Abstract
A 43-year-old man with a history of double sleeve right upper lobectomy for pulmonary sarcoma, presented with worsening haemoptysis. Bronchoscopic and positron emission tomography (PET)CT appearances were suspicious for disease recurrence; however, on attending for CT-guided biopsy, he was found to have a large pseudoaneurysm of his right pulmonary artery. The patient underwent placement of endovascular covered stent with fluoroscopic confirmation of pseudoaneurysm occlusion, and was discharged home on lifelong antiplatelet therapy. To our knowledge, this is the first reported case of pulmonary artery pseudoaneurysm following double (bronchovascular) sleeve resection of the lung, successfully treated by endovascular stenting.
Keywords: interventional cardiology, interventional cardiology, cardiothoracic surgery
Background
Pulmonary artery pseudoaneurysm (PAP) is an extremely rare, life-threatening complication following lung resection. We report the first known case of PAP following double (bronchovascular) sleeve resection of the lung, treated with endovascular covered stenting.
Case presentation
A 43-year-old man with a history of resected pulmonary sarcoma presented to hospital with a large episode of haemoptysis. He had undergone double sleeve right upper lobectomy with pericardial reconstruction, neoadjuvant chemotherapy and postoperative radiotherapy for pulmonary haemangiosarcoma 7 years preceding. This had been followed up with radiofrequency ablation for recurrent nodules several years later; the patient was subsequently troubled with pulmonary hypertension, chronic right-sided heart failure and required bioprosthetic tricuspid valve repair post treatment.
On this occasion, he was admitted suffering from a large pulmonary bleed, requiring intubation, ventilation and radiological guided embolisation of a bronchial artery. The bleeding resolved; however, appearances at subsequent bronchoscopy were noted to be suspicious for recurrence of sarcoma. Thus, a PET scan was arranged following discharge from hospital.
Investigations
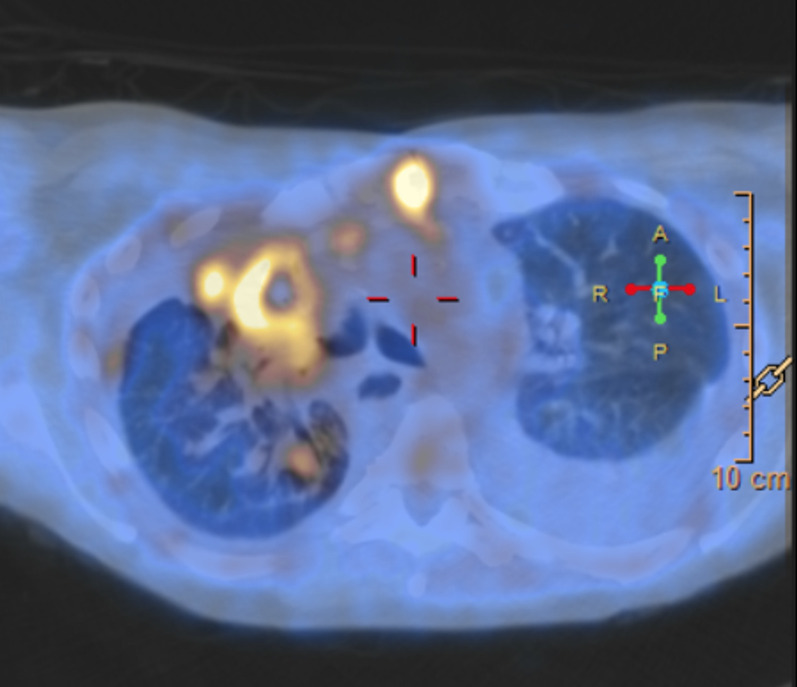
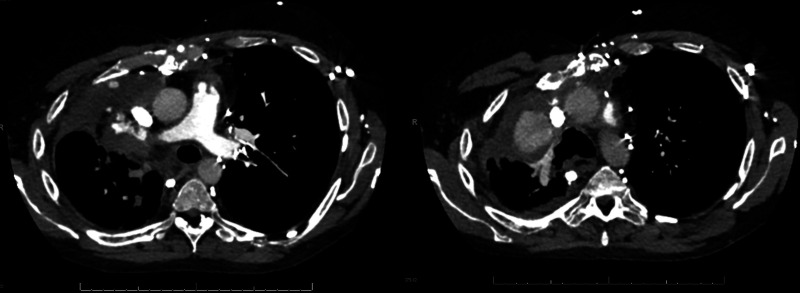
PET scanning showed an intensely FDG avid area of soft tissue containing calcification and cavities in the region of the right upper lobe, which was again suspicious for recurrence (figure 1). The patient was admitted for CT-guided lung biopsy of this region; however, the procedure was aborted on the discovery of a large right PAP (figure 2). Cardiac gated CT scan confirmed the presence of the pseudoaneurysm (figure 3), with apparent filling from the origin of the right lower lobe pulmonary artery, and significant perfusion difference between the remaining right lung and the left lung noted.
