Abstract
Objective:
To assess the association of burn size and community participation as measured by the LIBRE Profile.
Summary Background Data:
Burn size is an established clinical predictor of survival following burn injury. It is often a factor in guiding decisions surrounding early medical interventions, however, literature is inconclusive on its relationship to quality of life outcomes.
Methods:
This is a secondary data analysis of a cross-sectional survey of adult burn survivors. Self-reported data were collected between October 2014 and December 2015 from 601 burn survivors aged ≥18 years with ≥5% total body surface area (TBSA) or burns to critical areas. Sociodemographic characteristics were compared between participants with small burns (≤40% TBSA burned) and large burns (>40% TBSA burned). Ordinary least squares regression models examined associations between burn size and LIBRE Profile scale scores with adjustments for gender, current work status, burns to critical areas, and time since burn injury.
Results:
The analytic sample comprised 562 participants with data available for burn size. 42% of respondents had large burns (>40% TBSA burned) and 58% reported smaller burns (TBSA ≤40%). In adjusted regression models, patients with large burns tended to score lower on the Social Activities and Work & Employment scales (p<0.05) and higher on the Family & Friends scale (p<.05). Participants with burns >40% TBSA scored lower for several individual items in the Social Activities scale and one item in the Work & Employment scale (p<0.05).
Conclusions:
Increasing burn size was found to be negatively associated with selected items of Work & Employment, and Social Activities, but positively associated with aspects of Family & Friend Relationships. Future longitudinal studies are necessary to assess and understand the long-term social impact of burn injuries on adult populations.
Keywords: LIBRE, Community Participation, Burn Size, Burns, Burn Injury
Mini-Abstract
The Life Impact Burn Recovery Evaluation-Profile (LIBRE-Profile) was used to assess the association of burn size with long-term outcomes in 562 survivors. Most community participation scales were not associated with worse outcomes related to larger burns. However, Work & Employment, and Social Activities scales had negative associations with size of burn.
Introduction
Burn size is an established clinical predictor of survival and an essential factor in guiding decisions surrounding early medical interventions. However, less is known about its association with long-term outcomes of burn survivors. In severe cases with large burn size, an older patient1, or with crisis standards of care in place2, burn size can predict how and when certain therapies are initiated and affect decisions to initiate life-saving treatment.3–8 Before recent medical advancements, patients with burn injuries covering much of their body surface area were deemed rarely survivable. Due to therapeutic developments in the late 20th century including modern surgical critical care, nutritional care, and the advent of burn centers, the chance of survival after a severe burn has increased substantially.9 The result is a growing population of burn survivors whose long-term medical needs have not been well defined,1,10,11 making evident the need to assess patient reported outcomes focused on function, adjustment, and community participation.13–15 Stakeholders making triage and resuscitation decisions, allocating resources, and advocating for patients need long-term patient-centered data in addition to clinical information on which to base their decisions, identify risk factors for poor outcomes, and guide interventions.
The Life Impact Burn Recovery Evaluation (LIBRE) Profile is a computer-based questionnaire that measures the impact of burn injuries on the social participation of survivors age 18 and above.16,17 This assessment tool was created based on the World Health Organization’s International Classification of Functioning, Disability, and Health Framework18 with input from clinical experts and burn survivors.17 The conceptual framework was operationalized to create a 192-item survey, which was administered to 601 adult burn survivors for calibration and psychometric testing.16 The LIBRE Profile evaluates six scales of community participation, each representing important areas of social participation for this population.16
Although burn size is one of the most common characteristics assessed in the literature examining long-term outcomes19, findings remain inconclusive.19–26 In a prospective longitudinal study, Fauerbach et al.27 found that at six and twelve months post-burn, increasing burn size was associated with more physical impairment but not with psychological distress. Another longitudinal study found that larger burn size was related to lower recovery levels of physical function and some psychosocial domains such as family in young adults followed for three years after their burn.28 However, the authors did not find significant differences in the recovery trajectories of other areas such as romantic functioning. Other studies have found an association between burn size and reduction in physical function, but findings on the relationship between burn size and psychosocial domains remain uncertain.14,20–26 Given this gap in the literature and the importance of burn size in early burn care interventions, the following study aims to evaluate the association of burn size and community integration using the LIBRE Profile.
Methods
Study Design and Participants
This is a secondary analysis of a cross-sectional survey of adult burn survivors. The data were self-reported and collected as part of the field testing of the LIBRE Profile. Community-dwelling burn survivors were recruited between October 2014 and December 2015 through peer support groups, social media, burn clinics, the Phoenix Society for Burn Survivors, and the 2014 and 2015 Phoenix World Burn Congresses. Survivors aged ≥18 years and with injuries to ≥5% total body surface area (TBSA) or burns to critical areas (hands, feet, face, or genitals) were included. Subjects were able to complete the LIBRE Survey without assistance by a proxy. If eligible to complete the survey, participants were asked further questions regarding work and employment, romantic relationships, and sexual relationships to determine which items in the LIBRE Profile questionnaire were applicable to that individual. Demographic variables included age at time of survey, gender, race/ethnicity, education level, and marital status. Clinical variables included TBSA burned, presence of burns to critical areas, and time since burn injury. When a TBSA burned range was reported, the median value for that individual of the range was used for analysis. If a median was not attainable, the participant was assigned the nearest quintile.
