Background:
There is interest in hallux valgus deformity correction using internal fixation with the minimally invasive chevron and Akin osteotomies (MICA) technique. The objective of this study was to assess the correction measured on postoperative radiographs and clinical outcomes, using validated outcome measures, at 2 years following third-generation MICA.
Methods:
This is a prospective single-surgeon case series of 333 consecutive feet that underwent MICA surgery between July 2014 and April 2018. The primary clinical outcome measures included the Manchester-Oxford Foot Questionnaire (MOXFQ), EuroQol-5 Dimensions-5 Level (EQ-5D-5L) Index, EuroQol-visual analogue scale (EQ-VAS), and a VAS for pain (VAS-pain). Secondary outcome measures included radiographic parameters and complication rates.
Results:
Preoperative and 2-year postoperative patient-reported outcome measures (PROMs) were collected for 292 feet (87.7%). At a minimum 2-year follow-up, the MOXFQ scores (mean ± standard deviation [SD]) had improved in each domain—i.e., reduced from 44.5 ± 21.0 preoperatively to 9.4 ± 15.8 postoperatively for pain (p < 0.001), from 38.7 ± 23.4 to 6.5 ± 14.6 for walking and standing (p < 0.001), and from 48.0 ± 22.3 to 6.6 ± 13.5 for social interaction (p < 0.001). The VAS-pain score improved from 31.4 ± 22.7 preoperatively to 8.4 ± 16.4 at the 2-year follow-up (p < 0.001), the 1-2 intermetatarsal angle was reduced from 15.3° ± 3.6° preoperatively to 5.7° ± 3.2° at the 2-year follow-up (p < 0.001), and the hallux valgus angle was reduced from 32.9° ± 10.2° to 8.7° ± 5.2° (p < 0.001).
Conclusions:
The third-generation MICA provided significant improvement in clinical outcome measures at the 2-year follow-up and can be successfully used for correction of a range of hallux valgus deformities with a low rate of symptomatic recurrence.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Minimally invasive surgery (MIS) for hallux valgus has clinical and radiographic outcomes comparable with those of traditional open osteotomy approaches1-3.
Third-generation MIS for hallux valgus involves screw fixation of a distal metatarsal osteotomy site, resulting in greater stability than is provided by previous generations of the technique4,5. The MIS procedure has a learning curve of approximately 20 to 50 cases6,7. Advocates suggest that once technical proficiency has been achieved, potential benefits include reduced operative time, reduced morbidity, smaller scars, and quicker recovery compared with traditional open procedures1-3,8,9.
Previous studies of third-generation MIS have demonstrated improved clinical and radiographic outcomes for a wide range of hallux valgus deformities8-16. These studies are limited in number and consist of case series with small sample sizes, short follow-up, unvalidated outcomes, inconsistent techniques, and a high risk of bias. There is also substantial variability in the reporting of complications, with rates ranging from 0% to 42%1,2. There is a need for evidence based on validated patient-reported outcome measures (PROMs) to assess third-generation MIS for hallux valgus. Thus, the aim of the present study was to measure the change in PROMs at 2 years, assess deformity correction on radiographs made in the immediate postoperative period, and report the prevalence of complications following third-generation minimally invasive chevron and Akin osteotomies (MICA) for hallux valgus.
Materials and Methods
Third-Generation MICA Technique
The surgical technique was adapted as described by Redfern and Vernois8 and was similar for all cases. An extra-articular chevron osteotomy was made through a percutaneous incision at the metatarsal neck. Following displacement of the metatarsal head, the osteotomy site was fixed with 2 parallel screws. Medial ledge excision was performed, and any prominent medial exostosis were excised. A percutaneous Akin osteotomy and a lateral release of the first metatarsophalangeal joint (involving division of the lateral sesamoid-phalangeal ligament) were only performed if required to fully correct the hallux valgus deformity and restore first metatarsophalangeal joint congruity. Patients were allowed full weight-bearing in a flat rigid sandal immediately and were discharged the same day.
Study Design
This study was a prospective observational single-surgeon case series of consecutive patients.
Participants
Consecutive patients ≥16 years of age who underwent primary correction of hallux valgus (of any deformity severity) were included. Patients who underwent additional forefoot procedures—e.g., hammer-toe correction or distal metaphyseal metatarsal osteotomy—were included, but those who previously had hallux valgus surgery or had degenerative joint disease of the first ray were excluded.
Indications for MICA
Clinical judgment was used to decide on the indication for surgery. Symptoms included discomfort/pain in the medial eminence in footwear, transfer metatarsalgia, and/or symptomatic lesser-toe deformities associated with hallux valgus.
Data Collection
Each patient completed preoperative PROMs using a tablet device, remotely connected to PROM software (Amplitude Clinical Outcomes), during their first consultation. The PROMs were specifically designed for electronic completion by patients. Procedure data and intraoperative and/or postoperative complication data were inputted prospectively by the senior author (D.J.G.). The software automatically sent patients PROM questionnaires via email 2 years following the surgery. Those who did not complete these 2-year postoperative PROMs were contacted again via email and/or by telephone to prompt them to do so.
Outcome Measures and Study End Point
The clinical PROMs assessed were the EuroQol-5 Dimensions-5 Level (EQ-5D-5L) Index, EuroQol visual analogue scale (EQ-VAS), a VAS for pain (VAS-pain), and the Manchester-Oxford Foot Questionnaire (MOXFQ).