Figure 1.
PET CT scanning showing high uptake in region of right upper lobe.
Figure 2.

CT pulmonary angiogram showing large pseudoaneurysm of right pulmonary artery.
Figure 3.
Cardiac gated CT confirming presence of pseudoaneurysm.
Treatment
The patient was discussed at regional cardiac multidisciplinary meeting, and decision was made to proceed with endovascular management of the defect. Under general anaesthesia and with US-guided right femoral access, a 12 mm × 59 mm BeGraft aortic stent graft system (Bentley InnoMed, Hechingen, Germany) was placed in the right interlobar pulmonary artery overlying the pseudoaneurysm (figure 4). The procedure was successful, with fluoroscopic confirmation of occlusion of the pseudoaneurysm.
Figure 4.
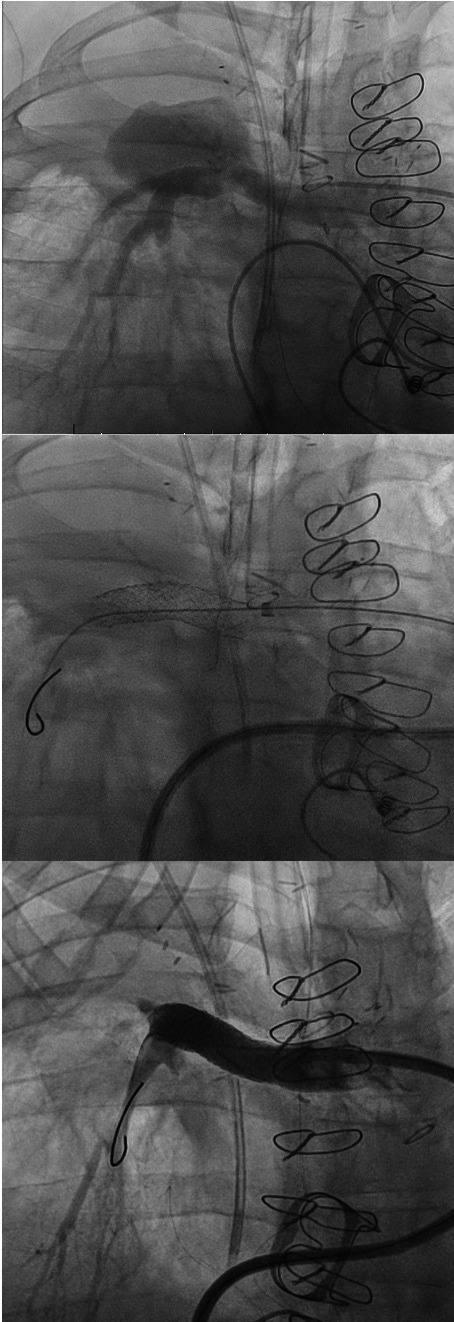
Fluoroscopic images of endovascular stent insertion.
Outcome and follow-up
The patient recovered well, was discharged home on day one postprocedure having been commenced on life-long antiplatelet therapy.
