Abstract
Covid 19 infection can result in various opportunistic infections. Altered immune response, associated comorbid conditions like diabetes, prolonged steroid and broad spectrum antibiotics usage with ICU interventions lead to increased chance of such superadded infections in covid 19 patients. Here we report a case of 31 year old male with covid 19 infection who had new onset Diabetes Mellitus, developed severe acute fulminant Mucormycosis during the treatment for covid 19 infection. He presented with severe headache, nasal obstruction and discharge, bilateral ophthalmoplegia and blindness with Cavernous Sinus Thrombosis. Patient underwent aggressive surgical debridement with frontal craniectomy, maxillectomy and right orbital evisceration and left endoscopic orbital decompression and judicious efforts to revert back the immunocompromised status with high dose of Liposomal amphotericin. Post operatively patient developed right temporal lobe abscess which was drained through Endonasal Endoscopic Trans Cavernous drainage of Temporal Lobe Abscess. Patient is in 2 months follow up, with bilateral blindness and tolerating oral feeds with improved left eye ophthalmoplegia. It is imperative to note that the rising trend of mucormycosis is there in Covid 19 infections and it should be dealt with high index of suspicion in high risk patients and early aggressive treatment can save the patient as the survival rate is not high in such infections.
Keywords: Rhino orbito cerebral mucormycosis, Covid 19 infection, Corona virus SARS-CoV-2, Cavernous sinus thrombosis, Ophthalmoplegia, Frontal craniectomy, Osteomyelitis
Introduction
Mucormycosis is a debilitating opportunistic invasive fungal infection that is often seen in immunocompromised patients. It is caused by fungus of class Zygomycetes which is an ubiquitous organism [1]. It is observed that there is an upsurge of Rhino Orbito Cerebral Mucormycosis(ROCM) in the Covid 19 pandemic [2]. Covid 19 infection caused by novel corona virus SARS-CoV-2 was announced as a pandemic by the WHO in March 2020. Since then, the infection has confronted the medical healthcare system with unprecedented challenges and caused crisis situation all over the world. The virus causes mild to severe pneumonia with high infectivity rate. It contributed to high morbidity and mortality all around the globe. Elderly patient with comorbid conditions like Diabetes or Lung diseases are more prone to develop treacherous complications. New evidences are emerging on the impact of viral infection on the human body. Recent reports point out to increasing occurrence of ROCM in patient suffering from Covid 19.This case report emphasizes about a 31 year old newly diagnosed Diabetes with Covid 19 infection who developed an acute fulminant invasive ROCM, the rare case scenario and its management are discussed.
Case Report
A 31 year old healthy male with no known comorbidity was diagnosed with novel Covid 19 infection (RT-PCR positive) and was treated with Antivirals and Steroids in a primary health centre. During the course of treatment, he developed right eye ptosis with chemosis and right facial paraesthesia. He was referred to higher centre for further management where he developed bilateral proptosis, loss of vision and ophthalmoplegia. Investigations revealed hyperglycaemia and his HbA1c was 6.1. Repeat RT-PCR for Covid 19 was found positive. Other laboratory investigations and serological tests were normal. MRI Brain with contrast done showed features consistent with invasive fungal sinusitis involving maxillary, ethmoid and sphenoid sinus on right side. CT Orbit with contrast showed mild thickening of the right medial, superior and inferior recti muscles with subtle retrobulbar fat stranding, likely inflammation. Patient was then started on intravenous Antifungals.
Patient’s condition deteriorated due to rapid progression of disease. CT PNS and Brain showed right sided chronic maxillary sinusitis, mixed sclerotic/lytic areas involving both frontal bones probably osteomyelitis,bilateral ethmoid, frontal and sphenoid sinusitis. Patient underwent Endoscopic endonasal debridement with Left orbital decompression with Right eye evisceration with all precautionary measures taken for covid 19 infection. Fungal stain showed many aseptate broad ribbon like hyphae. HPE showed sinus mucosa with chronic inflammation and necrosis with invasive Fungal hyphae morphology resembling Mucorales. MRI Brain post surgery showed postoperative changes in the paranasal sinuses, pthisisbulbi in right eye, diffuse swelling of the cavernous sinus suggesting fungal invasion with thrombosis, diffuse thrombosis with complete obstruction of Right internal carotid artery, diffuse erosion of the frontal bone with underlying meningeal thickening.
