ABSTRACT
Background: Many people with refugee backgrounds suffer from trauma-related complex social and psychological problems, and compliance with standard psychological treatment tends to be low. More culturally adaptable treatment options seem to be needed.
Objective: We aimed to investigate whether the music therapy method: ‘trauma-focused music and imagery’ (tr-MI), characterized by a particular focus on arousal and affect regulation, would be equally effective as the standard psychological talk therapies for ameliorating trauma symptoms in Danish refugees.
Methods: A pragmatic, noninferiority, parallel, randomized controlled trial with six-month follow-up was carried out at three clinics for refugees in the public mental health services of the Psychiatry (DK). Seventy-four adults diagnosed with posttraumatic stress disorder (PTSD) were allocated to either music therapy sessions (tr-MI, N = 39) or psychological treatment as usual (TAU, N = 35). Western classical music, new age music, and music from the participants’ own national culture were used to generate inner imagery, following a phased treatment protocol. Homework entailed listening to music. The primary outcome was the measurement of trauma symptoms by the Harvard Trauma Questionnaire, section IV (HTQ-IV); secondary measures were somatoform and psychoform dissociation (DSS-20), SDQ-20), attachment (RAAS), and well-being (WHO-5). Treatment effects reflected by primary and secondary measures were estimated using linear mixed models.
Results: Tr-MI was noninferior to TAU (mean difference at follow-up HTQ-IV: 0.14, CI (−0.10; 0.38), with a − 0.3 noninferiority margin). A high dropout rate of 40% occurred in the TAU group, compared to 5% in the music therapy group. Secondary measures generated small to medium effect sizes in both groups, with significant medium effect sizes for well-being and psychoform dissociation at follow-up in tr-MI.
Conclusions: Tr-MI is an innovative form of psychological treatment in refugee mental health services. Trials comparing music therapy to standardized therapy are needed to substantiate the evidence base for tr-MI therapy.
KEYWORDS: Refugees, trauma, dissociation, attachment, non-inferiority, music therapy, Guided Imagery and Music
HIGHLIGHTS
Music therapy was shown to be no less effective than standard psychological treatment regarding the decrease of posttraumatic stress disorder symptoms in a randomized clinical trial with 74 adult traumatized refugees.
Good retainment and significant changes in well-being and dissociation during six-month follow-up were found in music therapy.
Short abstract
Antecedentes: Muchas personas con antecedente de condición de refugiadas sufren complejos problemas psicológicos y sociales relacionados con el trauma, y el cumplimiento con el tratamiento psicológico estándar tiende a ser bajo. Parecen ser necesarias opciones de tratamiento más culturalmente adaptadas.
Objetivo: Apuntamos a investigar si el método de músico-terapia: ‘música e imaginería focalizada en el trauma’ (tr-MI), caracterizado por un enfoque particular en el nivel de alerta y regulación emocional, podría ser igualmente efectivo como las terapias psicológicas de conversación para aliviar síntomas de trauma en refugiados daneses.
Métodos: Se llevó a cabo un ensayo clínico aleatorizado controlado, pragmático, de no inferioridad, paralelo, con seis meses de seguimiento en tres clínicas para refugiados en servicios públicos de salud mental de Psiquiatría en Dinamarca. Setenta y cuatro adultos diagnosticados con Trastorno de estrés postraumático (TEPT) fueron asignados a sesiones de músico-terapia (tr-MI, N = 39) o al tratamiento psicológico de costumbre (TAU, N = 35). Se utilizó música clásica occidental, música new age, y música de la propia cultura nacional de los participantes, para generar imaginería interior, siguiendo un protocolo de tratamiento por fases. La tarea implicaba escuchar música. El resultado principal fue la medición de síntomas de trauma a través del Cuestionario de Trauma de Harvard, sección IV (HTQ-IV); las mediciones secundarias fueron disociación somatomorfa y psicomorfa (DSS-20, SDQ-20), apego (RAAS), y bienestar (WHO-5). Los efectos del tratamiento reflejados por mediciones primarias y secundarias fueron estimados usando modelos lineales mixtos.
Resultados: Tr-MI no fue inferior a TAU (diferencia promedio al seguimiento HTQ-IV: 0.14, IC −0.10; 0.38), con un margen de no-inferioridad de −0.3). Una alta tasa de deserción de un 40% ocurrió en el grupo TAU, comparado con un 5% en el grupo de músico-terapia. Las mediciones secundarias generaron tamaños de efecto pequeños a medianos en ambos grupos, con un tamaño del efecto mediano significativo para bienestar y disociación psicomorfa al seguimiento en tr-MI.
Conclusiones: Tr-MI es una forma innovadora de tratamiento psicológico en servicios de salud mental para refugiados. Se necesitan ensayos comparando músico-terapia con terapia estandarizada para probar la base de evidencia para la terapia tr-MI.
PALABRAS CLAVES: Refugiados, trauma, disociación, apego, no-inferioridad, músicoterapia, Imaginería Guiada y Música, Ensayo controlado aleatorizado, Salud Mental
Short abstract
背景:许多具有难民背景的人遭受创伤相关的复杂社会和心理问题, 对标准心理治疗的依从性较低。似乎需要更具文化适应性的治疗选择。
目的:我们旨在丹麦样本中考查音乐治疗方法:以格外注重唤起和情感调节为特点的‘聚焦创伤的音乐和影像’ (tr-MI) 是否与缓解创伤症状的标准心理谈话疗法同样有效。
方法:在精神病公共心理健康服务部门 (DK) 的三家难民诊所进行了一项为期六个月的实用, 非劣效, 平行, 随机对照试验。 74名被诊断为创伤后应激障碍 (PTSD) 的成年患者被分配到音乐治疗疗程 (tr-MI, N= 39) 或常规心理治疗 (TAU, N= 35) 。遵循阶段性的治疗方案, 西方古典音乐, 新时代音乐和参与者自身民族文化的音乐被用于生成内在图像。作业是听音乐。主要结果是通过哈佛创伤量表第四节 (HTQ-IV) 测量的创伤症状。次要测量是躯体形式和心理形式解离 (DSS-20, SDQ-20), 依恋 (RAAS) 和幸福感 (WHO-5) 。主要和次要措施所反映的治疗效果使用线性混合模型评估。
结果:Tr-MI不逊色于TAU (随访HTQ-IV的均值差:0.14, CI (−0.10; 0.38), 非劣效边际为-0.3。TAU组的退出率高达40%, 音乐治疗组为5%, 而次要测量在两组中均产生了小到中的效应量, 幸福感和心理形态的解离在tr-MI随访中具有显著的中等效应量。
结论:Tr-MI是难民心理健康服务中一种创新的心理治疗形式。需要比较音乐疗法与标准疗法的试验以证实tr-MI疗法的证据基础。
关键词: 难民, 创伤, 解离, 依恋, 非劣效, 音乐疗法, 图像和音乐指导, 随机对照试验, 心理健康
1. Introduction
Refugees have survived extreme traumatic experiences in war zones and during dangerous escapes from their home countries. Many have suffered multiple losses of identity, culture, family, and network. In a refugee population gaining asylum in Germany, as much as 50% were found to suffer from severe psychological after effects, such as posttraumatic stress disorder (PTSD, 34.9%; Nesterko, Jäckle, Friedrich, Holzapfel, & Glaesmer, 2019). A systematic review of general mental health in refugees has shown that torture severity, post-migration hardship, and waiting times for clinical services are all significantly associated with higher rates of mental health symptoms (Suhaiban, Grasser, & Javanbakht, 2019). Refugees and asylum seekers are known to have unmet mental health needs and to underutilize services in European host countries because of language problems, fear of stigma, low awareness, and differences in health-seeking behaviour (Satinsky, Fuhr, Woodward, Sondorp, & Roberts, 2019). A Swiss study of Syrian refugees and asylum seekers and their healthcare providers recommended a greater willingness to embrace innovative paths in treatment (Kiselev et al., 2020). Offering different treatments to accommodate patient preferences in this vulnerable group is essential to reaching out to and retaining refugees in treatment.
1.1. Treatment of traumatized refugees
A longitudinal study of clinical and functional improvement in the health of torture survivors demonstrated that medical, psychological, and social indicators all correlated with, or predicted, clinical outcomes such as trauma symptoms, depression, and anxiety (Hill & Everson, 2020). Evaluating nine studies of cognitive behavioural therapy (CBT) and narrative exposure therapy (NET) with torture survivors, a Cochrane review found no immediate posttreatment effect. In contrast, three NET studies, and a CBT study elicited medium effect sizes on trauma symptoms at six-month follow-up (Patel, Kellezi, & Williams, 2014), while a meta-analysis of torture survivors found that psychological interventions significantly reduced PTSD symptoms by the end of treatment, with a small SMD that remained at follow-up (Hamid, Patel, & Williams, 2019).
