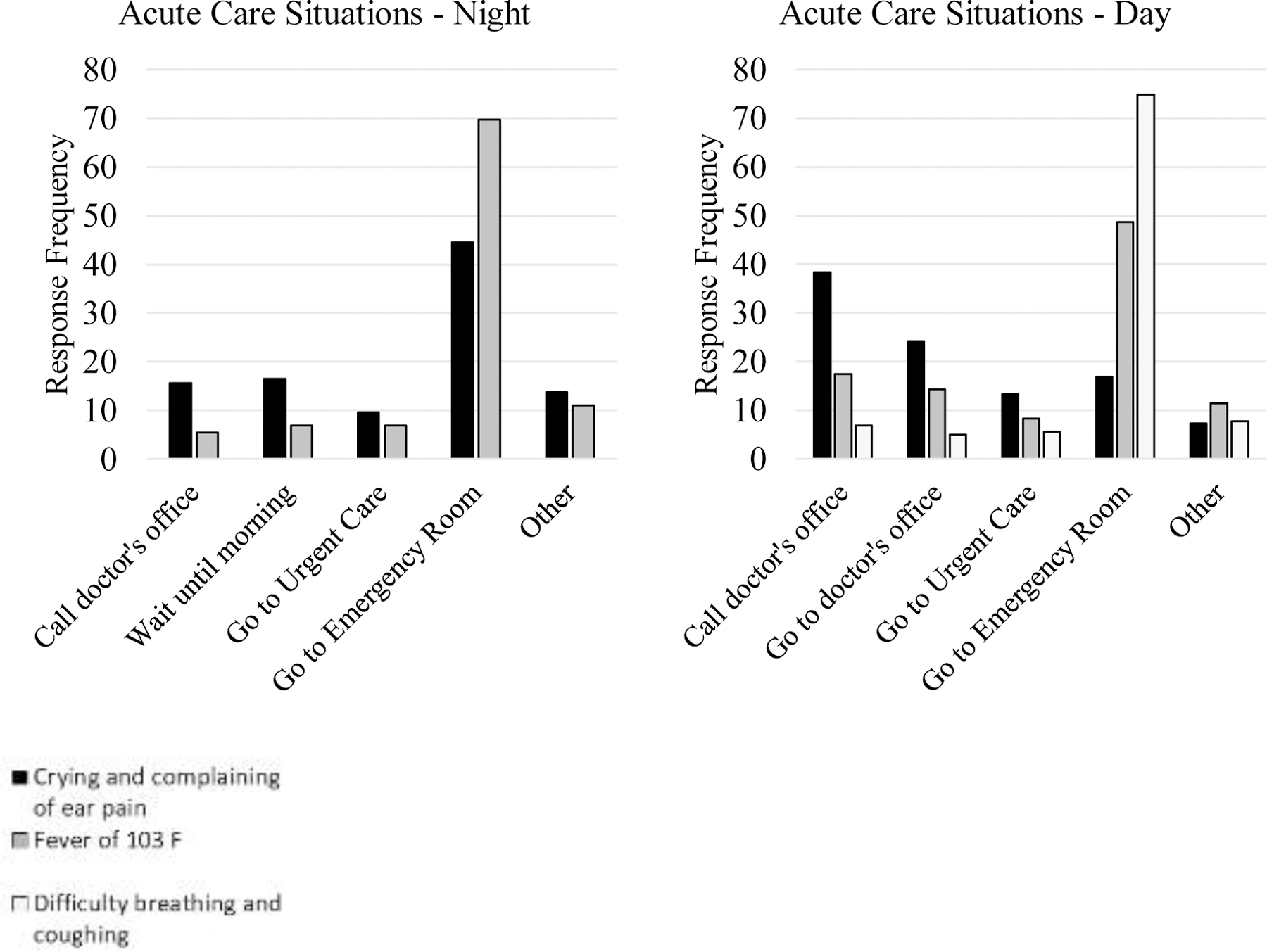
Self-Reported Situational Behaviors.
