Abstract
The use of a Viabahn VBX endoprosthesis (W. L. Gore & Associates, Flagstaff, Ariz) to exclude chronically thrombosed inferior vena cava (IVC) filters refractory to exclusion with self-expanding stents was evaluated. The mean duration of TrapEase IVC (Cordis, Milpitas, Calif) implantation was 7.6 years (range, 2-11 years). Symptoms included leg pain, edema, color changes, and back pain. The mean Villalta score and venous clinical severity score were 17 (range, 13-23) and 13 (range, 11-15), respectively. Indirect ultrasound evidence of stent patency was demonstrated at a mean of 8 months after intervention. The mean Villalta score and venous clinical severity score had decreased by 13 and 10, respectively, at a mean of 9.5 months after intervention. Iliocaval reconstruction with Viabahn VBX balloon expandable stent-graft exclusion of chronically thrombosed TrapEase IVC filters is safe, with favorable short-term results.
Keywords: Covered stents, Iliocaval thrombosis, IVC filters
A total of 2.8% to 3.9% of patients with an inferior vena cava (IVC) filter will develop filter-associated IVC thrombosis, which can cause pain, edema, phlegmasia, and ulceration.1,2 IVC filter retrieval success rates can be as high as 99.2%.3 However, cylindrical filters, such as the TrapEase (Cordis, Milpitas, Calif), have had decreased success rates.4 When filter retrieval is not possible, stent exclusion can be performed using self-expanding stents (SES) and balloon-expandable stents (BES).5 However, limited data are available on the use of BES grafts for this indication.6 In the present study, we evaluated the clinical and technical outcomes of iliocaval reconstruction using Viabahn VBX BES grafts (VBES; W. L. Gore & Associates, Flagstaff, Ariz) for IVC thrombosis secondary to chronically thrombosed and embedded cylindrical filters. All three patients provided written informed consent for the report of their case details and imaging studies. The institutional review board approved the present study, and the data were managed in accordance with the Health Insurance Portability and Accountability Act.
Case report
Patient 1
A 63-year-old man had presented with chronic bilateral lower extremity and back pain and limb discoloration. The Villalta score and venous clinical severity score (VCSS) were both 15. Computed tomography (CT) and venography demonstrated a thrombosed and calcified TrapEase IVC filter (Fig, A) with complete occlusion to the bilateral common femoral veins (CFVs; Fig, B). The filter had been placed 11 years previously. Recanalization was required for symptomatic iliocaval occlusion and was performed from the bilateral CFVs and right internal jugular vein (IJV). Pharmacomechanical thrombectomy was followed by filter exclusion and iliocaval reconstruction with parallel, bilateral, overlapping SES dilated using venoplasty to 12 to 16 mm. An acute clot had formed within the SES (Fig, C) secondary to severe narrowing by the filter (Fig, D). The SES were reinforced with parallel 11-mm × 79-mm VBES dilated to 16 mm (Fig, E). In-line flow was established from the lower extremities to the right atrium (Fig, F). The patient was hospitalized for 1 day. Ultrasound (US) at last imaging follow-up at 6 months after the intervention demonstrated patent bilateral CFVs, femoral veins (FVs), and popliteal veins (PVs). Both CFVs demonstrated increased waveforms during forced expiration, suggesting indirect iliac and IVC patency. The Villalta score and VCSS had decreased to 2 and 5, respectively, at the last clinical follow-up at 7 months. He continued taking rivaroxaban.
Fig.