Outcome Measures
After successful completion of a screening module, participants were administered the LIBRE-192, which contains 192 items used for field testing of the LIBRE Profile examining several areas of community participation after burn injury.16,17,29 The development of the 126-item LIBRE Profile from the LIBRE-192 has been described previously.16 Participants completed the LIBRE-192 in person, over the phone, or online. Individual items within each scale were on a 5-point Likert scale (1–5), with higher scores coded to denote better outcomes, 5 being the highest score. Specific items were reverse-coded as necessary. The final 126-item LIBRE Profile was previously validated using exploratory and confirmatory factor analyses and with IRT-based graded response models that derived 6 scales examining the following scales of community participation: Family & Friend, Social Interactions, Social Activities, Work & Employment, Romantic Relationships, and Sexual Relationships.16 Scale scores were standardized to a mean of 50 and a standard deviation of 10 based upon the entire sample of burn survivors.
Statistical Analysis
Sociodemographic and clinical characteristics were compared between participants with small (TBSA burned ≤40%) and large burns (TBSA burned >40%) using simple chi-square tests for categorical variables. Multivariable ordinary least squares regression models were run to estimate associations between TBSA burned by quintiles and LIBRE Profile scale scores with adjustments for gender, current work status, burns to critical areas, and time since burn injury. Scores on individual LIBRE Profile items were then compared between participants with burns ≤40% vs. >40% TBSA using t-tests in two ways: first, mean scores on each item were compared between the two groups; second, the percentage of participants scoring 1 or 2 vs. 3 or above on the 1–5 scale was compared for each item. Finally, adjusted multivariate regression models were run to estimate associations between TBSA burned by quintile and individual item scores on all items for which significant differences by burn size were observed using either of the two comparisons described above. A sensitivity analysis was conducted to determine differences between the included and excluded participants. Variance inflation factors were examined to assess collinearity between independent variables, and robustness of the parameter estimates was tested using bootstrap techniques. We assessed whether the point estimates and 95% confidence intervals of the regression coefficients remained stable across 200 bootstrap subsamples.
Ethical Approval
Human Studies Approval from the Boston University Medical Campus Institutional Review Board (Protocol H-32928) was obtained and all human subjects provided informed consent (oral for phone participants, written for self-administered participants) prior to participating in any research study activities.
Results
Of the 601 burn survivors who completed the LIBRE-192 assessment, 483 reported an exact TBSA burned, 76 reported a range from which the median value was used, and 3 reported a range from which a TBSA percentage quintile could be determined (e.g., <10%). This yielded an analytic sample of 562 participants (Figure 1). Included participants were less likely to have burns to critical areas compared to those who did not report TBSA (79.9% vs. 94.9%, p=0.02) but did not differ significantly on any other measured characteristics or mean LIBRE scale scores (data not shown in tables). The majority of included participants were white (79%) followed by African American (8%), Hispanic/Latino (7%), and other races/ethnicities (6%) (Table 1). The mean age of study participants was 44.5 years (standard deviation 16.0 years); slightly more than half of participants were women (55%), and slightly less than half were married (46%). Approximately 40% had a bachelor’s degree or higher (42%), and over one half were currently employed (55%). A large majority reported burns to critical areas (80%). The time since burn injury was greater than 10 years for approximately half of the patients (46.8%) (Table 1).
Figure 1:
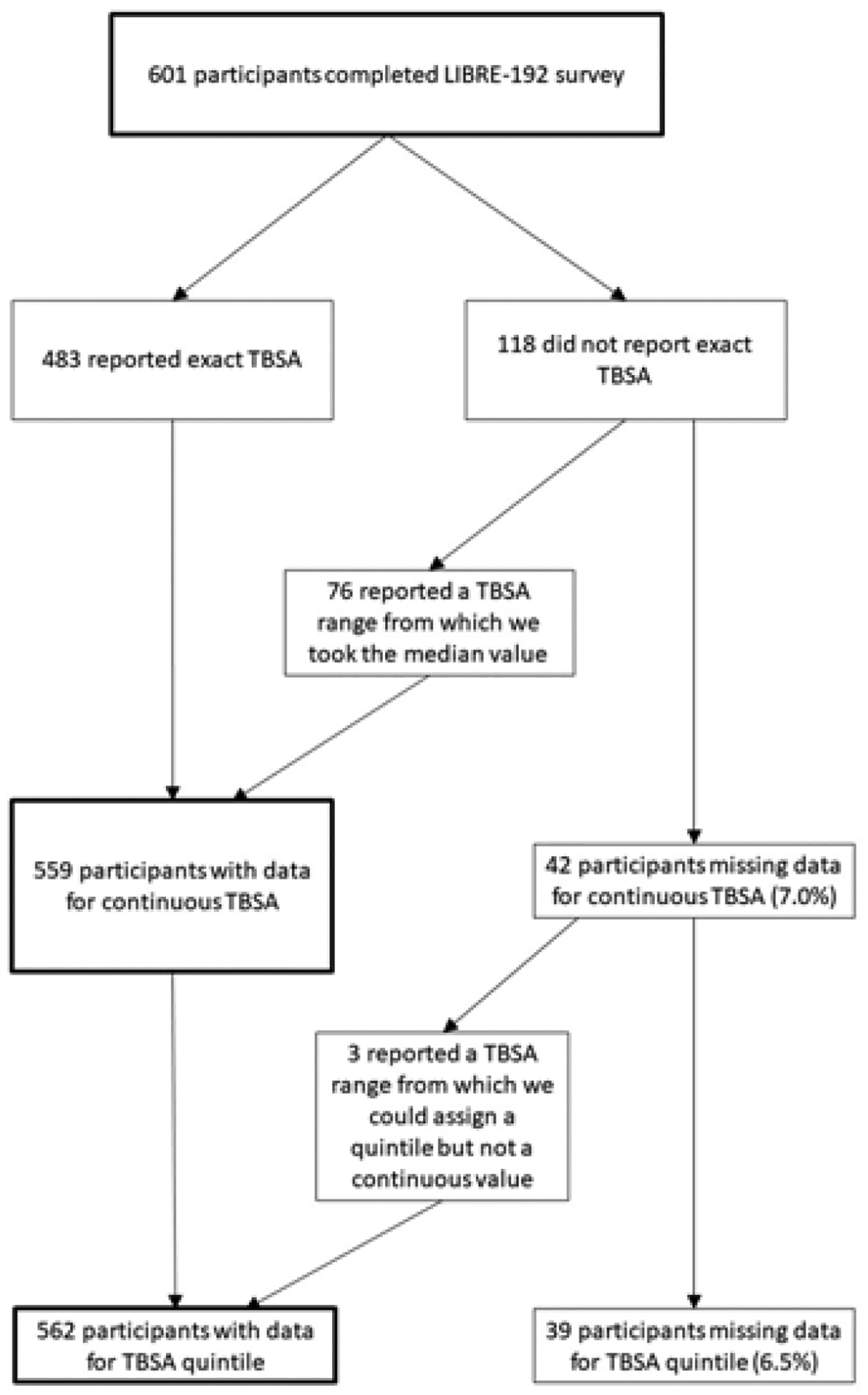
