In the last year, a growing number of articles addressed coronavirus disease 2019 (COVID-19), including its link with gastrointestinal (GI) (dys)function. We here highlight the most important findings regarding the role of the gut in this disease, with a focus on critically ill patients.
Clinical GI features related to COVID-19
The reported prevalence of GI symptoms in COVID-19 patients is highly variable and ranges from 11–95%, potentially related to differences in study design, population and definition of GI symptoms (Table 1) [1]. In general, symptoms were mild and non-specific, and included nausea, vomiting, diarrhea, and abdominal pain [1]. Patients with initial GI symptoms more frequently had fever, constitutional symptoms, shortness of breath and body aches [2]. Likewise, the presence of GI symptoms has been associated with higher illness severity, reflected in a higher need for hospital admission, intensive care unit (ICU) admission and intubation, even after adjustment for demographics, comorbidities, and other clinical symptoms [2].
Table 1.
Clinical features of gastrointestinal dysfunction in critically ill patients with vs. without COVID-19
| COVID | Non-COVID | |
|---|---|---|
| GI symptoms | 11–95% (1,16–18) | 60% (19,20) |
| Diarrhea | 15–45% (16,21–23) | 3–78% (24) |
| Bowel paralysis/constipation | 39% (16) | 20–83% (24) |
| Nausea/vomiting | 11–64% (16,21,22) | 15–38% (19,20,25) |
| Large GRV | 10–83% (21,23) | 8–67% (26,27) |
| Abdominal distension | 38–67% (16,21) | 21–45% (20,26) |
| Feeding intolerance | 32–63% (18,21,22) | 2–75% (26–28) |
| Mesenteric ischemia | 2–3% (1,16) | 1–5% in patients with shock or burns (29–31) |
| Gastrointestinal failurea | 8–50% (17,18) | 6–26% (20,26,32,33) |
| Association of GI dysfunction with outcome | Independent association with mortality (18,21) | Independent association with mortality (20,26,32,33) |
Studies considerably varied with regard to study design, population and definition of GI symptoms
aGastrointestinal failure was defined as AGI grade (34) III/IV or presence of ≥ 3 concomitant GI symptoms
References from 16–34 are available in the Supplementary material
In critically ill patients in general, GI dysfunction is prevalent and independently associated with adverse outcome [3]. In one study in patients with acute respiratory distress syndrome (ARDS), COVID-19 ARDS compared to non-COVID ARDS was more commonly associated with potentially severe GI complications, and these complications included, among others, ileus and mesenteric ischemia [4]. Additionally, acute pancreatitis and severe intra-abdominal hypertension have been described in COVID-19 patients [1].
Importantly, GI symptoms may persist in a considerable number of patients. A 6-months follow-up in 1733 patients hospitalized with COVID-19 revealed decreased appetite in 8%, and diarrhea or vomiting in 5% of discharged patients [5].
Pathophysiology
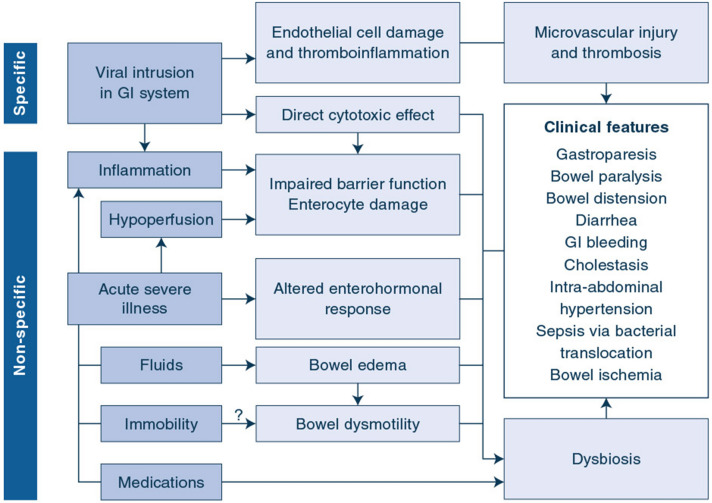
In critically ill COVID-19 patients, the GI tract may be affected directly by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) although GI dysfunction may also be related to critical illness, and its associated systemic inflammation and treatments (Fig. 1).
Fig. 1.