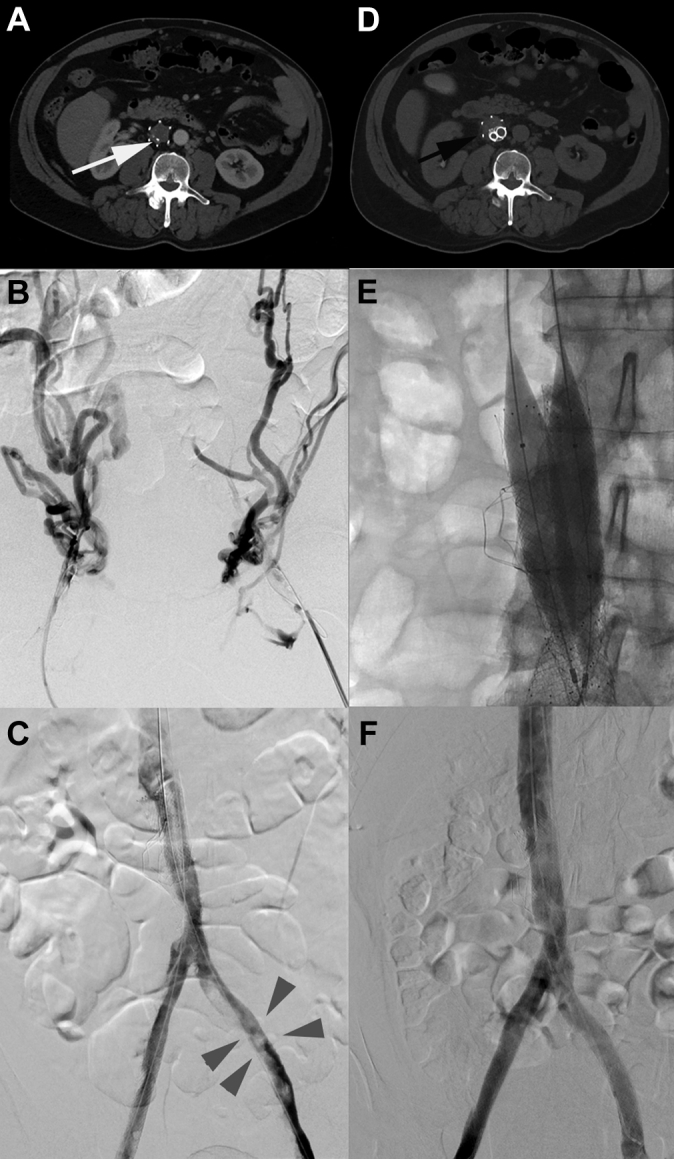
A, Contrast-enhanced abdominal and pelvic computed tomography (CT) scan demonstrating a completely thrombosed TrapEase (Cordis) inferior vena cava (IVC) filter with chronically calcified intraluminal thrombus (white arrow). B, Bilateral common femoral veins (CFVs) venography demonstrating complete occlusion of the iliocaval system with robust collateralization. C, Bilateral CFVs venography demonstrating iliocaval reconstruction with placement of overlapping S.M.A.R.T. stents (Cordis) and Wallstents (Boston Scientific, Waltham, Mass) at the level of the IVC filter. Sluggish flow and the development of acute thrombus was present within the stents (gray arrowheads). D, Non–contrast-enhanced CT scan of the abdomen during recanalization demonstrating parallel overlapping S.M.A.R.T. stents and Wallstents at the level of the calcified and thrombosed IVC filter with incomplete expansion of the right-sided stents (black arrow). E, Spot fluoroscopy demonstrating simultaneous deployment of parallel Viabahn VBX stents across the area of persistent narrowing. F, Venography from the bilateral CFVs demonstrating brisk in-line flow throughout the stent construct.