Sample Derivation for Total Body Surface Area (TBSA) Burned
Table 1:
Demographic and clinical characteristics by Total Body Surface Area (TBSA) burned
| Variable | Value | All participants | TBSA Burned ≤40% | TBSA Burned >40% |
|---|---|---|---|---|
| All participants | 562 (100.0) | 328 (100.0) | 234 (100.0) | |
| Age at time of survey | ≤30 | 148 (26.4) | 90 (27.5) | 58 (24.8) |
| 31–50 | 194 (34.6) | 115 (35.2) | 79 (33.8) | |
| 51–65 | 170 (30.3) | 91 (27.8) | 79 (33.8) | |
| >65 | 49 (8.7) | 31 (9.5) | 18 (7.7) | |
| Gender * | Female | 309 (55.1) | 189 (57.6) | 120 (51.5) |
| Male | 252 (44.9) | 139 (42.4) | 113 (48.5) | |
| Race/ethnicity | White non-Hispanic | 442 (79.4) | 267 (82.2) | 175 (75.4) |
| Black or African-American | 46 (8.3) | 24 (7.4) | 22 (9.5) | |
| Hispanic/Latino | 38 (6.8) | 18 (5.5) | 20 (8.6) | |
| Othera | 31 (5.6) | 16 (4.9) | 15 (6.5) | |
| Education level | High school or less | 228 (40.9) | 123 (38.0) | 105 (44.9) |
| Technical/trade training or associate’s degree | 96 (17.2) | 56 (17.3) | 40 (17.1) | |
| Bachelor’s degree | 156 (28.0) | 100 (30.9) | 56 (23.9) | |
| Graduate/professional/advanced degree | 78 (14.0) | 45 (13.9) | 33 (14.1) | |
| Marital status | Married/live with significant other | 257 (46.0) | 142 (43.7) | 115 (49.2) |
| Single/divorced/widowed/separated | 302 (54.0) | 183 (56.3) | 119 (50.9) | |
| Current work status * | Working | 306 (54.8) | 191 (59.0) | 115 (49.2) |
| Not working | 176 (31.5) | 89 (27.5) | 87 (37.2) | |
| Other | 76 (13.6) | 44 (13.6) | 32 (13.7) | |
| In a romantic relationship | Yes | 364 (64.8) | 210 (64.0) | 154 (65.8) |
| No | 198 (35.2) | 118 (36.0) | 80 (34.2) | |
| Sexually active | Yes | 365 (65.0) | 215 (65.6) | 150 (64.1) |
| No | 197 (35.1) | 113 (34.5) | 84 (35.9) | |
| Burns to critical areas * | Yes | 449 (79.9) | 240 (73.2) | 209 (89.3) |
| No | 113 (20.1) | 88 (26.8) | 25 (10.7) | |
| Time since burn injury * | <3 Years | 143 (25.4) | 108 (32.9) | 35 (15.0) |
| 3–10 Years | 156 (27.8) | 98 (29.9) | 58 (24.8) | |
| >10 Years | 263 (46.8) | 122 (37.2) | 141 (60.3) |
Other race/ethnicity includes Asian (N = 6), American Indian or Alaskan Native (4), Native Hawaiian or Pacific Islander (2), Multiracial (16), and other reported race/ethnicity (3).
indicates variables for which mean burn size differed significantly by stratum (p<.05)
In this study, 42% of patients had large burns (>40% TBSA). Of the patients with large burns, 89% had burns to critical areas, compared to 73% of patients with smaller burns (p<0.05; Table 1). Just under half (49%) of patients with large burns were currently working at the time of the survey, whereas 59% of patients with smaller burns were actively employed (p<0.05; Table 1). Approximately two-thirds of patients were sexually active (65% all participants) and in romantic relationships (65%). Education levels were also comparable between participants with large vs. small burns (Table 1).
In adjusted regression models, patients with large burns tended to score lower on the Social Activities and Work & Employment scales and higher on the Family & Friends scale (Table 2). In the comparison of individual item scores, participants with burns >40% TBSA tended to score lower for several items in the Social Activities scale regarding ability to be active or participate in family events (Tables 3 and 4), and for one item in the Work & Employment scale regarding employer satisfaction (Table 4). Participants with large burns tended to score higher for several items from the other four scales (Tables 3 and 4). Differences in individual item scores retained statistical significance in adjusted regression analyses for items in the Family & Friends, Social Activities, and Work & Employment scales, and for two items in the Sexual Relationships scale (“My partner is very sensitive to my needs,” and “I feel comfortable having my burns touched during sex”) (Table 5). All variance inflation factors were below 1.5, suggesting that collinearity was not a problem. The point estimates and 95% confidence intervals from bootstrap inferences assessing the relationship between burn size and outcomes remained stable throughout, supporting the robustness of the coefficients reported (data not shown).