Recently, three recent systematic reviews of the treatment of refugees and asylum seekers resettled in high-income countries have demonstrated the efficacy of psychosocial interventions on PTSD symptoms (Nosè et al., 2017; Thompson, Vidgen, & Roberts, 2018; Turrini, Purgato, Acarturk, & Anttila, 2019). Nosè et al. (2017) in 12 studies found large effect sizes on PTSD symptoms when comparing treatment to controls (SMD −1.03, 95% CI −1.55 to −0.51) in no less than 12 studies with NET as the most effective treatment (SMD −0.78, 95% CI −1.18 to −0.38). Accordingly, Thompson et al. (2018) identified large effect sizes when comparing trauma-focused psychotherapies with no treatment at all (SMD −1.14, 95% CI −1.80 to 1.47) and no differences in treatment effects when comparing treatment with active controls (SMD −0.03, 95% CI −0.21 to 0.14) in 15 RCTs. Evidence was found for EMDR and NET to alleviate PTSD symptoms. Based on 26 RCT studies Turrini et al. (2019) found a medium SMD (−0.71; 95% CI −1.01 to −0.41) and stated that only interventions based on cognitive-behavioural therapies with a trauma-focused component generated significant changes, compared to controls. After adjusting for investigator bias (leading to the exclusion of five outlier studies with very large effect sizes after treatment with culturally adapted CBT), the authors identified only a small effect size. Depression and anxiety symptom severity was shown to improve in several studies, while entities such as daily functioning and quality of life were measured only in five studies and did not differ significantly between intervention and control groups (Turrini et al., 2019). A number of studies have shown low scores on subjective wellbeing in refugees, as measured with WHO-Wellbeing-5. Out of 1215 Syrians 38% scored under 50, which indicates poor emotional well-being (Tinghög et al., 2017) and the average wellbeing scores in two other studies were found to be only 14 and 12.5, respectively (Sonne, Lohmann, Bech, Elklit, & Mortensen, 2016; Uygun, 2020).
Italian psychiatrist Liotti (2004) realized that complex trauma frequently is accompanied by symptoms of dissociation and insecure attachment, leading to the description of the term ‘the trauma triad’. An investigation of psychiatric symptoms in 85 refugees in a German reception centre accordingly showed that a majority suffered from posttraumatic stress disorder, typically combined with symptoms of dissociation (Belz, Belz, Ozkan, & Graef-Calliess, 2017). In a sample of 116 refugees seeking treatment, Palic (2013) found that 30% suffered from pathological dissociation, and this was even 16 years after their exposure to war trauma. With regard to attachment patterns, several recent studies have identified high levels of insecure attachment in refugees (Dalgaard, Todd, Daniel, & Montgomery, 2016; Riber, 2016; Van Ee, Kleber, & Jongmans, 2016), the most prevalent attachment patterns being disorganized (Riber, 2016) or avoidant (Morina, Schnyder, Schick, Nickerson, & Bryant, 2016).
1.2. Music therapy with refugees
Alternatives to talk therapies are called for in the protocol for an upcoming Cochrane overview of systematic reviews of prevention and treatment for refugees, asylum seekers, and internationally displaced persons. The authors state that, ‘[c]ompared to the general population, migrants who were forced to leave their home are more likely to experience common mental disorders, and the efficacy of psychological therapies (talk therapies) may be different in this population’ (Uphoff, Purgato, Churchill, & Barbui, 2019, p. 1).
Music therapy is defined as ‘the professional use of music and its elements as an intervention in medical, educational, and everyday environments with individuals, groups, families, or communities who seek to optimize their quality of life and improve their physical, social, communicative, emotional, intellectual, and spiritual health and wellbeing … ’ (World Federation of Music Therapy, 2011). Some evidence for the efficacy of music therapy has been demonstrated in Cochrane reviews where, for instance, RCT studies on adults with depression showed large effect sizes favouring music therapy and TAU over TAU alone (Aalbers et al., 2017), and RCT studies on music listening interventions for sleep insomnia demonstrated a very large effect size compared to controls (−2.80; 95% CI −3.42 to −2.17; p < .00001) (Jespersen, Koenig, Jennum, & Vuust, 2015).
A review of music therapy for refugees and asylum seekers suffering from PTSD demonstrated effects on all three symptom clusters: avoidance, hypervigilance, and intrusion (Beck & Mumm, 2015). In a theoretical review several mechanisms of music therapy related to PTSD treatment were identified, such as improved arousal regulation, grounding, mood alteration, and new positive social experiences (Landis-Schack et al., 2017). Jespersen and Vuust (2012) found significant changes in sleep quality in adult refugees after three weeks of music listening at bedtime. In a group of 17 patients, who had not improved after CBT, patients were randomized to either group music therapy or a waitlist control, and a significant decrease in symptoms was detected in the music therapy group (−20.18, 95% CI −31.23, −9.12) (Carr et al., 2012). In a study of abused women seeking help in domestic violence shelters, music therapy was shown to significantly improve sleep quality and reduce anxiety symptoms (Hernandez-Ruiz, 2005).
For the present study, we applied a trauma-focused adaptation of the Bonny Method of Guided Imagery and Music (GIM), a receptive music therapy method that focuses on spontaneous inner imagery stimulated by listening to music in an altered state of consciousness (Beck, 2018; Grocke, 2019). In a systematic review of 9 GIM studies with clinical and nonclinical populations, measures of anxiety, depression, mood disturbance, interpersonal problems, quality of life, sense of coherence, and/or psychiatric symptoms revealed medium to large effect sizes (McKinney & Honig, 2017). In another systematic review of the relationship between GIM and positive psychology, well-being, quality of life, mood states or sense of coherence were documented to improve in all of the 14 studies included in the review (Jerling & Heyns, 2020). Implemented across diverse populations (Grocke & Moe, 2015), GIM has been adapted to a variety of trauma treatments (Ahonen, 2019). A GIM outcome study showed very large effects on trauma and dissociation symptoms in women with complex PTSD caused by violence or sexual abuse (Maack, 2012). In two pilot studies, a medium effect size on trauma symptoms was found after 12 sessions of group GIM therapy with victims of violence (Rudstam, Elofsson, Søndergaard, Bonde, & Beck, 2017) and clinically significant reductions of trauma symptoms were identified in sexually abused female veterans after ten sessions of GIM (Story & Beck, 2017).
In a feasibility study, 16 weekly sessions of the GIM adaptation trauma-focused music and imagery (tr-MI) were offered to 16 traumatized refugees in a trauma clinic (Beck et al., 2017). With no dropouts, the participants accepted the intervention well, and all showed significant changes in trauma symptoms, well-being, sleep quality, and social function with medium to large effect sizes.
Following up on these results, we set out to perform a randomized controlled trial to investigate whether tr-MI could prove to be no less effective than standard clinical psychological treatment in relieving trauma symptoms. Noninferiority designs are often used to test the viability of new treatment options, which are more tolerable or have fewer side effects than the reference treatment (active control; Piaggio, Elbourne, Pocock, Evans, & Altman, 2012). As mentioned earlier, engaging and retaining help-seeking refugees in trauma treatment can be difficult for many reasons. These presumably include challenges related to cultural differences and language barriers. In the pilot study tr-MI offered a gentle approach to imaginal trauma exposure, and the use of music served as an intercultural and nonverbal therapy element mitigating language and cultural barriers.
2. Methods
The study was a pragmatic, noninferiority, parallel, randomized controlled trial comparing music therapy to standard psychotherapy (TAU). It was delivered by psychologists and music therapists at all three locations of a Danish trauma clinic for refugees. We hypothesized that music therapy would not be inferior to standard treatment in terms of changes effected in PTSD symptoms at the end of treatment (EOT) and at six-month follow-up (FU). We expected similar improvements in secondary measures of well-being, dissociation, and attachment at EOT and FU, as seen by a comparison of effect sizes. In an exploratory study, we hypothesized that at EOT and FU, the levels of salivary oxytocin, beta-endorphin, and substance p would be higher than at baseline. The published study protocol described the interventions and procedures in detail (Beck et al., 2018).
2.1. Procedures
Data were collected from May 2015 to November 2019 at the outpatient Clinic of Traumatized Refugees of the Department of Specialized Treatment, at the Psychiatry of Region Zealand, Denmark (from 1 October 2019, Psychiatry West, Region Zealand). The clinic receives 150–200 patients per year, most commonly referred by general practitioners for assessment and treatment of PTSD symptoms.