Discussion
Double sleeve (bronchovascular) lobectomy is a surgical option for centrally located tumours involving both bronchus and pulmonary artery.1 The technique involves resection of the tumour and surrounding tissue, with reanastomsis of both the bronchus and pulmonary arterial vasculature, and better results reported in terms of morbidity and mortality than for pneumonectomy.1 2 It is a relatively rare approach, with pulmonary artery reconstruction noted in less than 2% of lobectomies among units that practice conservative resection techniques.2
PAP is a rare entity in itself,3–7 with little over a hundred cases reported on PubMed.8 They are most commonly the result of infective, iatrogenic or traumatic aetiology,9 and can be associated with increases in pulmonary artery pressures.3 4 10 However, only seven cases have been reported following pulmonary resection3–5 9 11–13; one of which had involved pulmonary artery vascular reconstruction.8 Four of these necessitated surgical management, one was treated with coil embolisation,11 one with intra-aneurysmal N-butyl 2-cyanoacrylate injection3 and one with endovascular stent graft placement.13 PAP is important to recognise because of significant associated morbidity,5 7 including the potential for rupture causing life-threatening haemoptysis and suffocation, as well as distal embolization and thrombosis.5–7 9 11 14 Prompt diagnosis and treatment are vital as a result.3
Pseudoaneurysms result from a defect in arterial architecture, but unlike true aneurysms do not involve all three structural layers of the arterial wall—with blood collecting between the tunica media and tunica adventitia. This is an important distinction; pseudoaneurysms are consequently associated with a more fragile aneurysmal wall and higher risk of rupture.6 8 The gold standard for diagnosis of PAP is CT pulmonary angiography, which may also assist in determining the suitability of endovascular strategies of repair.5 7 10
PAP has been reported in patients with a broad range of aetiologies. These include infection (ie, aspergillosis, tuberculosis), systemic vasculitis (ie, Behçet’s syndrome), neoplasia, trauma and iatrogenic origin—most often after balloon inflation following Swan-Ganz catheter insertion.3 5 6 8 10 12 Proximally sited PAPs are often associated with pulmonary artery hypertension,15 which can be a sequelae of major lung resection due vascular remodelling secondary to the total cardiac output flowing through a smaller pulmonary vascular bed.16 17 PAPs are also known to occur as a result of pulmonary vascular manipulation at the time of surgical intervention.9
The aetiology of pseudoaneurysm in our case was thus likely related to previous surgical reconstruction of the pulmonary artery in the affected area, combined with his pulmonary hypertension post lung resection.
Treatment of PAP depends on size and anatomical location,18 with either surgical (via aneurysmectomy and/or lobectomy) or endovascular (radiological guided coil embolisation or stenting) strategies advocated.6 The latter is associated with lower morbidity and mortality than surgery, and embolisation is thus the first-line intervention.3 5 7 10 18 It can, however, pose a risk of iatrogenic rupture, or recurrence due to movement of the embolic material. Embolisation may also be unsuitable for large wide-necked aneurysms19 or at sites of previous surgical repair. Open surgery has been supported for cases involving pyogenic lung parenchyma,4 6 9 however given the long period since surgical resection and extent of anticipated adhesions, accompanied with existing pulmonary hypertension, meant this was an unsuitable option for our case. Covered stent grafts have been used with good effect in paediatric cases of PAP, and are felt to increase overall pulmonary artery diameter, thus reducing pressure gradients and decreasing right ventricular pressures.20 Hence, this was the management strategy employed for our patient, with promising immediate postprocedural outcome.
Learning points.
Pulmonary artery pseudoaneurysm (PAP) is a rare complication following pulmonary resection and pulmonary arterial reconstruction.
Pulmonary hypertension may contribute to development of PAP.
Management includes surgical and endovascular strategies, with embolisation currently recommended first line.
Endovascular stenting is a suitable option for large, wide-necked PAPs.