Table 2:
Adjusted regression analyses between Total Body Surface Area (TBSA) burned quintile and LIBRE Profile scale scores
| Scale | N | B | 95% CI | p-value |
|---|---|---|---|---|
| Sexual Relationships | 387 | 0.29 | −0.74, 1.32 | 0.58 |
| Family & Friends | 551 | 0.90 | 0.12, 1.67 | 0.02 |
| Social Interactions | 550 | 0.04 | −0.68, 0.75 | 0.92 |
| Social Activities | 550 | −1.09 | −1.82, −0.37 | 0.01 |
| Work & Employment | 297 | −1.30 | −2.26, −0.34 | 0.01 |
| Romantic Relationships | 359 | 0.41 | −0.54, 1.37 | 0.39 |
Models are adjusted for gender, current work status, burns to critical areas, and time since burn injury. Highlighting indicates scales for which participants with large burns did worse than those with small burns.
Table 3:
Mean score on individual LIBRE Profile items, stratified by burn size, items with significant differences between participants with Total Body Surface Area (TBSA) Burned ≤40% vs. >40%
| Item | TBSA Burned ≤40% | TBSA Burned >40% | p-value |
|---|---|---|---|
| Family & Friends | |||
| Q95 I would rather be alone than with my family | 3.75 | 3.96 | 0.03 |
| Q1017 I have trouble keeping friends | 3.97 | 4.16 | 0.04 |
| Social Interactions | |||
| Q613 I avoid doing things that might call attention to my burns | 3.38 | 3.62 | 0.04 |
| Q621 I don’t worry about other people’s attitudes towards me | 3.43 | 3.68 | 0.02 |
| Social Activities | |||
| Q57 My burns limit me being active | 3.96 | 3.64 | 0.01 |
| Q913 I am limited in what I can do for my family | 3.86 | 3.48 | 0.01 |
| Q1010 I am upset that my burns limit what I can do with friends | 4.11 | 3.83 | 0.01 |
| Q53 I am able to go to all the community events that are important to me | 4.46 | 4.23 | 0.01 |
| Q91 I am able to do all of my regular family activities | 4.29 | 4.09 | 0.02 |
| Romantic Relationships | |||
| Q77 I am afraid to share with my partner what I dislike about myself | 3.41 | 3.70 | 0.03 |
| Q107 I talk openly with friends | 4.08 | 4.17 | 0.01 |
| Q72 How often do you and your partner do things together? | 4.13 | 4.21 | 0.03 |
| Sexual Relationships | |||
| Q734 I do not want sex when my partner does | 3.69 | 3.96 | 0.02 |
| Q816 I am satisfied with the amount of emotional closeness during sexual activity | 3.78 | 4.02 | 0.03 |
| Q817 My partner is very sensitive to my sex needs | 3.58 | 3.96 | 0.01 |
| Q821 I feel comfortable having my burns touched during sex | 3.48 | 3.91 | 0.01 |
Highlighting indicates items for which participants with large burns did worse than those with small burns.
Table 4:
Percentage of participants with low scores (1 or 2 on the 1–5 scale) on individual LIBRE Profile items, stratified by burn size, items with significant differences between participants with Total Body Surface Area (TBSA) burned ≤40% vs. >40%
| Item | TBSA Burned ≤40% | TBSA Burned >40% | p-value |
|---|---|---|---|
| Family & Friends | |||
| Q1017 I have trouble keeping friends | 11.7 | 6.5 | 0.04 |
| Q920 Most family members are comfortable being with me | 7.1 | 3.0 | 0.04 |
| Q1030 My friends have helped me get out of the house | 13.2 | 6.8 | 0.02 |
| Social Interactions | |||
| Q621 I don’t worry about other people’s attitudes towards me | 29.1 | 19.7 | 0.01 |
| Social Activities | |||
| Q913 I am limited in what I can do for my family | 20.7 | 31.5 | 0.01 |
| Romantic Relationships | |||
| Q724 I shy away from being close to my partner | 12.4 | 8.8 | 0.02 |
| Q107 I talk openly with friends | 7.6 | 5.2 | 0.01 |
| Sexual Relationships | |||
| Q816 I am satisfied with the amount of emotional closeness during sexual activity | 16.7 | 7.0 | 0.01 |
| Q821 I feel comfortable having my burns touched during sex | 26.2 | 12.5 | 0.01 |
| Work & Employment | |||
| Q410 My boss feels I can do my work | 2.2 | 3.8 | 0.02 |
Highlighting indicates items for which participants with large burns did worse than those with small burns.
Table 5:
Adjusted regression analyses between Total Body Surface Area (TBSA) burned quintile and individual item scores, items where mean score or percentage of participants with low scores (1 or 2 on the 1–5 scale) differed significantly for those with burns ≤40% vs. >40% TBSA burned Adjusted models include gender, current work status, burns to critical areas, and time since burn injury.
| Item | B | 95% CI | p-value |
|---|---|---|---|
| Family & Friends | |||
| Q95 I would rather be alone than with my family | 0.12 | 0.03, 0.20 | 0.01 |
| Q920 Most family members are comfortable being with me | 0.08 | 0.01, 0.15 | 0.02 |
| Q1017 I have trouble keeping friends | 0.10 | 0.02, 0.18 | 0.01 |
| Q1030 My friends have helped me get out of the house | 0.11 | 0.03, 0.19 | 0.01 |
| Social Interactions | |||
| Q613 I avoid doing things that might call attention to my burns | 0.06 | −0.04, 0.16 | 0.25 |
| Q621 I don’t worry about other people’s attitudes towards me | 0.08 | −0.01, 0.17 | 0.09 |
Highlighting indicates items for which participants with large burns did worse than those with small burns.