The EQ-5D-5L and EQ-VAS are validated quality-of-life assessment measures. The VAS-pain is a validated measure of acute and chronic pain17. The MOXFQ is a PROM used specifically for patients undergoing foot surgery and has been validated for assessment of those undergoing hallux valgus surgery18-20. The MOXFQ consists of 3 domains (walking and standing, social interaction [based on the patient’s self-consciousness regarding their feet/shoes as well as the overall impact on social, recreational, work, and other everyday activities], and pain), with the score in each domain ranging from 0 (best possible score) to 100 (worst possible score). An overall summary “index” score was also calculated21. A detailed explanation of the MOXFQ can be found in the Appendix. The minimal clinically important difference (MCID) has been shown to be 16, 12, and 24 for the walking and standing, pain, and social interaction domains, respectively19.
Preoperative and 6-week postoperative weight-bearing radiographs were obtained to quantify preoperative and postoperative deformity correction (not recurrence). Radiographic parameters were measured retrospectively for all patients, in February 2020, by 1 of 2 fellowship-trained consultant surgeons (1 of whom [D.J.G.] performed all of the procedures). The 1-2 intermetatarsal angle (IMA) and hallux valgus angle (HVA) were measured according to the American Orthopaedic Foot & Ankle Society technique and categorized with regard to deformity severity22,23.
Operations performed on both feet of the same patient were usually carried out consecutively; however, there were a number of simultaneous cases. Patients who underwent consecutive procedures completed a set of PROMs before each operation in order to accurately reflect their health status at that point in time. Simultaneous bilateral cases were included as independent observations, as the MOXFQ is foot-specific18.
We selected the minimum 2-year follow-up because the existing literature on the results of third-generation MICA at this time point is extremely limited and of variable quality.
Complications identified by either the patient or the surgeon in outpatient clinics were registered on electronic PROM software at the point of diagnosis. We modified the Adapted Clavien-Dindo-Sink complication classification24,25 for hallux valgus surgery (Table I) and categorized all complications following a retrospective case review. Complication data were routinely collected for all patients until discharge from follow up (usually 6 months following surgery) and, beyond this, complication data were identified only if the patient reported it.
TABLE I.
Adverse Events and Complications Following Third-Generation MICA
| Grade/Description of Complication | No. of Cases | % of Cases (95% CI) |
| Grade I: adverse event with minimal clinical relevance that causes no deviation from routine follow-up during the postoperative period. Therapeutic regimens include analgesia, antibiotics, and physiotherapy. Complications include: | 25 | 7.5 (4.7, 10.3) |
| Delayed wound-healing | 2 | 0.6 |
| Superficial cellulitis (requiring oral antibiotics) | 15 | 4.5 |
| Transient neurapraxia* | 3 | 0.9 |
| FHL tendon injury* | 5 | 1.5 |
| Grade II: complication that is treatable but does not require additional surgical intervention or an unplanned hospital admission. Complications include: | 20 | 6.0 (3.5, 8.6) |
| Additional intraoperative fixation (e.g., Kirschner wire, additional screw) | 6 | 1.8 |
| Symptomatic osteotomy site displacement* | 1 | 0.3 |
| Symptomatic delayed union* | 5 | 1.5 |
| Transfer metatarsalgia/sesamoid pain | 3 | 0.9 |
| Intraoperative conversion to open surgery | 2 | 0.6 |
| Symptomatic recurrence of hallux valgus deformity | 3 | 0.9 |
| Grade III: complication that is treatable and requires surgical intervention or an unplanned hospital admission. Complications include: | 26 | 7.8 (4.9 10.7) |
| Osteotomy site displacement: bone-screw interface failure (fracture/screw cutout) | 6 | 1.8 |
| Osteotomy site displacement: delayed union/malunion/nonunion | 4 | 1.2 |
| Symptomatic prominent screw(s) | 8 | 2.4 |
| Prominent bone | 4 | 1.2 |
| Deep infection requiring surgical debridement and washout | 4 | 1.2 |
| All-cause screw-removal rate | 21 | 6.3 (3.7, 8.9) |
Not requiring operative intervention.
Bias
The use of consecutive prospectively collected data reduced selection bias. The operating surgeon (D.J.G.) had performed approximately 100 MICA procedures before the start of this study, potentially reducing “learning curve errors.”7 These cases are not included in this report because electronic data collection methods did not commence until 2014. Due to a change in practice setting, it was not possible to follow these cases.
Blinding
The 2 authors (D.J.G. and R.R.) who performed the radiographic assessment and complication analysis were blinded to the PROM outcomes when doing so to reduce bias.
Statistical Analysis Including Calculation of Study Size
A post-hoc power analysis was performed, and sample size calculations were based on an independently established MOXFQ MCID following hallux valgus surgery19. A sample of 208 feet was estimated to give a power of 0.99 and an alpha risk of 1%. A paired t test for parametric data and a Wilcoxon signed rank test for non-parametric data were used. All analyses were performed with the Python SciPy package26. Significance was defined as p < 0.05.
Associations between preoperative clinical and radiographic variables and the change in the 2-year MOXFQ index score compared with preoperatively were identified with a multivariable linear regression model built using ordinary least squares regression.
