Abstract
Background
In December 2020, Moderna released the mRNA-1273 vaccine. The most common side effects are headache, muscle pain, redness, swelling, and tenderness at the injection site. In addition, there have been dermatological adverse events, such as hypersensitivity reactions. Although rare, various bullous eruptions have been described following vaccination. Bullous pemphigoid has been reported to occur most often after receipt of influenza and the diphtheria-tetanus-pertussis vaccine. To the best of our knowledge, there have been no reports of bullous drug eruptions resulting from mRNA vaccines.
Case summary
A 66-years-old obese Guyanese male presented with a bullous rash following receipt of a commercial COVID-19 mRNA vaccine. He received the first dose uneventfully. However, within 24 h of receiving the second dose, he developed fever, myalgias, and malaise accompanied by a painful blistering rash of his torso, arms, and legs. His fever and myalgias improved after 24 h, but his painful rash did not, and five days after the initial symptoms, he presented to the hospital. There were many violaceous, poorly demarcated patches on his trunk, arms, and thighs on examination, many of which had large flaccid bullae within, and a few areas on his buttocks, posterior shoulder, and scrotum were eroded. The exam was also significant for lower extremity muscle tenderness, stiffness with preserved strength. A skin biopsy showed epidermal necrosis and sparse perivascular dermatitis concerning Stevens-Johnson syndrome or erythema multiforme. However, in the absence of mucous membrane involvement or targetoid lesions, the diagnosis of an extensive bullous fixed drug eruption was made.
Conclusion
This case illustrates that the bullae eruption occurred as a result of receiving the Moderna vaccination.
Keywords: Bullous drug, Moderna, 2019-nCoV, SARS-Cov-2, mRNA-1273 vaccine, Case report
Introduction
In 2019, a strain of coronavirus (SARS-CoV-2, which is an enveloped RNA coronavirus family member that causes severe acute respiratory syndrome) created a pandemic and global health crisis [1]. In December 2020, ModernaTX released the mRNA-1273 (Moderna) vaccine, which is a novel lipid nanoparticle (LNP)-an encapsulated mRNA-based vaccine that codes for the spike (S) protein of SARS-Cov-2 [2,3]. The most common side effects (90%) of the vaccination are headache, muscle pain, redness, swelling, and tenderness at the injection site [[2], [3], [4]]. There have been dermatological adverse events (AE) cases, such as hypersensitivity reactions to particular ingredients in the vaccine. Erythema multiforme (EM) is a hypersensitivity reaction characterized by a central duskiness in an expanding erythematous macule or papule, usually caused by mycoplasma, herpes simplex, and medications (sulfonamides, NSAIDs, and anticonvulsants) [5]. More severe hypersensitivity reactions include Stevens-Johnson syndrome (SJS), <10% body surface area (BSA), and toxic epidermal necrolysis (TEN), >30% BSA. Both involve bullae formation and sloughing of the skin [2]. EM, SJS, and TEN were rarely reported as a result of vaccination. Most cases were linked to childhood vaccination (combined measles, mumps, and rubella), DtaP, and varicella vaccination [4].
Compared to these vaccines based on conventional technologies, mRNA vaccines utilize a novel technology that induces robust immunogenicity and higher efficacy. Due to its novelty, little is known regarding the side effects of mRNA vaccines, especially dermatological side effects. To the best of our knowledge, there have been no reports of bullous fixed drug eruptions resulting from mRNA vaccines. Here we report a case of bullous fixed drug eruption occurring as a result of administration of the second dose of the Moderna vaccine.
Case report
A 66-years-old obese Guyanese male with a past medical history of hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease (CKD), coronary artery disease, and idiopathic hypothyroidism presented with a violaceous rash following receipt of a commercial COVID-19 mRNA vaccine. The patient received the first dose of the two-dose vaccination series uneventfully. However, within 24 h of receiving the second dose, he developed a fever and myalgias accompanied by a painful rash that evolved into large blisters. He did not report any known drug or food allergies or rheumatological disease. He reported a sibling who died of complications of myasthenia gravis. He denied smoking or recreational drug use; he endorsed drinking socially. His home medications included amlodipine PO 5 mg daily, aspirin PO 81 mg daily, brimonidine 0.1% solution topical twice daily, clopidogrel PO 75 mg daily, famotidine 20 mg PO twice daily, furosemide 20 mg PO daily, gabapentin 300 mg PO twice daily, insulin aspart 15 units subcutaneously twice daily, insulin glargine 50 units subcutaneously nightly, levothyroxine 50 μg PO daily, lisinopril 5 mg PO daily, metoprolol 50 mg PO daily, pravastatin 40 mg PO daily, and tamsulosin 0.4 mg PO daily.