Both interventions in the study followed the official clinical guidelines for the regional psychiatry treatment packages for traumatized refugees, including three hours of assessment, 16 one-hour trauma psychotherapy sessions and, if relevant, pharmacological treatments such as SSRIs, anxiolytics and antipsychotic medications for complex and/or comorbid psychiatric conditions, such as clinical depression, anxiety- and sleeping disorders and intermittent psychotic symptoms common in severe cases of PTSD and complex PTSD in refugees referred to the psychiatric outpatient clinic. Additional physiotherapy or psychomotor therapy, social counseling, and network meetings with social authorities at the end of treatment were commonly offered within the standard treatment package (National clinical recommendations, 2017). Eligible participants were Arabic-, English- or Danish-speaking adults (18–68 years) with temporary or permanent residence permit and a diagnosis of either PTSD (ICD-10 F43.1) or enduring personality change after catastrophic experiences (F62.0). The exclusion criteria included ongoing substance abuse, impaired hearing, suicidal risk, as well as severe dissociative and/or psychotic symptoms.
The assessment of PTSD symptoms included a semi-structured interview administered by a licenced psychologist, psychiatrist or leading physicist according to the ICD-10 and DSM-IV criteria for PTSD (APA; 2000; WHO, 1993). Trauma history, physical health and physical effects of torture, including persistent pain, current socioeconomic situation and social network were assessed as part of the intake procedure.
The diagnostic assessor was not excluded from serving as the patients’ therapist in the subsequent treatment programme, nor were they blinded to diagnoses and comorbidity. The patients were given oral and written information about the study and had one week to agree to participation by completing a written consent form. All data collection was carried out using the XPsy quality and research software, in which each question is presented on-screen in either Danish, English, or Arabic. If needed, translators were available to translate the questions and assist in entering data. The HTQ questions were administered by a licenced psychologist or a music therapist. In both cases, the rater could serve as the patient’s therapist. Following baseline testing, randomization to tr-MI or TAU took place by entering the participants’ location, sex (male/female), and ID numbers into the Sealed Envelope website. Sealed Envelope generated and kept a random sequence with stratification regarding location, sex, and random permuted blocks of four or six participants.
The primary outcome (HTQ) was rated at EOT and FU by external psychologists, who were blinded to the treatment group. The questionnaire data were blinded to the researchers and therapists until all data had been collected. The trial was monitored by a steering group that included the senior physicist, chief medical officer, and management representatives of the psychiatric department of the involved hospital and research departments. The study was approved by the Region Zealand Ethical Scientific Committee (SJ-529).
2.2. Interventions
Both treatment arms included a phase-oriented trauma therapy course of 16 weekly one-hour sessions in accordance with guidelines for trauma treatment (Nice, 2005, 2018). Treatment phases were not followed in a linear manner but progressed according to the patient’s condition. If severe destabilizing outer life events occurred late in the treatment course (a common stress factor in refugees, such as the loss of a family member due to the ensuing conflicts in their country of origin), up to 20 sessions were accepted to allow for sufficient time to conclude the therapy. A participant was considered to have dropped out if less than 12 sessions were completed.
TAU was carried out by three experienced government-authorized clinical psychologists and one newly trained psychologist, all with university training. Tr-MI was carried out by four music therapists holding master’s degrees and a GIM certification, which requires three years of specialized training. The age range (28–70 years) and clinical experience (1–30 years) of both therapist groups was diverse, and both groups included male and female therapists. Differences in work schedule and assignments meant that the number of therapies was not equally distributed between therapists.
On-site interpreters were used as needed; those working with the music therapy group were given a brief introduction to translation during the music and imagery sessions.
Trauma-focused music and imagery (tr-MI) sessions included verbal communication and, optionally, 5–20 minutes of music and imagery work with the patient in a seated or reclining position. With eyes open or closed, the patient was guided into a slightly altered state of consciousness, achieved by focusing on breathing, relaxation, and an opening image aligned with their current state of mind or situation. During music listening, the participant was encouraged to engage with spontaneous imagery and sensations in dialogue with the therapist. Following each music listening session, the experience was processed verbally with the therapist.
In accordance with the protocol, the stabilization phase introduced predictable slow-tempo music to decrease arousal. The music listening was also used to stimulate images of safe places, positive memories of social situations and to derive a sense of security towards the therapist.
Taking the individual susceptibility to emotional cues and triggers into account, increasingly emotionally evocative music was gradually introduced in order to reflect the patient’s trauma history and to help them contain and regulate complex and contradictory emotions. The exposure to the evoked trauma images was carefully managed, with the therapist giving increasingly direct guidance during music playback. In consultation with the patient, the music pieces were chosen by the therapists from the GIM repertoire of classical music pieces (Grocke, 2019), supplemented by pieces of light classical music, film music, meditative music, and pieces from the participant’s own musical tradition. The participants were instructed to use music and imagery between sessions as an everyday stress regulation tool. During each session, information about this home use was elicited. In the concluding phase of the therapy course, the participants were encouraged to imagine their future life situation and to implement their new coping skills in their everyday life.
Standard treatment (TAU) was delivered by the psychologists according to best-practice guidelines for PTSD treatment, including elements of trauma-focused CBT, psychodynamic, and narrative approaches (Foa, Keane, Friedman, & Cohen, 2009). In the initial phase, stabilization, the main focus was to establish a supportive therapeutic relationship, using psychoeducation to help the patient understand and cope with trauma symptoms, in order to increase their daily level of functioning. Patients were instructed in breathing techniques to regulate affect and increase affect tolerance. Trauma exposure included processing of traumatic memories, enabling the patient to break with avoidant behaviour and to begin integrating their traumatic memories into their current life narrative. In the reorientation phase, the main therapeutic focus was to encourage the patient to retain and develop social connections and set goals for work or education.
Detailed descriptions of the two interventions can be found in the study protocol (Beck et al., 2018).
Issues of treatment fidelity were evaluated at weekly clinical conferences and at monthly group supervision sessions in both therapist teams. No systematic evaluation of treatment fidelity was applied.
2.3. Measures
The primary outcome measures were the first 16 items of part IV of the Harvard Trauma Questionnaire (HTQ), assessing PTSD symptoms in accordance with the DSM-IV diagnostic criteria (Mollica et al., 1992). The items’ description of symptoms related to each item was read aloud by the rater, and the patient was asked to estimate the degree to which he or she had been affected by them in the past week, on a 4-point Likert scale ranging from not at all to most of the time. A cut-off value of 2.5 for the PTSD diagnosis indicated clinical change and was used to indicate remission (Mollica et al., 1992). The HTQ, with its three subscales of Intrusion, Avoidance, and Hypervigilance, has demonstrated acceptable reliability in several languages, including Arabic (Kleijn, Hovens, & Rodenburg, 2001).
The secondary outcome measures were Well-being, Somatoform dissociation, Psychoform dissociation, and Attachment.
The WHO Well-being Index (WHO-5) is scored on a 6-point Likert scale for five non-invasive questions measuring positive dimensions of subjective well-being, with a cut-off for poor emotional well-being (< 50). It has demonstrated high reliability, validity, and sensitivity to treatment response in psychiatric care (Bech, Olsen, Kjøller, & Rasmussen, 2003; Newnham, Hooke, & Page, 2010) and in clinical trials (Topp, Østergaard, Søndergaard, & Bech, 2015).
The Dissociative Symptoms Scale (DSS-20) is a 5-point Likert scale assessing levels of depersonalization, derealization, gaps in awareness or memory, and dissociative re-experiencing (Carlson & Waelde, 1999). The scale has demonstrated satisfactory psychometric properties in PTSD populations (Carlson et al., 2018).
The Somatoform Dissociation Questionnaire (SDQ-20) is also a 5-point Likert scale for evaluating somatic dissociation (Nijenhuis et al., 1996). Each positive answer corresponding to a possible symptom is followed by an additional question to assess whether a physical diagnosis (provided by a medical doctor) could explain the symptom in question. The scale has adequate psychometric properties and correlates with self-reported traumatization (Nijenhuis, 2010; Nijenhuis, Spinhoven, Van Dyck, Van Der Hart, & Vanderlinden, 1998).
The Revised Adult Attachment Scale (RAAS, Close Relationship version; Collins, 1996) measures the experience of emotional closeness or distance in close relationships by way of 18 items scored on a 5-point Likert scale, from not at all characteristic of me to very characteristic of me. Continuous variables indicate changes in the dimensions ‘Close’ (closeness with others), ‘Depend’ (trusting other people’s helpfulness), and attachment-related ‘Anxiety’ and ‘Avoidance’. Adequate psychometric properties have been documented in a variety of cultural settings (Fernández & Dufey, 2015; Ripardo, Ferreira, & Howat-Rodrigues, 2019) including a Danish study of 3,352 respondents (Pedersen, 2006).
All scales were available in Danish, English, and Arabic. The DSS-20 and the RAAS were translated into Arabic by SL together with an expert group of Arabic–Danish translators. A Swedish version of the SDQ-20 was translated into Danish by BB, assisted by a (Danish based) Swedish translator with special knowledge of health issues. Translation of research questionnaires followed the WHO guidelines for the (‘Process of translation and adaptation of instruments’ (WHO, n.d.). Saliva samples were collected for the analysis of oxytocin, beta-endorphin, and substance p; analyses of which have yet to be performed and are expected to be published in a later study.
