Abstract
This study examined interparental conflict as a linear and curvilinear predictor of subsequent changes in adolescents’ negative emotional reactivity and cortisol functioning during family conflict and, in turn, their psychological difficulties. In addition, adolescents’ negative emotional reactivity and cortisol functioning during family conflict were examined as subsequent predictors of their psychological difficulties. Participants included 258 adolescents (52% girls) and their parents and teachers who participated in three annual measurement occasions. Adolescents were 13 years old on average (SD = .57) at the first measurement occasion, were generally from middle and working class backgrounds, and identified mostly as White (e.g., 74%). Results of latent difference score analyses indicated that a multi-method and multi-informant assessment of interparental conflict linearly predicted subsequent changes in observational ratings of adolescent emotional reactivity and their overall cortisol output in response to family conflict over a one-year period. These changes, in turn, predicted increases in multi-informant reports of adolescent psychological problems over a two-year period. However, the linear association in the first link in the cascade was qualified by the quadratic effects of interparental conflict as a predictor. Consistent with risk saturation models, the relatively strong associations among interparental conflict and youth emotional reactivity and cortisol output at mild and moderate exposure to conflict weakened as exposure to conflict reached higher levels.
Keywords: interparental conflict, emotional reactivity, cortisol functioning, psychopathology, adolescence
Adolescents exposed to high levels of destructive interparental conflict characterized by hostility, coerciveness, and anger are at increased risk for developing behavioral, emotional, and social problems (Harold & Sellers, 2018; Jouriles, McDonald, & Kouros, 2016). In search of the mechanisms accounting for this risk, several process-oriented frameworks have proposed that youth emotional and cortisol responses to family stressors mediate their vulnerability to interparental conflict in a linear manner (Davies, Martin, & Sturge-Apple, 2016; Labella & Masten, 2018; Morris, Houltberg, Criss, & Bosler, 2017; Repetti, Robles, & Reynolds, 2011). Some studies have supported the notion that interparental conflict increases adolescent vulnerability to psychopathology by altering children’s emotional reactions and functioning in stress-sensitive physiological systems (for a review, see Repetti et al., 2011). By the same token, several conceptualizations have underscored that exposure to family adversity may have curvilinear effects on how adolescents respond to subsequent stressors and, ultimately, their psychological adjustment (e.g., Davies & Sturge-Apple, 2007; Koss & Gunnar, 2018; Repetti & Robles, 2016; Susman, 2006). Whereas some models have proposed that interparental conflict at mild or moderate levels enhances coping and, as a result, predicts heightened adolescent emotional and physiological responses in a U-shaped form, other models have posited that youths’ reactivity to interparental conflict progressively diminishes as conflict reaches high levels (Davies & Sturge-Apple, 2007; Repetti & Robles, 2016). However, research has yet to test the viability of these theoretical models. Thus, the goal of this study was to examine interparental conflict as a linear and curvilinear predictor of a cascade of adolescent responses to family conflict and, in turn, their psychological problems within a multiple-levels-of-analysis framework examining children’s behavioral (i.e., negative emotional reactivity) and physiological (i.e., cortisol) responses to family conflict as risk mechanisms (Hankin, 2015).
Linear Models of Response Processes Underlying Interparental Conflict
Family process models have postulated that sensitivity to stress within behavioral and adrenocortical domains of functioning are central carriers of risk in pathways between interparental conflict and child psychopathology (e.g., Davies et al., 2016; Repetti et al., 2011). According to emotional security theory (Davies et al., 2016), exposure to intense bouts of interparental conflict mobilizes youth to process and defend against threats in the family. Through this proposed sensitization process, children may experience heightened behavioral and physiological arousal in response to subsequent family conflicts and, over time, become progressively more vulnerable to psychopathology over time. At a behavioral level, this reactivity may be manifested in greater distress responses to family difficulties. Over time, greater distress and vigilance are posited to increase psychopathology by serving as templates for responding to other stressful interpersonal contexts and undermining intrinsic motivation toward approach-oriented goals (e.g., exploration, affiliation) (Davies & Martin, 2014). At a physiological level, the threat and insecurity in the aftermath of interparental conflicts is posited to increase adolescent vulnerability by altering the functioning of the hypothalamic-pituitary-adrenal (HPA) axis (Kamin & Kertes, 2017). With cortisol as its product, the HPA axis responds to adversity by mobilizing energy (e.g., glucose, oxygen) and modulating the processing, encoding, and memory consolidation of stressful events (Juster, Bizik, Picard, Arsenault-Lapierre, Sindi, Trepanier, …& Fiocco, 2011). Extending work on the HPA axis as a stress-sensitive system, sensitization models have theorized that the witnessing conflicts between parents poses a risk for youth mental health by amplifying cortisol and its neurotoxic effect on multiple brain regions (e.g., prefrontal cortex, hippocampus) that organize learning, memory, executive function, and emotion regulation processes (Koss & Gunnar, 2018; Martin, Davies, Cummings, & Cicchetti, 2017).
Research has found some support for youth emotional reactivity and cortisol activity as risk mechanisms underpinning interparental conflict. For example, empirical findings have indicated that children’s prolonged and intense distress responses to family stressors account for links between interparental conflict and child psychopathology (e.g., Buehler, Lange, & Franck, 2007; Davies, Cicchetti, & Martin, 2012). However, the modest strength of these pathways suggests that there is considerable variability between children in the explanatory power of emotional reactivity as a linear mediator of interparental conflict. Other studies have generated evidence for cortisol reactivity and diurnal activity as intermediary processes explaining the risk posed by interparental conflict. For example, heightened cortisol responding to parental discord has been empirically documented as a correlate of children’s experiences of destructive forms of interparental conflict, emotional insecurity, and psychopathology (Koss et al., 2013; Martin et al., 2017). Other studies have identified that poorer relationship quality between parents is associated with higher diurnal cortisol (e.g., Davies, Sturge-Apple, Cicchetti, Manning, & Zale, 2009; Pendry & Adam, 2007; Saltzman, Holden, & Holahan, 2005). However, findings do not definitively favor heightened cortisol reactivity and diurnal cortisol as risk mechanisms. For example, dampened cortisol reactivity to family conflict has also been linked with greater exposure to interparental conflict and more psychological problems in some studies (Davies, Sturge-Apple, Cicchetti, & Cummings, 2007; Sturge-Apple, Davies, Cicchetti, & Manning, 2012). In sum, although research provides some support for emotional reactivity, diurnal cortisol, and cortisol reactivity to family stress as mechanisms accounting for youth vulnerability to interparental conflict, the modest strength of the pathways and, in some cases, inconsistencies in the findings, suggest that the underlying risk processes may not readily conform to linear dose-response relations of risk.
Quadratic Models of Response Processes Underlying Interparental Conflict
As a complement to linear conceptualizations of children’s adaptation to interparental conflict, theoretical models have increasingly underscored that the intergenerational transmission of distress in models of family adversity may be curvilinear in form (e.g., Davies & Sturge-Apple, 2007; Jouriles et al., 2016; Repetti & Robles, 2016; Susman, 2006). Although there are several distinct proposals on the quadratic operation of family risk factors, the literature primarily coheres around two distinct curvilinear relations between family adversity and children’s coping and adaptation. Rooted in developmental psychopathology (Garmezy, Masten, & Tellegen, 1984; Rutter, 1987), the “challenge” model proposes that stressful conditions may enhance coping and inoculate individuals against subsequent psychological vulnerability, particularly when stressors are manageable in frequency (i.e., occasional occurrence), intensity (i.e., mild, well-regulated anger), and duration (i.e., brief) (Davies & Sturge-Apple, 2007; Jouriles et al., 2016; Repetti & Robles, 2016). Translated to interparental conflict, this model proposes that mild and manageable doses of discord between parents spur the development of coping skills necessary for the effective regulation of emotional and physiological functioning in the face of subsequent conflict. Thus, as shown in Figure 1a, a derivative hypothesis is that there will be a U-shaped relation between interparental conflict and emotional and physiological arousal in response to conflict. On the left side of the plot, increases in interparental conflict from negligible to moderate levels are specifically related to gradual decreases in emotional reactivity and pathogenic HPA axis functioning. Conversely, the right side of the figure illustrates the hypothesis that intensification of conflict from moderate to high levels should be associated with relatively steep increases in emotional and physiological risk responses.
Figure 1a.
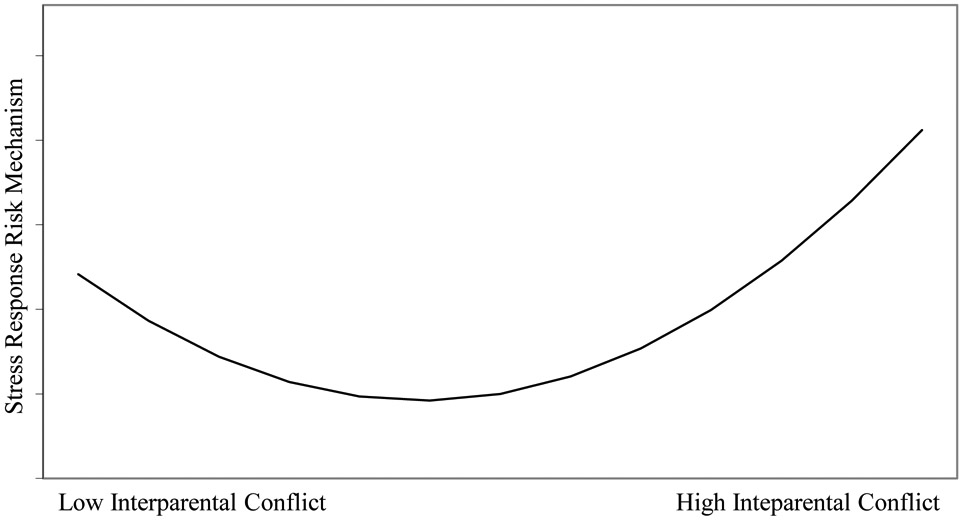
A challenge model formulation of the hypothesized curvilinear relationship between interparental conflict and youth reactivity to family conflict.
As the second set of curvilinear models, the risk saturation model illustrated in Figure 1b proposes a downward concave relation between interparental conflict and youth risk processes (Davies & Sturge-Apple, 2007; Susman, 2006). As depicted on the left side of the plot, interparental conflict is hypothesized to increase children’s reactivity to subsequent family adversity as youth exposure to conflict increases from low to moderate ranges of risk. However, risk saturation diverges from linear models of stress sensitization in its proposal that as conflicts intensify to high levels, the direct risk conferred by interparental conflict will reach a saturation point (Morris, Ciesla, & Garber, 2010). Thus, the relatively strong relation between interparental conflict and youth reactivity progressively fades to the point of reaching an asymptote at intense stress levels (Davies & Sturge-Apple, 2007). As a key source of conceptual support for risk saturation, the attenuation hypothesis proposes that greater emotional and cortisol arousal is a common consequence of repeated exposure to many forms of family threats (Kamin & Kertes, 2017; Susman, 2006). However, prolonged and intense levels of physiological and emotional arousal resulting from the sensitization process may have noxious effects on neurobiological systems. Accordingly, attenuation of arousal following exposure to highly destructive conflicts between parents may signify the activation of processes designed to prevent chronic arousal of the stress system in response to threat (Susman, 2006).