IDEAL Stage
This study followed Stage 2B of the IDEAL (Idea, Development, Exploration, Assessment, Long-term Follow-up) Framework27.
Ethical Approval
Local institutional review board approval was obtained, and all participants provided informed consent.
Results
Patient Demographics
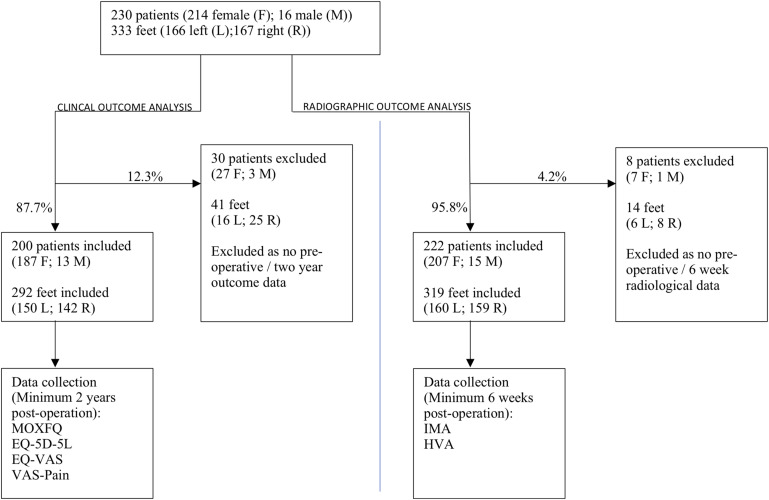
Between July 2014 and April 2018, 230 consecutive patients (214 female and 16 male) with a mean age of 55.0 years (range, 23.5 to 84.9 years; standard deviation [SD], 12.1 years) underwent primary MICA. A total of 333 feet (166 left and 167 right) were treated. Sixty-nine patients had the operation performed on both feet (a total of 138 feet; 41.4%) on the same day. Figure 1 demonstrates the participant flowchart for clinical and radiographic analysis.
Fig. 1.
A flowchart of patient participation in this study including the proportions analyzed for clinical and radiographic outcomes.
PROMs
Preoperative and 2-year PROMs were collected from 200 patients (187 female and 13 male) with 292 involved feet (150 left and 142 right). Thus, the PROM completion rate was 87.7% (292 of 333). The mean follow-up was 2.5 years (range, 2.0 to 5.5 years). A summary of the PROM scores is provided in Table II. There was a significant improvement that was greater than the MCID in each of the MOXFQ domains19. The quality-of-life assessment PROMs all improved significantly with the exception of the EQ-VAS.
TABLE II.
Preoperative and Minimum 24-Month Postoperative PROM Scores Following Third-Generation MICA*
| Outcome Measure | Preoperative Score | Postoperative Score | Change in Score | P Value | |||
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | 95% CI | ||
| MOXFQ | |||||||
| Walking and standing | 38.7 ± 23.4 | 39.0 (18.0-57.0) | 6.5 ± 14.6 | 0.0 (0.0-1.0) | −32.2 ± 25.5 | −33.7, −30.7 | <0.001 |
| Social interaction | 48.0 ± 22.3 | 50.0 (31.0-63.0) | 6.6 ± 13.5 | 0.0 (0.0-6.0) | −41.3 ± 24.7 | −42.8, −39.9 | <0.001 |
| Pain | 44.5 ± 21.0 | 45.0 (30.0-60.0) | 9.4 ± 15.8 | 0.0 (0.0-15.0) | −35.1 ± 23.7 | −36.5, −33.7 | <0.001 |
| Index | 42.8 ± 19.8 | 45.3 (26.8-58.4) | 7.4 ± 13.2 | 0.0 (0.0-7.8) | −35.4 ± 21.9 | −36.7, −34.1 | <0.001 |
| EQ-5D-5L Index | 0.75 ± 0.14 | 0.77 (0.71-0.84) | 0.90 ± 0.13 | 1.00 (0.84-1.00) | 0.17 ± 0.16 | 0.15, 0.18 | <0.001 |
| EQ-VAS | 83.5 ± 14.9 | 88.0 (79.0-92.0) | 84.2 ± 16.9 | 89.0 (80.0-95.0) | 0.8 ± 18.5 | −2.1, 0.5 | 0.563 |
| VAS-pain | 31.4 ± 22.7 | 27.0 (12.0-49.0) | 8.4 ± 16.4 | 1.0 (0.0-8.0) | −22.9 ± 26.4 | −24.7, −21.2 | <0.001 |
SD = standard deviation, IQR = interquartile range, CI = confidence interval, MOXFQ = Manchester-Oxford Foot Questionnaire, and VAS = visual analogue scale.
Radiographic Outcomes
Deformity correction was measured on preoperative and 6-week postoperative radiographs for 95.8% (319) of the feet (Fig. 2). There was a significant improvement in the IMA and HVA on the 6-week postoperative radiographs (Tables III and Tables IV). The maximum IMA correction was 21.2° (from 27.0° preoperatively to 5.8° at 6 weeks) while the maximum HVA correction was 51.3° (from 53.8° to 2.5°).
Fig. 2.