The patient presented to the emergency department five days after the onset of symptoms due to persistent skin lesions and pain. His vital signs were within normal range, with a BMI of 31.65. On examination, he had extensive areas of painful violaceous patches on his abdomen, buttocks, and lower extremities, many of which developed into large flaccid bullae (Fig. 1 ). He had no involvement in his mucous membranes, palms, soles, joints, or targetoid lesions. The exam was also significant for lower extremity muscle tenderness, stiffness, with preserved strength—Naranjo scale score 6.
Fig. 1.
The patient presented with multiple violaceous patches with the development of blisters on some patches.
Initial laboratory findings included hyperkalemia, hyperglycemia, mild transaminitis, serum CK of 347, and an incidental finding of mild AKI on CKD. Serum antibodies to bullous pemphigoid, BP 180 and BP 230, were 8 and <2 respectively (within the normal limit with range <20). A biopsy was taken from the right anterior thigh. The histopathology showed full-thickness epidermal necrosis and a very sparse lymphocytic inflammatory infiltrate (Fig. 2 ). Based on the clinical and histopathological findings, the diagnosis of a bullous drug eruption with features of Stevens-Johnson syndrome was made. The patient initially received ibuprofen to improve myalgias and high-dose oral prednisone. The patient's bullae were drained, and he was given mupirocin ointment with Vaseline combination for wound care. He was discharged on the 7th day of the hospital with a prednisone taper with outpatient dermatology follow-up.
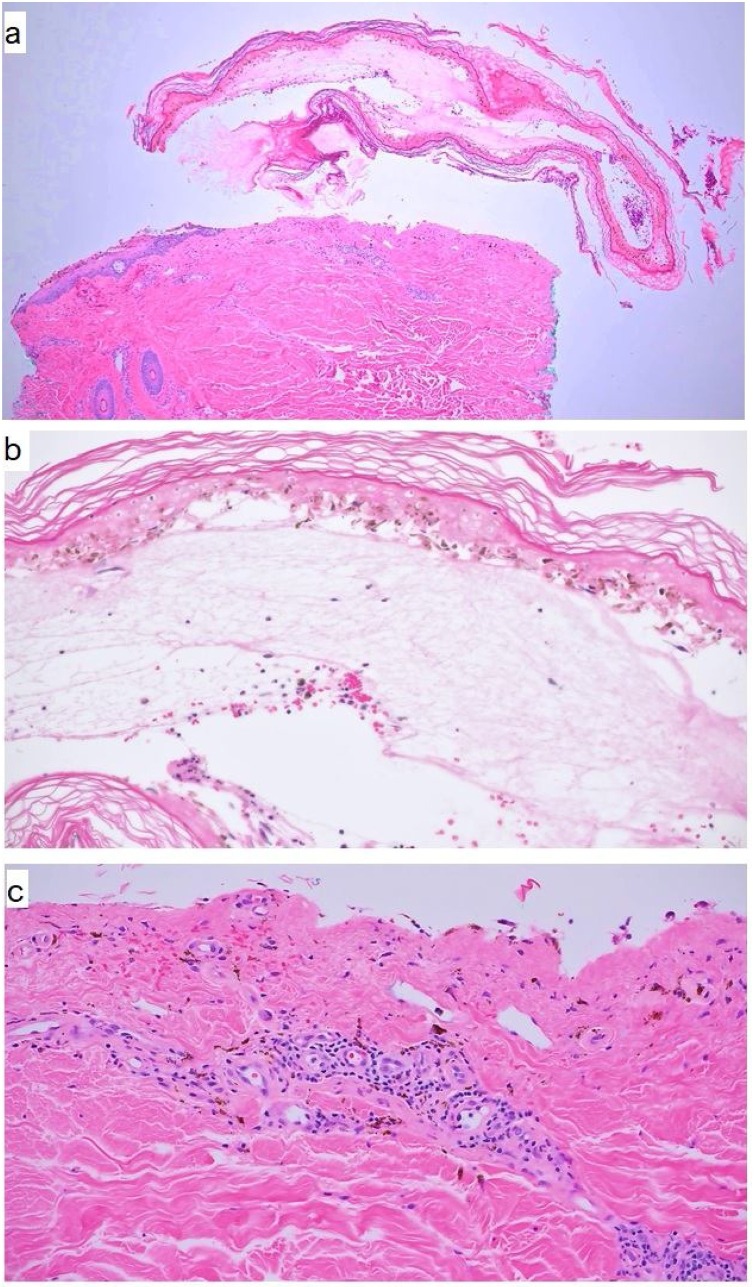
Fig. 2.
a: Full-thickness epidermal necrosis with detachment from the underlying dermis to form a subepidermal blister (H&E; ×40). b: Higher magnification demonstrates full-thickness epidermal necrosis (H&E; ×100). c: Higher magnification demonstrates subepidermal blister with extravasated red blood cells, melanophages, lymphocytic perivascular infiltrate with no evidence of vasculitis (H&E; ×100).