Figure 1b.
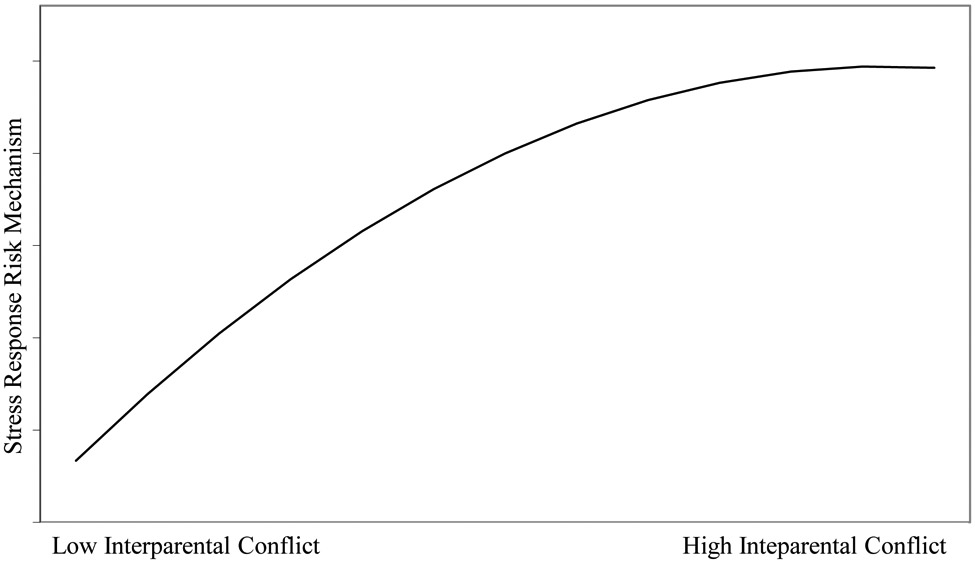
A risk saturation model formulation of the hypothesized curvilinear relationship between interparental conflict and youth reactivity to family conflict.
Integrated within the existing linear frameworks of interparental conflict (Davies et al., 2016; Repetti et al., 2011), the two classes of quadratic models share the assumption that the proposed indirect pathways involving interparental conflict, youth emotional and physiological arousal in contexts of family conflict, and their psychological difficulties will vary at different levels of interparental conflict. Given their focus on how exposure to interparental conflict may subsequently alter youth responses to conflict in curvilinear ways, challenge and risk saturation models propose that the level of interparental conflict may moderate the first link in the mediational pathways involving interparental conflict, adolescent’s subsequent emotional and adrenocortical responses to conflict, and their psychological difficulties. Accordingly, in this paper, we addressed the primary research question of whether the quadratic assessment of interparental conflict uniquely predicted youth emotional and cortisol responses to family conflict and, in turn, their psychological difficulties after taking into account the linear risk posed by interparental conflict.
Adolescence as a Sensitive Period
In drawing on the different conceptualizations of offspring reactivity to family conflict, we specifically focus on testing our research questions on offspring vulnerability to interparental conflict during the early half of adolescence. Our decision to focus on this age period was guided by several developmental considerations. The period of early and middle adolescence is marked by heightened negative emotional reactivity and affective lability that, in part, stems from accelerated neurobiological and behavioral sensitivity to threatening interpersonal cues (Ahmed, Bittencourt-Hewitt, & Sebastian, 2015; Guyer, Silk, & Nelson, 2016; Schriber & Guyer, 2016). In highlighting a comparable process of heightened HPA-axis sensitivity to adversity, studies have shown that stress evokes greater glucocorticoid levels during early adolescence relative to earlier developmental periods (e.g., Hankin, 2012; Ji, Negriff, Kim, & Susman, 2016). Consistent with findings on neurobiological and emotional reactivity, developmental models of interparental conflict have proposed that adolescents experience greater sensitivity to relationship difficulties between adults and stronger impulses to become involved in conflicts than do younger children (Davies et al., 2016; Fosco & Grych, 2010). In supporting this premise, research has shown that the prospective association between interparental conflict and adolescent emotional and behavioral responses to conflict is stronger for adolescents relative to preadolescent children (Cummings, Schermerhorn, Davies, Goeke-Morey, & Cummings, 2006). Finally, with rises in sensitivity to interpersonal threat and the growing demands to regulate emotions autonomously, early adolescence is commonly regarded as a period in which family stress and greater reactivity to conflict may amplify risk for psychopathology (Ahmed et al., 2015; Davies et al., 2016; Guyer et al., 2016).
The Present Study
In summary, a growing number of family process models postulate that the relation between interparental conflict and adolescent emotional and cortisol reactivity to family adversity may assume a quadratic form. However, to our knowledge, no studies have tested the curvilinear relation between interparental conflict and indices of youth reactivity to family stress and its implications for their psychological problems. To address this gap, we tested a developmental cascade whereby interparental conflict poses a risk for youth psychopathology through its possible role as a linear and curvilinear predictor of youth emotional and cortisol reactivity to family disagreements. Based on developmental conceptualizations of interparental conflict as conferring linear and quadratic risk, we hypothesized that adolescent adaptation to interparental conflict would assume both linear and quadratic forms. Although our goal was to examine interparental conflict as a predictor of adolescent emotional reactivity, physiological functioning, and psychological problems, several family models propose that children’s short-term emotional and physiological responses to family conflict are more proximal sequelae of than global, trait measures of general psychological adjustment (e.g., Davies et al., 2016; Jouriles et al., 2016; Repetti et al., 2011). Accordingly, we hypothesized that the linear and quadratic roles of interparental conflict as predictors of youth functioning would be specifically manifested in their emotional and physiological responses to family conflict. The paucity of empirical work precluded the formulation of specific hypotheses on the nature of the quadratic relation between interparental conflict and youth functioning. Therefore, our aim was to examine the relative correspondence between significant quadratic associations and the two prevailing conceptual models (i.e., challenge versus risk saturation) in the literature.
Although previous studies provide some support for the role of offspring emotional reactivity and HPA axis functioning as risk mechanisms in the link between interparental conflict and youth psychological difficulties (e.g., Buehler et al., 2007; Davies et al, 2007; 2012; Luecken, Kraft, & Hagan, 2009), research has generally assessed single static snapshots of child sequelae (i.e., mediator, outcome, or both). Failure to use repeated assessments of the endogenous variables in mediational models produces biased path estimates (Maxwell & Cole, 2007). Therefore, following quantitative guidelines for accurately testing mediation, we examined whether linear and quadratic indices of interparental conflict predicted successive cascades of change in the proposed mediators (i.e., emotional reactivity, cortisol functioning) and, in turn, the proposed outcome of youth psychological problems. Guided by curvilinear conceptualizations that have defined high levels of family conflict based on an aggregation of frequency, duration, and intensity (e.g., Repetti & Robles, 2016), our multi-method, multi-informant approach to assessing interparental conflict was designed to collectively capture these conflict parameters. Based on previous conceptualizations of security and emotion regulation in adverse socialization contexts (Davies et al., 2016; Morris et al., 2017), our measurement of negative emotional reactivity consisted of adolescent displays of heightened distress, intense efforts to regulate exposure to threat through avoidance or controlling behaviors, and diminished confidence, comfort, and assertiveness in response to family conflict. Finally, given the inconsistencies in the literature on the relative roles of cortisol reactivity and activity as risk mechanisms of interparental conflict (e.g., Davies et al., 2007; Pendry & Adam, 2007; Saltzman et al., 2005), we examined youth overall cortisol production and change across a family conflict task (Pruessner, Kirschbaum, Meinlshmidt, & Hellhammer, 2003).
Method
Participants
Participants were 258 adolescents and their parents who were recruited from local school districts and community centers in a moderately sized metropolitan area in the Northeastern US and a small city in the Midwestern US. Because assessing interparental conflict was a key focus of the study, inclusionary criteria required that mothers, fathers, and adolescents have regular contact with each other as a triad, defined by an average of 3 days per week during the previous year (Mean = 6 days per week). Adolescents were in seventh grade at Wave 1, and, on average, 13 years old (SD = .57; range 11 to 14). Girls comprised 52% of the sample. Median household income of the families was between $55,000 and $74,999 per year. Median education level of mothers and fathers was some college education. Most parents (i.e., 86%) were married at the outset of the study. For racial background, 74% of adolescents were White, followed by smaller percentages of Black (17%), multi-racial (8%), and other races (21%). In terms of US ethnicity designations, 6% of youth were Latino. Adolescents lived with their biological mother in most cases (93%), with the remainder living with an adoptive or stepmother (4%) or a female guardian (3%). Children also lived with their biological father in most cases (79%), with the remainder of the sample living with either an adoptive or stepfather (17%) or a male guardian (4%). The longitudinal design of the study consisted of three annual measurement occasions. Retention rates were 91% and 94% across each of the two contiguous waves of data collection. Data were collected between 2007 and 2011.
Procedures
Families visited the laboratory at one of two data collection sites at three annual measurement occasions. Laboratories at each site included: (a) an observation room that was decorated to resemble a living room and equipped with audiovisual equipment to capture family interactions; and (b) interview rooms for completing interview and survey measures. The study, titled “Family process, emotional security, and child adjustment” was approved by the Institutional Review Board from the University of Rochester under Protocol #00014997. Families were compensated for participation in cash and gift cards totaling $240 at Wave 1, $280 at Wave 2, and $310 at Wave 3.
Interparental problem-solving task (IPST).
At Wave 1, mothers and fathers participated in an interparental interaction task in which they discussed two common, intense interparental disagreements that they viewed as problematic in their relationship. Following similar procedures in previous research (Du Rocher Schudlich, Papp, & Cummings, 2004), couples selected two common and problematic topics of disagreement in their relationship that they felt comfortable discussing from independent lists of topics that each partner generated. Couples were asked to address the topics in a way they normally would at home and discussed each topic for seven minutes while they were alone in the laboratory room. The IPST was video recorded for later coding of maternal and paternal interparental conflict tactics. Following the IPST, mothers and fathers completed a post-interaction survey in separate rooms to assess their ratings of negative affect experienced by themselves and their partners.
Triadic family problem-solving task (FPST).
At Waves 1 and 2, mothers, fathers, and youth engaged in a seven-minute problem-solving task. Each family member generated a list of problematic topics to discuss and then conferred for two minutes to select one topic to discuss for the FPST. Families were instructed to discuss the topic as they normally would at home. Discussions were videotaped for later coding of adolescent emotional reactivity to the family conflict task at Waves 1 and 2.
Survey assessments.
At Wave 1, mothers and fathers also completed questionnaires to assess interparental conflict. In addition, measures of adolescent psychological problems were obtained from mother, father, and teacher survey measures at Waves 1 and 3.
Measures
Interparental Conflict.