Radiographs made before (left) and 6 weeks (middle) and 6 months (right) after a third-generation MICA with screw fixation. The patient had union of the osteotomy site and resolution of soft-tissue swelling.
TABLE III.
Radiographic Hallux Valgus Deformity Categories
| Category* | No. (%) of Feet |
| Mild: HVA 15° to <20° and/or IMA 9° to <14° | 25 (7.8%) |
| Moderate: HVA 20° to <40° and/or IMA 14° to <20° | 209 (65.5%) |
| Severe: HVA ≥40° and/or IMA ≥20° | 85 (26.6%) |
| Total | 319 |
HVA = hallux valgus angle, and IMA = 1-2 intermetatarsal angle. When the HVA and IMA in the same patient did not fit into the same category, the more severe of the 2 angles was used to represent the severity of the deformity20.
TABLE IV.
Hallux Valgus Correction Data*
| IMA (deg) | HVA (deg) | |||||||
| Preop. | Postop. | Mean Deformity Correction | P Value | Preop. | Postop. | Mean Deformity Correction | P Value | |
| Mean ± SD | 15.3 ± 3.6 | 5.7 ± 3.2 | 9.6 ± 3.8 | <0.001 | 32.9 ± 10.2 | 8.7 ± 5.2 | 24.1 ± 9.7 | <0.001 |
| Minimum | 6.5 | −0.7 (valgus) | 8.6 | −4.1 (varus) | ||||
| Maximum | 27.0 | 18.1 | 63.9 | 32.1 | ||||
IMA = 1-2 intermetatarsal angle, HVA = hallux valgus angle, and SD = standard deviation,
Complications
The grades and rates of complications are shown in Table I. The rate of grade-2 and 3 complications combined was 13.8%, and the overall complication rate was 21.3% (95% confidence interval [CI] = 16.9% to 25.7%). The all-cause screw-removal rate was 6.3% (n = 21 feet). Three feet (0.9%) had clinical and radiographic evidence of recurrent hallux valgus following the MICA. One of these recurrences was due to undercorrection by the chevron osteotomy and failure of the Akin osteotomy screw due to cutout, the second was due to undercorrection by the chevron osteotomy, and the third was due to soft-tissue stretching over a prolonged period of time. One case of chevron screw cutout required revision MICA fixation.
Patients with postoperative displacement of the osteotomy site had ongoing clinical and radiographic follow-up until union occurred. Osteotomy site displacement occasionally resulted in metatarsal shortening (which was not measured) and/or minor loss of correction by the time of osseous union; however, none of these cases met the criteria for recurrence.
A grade-1 complication of note was flexor hallucis longus (FHL) tendon injury (prevalence = 1.5%); this may have occurred during the lateral release as the FHL may have displaced to a lateral position, which can happen particularly in cases with severe deformities. FHL tendon injury has not been commonly reported, which we believe is most likely due to the small case numbers previously published and the subtle clinical consequences of the complication. A recent cadaveric study from the Groupe de Recherche et d’Etude en Chirurgie Mini-Invasive du Pied (GRECMIP) showed 1 case of complete FHL tendon laceration in 22 feet28, supporting our suspicion that this complication is underreported in the literature.
There were no cases of osteonecrosis of the first metatarsal head or symptomatic dorsal or plantar malunion, although the study procedures were not designed to detect them. There were no clinically apparent deep vein thromboses or pulmonary emboli at any point during follow-up.
Multivariable Linear Regression Analysis
The results of the multivariable linear regression model are shown in Table V. We identified a ceiling effect of the MOXFQ index score at 2 years and therefore decided to utilize the 2-year change in MOXFQ index score compared with preoperatively as the outcome measure. The R2 of the model was 0.912. The only radiographic variable significantly associated with the change in the MOXFQ index score was the change in the HVA. Neither preoperative nor postoperative deformity as measured on radiographs was associated with the change in the MOXFQ index score. We also did not find an association between the EQ-5D PROMs and the change in the MOXFQ index score.
TABLE V.
Variables Included in Model and Calculated Coefficients to Predict Change in MOXFQ Index Score at 2 Years*
| Preop. Variable† | Coefficient | SE | Odds Ratio | 95% CI | P Value |
| MOXFQ | |||||
| Pain | 0.094 | 0.070 | 1.09 | 0.96-1.26 | 0.182 |
| Social interaction | 0.383 | 0.062 | 1.47 | 1.30-1.66 | <0.001 |
| Walking/standing | 0.454 | 0.071 | 1.57 | 1.37-1.81 | <0.001 |
| Radiographic deformity | |||||
| Preop. IMA | 0.338 | 0.203 | 1.40 | 0.94-2.09 | 0.098 |
| Preop. HVA | 0.022 | 0.086 | 1.02 | 0.86-1.21 | 0.796 |
| Postop. IMA | 0.049 | 0.211 | 1.05 | 0.69-1.59 | 0.818 |
| Postop. HVA | 0.207 | 0.126 | 1.23 | 0.96-1.58 | 0.103 |
| IMA deformity correction | 0.289 | 0.182 | 1.34 | 0.93-1.91 | 0.114 |
| HVA deformity correction | −0.185 | 0.090 | 0.83 | 0.70-0.99 | 0.042 |
| EQ-5D-5L Index | −6.565 | 8.892 | <0.01 | <0.01->100 | 0.461 |
| EQ-VAS | 0.113 | 0.072 | 1.12 | 0.97-1.29 | 0.121 |
| VAS-pain | −0.073 | 0.048 | 0.93 | 0.85-1.02 | 0.135 |
| Age | −0.224 | 0.086 | 0.80 | 0.67-0.95 | 0.010 |
SE = standard error of coefficient, CI = confidence interval for odds ratio, MOXFQ = Manchester-Oxford Foot Questionnaire, IMA = 1-2 intermetatarsal angle, and HVA = hallux valgus angle.
