Abstract
Background
Even though malaria cases have drastically come down in the last decade, malaria remains a serious public health concern in many parts of India. National Framework for Malaria Elimination in India (2016–2030) has been launched with the goal to eliminate malaria by 2030. Understanding the socio-economic and household determinants of malaria at the national level will greatly aid India’s malaria elimination efforts.
Methods
The data from Longitudinal Ageing Survey of India (LASI) Wave 1 (2017–2018) survey comprising 70,671 respondents ≥ 45 years across all the States and Union Territories were used for the analysis. Simple and multiple logistic regressions were used to obtain the unadjusted and adjusted odds ratio respectively of the socio-economic and household variables.
Results
The major socio-economic variables that increase the likelihood of malaria are caste (‘scheduled tribes’), low education levels and rural residence. The scheduled tribes have 1.8 times higher odds of malaria than the scheduled castes (AOR: 1.8; 95% CI: 1.5–2.1). Respondents with high school education (6–12 grade) (AOR: 0.7; 95% CI: 0.6–0.8) and college education (AOR: 0.5; 95% CI: 0.4–0.6) had a very low risk of malaria than those with no school years. Rural residence and occupation (agriculture and allied jobs) also increases the odds of malaria. The major housing determinants are household size (≥ 6), housing type (kutcha), use of unclean fuel, outside water source, improper sanitation (toilet facilities) and damp wall/ceiling.
Conclusions
The study has identified the major socio-economic and housing factors associated with malaria in adults aged 45 and above. In addition to vector and parasite control strategies in the tribal dominated regions of India, improving literacy and housing conditions may help India’s malaria elimination efforts.
Keywords: LASI, Socio-economic determinants of malaria, Household determinants of malaria, Schedule tribe and malaria, Unclean cooking fuel and malaria
Background
Globally, vector borne diseases account for > 17% of all the infectious diseases, and account for > 700,000 deaths annually [1]. Malaria is a major vector borne disease, and is a serious public health concern in many parts of India [2–5]. Malaria situation in India is complex with varied distribution of Plasmodium vivax and Plasmodium falciparum [6]. According to the World Health Organization (WHO), 93% of the population in India are at risk of malaria [7]. From 2000 to 2017, malaria morbidity and mortality in India have declined by 59 and 89%, respectively [8]. In India, malaria is transmitted by several Anopheles spp., and the geography determines the primary Anopheles vector; Anopheles stephensi, Anopheles culicifacies, Anopheles dirus, Anopheles fluviatilis, Anopheles minimus and Anopheles sundaicus are considered to be the primary malaria vectors in India [9].
In 2015, India has committed to elimination of malaria by 2030 at the Asia Pacific Leaders Malaria Alliance meeting in Kuala Lampur [10]. The National Vector Borne Disease Control Programme (NVBDCP) launched the National Framework for Malaria Elimination in India (2016–2030) in 2016 with two major goals: (1) Eliminating malaria throughout India by 2030 and (2) Maintaining malaria-free status in regions where malaria transmission is disrupted, and preventing re-introduction of malaria [11]. Furthermore, Malaria Elimination Research Alliance has been launched under the umbrella of Indian Council of Medical Research (ICMR) to “identify, articulate, prioritize and respond to the research needs of the country to eliminate malaria from India by 2030” [8].
India’s malaria control strategies focuses on effective vector control using indoor residual spraying, long-lasting insecticidal nets, chemical insecticides, bacterial pesticides and larvivorous fish [12]. Chemotherapy using artemisinin-based combination therapy for P. falciparum and chloroquine/primaquine for P. vivax are the major treatment strategies under the national drug policy [13].
Malaria transmission is influenced by several factors, including socio-economic and demographic characteristics of the study area [14]. In addition, housing factors have also been shown to play an important role in malaria transmission [15, 16]. In India, studies on socio-economic and household determinants of malaria are very limited, and are focused on selected districts [14, 17–19]. Type of house, toilet facility and water-source were the major housing risk factors [17], while, social groups, family size [14], monthly income [18] were some of the key socio-economic determinants reported in these Indian studies.
A pan-India study on the socio-economic and household determinants of malaria may give important insights on the major risk factors, and aid in country’s malaria control and elimination efforts. Longitudinal Ageing survey of India-1 (LASI-1) carried out across India from April 2017 to December 2018 provides important insight into various health parameters of elderly individuals (≥ 45 years), including the socio-economic and housing conditions of self-reported cases of malaria in the past two years before the survey. This LASI data set from 70,671 individuals was used to analyse the key socio-economic and housing determinants of malaria, and the results are detailed.
Methods
Data and participants
Data from the LASI Wave 1 (2017–2018) survey carried out by the International Institute for Population Sciences (IIPS) in Mumbai across 28 states (except Sikkim) and seven Union Territories (UT) were used for the analysis. A multi-stage cluster sampling was used to collect data on many social, economic and health indicators. The LASI Wave-1 surveyed 70,671 respondents ≥ 45 years and their spouses (even if they are < 45). There were 28,754 (41 %) aged 45–54 years, 28,579 (40.4 %) aged 55–69 years, 13,338 (19 %) aged ≥ 70 years, and 40,877 (58 %) females. The LASI has employed Computer-Assisted Personal Interview techniques to record the responses of survey participants.
Study variables
Outcome variable
The outcome of interest is malaria, and was based on the following question: 1. In the past 2 years, have you had malaria? The options were: (1) Yes, and (2) No. The response was coded as a binary variable (No—0: absence of malaria; Yes—1: presence of malaria).