Footnotes
Contributors: Both authors contributed equally to this submission. PM conceived of the idea for the case report, and supervised the writing of the body of the text. JD researched and wrote the submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Maurizi G, D'Andrilli A, Venuta F, et al. Bronchial and arterial sleeve resection for centrally-located lung cancers. J Thorac Dis 2016;8:S872–81. 10.21037/jtd.2016.06.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vannucci J, Matricardi A, Potenza R, et al. Lobectomy with angioplasty: which is the best technique for pulmonary artery reconstruction? J Thorac Dis 2018;10:S1892–8. 10.21037/jtd.2018.05.174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg A, Chandrasekaran K, Jadhav S, et al. Intra-aneurysmal glue embolisation of a giant pulmonary artery pseudoaneurysm after left upper lobe lobectomy: case report. Korean J Radiol 2013;14:455–9. 10.3348/kjr.2013.14.3.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaaban H, Sharma H, Rao J, et al. A pulmonary artery false aneurysm after right middle lobectomy: a case report. J Med Case Rep 2007;1:70. 10.1186/1752-1947-1-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanayama M, Ichiki Y, Tanaka F. Right completion pneumonectomy for impending rupture of a pulmonary artery pseudoaneurysm. Gen Thorac Cardiovasc Surg 2019;67:558–60. 10.1007/s11748-018-0977-z [DOI] [PubMed] [Google Scholar]
- 6.Koneru H, Biswas Roy S, Islam M, et al. Pulmonary artery pseudoaneurysm: a rare cause of fatal massive hemoptysis. Case Rep Pulmonol 2018;2018:1–4. 10.1155/2018/8251967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y, Gilman MD, Humphrey KL, et al. Pulmonary artery Pseudoaneurysms: clinical features and CT findings. AJR Am J Roentgenol 2017;208:84–91. 10.2214/AJR.16.16312 [DOI] [PubMed] [Google Scholar]
- 8.Gupta M, Agrawal A, Iakovou A, et al. Pulmonary artery aneurysm: a review. Pulm Circ 2020;10:2045894020908780. 10.1177/2045894020908780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bao M, Zhou Y, Jiang G, et al. Pulmonary artery pseudoaneurysm after a left upper sleeve lobectomy. World J Surg Oncol 2013;11:272. 10.1186/1477-7819-11-272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park HS, Chamarthy MR, Lamus D, et al. Pulmonary artery aneurysms: diagnosis & endovascular therapy. Cardiovasc Diagn Ther 2018;8:350–61. 10.21037/cdt.2018.04.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsumura Y, Shiono S, Saito K, et al. Pulmonary artery pseudoaneurysm after lung resection successfully treated by coil embolization. Interact Cardiovasc Thorac Surg 2010;11:364–5. 10.1510/icvts.2010.236661 [DOI] [PubMed] [Google Scholar]
- 12.Amore D, Bocchini G, Casazza D, et al. Left pulmonary artery pseudoaneurysm secondary to post-operative lung abscess. Respirol Case Rep 2020;8:e00598. 10.1002/rcr2.598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klobuka AJ, Short RF. Endovascular stent graft placement in the left main pulmonary artery for management of a giant pulmonary artery pseudoaneurysm. J Vasc Interv Radiol 2016;27:1706–7. 10.1016/j.jvir.2016.06.025 [DOI] [PubMed] [Google Scholar]
- 14.Keymel S, Merx MW, Zeus T, et al. Stenting as a rescue treatment of a pulmonary artery false aneurysm caused by Swan-Ganz catheterization. Case Rep Pulmonol 2014;2014:1–4. 10.1155/2014/893647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guillaume B, Vendrell A, Stefanovic X, et al. Acquired pulmonary artery pseudoaneurysms: a pictorial review. Br J Radiol 2017;90:20160783. 10.1259/bjr.20160783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rol N, Happé C, Beliën JAM, et al. Vascular remodelling in the pulmonary circulation after major lung resection. Eur Respir J 2017;50:1700806. 10.1183/13993003.00806-2017 [DOI] [PubMed] [Google Scholar]
- 17.Potaris K, Athanasiou A, Konstantinou M, et al. Pulmonary hypertension after pneumonectomy for lung cancer. Asian Cardiovasc Thorac Ann 2014;22:1072–9. 10.1177/0218492314527992 [DOI] [PubMed] [Google Scholar]
- 18.Huet N, Rodiere M, Badet M, et al. Covered stent and coils embolization of a pulmonary artery pseudoaneurysm after gunshot wound. Cardiovasc Intervent Radiol 2016;39:778–81. 10.1007/s00270-015-1257-2 [DOI] [PubMed] [Google Scholar]
- 19.Park A, Cwikiel W. Endovascular treatment of a pulmonary artery pseudoaneurysm with a stent graft: report of two cases. Acta Radiol 2007;48:45–7. 10.1080/02841850601045104 [DOI] [PubMed] [Google Scholar]
- 20.Dallaudière B, Hummel V, Pierre Laissy J. The use of covered stents for treatment of pulmonary artery pseudoaneurysms. J Vasc Interv Radiol 2013;24:296–8. 10.1016/j.jvir.2012.10.024 [DOI] [PubMed] [Google Scholar]