Pathophysiological mechanisms of gastrointestinal dysfunction in critically ill patients with COVID-19
Cytotoxic enterocyte injury
Evidence suggests a cytotoxic effect of SARS-CoV-2 on enterocytes. Indeed, enterocytes express both the ACE2 receptor and TMPRSS2, required for intracellular entry of SARS-CoV-2, and cells were rapidly infected in a human small intestinal organoid model, producing infectious virion [1]. SARS-CoV-2 RNA and intracytoplasmatic viral proteins have been observed in biopsies from different parts of the GI tract, supporting viral intrusion in vivo [6, 7]. SARS-CoV-2 RNA was also found in feces of more than half of studied COVID-19 patients, yet without a clear association with GI symptoms [6, 7]. Observed pathomorphological features include infiltration of plasma cells and lymphocytes in the lamina propria in different parts of the GI tract (Supplementary reference).
Microvascular injury and thromboinflammation
Numerous studies have indicated a substantial activation of coagulation in COVID-19 patients, with a significantly elevated risk of thrombosis in various organs, including the lung and GI tract [4, 8]. Activation of coagulation is potentially related to endothelial injury. Indeed, in postmortem lung biopsies, a prominent pathophysiological feature of COVID-19 was pulmonary endothelial injury associated with the presence of intracellular SARS-CoV-2, and accompanied by inflammation, microvascular thrombosis and angiogenesis [9]. Similar endotheliitis and inflammatory cell death has been identified in intestinal biopsies of patients who died of COVID-19 or who underwent bowel resection because of mesenteric ischemia [10, 11].
Non-specific critical illness-related GI dysfunction
All etiological factors leading to GI dysfunction in non-COVID patients are also important in critically ill COVID patients, including systemic inflammation, hypoperfusion, and frequently administered drugs such as opioids (Fig. 1). Critically ill COVID-19 patients often require deep sedation and neuromuscular blockade, leading to prolonged immobility, which may contribute to bowel dysmotility and paralysis. Moreover, prone position is not necessarily optimal with regard to enteral feeding tolerance. However, although data are limited, prone positioning is not considered a contraindication for enteral nutrition [12].
Recently, an important role of the microbiome has been suggested for a considerable number of diseases, including COVID-19 (Supplementary references). Indeed, COVID-19 patients were found to have significantly reduced bacterial diversity, with a reduction in bacteria with known immunomodulatory potential and relative increases in opportunistic pathogens (Supplementary references). Alterations in the microbiome were found to be related to COVID-19 severity and biochemical markers of inflammation, whereas changes at species level were not associated with fecal viral load (Supplementary reference). However, an observational study reported that the reduced bacterial diversity was less pronounced in COVID-19 patients compared to patients with H1N1 influenza, although it is not clear if patients were sufficiently matched for illness severity (Supplementary reference). Future studies should further elucidate the role of the microbiome in relation to disease severity.
Bacterial translocation due to gut barrier failure is a hypothetical mechanism of sustaining multiple organ failure in critical illness, however, with very limited and circumstantial data [3]. A matched case-cohort study reported higher incidence of ICU-acquired bloodstream infections in COVID-19 vs. non-COVID patients, which were more frequently of unknown source [13].
GI dysfunction in severe COVID-19 vs. other critical illnesses
It remains unclear whether COVID-19-associated GI dysfunction substantially differs from GI dysfunction observed in other critical conditions, since there are many similarities regarding pathophysiological mechanisms, concomitant factors and clinical manifestations (Fig. 1, Table 1). In this regard, experts have recommended similar risk assessment, medical and nutritional management as in non-COVID patients with GI dysfunction [14].
Additionally, there is no solid evidence whether COVID-19-specific treatments impact on GI dysfunction. Selected randomized controlled trials demonstrating survival benefit by administration of corticosteroids and IL-6 receptor antagonists have not reported on GI manifestations. Additionally, data on the impact of antiviral treatment and anticoagulation on GI dysfunction are lacking, and data on nutritional support are limited.
The overwhelming urgency of the COVID-19 pandemic has led to many publications and various hypotheses based on limited evidence [15] with an overall quality that is below the pre-pandemic level (Supplementary reference). Data on the role of GI tract in COVID-19 are no exception, calling for the need for well conducted studies addressing this important topic. Future mechanistic studies should further elucidate pathophysiological mechanisms, and clinical studies should assess the impact of COVID-19-specific treatments on GI complications in relation to outcome, as well as the ideal feeding strategy. Such studies will be essential for making definitive statements and suggesting any specific treatment.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All the authors contributed equally to the concept, assessment of literature and writing of the manuscript.