Discussion
While prior literature has focused on factors that contribute to survival in patients with large burns, there is a paucity of quantitative data regarding social and community integration in association with burn severity. This study examined the relationship between burn size and social outcomes in 562 burn survivors. Utilizing the LIBRE Profile,16 patients with large burns (defined as TBSA burned >40%) were directly compared to those with small burns (defined as TBSA burned ≤40%). The cross-sectional data showed that patients with large burns experienced worse recovery in specific outcomes within Work & Employment and Social Activities scale, but performed better than those with smaller burns in other scales including Family & Friends and Sexual Relationships. It is well established that burn size has severe implications for physical rehabilitation;27 however, results of the present study suggest that in relation to community integration the effects may be multidirectional. Previous research has shown that individuals with burn injuries are able to make significant progress in recovery, but often do not reach pre-morbid levels.21 In patients with extensive injuries, burn-related health impairments can persist and impact all areas of life.22 For that reason, one publication suggests that burn injury evolves from an acute illness to a chronic condition.30 Furthermore, it is estimated that approximately one-third of burn survivors experience moderate to severe difficulties with social integration.13,15 Burn size has widely been used as a guiding point for clinical interventions, yet a systematic review from 2018 found that only 29% of the identified studies reported a statistically significant inverse relationship between TBSA and health-related quality of life.19 In line with this finding, prior studies have indicated that burn size may be more strongly associated with physical outcomes than with community participation.27,28 In contrast, a recent study conducted by Kishawi et al.,31 using a total score from the Burn Specific Health Scale (BSHS), concluded that burn size was negatively associated with quality of life. However, Amtmann et al.32 studied the psychometric properties of the BSHS and found that a total score does not have a meaningful interpretation. Rather, the BSHS should be analyzed by individual domain scores. Therefore, it is problematic to draw conclusions based on a cumulative score. The present study builds on the literature to date by assessing burn size in relation to the specific domains of the LIBRE Profile.
Patients in the present study with large burns did better in the Family & Friends scale and for several items within the Sexual Relationships scale. Patients with large burns had better outcomes when asked about spending time alone versus with the family, keeping friends, having friends help them get out of the house, and feeling that family members are comfortable in their presence. Returning to a pre-burn social life can be challenging for burn survivors.15 Post-traumatic growth (PTG), resiliency, and coping adaptation skills may contribute to the study findings in which patients with large burns scored better than those with small burns. Post-traumatic growth, or experiencing positive psychological change as a result of trauma,33 has been reported in survivors of large burn injuries.33,34 One study identified a positive association between burn size and PTG.34 Additionally, Martin et al. found that a key component of PTG for burn survivors is personal growth due to the ‘sink or swim’ nature of the challenging rehabilitation process.33 For PTG to occur, the burn must be severe enough to disturb everyday life, which may explain why individuals with large burns scored better on certain scales.34 One study assessing the long-term impact of facial burn injuries on recovery found that in both the group with facial burns and the group without facial burns, differences in psychosocial recovery gradually diminished over time and simultaneously improved.35 Those results speak to the presence and importance of resiliency within the burn survivor community. Although patients with large burns are likely to experience more significant physical impairment, this may explain why patients with large burns scored better on a number of social recovery items in comparison to those with smaller burns.
Within the Sexual Relationships scale, patients with large burns scored better on several items. The results of the present study suggest an association, albeit weak, between burn size and sexual relationships post-burn. The importance of engaging in sexual relationships during recovery has been studied previously36,37 and has been established as an important aspect of community participation and psychological rehabilitation.38 Ohrtman et al. found that concerning sexual activity, the burn survivor population does not differ significantly in comparison to a non-burn adult population.38 These results may be explained by a reported increased closeness and connectedness with their partners post-burn38, in addition to the centrality of relationships in PTG and resiliency.34
This study also identified items in which patients with large burns had worse scores when compared to those with small burns. Within the Work & Employment scale, those with large burns were less likely to be employed and reported concerns about their employer’s confidence in their ability to do their work (p<0.01). Barriers impacting employment after burn injury have been studied previously. The most common barriers are pain,39,40 neurologic problems,41 impaired mobility,41 severity of the burn,28,42 psychiatric issues,41 psychosocial factors,43 and working conditions.39,43 Schneider et al. found that pain was the most frequent barrier to returning to work at all time periods among burn survivors.41 Dyster-Aas et al.40 found that unemployment was associated with poorer outcomes in both psychosocial and physical domains of the Burn Specific Health Scale, including body image and interpersonal relationships. In addition, patients experiencing social stigma44 from employers or colleagues may face additional barriers in returning to work. A systematic review found that only 37% of burn survivors return to work with the same employer without accommodations.45 Because the primary goal of rehabilitation after burn injury is integration into society, employment status is an important surrogate outcome measure of functional recovery. As prior literature has primarily examined barriers to returning to work, the present study fills a gap by providing insight into functioning at work. Findings show that patients with large burns have worse outcomes in the scale of Work & Employment, pointing to the need for dedicated employment counseling and advocacy for this patient population throughout their recovery.