2.4. Statistics
Based on previous RCT intervention studies using the Harvard Trauma Questionnaire with refugees (see protocol by Beck et al., 2018), we estimated a noninferiority margin of −0.3, corresponding to 10% on the HTQ scale, the least clinically significant difference. Based on the selected studies, we calculated a standard deviation of 0.48 and chose a power of 0.8. Applying a two-tailed significance level of 0.05, we carried out the power calculation using Epi-info 7 software (Epiinfo, n.d.) in cooperation with statisticians from Region Zealand’s Production, Research, and Innovation (PFI) Centre. A total of 64 participants was needed, which was increased to 74 to account for potential dropouts.
The baseline demographics and psychosocial characteristics of the groups were compared with parametric and nonparametric tests. One of the present authors (IP), a statistician at the Biostatistics Department, Odense University Hospital, carried out primary outcome noninferiority analysis and constructed a constrained linear mixed effects model to compare differences in treatment effect (TAU versus tr-MI) on HTQ data, to ensure that missing values were missing at random (MAR). Unbiased results were thus generated by estimating the parameters using maximum-likelihood procedures. The analysis was adjusted for baseline HTQ, as proposed by Twisk et al. (2018), by fitting a repeated measurement model, leaving out an isolated treatment effect as a fixed effect, i.e.:
We followed the procedures suggested by Acierno et al. (2017) to assess noninferiority. Hence, one-sided 90% confidence intervals of the parameters (difference of treatment effect at EOT) and (difference of treatment effect at the six-month follow-up session) were estimated and compared to the noninferiority margin (Δ = −0.3 for HTQ). A noninferior treatment effect at follow-up sessions was established for HTQ when the lower limit of the 90% confidence intervals was higher than the noninferiority margin.
The noninferiority test was carried out using both per-protocol (PP) and intention-to-treat (ITT) approaches, as recommended by Acierno et al. (2017). The primary outcome results were drawn from the PP analyses in consistency with the guidelines of Schumi and Wittes (2011).
Secondary outcomes (ITT) were analysed using a constrained linear mixed model, with an assumption of an equal baseline, as suggested by Liu, Lu, Mogg, Mallick, and Mehrotra (2009). Effect sizes were calculated from the model, as indicated by the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1, chapter 7 (Higgins & Green, 2011). The PP mean and standard deviations for secondary measures are reported in Table 2. PP effect sizes, based on Cohen’s d- and p-values using t-tests, are given in Table 4. Although we found deviations from normality, except in the case of the results of the DSS, t-testing has been shown to be robust (Fagerland, Sandvik, & Mowinckel, 2011).
Table 2.
Within-group changes in trauma, well-being, dissociation, and attachment (PP)
| |
Means (Standard deviation) |
|||||
|---|---|---|---|---|---|---|
| tr-MI Baseline |
tr-MI EOT |
tr-MI FU |
TAU Baseline |
TAU EOT |
TAU FU |
|
| HTQ Intrusion | 3.44 (0.52) | 3.42 (0.59) | 3.03 (0.80) | 3.30 (0.52) | 3.17 (0.36) | 3.24 (0.57) |
| HTQ Avoidance | 2.95 (0.60) | 2.92 (0.53) | 2.79 (0.76) | 2.80 (0.51) | 2.73 (0.60) | 2.84 (0.56) |
| HTQ Hypervigilance | 3.49 (0.50) | 3.26 (0.67) | 3.09 (0.81) | 3.30 (0.68) | 3.24 (0.55) | 3.20 (0.65) |
| HTQ Total | 3.24 (0.47) | 3.15 (0.4) | 2.94 (0.72) | 3.08 (0.47) | 3.00 (0.42) | 3.05 (0.45) |
| WHO-5 | 18.4 (16.9) | 29.2 (24.8) | 31.7 (27.1) | 17.1 (18.3) | 19.2 (12.5) | 21.6 (19.7) |
| DSS-20 | 35.5 (17.1) | 29.4 (18.3) | 23.3 (16.6) | 29.0 (14.9) | 24.0 (14.4) | 22.9 (17.3) |
| SDQ-20 | 39.1 (11.6) | 38.8 (11.3) | 37.1 (12.7) | 35.7 (10.7) | 38.2 (12.4) | 32.6 (9.5) |
| RAAS Close | 16.8 (5.0) | 17.6 (6.2) | 18.4 (6.3) | 18.7 (4.3) | 16.8 (4.9) | 19.2 (6.5) |
| RAAS Depend | 15.3 (4.4) | 16.4 (3.8) | 16.0 (5.5) | 14.6 (4.3) | 14.7 (4.9) | 15.2 (6.5) |
| RAAS Anxiety | 18.6 (6.7) | 17.7 (5.1) | 16.2 (6.7) | 15.1 (4.8) | 15.1 (4.6) | 17.0 (6.4) |
| RAAS Avoidant | 39.9 (7.9) | 37.9 (8.8) | 37.6 (10.7) | 38.7 (6.9) | 40.5 (10.4) | 37.6 (11.1) |
PP: Per Protocol (N = 35/18), HTQ: Harvard Trauma Questionnaire; WHO-5: Well-being scale; DSS-20: Dissociative Symptoms Scale; SDQ-20: Somatic Dissociation Questionnaire; RAAS: Revised Adult Attachment Scale.
Table 4.
Within-group effect sizes (Cohen’s d) for secondary outcomes (PP)
| |
Effect size (Cohen’s d) |
|||
|---|---|---|---|---|
| Baseline to EOT tr-MI |
Baseline to FU tr-MI |
Baseline to EOT TAU |
Baseline to FU TAU |
|
| WHO-5 | 0.52* | 0.55* | 0.05 | 0.13 |
| DSS-20 | 0.35* | 0.71*** | 0.30 | 0.38 |
| SDQ-20 | 0.03 | 0.10 | −0.21 | 0.26 |
| RAAS Close | 0.15 | 0.25 | 0.33 | 0.01 |
| RAAS Depend | 0.28 | 0.15 | 0.00 | 0.05 |
| RAAS Anxiety | 0.15 | 0.35 | −0.07 | −0.40 |
| RAAS Avoidant | 0.24 | 0.23 | 0.23 | 0.26 |
PP: Per Protocol (n = 35/18), WHO-5: Well-being scale; DSS-20: Dissociative Symptoms Scale; SDQ-20: Somatic Dissociation Questionnaire; RAAS: Revised Adult Attachment Scale. Significance levels * p < .05, ** p < .01, *** p < .001 (t-tests).
The significant variables for the dropouts were included in the mixed models as an alternative to imputation for missing data.
3. Results
3.1. Sample characteristics
The sample consisted of 74 participants with a PTSD diagnosis. The average age was 42 years, with a slight excess of males (58%). As seen in Tables 1, 57% of the participants had arrived from Syria (including Palestinians and Kurds) after 2000. Fifteen per cent came from Iraq, and 11% from Bosnia or Kosovo. The remaining participants had arrived from Lebanon, Iran, Afghanistan, Somalia, Sri Lanka, or Chechnya. Of the sample, 65% had experienced imprisonment for 0–3 years and 50% (all of whom were males) had been exposed to torture. Violence or sexual abuse in childhood was reported by 35%. Baseline levels of medication showed that 38% had prescriptions for antidepressants, antipsychotics, or a combination of both. Demographic and psychosocial characteristics did not differ between the two treatment groups. Supplementary treatment sessions were given equally to the two groups (tr-MI or TAU): 15/12 participants received on average 5.2/5.8 psychomotor/physiotherapy sessions, and 9/10 participants received on average 3.0/2.2 sessions with a social worker.
Table 1.