Patient 2
A 66-year-old man had presented with a 2-week history of bilateral lower extremity edema and pain. The Villalta score and VCSS were 13 and 11, respectively. CT demonstrated a calcified and thrombosed TrapEase IVC filter with partial occlusion of the left common and external iliac veins. The filter had been placed 10 years previously. Recanalization was required for symptomatic iliocaval occlusion and was performed from the right CFV, left PV, and right IJV. Pharmacomechanical thrombectomy was followed by attempted IVC filter retrieval using the excimer laser (Spectranetics, Colorado Springs, Colo) and endobronchial forceps (No. 4162; LYMOL Medical, Woburn, Mass) but was unsuccessful due to the large volume of calcified thrombus, which prevented laser sheath advancement. IVC filter exclusion and iliocaval reconstruction were performed with parallel bilateral overlapping SES dilated using venoplasty to 12 to 16 mm. The SES at the level of the IVC filter were narrowed, with repeated high-pressure balloon rupture. They were reinforced with parallel 11-mm × 79-mm VBES dilated to 16 mm. In-line flow was established from the lower extremities to the right atrium. The patient was hospitalized for 2 days. US at the last imaging follow-up at 9 months after the intervention demonstrated patent bilateral CFVs, FVs, and PVs. Both CFVs demonstrated increased waveforms during forced expiration, suggesting indirect iliac and IVC patency. The Villalta score and VCSS had decreased to 3 and 4, respectively, at his last clinical follow-up at 11 months after the intervention. He continued taking rivaroxaban.
Patient 3
A 72-year-old man had presented with a 7-day history of bilateral lower extremity swelling and pain. The Villalta score and VCSS were 23 and 14, respectively. CT demonstrated a thrombosed TrapEase IVC filter with completely thrombosed, expanded, and edematous bilateral iliofemoral and PVs. The IVC filter had been placed 2 years previously. Recanalization was required for symptomatic iliocaval occlusion and was performed from the bilateral PVs and right IJV. Pharmacomechanical thrombectomy was followed by IVC filter exclusion and iliocaval reconstruction with parallel bilateral overlapping SES dilated using venoplasty to 12 to 16 mm. Because of the recurrent thrombus formation within the stents that developed overnight, thrombolysis was initiated. Subsequently, the thrombus burden improved; however, the SES were severely narrowed by the IVC filter. Thus, they were reinforced with parallel 11-mm × 79-mm VBES dilated to 16 mm. In-line flow was established from the lower extremities to the right atrium. This patient developed transient acute kidney injury from contrast administration. He was hospitalized for 7 days; his creatinine had increased from 0.89 to 1.53 mg/dL but had normalized to 0.75 mg/dL at discharge. US at the last imaging follow-up at 11 months after the intervention demonstrated patent bilateral CFVs, FVs, and PVs. Both CFVs demonstrated increased waveforms during forced expiration, suggesting indirect iliac and IVC patency. The Villalta score and VCSS had decreased to 6 and 4, respectively, at his last follow-up at 11 months after the intervention. He continued taking enoxaparin.
For all three patients, the intraprocedural activated clotting time was maintained at >250 seconds with heparin, and stent selection was determined by operator preference and availability (Table). Finally, additional stenting was not needed after VBES placement. None of the patients experienced pulmonary embolism or renal vein thrombosis or required reintervention. The contrast agent used was iohexol (Omnipaque 300; mean, 265 mL; range, 230-325 mL), with a mean fluoroscopy time of 187 minutes (range, 90-249 minutes). The mean serum creatinine was 0.78 mg/dL (range, 0.70-0.89 mg/dL). Antiplatelet agents were not used. All patients wore above the knee compression stockings with 30 to 40 mm Hg of compression, and none had had venous ulcers.
Table.
Stent type, number, and size used per patient
| Stent type | Stent size (No. used) |
||
|---|---|---|---|
| Patient 1 | Patient 2 | Patient 3 | |
| S.M.A.R.T stent | 12 mm × 80 mm (2); 14 mm × 80 mm (2) | 12 mm × 80 mm (6); 14 mm × 80 mm (2) | NA |
| Wallstent (Boston Scientific, Waltham, Mass) | 12 mm × 60 mm (2); 14 mm × 90 mm (2) | 14 mm × 90 mm (2); 16 mm × 90 mm (1) | NA |
| Protege stent (Medtronic, Dublin, Ireland) | NA | NA | 10 mm × 80 mm (2) |
| Vici Venous stent (Boston Scientific) | NA | NA | 14 mm × 120 mm (2); 16 mm × 90 mm (2) |
| Viabahn VBX stent (W. L. Gore) | 11 mm × 79 mm (2)a | 11 mm × 79 mm (2)a | 11 mm × 79 mm (2)a |
NA, Not applicable.