Patients with large burns also reported worse outcomes in the Social Activities scale. These patients felt restricted in what they could do for their families, were limited in attending community events, and reported disappointment because their burns limited activities with friends. These findings are important as social interactions and activities are essential components of social recovery.13–15 Although physical limitations may contribute to lower social participation scores,28 psychological challenges have also been found to interfere with social participation.15 For example, Ryan et al. found that poor perceived appearance was a contributing factor in social functioning among young adult burn survivors.28 For this reason, the identification of specific social barriers should be a priority for clinicians and patients in the rehabilitation process.
As the focus of burn care begins to shift beyond mortality and towards quality of life, considerations for long-term patient recovery must be comprehensively understood. Measurement tools such as the LIBRE Profile have the potential to support both clinicians and patients of all ages during recovery. Individual burn survivor scale scores on the LIBRE Profile are valuable to ensure the patient that they are recovering as expected and provide opportunities for the clinician to offer additional support in specific areas, such as psychiatric care,27 peer support,46 and psychosocial28 interventions to assist patients with the social integration process.
Limitations
There are several limitations to this study. First, while the study reports associations between burn size and perceived gains in integration, causal relationships cannot be asserted. Because many study participants were recruited from the Phoenix Society SOARS program (Survivors Offering Assistance in Recovery)48 and the World Burn Congress,49 the study sample may represent a self-selected group of individuals with attributes contributing to better adjustment and positive social supports, and thus may be subject to selection bias. Second, there is a higher percentage of females in this study sample than in the National Burn Registry11, which may result in limiting the generalizability of results. Third, the participants with significantly large TBSA burn injuries tended to be farther out in time from their injuries. These individuals may thus represent a group that has had a longer time to try different support and coping styles that may improve overall adjustment. However, the study sample does represent a diverse population of burn survivors across all ages, races, and education levels. Fourth, the magnitude of the observed associations was small (less than 1.5 points or 15% of a standard deviation for scale scores, and less than .25 points on a 1–5 scale for individual items). However, while the associations are small yet significant, they do suggest that small differences may be important and require further study. Lastly, the data in this study was collected five years ago. However, the results of this study continue to be clinically relevant as they were when the data was first collected.
Conclusion
This cross-sectional study, utilizing the LIBRE Profile, aimed to characterize the relationship between burn size and social and community participation in a cohort of 562 adult burn patients. Larger burn size was found to be negatively associated with aspects of Work & Employment and Social Activities, but positively associated with items within Family & Friend relationships and sexual relationships. Notably, patients experienced impairment with community participation regardless of burn size. This suggests that the relationship between burn size and psychosocial functioning may be more complex than that for physical functioning. Measuring and understanding the impact of burn injuries on social recovery and outcomes expanding beyond survival has important implications to assist clinicians in making critical medical decisions. Future longitudinal and qualitative studies are needed to assess and understand the social impact of burn injuries on adult populations.
Acknowledgments
The authors of this paper would like to thank all the staff and members of the LIBRE advisory board for their help on this project, including Alan Jette, PhD, Amy Acton, BSN, Austin F. Lee, PhD, Pengsheng Ni, MD, MPH, Linda J. Resnick, PT, PhD, Mary Slavin, PT, PhD, Ronald Tompkins, MD, ScD, Ross D. Zafonte, DO, Kevin Foster, MD, MBA, FACS, Bohdan Pomahač, MD, Indranil Sinha, MD, Nick Faoro, RN, Nicole Gibran, MD, Gretchen Carrougher, RN, Frederick Edorf, MD, Philip H. Chang, MD, John T. Shulz, III, MD, Robert L. Sheridan, MD, Jim Fauerbach, MD, Debra Reilly, MD, FACS, James Hwang, MD, Amy Clark, Pamela Peterson, RN, Nicole Kopari, MD, David Harrington, MD, David Herndon, MD, Philip Fidler, MD, Victor Joe, MD, Karen Badger, PhD, MSW, Lucy Wibbenmeyer, MD, Benjamin Levi, MD, Leopoldo C. Cancio, MD, Karen Kowalske, MD, Radha Halavanahalli, PhD, Lee Faucher, MD, Abraham Houng, MD. In addition, we would like to thank all of the burn survivors who gave us their time and involvement in the study.
Conflicts of Interest and Sources of Funding:
The authors have nothing to disclose. This study was supported by the Shriners Hospitals for Children Grants #72000 and #79145, the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) Grant # 90DPBU0001, H133A130023, and H133A120034, and the Fraser Fund of Massachusetts General Hospital. The sponsors had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Publication History: Preliminary results were presented and received as an abstract award at the American Burn Association Conference in May 2016 in Las Vegas, Nevada.