Demographic and psychosocial characteristics of the participants
| tr-MI (n = 39) ITT | TAU (n = 35) ITT | tr-MI (n = 37) PP | TAU (n = 21) PP | |
|---|---|---|---|---|
| Sex | ||||
| Males | 22 (56.4%) | 21 (60.0%) | 20 (54.1%) | 14 (66.7%) |
| Females | 17 (43.6%) | 14 (40.0%) | 17 (45.9%) | 7 (33.3%) |
| Age | ||||
| 18–29 y | 5 (12.8%) | 4 (11.4%) | 3 (8.1%) | 3 (14.3%) |
| 30–39 y | 9 (23.1%) | 10 (28.6%) | 9 (24.3%) | 4 (19.0%) |
| 40–49 y | 12 (30.8%) | 13 (37.1%) | 12 (32.4%) | 9 (42.9%) |
| 50–59 y | 11 (28.2%) | 8 (22.9%) | 11 (29.7%) | 5 (23.8%) |
| Over 60 y | 2 (5.1%) | 0 (0.0%) | 2 (5.4%) | 0 (0.0%) |
| Married | ||||
| No | 11 (28.2%) | 9 (25.7%) | 10 (27.0%) | 5 (23.8%) |
| Yes | 28 (71.8%) | 26 (74.3%) | 27 (73%) | 16 (76.2%) |
| Social contact | ||||
| None | 1 (2.6%) | 2 (5.7%) | 1 (2.7%) | 1 (4.8%) |
| Occasionally | 5 (12.8%) | 6 (17.1%) | 5 (13.5%) | 2 (9.5%) |
| Regularly | 12 (30.8%) | 13 (37.1%) | 11 (29.7%) | 8 (38.1%) |
| Daily | 21 (53.9%) | 13 (37.1%) | 20 (54.1%) | 10 (47.6%) |
| Unknown | 0 (0.0%) | 1 (2.9%) | 0 (0.0%) | 0 (0.0%) |
| Education length | ||||
|
11 (28.2%) | 11 (31.4%) | 9 (24.3%) | 8 (38.1%) |
| 6–10 years | 16 (41.0%) | 9 (25.7%) | 16 (43.2%) | 7 (33.3%) |
| >10 years | 12 (30.8%) | 13 (37.1%) | 12 (32.4%) | 5 (23.8%) |
| Unknown | 0 (0.0%) | 2 (5.7%) | 0 (0.0%) | 1 (4.8%) |
| Arrival in DK | ||||
| Before 1990 | 2 (5.1%) | 2 (5.7%) | 2 (4.5%) | 2 (9.5%) |
| 1990–2000 | 6 (15.4%) | 10 (28.6%) | 6 (16.2%) | 6 (28.6%) |
| After 2000 | 31 (79.5%) | 23 (65.7%) | 29 (78.4%) | 13 (61.9%) |
| Home country | ||||
| Syria | 17 (43.6%) | 16 (45.7%) | 16 (43.2%) | 10 (47.6%) |
| Iraq | 7 (17.9%) | 5 (14.3%) | 7 (18.9%) | 2 (9.5%) |
| Palestine | 6 (15.4%)) | 3 (8.6%) | 6 (16.2%) | 1 (4.8%) |
| Bosnia/Kosovo | 3 (7.7%) | 5 (14.3%) | 3 (8.1%) | 3 (14.3%) |
| Other | 6 (15.4%) | 6 (17.1%) | 5 (13.5%) | 5 (23.8%) |
| Childhood abuse | ||||
| Yes | 15 (38.5%) | 11 (31.4%) | 14 (37.8%) | 6 (28.6%) |
| No | 24 (61.5%) | 24 (68.6%) | 23 (62.2%) | 15 (71.4%) |
| Adult abuse | ||||
| Yes | 20 (51.3%) | 15 (42.9%) | 19 (51.4%) | 12 (57.1%) |
| No | 19 (48.7%) | 20 (57.1%) | 18 (48.6%) | 12 (57.1%) |
| Torture | ||||
| Yes | 21 (53.8%) | 17 (48.6%) | 19 (51.4%) | 12 (57.1%) |
| No | 18 (46.2%) | 18 (51.4%) | 18 (48.6%) | 9 (42.9%) |
|
Weeks in prison (n = 48) |
||||
| Mean (SD) (weeks) | 11.8 (29.1) | 10.8 (27.3) | 11.36 (30.0) | 16.8 (33.8) |
| Range (weeks) | 0–160 | 0–127 | 0–160 | 0–127 |
| Unknown (N) | 4 | 2 | 4 | 1 |
| Medication | ||||
| Antidepressants | 6 (15.4%) | 7 (20.0%) | 6 (16.2%) | 6 (28.8%) |
| Antipsychotics | 3 (7.7%) | 0 (0.0%) | 3 (8.1%) | 0 (0.0%) |
| Combined | 6 (15.4%) | 6 (17.1%) | 6 (16.2%) | 5 (23.8%) |
| None | 24 (61.5%) | 22 (62.9%) | 22 (59.5%) | 10 (47.6%) |
| Number of sessions | ||||
| Norm (16 sess.) | 26 (68.4%) | 6 (17.1%) | 26 (72.2%) | 6 (28.6%) |
| Higher (17–20 sess.) | 10 (26.3%) | 11 (31.4%) | 10 (27.8%) | 11 (52.4%) |
| Lower (12–15 sess.) | 0 (0.0%) | 5 (14.3%) | 0 (0.0%) | 4 (19.0%) |
| Interpreter | ||||
| Yes | 24 (61.5%) | 16 (45.7%) | 23 (62.2%) | 10 (47.6%) |
| No | 15 (38.5%) | 19 (54.3%) | 14 (37.8%) | 11 (52.4%) |
|
Supplementary treatment sessions |
||||
| Yes | 14 (35.9%) | 13 (37.1%) | 14 (37.8%) | 10 (47.6%) |
| No | 25 (64.1%) | 22 (62.9%) | 23 (62.2%) | 11 (52.4%) |
All chi-square tests (ANOVA for Weeks in prison) were nonsignificant between groups.
3.1.1. Attendance
As shown in the flow chart (Figure 1), 74 participants were randomized to tr-MI (N = 39) or TAU (N = 35). In total, 58 participants completed treatment, 37 in tr-MI, and 21 in TAU, which elicited a significant discharge of 14 patients in the TAU group during treatment (40%) compared to two patients in the tr-MI group (5%) (p < .001). Dropout was caused by ill-health, moving away, economic facts (lack of money for transportation or the need to seek work or study activity) and not meeting for treatment (unknown reason). Five participants did not complete FU measurements, resulting in a total dropout rate of 49% in TAU and 10% in tr-MI. Apart from dropout to EOT and FU measurements, data missingness was 0.12%.
Figure 1.
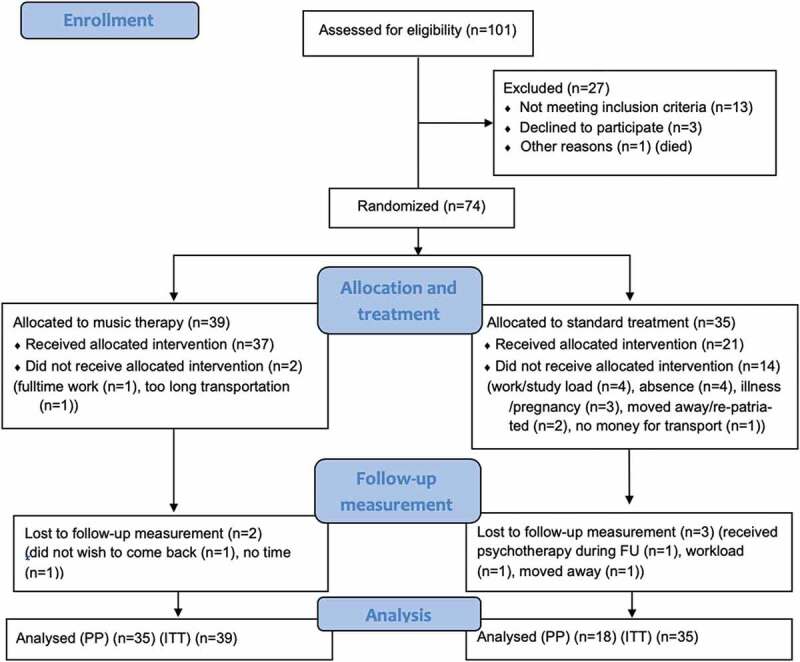
CONSORT flow chart
3.1.2. PP and ITT samples
The per-protocol (PP) sample included participants who received allocated treatment and completed EOT or FU measures. The intention to treat (ITT) sample consisted of all assigned participants; dropouts completed only the baseline measures. Two patients missed EOT but completed FU measurements.
3.2. Efficacy
3.2.1. Primary outcome
Figure 2 shows a difference between treatment effects in the PP analysis of 0.07 (CI −.29; .15) at EOT and 0.16 (−.07; .38) at FU, both higher than the noninferiority margin of −0.3, indicating significant noninferiority of tr-MI. Correspondingly, the lower limit of the 90% confidence intervals in the ITT analysis was exactly at the noninferior limit at EOT 0.07 (−.30; .15) and above the limit at FU 0.14 (−.10; .38).
Figure 2.