Socio-economic status and demographic variables
The socio-economic status (SES) and demographic variables used for this analysis are age-group (45–54 years, 55–69 years and ≥ 70 years), sex (male or female), place of residence (rural or urban), income category based on Monthly Per capita Consumption Expenditure (MPCE) (poorest, poor, middle, richer and richest), educational level (0 school years, 1–5 school years, 6–12 school years and college), work (not working, agricultural and allied, self-employed and wage/salary worker), and caste (SC, ST, OBC and forward caste). The terms ‘SC’ (Scheduled Castes) and ‘ST’ (Scheduled Tribes) are officially used in the government documents to identify the socially weaker sections and tribes in the country. The major class of the country is OBC (Other Backward Classes), and comprises 40–50 % of the population.
Household conditions
Household variables used are household size (1–5/≥ 6 members), type of house (pucca/kutcha), location of water source (own dwelling, yard/plot or outside dwelling), toilet type (improved: flushed to piped sewer system/septic tank/pit latrine/twin pit/composting toilet; unimproved sanitation: open defecation), cooking fuel (clean fuel: LPG, biogas and electricity; unclean fuel: kerosene, charcoal, coal, crop residue, wood/shrub and dung cake) and damp wall or ceiling (yes/no).
Statistical analysis
A frequency distribution table was prepared for all the variables used in this study. Prevalence of malaria with each of the SES (age group, sex, residence area, education level, MPCE quintiles, caste, and work) and household variables (household size, type of house, location of water source, toilet type, cooking fuel, and damp wall or ceiling) were reported. Simple logistic regression was used to obtain the unadjusted odds ratio (UOR), and those independent variables found significant (P < 0.05) were included in the multiple logistic regression to arrive at the Adjusted Odds Ratio (AOR) of SES and household variables in association with malaria. All the independent variables were significant at the alpha value of 5 % except for the variable ‘sex’ in the univariable logistic regression analysis. The variable ‘sex’ was used in the multivariable logistic regression despite not found significant in the univariable analysis because ‘sex’ is an important variable to adjust for in the analysis. Sampling weights calculated by LASI were applied during the analysis to obtain accurate estimates. All analyses were performed using STATA MP statistical software version 16.
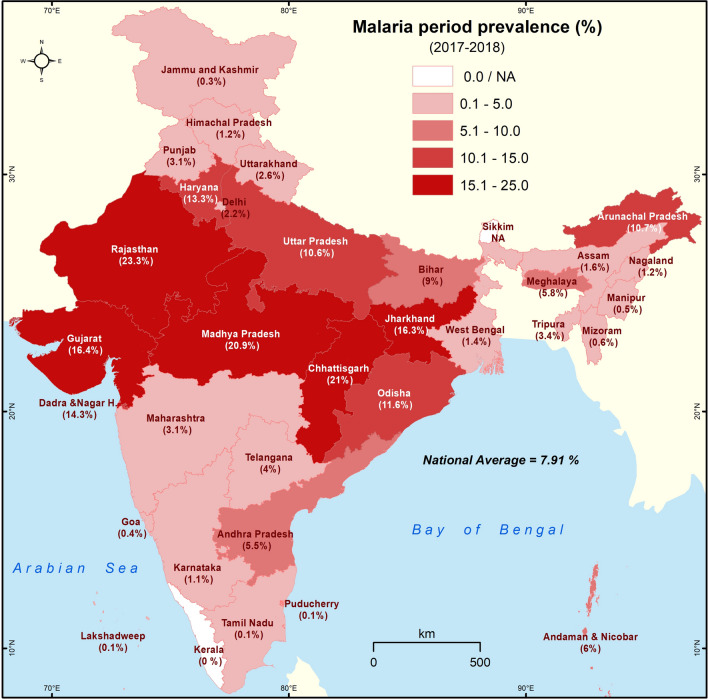
Spatial analysis
The malaria prevalence (%) data was added as attribute in State and UT boundaries of India using ArcGIS software. The histogram of the malaria prevalence data was analysed, and was used to determine the four class intervals for mapping; the national average of malaria period prevalence is 7.91 %. The rounded off class interval 0.1–5.0 represents below national average States/UT, 5.1–10.0 represents national average, 10.1–15.0 denotes above national average, and 15.1–25.0 shows twice the national average. The choropleth techniques were used for mapping, and darker colors denote higher values.
Results
Prevalence of malaria in adults ≥ 45 years
The frequency distribution of all the study variables is shown in Table 1. The prevalence of malaria during the period 2017–2018 in adults ≥ 45 years is 7.9 %. The self-reported period prevalence of malaria across all the States and UT of India during the survey is shown in Fig. 1. The period prevalence of malaria is high in Central and Western India when compared to the South, North and Eastern regions. The states with very high (> 15 %) prevalence include Rajasthan (23.3 %), Chhattisgarh (21 %), Madhya Pradesh (20.9 %), Gujarat (16.4 %) and Jharkhand (16.3 %). The above national average (10–15 %) prevalence is reported in the States/UT surrounding Central India─Dadra and Nagar Haveli (14.3 %), Haryana (13.3 %), Odisha (11.6 %), Uttar Pradesh (10.6 %) and Bihar (9 %). The States/UT that exceeded 5 % prevalence in the South are Andhra Pradesh (5.5 %) and Andaman & Nicobar Islands (6 %), and in the North-East (NE), it is Arunachal Pradesh (10.7 %) and Meghalaya (5.8 %). The northern-most States/UT (Jammu & Kashmir, Himachal Pradesh, Punjab and Uttarakhand) show very low (0–5 %) prevalence of malaria.
Table 1.
