Abstract
Synovial sarcoma is a soft tissue sarcoma. Its occurrence as a primary mediastinal neoplasm is very rare. We report a case of mediastinal synovial sarcoma in a 14‐year‐old girl with exertive dyspnoea at presentation. On physical examination, there was a superior vena cava syndrome and café‐au‐lait spots. Chest X‐ray revealed a white left hemithorax with mediastinal deviation to the opposite side. Thoraco‐abdomino‐pelvic scanner showed a voluminous posterior cervico‐mediastinal tissue mass. Computed tomography (CT)‐guided biopsy of the mediastino‐pleural mass was performed. Histological examination reported fusocellular malignant mesenchymal proliferation. A complementary immunohistological study with a broad range of antibodies was performed with a high‐grade single‐phase spindle cell synovial sarcoma of the mediastinum. She presented a respiratory distress, did not respond to resuscitation, and died. Mediastinal synovial sarcoma is a rare tumour that is difficult to diagnose. Its slow progression and delay in diagnosis may lead to a fatal evolution.
Keywords: Immunochemistry, mediastinum, prognosis, synovial sarcoma
Synovial sarcoma is a soft tissue sarcoma. Its occurrence as a primary mediastinal neoplasm is very rare. We report a fatal case of mediastinal synovial sarcoma in a 14‐year‐old girl with exertive dyspnoea at presentation. We highlight the role of imaging, the means of diagnosis, and the importance of the speed of therapeutic management. Mediastinal synovial sarcoma is a rare tumour that is difficult to diagnose. Its slow progression and delay in diagnosis may lead to a fatal evolution.
Introduction
Synovial sarcoma is a rare malignant tumour of young male adults, encountered in more than 85% of cases around the extremities [1]. Thoracic localization is rare and mediastinal localization is exceptional [1]. Primary mediastinal synovial sarcomas are tumours with low incidence, no specific clinical manifestations, and lack of unified and effective treatments [2]. We report a case of synovial sarcoma in a young girl admitted to our thoracic surgery department with emphasis on imaging, the means of diagnosis, and the importance of the speed of therapeutic management.
Case Report
A 14‐year‐old girl with no significant pathological history presented an exertive dyspnoea for four months, neglected by the patient initially. Then, she consulted a doctor of free practice.
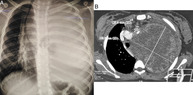
A physical examination revealed a superior vena cava syndrome; pilgrim oedema involving the neck, face, and top of the thorax, with filling of the supraclavicular hollows; and café‐au lait‐spots on the trunk and lower limbs, without other palpable masses or nodes. Chest X‐ray demonstrated a white left hemithorax with mediastinal deviation. Thoraco‐abdomino‐pelvic scanner showed a heterogeneous mediastinal tissue mass measuring 120 × 109 × 142 mm with cervical extension. The mass was pushing the heart, vascular axes, and trachea to the right. A scalloping on the anterior wall of vertebrae D3, D4, and D5 was observed. It resulted in low abundance of left pleural effusion with atelectasis of the lower left lobe and the lingual (Fig. 1). Tumour markers, alpha‐foetoprotein and beta‐human chorionic gonadotropin (HCG), were negative. A computed tomography (CT)‐guided biopsy of the mass was performed. Histological examination of the various samples reported fusocellular malignant mesenchymal proliferation. A complementary immunohistological study with a broad range of antibodies was performed with a high‐grade (grade 3 FNCLCC : grading proposed by the. National Federation of Centers for the Fight Against the Cancer) single‐phase spindle cell synovial sarcoma of the mediastinum (Fig. 2). Because of the aggravation of her dyspnoea, the patient was referred in emergency to our thoracic surgery department. She had an ambient air saturation of 86%. Arterial blood gas assessed respiratory acidosis, hypercapnia, partial pressure of carbon dioxide = 65%, pH = 7.01, and bicarbonates (HCO3 −) of 45 mmol/L. She initially received oxygen through a high‐concentration oxygen mask. The case was discussed in multidisciplinary consultation meeting. The appropriate treatment was challenging. A decompressive radiotherapy was planned. Unfortunately, the patient presented a respiratory distress. She was hospitalized in our reanimation unit. Her respiratory and neurological conditions quickly deteriorated requiring intubation. The patient did not respond to resuscitation and died.
Figure 1.
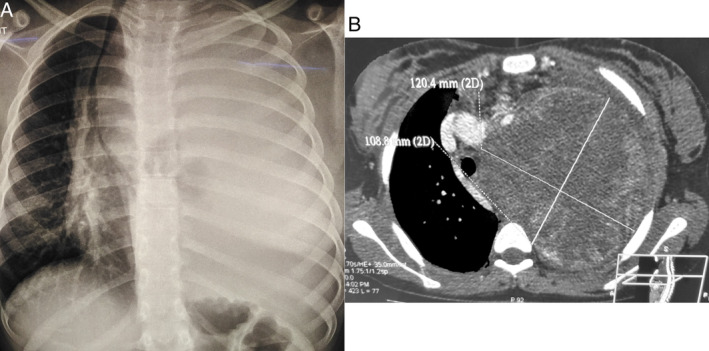
(A) Chest X‐ray. White left hemithorax with mediastinal deviation to the opposite side. (B) Thoraco‐abdomino‐pelvic scanner. Heterogeneous mediastinal tissue mass measuring 120 × 109 × 142 mm with cervical extension. It pushes the heart, vascular axes, and the trachea to the right. There is a scalloping on the anterior wall of vertebrae D3, D4, and D5.
Figure 2.
