Case description
Acute macular outer retinopathy (AMOR) or type 2 acute macular neuroretinopathy (AMN) is a rare retinal disorder initially described by Bos and Deutman in 1975 [1]. Its pathogenesis is still unclear, but deep capillary retinal ischemia due to various causes has been incriminated, flu-like illness being the most commonly reported association [2].
We report a case of unilateral AMOR following a SARS-CoV-2 infection, assessed with multimodal imaging.
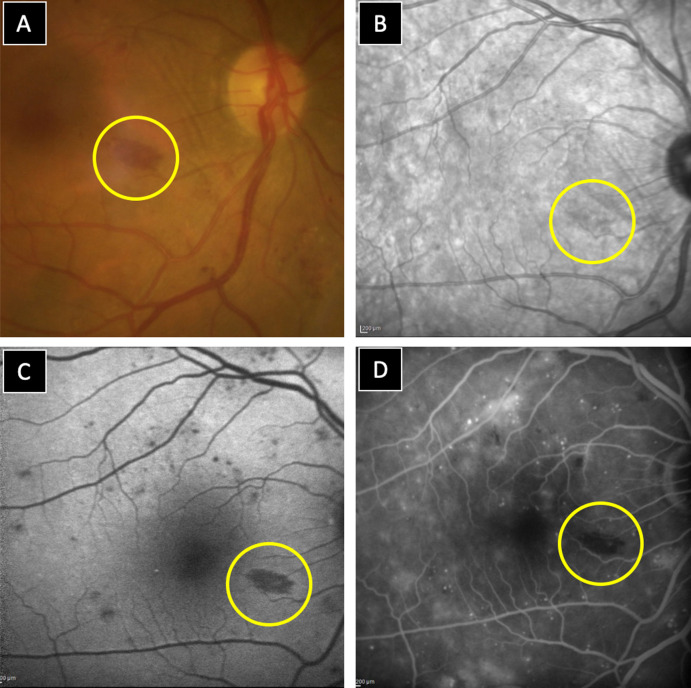
A 75-year-old diabetic female patient was referred to our department for diabetic retinopathy screening. Fundus examination and colour fundus photography (CFP) showed non proliferative DR in both eyes, but we noted the presence of an intermaculopapillary reddish-brown well-limited rectangular lesion in the right eye (RE). It looked like a too well-limited deep retinal hemorrhage (Fig. 1 A).
Figure 1.
Multimodal imaging of AMOR lesion in the RE (yellow circles) showing an intermaculopapillary reddish-brown well-limited rectangular lesion on CFP (A), with a slightly hypo-reflective appearance on IR (B), a well-demarcated hypoautofluorescence on blue-light FAF (C) and hypofluorescnce on FA (D).
On infrared imaging (IR), the lesion appeared slightly hypo-reflective (Fig. 1B). It was better identified on blue-light fundus autofluorescence (FAF) as a well-demarcated hypoautofluorescent lesion (Fig. 1-C). Besides, we noted the presence of multiple hypoautofluorescent spots corresponding to retinal hemorrhages. On fluorescein angiography (FA), the lesion appeared hypofluorescent throughout the angiographic sequence (Fig. 1D). Moreover, FA revealed severe non proliferative diabetic retinopathy (NPDR) signs with peripheral retinal ischemia in both eyes.