Distribution of socio-demographic and household variables of adults ≥ 45 years in India, LASI-1 (2017–2018)
| Variables | n | % |
|---|---|---|
| Malaria | 5589 | 7.9 |
| Age group (44–54 years) | 28,754 | 40.7 |
| 55–69 years | 28,579 | 40.4 |
| ≥ 70 years | 13,338 | 18.9 |
| Sex (female) | 40,877 | 57.8 |
| Male | 29,795 | 42.2 |
| Residence (rural) | 48,921 | 69.2 |
| Urban | 21,750 | 30.8 |
| MPCE quintile (poorest) | 14,790 | 20.9 |
| Poorer | 15,023 | 21.3 |
| Middle | 14,268 | 20.2 |
| Richer | 13,781 | 19.5 |
| Richest | 12,809 | 18.1 |
| Education (0 school years) | 35,081 | 49.6 |
| 1–5 school years | 12,334 | 17.5 |
| 6–12 school years | 18,883 | 26.7 |
| College | 4372 | 6.2 |
| Caste (SC) | 13,612 | 20.0 |
| ST | 6033 | 8.9 |
| OBC | 31,530 | 46.3 |
| Forward | 16,924 | 24.9 |
| Main job (not woking) | 35,590 | 50.1 |
| Agricultural and allied | 19,961 | 28.1 |
| Self-employed | 6072 | 8.55 |
| Wage/salary worker | 9406 | 13.2 |
| Household-size (1–5 members) | 44,815 | 63.0 |
| ≥ 6 members | 26,319 | 37.0 |
| Type of house (pucca/semi pucca) | 58,912 | 83.3 |
| Kutcha | 11,834 | 16.7 |
| Water source (own dwelling/plot/yard) | 46,231 | 68.7 |
| Outside dwelling | 21,056 | 31.3 |
| Toilet facility (improved sanitation) | 51,652 | 73.4 |
| Unimproved | 18,766 | 26.7 |
| Cooking fuel (clean) | 36,858 | 52.3 |
| Unclean | 33,559 | 47.7 |
| Damp wall/ceiling (no) | 55,684 | 79.1 |
| Yes | 14,748 | 20.9 |
Fig. 1.
Self-reported prevalence of malaria in different States and Union Territories of India (LASI-1 2017–2018). The intervals represent malaria prevalence. The darker the shade, higher is the prevalence
The prevalence of malaria associated with SES and household variables in adults ≥ 45 is shown in Table 2. Malaria prevalence is similar in all age groups, and is slightly higher in males (8.1 %) than in females (7.8 %). Malaria is higher in the rural (9.6 %) than in urban (4 %) respondents. The prevalence of malaria is highest in the ST population (15 %) when compared to the other social groups. Malaria prevalence reduced with increasing levels of education (9.7 % in illiterates vs. 3 % in the college educated) and income of households (9.2 % in the poorest vs. 6.9 % in the richest). Malaria prevalence is highest in those working in agriculture and allied jobs (10.5 %), and is lowest in wage/salaried workers (5.2 %). Malaria is highest in households with ≥ six members (9.5 %), and in those living in kutcha houses (12 %). The prevalence of malaria is more in adults with no source of drinking water inside the house (10.6 %) than those who have a water-source within their residence (6.9 %). Malaria is more in households (11.7 %) with poor sanitation (unimproved toilet facility) compared to households (5 %) that have improved sanitation facilities. Malaria in households using unclean fuel is 11.2 %, and in households with damp wall/ceiling, it is 9.6 %.
Table 2.
Prevalence of malaria by socio-demographic and household variables in adults ≥ 45 years in India, LASI-1 (2017–2018)
| Variables | n | % | Total |
|---|---|---|---|
| Age group (44–54 years) | 2107 | 7.3 | 28,757 |
| 55–69 years | 2415 | 8.4 | 28,591 |
| ≥ 70 years | 1067 | 8.0 | 13,340 |
| Sex (female) | 3170 | 7.8 | 40,884 |
| Male | 2419 | 8.1 | 29,803 |
| Residence (rural) | 4717 | 9.6 | 48,931 |
| Urban | 873 | 4.0 | 21,756 |
| MPCE quintile (poorest) | 1366 | 9.2 | 14,794 |
| Poorer | 1293 | 8.6 | 15,026 |
| Middle | 1072 | 7.5 | 14,267 |
| Richer | 972 | 7.1 | 13,791 |
| Richest | 885 | 6.9 | 12,810 |
| Education (0 school years) | 3400 | 9.7 | 35,087 |
| 1–5 school years | 1049 | 8.5 | 12,336 |
| 6–12 school years | 1010 | 5.3 | 18,890 |
| College | 130 | 3.0 | 4373 |
| Caste (SC) | 1118 | 8.2 | 13,612 |
| ST | 904 | 15.0 | 6035 |
| OBC | 2387 | 7.6 | 31,542 |
| Forward | 1086 | 6.4 | 16,927 |
| Main job (not working) | 2691 | 7.6 | 35,369 |
| Agricultural and allied | 2076 | 10.5 | 19,837 |
| Self-employed | 331 | 5.5 | 6043 |
| Wage/salary worker | 485 | 5.2 | 9333 |
| Household-size (1–5 members) | 3117 | 7.0 | 44,571 |
| ≥ 6 Members | 2472 | 9.5 | 26,116 |
| Type of house (pucca/semi pucca) | 4166 | 7.1 | 58,552 |
| Kutcha | 1402 | 11.9 | 11,751 |
| Water source (own dwelling/plot/yard) | 3236 | 7.0 | 45969 |
| Outside dwelling | 2214 | 10.6 | 20897 |
| Toilet facility (Improved sanitation) | 3374 | 6.5 | 51663 |
| Unimproved | 2204 | 11.7 | 18771 |
| Cooking fuel (clean) | 1828 | 5.0 | 36875 |
| Unclean | 3751 | 11.2 | 33557 |
| Damp wall/ceiling (No) | 4160 | 7.5 | 55684 |
| Yes | 1419 | 9.6 | 14748 |
Association between socio-economic and housing conditions with malaria in adults ≥ 45 years
The SES and household variables analysed by simple and multiple logistic regressions are shown in Table 3. Rural residence, richest, illiterates, less educated, ST population, working in agriculture and allied jobs, not working, household size with ≥ six members, no water-source within a dwelling, unimproved toilet facility, using unclean fuel for cooking, and damp wall/ceiling are associated with an increased risk for malaria.