Gore Viabahn VBX stents were simultaneously ballooned to 16 mm.
Discussion
Cylindrical filters have been shown to have decreased retrieval success.4,7 When retrieval is not possible, iliocaval reconstruction with stent exclusion of chronically embedded IVC filters has had technical and clinical success of 83% to 100%5,8, 9, 10 and 60% to 96%,5,9 respectively. Most studies have used SES,5,8, 9, 10, 11, 12 although some have demonstrated success with BES.8,9,13 IVC filters will typically be excluded with SES; however, when compression is refractory, the options become limited to placing additional overlapping SES, a bare metal BES, or a BES graft such as a VBES. Compared with bare metal BES, the VBES has longer diameters to span the entire IVC filter and is covered to prevent balloon rupture. In the present study, parallel reinforcement of chronic and calcified intrafilter thrombus with VBES restored in-line flow in all three patients. US demonstrated patent PVs to CFVs and indirect iliocaval patency during follow-up (mean, 8 months; range, 6-11 months). The average Villalta score and VCSS had decreased by 13 and 10, respectively, at the last follow-up (mean, 9.5 months; range, 7-11 months). No technical complications developed, and no reinterventions were required. One patient had developed transient acute kidney injury.
VBES have been successfully used in occluded pediatric mesoportal shunts,14 non–filter-associated iliocaval occlusion,15 and axillary vein injury.16 Although stent-grafts have had high success rates to treat hemodialysis outflow stenosis,17 the iliocaval system has substantially lower flow and the available data are limited. A literature review demonstrated the successful use of iliocaval stent-grafts for aortocaval fistula, thrombosis, IVC injury, and IVC agenesis, with patent stents at the last follow-up (range, 1 week to 7 years).18, 19, 20, 21, 22, 23, 24, 25, 26, 27 The largest retrospective review demonstrated 90% primary patency in 10 patients who had received stent-grafts for chronic iliocaval disease.28 Overall, the reported data have demonstrated favorable short-term results, similar to the findings from the present study. VBES can theoretically cause filter fracture, embolization, and displacement into nearby structures from the pressure exerted by stent placement. Furthermore, the long-term patency of iliocaval stent-grafts is unknown.
Conclusions
Iliocaval reconstruction with VBES exclusion of chronically thrombosed TrapEase IVC filters is safe, with favorable short-term results.
Footnotes
Author conflict of interest: B.B.T. is an advisor for BTG, Johnson & Johnson, Boston Scientific, and AstraZeneca. C.A.R. has a current consulting agreement with Baxter and had had a consulting agreement with BTG that ended in January 2020. M.E., A.R.L., G.T.F., and Z.D. have no conflicts of interest.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Angel L.F., Tapson V., Galgon R.E., Restrepo M.I., Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol. 2011;22:1522–1530.e3. doi: 10.1016/j.jvir.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Jia Z., Fuller T.A., McKinney J.M., Paz-Fumagalli R., Frey G.T., Sella D.M. Utility of retrievable inferior vena cava filters: a systematic literature review and analysis of the reasons for nonretrieval of filters with temporary indications. Cardiovasc Intervent Radiol. 2018;41:675–682. doi: 10.1007/s00270-018-1880-9. [DOI] [PubMed] [Google Scholar]