The frequency of participant response to each situation during the night and day are presented for the three illness scenarios. The preferred response to each situation would be to call or visit the doctor’s office. We did not ask about difficulty breathing or coughing at night.
PDRQ-9 and Outcome Data
The average PDRQ-9 score was 39.8 ± 7.3 points. The average score of individual items ranged from 4.2 to 4.5 (Table 2). Higher PDRQ-9 scores suggest higher patient-PCP connectedness.
Table 2:
PDRQ-9: Mean Response Score for Each Item on the PDRQ-9 and Correlations with Number of Non-urgent ED visits.
| Question | Mean (SD) | Correlation | p-value |
|---|---|---|---|
| My PCP helps me | 4.455 (0.924) | 0.0029 | 0.97 |
| My PCP has enough time for me | 4.329 (0.998) | 0.051 | 0.46 |
| I trust my PCP | 4.519 (0.823) | 0.082 | 0.24 |
| My PCP understands me | 4.460 (0.849) | 0.089 | 0.20 |
| My PCP is dedicated to help me | 4.429 (0.959) | 0.069 | 0.32 |
| My PCP & I agree on the nature of my medical symptoms | 4.451 (0.849) | 0.041 | 0.55 |
| I can talk to my PCP | 4.491 (0.868) | −0.038 | 0.58 |
| I feel content with my PCP’s treatment | 4.526 (0.833) | −0.0043 | 0.95 |
| I find my PCP easily accessible | 4.216 (1.116) | 0.057 | 0.41 |
| PDRQ-9 Overall Score | 39.812 (7.305) | 0.051 | 0.46 |
The number of non-urgent ED visits in a 12-month period was the primary outcome of this study, with a mean value of 0.6 ± 0.9. 32.6% of participants had one or more non-urgent visits. In this population, 68.4% of participants had no non-urgent visits during the study period, 19.3% had 1 non-urgent visit, 7.8% had 2, 3.2% had 3, and 2.3% had four. Only 5 ED visits by 4 participants were preceded by a phone call to the PCP office, the remainder were “self-referred.” 27.4% of non-urgent visits occurred during regular work hours, and 72.6% occurred outside of work hours.
Bivariate (Unadjusted) Associations
There was no statistical significance between the reported PDRQ-9 score and the number of non-urgent ED visits in the past year (p=0.46, Table 2). When stratified by number of non-urgent ED visits, the mean PDRQ-9 score ranged from 38.0 – 44.2. This result was consistent on logistic regression analysis and on analysis excluding the individuals with missing data for the PDRQ-9. There were also no significant associations between any of the individual questions within the PDRQ-9 and non-urgent ED visits (Table 2).
Lower child age (p < 0.001), decreased length of time attending the primary care practice (p<0.001), higher number of well visits in 12 months (p = 0.002), higher number of phone calls to the practice (p = 0.002), and fewer weeks from last primary care visit (p < 0.001) were associated with increased non-urgent ED visits in 12 months. There was no significant relationship found between knowledge of practice resources and number of non-urgent ED visits in 12 months. Additionally, presence of other medical conditions and insurance type were not associated with the number of non-urgent ED visit. However, there was a trend toward significance for insurance type: 16.0% of private insurance patients had a non-urgent ED visit vs. 36.2% for public insurance (p=0.07).
Secondary analyses
In order to determine whether people who appropriately used the PCP office were less likely to use the ED non-urgently, we stratified by type of visit on date of survey. Presumably, if the date-of-survey visit was an acute visit, it might pre-select those who are appropriately using their PCP office, but there was no significant relationship with the total PDRQ-9 scores (p = 0.90) or the number of non-urgent visits (p = 0.28, Table 3). Stratification by age showed the highest frequency of non-urgent visits in the 1–3 year old age group (32%), and generally younger children had a higher rate of non-urgent ED visits (p< 0.001).