Patient was referred to our hospital with persistent complaints of headache, fever and nose block. On examination he was conscious and oriented, vitals were stable. Right pthisis bulbi present. Left eye proptosis with ophthalmoplegia and loss of vision. Repeat RTPCR for Covid was negative.
CT Brain with Paranasal sinuses Plain with contrast showed mucosal thickening in bilateral maxillary, frontal, ethmoid and sphenoid sinuses. Peripherally enhancing soft tissue densities are seen extending from the bilateral maxillary sinus and nasal cavities into the medial portion of the corresponding orbits. Pthisis bulbi of the right eyeball. Right cavernous sinus thrombosis with right internal carotid artery thrombosis (Fig. 1) CT PNS with 3d reconstruction showed postoperative changes and new ill-defined lytic lesions with intermittent destruction of the bones are seen involving the wall of the bilateral maxillary, ethmoid, frontal and sphenoid sinuses (Fig. 2).
Fig. 1.
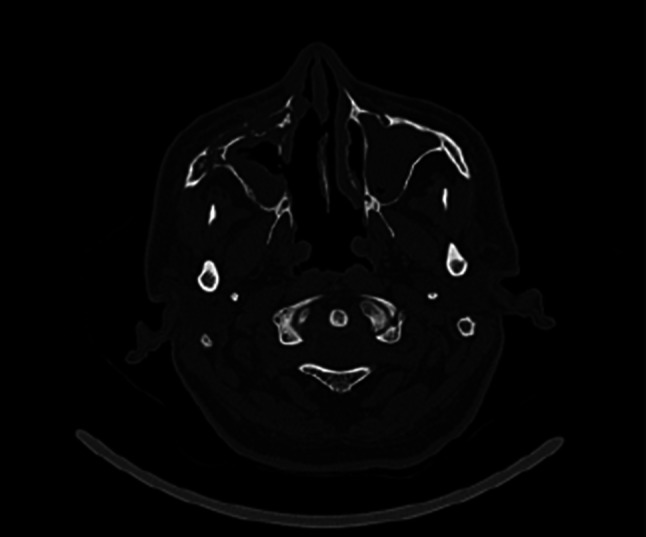
Postoperative changes in the walls of right maxillary sinus and right nasal cavity With mucosal thickening in bilateral maxillary sinus
Fig. 2.

CT with 3D Reconstruction: Ill-defined lytic and sclerotic area with intermittent areas of bone destruction involving bilateral paranasal sinuses and maxilla, right frontal bone, orbit and zygoma
Patient was started on Liposomal Amphotericin B injection. High risk consent was obtained in view of acute fulminant fungal infiltration with intracranial extension and postoperative neurological complications. He underwent Endoscopic and external debridement of Nose and Paranasal sinuses and Orbit with Transoral Bilateral Maxillectomy and Right Frontal craniectomy with Debridement and repair with Titanium mesh. (Figures. 3, 4) HPE showed features consistent with Mucormycosis and negative for Aspergillosis. Inj. Liposomal Amphotericin was continued. Pus culture from nasal cavity showed multidrug resistant Pseudomonas aeruginosa for which he was started on Polymixin B injection.
Fig. 3.
