Coronavirus disease (COVID-19) has been related with numerous neurological manifestations [1]. Cranial neuropathies have been reported in patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [2], mainly affecting cranial nerves related to the senses of smell and taste, facial nerve palsy and oculomotor paresis. However, optic nerve involvement has rarely been reported associated with COVID-19 [3], [4]. Substantial evidence has suggested that severe SARS-CoV-2 infection may predispose to venous and arterial thromboembolism, particularly in critically ill patients such our case [5]. Multiple factors associated with COVID-19 might contribute to these vascular events, including hypercoagulability, dysregulated immune response and endothelial cells damage leading to thrombosis among others [6], [7], [8]. Hence, these vascular phenomena related to COVID-19 may lead to ischemic complications at different levels, including the cranial nerves [1], [3].
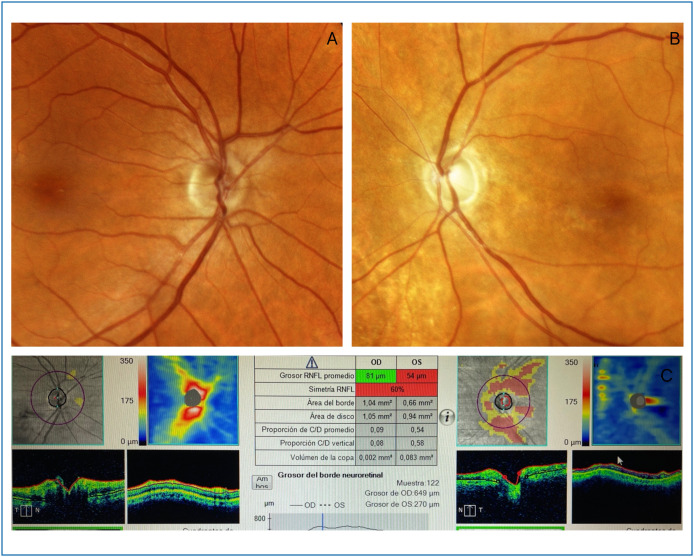
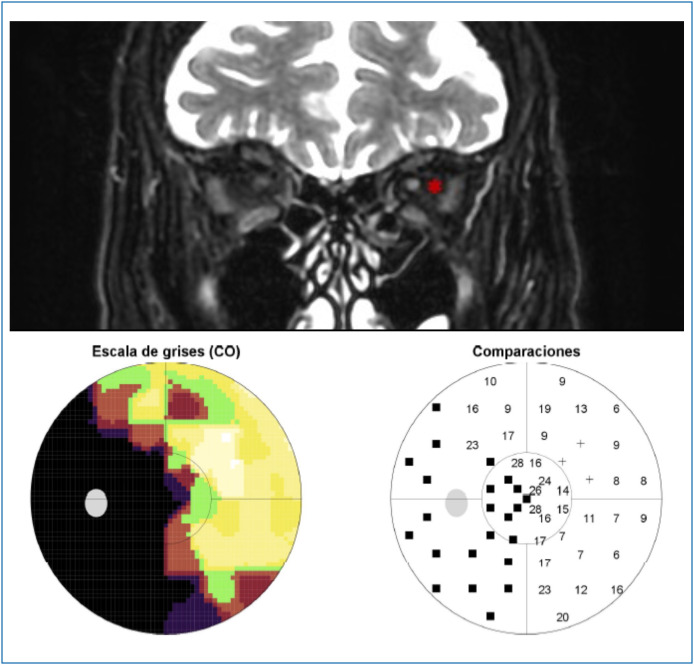
A 66-year-old healthy woman with unremarkable medical history was admitted to the internal medicine unit for bilateral pneumonia due to COVID-19 with severe respiratory failure requiring admission to the intensive care unit (ICU). The patient reported painless vision loss in the left eye upon awakening after 40 days in the ICU. Ophthalmologic examination revealed visual acuity of 0.9 in the right eye (OD) and hand movement in the left eye (OS), with a relative afferent pupillary defect in OS. Fundus examination of the right eye was unremarkable, while the left eye showed a marked optic nerve head pallor and large cupping, in the absence of edema, hemorrhages or other lesions. Narrowing of the retinal arterioles was also present in that eye (Fig. 1A). Optical coherence tomography (OCT) of the OI evidenced a severe reduction of the peripapillary retinal nerve fiber layer thickness (Fig. 1B) that correlated with a significant temporal visual field defect in that eye (Fig. 2 ). Orbital MRI showed a discrete signal enhancement in the left optic nerve suggestive of optic neuropathy, without any parenchymal ischemic alteration (Fig. 1C).
Figure 1.
A. Fundus photography of both eyes, showing a marked pallor of the optic nerve head of the left eye and unremarkable findings in the right eye. B. Optical coherence tomography (OCT) scan depicting a reduction of the peripapillary retinal nerve fiber layer thickness in the left eye. C. Visual field of the left eye performed by Octopus campimetry showing a significant temporal visual field defect.
Figure 2.
Orbital MRI revealing a discrete signal enhancement in the left optic nerve (*) without any parenchymal ischemic alteration.
Given that the patient presented in this case had no cardiovascular risk factors and a positive temporal relationship between the onset of visual symptoms and COVID-19, in this setting a supervening vascular phenomenon as a consequence of the disease may be a plausible mechanism leading to optic nerve damage.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Favas T.T., Dev P., Chaurasia R.N., Chakravarty K., Mishra R., Joshi D., et al. Neurological manifestations of COVID-19: a systematic review and meta-analysis of proportions. Neurol Sci. 2020;41:3437–3470. doi: 10.1007/s10072-020-04801-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello F., Dalakas M.C. Cranial neuropathies and COVID-19: neurotropism and autoimmunity. Neurology. 2020;95:195–196. doi: 10.1212/WNL.0000000000009921. [DOI] [PubMed] [Google Scholar]
- 3.Rho J., Dryden S.C., McGuffey C.D., Fowler B.T., Fleming J. A case of non-arteritic anterior ischemic optic neuropathy with COVID-19. Cureus. 2020;12:e11950. doi: 10.7759/cureus.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodrigo-Armenteros P., Uterga-Valiente J.M., Zabala-Del-Arco J., Taramundi-Argüeso S., Antón-Méndez L., Gómez-Muga J.J., et al. Optic neuropathy in a patient with COVID-19 infection. Acta Neurol Belg. 2021 doi: 10.1007/s13760-021-01600-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers DAMPJ, Kant K.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abou-Ismail M.Y., Diamond A., Kapoor S., Arafah Y., Nayak L. The hypercoagulable state in COVID-19: incidence, pathophysiology, and management. Thromb Res. 2020;194:101–115. doi: 10.1016/j.thromres.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F., et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gris J.-C., Perez-Martin A., Quéré I., Sotto A. COVID-19 associated coagulopathy: the crowning glory of thrombo-inflammation concept. Anaesthesia. Crit Care Pain Med. 2020;39:381–382. doi: 10.1016/j.accpm.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]