Table 3:
Non-urgent ED Visits and PDRQ-9 Scores Stratified by Visit Type on Date of Survey
| Non-Urgent ED Visits | PDRQ-9 Score | |||
|---|---|---|---|---|
| Frequency of Visit Type (n=216) | Mean ± SD (Range) | Frequency of Visit Type (n=213) | Mean ± SD (Range) | |
| Sick Visit | 31% | 0.53 ± 0.90 (0 – 4) | 31% | 39.7 ± 7.96 (10 – 45) |
| Other | 4% | 0.56 ± 0.73 (0 – 2) | 4% | 41.8 ± 5.45 (28 – 45) |
| Well Visit | 57% | 0.57 ± 0.98 (0 – 4) | 56% | 40.0 ± 7.12 (9 – 45) |
| Follow-up | 5% | 1.10 ± 1.10 (0 – 3) | 5% | 38.5 ± 6.33 (27 – 45) |
PDRQ-9 scores are based on a 9-item survey, each graded on a 5-point Likert scale. The maximum score is a 45, indicating the strongest evaluation of relationship with a physician. The type of visit on the date of survey was not significantly associated with either non-urgent ED visits (p = 0.28) or PDRQ-9 score (p = 0.90).
Discussion
We did not find a significant relationship of patient PCP relationship (as measured by the PDRQ-9) with the number of non-urgent pediatric ED visits in the previous 12 months. A surprisingly low percent of caregivers were aware of clinic resources despite posted signage in the waiting room and patient rooms, annual mailers, new patient magnets, and other advertising (19.6% – 57.1% of were unsure of each the resources listed), and even fewer would elect to use those resources when presented with them in hypothetical care situations. Even when given the option of first calling or visiting their PCP, most participants selected to go to an ED for four common pediatric non-urgent health complaints. These results demonstrated a low level of knowledge of PCP resources, care-seeking choices that fragment patient care, and a general preference to choose the ED in non-urgent situations.
While there was a full range of PDRQ-9 scores, caregivers seeking care at this primary care practice tended to evaluate their relationship as strong with an average PDRQ-9 score of 39.8/45. While we did not observe a relationship between the PDRQ-9 and non-urgent ED usage, other factors including age, were more strongly related to non-urgent ED use in our population. Even when stratified by visit type on date of survey and patient age, there was no relationship of PDRQ-9 with non-urgent ED use. This reflects that there are likely other drivers in the PCP setting which determine acute care choice.
We did find a significant relationship between age-related factors and resource utilization with non-urgent ED visits. We observed a higher rate of non-urgent ED usage in those patients who have had fewer years attending the primary care practice, decreased time between primary care visits, and with a younger child age. Many of these variables reflect younger age, but could also serve as a proxy for connectedness with the practice. We observed children with higher non-urgent ED utilization to have increased number of calls to the primary care practice and to prefer the ED when their child is sick. These may be proxy for a more “anxious” parent. Other works reports that within the pediatric population, 12% of children under 1 year old had at least one non-urgent ED visit and are considered to be some of the highest utilizers with 987 visits per 1,000 persons – more than double the average overall rate of 458 visits per 1,000 persons.26,27 Previous studies have confirmed a similarly young population, with a greater probability of avoidable hospitalization with younger age and a negative correlation found between age and number of preventive care visits.28 Studying this younger pediatric population within the context of their higher utilization of healthcare resources may be an important next step in addressing inappropriate over-utilization of high cost interventions, such as ED visits for non-urgent acute care.
Despite previously documented connections between ED usage and continuity of care, the patient relationship as represented by the PDRQ-9 was not significantly related to that decision-making process.1,6,8 Continuity of care may be more related to connection to or education about health care resources. While opening more financial access to a PCP increases the number of preventive visits in pediatric populations, it is thought to have no change, or possibly increase ED usage overall.28 This may demonstrate the complexity of the decision-making process connected to overarching increased utilization within subsets of the pediatric population, such as infants.