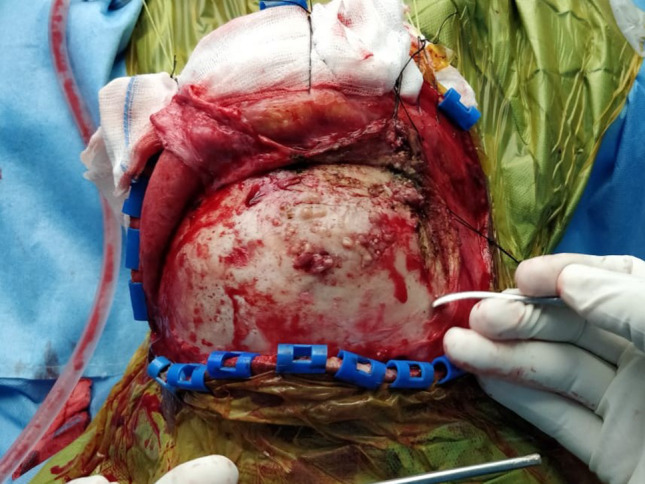
Intraoperative picture showing necrosis and osteomyelitis of right frontal bone
Fig. 4.
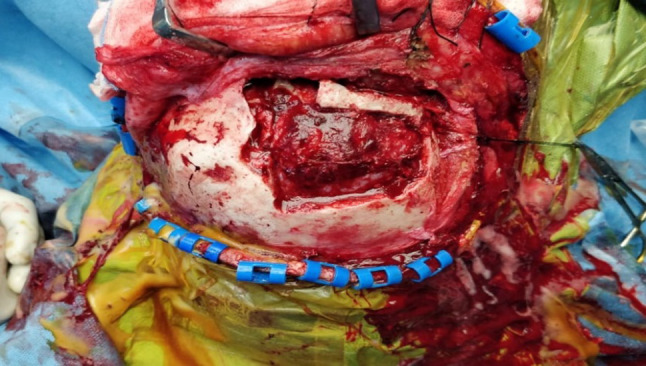
Intraoperative picture showing right frontal craniectomy with external debridement of bilateral frontal sinus
He had persistent hypomagnesemia and hypokalemia throughout the course of stay and were treated accordingly. Renal function test monitored on alternate days. Ophthalmologist advised oculoplasty on a later date. Under endoscopic vision, wound debridement of the oral and nasal cavity was done periodically. Total cumulative dose of 3000 mg of liposomal amphotericin B was given. Patient was then treated with oral Posaconazole. Prosthodontist opinion obtained for obturator fixation. Patient was started on orals after obturator fixation. Postoperatively MRI Brain with contrast done showed bilateral cavernous sionus thrombosis. Complete thrombosis of the cavernous segment of right internal carotid artery and the Circle of Willis anastomosis was found well developed which prevented hemiplegia and a well defined ring enhancing lesion in the right anterior temporal lobe suggestive of cerebral abscess were noted. Patient was referred to neurosurgery department and underwent Endonasal Endoscopic Trans Cavernous drainage of Temporal Lobe Abscess using Navigation.
Patient is on regular follow up for past one month and is presently doing well without any focal neurological deficit. There is no vision in both the eyes. Right eye Pthisis bulbi and Ophthalmoplegia in left eye is improved. Patient is tolerating oral feeds well with permanent obturator in place (Figs. 5, 6).
Fig. 5.
Postoperative image of patient with Obturator in place
Fig. 6.

Postoperative image of bilateral transoral maxillectomy after one month without Obturator
Discussion
Mucormycosis is caused by fungus belonging to order Mucorales, an ubiquitous fungi that are aseptate molds with irregular branching pattern [1]. It is common in immunocompromised patients. The most common organisms are Rhizopus, Mucor and Rhizimucor. These fungi produce numerous spores in the environment thar are inhaled by the hosts. In immunocompetent hosts, they are pushed towards the pharynx by mucociliary system and terminated through gastrointestinal system.
They are unique in causing severe angioinvasion with necrosis of the tissues leading to complications in immunocompromised patients like diabetic ketoacidosis and patients on steroid therapy [3]. The ketone reductase system in Zygomycetes help in the survival of the fungi in diabetic ketoacidosis patient. The impaired phagocytosis and increased free iron availability in the blood of the diabetic patients provide good support for the progression of the disease in these patients [3].