Discussion
Bullous drug eruptions with erythema multiforme, Stevens–Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN) have rarely been reported as post-vaccination adverse events [4]. The incidence is 1.2–6.0 per million person-years for SJS and 0.4–1.2 per million person-years for TEN [6]. After vaccination, the onset of symptoms typically occurs within 14 days; most SJS begins within three days of vaccination [4]. Symptoms usually include a prodromal with flu-like symptoms that appear 1–3 days prior to the eruptions [4]. Skin lesions can initially be macular erythema or an exanthematous eruption but can also form bullae, then desquamate [5]. Lesions on mucosal surfaces are often involved. Most reports of EM (91%) were non-life-threatening, while most cases of SJS (52%), and all reports of SJS/TEN and TEN were serious [4].
Treatment of bullous drug eruption is symptomatic. Management includes discontinuation of the offending agent. Lesions generally resolve without treatment and leave postinflammatory hyperpigmentation. Antihistamines such as diphenhydramine and hydroxyzine help relieve pruritis [7]. Patients with bullous lesions and generalized drug eruption are generally placed on a short course of high-dose oral corticosteroids.
We describe a patient with a severe skin reaction within 24 h after the second Moderna vaccination, clinically concerning for a severe bullous fixed drug eruption but with features of Stevens–Johnson Syndrome on pathology. However, given the lack of mucous membrane involvement or targetoid lesions, diagnosis of extensive bullous fixed drug eruption was made. He denies any new changes in medications or lifestyle habits besides obtaining his vaccination. Typical cutaneous manifestations of COVID-19 disease are morbilliform rash, urticarial, vesicular eruptions, acral lesions, and livedoid eruption [7]. Our patient was tested negative for COVID-19. This case illustrates that the bullae eruption occurred as a result of receiving the Moderna vaccination and rather than the COVID-19.
Funding
None.
Competing interests
The authors confirm the absence of personal and financial interests impacting the outcomes of this research study.
Informed consent
Written informed consent was obtained for pictures and publication.
Author contributions
All authors contributed equally in writing and reviewing this case report.
Acknowledgments
None.
References
- 1.Pal M., Berhanu G., Desalegn C., Kandi V. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): an update. Cureus. 2020;12(3) doi: 10.7759/cureus.7423. PMID: 32337143; PMC7182166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson E.J., Rouphael N.G., Widge A.T., Jackson L.A., Roberts P.C., Makhene M. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N Engl J Med. 2020;383(25):2427–2438. doi: 10.1056/NEJMoa2028436. PMID: 32991794; PMC7556339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jackson L.A., Anderson E.J., Rouphael N.G., Roberts P.C., Makhene M., Coler R.N. An mRNA vaccine against SARS-CoV-2—preliminary report. N Engl J Med. 2020;383(20):1920–1931. doi: 10.1056/NEJMoa2022483. PMID: 32663912; PMC7377258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su J.R., Haber P., Ng C.S., Marquez P.L., Dores G.M., Perez-Vilar S. Erythema multiforme, Stevens Johnson syndrome, and toxic epidermal necrolysis reported after vaccination, 1999–2017. Vaccine. 2020;38(7):1746–1752. doi: 10.1016/j.vaccine.2019.12.028. PMID: 31870573; PMC7008074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habif T.P. sixth edition. Elsevier; 2016. Clinical dermatology: a color guide to diagnosis and therapy. [Google Scholar]
- 6.Klimas N., Quintanilla-Dieck J., Vandergriff T. Stevens–Johnson syndrome and toxic epidermal necrolysis. Cutaneous Drug Eruptions. 2015:259–269. doi: 10.1007/978-1-4471-6729-7_24. PMID: PMC7121137. [DOI] [Google Scholar]
- 7.Young S., Fernandez A.P. Skin manifestations of COVID-19. Cleve Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc031. PMID: 32409442. [DOI] [PubMed] [Google Scholar]