Health literacy itself may not have the same connection with the relationship between PCP and caregiver that we had anticipated. Education surrounding health management has been shown to impact non-urgent ED visits in the long-term, but levels of health literacy have also been shown to impact how highly caregivers value and trust their PCP.10,21 In the ED, as many as one to two thirds of caregivers overestimate the urgency of their child’s ED visit, and research is still needed to develop how relationships within the healthcare system can provide appropriate education.6,8,11 This also highlights the importance of conversations about expectations, as some studies have shown that while PCPs expect for caregivers to call before going to the ED, only 29.4% of caregivers share that same expectation.3,11 Further studies that parse out the distinctions between PCP contact, provision of adequate resources with caregiver awareness, and the relationship between the two may help identify areas for intervention.
The ED is not the only setting in which caregivers seek acute, non-urgent care. Urgent care centers also provide a possible point of care for children. While our EMR incorporates ED visits throughout the state, it does not reliably do so for urgent care visits, and as such, we could not include them in our analysis. A recent study focused on a large population of pediatric patients reported that increasing urgent care use was associated with lower primary care and specialist use in the pediatric population.29 The study also reported increasing urgent care use did not increase ED use, and those children found to have high reliance on urgent care tended to have lower proportional ED use than their low reliance counterparts.29 That study therefore suggests that while urgent care use might interrupt the doctor-patient primary care relationship, it decreases ED use.
There are some limitations to this project. A first limitation is the age restrictions. T account for seasonal variation in childhood illnesses, we chose to study 12 months of ED visits. This led to a decision to exclude children younger than 12 months so that there would be no censored data. Thus, we cannot conclude anything about PCP connectedness and non-urgent ED use among children under one year. A second potential limitation is the outcome variable definition. Defining urgent ED visits is not standardized across studies, but we used an ESI based definition that is consistent with other studies.2,3,10,15,16,19–22 We chose to use the requirement of PCP referral OR ESI score <4 as a definition, which may even be a little conservative. This PCP referral was defined as a recorded phone call prior to ED presentation recommending ED-level care. While all participants receive primary care at the same institution where phone calls would be recorded, it is possible that other contact with outside medical professionals (like insurance company advice lines) over the phone was not recorded. A third limitation is the challenge of defining primary care provider connectedness. While we used a validated and standardized tool, the PDRQ-9, we had the limitation of heavily skewed data – most families reported positive relationships. Caregivers were reminded of the confidentiality of survey responses, but this may not have completely eliminated any social pressure to report a positive relationship. Fourth, there may be unmeasured factors related to non-urgent ED use such as parental age, presence of older siblings, and parent educational attainment. Future studies will need to address these factors. Lastly, the sample reflects children already engaged with a PCP and does not reflect children who may not attend any pediatric practice.
While PCP connectedness was not associated with non-urgent ED use in this study, we have identified areas for future research. In addition to exploring factors and interventions specific to this younger subset of the pediatric population, future studies may discern the utility of separate analyses of primary care-based and ED-based populations. Additionally, the influence of parental age, education, or older siblings may also serve as indicators of familiarity with the healthcare system and should be explored in relation to health literacy. Overall, the study has provided insight on another factor in the complex decision-making process that influences where caregivers elect to take their children for non-urgent acute medical events. While we did not find a significant relationship between the PDRQ-9, a proven instrument in the measurement of patient-doctor relationships, we were able to identify characteristics of high-resource utilizing populations that may be targeted in further interventions to decrease nonurgent ED utilization.
What’s New:
Caregiver decision-making in non-urgent medical situations is poorly understood. We did not find an association of patient-doctor relationship strength with non-urgent emergency department usage, but we documented poor knowledge and use of practice resources and association with younger patient age.
Acknowledgements
We acknowledge the support of the University of Maryland, Baltimore, Institute for Clinical & Translational Research (ICTR) and the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) grant number 1UL1TR003098. This research was also supported in part by the Proposed Research Initiated by Students and Mentors (PRISM) Program, University of Maryland School of Medicine Office of Student Research.