Funding
ARB holds a grant from Estonian Research Council (PRG1255). JG holds a postdoctoral research fellowship granted by the University Hospitals Leuven.
Availability of data and material
Not applicable
Code availability
Not applicable
Declarations
Conflicts of interest
ARB received speaker fees from Fresenius Kabi and Nestlé and consulting fee from VIPUN Medical. University of Tartu received a study grant form Fresenius Kabi. KU Leuven received fees from VIPUN Medical for consultancy by JG. YMA reports no relevant COI.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kariyawasam JC, Jayarajah U, Riza R, Abeysuriya V, Seneviratne SL. Gastrointestinal manifestations in COVID-19. Trans R Soc Trop Med Hyg. 2021 doi: 10.1093/trstmh/trab042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bishehsari F, Adnan D, Deshmukh A, Khan SR, Rempert T, Dhana K, Mahdavinia M. Gastrointestinal symptoms predict the outcomes from COVID-19 infection. J Clin Gastroenterol. 2021 doi: 10.1097/MCG.0000000000001513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reintam Blaser A, Preiser JC, Fruhwald S, Wilmer A, Wernerman J, Benstoem C, Casaer MP, Starkopf J, van Zanten A, Rooyackers O, Jakob SM, Loudet CI, Bear DE, Elke G, Kott M, Lautenschläger I, Schäper J, Gunst J, Stoppe C, Nobile L, Fuhrmann V, Berger MM, Oudemans-van Straaten HM, Arabi YM, Deane AM, Working Group on Gastrointestinal Function within the Section of Metabolism, Endocrinology and Nutrition (MEN Section) of ESICM Gastrointestinal dysfunction in the critically ill: a systematic scoping review and research agenda proposed by the Section of Metabolism, Endocrinology and Nutrition of the European Society of Intensive Care Medicine. Crit Care. 2020;24(1):224. doi: 10.1186/s13054-020-02889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El Moheb M, Naar L, Christensen MA, Kapoen C, Maurer LR, Farhat M, Kaafarani HMA. Gastrointestinal complications in critically ill patients with and without COVID-19. JAMA. 2020;324(18):1899–1901. doi: 10.1001/jama.2020.19400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Li Y, Xie W, Cui D, Shang L, Fan G, Xu J, Wang G, Wang Y, Zhong J, Wang C, Wang J, Zhang D, Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deinhardt-Emmer S, Wittschieber D, Sanft J, Kleemann S, Elschner S, Haupt KF, Vau V, Häring C, Rödel J, Henke A, Ehrhardt C, Bauer M, Philipp M, Gaßler N, Nietzsche S, Löffler B, Mall G. Early postmortem mapping of SARS-CoV-2 RNA in patients with COVID-19 and the correlation with tissue damage. Elife. 2021;10:e60361. doi: 10.7554/eLife.60361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–3.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, Merdji H, Clere-Jehl R, Schenck M, Fagot Gandet F, Fafi-Kremer S, Castelain V, Schneider F, Grunebaum L, Anglés-Cano E, Sattler L, Mertes PM, Meziani F, CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis) High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stahl K, Bräsen JH, Hoeper MM, David S. Direct evidence of SARS-CoV-2 in gut endothelium. Intensive Care Med. 2020;46(11):2081–2082. doi: 10.1007/s00134-020-06237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reintam Blaser A, Starkopf J, Alhazzani W, Berger MM, Casaer MP, Deane AM, Fruhwald S, Hiesmayr M, Ichai C, Jakob SM, Loudet CI, Malbrain ML, Montejo González JC, Paugam-Burtz C, Poeze M, Preiser JC, Singer P, van Zanten AR, De Waele J, Wendon J, Wernerman J, Whitehouse T, Wilmer A, Oudemans-van Straaten HM, ESICM Working Group on Gastrointestinal Function Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2017;43(3):380–398. doi: 10.1007/s00134-016-4665-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buetti N, Ruckly S, de Montmollin E, Reignier J, Terzi N, Cohen Y, Siami S, Dupuis C, Timsit JF. COVID-19 increased the risk of ICU-acquired bloodstream infections: a case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med. 2021;47(2):180–187. doi: 10.1007/s00134-021-06346-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, Pirlich M, Singer P, endorsed by the ESPEN Council, ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020;39(6):1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salluh JIF, Arabi YM, Binnie A. COVID-19 research in critical care: the good, the bad, and the ugly. Intensive Care Med. 2021;47(4):470–472. doi: 10.1007/s00134-021-06367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable
Not applicable