Bolded variables indicate a significant association.
Discussion
To our knowledge, this prospective study is the largest series of third-generation MICA procedures demonstrating, with use of validated outcome measures, the effectiveness of the technique for hallux valgus deformity correction.
MOXFQ Score
The MOXFQ is a PROM specifically validated for the assessment of hallux valgus19. A significant improvement between preoperatively and 2 years postoperatively was demonstrated in all domains (walking and standing, social interaction, and pain). The mean improvement in each domain was greater than the MCID, demonstrating the clinical efficacy of MICA19. Table VI shows that the mean MOXFQ scores were lower than those in other studies investigating the third-generation MICA technique12,13,16. As in those other studies, we demonstrated a significant improvement in social interaction following hallux valgus surgery, suggesting that the patients’ self-consciousness regarding their feet and shoes as well as the adverse overall impact of the deformity on social, recreational, work, and other everyday activities significantly decreased following surgery. The mean preoperative and postoperative scores were lower than those in the comparative studies, which may reflect the different practice settings, sample size, and follow-up duration. The use of validated PROMs allows comparison with other osteotomy techniques for correction of hallux valgus. For example, this study demonstrated a greater mean improvement in every MOXFQ domain compared with a large study using the scarf osteotomy technique19.
TABLE VI.
MOXFQ and Radiographic Outcomes from Other Studies Investigating Third-Generation Minimally Invasive Osteotomies for Hallux Valgus Correction*
| Studies Reporting Third-Generation MIS | No. of Feet | Mean Follow-up (mo) | Mean Preop./Postop. MOXFQ Score | Mean Preop./Postop. Radiographic Deformity (deg) |
Adverse Event or Complication Rate (%) | Screw-Removal Rate (%) | |||
| Pain | Walking/Standing | Social Interaction | IMA | HVA | |||||
| Present study | 292 | 30 | 44.5/9.4 | 38.7/6.5 | 48.0/6.6 | 15.3/5.7 | 32.9/8.7 | 21.3 | 6.3 |
| Brogan et al.12 (2014) | 45 | 6 | 50.8/17.4 | 43.2/9.8 | 47.6/13.1 | 14.6/7.1 | 30.5/10.4 | 6.67 | 2.2 |
| Brogan et al.16 (2016) | 48 | 24 | 49.2/16.5 | 42.6/9.2 | 49.2/24.3 | 11.7/4.4 | 26.6/10.4 | 18.8 | 8.3 |
| Holme et al.13 (2020) | 40 | 12 | 65.6/10.9 | 56.3/8.7 | 53.4/9.7 | 13.2/6.7 | 31.7/12.1 | 10.0 | 10.0 |
| Lee et al.15 (2017) | 25 | 6 | 15.6/6.4 | 31.4/7.6 | 13.3 | 24.0 | |||
| Jowett and Bedi10 (2017) | 106 | 25 | 14/7.6 | 29.7/10.3 | 42 | 15.1 | |||
| Lucas y Hernandez et al.14 (2016) | 45 | 60 | 11.8/7.9 | 26.6/9.6 | 15.5 | 8.9 | |||
| Frigg et al.29 (2019) | 48 | 24 | 13/6 | 25/7 | 31.3 | 27.1 | |||
| Lam et al.30 (2015) | 23 | 18 | 13.8/8.0 | 31.7/14.4 | 17 | 26.1 | |||
| Redfern and Vernois8 (2016) | 100 | 12-36 | 14.5/5.5 | 33.7/7.3 | 2 | 2.1 | |||
| Lai et al.9 (2018) | 29 | 24 | 14.6/10.3 | 29.9/8.8 | 0 | 16.7 | |||
MOXFQ = Manchester-Oxford Foot Questionnaire, IMA = 1-2 intermetatarsal angle, and HVA = hallux valgus angle.
There was a significant improvement in quality of life as reflected by the EQ-5D-5L Index and VAS-pain score although no significant change in the EQ-VAS score. This is likely due to the latter scale measuring an overall quality of health and potentially not being sensitive enough to pick up changes following hallux valgus correction. Lai et al. found an improvement in both physical and mental function subscale scores of the Short Form-36 (SF-36) quality-of-life assessment measure following MIS osteotomies; however, they did not report if this was statistically significant9.
Radiographic Outcomes
This study included a wide range of hallux valgus deformities, with >25% categorized as “severe” preoperatively. The mean preoperative IMA and HVA and postoperative deformity correction in this study were greater than or comparable with those in other series8-10,12-16,29,30 (Table VI). This supports the view that MICA can be used to treat a wide range of deformity severity. However, radiographic follow-up was not routinely extended beyond 6 weeks; therefore, it is unknown whether the HVA and IMA correction is maintained over time. Rates of hallux valgus recurrence after surgery have been reported to be as high as 16%31. The rate of symptomatic recurrence was only 0.9% in our study, although radiographs were not obtained after 6 weeks unless there were clinical concerns. Therefore, we are unable to be certain about the radiographic recurrence rate after MICA. The HVA and IMA can progressively deteriorate following hallux valgus correction32; however, Kaufmann et al. found only minor loss of HVA/IMA correction between 6 weeks and 12 weeks, 9 months, and 5 years after use of a second-generation MIS technique33.