We utilized a multi-method, multi-informant measurement battery to assess interparental conflict at Wave 1. First, mothers and fathers completed the O’Leary Porter Scale (OPS; Porter & O’Leary, 1980), a 10-item survey assessing interparental hostility (e.g., “How often do you and/or your partner display verbal hostility [raised voices, etc.] in front of your child?”) over the past year. Internal consistency coefficients (ICC) were .78 and .80 for mothers and fathers, respectively. Second, after participating in the IPST, mothers and fathers completed a survey indexing their ratings of the affective intensity of the conflict. The four items specifically measured the intensity of their own feelings (i.e., angry, upset) and appraisals of their partner’s feelings (i.e., angry, upset) on six-point scales ranging from 0 “Not at All” to 5 “A Whole Lot” (ICC = .88 and .89 for mother and father IPST reports respectively). Third, trained coders rated maternal and paternal conflict behaviors in the IPST on dimensional scales from the System for Coding Interactions in Dyads (SCID; Malik & Lindahl, 2004). Mothers and fathers were coded separately for levels of: (1) Verbal Aggression, defined as the level of hostile or aggressive behaviors and verbalizations; (2) Negativity and Conflict, reflected in the level of tension, frustration, and anger displayed by each partner; and (3) Coerciveness, characterized by threatening and controlling verbalizations, tones of voice, and body language. Interrater reliability coefficients, which were calculated based on coders’ independent ratings on 20% of the interactions, ranged from .72 to .89 across codes (Mean ICC = .84). Ratings on the scales were averaged together into more parsimonious indicators of observed maternal (α = .80) and paternal (α = .80) destructive interparental conflict behaviors. As a final data reduction step, we aggregated the six standardized measures (i.e., maternal and paternal OPS, maternal and paternal IPST survey ratings, observer ratings of maternal and paternal destructive conflict behaviors in the IPST) into a single multi-method composite of interparental conflict (α = .80).
Youth emotional reactivity to conflict.
Coders rated youth emotional reactivity to the FPST at each wave using six dimensional codes ranging from 1 (Not at All Characteristic) to 9 (Mainly Characteristic). To obtain a balanced assessment of reactivity, codes were evenly divided into indicators of dysregulated, intense responses and regulated responses to conflict. Dysregulated emotional responses included: (1) Affected Behavior, characterized by intense and demonstrative displays of distress, whining, and fretting; (2) Mobilizing Behavior, reflected in a pattern of high sensitivity to interpersonal threat manifested in blatant, unvarnished expressions of distress and efforts to regulate the conflict through avoidance and/or intervention behaviors (e.g., alliance formation with one parent); and (3) Controlling Behavior, defined by youth aversive complaints, protests, and dogmatic assertions of their viewpoints. Regulated responses indexing low emotional reactivity included: (1) Comfort, reflected in verbal, facial, and postural displays of comfort, satisfaction, and positive affect; (2) Assertiveness, defined by youth communication of viewpoints in a confident, well-regulated, and constructive manner; and (3) Security, defined as an overall pattern of responding characterized by high levels of confidence, comfort, and constructive problem-solving efforts that reflect a balanced consideration of self and parent-oriented goals. ICC values, indexing interrater reliability based on independent coder ratings of over 20% of the videos, ranged from .77 to .92 (Mean ICC = .85) across the two waves. After reverse scoring the three regulated reactivity codes so they were scaled in the same direction as the dysregulated codes, we averaged the six observational codes into composites of youth negative emotional reactivity at Waves 1 (α = .81) and 2 (α = .75).
Youth cortisol responding to conflict.
At Waves 1 and 2, adolescents provided one pre-task and three post-task saliva samples to assess cortisol levels in the context of the FPST. Youth rinsed their mouths with water 10 min. prior to providing the first sample. Samples were collected through passive drool with the aid of a straw. A pre-task saliva assessment was obtained approximately 40 min. after the start of the visit to allow time for cortisol to return to baseline levels following their arrival to the laboratory. To capture youth cortisol levels in response to the family conflict, post-task samples were collected 10, 20, and 30 min. after the midpoint of the FPST, resulting in the collection of saliva samples at 14, 24, and 34 min. after the start of the task. Family visits took place predominantly in the late afternoon and evening hours to minimize the effects of diurnal cortisol patterns (M pre-task sampling time = 5:10 pm; SD = 1 hour and 43 min at Wave 1; and 4:54 pm; SD = 2 hours and 14 min at Wave 2). Cortisol data were missing for 9% of the samples at Wave 1 and 15% of the samples for participating families at Wave 2. Saliva samples collected at Waves 1 and 2 were assayed for cortisol using a highly sensitive immunoassay at Salimetrics Inc. (State College, PA). The test uses 25 μl of saliva per determination and assays were conducted in duplicate form. The assay has a lower test sensitivity of 0.007 μg/dl and an upper test sensitivity of 3.00 μg/dl. The average intra-assay coefficient of variation is 5.75%. Method accuracy, determined by spike and recovery, and linearity, determined by serial dilution, are 100.8% and 91.7%, respectively. The values from matched serum and saliva samples show the expected strong linear relation, r = .91.
We calculated two indices of cortisol activity at each wave: (1) area under the curve with respect to ground (AUCG), which is an index of the total cortisol output across the four assessments; and (2) area under the curve with respect to increase (AUCI), indexing the degree of change from the pre-task value to the three post-task assessments (see Pruessner et al., 2003). Because two cortisol values at Wave 1 (i.e., both post assessments) were beyond the upper test sensitivity limits, they were dropped prior to calculating the AUC measures. To normalize their distributions, AUCI and AUCG values that were beyond 3.5 standard deviations from the mean were winsorized to 3.5 standard deviations within the mean. Winsorizing was necessary for 6 Wave 1 AUCI, 4 Wave 2 AUCI, 7 Wave 1 AUCG, and Wave 1 2 AUCG values. Adolescents were instructed to refrain from eating or drinking an hour before the visit. Because some adolescents consumed food, drinks, or candy/gum within the hour prior to the visit (mean = 7.7%; range = 3.9% to 15.3%), we examined whether eating or drinking was associated with AUCG or AUCI values. None of the findings were significant at Waves 1 or 2. In addition, adolescent smoking and medication use (i.e., corticosteroid/contraceptive use) were also unrelated to AUCG or AUCI values at each wave. However, time since awake was significantly associated with AUCg at Waves 1 (r = −.31, p < .001) and 2 (r = −.34, p < .001) and AUCI at Wave 2 (r = .19, p = .008). Therefore, the difference in time since awake across the two waves was retained as a covariate in the analyses of change in AUCG or AUCI.
Youth psychological problems.
Mothers, fathers, and teachers completed surveys of adolescent emotional, behavioral, and social problems at Waves 1 and 3 to provide assessments of their collective psychological difficulties. Mothers and fathers completed an overall psychological symptoms measure consisting of the sum of the Anxious/Depressed (e.g., “nervous, high-strung, or tense”), Withdrawn/Depressed (e.g., “unhappy, sad, or depressed”), Rule-Breaking Behavior (e.g., “lying or cheating”), Aggressive Behavior (e.g., “gets in many fights”), and Social Problems (e.g., “gets teased a lot”) Scales from the Child Behavior Checklist (CBCL; Achenbach, Dumenci, & Rescorla, 2003). Alpha coefficients for the mother and father report measures of total problems ranged from .92 to .94 across the two waves. In addition, we obtained teacher reports of youth psychological problems using the Conduct Problems (e.g., “often fights with other youth or bullies them,” “often lies and cheats”), Emotional Problems (e.g., “many worries or often seems worried,” “often unhappy, depressed, or tearful”), and Peer Problems (e.g., “picked on or bullied by other children”) Scales of the Strengths and Difficulties Questionnaire (SDQ; Goodman & Scott, 1999). Internal consistencies for teacher reports of total problems were .82 at Wave 1 and .78 at Wave 3. The sound psychometric properties (i.e., validity, reliability) of the CBCL and SDQ are documented in previous research (Achenbach et al., 2003; Goodman & Scott, 1999). Mother, father, and teacher report measures were specified as indicators of a latent construct of psychological problems at each wave.
Covariates:
Youth gender, age, and race, and family income and parental marital status were specified as general covariates for adolescent cortisol activity and reactivity, emotional reactivity, and psychological problems based on their links with youth cortisol and psychological functioning in some previous studies (e.g., Adam & Kumari, 2009; Chaplin & Aldao, 2013; Evans & Kim, 2013; Kraft & Luecken, 2009; Laursen & Collins, 2009). Because the data were collected at two research sites in different regions of the US, we also included data collection site as a covariate for the four indices of adolescent functioning. Quantification of these covariates was as follows: (1) adolescent gender (0 = Male; 1 = Female); (2) adolescent age (years); (3) adolescent race (i.e., 0 = White; 1 = Black); (4) parental marital status (0 = married; 1 = unmarried); (5) parent report of annual household income ranging from 1 (< $6,000) to 13 ($125,000 or more); and (6) data collection site (1 = Northeast; 2 = Midwest). Following guidelines for addressing potential confounds in the assessment of cortisol (see Adam & Kumari, 2009), we also initially assessed several possible covariates in cortisol analyses including: (1) adolescent consumption of food; (2) drinks; and (3) gum/candy in the hour prior to the cortisol assessment; (4) medication use (i.e., corticosteroid and contraceptive use); (5) smoking; and (6) time since awake.
Data Analysis Plan
Prior to conducting our analyses, we first examined whether data for the primary variables were missing completely at random (MCAR). The missing data analyses using Little’s MCAR (Little, 1988; Schlomer, Bauman, & Card, 2010) test indicated that the data were MCAR (χ2 = 409.188, df = 412, p = .53). Full-information maximum likelihood (FIML) methods for estimating data successfully minimize bias in regression and standard error estimates for all types of missing data when the amount of missing data is less than 20% (Schlomer et al., 2010). Therefore, given that data in our sample were missing for 13% of the values, we used FIML to retain the full sample of families for primary analyses. All primary analyses were conducted using structural equation model (SEM) analyses with Amos 25.0 software (Arbuckle, 2014).
To test the linear and curvilinear nature of interparental conflict in the proposed risk cascade, we used latent difference score (LDS; McArdle, 2009) analyses to capture individual differences in intraindividual change in youth reactivity and problems. LDS change analyses were specifically estimated for adolescent: (1) AUCG and AUCI cortisol in the period surrounding family conflict from Waves 1 to 2; (2) emotional reactivity to family conflict from Waves 1 to 2; and (3) psychological problems from Waves 1 to 3. Following recommended practices for LDS analyses, we specifically regressed the later assessment of each target construct onto the previous assessment of the variable and the latent difference score while constraining both paths to 1 (see McArdle, 2009). Using the standard approach for estimating the proportional change components in the LDS analyses, we also specified a structural path between the initial level of the variable and the latent growth parameter for the youth cortisol, emotional reactivity, and psychological problems constructs (e.g., McArdle, 2009).