- 3.Kuo W.T., Odegaard J.I., Rosenberg J.K., Hofmann L.V. Laser-assisted removal of embedded vena cava filters: a 5-year first-in-human study. Chest. 2017;151:417–424. doi: 10.1016/j.chest.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 4.Pratt W.B., Sandhu H.K., Leake S.S., Jamshidy I., Sola C.N., Afifi R.O. Asymptomatic patients with unsuccessful percutaneous inferior vena cava filter retrieval rarely develop complications despite strut penetrations through the caval wall. J Vasc Surg Venous Lymphat Disord. 2020;8:54–61. doi: 10.1016/j.jvsv.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Chick J.F.B., Jo A., Meadows J.M., Abramowitz S.D., Khaja M.J., Cooper K.J. Endovascular iliocaval stent reconstruction for inferior vena cava filter–associated iliocaval thrombosis: approach, technical success, safety, and two-year outcomes in 120 patients. J Vasc Interv Radiol. 2017;28:933–939. doi: 10.1016/j.jvir.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Krankenberg H., Zeller T., Ingwersen M., Schmalstieg J., Gissler H.M., Nikol S. Self-expanding versus balloon-expandable stents for iliac artery occlusive disease: the randomized ICE trial. JACC Cardiovasc Interv. 2017;10:1694–1704. doi: 10.1016/j.jcin.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Kuo W.T., Odegaard J.I., Rosenberg J.K., Hofmann L.V. Excimer laser-assisted removal of embedded inferior vena cava filters: a single-center prospective study. Circ Cardiovasc Interv. 2013;6:560–566. doi: 10.1161/CIRCINTERVENTIONS.113.000665. [DOI] [PubMed] [Google Scholar]
- 8.Vedantham S., Vesely T.M., Parti N., Darcy M.D., Pilgram T.K., Sicard G.A. Endovascular recanalization of the thrombosed filter-bearing inferior vena cava. J Vasc Interv Radiol. 2003;14:893–903. doi: 10.1097/01.rvi.0000083842.97061.c9. [DOI] [PubMed] [Google Scholar]
- 9.Arabi M., Krishnamurthy V., Cwikiel W., Vellody R., Wakefield T.W., Rectenwald J. Endovascular treatment of thrombosed inferior vena cava filters: techniques and short-term outcomes. Indian J Radiol Imaging. 2015;25:233–238. doi: 10.4103/0971-3026.161436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Partovi S., Kalva S.P., Walker T.G., Taj S.M., Ganguli S. Long term follow-up of endo-vascular recanalization of chronic inferior vena cava occlusion secondary to inferior vena cava filters. Vasa. 2017;46:121–126. doi: 10.1024/0301-1526/a000593. [DOI] [PubMed] [Google Scholar]
- 11.Desai K.R., Xiao N., Karp J., Salem R., Rodriguez H., Eskandari M. Single-session inferior vena cava filter removal, recanalization, and endovenous reconstruction for chronic iliocaval thrombosis. J Vasc Surg Venous Lymphat Disord. 2019;7:176–183. doi: 10.1016/j.jvsv.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Ye K., Lu X., Li W., Yin M., Liu X., Qin J. Outcomes of stent placement for chronic occlusion of a filter-bearing inferior vena cava in patients with severe post-thrombotic syndrome. Eur J Vasc Endovasc Surg. 2016;52:839–846. doi: 10.1016/j.ejvs.2016.08.050. [DOI] [PubMed] [Google Scholar]
- 13.Meltzer A.J., Connolly P.H., Kabutey N.K., Jones D.W., Schneider D.B. Endovascular recanalization of iliocaval and inferior vena cava filter chronic total occlusions. J Vasc Surg Venous Lymphat Disord. 2015;3:86–89. doi: 10.1016/j.jvsv.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Stein E.J., Shivaram G.M., Koo K.S.H., Dick A.A.S., Healey P.J., Monroe E.J. Endovascular treatment of surgical mesoportal and portosystemic shunt dysfunction in pediatric patients. Pediatr Radiol. 2019;49:1344–1353. doi: 10.1007/s00247-019-04458-6. [DOI] [PubMed] [Google Scholar]
- 15.McDevitt J.L., Srinivasa R.N., Hage A.N., Bundy J.J., Gemmete J.J., Srinivasa R.N. Total endovenous recanalization and stent reconstruction for naïve non-inferior vena cava filter-associated chronic iliocaval occlusive disease: placement of 352 venous stents in 69 debilitated patients. Vasc Med. 2019;24:349–358. doi: 10.1177/1358863X19834354. [DOI] [PubMed] [Google Scholar]