Table 3.
Odds ratios of malaria in adults ≥ 45 years, LASI-1 (2017–2018)
| Variables | Malaria | ||
|---|---|---|---|
| UOR | AOR | 95 % CI | |
| Age group (44–54 years) | 1 | ||
| 55–69 years | 1.2** | 1.0 | 0.9–1.1 |
| 70 + years | 1.1 | 0.9 | 0.8–1.1 |
| Sex (female) | 1 | ||
| Male | 1.1 | 1.2** | 1.0–1.3 |
| Residence (rural) | 1 | ||
| Urban | 0.4** | 0.7** | 0.6–0.8 |
| MPCE quintile (poorest) | 1 | ||
| Poorer | 0.9 | 1.1 | 1.0–1.2 |
| Middle | 0.8** | 1.0 | 0.9–1.2 |
| Richer | 0.7** | 1.1 | 0.9–1.2 |
| Richest | 0.7** | 1.2** | 1.1–1.5 |
| Education (0 school years) | 1 | ||
| 1–5 school years | 0.8* | 1.0 | 0.9–1.1 |
| 6–12 school years | 0.5** | 0.7** | 0.6–0.8 |
| College/university | 0.3** | 0.5** | 0.4–0.7 |
| Caste (SC) | 1 | ||
| ST | 1.9** | 1.7** | 1.5–1.9 |
| OBC | 0.9 | 1.1 | 1.0–1.2 |
| Forward | 0.8** | 1.0 | 0.9–1.2 |
| Main Job (wage/salary worker) | 1 | ||
| Agricultural and allied | 2.1** | 1.3* | 1.1–1.5 |
| Self-employed | 1.1 | 1 | 0.8–1.3 |
| Not working | 1.5** | 1.3** | 1.1–1.5 |
| Household size (1–5 members) | 1 | ||
| ≥ 6 members | 1.4** | 1.3** | 1.2–1.4 |
| Type of house (pucca/semi pucca) | 1 | ||
| Kutcha | 1.8** | 1.1** | 1.0–1.3 |
| Water source (own dwelling/yard/plot) | 1 | ||
| Outside dwelling | 1.6** | 1.1** | 1.0–1.2 |
| Toilet facility (improved sanitation) | 1 | ||
| Unimproved | 1.9** | 1.2** | 1.1–1.3 |
| Cooking fuel (clean) | 1 | ||
| Unclean | 2.4** | 1.5** | 1.4–1.7 |
| Damp wall/ceiling (no) | 1 | 1 | |
| Yes | 1.3** | 1.2** | 1.1–1.3 |
UOR unadjusted odds ratio, AOR adjusted odds ratio
*P<0.05 ** P<0.01
Residing in an urban area reduced the risk of malaria (AOR: 0.7; 95 % CI: 0.6–0.8). Males have slightly higher odds for malaria than females (AOR: 1.1; 95 % CI: 1.0-1.3). Richest are 1.2 times more at risk for malaria than the poorest (AOR: 1.3; 95 % CI: 1.1–1.5). Respondents who did high school education (6–12 grade) (AOR: 0.7; 95 % CI: 0.6–0.8) and college education (AOR: 0.5; 95 % CI: 0.4–0.6) have a very low risk of malaria than those with no school education. The ST have 1.8 times higher odds of malaria than the SC (AOR: 1.8; 95 % CI: 1.5–2.1). Malaria odds are higher for those working in agriculture and allied jobs, and in those who are ‘not working’ (AOR: 1.3; 95 % CI: 1.1–1.5) when compared to wage/salaried workers. Households with more than five members have a higher likelihood for malaria (AOR: 1.5; 95 % CI: 1.3–2.7). Respondents in kutcha houses have more odds for malaria (AOR: 1.1; 95 % CI: 1.1–1.3) than those in pucca houses. Households with water-source not in the dwelling (AOR: 1.1; 95 % CI: 1.1–1.4), and unimproved toilet facility (AOR: 1.2; 95 % CI: 1.1–1.3) have more odds for malaria. Households using unclean fuel for cooking have 1.5 times higher odds (AOR: 1.5; 95 % CI: 1.4–1.7) when compared to households that are using LPG/electricity/biogas for cooking. Also, households with damp wall/ceiling have 1.2 times higher odds of malaria (AOR: 1.2 95 % CI 1.1–1.3) than those with no damp wall/ceiling.