Diabetes Mellitus is also an important risk factor for developing covid 19 infection. Covid 19 was first described in Wuhan in December 2019. It has caused severe impact to the health care system. Patients infected with theSars-cov-2 present with respiratory illness that can progress to cause acute respiratory distress syndrome(ARDS). Patients are treated with antiviral Remdisivir and Steroids to counteract the effect of the virus and the inflammatory injury caused by the immune system. Clexane are added in patients with increased D Dimer to alleviate the formation of thrombi in the lungs [4]. Prolonged high dose steroid usage in such patients increases the risk of developing Mucormycosis. The tendency of Covid 19 to form thrombi further enhances the iron availability to the fungus which enhances the growth of the organism. Increased Serum Ferritin and decreased iron binding capacity of transferrin in ketoacidotic status of diabetic patient with coexisting Covid 19 infection can contribute the iron needed for the growth of the zygomycetes [3]. Patients infected with Sars-CoV-2 also have superadded bacterial and fungal infections due to the impaired immune system. This adds on to the morbidity and mortality in such patients.
This case has been reported for the occurrence of acute fulminant Rhino Orbital Cerebral Mucormycosis in a covid 19 patient who was incidentally noted to have a brief perod of hyperglycemia and also for the dramatic presenting clinical features of Bilateral cavernous sinus thrombosis, Ophthalmoplegia, Bilateral loss of vision, Right internal carotid artery thrombosis with no specific CNS manifestations due to adequate collateral circulation that had developed.
Various reports mention about the opportunistic infections in the patients having viral pneumonia especially with co morbidities like Diabetes and pre existing lung pathology. Chen et al. reported 5% of fungal culture positive infection in a study of 99 patients with covid 19 infection, and the organisms being Candida and Aspergillosis [5]. Michelle Bartoletti identified that 27.7% of patients treated in the intensive care unit with Covid 19 infection developed CAPA- Corona virus Associated Pulmonary Aspergillosis [6]. Cornely OA et al. reported that there is increased chance to develop Mucormycosis in diabetes patients infected with corona virus [7].
In 2003, during the SARS infection by Sars-CoV-1 it is reported that opportunistic fungal infections by Candida, Mucorales, Aspergillosis or Cryptococcus have caused considerable morbidity and mortality. Zhang et al. reported that superadded fungal infections had incidence of 14.8–27% [8]. Li CS and Pan SF reported that opportunistic fungal infection accounted for 25–73.7%of mortality during 2003 SARS [9].
The clinical presentation of Mucormycosis are non-specific headache with nasal block, purulent discharge with epistaxis, numbness over the face. The disease can spread rapidly by angioinvasion and direct bone erosion to the orbit and the brain. Ophthalmoplegia with loss of vision will ensue with involvement of Cavernous Sinus and cranial nerve palsies and finally lead to coma and death. The timely establishment of anastomosis in the Circle of Willis is very essential. Failure of this anastomosis may have caused hemiplegia in this patient as there was complete obliteration of Internal Carotid Artery in the Cavernous sinus. The involvement of the cavernous sinus with multiple cranial nerve palsies caused severe debilitation to the patient and vigilant action was taken and extensive surgical debridement was carried out to save the patient. Survival rate of such patients with diabetes is only 47% as observed by Yoav P Talmi et al.[10]
Radiological investigation make an invaluable contribution in the management of Mucormycosis. CT provide the bony erosions and the spread of the disease whereas MRI enumerates the intra orbital and intra cranial involvement [11]. Prompt surgical debridement with high dose of Amphotericin and judicious efforts to reverse the immunosuppressed state is prudent in the management. There is rising trend of ROCM with Covid 19 and it is imperative for the medical fraternity to make an early diagnosis in suspicious patients which will enhance the chance of survival and prevent gross morbidity in such patients.