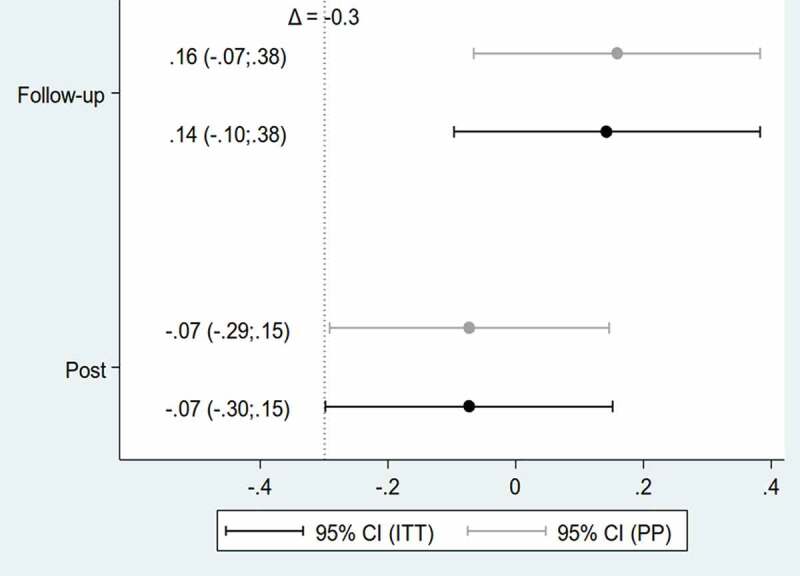
Noninferiority of music therapy compared to standard treatment of trauma symptoms (primary outcome) (PP/ITT)
HTQ: Harvard Trauma Questionnaire, part IV. Intention to treat (ITT), N = 74 (tr-MI 39/TAU 35); Per protocol (PP), N = 58 (tr-MI 35/TAU 18).
We saw remission of 12 participants at FU, 10 in the music group, and two in the TAU group (p = .185, Fisher’s exact test).
3.2.2. Secondary outcomes
Table 2 demonstrates a decrease in mean values in DSS, SDQ, RAAS (anxiety and avoidant), and increasing mean values for well-being and RAAS (depend and close), indicating an improving trend across all measures in tr-MI, except for RAAS avoidant. Tables 3 and 4 report the effect sizes for the ITT and PP samples. In the ITT sample, the Well-being (WHO-5) scores changed significantly within the tr-MI group, with large effect sizes (ES) after EOT and FU (0.58, p = .005 and 0.61, p = .004), whereas the ESs in the TAU comparator were small (0.06 and 0.18). Psychoform dissociation (DSS-20) ES in the tr-MI group was small at EOT (0.35), but large and significant at FU (0.71, p = .0002), whereas in the TAU group, ESs were medium (0.31, 0.41). Somatoform dissociation (SDQ-20) showed a negative tendency in both tr-MI and TAU at EOT (−0.01, −0.04), and small ESs were found at FU (0.10; 0.28).
Table 3.
Within-group effect sizes (Cohen’s d) for secondary outcomes (ITT)
| |
Effect size (Cohen’s d) |
|||
|---|---|---|---|---|
| Baseline to EOT tr-MI |
Baseline to FU tr-MI |
Baseline to EOT TAU |
Baseline to FU TAU |
|
| WHO-5 | 0.58** | 0.61** | 0.06 | 0.18 |
| DSS-20 | 0.35 | 0.70*** | 0.31 | 0.41 |
| SDQ-20 | −0.01 | 0.10 | −0.04 | 0.28 |
| RAAS Close | 0.18 | 0.25 | 0.37* | 0.06 |
| RAAS Depend | 0.37* | 0.20 | 0.02 | 0.04 |
| RAAS Anxiety | 0.02 | 0.18 | 0.21 | −0.11 |
| RAAS Avoidant | 0.26 | 0.25 | −0.17 | 0.05 |
ITT: Intention to treat (N = 39/35), WHO-5: Well-being scale; DSS-20: Dissociative Symptoms Scale; SDQ-20: Somatic Dissociation Questionnaire; RAAS: Revised Adult Attachment Scale. Significance levels * p < .05, ** p < .01, *** p < .001 (constrained linear mixed model).
In the four attachment (RAAS) dimensions, ESs in tr-MI were found to be small to medium (0.20–0.37), while ESs in TAU were negative to small (−0.17 to 0.21). A significant change in the attachment dimension close proved an exception, with a medium effect size (0.37, p = .0496) at EOT. Two small negative ESs were found in TAU for avoidance and anxiety (−0.17 and −0.11). In the tr-MI group, a significant change in the depend dimension (0.37, p = .048) was found at EOT.
4. Discussion
The study results showed noninferiority of tr-MI to TAU for PTSD symptoms in the PP sample at both EOT and FU and at FU in the ITT sample. All confidence intervals except for ITT at EOT were above the noninferiority margin of −0.3, which represents a 10% tolerance of difference on the HTQ scale. We note that the HTQ scores and HTQ effects had large standard deviations, indicating considerable variation in both PTSD symptoms and their improvements in participants. To our knowledge, this is the first music therapy trial for PTSD-patients with an active control; whereas previous studies comparing music therapy to waitlist controls have demonstrated a reduction of trauma symptoms (Carr et al., 2012; Rudstam et al., 2017).
A basic principle of noninferiority trials is that the active control is a validated and evidence-based treatment although Greene, Morland, Durkalski, and Frueh (2008) have shown that this is not always the case. The standard treatment in this study was not tested and validated statistically, and we had to assume that its efficacy was comparable to standard evidence-based treatment regimes in the field, arguing that the treatment was carried out by experienced therapists, according to international guidelines on refugee treatment implemented as local guidelines for treatment packages including CBT elements. The number of comparable manualized refugee studies with CBT elements performed before 2015 was sparse (only one could be found in a review of 25 studies (Palic & Elklit, 2011), a non-randomized study with manualized Cognitive Processing Treatment (ES = 2.6, Schulz, Resick, Huber, & Griffin, 2006). Another non-randomized follow-up study with manualized CBT, Buhmann, Mortensen, Nordentoft, Ryberg, and Ekstrøm (2015) demonstrated a medium effect size (0.68). However, the lack of standardization and manualization of the reference treatment in this study means that the results should be interpreted with caution.
Significant within-group changes concerning well-being, psychoform dissociation and depend attachment were identified in the tr-MI group, and a significant change with a medium effect in close attachment was found in the TAU condition. Psychological dissociation similarly was found to decrease in other trauma studies using music and imagery approaches (Maack, 2012; Rudstam et al., 2017). The change in close and depend attachment dimensions can be interpreted as an indication of improved tolerance of closeness and being positively dependent in social relationships.
Many CBT studies have failed to report on well-being or quality of life, and those that have included these measures have demonstrated only small effect sizes (Turrini et al., 2019). Our study identified a medium effect size on well-being after music therapy, indicating general improvement in the participants’ quality of life.
We unexpectedly found much higher retainment and remission rates in the music therapy group than in the active control. Possible explanations for the low dropout rate and positive outcomes following music therapy include the standardized approach of this intervention and the use of music and imagery for self-care at home. According to the weekly qualitative feedback from participants home music listening and imagery formation helped the participants to downregulate their stress level, access inner resources, process intrusive memories and regulate their mood. A theoretical explanation could also be that the small dropout was due to a strong therapeutic alliance with the music therapists and motivational factors elicited by the enthusiasm of the music therapists who initiated and performed the study.
The TAU group’s high dropout rate (40% at EOT) is higher than that of other comparable studies with refugee populations, which have reported rates ranging from 25% to 34% (Buhmann et al., 2015; Buhmann, Nordentoft, Ekstroem, Carlsson, & Mortensen, 2018; Carlsson et al., 2018). Non-refugee PTSD studies reported a mean dropout rate of 18% (95% CI 14.85–21.75; Imel, Laska, Jakupcak, & Simpson, 2013). An analysis of the dropouts from our study demonstrated higher symptom loads at baseline than in the remainers. Reasons for dropout were logistic problems, physical illness and absenteeism, which complies with other studies in refugees and asylum seekers who typically have difficulties maintaining treatment because of language barriers, fear of stigmatization, complex life challenges, illness, and various other obstacles (Kiselev et al., 2020; Satinsky et al., 2019). Generally, one in three planned sessions in the trauma clinic are cancelled. Four dropouts (almost a third) in the TAU group were discharged by the clinic because of a minimum of three missed appointments without proper cancellations, in accordance with clinical guidelines. An established CBT based intervention delivered according to a manualized approach with established efficacy might have contributed to a higher retainment. A reason for dropout could also have been symptom improvement and no further need of therapy in the TAU group, but a thorough analysis of clinical journals and reported reasons for dropout did not indicate any such improvement (unpublished data, can be obtained on request).
While secondary measures in the TAU group showed improvement following the conclusion of treatment, the positive effects were not sustained until FU, whereas in the tr-MI arm the positive effects were mostly manifest at FU. As music therapy works partly through nonverbal processes, the patients may have needed more time to integrate and recognize its effect. The at-home use of music and imagery to regulate stress between EOT and FU could also have helped stabilize the tr-MI patients and further integrate the benefits of the therapy for continual progress. As with the results of the aforementioned Cochrane review of psychosocial interventions with torture survivors, the treatment effect was seen at FU rather than immediately after treatment (Patel et al., 2014).