References
- 1.Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. Published online 1998. doi: 10.1056/NEJM199802053380604 [DOI] [PubMed] [Google Scholar]
- 2.Kearns RD, Bettencourt AP, Hickerson WL, et al. Actionable, Revised (v.3), and Amplified American Burn Association Triage Tables for Mass Casualties: A Civilian Defense Guideline. J Burn Care Res. 2020;41(4). doi: 10.1093/JBCR/IRAA050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hagstrom M, Wirth GA, Evans GRD, Ikeda CJ. A review of emergency department fluid resuscitation of burn patients transferred to a regional, verified burn center. Ann Plast Surg. Published online 2003. doi: 10.1097/01.SAP.0000058494.24203.99 [DOI] [PubMed] [Google Scholar]
- 4.Saffle JR. Practice Guidelines for burn care. J Burn Care Rehabil. 2001;22:S1–69. [Google Scholar]
- 5.Monafo WW. Initial management of burns. N Engl J Med. Published online 1996. doi: 10.1056/NEJM199611213352108 [DOI] [PubMed] [Google Scholar]
- 6.Ramzy PI, Barret JP, Herndon DN. Thermal injury. Crit Care Clin. Published online 1999. doi: 10.1016/S0749-0704(05)70058-0 [DOI] [PubMed] [Google Scholar]
- 7.Wasiak J, Cleland H, Jeffery R. Early versus delayed enteral nutrition support for burn injuries. In: Cochrane Database of Systematic Reviews.; 2006. doi: 10.1002/14651858.cd005489.pub2 [DOI] [PubMed] [Google Scholar]
- 8.Kazis L, Marino M, Ni P, et al. Development of the LIBRE Profile: Assessing the Social Impact of Burns. Arch Phys Med Rehabil. Published online 2016. doi: 10.1016/j.apmr.2016.08.267 [DOI] [Google Scholar]
- 9.Tompkins RG. Survival from burns in the new millennium 70 years’ experience from a single institution. Ann Surg. Published online 2015. doi: 10.1097/SLA.0000000000000623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saffle Md JR, Davis Phd B, Williams Rn P. Recent outcomes in the treatment of burn injury in the united states: A report from the american burn association patient registry. J Burn Care Rehabil. Published online 1995. doi: 10.1097/00004630-199505000-00002 [DOI] [PubMed] [Google Scholar]
- 11.Miller SF, Bessey PQ, Schurr MJ, et al. National Burn Repository 2005: A ten-year review. J Burn Care Res. Published online 2006. doi: 10.1097/01.BCR.0000226260.17523.22 [DOI] [PubMed] [Google Scholar]
- 12.Bartley CN, Atwell K, Cairns B, Charles A. Predictors of withdrawal of life support after burn injury. Burns. Published online 2019. doi: 10.1016/j.burns.2018.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blakeney PE, Rosenberg L, Rosenberg M, Faber AW. Psychosocial care of persons with severe burns. Burns. Published online 2008. doi: 10.1016/j.burns.2007.08.008 [DOI] [PubMed] [Google Scholar]
- 14.Spronk I, Legemate C, Oen I, van Loey N, Polinder S, van Baar M. Health related quality of life in adults after burn injuries: A systematic review. PLoS One. Published online 2018. doi: 10.1371/journal.pone.0197507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emily AO, Gabriel DS, Laura CS, et al. Social Interactions and Social Activities After Burn Injury: A Life Impact Burn Recovery Evaluation (LIBRE) Study. J Burn Care Res. 2018;39(6). doi: 10.1093/JBCR/IRY038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kazis LE, Marino M, Ni P, et al. Development of the life impact burn recovery evaluation (LIBRE) profile: assessing burn survivors’ social participation. Qual Life Res. Published online 2017. doi: 10.1007/s11136-017-1588-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marino M, Soley-Bori M, Jette AM, et al. Development of a conceptual framework to measure the social impact of burns. J Burn Care Res. Published online 2016. doi: 10.1097/BCR.0000000000000358 [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. International Classification of Functioning, Disability and Health (ICF). World Health Organization; 2001. [Google Scholar]
- 19.Spronk I, Legemate CM, Dokter J, van Loey NEE, van Baar ME, Polinder S. Predictors of health-related quality of life after burn injuries: A systematic review. Crit Care. Published online 2018. doi: 10.1186/s13054-018-2071-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gojowy D, Kauke M, Ohmann T, Homann HH, Mannil L. Early and late-recorded predictors of health-related quality of life of burn patients on long-term follow-up. Burns. 2019;45(6):1300–1310. doi: 10.1016/j.burns.2019.03.016 [DOI] [PubMed] [Google Scholar]
- 21.Wasiak J, Paul E, Lee SJ, et al. Patterns of recovery over 12 months following a burn injury in Australia. Injury. Published online 2014. doi: 10.1016/j.injury.2014.02.018 [DOI] [PubMed] [Google Scholar]
- 22.Xie B, Xiao SC, Zhu SH, Xia ZF. Evaluation of long term health-related quality of life in extensive burns: A 12-year experience in a burn center. Burns. Published online 2012. doi: 10.1016/j.burns.2011.09.003 [DOI] [PubMed] [Google Scholar]
- 23.Koljonen V, Laitila M, Sintonen H, Roine RP. Health-related quality of life of hospitalized patients with burns - Comparison with general population and a 2-year follow-up. Burns. Published online 2013. doi: 10.1016/j.burns.2012.07.024 [DOI] [PubMed] [Google Scholar]
- 24.Druery M, Brown TLH, Muller M. Long term functional outcomes and quality of life following severe burn injury. Burns. Published online 2005. doi: 10.1016/j.burns.2005.03.001 [DOI] [PubMed] [Google Scholar]
- 25.Wasiak J, Lee SJ, Paul E, et al. Predictors of health status and health-related quality of life 12 months after severe burn. Burns. Published online 2014. doi: 10.1016/j.burns.2014.01.021 [DOI] [PubMed] [Google Scholar]