Discussion
According to LASI (2017-18), the States/UT with over 10 % prevalence include Rajasthan, Chhattisgarh, Madhya Pradesh, Gujarat, Jharkhand, Dadra and Nagar Haveli, Haryana, Odisha, Uttar Pradesh and Arunachal Pradesh. Among these, Odisha, Chhattisgarh, Jharkhand and Madhya Pradesh are highly endemic for malaria. From July 2019, High Burden to High Impact strategy of WHO has been initiated in Jharkhand, Chhattisgarh, Madhya Pradesh and West Bengal [20, 21]. Considering the known endemicity of malaria in different States, the overall trends of malaria prevalence are on expected lines. However, there are surprising high and low prevalence data of malaria in specific States. Two striking observations stand-out in this survey: (1) Rajasthan at 23.3 % ranks number 1 in the self-reported cases and (2) The NE State of Mizoram is among the lowest with 0.5 %. Even though, malaria (esp. P. vivax) is prevalent in Rajasthan, it is not considered to be among the top 5 malaria endemic states in India [22, 23]. On the other hand, Mizoram is considered to be one of the highly malaria endemic States in India [24, 25]. One explanation for the unexpected numbers could be the study sites where the survey was undertaken. For example, in Mizoram, the district of Aizawl reported 57 malaria cases in 2018, while the malaria-endemic districts of Lawngtlai, Lunglei and Mamit reported 2222, 1092 and 772, respectively. Therefore, if the survey was carried out at Aizawl, the capital of Mizoram, the self-reported malaria cases will be lower. Another possibility could be the adults in Mizoram may be asymptomatic due to various types of adaptive or acquired immunity [26]. In sub-Saharan Africa, many adults who harbour the parasites rarely show clinical symptoms [26]. At Mamit, the average annual parasite index (API) from 2010 to 2018 was 34.4 (34 cases / 1000), one of the highest in the country [24]. During 2014 to 2015, there was a big spike in malaria cases in Mizoram, and in Mamit district, nearly 50 % of the total population (8766 cases out of 17,731) were affected in 2015 [24].
Despite the significant strides India has made in decreasing malaria mortality and morbidity in the last two decades (from 2000 to 2019, malaria cases and deaths have declined by 71.8 and 73.9 %, respectively) [27], malaria remains a serious public health issue in several parts of the country. The NVBDCP has developed a comprehensive strategic plan to achieve malaria-free India by 2030 [28]. For devising effective malaria control and elimination strategies, understanding the socio-economic and household variables that affect malaria transmission is imperative. Analysis indicates rural residence, occupation (agricultural and allied), education levels (illiterates and primary), caste (ST), household size (≥ 6), sanitation (poor toilet facility), unclean cooking fuel, water-source not in dwelling, damp wall/ceiling are the major socio-economic and household risk factors that affect malaria transmission.
Not surprisingly, ST population are at a higher malaria risk. Jharkhand, Chhattisgarh, Madhya Pradesh, Odisha and malaria-endemic NE States (Tripura, Meghalaya, Mizoram and Arunachal Pradesh) have a high ST population. The geographical terrain that includes many forested areas, poor accessibility, frequent natural hazards, perennial P. falciparum transmission, very efficient anthropophillic vectors, and socio-cultural practices greatly hinder malaria control efforts in many rural tribal areas of India [6, 29]. The orthodox health beliefs of tribal population have restrained them from accessing health services despite them being highly vulnerable to various health hazards, including malaria [29, 30]. In addition, the dense forest cover and high rainfall in the tribal belts are conducive for mosquito breeding, and malaria transmission [29, 30]. Many of the tribal pockets where malaria is endemic are characterized by poor housing conditions. Residents in kutcha houses have higher odds of malaria; kutcha houses may have holes and gaps that allow easy entry of mosquitoes. This is in line with earlier Indian studies where kutcha houses/walls made of dung and earth have shown to be a risk factor for malaria [14, 17]. Positive association between mosquito bites/day and bamboo houses has been reported in Assam, India [18].
Literacy has a negative association with malaria; illiterates and those with just primary education have higher risk of malaria. This was expected as literacy gives a better understanding of infectious diseases and the protective measures required. However, earlier studies [14, 18] in India did not find an association between education and malaria risk. In Yadav et al. [18], the sample size was just 71 households, while in Sharma et al. [14], only no schooling, primary and secondary grades were included, and college education was not included in the education characteristics. ST who are at higher risk of malaria have lower literacy rate (59 %), when compared to the national average of 73 % [31].
Malaria risk is higher in those who carry out agricultural and allied activities when compared to respondents who are self-employed or get wage/salary. Agricultural activities require significant time to be spent outdoors, and these individuals are at higher risk of mosquito bites. A recent study from Mandla district in Madhya Pradesh shows households having own farmlands to have a significant association with malaria [17].
Size of the household (≥ 6 members) contributed a significant risk to malaria prevalence. Family size/number of people in the house/number of people per room is an important risk factor for malaria [14, 17, 32–35], as crowding attracts more mosquitoes due to strong olfactory signals [36]. As observed in studies carried out in India [14, 17], Ethiopia [37], Indonesia [38], and sub-Saharan Africa [39], access to outside water-source is a major malaria risk factor, as dependence on outside source for water, especially in dusk and dawn increases the chances of mosquito bite. Furthermore, households using tube-wells as outside water-source have risk of malaria [17], as tube-wells are suggested to have more stagnant water around them due to improperly maintained drainage facilities [40]. Poor toilet facility (sanitation) is another important household risk factor of malaria, and is in-line with earlier studies carried out in India [17] and elsewhere [37–39, 41]. Use of unclean cooking fuel is also a major risk factor (odds increase by 1.5 times) for malaria. In addition, damp wall/ceiling is also associated with increased malaria risk; damp walls favour indoor resting of mosquitoes [42]. The three household determinants: outside water-source, improper toilet facility and unclean cooking fuel increases the likelihood of mosquito bites outside the house. Increased time required for outdoor cooking using unclean cooking fuel could be a reason for its higher odds. Free clean cooking fuel (liquid petroleum gas connection) has been given to > 80 million Indian households through the Pradhan Mantri Ujjwala Yojana (PMUY) scheme [43]. Through this scheme, it is expected that 80 % of the households will have clean cooking fuel by 2019 [44]. In addition to improving the standard of living, the PMUY scheme may also help in malaria control and elimination efforts.