Complications
First and second-generation percutaneous hallux valgus surgery (without internal fixation) has been shown to be followed by high rates of loss of correction or malunion34 with complication rates ranging between 0% and 42%10,35. Higher complication rates have been associated with early-learning-curve experiences as this is a technically demanding procedure that requires specific training and performing approximately 20 to 50 cases to reach technical proficiency6,7. The overall adverse-event rate in this study was 21.3% although the rate of major complications (necessitating a return to the operating theater) was 7.8%, including a deep infection rate of 1.2%. The all-cause screw-removal rate was 6.3%, which was lower than that in the majority of other third-generation-MIS studies (Table VI). There were no patient-reported cases of stiffness of the first metatarsophalangeal joint or metatarsal head osteonecrosis, as others have reported1,3,35,36, although we did not typically obtain radiographs beyond 6 weeks postoperatively. The complication rates that we reported are comparable with those in other series of third-generation MIS, as seen in Table VI, although there is substantial variation in the quality of complication reporting in the MIS literature.
Multivariable Linear Regression Analysis
The model identified that the significant factors affecting the change in the MOXFQ index score following MICA are the preoperative MOXFQ scores in the social interaction and walking/standing domains, change in the HVA, and age. The effect of the other variables on the change in the MOXFQ index score varied but none were statistically significant. The multivariable linear regression results are consistent with expected findings in clinical practice—for example, patients with an improvement in the HVA may well be expected to have an improvement in their MOXFQ index score. The preoperative MOXFQ pain score was not significantly related to the change in the MOXFQ index score 2 years following surgery. We were unable to identify other studies performing regression analysis for minimally invasive hallux valgus surgery, which prevented us from making comparisons. However, Chong et al. performed regression analysis on a population consisting predominantly of patients treated with scarf osteotomies and found no association between radiographic evidence of severity or the degree of correction and the MOXFQ score; the latter finding contradicts ours37.
Strengths
The strengths of this study include the large number of feet (292 for the MOXFQ analysis and 319 for the radiographic analysis) and utilization of validated outcome measures. Data were collected prospectively for consecutive patients, and there was an in-depth analysis of all adverse events. There was consistency in operative technique, as it was a single-surgeon series (accounting for the learning curve). Patients with a severe HVA or IMA were not excluded from surgery, enabling a valid assessment of third-generation MICA for a large spectrum of deformities. The duration of and small loss to follow-up provide representative insight into the 2-year outcomes of this technique.
Limitations
The main limitation of this study is the lack of long-term radiographic follow-up, which may lead to a different estimation of the recurrence rate, osteonecrosis, and degenerative changes. Radiographic assessments were based on imaging performed 6 weeks postoperatively, when incomplete weight-bearing on the medial column may have potentially altered the “true” IMA and HVA38. Also, the high female sex proportion in this cohort may reduce the applicability of this procedure in males. In addition, because there was no comparator cohort, we were unable to compare MICA with other osteotomy techniques.
Generalizability
The results are generalizable to the wider population of patients once the practicing surgeon has achieved technical proficiency. The range of preoperative deformities and the pragmatic treatment of related lesser-toe abnormalities reflect true clinical practice. The PROMs used are validated and will allow surgeons to draw a comparison between studies of different osteotomy techniques.
Conclusions
The third-generation MICA technique provided significant improvement in clinical measures at a 2-year follow-up with a low rate of symptomatic recurrence in our study of a wide range of hallux valgus deformities. Future research with radiographic and comparative studies to define the role of MICA in treatment for hallux valgus is required.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/G426).
Acknowledgments
Note: The authors thank Mollie Cresswell from Amplitude Clinical Outcomes for her help with this study.
Footnotes
Investigation performed at The London Clinic, London, United Kingdom
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/G425).