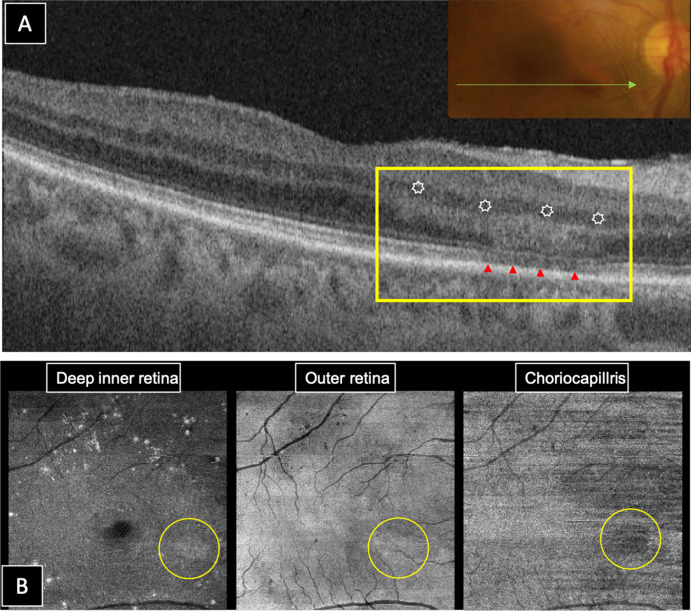
Structural swept source (SS) optical coherence tomography (OCT) showed a large well-limited hyper-reflective band involving the outer nuclear layer (ONL) and the outer plexiform layer (OPL), associated to a fragmented ellipsoid zone (EZ) underneath the lesion, consistent with a long-standing AMOR (Fig. 2 A). On en face SS-OCT, the lesion appeared slightly hyper-reflective at the level of the deep inner retina and outer retina, and hyporeflective at the level of the choriocapillaris layer (Fig. 2B).
Figure 2.
Structural SS-OCT of AMOR lesion in the RE. B-Scan OCT passing through the lesion (A) showing a large well-limited hyper-reflective band involving the ONL and the OPL (white stars) associated to a fragmented EZ (red arrowheads). En face OCT (6 × 6 mm) (B) showing a slightly hyper-reflective lesion at the level of the deep inner retina and outer retina, and hyporeflective lesion at the level of the choriocapillaris layer (yellow circles).
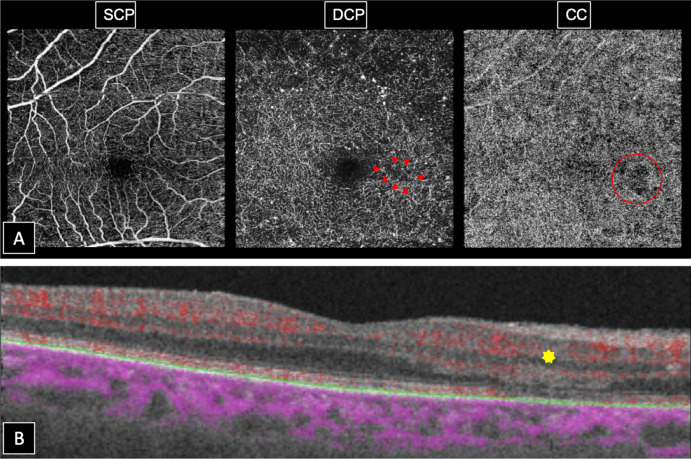
En face OCT angiography (OCT-A) did not show any vascular density anomaly in the superficial capillary plexus (SCP). However, it showed an asymmetry in vascular density between the temporal and nasal areas within the deep capillary plexus (DCP), with an area of reduced capillary flow adjacent to the lesion territory. Moreover, we noted the presence of a well-limited area of choriocapillaris (CC) flow deficit corresponding to the area of fragmented EZ on SS-OCT (Fig. 3 A). Cross sectional OCT-A findings were interesting as the flow deficit within the DCP was more detectable with a markedly reduced flow overlay within the hyperreflective lesion (Fig. 3B).
Figure 3.
OCT-Angiography of AMOR lesion in the RE. En face OCT-A (6 × 6 mm) (A) showing a normal vascular density in the SCP, a reduced capillary flow adjacent to the lesion territory in the DCP (red arrowheads) and a well-limited area of flow deficit in the CC (red circle). Cross-sectional OCT-A revealing a markedly reduced flow overlay within the hyperreflective lesion (yellow star).
Anamnesis revealed that the patient had a history of COVID-19 with nasopharyngeal swab confirmed SARS-CoV-2 infection 3 months ago. She also reported perceiving an abrupt onset relative paracentral scotoma in her RE, one month following the infection. The scotoma resolved progressively over 2 months, according to the patient. We did not complete with visual field test in presence of this typical AMOR lesion. Besides, the results would had been barely interpretable in presence of severe NPDR.