To test our primary aim of examining curvilinear effects, we estimated paths running from: (1) interparental conflict and its quadratic term to LDS changes from Waves 1 to 2 in adolescent emotional reactivity, AUCG cortisol, AUCI cortisol, and psychological problems, and (2) LDS changes in adolescent emotional reactivity, AUCG cortisol, and AUCI cortisol and LDS changes in their psychological problems from Waves 1 to 3. The interparental conflict composite was centered prior to creation of the quadratic interparental conflict term. Given the significant relations between time since awake and the cortisol measures, the difference in time since awake was examined as a covariate of LDS changes in AUCG and AUCI cortisol. As general covariates, family income, marital status, data collection site, and adolescent age, race, gender, and the difference in time since awake from Waves 1 to 2 were also initially estimated as predictors of LDS changes in all four endogenous variables. However, marital status, family income, adolescent age, and adolescent race did not predict any of the endogenous variables or alter the pattern of significant findings in the analyses. Therefore, only adolescent gender and data collection site were retained in the primary analyses due to their roles as significant predictors of at least one endogenous variable. In addition, we estimated correlations among: (1) all the variables assessed at Wave 1, (2) the residuals of the LDS growth parameters for the three mediators, and (3) error terms of comparable manifest indicators of psychological problems across the waves to control for informant variance. For clarity of presentation, correlations between exogenous predictors are not depicted in the figure (see Table 2 for correlations).
Table 2.
Means, Standard Deviations, and Correlations Among the Primary Variables in the Study.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariates & Predictors | |||||||||||||||
| 1. Child Gender | -- | ||||||||||||||
| 2. Data Collection Site | .04 | -- | |||||||||||||
| 3. ΔW1-W2 Time Since Awake | .07 | −.05 | -- | ||||||||||||
| 4. Wave 1 Interparental Conflict | −.01 | .09 | .03 | -- | |||||||||||
| Wave 1 Youth Reactivity to Family Conflict | |||||||||||||||
| 5. Behavioral Distress | .09 | −.01 | −.03 | .18* | -- | ||||||||||
| 6. AUCG Cortisol | .10 | −.04 | .17* | −.11 | .01 | -- | |||||||||
| 7. AUCI Cortisol | −.15* | .02 | −.07 | .08 | −.02 | −.40* | -- | ||||||||
| Wave 2 Youth Reactivity to Family Conflict | |||||||||||||||
| 8. Behavioral Distress | .29 | −.01 | .07 | .33* | .53* | .11 | −.12 | -- | |||||||
| 9. AUCG Cortisol | .01 | −.15* | −.23* | .02 | .02 | .37* | −.01 | .04 | -- | ||||||
| 10. AUCI Cortisol | −.05 | .08 | .17* | .02 | −.01 | −.18* | .04 | .02 | −.40* | -- | |||||
| Wave 1 Youth Psychological Problems | |||||||||||||||
| 11. Maternal Report | −.05 | −.01 | .00 | .09 | .20* | .00 | −.04 | .17* | −.07 | .04 | -- | ||||
| 12. Paternal Report | −.02 | .05 | −.02 | .20* | .13* | −.09 | −.01 | .14* | −.01 | .16* | .62* | -- | |||
| 13. Teacher Report | −.04 | −.05 | .00 | .17* | .19* | −.04 | −.05 | .10 | .03 | .11 | .39* | 36* | -- | ||
| Wave 3 Youth Psychological Problems | |||||||||||||||
| 14. Maternal Report | .00 | .06 | −.13 | .10 | .04 | −.01 | −.02 | .11 | .02 | .00 | .71* | .54* | .30* | -- | |
| 15. Paternal Report | −.02 | .09 | −.04 | .16* | .04 | −.03 | .03 | .15* | .12 | .15* | .52* | .74* | .28* | .61* | -- |
| 16. Teacher Renort | 01 | −.08 | .04 | .07 | .04 | −.09 | .00 | .06 | −.01 | .16* | .38* | .43* | .72* | .34* | .35* |
Note. Child gender: 0 = boys; 1 = girls. Data collection site: 1 = Northeast; 2 = Midwest. Bolded coefficients denote correlations among the indicators of the higher order constructs of adolescent psychological problems.
p ≤ .05.
Finally, we also tested the measurement invariance for the latent construct of youth psychological problems by comparing the fit of a model in which indicators of each latent variable over time were constrained to be equal with a model in which the factor loadings were permitted to vary freely across the waves. Based on analytic recommendations (e.g., Schwartz, Rosiers, Huang, Zamboanga, Unger, Knight, … & Szapocznik, 2013), at least two of the following three conditions must be satisfied to accept the constrained model over the free-to-vary model: (1) the chi-square difference is non-significant; (2) decrease in CFI is no more than .01; and (3) increase in RMSEA is no more than .01. All conditions for supporting measurement invariance were met (Δ χ2 = 2.24, df = 2, p = .33; Δ CFI = .000; Δ RMSEA = .000). Thus, we adopted a more conservative approach of using the constrained measurement model in the primary analyses.
Results
Descriptive Analyses
Table 1 shows the means, standard deviations, and ranges for the primary variables and the specific indicators of composited variables. Consistent with previous research (e.g., Gunnar, Talge, & Herrera, 2009; Kobak, Zajac, Levine, 2009), the negative AUCI values reflect that the adolescents, on average, experienced decreases in cortisol levels from the pre-task to post-task assessments surrounding the family conflict task and are consistent with the normative diurnal pattern of cortisol (Saxbe, Margolin, Spies, Shaprio, & Baucom, 2012). However, positive AUC values for 22% of the sample at each wave indicates that a notable subset of adolescents exhibited increases in cortisol from the pre-conflict to post-conflict assessments. Thus, as a measure of cortisol reactivity to interparental conflict (Saxbe et al., 2012), AUCI captures change (i.e., increases and decreases) rather than simply cortisol increases (Khoury Gonzalez, Levitan, Pruessner, Chopra, Santo Basile, … & Atkinson, 2015). Table 2 displays the correlations between the covariates and primary variables in the analyses. As denoted by the bolded coefficients in the table, correlations among the indicators of the higher order constructs of adolescent psychological problems at each wave were generally moderate to strong in magnitude (Mean r = .45).
Table 1.
Means, standard deviations, and ranges for key variables in the study.
| Mean | SD | Range | |
|---|---|---|---|
| Wave 1 Interparental Conflict | 0.00 | 0.71 | −1.09-2.68 |
| 1. Maternal OPS | 9.75 | 5.08 | 0-30 |
| 2. Paternal OPS | 10.15 | 5.15 | 0-27 |
| 3. Maternal IPST survey rating | 0.87 | 1.02 | 0-4.25 |
| 4. Paternal IPST survey rating | 0.76 | 1.01 | 0-5 |
| 5. Observer ratings of maternal IPST behavior | 1.90 | 0.87 | 0-4.83 |
| 6. Observer ratings of paternal IPST behavior | 1.68 | 0.88 | 0-4.83 |
| Wave 1 Cortisol (μg/dl) | -- | -- | -- |
| 7. Baseline | .09 | .09 | .01-.60 |
| 8. Post I | .08 | .07 | .01-.65 |
| 9. Post II | .06 | .05 | .01-.39 |
| 10. Post III | .06 | .05 | .01-.42 |
| 11. AUCG | 3.38 | 2.23 | 0.46-11.19 |
| 12. AUCI | −.58 | 0.92 | −3.81-2.63 |
| Wave 2 Cortisol (μg/dl) | -- | -- | -- |
| 7. Baseline | .10 | .08 | .01-.85 |
| 8. Post I | .08 | .09 | .01-1.15 |
| 9. Post II | .08 | .13 | .01-1.76 |
| 10. Post III | .07 | .04 | .01-.30 |
| 11. AUCG | 3.72 | 2.11 | .50-11.11 |
| 12. AUCI | −.59 | 0.96 | −3.95-2.77 |
| Wave 1 Adolescent Distress | 4.89 | 1.73 | 1.33-8.67 |
| 13. Affected Behavior | 4.54 | 2.51 | 1-9 |
| 14. Mobilizing Behavior | 4.66 | 2.43 | 1-9 |
| 15. Controlling | 4.19 | 2.70 | 1-9 |
| 16. Assertiveness (reverse scored) | 5.34 | 2.09 | 1-9 |
| 17. Comfort (reverse scored) | 5.57 | 2.19 | 1-9 |
| 18. Security (reverse scored) | 5.05 | 2.31 | 1-9 |
| Wave 2 Adolescent Distress | 4.64 | 1.52 | 1.33-8.17 |
| 10. Affected Behavior | 4.03 | 2.35 | 1-9 |
| 20. Mobilizing Behavior | 4.20 | 2.31 | 1-9 |
| 21. Controlling | 4.28 | 2.58 | 1-9 |
| 22. Assertiveness (reverse scored) | 5.30 | 2.04 | 1-9 |
| 23. Comfort (reverse scored) | 5.14 | 2.07 | 1-9 |
| 24. Security (reverse scored) | 4.90 | 2.31 | 1-9 |
| Wave 1 Adolescent Psychological Problems | -- | -- | -- |
| 25. Mother | 11.61 | 10.71 | 0-52 |
| 26. Father | 11.54 | 11.06 | 0-57 |
| 27. Teacher | 2.93 | 3.57 | 0-21 |
| Wave 2 Adolescent Psychological Problems | -- | -- | -- |
| 28. Mother | 9.23 | 9.41 | 0-54 |
| 29. Father | 9.74 | 10.80 | 0-67 |
| 30. Teacher | 2.73 | 2.87 | 0-17 |
Primary Analyses: Curvilinear Risk of Interparental Conflict
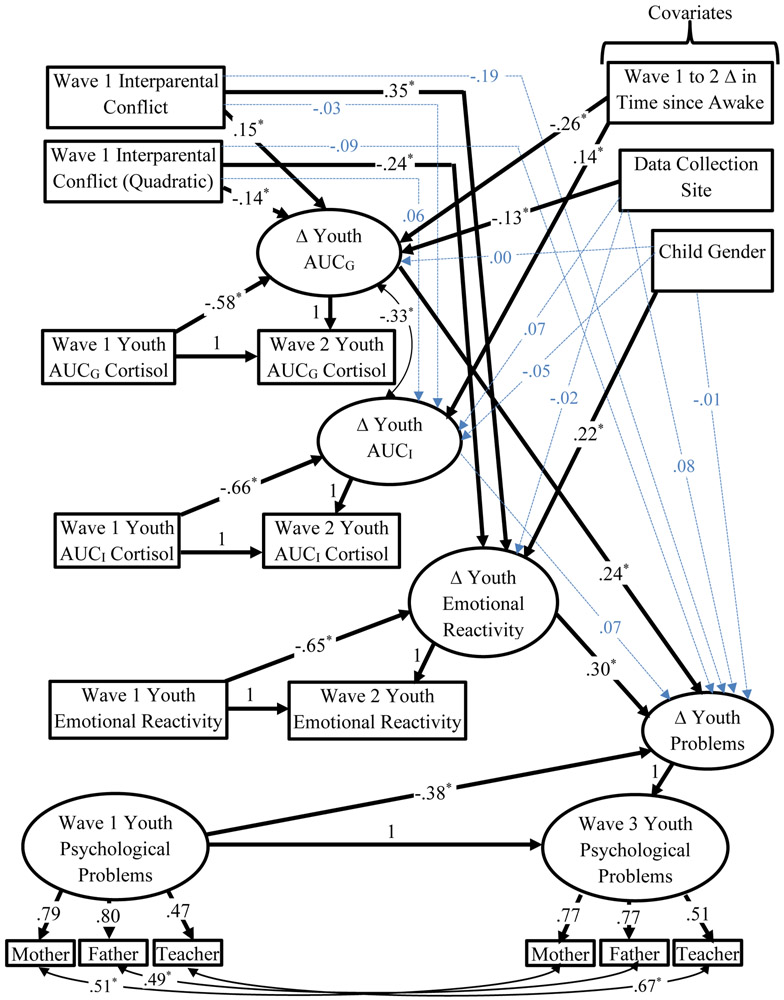
As a first step in conducting the analyses, we examined whether the inclusion of the quadratic interparental conflict term added any unique explanatory power to the primary model depicted in Figure 2. Comparison of a model in which the four predictive paths involving the quadratic term (i.e., LDS change in adolescent emotional reactivity, AUCG cortisol, AUCI cortisol, and psychological problems) were permitted to vary freely with a model in which they were constrained to 0 indicated that the free-to-vary model was a significantly better fit, Δ χ2 (4, N = 258) = 14,41, p = .006. Given that the inclusion of the quadratic interparental conflict term offered unique power as a predictor, we proceeded to report the results of the freely estimated model presented in the analysis plan. The model, which is presented in Figure 2, provided a good representation of the data, χ2 (65, N = 258) = 93.82, p = .01, RMSEA = .04, CFI = .97, and χ2/df ratio = 1.44. Supporting the measurement model, loadings of the manifest indicators for the latent constructs were significant (p < .001) and, on average, moderate to high in strength (mean loading = .69). Consistent with prior associations between initial level and change in psychological functioning over time (e.g., King, King, McArdle, Shaley, & Doron-LaMarca, 2009), Wave 1 levels of emotional reactivity, cortisol, and psychological problems were all negatively correlated with their subsequent change over time. For the covariates, child gender predicted latent change in youth emotional reactivity to family conflict (β = .21, p < .001), with girls exhibiting greater emotional reactivity over time than boys. As expected, increases in time since awake from Waves 1 to 2 were associated with decreases in AUCG cortisol, β = −.26, p < .001, and increases in AUCI cortisol, β = .14, p = .009. Finally, the only other significant covariate path between data collection site and AUCG cortisol indicated that youth from the Northeastern site exhibited greater AUCG cortisol than their Midwestern counterparts, β = −.13, p = .01.