References
- 1.Bia A, Guerra-Pinto F, Pereira BS, Corte-Real N, Oliva XM. Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg. 2018. Jan-Feb;57(1):123-30. Epub 2017 Sep 1. [DOI] [PubMed] [Google Scholar]
- 2.Malagelada F, Sahirad C, Dalmau-Pastor M, Vega J, Bhumbra R, Manzanares-Céspedes MC, Laffenêtre O. Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop. 2019. March;43(3):625-37. Epub 2018 Sep 14. [DOI] [PubMed] [Google Scholar]
- 3.Maffulli N, Longo UG, Marinozzi A, Denaro V. Hallux valgus: effectiveness and safety of minimally invasive surgery. A systematic review. Br Med Bull. 2011;97:149-67. Epub 2010 Aug 14. [DOI] [PubMed] [Google Scholar]
- 4.del Vecchio JJ, Dalmau-Pastor M, Ghioldi ME. Third-generation percutaneous forefoot surgery. In: Badekas T, editor. Update in management of foot and ankle disorders. InTechOpen; 2018. p 101-114. [Google Scholar]
- 5.Del Vecchio JJ, Ghioldi ME. Evolution of minimally invasive surgery in hallux valgus. Foot Ankle Clin. 2020. March;25(1):79-95. Epub 2019 Nov 30. [DOI] [PubMed] [Google Scholar]
- 6.Palmanovich E, Ohana N, Atzmon R, Slevin O, Brin Y, Feldman V, Segal D. MICA: a learning curve. J Foot Ankle Surg. 2020. Jul-Aug;59(4):781-3. Epub 2020 Apr 25. [DOI] [PubMed] [Google Scholar]
- 7.Bedi H, Hickey B. Learning curve for minimally invasive surgery and how to minimize it. Foot Ankle Clin. 2020. September;25(3):361-71. Epub 2020 Jul 11. [DOI] [PubMed] [Google Scholar]
- 8.Redfern D, Vernois J. Minimally Invasive chevron Akin (MICA) for correction of hallux valgus. Tech Foot Ankle Surg. 2016. March;15(1):3-11. [Google Scholar]
- 9.Lai MC, Rikhraj IS, Woo YL, Yeo W, Ng YCS, Koo K. Clinical and radiological outcomes comparing percutaneous chevron-Akin osteotomies vs open scarf-Akin osteotomies for hallux valgus. Foot Ankle Int. 2018. March;39(3):311-7. Epub 2017 Dec 14. [DOI] [PubMed] [Google Scholar]
- 10.Jowett CRJ, Bedi HS. Preliminary results and learning curve of the minimally invasive chevron Akin operation for hallux valgus. J Foot Ankle Surg. 2017. May-Jun;56(3):445-52. Epub 2017 Feb 22. [DOI] [PubMed] [Google Scholar]
- 11.Lam P, Lee M, Xing J, Di Nallo M. Percutaneous surgery for mild to moderate hallux valgus. Foot Ankle Clin. 2016. September;21(3):459-77. [DOI] [PubMed] [Google Scholar]
- 12.Brogan K, Voller T, Gee C, Borbely T, Palmer S. Third-generation minimally invasive correction of hallux valgus: technique and early outcomes. Int Orthop. 2014. October;38(10):2115-21. Epub 2014 Aug 17. [DOI] [PubMed] [Google Scholar]
- 13.Holme TJ, Sivaloganathan SS, Patel B, Kunasingam K. Third-generation minimally invasive chevron Akin osteotomy for hallux valgus. Foot Ankle Int. 2020. January;41(1):50-6. Epub 2019 Sep 14. [DOI] [PubMed] [Google Scholar]
- 14.Lucas y. Hernandez J, Golanó P, Roshan-Zamir S, Darcel V, Chauveaux D, Laffenêtre O. Treatment of moderate hallux valgus by percutaneous, extra-articular reverse-L chevron (PERC) osteotomy. Bone Joint J. 2016. March;98-B(3):365-73. [DOI] [PubMed] [Google Scholar]
- 15.Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P. Hallux valgus correction comparing percutaneous chevron/Akin (PECA) and open scarf/Akin osteotomies. Foot Ankle Int. 2017. August;38(8):838-46. Epub 2017 May 5. [DOI] [PubMed] [Google Scholar]
- 16.Brogan K, Lindisfarne E, Akehurst H, Farook U, Shrier W, Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int. 2016. November;37(11):1197-204. Epub 2016 Jul 4. [DOI] [PubMed] [Google Scholar]
- 17.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983. September;17(1):45-56. [DOI] [PubMed] [Google Scholar]
- 18.Dawson J, Coffey J, Doll H, Lavis G, Cooke P, Herron M, Jenkinson C. A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res. 2006. September;15(7):1211-22. Epub 2006 Sep 25. [DOI] [PubMed] [Google Scholar]
- 19.Dawson J Doll H Coffey J Jenkinson C; Oxford and Birmingham Foot and Ankle Clinical Research Group. Responsiveness and minimally important change for the Manchester-Oxford Foot Questionnaire (MOXFQ) compared with AOFAS and SF-36 assessments following surgery for hallux valgus. Osteoarthritis Cartilage. 2007. August;15(8):918-31. Epub 2007 Mar 26. [DOI] [PubMed] [Google Scholar]
- 20.Dawson J, Boller I, Doll H, Lavis G, Sharp R, Cooke P, Jenkinson C. Responsiveness of the Manchester-Oxford Foot Questionnaire (MOXFQ) compared with AOFAS, SF-36 and EQ-5D assessments following foot or ankle surgery. J Bone Joint Surg Br. 2012. February;94(2):215-21. [DOI] [PubMed] [Google Scholar]
- 21.Morley D, Jenkinson C, Doll H, Lavis G, Sharp R, Cooke P, Dawson J. The Manchester-Oxford Foot Questionnaire (MOXFQ): development and validation of a summary index score. Bone Joint Res. 2013. April 3;2(4):66-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coughlin MJ, Saltzman CL, Nunley JA, 2nd. Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002. January;23(1):68-74. [DOI] [PubMed] [Google Scholar]