Malaria is considered to be a disease of the poor [45–47], and several studies have shown significant association between poverty and malaria [48, 49]. There are also studies that have shown no significant association between malaria and SES of the household [17, 50–52]. Interestingly, even though prevalence of malaria is higher in poorest, after adjusting the other socio-economic variables, richest were found to have slightly higher risk of malaria than the other economic categories. Urban malaria is predominantly caused by P. vivax, and as this is a pan-India study, a higher proportion of respondents positive for P. vivax could have been from urban cities, and are likely to be socio-economically forward. For example, Uttar Pradesh, the most populous State in India has predominantly P. vivax [23]. Furthermore, richest, especially in urban cities may get tested promptly, and report accurately. However, the socio-economic-housing risk factors like rural residence, caste (ST), education levels, housing conditions, sanitation, unclean cooking fuel, improper water source and damp wall/ceiling strongly suggest poverty to be a risk factor for P. falciparum malaria, especially in the tribal dominated States of Jharkhand, Chhattisgarh, Madhya Pradesh, Odisha, Mizoram, Tripura and Meghalaya.
The major limitation of the study is that it is limited to adults ≥ 45 years old. Malaria affects all age groups, and this study captures only a particular age group. Furthermore, as malaria prevalence is self-reported, the accuracy cannot be verified.
Conclusions
Overall, the study gives important insights on socio-economic and housing determinants of malaria. In parallel to parasite and vector control strategies, improving the socio-economic and living conditions, especially in malaria dominated tribal pockets may assist the malaria elimination efforts.
Acknowledgements
The authors thank IIPS Mumbai for providing permission to use the data. The authors also thank Central University of Tamil Nadu for providing facilities to carry out the analysis.
Abbreviations
- LASI
Longitudinal Ageing Survey of India
- IIPS
International Institute for Population Sciences
- ICMR
Indian Council for Medical Research
- AOR
Adjusted odds ratio
- UOR
Unadjusted odds ratio
- NVBDCP
National Vector Borne Disease Control Programme
- NE
North-East
- ST
Scheduled Tribes
- SC
Scheduled Castes
- PMUY
Pradhan Mantri Ujjwala Yojana
- SES
Socio-economic status
- UT
Union Territories
Authors’ contributions
PBN designed the study. IM, NKK, PBN, BK carried out the experiments and analysed the data. PBN, IM, SKB, GN helped in writing and editing the manuscript. All authors read and approved the final manuscript.
Funding
This work received no funding support.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Declarations
Ethics approval and consent to participate
The ICMR provided guidance and ethical approval for conducting the LASI. The IIPS in Mumbai carried out the study in collaboration with Harvard T.H. Chan School of Public health and the University of Southern California, USA. Written consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vector-borne diseases https://www.who.int/news-room/fact-sheets/detail/vector-borne-diseases (Accessed on April 25 2021)].
- 2.Dash AP, Valecha N, Anvikar AR, Kumar A. Malaria in India: challenges and opportunities. J Biosci. 2008;33:583–92. doi: 10.1007/s12038-008-0076-x. [DOI] [PubMed] [Google Scholar]
- 3.Dash AP, Adak T, Raghavendra K, Singh OP. The biology and control of malaria vectors in India. Curr Sci. 2007;92:1571–8. [Google Scholar]
- 4.Kumar A, Valecha N, Jain T, Dash AP. Burden of malaria in India: retrospective and prospective view. Am J Trop Med Hyg. 2007;77:69–78. doi: 10.4269/ajtmh.2007.77.69. [DOI] [PubMed] [Google Scholar]
- 5.Singh V, Mishra N, Awasthi G, Dash AP, Das A. Why is it important to study malaria epidemiology in India? Trends Parasitol. 2009;25:452–7. doi: 10.1016/j.pt.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Sarma DK, Mohapatra PK, Bhattacharyya DR, Chellappan S, Karuppusamy B, Barman K, et al. Malaria in North-East India: importance and implications in the era of elimination. Microorganisms. 2019;7:673. doi: 10.3390/microorganisms7120673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. World Malaria R 2018. Geneva WH, Organization. 2018. [Available from: https://www.who.int/malaria/publications/country-profiles/profile_ind_en.pdf?ua=1 (Accessed on May 25, 2020)].
- 8.Rahi M, Anvikar A, Singh O, Jambulingam P, Vijayachari P, Das A, et al. MERA India: malaria elimination research alliance India. J Vector Borne Dis. 2019;56:1–3. doi: 10.4103/0972-9062.257766. [DOI] [PubMed] [Google Scholar]
- 9.Dev V, Sharma V. The dominant mosquito vectors of human malaria in India, Anopheles mosquitoes - New insights into malaria vectors. In: Anopheles mosquitoes, new insights into malaria vectors. Manguin S, Editor. Rijeka: IntechOpen; 2013 (https://www.intechopen.com/books/anopheles-mosquitoes-new-insights-into-malaria-vectors/the-dominant-mosquito-vectors-of-human-malaria-in-india Accessed on April 30, 2021).
- 10.Asia Pacific Leaders Malaria Alliance. [https://www.aplma.org/upload/book/leaders-roadmap.pdf (Accessed on May 26, 2020)].
- 11.National Framework Malaria Elimination. India 2016–2030 [https://www.who.int/docs/default-source/searo/india/health-topic-pdf/national-framework-malaria-elimination-india-2016-2030.pdf?sfvrsn=606b352a_2 (Accessed on April 30, 2021)].