Figure 2.
Structural equation model testing interparental conflict as a curvilinear predictor of a mediational cascade of youth changes in cortisol, negative emotional reactivity to family conflict and psychological problems using latent difference score analyses. Note. * p < .05.
For paths relevant to our research questions, latent change in adolescent AUCI cortisol was not significantly related to the linear and quadratic interparental conflict variables or their changes in psychological problems from Waves 1 to 3. However, interparental conflict was a significant predictor of greater youth AUCG cortisol, β = .15, p = .03, and emotional reactivity to family conflict, β = .35, p < .001, over the one-year period. Changes in AUCG cortisol and emotional reactivity to conflict, in turn, were each predictors of adolescent psychological problems across a two-year span: β = .21, p = .02 and β = .30, p = .002, respectively. Asymmetrical confidence interval analyses provided additional support for the mediational role of AUCG cortisol and emotional reactivity to conflict (Preacher & Hayes, 2008). Indirect paths involving interparental conflict and adolescent psychological problems were specifically significant for youth AUCG cortisol, 95% CI [.23, 1.16]; and their emotional reactivity to family conflict, 95% CI [.12, .53] as explanatory mechanisms.
However, the paths in the first links of the mediational chains were further qualified by the role of the quadratic interparental conflict term in significantly predicting LDS change in AUCG cortisol, β = −.14, p = .04, r2 = .064, and emotional reactivity to family conflict, β = −.24, p < .001, r2 = .105, across the one-year period. Additional asymmetrical confidence interval analyses supported the roles of AUCG cortisol and emotional reactivity to conflict as mediators of the association between the quadratic interparental conflict variable and adolescent psychological difficulties. More specifically, the indirect path for the quadratic interparental conflict term, adolescent AUCG cortisol, and their psychological difficulties was significant, 95% CI [−.39, −.01]. Likewise, the comparable path for the interparental conflict term, adolescent AUCG cortisol, and their psychological difficulties was also significant, 95% CI [−.83, −.19].
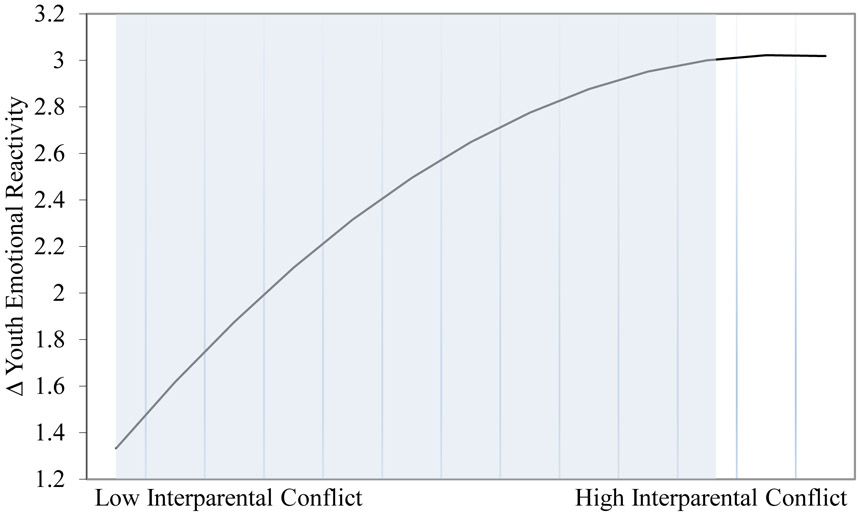
To characterize the form of the quadratic relation between interparental conflict and adolescent emotional reactivity, we calculated graphical plots at +/− 1 SD from the mean of interparental conflict as a moderator. As shown in Figure 3, the quadratic effect of interparental conflict followed a concave downward function whereby the relatively strong positive association between interparental conflict and subsequent change in youth emotional reactivity progressively decreased with increases in interparental conflict. Simple slope analyses revealed that interparental conflict was a significant predictor of subsequent increases in youth negative emotional reactivity to conflict at both low (− 1 SD), b = 1.09, p < .001, and high (+ 1 SD), b = 0.50, p < .001, levels of interparental conflict. As denoted by the gray shading in Figure 3, follow up regions of significance (RoS) on Z tests indicated that the association between interparental conflict and emotional reactivity was significant for all youth except for those who were exposed to very high levels of conflict (interparental conflict values ≥ 1.27). Analysis of the observed range of interparental conflict values revealed that 5% of the sample experienced levels of conflict in the very high region where interparental conflict was not a predictor of significant increases in their emotional reactivity.
Figure 3.
Graphical plot of the relation between the quadratic interparental conflict variable and subsequent LDS change in youth emotional reactivity to family conflict over a one year period. Gray shading denotes regions of significance for interparental conflict values below 1.27
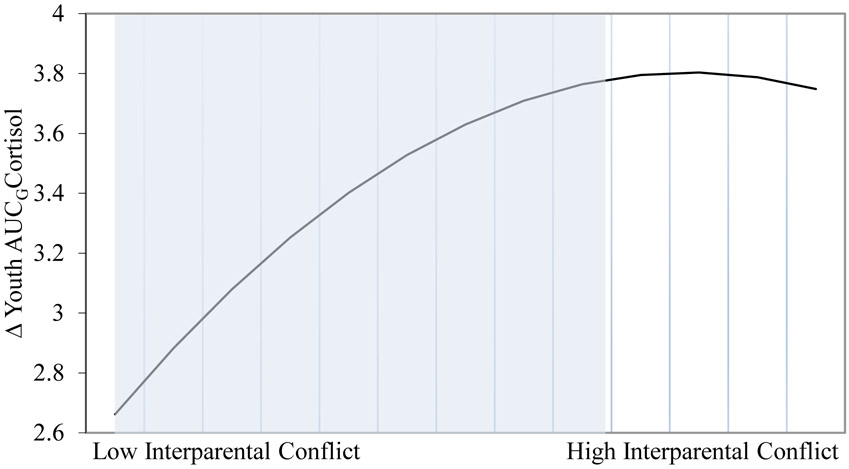
Figure 4 depicts the graphical plot for the curvilinear relation between interparental conflict and AUCG at +/− 1 SD from the mean of interparental conflict. Consistent with the downward concave shape of the emotional reactivity findings, the plot showed that the magnitude of the positive association between interparental conflict and subsequent change in AUCG cortisol successively weakened as adolescent exposure to conflict increased. In accord with the emotional reactivity results, simple slope analyses indicated that interparental conflict was a significant predictor of adolescent AUCG cortisol at low levels of conflict (−1 SD), b = 0.78, p = .02. However, the association between interparental conflict and adolescent AUCG cortisol was not significant at high levels of conflict (+1 SD), b = 0.24, p = .20. As depicted in the gray shaded region of Figure 4, RoS on Z tests showed that interparental conflict was a significant predictor of cortisol output for most of the youth (i.e., interparental conflict values < .25). Analysis of the observed range of interparental conflict values further revealed that interparental conflict was not a significant predictor of AUCG cortisol for the approximately 30% of the sample who were exposed to high levels of conflict.
Figure 4.
Graphical plot of the relation between the quadratic interparental conflict variable and subsequent LDS change in youth AUCG cortisol in the period around the family conflict across a one year period. Gray shading denotes regions of significance for interparental conflict values below .25.
Given that AUCG and AUCI cortisol were moderately correlated, it is also possible that the linear and curvilinear pathways involving AUCG as a mediator may be an artifact of collinearity among the cortisol measures. To test the stability of our findings for AUCG, we re-ran the model depicted in Figure 2 without AUCI cortisol. Reflecting the stability of the findings, the streamlined analyses yielded an identical pattern of significant results. In addition, the shape of the quadratic relationship between interparental conflict and youth emotional reactivity and AUCG cortisol followed the same concave downward shape as the original analyses.