- 23.Robinson AHN, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005. August;87(8):1038-45. [DOI] [PubMed] [Google Scholar]
- 24.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012. August;470(8):2220-6. Epub 2012 Apr 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dodwell ER, Pathy R, Widmann RF, Green DW, Scher DM, Blanco JS, Doyle SM, Daluiski A, Sink EL. Reliability of the modified Clavien-Dindo-Sink complication classification system in pediatric orthopaedic surgery. JB JS Open Access. 2018. October 23;3(4):e0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Virtanen P, Gommers R, Oliphant TE, Haberland M, Reddy T, Cournapeau D, Burovski E, Peterson P, Weckesser W, Bright J, van der Walt SJ, Brett M, Wilson J, Millman KJ, Mayorov N, Nelson ARJ, Jones E, Kern R, Larson E, Carey CJ, Polat İ, Feng Y, Moore EW, VanderPlas J, Laxalde D, Perktold J, Cimrman R, Henriksen I, Quintero EA, Harris CR, Archibald AM, Ribeiro AH, Pedregosa F, van Mulbregt P; SciPy 1.0 Contributors. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods. 2020. March;17(3):261-72. Epub 2020 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, Nicholl J, Aronson JK, Barkun JS, Blazeby JM, Boutron IC, Campbell WB, Clavien PA, Cook JA, Ergina PL, Feldman LS, Flum DR, Maddern GJ, Nicholl J, Reeves BC, Seiler CM, Strasberg SM, Meakins JL, Ashby D, Black N, Bunker J, Burton M, Campbell M, Chalkidou K, Chalmers I, de Leval M, Deeks J, Ergina PL, Grant A, Gray M, Greenhalgh R, Jenicek M, Kehoe S, Lilford R, Littlejohns P, Loke Y, Madhock R, McPherson K, Meakins J, Rothwell P, Summerskill B, Taggart D, Tekkis P, Thompson M, Treasure T, Trohler U, Vandenbroucke J; Balliol Collaboration. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009. September 26;374(9695):1105-12. [DOI] [PubMed] [Google Scholar]
- 28.Dalmau-Pastor M, Malagelada F, Cordier G, Del Vecchio JJ, Ghioldi ME, Vega J. Anatomical study of minimally invasive lateral release techniques for hallux valgus treatment. Foot Ankle Int. 2020. August;41(8):984-92. Epub 2020 May 26. [DOI] [PubMed] [Google Scholar]
- 29.Frigg A, Zaugg S, Maquieira G, Pellegrino A. Stiffness and range of motion after minimally invasive chevron-Akin and open scarf-Akin procedures. Foot Ankle Int. 2019. May;40(5):515-25. Epub 2019 Jan 28. [DOI] [PubMed] [Google Scholar]
- 30.Lam KLK, Kong SW, Chow YH. Percutaneous chevron osteotomy in treating hallux valgus: Hong Kong experience and mid-term results. J Orthop Trauma Rehab. 2015;19(1):25-30. [Google Scholar]
- 31.Lee KT, Park YU, Jegal H, Lee TH. Deceptions in hallux valgus: what to look for to limit failures. Foot Ankle Clin. 2014. September;19(3):361-70. Epub 2014 Jul 2. [DOI] [PubMed] [Google Scholar]
- 32.Park CH, Lee WC. Recurrence of hallux valgus can be predicted from immediate postoperative non-weight-bearing radiographs. J Bone Joint Surg Am. 2017. July 19;99(14):1190-7. [DOI] [PubMed] [Google Scholar]
- 33.Kaufmann G, Mörtlbauer L, Hofer-Picout P, Dammerer D, Ban M, Liebensteiner M. Five-year follow-up of minimally invasive distal metatarsal chevron osteotomy in comparison with the open technique: a randomized controlled trial. J Bone Joint Surg Am. 2020. May 20;102(10):873-9. Epub 2020 Mar 5. [DOI] [PubMed] [Google Scholar]
- 34.Kadakia AR, Smerek JP, Myerson MS. Radiographic results after percutaneous distal metatarsal osteotomy for correction of hallux valgus deformity. Foot Ankle Int. 2007. March;28(3):355-60. [DOI] [PubMed] [Google Scholar]
- 35.Filippi J, Briceno J. Complications after metatarsal osteotomies for hallux valgus: malunion, nonunion, avascular necrosis, and metatarsophalangeal osteoarthritis. Foot Ankle Clin. 2020. March;25(1):169-82. Epub 2019 Nov 26. [DOI] [PubMed] [Google Scholar]
- 36.de Lavigne C, Guillo S, Laffenêtre O, De Prado M, 2nd GRECMIP . The treatment of hallux valgus with the mini-invasive technique. Interactive Surgery. 2007;2:31-7. [Google Scholar]
- 37.Chong A, Nazarian N, Chandrananth J, Tacey M, Shepherd D, Tran P. Surgery for the correction of hallux valgus: minimum five-year results with a validated patient-reported outcome tool and regression analysis. Bone Joint J. 2015. February;97-B(2):208-14. [DOI] [PubMed] [Google Scholar]
- 38.Kuyucu E, Ceylan HH, Surucu S, Erdil I, Kara A, Gulenc BG, Bulbul M, Erdil M. The effect of incorrect foot placement on the accuracy of radiographic measurements of the hallux valgus and inter-metatarsal angles for treating hallux valgus. Acta Chir Orthop Traumatol Cech. 2017;84(3):196-201. [PubMed] [Google Scholar]