- 12.Subbarao SK, Nanda N, Rahi M, Raghavendra K. Biology and bionomics of malaria vectors in India: existing information and what more needs to be known for strategizing elimination of malaria. Malar J. 2019;18:396. doi: 10.1186/s12936-019-3011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Drug Policy on Malaria. [https://nvbdcp.gov.in/Doc/National-Drug-Policy-2013.pdf (Accessed on April 30, 2021)].
- 14.Sharma RK, Singh MP, Saha KB, Bharti PK, Jain V, Singh PP, et al. Socio-economic & household risk factors of malaria in tribal areas of Madhya Pradesh, central India. Indian J Med Res. 2015;141:567–75. doi: 10.4103/0971-5916.159515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gamage-Mendis AC, Carter R, Mendis C, De Zoysa AP, Herath PR, Mendis KN. Clustering of malaria infections within an endemic population: risk of malaria associated with the type of housing construction. Am J Trop Med Hyg. 1991;45:77–85. doi: 10.4269/ajtmh.1991.45.77. [DOI] [PubMed] [Google Scholar]
- 16.Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes M, Lindsay SW, Byass P. Household risk factors for malaria among children in the Ethiopian highlands. Trans R Soc Trop Med Hyg. 2000;94:17–21. doi: 10.1016/S0035-9203(00)90424-3. [DOI] [PubMed] [Google Scholar]
- 17.Sharma RK, Rajvanshi H, Bharti PK, Nisar S, Jayswar H, Mishra AK, et al. Socio-economic determinants of malaria in tribal dominated Mandla district enrolled in Malaria Elimination Demonstration Project in Madhya Pradesh. Malar J. 2021;20:7. doi: 10.1186/s12936-020-03540-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yadav K, Dhiman S, Rabha B, Saikia P, Veer V. Socio-economic determinants for malaria transmission risk in an endemic primary health centre in Assam, India. Infect Dis Poverty. 2014;3:19. doi: 10.1186/2049-9957-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh MP, Saha KB, Chand SK, Savargaonkar D. Socioeconomic determinants of community knowledge and practice in relation to malaria in high- and low-transmission areas of central India. J Biosoc Sci. 2020;52:317–29. doi: 10.1017/S0021932019000440. [DOI] [PubMed] [Google Scholar]
- 20.WHO. World Malaria Report 2020: India continues to make impressive gains in reduction of malaria burden [https://pib.gov.in/Pressreleaseshare.aspx?PRID=1677601 (Accessed on April 30, 2021)].
- 21.WHO. Malaria. [https://www.who.int/india/health-topics/malaria (Accessed on April 30, 2021)].
- 22.Lingala MAL. Effect of meteorological variables on Plasmodium vivax and Plasmodium falciparum malaria in outbreak prone districts of Rajasthan, India. J Infect Public Health. 2017;10:875–80. doi: 10.1016/j.jiph.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Anvikar AR, Shah N, Dhariwal AC, Sonal GS, Pradhan MM, Ghosh SK, et al. Epidemiology of Plasmodium vivax malaria in India. Am J Trop Med Hyg. 2016;95:108–20. doi: 10.4269/ajtmh.16-0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zomuanpuii R, Hmar CL, Lallawmzuala K, Hlimpuia L, Balabaskaran Nina P, Senthil Kumar N. Epidemiology of malaria and chloroquine resistance in Mizoram, northeastern India, a malaria-endemic region bordering Myanmar. Malar J. 2020;19:95. doi: 10.1186/s12936-020-03170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karuppusamy B, Sarma DK, Lalmalsawma P, Pautu L, Karmodiya K, Nina PB. Effect of climate change and deforestation on vector borne diseases in the North-Eastern Indian state of Mizoram bordering Myanmar. J Climate Change Health. 2021;2:100015. doi: 10.1016/j.joclim.2021.100015. [DOI] [Google Scholar]
- 26.Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36. doi: 10.1128/CMR.00025-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO. World Malaria R. 2020. Geneva, World Health Organization, [https://pib.gov.in/PressReleasePage.aspx?PRID=1677601#:~:text=India%20has%20sustained%20Annual%20Parasitic,less%20than%20one %20since%202012&text=The%20World%20Malaria%20Report%20(WMR,in%20reducing%20its%20malaria%20burden (Accessed on April 30, 2021).].
- 28.Rahi M, Anvikar AR, Singh OP, Jambulingam P, Vijayachari P, Das A, et al. MERA India: Malaria Elimination Research Alliance India. J Vector Borne Dis. 2019;56:1–3. doi: 10.4103/0972-9062.257766. [DOI] [PubMed] [Google Scholar]
- 29.Singh N, Mishra AK, Saha KB, Bharti PK, Sisodia DS, Sonal GS, et al. Malaria control in a tribal area of central India using existing tools. Acta Trop. 2018;181:60–8. doi: 10.1016/j.actatropica.2017.12.018. [DOI] [PubMed] [Google Scholar]
- 30.Sharma RK, Thakor HG, Saha KB, Sonal GS, Dhariwal AC, Singh N. Malaria situation in India with special reference to tribal areas. Indian J Med Res. 2015;141:537–45. doi: 10.4103/0971-5916.159510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ministry of Tribal Affairs [https://tribal.nic.in/downloads/Statistics/Statistics8518.pdf (Accessed on April 30, 2021)].