Discussion
Although curvilinear models of family risk have gained considerable traction over the past decade, there is a paucity of research addressing the role of family factors as quadratic predictors of youth stress reactivity and their psychological adjustment (Davies & Sturge-Apple, 2007; Jouriles et al., 2016; Susman, 2006). Against this backdrop, the present study was designed to break new ground by exploring whether interparental conflict increased adolescent risk for psychological problems through its linear and curvilinear associations with their emotional reactivity and cortisol responses to family conflict. In accord with linear models of emotional and physiological functioning as risk mechanisms of interparental conflict (e.g., Davies et al., 2016; Labella & Masten, 2018; Morris et al., 2017), the findings indicated that interparental conflict predicted increases over a one-year period in youth emotional reactivity to family conflict and overall cortisol (i.e., AUCG) output during their lab visit. Increases in emotional reactivity and cortisol output, in turn, were positively associated with changes in psychological problems over a two-year period. However, consistent with curvilinear risk models of interparental conflict, these linear pathways were further qualified by quadratic associations in the first link in the risk chain. More specifically, the quadratic interparental conflict term was a significant predictor of subsequent increases in youth negative emotional reactivity and AUCG cortisol. Findings from follow up analyses and graphic plots were consistent with the downward concave function proposed by risk saturation models (Morris et al., 2010; Susman, 2006). Thus, the relatively strong relation between interparental conflict and adolescent emotional reactivity to family conflict and overall cortisol output became progressively weaker at higher levels of conflict.
Findings from the linear analyses indicating that adolescent emotional reactivity and AUCG cortisol served as explanatory mechanisms linking interparental conflict with an increased likelihood of psychological problems are consistent with several theoretical models. For example, the risky family model posits that interparental conflict is a form of family adversity that, over the longer term, gradually increases children’s psychological problems by progressively sensitizing their short-term emotional reactivity and physiological arousal (Repetti et al., 2011). In this conceptualization, the dynamic nature of children’s adaptation to family stress and their broader psychological adjustment are metaphorically represented as a series of interlocking, shifting gears. Our LDS tests of mediation represent a first step in supporting this unfolding cascade of risk by demonstrating that interparental conflict was associated with greater emotional reactivity and cortisol output over time. As part of the metaphorical turning of gears, these changes, in turn, predicted interlocking and successive changes in youth psychological difficulties across a two-year period.
Emotional security theory provides a further conceptual context for interpreting findings on the mediational role of emotional reactivity (Davies et al., 2016; Jouriles et al., 2016). According to this theory, interparental conflict increases offspring vulnerability to emotional, behavioral, and social problems by increasing their prioritization of defending against social danger in the family. Because greater negative emotional reactivity is conceptualized as a central barometer of threats to children’s security in the family, emotional security theory proposes that it is a robust risk mechanism underpinning the risk of exposure to interparental hostility. Thus, greater emotional reactivity following exposure to frequent, lengthy, and intense bouts of interparental conflict may reflect adolescents’ increasing concerns about their safety. Moreover, according to emotional security theory, greater emotional reactivity to family conflict may confer more proximal risk for psychopathology through several mechanisms. For example, insecurity underlying emotional reactivity is proposed to undermine mental health by disrupting sleep quality (El-Sheikh, Buckhalt, Cummings, & Keller, 2006). Likewise, the saliency of defending against interpersonal threat may limit the pursuit of other important approach-oriented goals (e.g., exploration, affiliation) that lay the foundation for social competence, prosocial behavior, and mastery of the physical world (Davies & Martin, 2014). Finally, increases in emotional reactivity may increase psychopathology over time through the proliferation of hyper-vigilant templates of responding (e.g., hostile attribution biases) to other interpersonal contexts outside the family (e.g., peer contexts) (Luebbe, Bell, Allwood, Swenson, & Early, 2010).
Although relatively little is known about why greater cortisol output during the day may mediate the risk associated with interparental conflict, neurobiological models have posited that upregulation of cortisol resulting from exposure to family discord may result in neuronal degeneration in multiple brain regions that are critical to mental health (DeBellis & Thomas, 2003; Laurent, Gilliam, Wright, & Fisher, 2015). For example, stress-related increases in cortisol have been linked with damage to the prefrontal cortex and resulting impairments in executive functions (e.g., working memory, attention, planning), self-control, and emotion regulation (Kamin & Kertes, 2017; Roberts & Lopez-Duran, 2019). Likewise, some research supports the hypothesis that elevated cortisol levels may disrupt learning, processing, and memory for emotionally significant events and the regulation of fear and stress responses by triggering cell death in the amygdala and hippocampus (Kamin & Kurtes, 2017; Roberts & Lopez-Duran, 2019; Simmons, Howard, Simpson, Akil, & Clinton, 2012). Consistent with this premise, previous findings have indicated that children’s elevated diurnal cortisol is associated with their exposure to interparental discord and subsequent vulnerability to internalizing and externalizing problems (Pendry & Aadm, 2007; Saltzman et al., 2005; Shirtcliff & Essex, 2008).
Guided by curvilinear models of family risk, our results also revealed that quadratic associations among interparental conflict and changes in youth emotional reactivity to family conflict and overall cortisol output during the lab visit qualified the linear relations among these variables. In characterizing the nature of the quadratic effects, we specifically examined two complementary conceptualizations prevailing in the literature. According to the challenge model, mild to moderate levels of interparental conflict facilitate the development of effective coping strategies that inoculate children from subsequent stress and reduce levels of behavioral (i.e., emotional distress) and hormonal (i.e., cortisol) stress responses (Davies & Sturge-Apple, 2007; Jouriles et al., 2016; Repetti & Robles, 2016). Thus, this model proposes a U-shaped function reflecting that low and high levels of destructive conflict engender the most reactivity (see Figure 1a) and physiological arousal. As a theoretical complement (see Figure 1b), the risk saturation model proposes a downward concave form of risk in which the sensitizing effect of interparental conflict on stress reactivity and arousal wanes when discord reaches severe levels (Davies & Sturge-Apple, 2007; Morris et al., 2010; Susman, 2006). The shape of the curvilinear effects in our study provided decisive support for the risk saturation model over the challenge model. More specifically, the relatively potent role of interparental conflict as a predictor of youth emotional reactivity to conflict and overall cortisol output (i.e., AUCG) over a one-year period became significantly weaker as conflict increased to high levels.
Why might the risk of interparental conflict become saturated when discord reaches high levels? As one possible explanation, youth emotional reactivity and physiological arousal may stabilize when the hostility between parents becomes intense or protracted because it triggers dissociation or defensive exclusion of the interpersonal threat. In support of this explanation, the emotional security theory proposes that the tendency to actively avoid and inhibit negative response processes is a common strategy for coping when hostility and anger between parents is intense (Davies et al., 2016). In offering a complementary interpretation, the attenuation hypothesis postulates that sensitization of stress systems operates within constrained boundaries of exposure to environmental adversity. Accordingly, as adversity increases beyond ill-defined levels, it is theorized to trigger down regulation in physiological and emotional systems (Kamin & Kertes, 2017; Susman, 2006). Interpreted within this framework, the progressively weaker association between interparental conflict and youth emotional and physiological arousal may reflect the beginning of this down regulation process. In drawing on stress autonomy and experiential canalization models in developmental psychopathology (Blair & Raver, 2012; Monroe & Harkness, 2005; Morris et al., 2010), a related explanation is that negative emotional reactivity and cortisol levels reach asymptotes after long histories of exposure to interparental adversity. Thus, the intense conflicts may be a proxy for long histories of exposure to interparental conflict that engender highly automatic and intractable forms of emotional reactivity and physiological arousal, which, over development, become canalized and resistant to subsequent environmental stressors. These conceptual explanations highlight several properties of interparental conflict (e.g., intensity, history of exposure, unpredictability) that may underpin the curvilinear risk. Therefore, parsing relations between specific properties of interparental conflict and youth reactivity to family conflict is an important direction for future research.
Towards further integrating our findings into the literature, it is also important to note that our findings diverge from some studies on reactivity to conflict in two developmentally meaningful ways. First, in highlighting the complexity of the cortisol literature, previous evidence is mixed regarding whether elevated or dampened HPA axis activity is a risk mechanism underlying family adversity. For example, destructive interparental conflict has been associated with dampened cortisol responding to family stressors in some studies (e.g., Davies et al., 2007; Luecken et al, 2009). However, these studies focused on childhood or early adulthood rather than adolescence. In the broader developmental psychopathology literature, research suggests that a distinctive shift in HPA axis functioning occurs during early adolescence. Research specifically indicates that adolescents experiencing risk evidence heightened, rather than dampened, cortisol output in response to stressors (e.g., Gunnar, Wewerka, Frenn, Long, & Griggs, 2009; Hankin, 2012). Consistent with this work, neurobiological models have suggested that this developmental switch may result from changes in the HPA axis itself (e.g., stress reactivity of the pituitary gland and adrenal cortex) and brain regions (e.g., limbic system, prefrontal cortex) that organize responses to interpersonal threat (Folib, Lui, & Romeo, 2011; Kamin & Kertes, 2017; Marceau, Ruttle, Shirtcliff, Essex, & Susman, 2014).
Second, in contrast to previous empirical evidence supporting the linkage between heightened emotional reactivity and cortisol responses to family stress (Davies et al., 2008; Koss et al., 2013), youth cortisol activity (AUCG) and reactivity (AUCI) to family conflict in our study were unrelated to their emotional reactivity. Even though the results showed that emotional reactivity and overall cortisol activity function were comparable in their roles as risk mechanisms, they functioned independently from each other in the pathogenic cascade. It is possible that variations in findings between our study and previous research result from differences in measurement (e.g., actual family conflict task versus simulated parental conflict) and design (e.g., lagged longitudinal versus largely cross-sectional data). However, from a theoretical perspective, it is also plausible that the independent operation of physiological and behavioral systems is the result of an orthogenetic process of increasing differentiation and hierarchical reorganization of domains of functioning across development (Raeff, 2011). For example, as noted above, changes in components of the HPA axis, interrelated neurobiological systems (e.g., hypothalamic-pituitary-gonadal axis), and brain regions organizing the processing of socio-emotional stimuli and regulation of emotion during adolescence may be implicated in increasing compartmentalization of behavioral and HPA systems. Consistent with this interpretation, studies documenting associations between behavioral and cortisol reactivity to family conflict were conducted with elementary school children (e.g., Davies et al., 2008; Koss et al., 2013).
The orthogonality of the systems may also reflect that different mechanisms underpin the curvilinear relations between interparental conflict and youth emotional reactivity to family conflict and their overall cortisol arousal. For example, whereas emotional security theory has largely centered on understanding the development of behavioral forms of children’s reactivity to conflict (Davies et al., 2016), the attenuation model is predominantly focused on identifying the antecedents and course of HPA functioning (Kamin & Kertes, 2017; Susman, 2006). Further underscoring the distinctive operation of the HPA axis from emotional reactivity, the findings did not support the role of adolescent cortisol reactivity to family conflict (AUCI) as mediating mechanism of interparental conflict. Rather, the findings indicated that interparental conflict was a linear and quadratic predictor of increases in overall cortisol arousal (AUCG) in the lab visit over the course of the year, with cortisol arousal, in turn, increases in adolescent psychological problems. Thus, this raises the possibility that exposure to interparental conflict may play a role in altering how the HPA axis operates beyond the confines of family conflicts to the lab setting or, even more pervasively, to other challenging contexts.