- 16.Kumar V. Endovascular treatment of penetrating injury of axillary vein with Viabahn endoprosthesis. J Vasc Surg. 2004;40:1243–1244. doi: 10.1016/j.jvs.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 17.Boutrous M.L., Alvarez A.C., Okoye O.T., Laws J.C., Jacobs D.L., Smeds M.R. Stent-graft length is associated with decreased patency in treatment of central venous stenosis in hemodialysis patients. Ann Vasc Surg. 2019;59:225–230. doi: 10.1016/j.avsg.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Harmon T.S., Villescas V.V., Hood P., Meyer T.E., Matteo J. When technology exceeds its application: the first reported reconstruction of the iliocaval confluence using an aortic endograft. Cureus. 2019;11:e4640. doi: 10.7759/cureus.4640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braun J.D., McCluskey K., Pinter J., Kilbridge M. Complete external iliac vein transection during hip arthroplasty requiring stent graft reconstruction with long-term follow-up. J Vasc Interv Radiol. 2019;30:1060–1061. doi: 10.1016/j.jvir.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 20.Watarida S., Nishi T., Furukawa A., Shiraishi S., Kitano H., Matsubayashi K. Fenestrated stent-graft for traumatic juxtahepatic inferior vena cava injury. J Endovasc Ther. 2002;9:134–137. doi: 10.1177/152660280200900122. [DOI] [PubMed] [Google Scholar]
- 21.Briggs C.S., Morcos O.C., Moriera C.C., Gupta N. Endovascular treatment of iatrogenic injury to the retrohepatic inferior vena cava. Ann Vasc Surg. 2014;28:1794.e13–1794.e15. doi: 10.1016/j.avsg.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 22.El Khoury R., Kunda N.M., Keldahl M.L. Endovascular treatment of a penetrating injury of the suprarenal inferior vena cava. J Vasc Surg Venous Lymphat Disord. 2019;7:247–250. doi: 10.1016/j.jvsv.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Chick J.F.B., Khaja M.S., Han S., Cooper K.J., Meadows J.M., Williams D.M. Single-session total endovascular iliocaval reconstruction with stent grafting for the treatment of inferior vena cava agenesis and concurrent iliac venous aneurysm rupture. J Vasc Surg Cases Innov Tech. 2017;3:132–135. doi: 10.1016/j.jvscit.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hinojosa C.A., Lizola R., Laparra-Escareno H., Anaya-Ayala J.E. Endovascular recanalisation of a chronic occlusion of the retrohepatic IVC associated to a filter in a patient with antiphospholipid syndrome. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2016-218697. bcr2016218697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frenk N.E., Salazar G.M., Vazquez R., Irani Z. Intravascular cement leak after vertebroplasty treated with stent graft placement in the inferior vena cava. J Vasc Interv Radiol. 2019;30:74–75. doi: 10.1016/j.jvir.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Falkowski A., Wiernicki I. Stent-graft implantation to treat an inferior vena cava aneurysm. J Endovasc Ther. 2013;20:714–717. doi: 10.1583/13-4368R.1. [DOI] [PubMed] [Google Scholar]
- 27.Erzurum V.Z., Shoup M., Borge M., Kalman P.G., Rodriguez H., Silver G.M. Inferior vena cava endograft to control surgically inaccessible hemorrhage. J Vasc Surg. 2003;38:1437–1439. doi: 10.1016/s0741-5214(03)00919-4. [DOI] [PubMed] [Google Scholar]
- 28.Flynn S., Jensen R., Lane J., Bandyk D., Malas M., Barleben A. Novel approach to treatment of chronic iliocaval occlusion utilizing covered stents. Ann Vasc Surg. 2020;67:300–305. doi: 10.1016/j.avsg.2020.02.010. [DOI] [PubMed] [Google Scholar]