Conclusion
Covid 19 associated ROCM is being reported with increasing frequency. Altered immune system with increased availability of iron in these patients especially when associated with Diabetes mellitus predispose to the flaring up of Mucormycosis.
With the second wave of Covid 19 infection in the rise, a high index of suspicion towards ROCM needed when managing Covid 19 patient with persistent signs and symptoms of nasal inflammation.
This case report highlights the unique presentation of rapidly spreading ROCM in a young patient with severe complication of bilateral Cavernous Sinus thrombosis leading to blindness and also enumerates the associated factors for the development of Mucor in Covid 19 patients.
Funding
None.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sudhagar Eswaran, Email: sudhagar@sriramachandra.edu.in.
Sarath Kumar Balan, Email: sarathkumarbalan@gmail.com.
Prasanna Kumar Saravanam, Email: sprasannakumar10@gmail.com.
References
- 1.Goldstein EJ, Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J, Jr, Ibrahim AS. Recent advances in the management of mucormycosis: from bench to bedside. Clin Infect Dis. 2009;48(12):1743–1751. doi: 10.1086/599105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song G, Liang G, Liu W. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia. 2020;31:1–8. doi: 10.1007/s11046-020-00462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rammaert B, Lanternier F, Poirée S, Kania R, Lortholary O. Diabetes and mucormycosis: a complex interplay. Diabetes Metab. 2012;38(3):193–204. doi: 10.1016/j.diabet.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Lamontagne F, Agoritsas T, Macdonald H, Leo YS, Diaz J, Agarwal A, Appiah JA, Arabi Y, Blumberg L, Calfee CS, Cao B. A living WHO guideline on drugs for covid- BMJ. 2020;4:370. doi: 10.1136/bmj.m3379. [DOI] [PubMed] [Google Scholar]
- 5.Antinori S, Galimberti L, Milazzo L, Ridolfo AL. Bacterial and fungal infections among patients with SARS-CoV-2 pneumonia. Hospitals. 2020;85(77):90–96. [PubMed] [Google Scholar]
- 6.Bartoletti M, Pascale R, Cricca M, Rinaldi M, Maccaro A, Bussini L, Fornaro G, Tonetti T, Pizzilli G, Francalanci E, Giuntoli L. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SC, Dannaoui E, Hochhegger B, Hoenigl M, Jensen HE, Lagrou K, Lewis RE, Mellinghoff SC. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European confederation of medical mycology in cooperation with the mycoses study group education and research consortium. Lancet Infect Dis. 2019;19(12):e405–e421. doi: 10.1016/S1473-3099(19)30312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Li WX, Huang KW, Cao ZX, Hao JY. Hospital acquired pneumonia occurring after acute stage of the serious SARS and its treating strategies. Chin J Nosocomiol. 2003;11(13):1081–1087. [Google Scholar]
- 9.Li CS, Pan SF (2003) Analysis and causation discussion of 185 severe acute respiratory syndrome dead cases. Zhongguo wei zhong bing ji jiu yi xue= Chinese critical care medicine= Zhongguo weizhongbing jijiuyixue, 15(10): 582–4. [PubMed]
- 10.Talmi YP, Goldschmied-Reouven A, Bakon M, Barshack I, Wolf M, Horowitz Z, Berkowicz M, Keller N, Kronenberg J. Rhino-orbital and rhino-orbito-cerebral mucormycosis. Otolaryngology-Head and Neck Surgery. 2002;127(1):22–31. doi: 10.1067/mhn.2002.126587. [DOI] [PubMed] [Google Scholar]
- 11.Herrera DA, Dublin AB, Ormsby EL, Aminpour S, Howell LP. Imaging findings of rhinocerebral mucormycosis. Skull Base. 2009;19(2):117. doi: 10.1055/s-0028-1096209. [DOI] [PMC free article] [PubMed] [Google Scholar]