Discussion of the limitations of the paper are also warranted. First, the findings from our largely working and middle-class sample of families are not necessarily generalizable to families from other backgrounds (e.g., economic impoverishment or privilege). Second, it is important to note that the magnitude of pathways between interparental conflict, youth reactivity, and their psychological problems were modest, particularly for cortisol output. Third, the null findings for AUCI cortisol as both an outcome of interparental conflict and a predictor of psychological problems may reflect the need for alternative methodological approaches for capturing cortisol reactivity. For example, although our three post-stressor measures of cortisol corresponded with the rise and peak in cortisol in response to stressors, it is possible that more frequent or lengthier assessments of saliva have increased the sensitivity of the cortisol variables. Fourth, although we considered several potential covariates, our approach may have missed other potential confounds (e.g., physical health, pubertal status), particularly in the analysis of adrenocortical functioning (Adam & Kumari, 2009). For example, early adolescence is a period of considerable pubertal change and some studies have reported that more advanced pubertal status is associated with previous experiences with family adversity and higher youth cortisol levels (e.g., Belsky, 2019; Gunnar et al., 2009; Shirtcliff et al., 2011). Thus, research has yet to examine the interplay between interparental conflict and youth cortisol levels, the existing findings raise the possibility that quicker pubertal timing or tempo may underpin links between interparental conflict and increases in adolescent cortisol (AUCG) levels during the lab visit. Thus, incorporating measures of puberty into studies on family conflict, youth cortisol levels, and psychopathology is an important direction for future research.
In concluding the limitations, it is also important to consider diversifying the conceptualization and operationalization of risk factors and processes. At the level of risk factors, the collective assessment of frequency, intensity, and duration in our composite of interparental conflict was based on quadratic models of family discord (Repetti & Robles, 2016). However, identifying the specific dimensions of interparental conflict that are responsible for the curvilinear nature of the risk is an important future direction. For example, in light of the significance of childhood experiential histories of family adversity for adolescent cortisol functioning (e.g., Martin et al., 2017; Stroud, Chen, Doane, & Granger, 2019), the duration and timing of exposure to interparental conflict may be key factors underpinning curvilinear risk. Relatedly, although our approach to assessing change in AUCG cortisol over the period of one year yielded findings that are consistent with previous theory and research, it is possible that relations between interparental conflict and AUCG and AUCI cortisol also operate on other time scales. For example, research suggests that some cortisol measures are more sensitive to changes in family conflict over periods of weeks rather than months (Kuhlman, Repetti, Reynolds, & Robles, 2016; Kuhlman, Ryan, Repetti, Reynolds, & Robles, 2018). Likewise, our measure of general psychopathology encompassing emotional, behavioral, and social problems may have masked distinctive pathways between dimensions of youth reactivity and forms of psychological problems. For example, some studies have indicated that elevated cortisol functioning predicts greater internalizing symptoms, whereas attenuated cortisol levels are related to more externalizing problems (Nelemans, Hale, Branje, van Lier, Jansen, Platje, & … Meeus, 2014; Shirtcliff, Granger, Booth, & Johnson, 2005; Smider, Essex, Kalin, Buss, Klein, Davidson, & Goldsmith, 2002). However, evidence for specificity in the sequelae of different cortisol dimensions is mixed (e.g., Stroud et al., 2019). Moreover, our decision to assess general psychopathology was guided by the repeated documentation of the prevalence and public health significance of a higher-order global psychopathology factor (e.g., Laceulle, Vollebergh, & Ormel, 2015).
Despite these limitations, this study broke new ground by examining the role of adolescent emotional responses to family conflict and overall cortisol arousal as explanatory mechanisms in prospective links between exposure to interparental conflict and their psychological problems. Our results supported a cascade in which interparental conflict ultimately increased youth vulnerability to psychopathology over a two-year period by serving as a linear predictor of increases over the subsequent year in their negative emotional reactivity to family conflict and overall cortisol levels during the lab visit. However, the linear associations among interparental conflict and the adolescent emotional reactivity and overall cortisol arousal were further qualified by a quadratic effect. Consistent with a risk saturation model (Davies & Sturge-Apple, 2007; Morris et al., 2010; Susman, 2006), the magnitude of interparental conflict as a predictor of emotional reactivity and cortisol output (i.e., AUCG cortisol) became progressively weaker as youth exposure to conflict increased, eventually reaching an asymptote at very high levels. At a mechanistic level, the findings may reflect the operation of several processes including defensive exclusion or dissociation as strategies to defuse intense threat (Davies et al., 2016), physiological attenuation to reduce toxic effects of physiological arousal (Susman, 2006), and the increasing canalization and intractability of high levels of reactivity to family conflict (Blair & Raver, 2012; Monroe & Harkness, 2005).
Acknowledgments
This research was supported by the National Institute of Mental Health (2R01 MH57318). We are grateful to the children, parents, and school staff who participated in the project, and to the project personnel at the University of Rochester and University of Notre Dame.
Contributor Information
Patrick T. Davies, University of Rochester
Lucia Q. Parry, University of Rochester
Sonnette M. Bascoe, Roberts Wesleyan College
Dante Cicchetti, University of Minnesota.
E. Mark Cummings, University of Notre Dame.
References
- Achenbach TM, Dumenci L, & Rescorla LA (2003). Are American children’s problems still getting worse? A 23-year comparison. Journal of Abnormal Child Psychology, 31, 1–11. 10.1023/A:1021700430364 [DOI] [PubMed] [Google Scholar]
- Adam EK, & Kumari M (2009). Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology, 34, 1423–1436. [DOI] [PubMed] [Google Scholar]
- Ahmed SP, Bittencourt-Hewitt A, & Sebastian CL (2015). Neurocognitive bases of emotion regulation development in adolescence. Developmental cognitive neuroscience, 15, 11–25. doi: 10.1016/j.dcn.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle JL (2017). Amos (Version 25.0) [Computer Program]. Chicago, IL: IMP SPSS. [Google Scholar]
- Blair C, & Raver CC (2012). Child development in the context of adversity: experiential canalization of brain and behavior. American Psychologist, 67, 309–318. doi: 10.1037/a0027493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehler C, Lange G, & Franck KL (2007). Adolescents' cognitive and emotional responses to marital hostility. Child development, 78, 775–789. 10.1111/j.1467-8624.2007.01032.x [DOI] [PubMed] [Google Scholar]
- Chaplin TM, & Aldao A (2013). Gender differences in emotion expression in children: A meta-analytic review. Psychological bulletin, 139, 735–765. doi: 10.1037/a0030737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings EM, Schermerhorn AC, Davies PT, Goeke-Morey MC, & Cummings JS (2006). Interparental discord and child adjustment: Prospective investigations of emotional security as an explanatory mechanism. Child development, 77, 132–152. DOI: 10.1111/j.1467-8624.2006.00861.x [DOI] [PubMed] [Google Scholar]
- Davies PT, Cicchetti D, & Martin MJ (2012). Toward greater specificity in identifying associations among interparental aggression, child emotional reactivity to conflict, and child problems. Child Development, 83, 1789–1804. doi: 10.1111/j.1467-8624.2012.01804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies P & Martin M (2014). Children’s coping and adjustment in high-conflict homes: The reformulation of emotional security theory. Child Development Perspectives, 8, 242–249. DOI: 10.1111/cdep.12094 [DOI] [Google Scholar]
- Davies PT, Martin MJ, & Sturge-Apple ML (2016). Emotional security theory and developmental psychopathology. In Cicchetti D (Ed.), Developmental Psychopathology: Vol. 1. Theory and Methods (3rd ed., 199–264). New York: Wiley. [Google Scholar]
- Davies PT, & Sturge-Apple ML (2007). Advances in the formulation of emotional security theory: An ethologically based perspective. Advances in child development and behavior, 35, 87–137. DOI: 10.1016/B978-0-12-009735-7.50008-6 [DOI] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cicchetti D, & Cummings EM (2007). The role of child adrenocortical functioning in pathways between interparental conflict and child maladjustment. Developmental psychology, 43, 918–930. doi: 10.1037/0012-1649.43.4.918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cicchetti D, Manning LG, & Zale E (2009). Children’s patterns of emotional reactivity to conflict as explanatory mechanisms in links between interpartner aggression and child physiological functioning. Journal of Child Psychology and Psychiatry, 50, 1384–1391. doi: 10.1111/j.1469-7610.2009.02154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, & Thomas LA (2003). Biologic findings of post-traumatic stress disorder and child maltreatment. Current psychiatry reports, 5, 108–117. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, & Cummings EM (2004). Relations of husbands' and wives' dysphoria to marital conflict resolution strategies. Journal of Family Psychology, 18, 171–183. 10.1037/0893-3200.18.171 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA, Cummings EM, & Keller P (2007). Sleep disruptions and emotional insecurity are pathways of risk for children. Journal of Child Psychology and Psychiatry, 48, 88–96. doi: 10.1111/j.1469-7610.2006.01604.x [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P (2013). Childhood poverty, chronic stress, self-regulation, and coping. Child Development Perspectives, 7, 43–48. 10.1111/cdep.12013 [DOI] [Google Scholar]
- Folib AR, Lui P, Romeo RD (2011). The transformation of hormonal stress responses throughout puberty and adolescence. Journal of Endocrinology, 210, 391–398. doi: 10.1530/JOE-11-0206. [DOI] [PubMed] [Google Scholar]
- Fosco GM, & Grych JH (2010). Adolescent triangulation into parental conflicts: Longitudinal implications for appraisals and adolescent-parent relations. Journal of Marriage and Family, 72, 254–266. 10.1111/j.1741-3737.2010.00697.x [DOI] [Google Scholar]
- Garmezy N, Masten AS, & Tellegen A (1984). The study of stress and competence in children: A building block For developmental psychopathology. Child development, 97–111. DOI: 10.2307/1129837 [DOI] [PubMed] [Google Scholar]
- Goodman R, & Scott S (1999). Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: is small beautiful? Journal of Abnormal Child Psychology, 27, 17–24. 10.1023/A:1022658222914 [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Talge NM, & Herrera A (2009). Stressor paradigms in developmental studies: What does and does not work to produce mean increases in salivary cortisol. Psychoneuroendocrinology, 34, 953–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar MR, Wewerka S, Frenn K, Long JD, & Griggs C (2009). Developmental changes in hypothalamus–pituitary–adrenal activity over the transition to adolescence: normative changes and associations with puberty. Development and psychopathology, 21, 69–85. doi: 10.1017/S0954579409000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyer AE, Silk JS, & Nelson EE (2016). The neurobiology of the emotional adolescent: From the inside out. Neuroscience & Biobehavioral Reviews, 70, 74–85. doi: 10.1016/j.neubiorev.2016.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2012). Future directions in vulnerability to depression among youth: integrating risk factors and processes across multiple levels of analysis. Journal of Clinical Child & Adolescent Psychology, 41, 695–718. doi: 10.1080/15374416.2012.711708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2015). Depression from childhood through adolescence: risk mechanisms across multiple systems and levels of analysis. Current Opinion in Psychology, 4, 13–20. DOI: 10.1016/j.copsyc.2015.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harold GT, & Sellers R (2018). Annual Research Review: Interparental conflict and youth psychopathology: An evidence review and practice focused update. Journal of Child Psychology and Psychiatry, 59, 374–402. doi: 10.1111/jcpp.12893 [DOI] [PubMed] [Google Scholar]