Financial Disclosures:
Financial support was provided by the University of Maryland, Baltimore, Institute for Clinical & Translational Research (ICTR) and the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) grant number 1UL1TR003098 and the Proposed Research Initiated by Students and Mentors (PRISM) Program, University of Maryland School of Medicine, Office of Student Research. This support had no role in study design, collection, analysis, or interpretation of data, writing of the report, or decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
References:
- 1.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: Systematic literature review. Am J Manag Care 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 2.Sturm JJ, Hirsh DA, Lee EK, Massey R, Weselman B, Simon HK. Practice Characteristics That Influence Nonurgent Pediatric Emergency Department Utilization. Acad Pediatr 2010;10(1):70–74. doi: 10.1016/j.acap.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 3.Long CM, Mehrhoff C, Abdel-Latief E, Rech M, Laubham M. Factors Influencing Pediatric Emergency Department Visits for Low-Acuity Conditions. Pediatr Emerg Care July 2018:1. doi: 10.1097/pec.0000000000001553 [DOI] [PubMed] [Google Scholar]
- 4.Luo X, Liu G, Frush K, Hey LA. Children’s health insurance status and emergency department utilization in the United States. Pediatrics 2003;112(2 I):314–319. doi: 10.1542/peds.112.2.314 [DOI] [PubMed] [Google Scholar]
- 5.Kubicek K, Liu D, Beaudin C, et al. A profile of nonurgent emergency department use in an Urban pediatric hospital. Pediatr Emerg Care 2012;28(10):977–984. doi: 10.1097/PEC.0b013e31826c9aab [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics 2001;107(3):524–529. doi: 10.1542/peds.107.3.524 [DOI] [PubMed] [Google Scholar]
- 7.Corwin GS, Parker DM, Brown JR. Site of Treatment for Non-Urgent Conditions by Medicare Beneficiaries: Is There a Role for Urgent Care Centers? Am J Med 2016;129(9):966–973. doi: 10.1016/j.amjmed.2016.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raphael JL, Tapia C, Fischer LS, McKeever J, Giardino AP. The medical home experience of low-income children with non-urgent encounters in acute care settings. J Health Care Poor Underserved 2016;27(4):1885–1898. doi: 10.1353/hpu.2016.0169 [DOI] [PubMed] [Google Scholar]
- 9.Kurt F, Beğde F, Oğuz S, Tekin D, Suskan E. How Important Are Parental Age and Educational Level in Nonurgent Admissions to the Pediatric Emergency Department? Pediatr Emerg Care August 2019:1. doi: 10.1097/pec.0000000000001886 [DOI] [PubMed] [Google Scholar]
- 10.May M, Brousseau DC, Nelson DA, et al. Why Parents Seek Care for Acute Illness in the Clinic or the ED: The Role of Health Literacy. Acad Pediatr 2018;18(3):289–296. doi: 10.1016/j.acap.2017.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doobinin KA, Heidt-Davis PE, Gross TK, Isaacman DJ. Nonurgent pediatric emergency department visits: Care-seeking behavior and parental knowledge of insurance. Pediatr Emerg Care 2003;19(1):10–14. doi: 10.1097/00006565-200302000-00003 [DOI] [PubMed] [Google Scholar]
- 12.Morrison AK, Chanmugathas R, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. Caregiver low health literacy and nonurgent use of the pediatric emergency department for febrile illness. Acad Pediatr 2014;14(5):505–509. doi: 10.1016/j.acap.2014.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salami O, Salvador J, Vega R. Reasons for Nonurgent Pediatric Emergency Department Visits. Pediatr Emerg Care 2012;28(1):43–46. doi: 10.1097/PEC.0b013e31823f2412 [DOI] [PubMed] [Google Scholar]