Both study interventions used trauma-focused approaches adapting a phased treatment regime with attention to the specific vulnerability of traumatized patients, such as risk of re-traumatization, dissociation, and overwhelm. The participants’ feedback on the sessions emphasized the importance of the therapeutic relationship and the strengthening of hope they derived from improved emotional containment and imagery. Believing that music therapy (tr-MI) holds specific potential for instant arousal regulation and establishing contact with inner resources, we nevertheless find it vital to remind readers that both study interventions took place within a team-based treatment context that attempted to address all psychosocial dimensions of the patients’ complex situations.
4.1. Limitations and strengths
It is a weakness of our study that the standard intervention did not follow a fixed protocol with established validity, other than the research-based national treatment guidelines. The limitations furthermore include the unblinded collection and statistical analysis of secondary outcomes and the absence of a systematically assessed self-rated treatment fidelity.
Among the strengths of this study, we stress that it is the first trial to involve music therapy in a refugee population, that its execution occurred in three locations in naturalistic settings, and that the random sequences were generated, kept and allocated by an external agency. Neutrality to the primary variable was secured by blinding the assessors to the scoring of the HTQ data. The randomization ensured that both musically and non-musically engaged patients were placed in the music therapy group, thus mitigating the influence of musical interest as a confounding variable.
4.2. Perspectives
RCT superiority studies with large samples would be warranted to substantiate GIM therapy against non-active treatments. Qualitative research into the use of music therapy in combination with listening to music at home as a self-help method for refugees with PTSD would likewise provide new knowledge of patient preferences and mechanisms of change, with the potential to improve treatment for this vulnerable group.
In a clinical perspective, the study results indicate that trauma-focused work involving music and imagery may offer a helpful intervention in refugee trauma clinics. The method could be extended in timeframe to better accommodate refugee patients with complex PTSD, who would benefit more from a longer treatment period, and it could be adapted to other trauma populations, such as war veterans, victims of abuse and violence, and work-related trauma sufferers.
5. Conclusion
The music therapy method tr-MI employing trauma-focused music and imagery proved to be noninferior to standard treatment in this study, in terms of its ability to decrease trauma symptoms after treatment and during six-month follow-up. Noninferiority with respect to trauma symptoms was supported by improvements in well-being and fewer symptoms of psychoform dissociation after music therapy. Further research involving comparative trials to substantiate the evidence for music and imagery work with refugees and other trauma populations is warranted.
Acknowledgments
We wish to thank the patients for their willingness to participate in this study, and the psychologists for their contributions to the research and data collection. We also gratefully acknowledge the Trauma Clinic for its hosting of the study and all manner of practical help and support from our colleagues there.
Funding Statement
This study was supported by research grants from The Obel Family Foundation and from the Psychiatric Research fund of Region Zealand. The funding sources played no role in designing the study. The collection, analysis, and interpretation of data, the writing of the report, and the decision to submit the paper for publication were thus the sole responsibility of the authors.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The datasets generated by the study will not be publicly available due to the rules of the Danish Data Protection Agency, but will be available from the corresponding author, after publication, on reasonable request and following signed confidentiality agreement with PI and the Danish Data Protection Agency Region Zealand.
References
- Aalbers, S., Fusar-Poli, L., Freeman, R. E., Spreen, M., Ket, J. C. F., Vink, A. C., … Gold, C. (2017). Music therapy for depression. Cochrane Database of Systematic Reviews 11. Art. No.: CD004517. doi: 10.1002/14651858.CD004517.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno, R., Knapp, R., Tuerk, P., Gilmore, A. K., Lejuez, C., Ruggiero, K., … Foa, E. B. (2017). A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behavior Research and Therapy, 89, 57–15. doi: 10.1016/j.brat.2016.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahonen, H. (2019). Putting the lights on in the room: Guided Imagery and Music (GIM) with trauma survivors. In Grocke D. (Ed.), Guided Imagery and Music – The Bonny method and beyond (2nd ed., ch. 9, pp. 149–186). Barcelona Publishers. [Google Scholar]
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Bech, P., Olsen, L. R., Kjøller, M., & Rasmussen, N. K. (2003). Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. International Journal of Methods in Psychiatric Research, 12(2), 85–91. doi: 10.1002/mpr.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, B., Messell, C., Meyer, S., Cordtz, T., Simonsen, E., Søgaard, U., & Moe, T. (2017). Feasibility of trauma-focused Guided Imagery and Music with adult refugees diagnosed with PTSD – A pilot study. Nordic Journal of Music Therapy, 27(1), 67–86. DOI: 10.1080/08098131.2017.1286368 [DOI] [Google Scholar]
- Beck, B., & Mumm, H. (2015). Forskning i musikterapi og posttraumatisk stress (PTSD) [Research on music therapy and posttraumatic stress]. Dansk Musikterapi, 12(1), 10–20. https://vbn.aau.dk/ws/portalfiles/portal/212374412/2015F_Forskning_i_musikterapi_PTSD.pdf [Google Scholar]
- Beck, B. D. (2018). Music therapy with refugees. In Jacobsen S. L., Petersen I. N., & Bonde L. O. (Eds.), A comprehensive guide to music therapy (pp. 342–352). Philadelphia, PA: Jessica Kingsley Publishers. [Google Scholar]
- Beck, B. D., Lund, S. T., Søgaard, U., Simonsen, E., Tellier, T., Cordtz, T., … Moe, T. (2018). Music therapy versus treatment as usual for refugees diagnosed with posttraumatic stress disorder (PTSD): Study protocol for a randomized controlled trial. Trials, 19(1), 301. doi: 10.1186/s13063-018-2662-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belz, M., Belz, M., Ozkan, I., & Graef-Calliess, I. T. (2017). Posttraumatic stress disorder and comorbid depression among refugees: Assessment of a sample from a German refugee reception center. Transcultural Psychiatry, 54(5–6), 595–610. DOI: 10.1177/1363461517745473 [DOI] [PubMed] [Google Scholar]
- Buhmann, C., Mortensen, E. L., Nordentoft, M., Ryberg, J., & Ekstrøm, M. (2015). Follow-up study of the treatment outcomes at a psychiatric trauma clinic for refugees. Torture, 25, 1. http://doc.rct.dk/doc/TORT2015.1.1.pdf [PubMed] [Google Scholar]
- Buhmann, C. B., Nordentoft, M., Ekstroem, M., Carlsson, J., & Mortensen, E. L. (2018). Long-term treatment effect of trauma-affected refugees with flexible cognitive behavioural therapy and antidepressants. Psychiatry Research, 264, 217–223. doi: 10.1016/j.psychres.2018.03.069 [DOI] [PubMed] [Google Scholar]
- Carlson, E. B., & Waelde, L. C. (1999). The dissociative symptoms scale. Menlo Park: National Center for Posttraumatic Stress Disorder. [Google Scholar]
- Carlson, E. B., Waelde, L. C., Palmieri, P. A., Macia, K. S., Smith, S. R., & McDade-Montez, E. (2018). Development and validation of the dissociative symptoms scale. Assessment, 25(1), 84–98. doi: 10.1177/1073191116645904 [DOI] [PubMed] [Google Scholar]
- Carr, C., d’Ardenne, P., Sloboda, A., Scott, C., Wang, D., & Priebe, S. (2012). Group music therapy for patients with persistent posttraumatic stress disorder—An exploratory randomized controlled trial with mixed methods evaluation. Psychology and Psychotherapy: Theory, Research, and Practice, 85(2), 179–202. doi: 10.1111/j.2044-8341.2011.02026.x [DOI] [PubMed] [Google Scholar]
- Collins, N. L. (1996). Working models of attachment: Implications for explanation, emotion, and behavior. Journal of Personality and Social Psychology, 71(4), 810–832. doi: 10.1037/0022-3514.71.4.810 [DOI] [PubMed] [Google Scholar]
- Dalgaard, N. T., Todd, B. K., Daniel, S. I. F., & Montgomery, E. (2016). The transmission of trauma in refugee families: Associations between intra-family trauma communication style, children’s attachment security and psychosocial adjustment. Attachment & Human Development, 18(1), 69–89. doi: 10.1080/14616734.2015.1113305 [DOI] [PubMed] [Google Scholar]
- Epiinfo . (n.d.). Retrieved from http://wwwn.cdc.gov/epiinfo/
- Fagerland, M. W., Sandvik, L., & Mowinckel, P. (2011). Parametric methods outperformed non-parametric methods in comparisons of discrete numerical variables. BMC Medical Research Methodology, 11(1), 44. doi: 10.1186/1471-2288-11-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández, A. M., & Dufey, M. (2015). Adaptation of Collins’ revised adult attachment dimensional scale to the Chilean context. Psicologia: Reflexão E Crítica, 28(2), 242–252. doi: 10.1590/1678-7153.201528204 [DOI] [Google Scholar]
- Foa, E. B., Keane, T. M., Friedman, M. J., & Cohen, J. A. (Eds.). (2009). Effective treatments for PTSD. Practice guidelines from the international society for traumatic stress studies (2nd ed.). New York City: The Guildford Press. [Google Scholar]
- Greene, C. J., Morland, L. A., Durkalski, V. L., & Frueh, B. C. (2008). Noninferiority and equivalence designs: Issues and implications for mental health research. Journal of Traumatic Stress, 21(5), 433–439. doi: 10.1002/jts.20367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grocke, D. (Ed.). (2019). Guided imagery and music – The Bonny method and beyond (2nd ed.). Dallas, TX: Barcelona Publishers. [Google Scholar]
- Grocke, D., & Moe, T. (Eds.). (2015). Guided imagery & music (GIM) and music imagery methods for individual and group therapy. Philadelphia, PA: Jessica Kingsley. [Google Scholar]
- Hamid, A., Patel, N., & Williams, A. C. (2019). Psychological, social, and welfare interventions for torture survivors: A systematic review and meta-analysis of randomised controlled trials. PLOS Medicine, 16(9), e1002919. doi: 10.1371/journal.pmed.1002919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández-Ruiz, E. (2005). Effect of music therapy on the anxiety levels and sleep patterns of abused women in shelters. Journal of Music Therapy, 42(2), 140–158. DOI: 10.1093/JMT/42.2.140 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., & Green, S. (Eds.). (2011). Cochrane handbook for systematic reviews of interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Retrieved from www.handbook.cochrane.org.