- Ji J, Negriff S, Kim H, & Susman EJ (2016). A study of cortisol reactivity and recovery among young adolescents: heterogeneity and longitudinal stability and change. Developmental psychobiology, 58, 283–302. 10.1177/1099800417697380 [DOI] [PubMed] [Google Scholar]
- Jouriles EN, McDonald R, & Kouros CD (2016). Interparental conflict and child adjustment. In Cicchetti D (Ed.), Developmental psychopathology: Vol. 4: Risk, resilience, and intervention (pp. 608–659). New York: Wiley. doi: 10.1002/9781119125556.devpsy412 [DOI] [Google Scholar]
- Juster RP, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, … & Fiocco AJ (2011). A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Development and Psychopathology, 23, 725–776. doi: 10.1017/S0954579411000289. [DOI] [PubMed] [Google Scholar]
- Kamin HS, & Kertes DA (2017). Cortisol and DHEA in development and psychopathology. Hormones and Behavior, 89, 69–85. doi: 10.1016/j.yhbeh.2016.11.018. [DOI] [PubMed] [Google Scholar]
- Koss KJ, George MR, Davies PT, Cicchetti D, Cummings EM, & Sturge-Apple ML (2013). Patterns of children's adrenocortical reactivity to interparental conflict and associations with child adjustment: A growth mixture modeling approach. Developmental Psychology, 49, 317–326. 10.1037/a0028246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss KJ, & Gunnar MR (2018). Annual research review: Early adversity, the hypothalamic–pituitary–adrenocortical axis, and child psychopathology. Journal of Child Psychology and Psychiatry, 59, 327–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury JE, Gonzalez A, Levitan RD, Pruessner JC, Chopra K, Santo Basile V, … & Atkinson L (2015). Summary cortisol reactivity indicators: Interrelations and meaning. Neurobiology of Stress, 2, 34–43. 10.1016/j.ynstr.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DW, King LA, McArdle JJ, Shalev AY, & Doron-LaMarca S (2009). Sequential temporal dependencies in associations between symptoms of depression and posttraumatic stress disorder: An application of bivariate latent difference score structural equation modeling. Multivariate Behavioral Research, 44, 437–464. doi: 10.1080/00273170903103308 [DOI] [PubMed] [Google Scholar]
- Kobak R, Zajac K, & Levine S (2009). Cortisol and antisocial behavior in early adolescence: The role of gender in an economically disadvantaged sample. Development and Psychopathology, 21, 579–591. doi: 10.1017/S0954579409000315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraft AJ, & Luecken LJ (2009). Childhood parental divorce and cortisol in young adulthood: evidence for mediation by family income. Psychoneuroendocrinology, 34(9), 1363–1369. [DOI] [PubMed] [Google Scholar]
- Kuhlman KR, Repetti RL, Reynolds BM, & Robles TF (2016). Change in parent-child conflict and the HPA-axis: Where should we be looking and for how long?. Psychoneuroendocrinology, 68, 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlman KR, Repetti RL, Reynolds BM, & Robles TF (2018). Interparental conflict and child HPA-axis responses to acute stress: Insights using intensive repeated measures. Journal of Family Psychology, 32, 773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labella MH, & Masten AS (2018). Family influences on the development of aggression and violence. Current opinion in psychology, 19, 11–16. doi: 10.1016/j.copsyc.2017.03.028. [DOI] [PubMed] [Google Scholar]
- Laceulle OM, Vollebergh WA, & Ormel J (2015). The structure of psychopathology in adolescence: replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science, 3, 850–860. 10.1177/2167702614560750 [DOI] [Google Scholar]
- Laurent HK, Gilliam KS, Wright DB, & Fisher PA (2015). Child anxiety symptoms related to longitudinal cortisol trajectories and acute stress responses: Evidence of developmental stress sensitization. Journal of abnormal psychology, 124, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen B, & Collins WA (2009). Parent—child relationships during adolescence. Handbook of adolescent psychology, 2. [Google Scholar]
- Little RJ (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, 1198–1202. DOI: 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Luebbe AM, Bell DJ, Allwood MA, Swenson LP, & Early MC (2010). Social information processing in children: Specific relations to anxiety, depression, and affect. Journal of Clinical Child & Adolescent Psychology, 39, 386–399. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Kraft A, & Hagan MJ (2009). Negative relationships in the family-of-origin predict attenuated cortisol in emerging adults. Hormones and Behavior, 55, 412–417. doi: 10.1016/j.yhbeh.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik NM, & Lindahl KM (2004). System for coding interactions in dyads (SCID). Couple observational coding systems, 173–188. 10.4324/9781410610843 [DOI] [Google Scholar]
- Marceau K, Ruttle PL, Shirtcliff EA, Essex MJ, & Susman EJ (2015). Developmental and contextual considerations for adrenal and gonadal hormone functioning during adolescence: Implications for adolescent mental health. Developmental Psychobiology, 57, 742–768. doi: 10.1002/dev.21214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin MJ, Davies PT, Cummings EM, & Cicchetti D (2017). The mediating roles of cortisol reactivity and executive functioning difficulties in the pathways between childhood histories of emotional insecurity and adolescent school problems. Development and psychopathology, 29, 1483–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12, 23–44. DOI: 10.1037/1082-989X.12.1.23 [DOI] [PubMed] [Google Scholar]
- McArdle JJ (2009). Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology, 60, 577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- Monroe SM, & Harkness KL (2005). Life stress, the" kindling" hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychological Review, 112, 417–445. DOI: 10.1037/0033-295X.112.2.417 [DOI] [PubMed] [Google Scholar]
- Morris MC, Ciesla JA, & Garber J (2010). A prospective study of stress autonomy versus stress sensitization in adolescents at varied risk for depression. Journal of Abnormal Psychology, 119, 341–354. 10.1037/a0019036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Houltberg BJ, Criss MM, & Bosler CD (2017). Family context and psychopathology: The mediating role of children's emotion regulation. In Centifanti LC & Williams DM (Eds.), The Wiley Handbook of Developmental Psychopathology (pp. 365–389). Hoboken, NJ: Wiley. 10.1002/9781118554470.ch18 [DOI] [Google Scholar]
- Nelemans SA, Hale WW, Branje SJ, van Lier PA, Jansen LM, Platje E, … & Meeus WH (2014). Persistent heightened cortisol awakening response and adolescent internalizing symptoms: a 3-year longitudinal community study. Journal of Abnormal Child Psychology, 42, 767–777. DOI: 10.1007/s10802-013-9820-2 [DOI] [PubMed] [Google Scholar]
- Pendry P, & Adam EK (2007). Associations between parents' marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development, 31, 218–231. 10.1177/0165025407074634 [DOI] [Google Scholar]
- Porter B, & O'Leary KD (1980). Marital discord and childhood behavior problems. Journal of Abnormal Child Psychology, 8, 287–295. 10.1007/BF00916376 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, & Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology, 28, 916–931. doi: 10.1016/S0306-4530(02)00108-7 [DOI] [PubMed] [Google Scholar]
- Raeff C (2011). Distinguishing between development and change: Reviving organismic-developmental theory. Human Development, 54, 4–33. 10.1159/000324334 [DOI] [Google Scholar]
- Repetti RL, & Robles TF (2016). Nontoxic family stress: Potential benefits and underlying biology. Family Relations, 65, 163–175. 10.1111/fare.12180 [DOI] [Google Scholar]
- Repetti RL, Robles TF, & Reynolds B (2011). Allostatic processes in the family. Development and Psychopathology, 23, 921–938. 10.1017/S095457941100040X [DOI] [PubMed] [Google Scholar]
- Roberts AG, & Lopez-Duran NL (2019). Developmental influences on stress response systems: Implications for psychopathology vulnerability in adolescence. Comprehensive psychiatry, 88, 9–21. [DOI] [PubMed] [Google Scholar]
- Rutter M (1987). Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry, 57, 316–331. 10.1111/j.1939-0025.1987.tb03541.x [DOI] [PubMed] [Google Scholar]
- Saltzman KM, Holden GW, & Holahan CJ (2005). The psychobiology of children exposed to marital violence. Journal of Clinical Child and Adolescent Psychology, 34, 129–139. 10.1207/s15374424jccp3401_12 [DOI] [PubMed] [Google Scholar]
- Saxbe DE, Margolin G, Shapiro LA, & Baucom BR (2012). Does dampened physiological reactivity protect youth in aggressive family environments. Child Development, 83, 831–830. DOI: 10.1111/j.1467-8624.2012.01752.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, & Card NA (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57, 1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Schriber RA, & Guyer AE (2016). Adolescent neurobiological susceptibility to social context. Developmental Cognitive Neuroscience, 19, 1–18. doi: 10.1016/j.dcn.2015.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, Rosiers SD, Huang S, Zamboanga BL, Unger JB, Knight, …, & Szapocznik J (2013). Developmental trajectories of acculturation in Hispanic adolescents: Associations with family functioning and adolescent risk behavior. Child Development, 84, 1355–1372. doi: 10.1111/cdev.12047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, Allison AL, Armstrong JM, Slattery MJ, Kalin NH, & Essex MJ (2012). Longitudinal stability and developmental properties of salivary cortisol levels and circadian rhythms from childhood to adolescence. Developmental Psychobiology, 54, 493–502. DOI 10.1002/dev.20607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, & Essex MJ (2008). Concurrent and longitudinal associations of basal and diurnal cortisol with mental health symptoms in early adolescence. Developmental Psychobiology, 50, 690–703. DOI 10.1002/dev.20336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, Granger DA, Booth A, & Johnson D (2005). Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology, 17, 167–184. 10.1017/S0954579405050091 [DOI] [PubMed] [Google Scholar]
- Simmons RK, Howard JL, Simpson DN, Akil H, & Clinton SM (2012). DNA methylation in the developing hippocampus and amygdala of anxiety-prone versus risk-taking rats. Developmental neuroscience, 34, 58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smider NA, Essex MJ, Kalin NH, Buss KA, Klein MH, Davidson RJ, & Goldsmith HH (2002). Salivary cortisol as a predictor of socioemotional adjustment during kindergarten: A prospective study. Child Development, 73, 75–92. 10.1111/1467-8624.00393 [DOI] [PubMed] [Google Scholar]
- Sturge-Apple ML, Davies PT, Cicchetti D, & Manning LG (2012). Interparental violence, maternal emotional unavailability and children's cortisol functioning in family contexts. Developmental psychology, 48, 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud CB, Chen FR, Doane LD, & Granger DA (2019). Early adversity and internalizing symptoms in adolescence: Mediation by individual differences in latent trait cortisol. Development and Psychopathology, 31, 509–524. doi: 10.1017/S0954579418000044. [DOI] [PubMed] [Google Scholar]
- Susman EJ (2006). Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities and the attenuation hypothesis. Neuroscience & Biobehavioral Reviews, 30, 376–389. DOI: 10.1016/j.neubiorev.2005.08.002 [DOI] [PubMed] [Google Scholar]