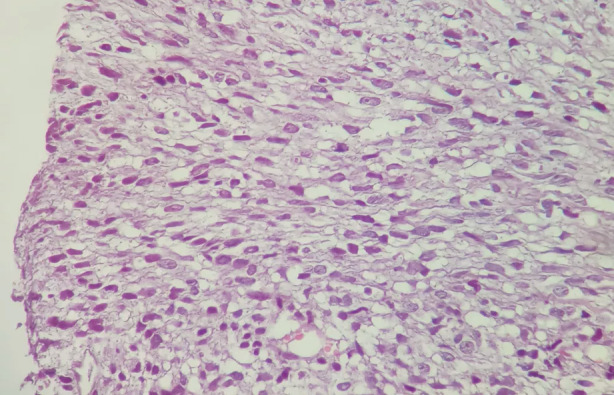
Immunohistological features of the biopsy. Photomicrograph showing a densely involved fusocellular and malignant spindle cell in mesenchymal proliferation. The tumour cells were stained with TLE1, ELI1, and Ki67 (proliferation index >75%) with focal positivity of pancytokeratin and CD99 and were negative for CD34, AML, and myogenin. They were also negative for S100.
Discussion
Synovial sarcoma is a mesenchymal tissue tumour with epithelial differentiation, which occurs most frequently in extremities and is widespread among adolescents and young adults aged 15–40 years [2].
Primary synovial sarcoma is a malignant tumour with no specific differences from other mediastinal tumours in terms of clinical and imaging features, so it is difficult to diagnose. It may have common symptoms such as shortness of breath, cough, chest pain, or haemoptysis. However, most patients remain asymptomatic for a long time with a slow growing mass, in a way similar to our case [3].
Chest radiograph showed a uniform, well‐circumscribed, rounded or lobulated borders lesion [3]. CT may demonstrate a heterogeneous soft tissue mass. This tumour typically grows in centrifugal fashion and can also compress the surrounding structures [3]. In our patient, the tumour was voluminous, measuring 14 cm in the long axis (>5 cm) and compressing the neighbouring organs. The tumour was very large, extended to the posterior mediastinum and to the cervical area which is unusual. Lymphadenopathies are rare [3]. Magnetic resonance imaging (MRI) shows better tumour heterogeneity related to tumour, haemorrhagic, and necrotic intralesional quotas. The triple sign associated in the T2 sequence: a fluid or haemorrhagic hypersignal, a tissue intermediate signal, and a calcium or fibrous hyposignal, is found in peripheric locations [3].
Positron emission tomography can be of value in the pre‐treatment assessment to detect concomitant lesions, assess the primary nature of the tumour, and evaluate response to neoadjuvant chemotherapy, and can detect local recurrence particularly in lesions indeterminable on radiologic tomography [4, 5].
Differential diagnosis of these tumours, when arising in the mediastinum, is challenging because a wide range of spindle cell neoplasms can present as a primary tumour in the mediastinum [3]. Distinguishing the monophasic spindle cell variant of synovial sarcoma from other spindle cell neoplasms is more commonly encountered at the mediastinum. In our case, the diagnosis was made based on a complementary immunohistological study through a broad panel of antibodies. The tumour cells stained with TLE1, ELI1, and Ki67 with focal positivity of pancytokeratin and CD99 and did not stain with CD34, acute myeloblastic leukemia marquer (AML) nor myogenin. They were also negative for S100. We can exclude two entities that can resemble monophasic synovial sarcoma in this location, solitary fibrous tumour (CD34 positive) and malignant peripheral nerve sheath tumour (S100 positive). It was indicated that vimentin, cytokeratin, and membrane epithelial antigen (EMA) positivity, combined with CD34 negativity, are the most useful protein biomarkers for the diagnosis of monophasic synovial sarcoma [2].
Surgery remains the cornerstone of synovial sarcoma treatment. Its purpose is to resect the tumour with adequate margins and the minimal long‐term sequelae. Chemotherapy or radiotherapy should be performed to reduce the tumour mass and make it more accessible for subsequent surgery [5].
In conclusion, mediastinal synovial sarcoma is a rare tumour with a prognosis related to the feasibility of surgical resection, the size, and the extent of local invasion. Diagnosing these tumours may be difficult because their slow progression may sometimes lead to a fatal evolution.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Author Contribution Statement
Asma Saad and Bechir Ben Radhia: Acquisition, interpretation and writing data. Imen Bouacida, Hazem Zribi, Amira Dridi, and Adel Marghli: Drafting and revising the article. All authors read and approved the final manuscript.
Saad, A , Bouacida, I , Ben Radhia, B , Zribi, H , Dridi, A , Marghli, A . (2021) Primary synovial sarcoma of the mediastinum: a poor prognosis in a 14‐year‐old girl. Respirology Case Reports, 9(8), e00811. 10.1002/rcr2.811
Associate Editor: James Ho
References
- 1. Pal M, Ghosh B, Roy C, et al. 2010. Posterior mediastinal biphasic synovial sarcoma in a 12 year old boy: a case report and review of literature. J. Cancer Res. Ther. 6(4):564–566. [DOI] [PubMed] [Google Scholar]
- 2. Zhou Y, Dong W, Zou F, et al. 2014. Primary giant mediastinal synovial sarcoma of the neck: a case report and review of the literature. Oncol. Lett. 7(1):140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Henninger B, Freund M, Zelger B, et al. 2009. Primary mediastinal synovial sarcoma: a case report and review of the literature. Cases J. 2(1):6948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schwarzbach MHM, Dimitrakopoulou‐Strauss A, Willeke F, et al. 2000. Clinical value of [18‐F] fluorodeoxyglucose positron emission tomography imaging in soft tissue sarcomas. Ann. Surg. 231(3):380–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jeganathan R, Davis R, Wilson L, et al. 2007. Primary mediastinal synovial sarcoma. Ulster Med. J. 76:109–111. [PMC free article] [PubMed] [Google Scholar]