- 26.Palmu R, Partonen T, Suominen K, Saarni SI, Vuola J, Isometsä E. Health-related quality of life 6 months after burns among hospitalized patients: Predictive importance of mental disorders and burn severity. Burns. Published online 2015. doi: 10.1016/j.burns.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 27.Fauerbach JA, Lezotte D, Hills RA, et al. Burden of burn: A norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function. J Burn Care Rehabil. Published online 2005. doi: 10.1097/01.BCR.0000150216.87940.AC [DOI] [PubMed] [Google Scholar]
- 28.Ryan CM, Lee A, Kazis LE, et al. Recovery trajectories after burn injury in young adults: Does burn size matter? J Burn Care Res. Published online 2015. doi: 10.1097/BCR.0000000000000214 [DOI] [PubMed] [Google Scholar]
- 29.Marino M, Soley-Bori M, Jette AM, et al. Measuring the Social Impact of Burns on Survivors. J Burn Care Res. Published online 2017. doi: 10.1097/BCR.0000000000000398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kelter BM, Holavanahalli R, Suman OE, Ryan CM, Schneider JC. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns. 2020;46(2):493–496. doi: 10.1016/j.burns.2019.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kishawi D, Wozniak AW, Mosier MJ. TBSA and length of stay impact quality of life following burn injury. Burns. 2020;46(3):616–620. doi: 10.1016/j.burns.2019.09.007 [DOI] [PubMed] [Google Scholar]
- 32.Amtmann D, Bocell FD, McMullen K, Carrougher GJ, Fauerbach J, Gibran NS, Holavanahalli R, Liljenquist K, Meyer W, Ryan CM SJ. The psychometric properties of the Burn Specific Health Scale Brief. J Burn Care Res. 2017; (American Burn Association Meeting). [Google Scholar]
- 33.Martin L, Byrnes M, McGarry S, Rea S, Wood F. Posttraumatic growth after burn in adults: An integrative literature review. Burns. 2017;43(3):459–470. doi: 10.1016/j.burns.2016.09.021 [DOI] [PubMed] [Google Scholar]
- 34.Baillie SE, Sellwood W, Wisely JA. Post-traumatic growth in adults following a burn. Burns. 2014;40(6):1089–1096. doi: 10.1016/j.burns.2014.04.007 [DOI] [PubMed] [Google Scholar]
- 35.Ryan CM, Lee A, Stoddard FJJ, et al. The Effect of Facial Burns on Long-Term Outcomes in Young Adults: A 5-Year Study. J Burn Care Res. 2018;39(4). doi: 10.1093/JBCR/IRX006 [DOI] [PubMed] [Google Scholar]
- 36.Öster C, Sveen J. Is sexuality a problem? A follow-up of patients with severe burns 6 months to 7 years after injury. Burns. 2015;41(7):1572–1578. doi: 10.1016/j.burns.2015.04.017 [DOI] [PubMed] [Google Scholar]
- 37.Pandya AA, Corkill HA, Goutos I. Sexual function following burn injuries: Literature review. J Burn Care Res. 2015;36(6):e283–e293. doi: 10.1097/BCR.0000000000000196 [DOI] [PubMed] [Google Scholar]
- 38.Ohrtman EA, Shapiro GD, Wolfe AE, et al. Sexual Activity and Romantic Relationships after Burn Injury: A Life Impact Burn Recovery Evaluation (LIBRE) Study. Burns. 2020;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mason ST, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K. Return to work after burn injury: A systematic review. J Burn Care Res. 2012;33(1):101–109. doi: 10.1097/BCR.0b013e3182374439 [DOI] [PubMed] [Google Scholar]
- 40.Dyster-Aas J, Kildal M, Willebrand M, Gerdin B, Ekselius L. Work status and burn specific health after work-related burn injury. Burns. Published online 2004. doi: 10.1016/j.burns.2004.05.010 [DOI] [PubMed] [Google Scholar]
- 41.Schneider JC, Bassi S, Ryan CM. Barriers impacting employment after burn injury. J Burn Care Res. Published online 2009. doi: 10.1097/BCR.0b013e318198a2c2 [DOI] [PubMed] [Google Scholar]
- 42.Quinn T, Wasiak J, Cleland H. An examination of factors that affect return to work following burns: A systematic review of the literature. Burns. 2010;36(7):1021–1026. doi: 10.1016/j.burns.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 43.Esselman PC, Wiechman Askay S, Carrougher GJ, et al. Barriers to Return to Work After Burn Injuries. Arch Phys Med Rehabil. 2007;88(12 SUPPL. 2). doi: 10.1016/j.apmr.2007.09.009 [DOI] [PubMed] [Google Scholar]
- 44.Macleod R, Shepherd L, Thompson AR. Posttraumatic stress symptomatology and appearance distress following burn injury: An interpretative phenomenological analysis. Heal Psychol. 2016;35(11):1197–1204. doi: 10.1037/hea0000391 [DOI] [PubMed] [Google Scholar]
- 45.Brych SB, Engrav LH, Rivara FP, et al. Time Off Work and Return to Work Rates after Burns: Systematic Review of the Literature and a Large Two-Center Series. J Burn Care Rehabil. 2001;22(6):401–405. doi: 10.1097/00004630-200111000-00010 [DOI] [PubMed] [Google Scholar]
- 46.Grieve B, Shapiro GD, Wibbenmeyer L, et al. Long-Term Social Reintegration Outcomes for Burn Survivors With and Without Peer Support Attendance: A Life Impact Burn Recovery Evaluation (LIBRE) Study. In: Archives of Physical Medicine and Rehabilitation. Vol 101. W.B. Saunders; 2020:S92–S98. doi: 10.1016/j.apmr.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ryan CM, Stoddard FJ, Kazis LE, Schneider JC. COVID-19 pandemic and the burn survivor community: A call for action. Burns. Published online April 2020. doi: 10.1016/j.burns.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phoenix SOAR | Phoenix Society. Accessed July 17, 2020. https://www.phoenix-society.org/phoenix-soar
- 49.Phoenix WBC | Phoenix Society. Accessed July 17, 2020. https://www.phoenix-society.org/phoenix-wbc