- 14.Brousseau DC, Gorelick MH, Hoffmann RG, Flores G, Nattinger AB. Primary Care Quality and Subsequent Emergency Department Utilization for Children in Wisconsin Medicaid. Acad Pediatr 2009;9(1):33–39. doi: 10.1016/j.acap.2008.11.004 [DOI] [PubMed] [Google Scholar]
- 15.Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why Do Parents Bring Children to the Emergency Department for Nonurgent Conditions? A Qualitative Study. Ambul Pediatr 2008;8(6):360–367. doi: 10.1016/j.ambp.2008.07.001 [DOI] [PubMed] [Google Scholar]
- 16.Sturm JJ, Hirsh D, Weselman B, Simon HK. Reconnecting Patients With Their Primary Care Provider. Clin Pediatr (Phila) 2014;53(10):988–994. doi: 10.1177/0009922814540987 [DOI] [PubMed] [Google Scholar]
- 17.Van Der Feltz-Cornelis CM, Van Oppen P, Van Marwijk HWJ, De Beurs E, Van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: Development and psychometric evaluation. Gen Hosp Psychiatry 2004;26(2):115–120. doi: 10.1016/j.genhosppsych.2003.08.010 [DOI] [PubMed] [Google Scholar]
- 18.Eveleigh RM, Muskens E, Van Ravesteijn H, Van Dijk I, Van Rijswijk E, Lucassen P. An overview of 19 instruments assessing the doctor-patient relationship: Different models or concepts are used. J Clin Epidemiol 2012;65(1):10–15. doi: 10.1016/j.jclinepi.2011.05.011 [DOI] [PubMed] [Google Scholar]
- 19.Green NA, Durani Y, Brecher D, Depiero A, Loiselle J, Attia M. Emergency severity index version 4: A valid and reliable tool in pediatric emergency department triage. Pediatr Emerg Care 2012;28(8):753–757. doi: 10.1097/PEC.0b013e3182621813 [DOI] [PubMed] [Google Scholar]
- 20.Brousseau DC, Nimmer MR, Yunk NL, Nattinger AB, Greer A. Nonurgent emergency-department care: Analysis of parent and primary physician perspectives. Pediatrics 2011;127(2):e375–e381. doi: 10.1542/peds.2010-1723 [DOI] [PubMed] [Google Scholar]
- 21.Herman A, Young KD, Espitia D, Fu N, Farshidi A. Impact of a Health Literacy Intervention on Pediatric Emergency Department Use. Pediatr Emerg Care 2009;25(7):434–438. doi: 10.1097/PEC.0b013e3181ab78c7 [DOI] [PubMed] [Google Scholar]
- 22.Chin NP, Goepp JG, Malia T, Harris L, Poordabbagh A. Nonurgent Use of a Pediatric Emergency Department. Pediatr Emerg Care 2006;22(1):22–27. doi: 10.1097/01.pec.0000195756.74328.21 [DOI] [PubMed] [Google Scholar]
- 23.Agency for Healthcare Research. Emergency Severity Index (ESI) A Triage Tool for Emergency Department Care Implementation Handbook 2012 Edition http://www.ahrq.gov. Accessed April 28, 2020.
- 24.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma V, Simon SD, Bakewell JM, Ellerbeck EF, Fox MH, Wallace DD. Factors influencing infant visits to emergency departments. Pediatrics 2000;106(5 I):1031–1039. doi: 10.1542/peds.106.5.1031 [DOI] [PubMed] [Google Scholar]
- 27.The Latest Emergency Department Utilization Numbers Are In - ACEP Now https://www.acepnow.com/article/the-latest-emergency-department-utilization-numbers-are-in/?elq_mid=40304&elq_cid=20112459&utm_campaign=25426&utm_source=eloquaEmail&utm_medium=email&utm_content=Email-Research-IssueAlert-ACEPeNOW_11-03-19_10-30-19.html&singlepage=1. Accessed April 28, 2020.
- 28.Gadomski A, Jenkins P, Nichols M. Impact of a Medicaid primary care provider and preventive care on pediatric hospitalization. Pediatrics 1998;101(3). doi: 10.1542/peds.101.3.e1 [DOI] [PubMed] [Google Scholar]
- 29.Burns RR, Alpern ER, Rodean J, et al. Factors Associated With Urgent Care Reliance and Outpatient Health Care Use Among Children Enrolled in Medicaid. JAMA Netw open 2020;3(5):e204185. doi: 10.1001/jamanetworkopen.2020.4185 [DOI] [PMC free article] [PubMed] [Google Scholar]