The pathophysiology of AMOR remains unclear but in the era of OCT-A we have valuable data supporting the retinal vascular origin of this rare condition. Some authors suggested DCP ischemia [3] at the origin of the lesion, while others identified flow deficits at the level of the CC [4]. It is most likely that both DCP and CC are incriminated in the disease pathogenesis. Moreover, cross-sectional OCT-A has shown very useful highlighting areas of flow deficit or reduction within different retinal layers and choriocapillaris, as observed in our case [5].
AMOR has been previously linked to viral infections [2]. Besides, since the beginning of COVID-19 epidemic, we observed an increasing number of papers reporting presumed and confirmed ocular manifestations of COVID-19 [6]. Indeed, ocular involvement by COVID-19 is no longer refutable and the association of both types of AMN and SARS-CoV-2 infection have been reported in few isolated cases [7], [8], [9]. AMOR might be more frequently associated to COVID-19 than expected, however subjective ocular signs as relative paracentral scotomas might go unnoticed in presence of severe systemic manifestations of COVID-19.
Our patient developed ocular symptoms one month following confirmed SARS-CoV-2 infection and diagnosis of AMOR was incidentally made upon a systematic multimodal assessment of a diabetic patient. In our case, AMOR has been presumed as probable manifestation of COVID-19.
A larger series of systematic multimodal retinal imaging of patients following COVID-19 is necessary to determine if there is a true association indeed.
Disclosure of interest
The authors declare that there is no competing interest.
Funding
The authors declare not to have received any grant support or research funding for this article.
Ethical approval
This work was approved by the local ethics committee of “Institut Hedi Rais d’ophtalmologie de Tunis”.
Patient consent
Patient has consented for the submission and the publication of this case report.
References
- 1.Bos P.J., Deutman A.F. Acute macular neuroretinopathy. Am J Ophthalmol. 1975;80:573–584. doi: 10.1016/0002-9394(75)90387-6. [DOI] [PubMed] [Google Scholar]
- 2.Munk M.R., Beck M., Kolb S., Larsen M., Hamann S., Valmaggia C., et al. Quantification of retinal layer thickness changes in acute macular neuroretinopathy. Br J Ophthalmol. 2017;101:160–165. doi: 10.1136/bjophthalmol-2016-308367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhavsar K.V., Lin S., Rahimy E., Joseph A., Freund K.B., Sarraf D., et al. Acute macular neuroretinopathy: a comprehensive review of the literature. Surv Ophthalmol. 2016;61:538–565. doi: 10.1016/j.survophthal.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Thanos A., Faia L.J., Yonekawa Y., Randhawa S. Optical coherence tomographic angiography in acute macular neuroretinopathy. JAMA Ophthalmol. 2016;134:1310. doi: 10.1001/jamaophthalmol.2016.3513. [DOI] [PubMed] [Google Scholar]
- 5.Chu S., Nesper P.L., Soetikno B.T., Bakri S.J., Fawzi A.A. Projection-resolved OCT angiography of microvascular changes in paracentral acute middle maculopathy and acute macular neuroretinopathy. Investig Opthalmology Vis Sci. 2018;59:2913. doi: 10.1167/iovs.18-24112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nasiri N., Sharifi H., Bazrafshan A., Noori A., Karamouzian M., Sharifi A. Ocular manifestations of COVID-19: a systematic review and meta-analysis. J Ophthalmic Vis Res. 2021;16:103–112. doi: 10.18502/jovr.v16i1.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Komro J, Bogaard JD, Warren CC. Acute macular neuroretinopathy as a manifestation of covid-19. Ophthalmol Case Reports n.d.;5. 10.35841/OPHTHALMOLOGY.4.3.1-1.
- 8.Gascon P., Briantais A., Bertrand E., Ramtohul P., Comet A., Beylerian M., et al. Covid-19-associated retinopathy: a case report. Ocul Immunol Inflamm. 2020;28:1293–1297. doi: 10.1080/09273948.2020.1825751. [DOI] [PubMed] [Google Scholar]
- 9.Virgo J., Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye. 2020;34:2352–2353. doi: 10.1038/s41433-020-1069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]