- 32.Thomas S, Ravishankaran S, Asokan A, Johnson Amala Justin NA, Maria Jusler Kalsingh T, Mathai MT, et al. Socio-demographic and household attributes may not necessarily influence malaria: evidence from a cross sectional study of households in an urban slum setting of Chennai, India. Malar J. 2018;17:4. doi: 10.1186/s12936-017-2150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saha KB, Sharma RK, Mishra R, Verma A, Tiwari BK, Singh N. Establishing communication mechanism for malaria prevention in Baiga tribal villages in Baiga Chak area of Dindori district, Madhya Pradesh. Indian J Med Res. 2015;141:576–83. doi: 10.4103/0971-5916.159516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Butraporn P, Sornmani S, Hungsapruek T. Social, behavioural, housing factors and their interactive effects associated with malaria occurrence in east Thailand. Southeast Asian J Trop Med Public Health. 1986;17:386–92. [PubMed] [Google Scholar]
- 35.Guthmann JP, Hall AJ, Jaffar S, Palacios A, Lines J, Llanos-Cuentas A. Environmental risk factors for clinical malaria: a case-control study in the Grau region of Peru. Trans R Soc Trop Med Hyg. 2001;95:577–83. doi: 10.1016/S0035-9203(01)90084-7. [DOI] [PubMed] [Google Scholar]
- 36.Riabinina O, Task D, Marr E, Lin C-C, Alford R, O’Brochta DA, et al. Organization of olfactory centres in the malaria mosquito Anopheles gambiae. Nat Commun. 2016;7:13010. doi: 10.1038/ncomms13010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ayele DG, Zewotir TT, Mwambi HG. Prevalence and risk factors of malaria in Ethiopia. Malar J. 2012;11:195. doi: 10.1186/1475-2875-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hasyim H, Dhimal M, Bauer J, Montag D, Groneberg DA, Kuch U, et al. Does livestock protect from malaria or facilitate malaria prevalence? A cross-sectional study in endemic rural areas of Indonesia. Malar J. 2018;17:302. doi: 10.1186/s12936-018-2447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang D, He Y, Wu B, Deng Y, Li M, Yang Q, et al. Drinking water and sanitation conditions are associated with the risk of malaria among children under five years old in sub-Saharan Africa: a logistic regression model analysis of national survey data. J Adv Res. 2020;21:1–13. doi: 10.1016/j.jare.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foster T. Predictors of sustainability for community-managed handpumps in sub-Saharan Africa: evidence from Liberia, Sierra Leone, and Uganda. Environ Sci Technol. 2013;47:12037–46. doi: 10.1021/es402086n. [DOI] [PubMed] [Google Scholar]
- 41.Semakula HM, Song G, Zhang S, Achuu SP. Potential of household environmental resources and practices in eliminating residual malaria transmission: a case study of Tanzania, Burundi, Malawi and Liberia. Afr Health Sci. 2015;15:819–27. doi: 10.4314/ahs.v15i3.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malaria entomology and vector control. [https://apps.who.int/iris/bitstream/handle/10665/85890/9789241505819_eng.pdf%3Bjsessionid%3D499D39C26B9EE5E5E260FF9D10DD6492%3Fsequence%3D1(Accessed on April 30, 2021)].
- 43.Ministry of Petroleum and Natural Gas. Official Website of PradhanMantriUjjwalaYojana. [http://www.pmujjwalayojana.com/ (Accessed on April 30, 2021)].
- 44.Times of India. [https://timesofindia.indiatimes.com/india/pm-modi-10-crore-lpg-connections-given-in-4-years-against-13-crore-in-6-decades/articleshow/64350785.cms (August 2, 2018, date last accessed)].
- 45.Sharma VP. Malaria and poverty in India. Curr Sci. 2003;84:513–5. [Google Scholar]
- 46.Worrall E, Basu S, Hanson K. Is malaria a disease of poverty? A review of the literature. Trop Med Int Health. 2005;10:1047–59. doi: 10.1111/j.1365-3156.2005.01476.x. [DOI] [PubMed] [Google Scholar]
- 47.Amegah AK, Damptey OK, Sarpong GA, Duah E, Vervoorn DJ, Jaakkola JJ. Malaria infection, poor nutrition and indoor air pollution mediate socioeconomic differences in adverse pregnancy outcomes in Cape Coast, Ghana. PLoS One. 2013;8:e69181. doi: 10.1371/journal.pone.0069181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Somi MF, Butler JR, Vahid F, Njau J, Kachur SP, Abdulla S. Is there evidence for dual causation between malaria and socioeconomic status? Findings from rural Tanzania. Am J Trop Med Hyg. 2007;77:1020–7. doi: 10.4269/ajtmh.2007.77.1020. [DOI] [PubMed] [Google Scholar]
- 49.Asif AM, Tahir MR, Arshad IA. Socioeconomic condition and prevalence of malaria fever in Pakistani children: findings from a community health survey. J Trop Pediatr. 2018;64:189–94. doi: 10.1093/tropej/fmx047. [DOI] [PubMed] [Google Scholar]
- 50.Tusting LS, Rek JC, Arinaitwe E, Staedke SG, Kamya MR, Bottomley C, et al. Measuring socioeconomic inequalities in relation to malaria risk: a comparison of metrics in rural Uganda. Am J Trop Med Hyg. 2016;94:650–8. doi: 10.4269/ajtmh.15-0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woyessa A, Deressa W, Ali A, Lindtjorn B. Malaria risk factors in Butajira area, south-central Ethiopia: a multilevel analysis. Malar J. 2013;12:273. doi: 10.1186/1475-2875-12-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ernst KC, Lindblade KA, Koech D, Sumba PO, Kuwuor DO, John CC, et al. Environmental, socio-demographic and behavioural determinants of malaria risk in the western Kenyan highlands: a case-control study. Trop Med Int Health. 2009;14:1258–65. doi: 10.1111/j.1365-3156.2009.02370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.