- Hill, M., & Everson, M. L. (2020). Indicators likely to contribute to clinical and functional improvement among survivors of politically-sanctioned torture. Torture Journal, 29(3), 5–26. doi: 10.7146/torture.v29i3.115202 [DOI] [PubMed] [Google Scholar]
- Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. doi: 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerling, P., & Heyns, M. (2020). Exploring Guided Imagery and Music as a well-being intervention: A systematic literature review. Nordic Journal of Music Therapy, 29(4), 371–390. doi: 10.1080/08098131.2020.1737185 [DOI] [Google Scholar]
- Jespersen, K. V., Koenig, J., Jennum, P., & Vuust, P. (2015). Cochrane database of systematic reviews. Music for Insomnia in Adults, 8. Art. No.: CD010459. doi: 10.1002/14651858.CD010459.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jespersen, K. V., & Vuust, P. (2012). The effect of relaxation music listening on sleep quality in traumatized refugees: A pilot study. Journal of Music Therapy, 49(2), 205–229. doi: 10.1093/jmt/49.2.205 [DOI] [PubMed] [Google Scholar]
- Kiselev, N., Pfaltz, M., Haas, F., Schick, M., Kappen, M., Sijbrandij, M., … Morina, N. (2020). Structural and socio-cultural barriers to accessing mental healthcare among Syrian refugees and asylum seekers in Switzerland. European Journal of Psychotraumatology, 11(1), 1717825. doi: 10.1080/20008198.2020.1717825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleijn, W. C., Hovens, J. E., & Rodenburg, J. J. (2001). Posttraumatic stress symptoms in refugees: Assessments with the Harvard Trauma Questionnaire and the Hopkins symptom checklist-25 in different languages. Psychological Reports, 88(2), 527–532. doi: 10.2466/pr0.2001.88.2.527 [DOI] [PubMed] [Google Scholar]
- Landis-Shack, N., Heinz, A. J., & Bonn-Miller, M. O. (2017). Music therapy for posttraumatic stress in adults: A theoretical review. Psychomusicology. 27(4), 334–342. DOI: 10.1037/pmu0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liotti, G. (2004). Trauma, dissociation, and disorganized attachment: Three strands of a single braid. Psychotherapy: Theory, Research, Practice, Training, 41(4), 472–486. doi: 10.1037/0033-3204.41.4.472 [DOI] [Google Scholar]
- Liu, G. F., Lu, K., Mogg, R., Mallick, M., & Mehrotra, D. V. (2009). Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Statistics in Medicine, 28(20), 2509–2530. doi: 10.1002/sim.3639 [DOI] [PubMed] [Google Scholar]
- Maack, C. (2012). Outcomes and processes of the Bonny Method of Guided Imagery and Music (GIM) and its adaptations and Psychodynamic Imaginative Trauma Therapy (PITT) for women with Complex PTSD. Ph.D. thesis, Department of Communication and Psychology, Aalborg University. [Google Scholar]
- McKinney, C. H., & Honig, T. J. (2017). Health outcomes of a series of Bonny Method of Guided Imagery and Music sessions: A systematic review. Journal of Music Therapy, 54(1), 1–34. doi: 10.1093/jmt/thw016 [DOI] [PubMed] [Google Scholar]
- Mollica, R. F., Caspi-Yarvin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- Morina, N., Schnyder, U., Schick, M., Nickerson, A., & Bryant, R. A. (2016). Attachment style and interpersonal trauma in refugees. Australian and New Zealand Journal of Psychiatry, 50(12), 1161–1168. doi: 10.1177/0004867416631432 [DOI] [PubMed] [Google Scholar]
- National clinical recommendations (2017). Pakkeforloeb for traumatisede flygtninge [Treatment package for traumatized refugees]. Retrieved from https://www.sundhed.dk/content/cms/64/75764_pakkeforloeb-for–traumatiserede-flygtninge.pdf
- Nesterko, Y., Jäckle, D., Friedrich, M., Holzapfel, L., & Glaesmer, H. (2019). Prevalence of posttraumatic stress disorder, depression and somatization in recently arrived refugees in Germany: An epidemiological study. Epidemiologic and Psychiatric Sciences, 29, e40. doi: 10.1017/S2045796019000325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newnham, E. A., Hooke, G. R., & Page, A. C. (2010). Monitoring treatment response and outcomes using the World Health Organization’s Wellbeing Index in psychiatric care. Journal of Affective Disorders, 122(1–2), 133–138. doi: 10.1016/j.jad.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Nice . (2005, March 23). Post-traumatic stress disorder: Management. Clinical guideline [CG26]. Retrieved from https://www.nice.org.uk/guidance/ng116/evidence/march-2005-full-guideline-pdf-6602623598
- Nice . (2018, December 12). Clinical guidelines PTSD [NG116]. Retrieved from https://www.nice.org.uk/guidance/ng116
- Nijsenhuis, E. (2010). The scoring and interpretation of the SDQ-20 and SDQ-5. Journal of Neurocognitive Research, 52. http://www.activitas.org/index.php/nervosa/article/view/82 [Google Scholar]
- Nijenhuis, E. R. S., Spinhoven, P., Van Dyck, R., Richard, M. D., Van Der Hart, O., & Vanderlinden, J. (1996). The development and psychometric characteristics of the Somatoform Dissociation Questionnaire (SDQ-20). The Journal of Nervous and Mental Disease, 184(11), 688–694. doi: 10.1097/00005053-199611000-00006 [DOI] [PubMed] [Google Scholar]
- Nijenhuis, E. R. S., Spinhoven, P., Van Dyck, R., Van Der Hart, O., & Vanderlinden, J. (1998). Degree of somatoform and psychological dissociation in dissociative disorder is correlated with reported trauma. Journal of Traumatic Stress, 11(4), 711–730. doi: 10.1023/A:1024493332751 [DOI] [PubMed] [Google Scholar]
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Wietse, T., … Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PLOS ONE, 12(2), e0171030. doi: 10.1371/journal.pone.0171030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palic, S. (2013). Measurement and documentation of complex PTSD in treatment seeking traumatized refugees. PhD thesis. Denmark: Syddansk University. [Google Scholar]
- Palic, S., & Elklit, A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. Journal of Affective Disorders, 131(1–3), 8–23. doi: 10.1016/j.jad.2010.07.005 [DOI] [PubMed] [Google Scholar]
- Patel, N., Kellezi, B., & Williams, A. C. D. C. (2014). Psychological, social, and welfare interventions for psychological health and well-being of torture survivors. Cochrane Database of Systematic Reviews. DOI: 10.1002/14651858.CD009317.pub2 [DOI] [PMC free article] [PubMed]
- Pedersen, F. S. (2006). Attachment and trauma: A study of correlations between attachment, social support and PTSD and validation of the Revised Adult Attachment Scale. Psykologisk Studieskriftserie, 9(2), 1–155. [Google Scholar]
- Piaggio, G., Elbourne, D. R., Pocock, S. J., Evans, S. J. W., & Altman, D. G. (2012). CONSORT Group FT. Reporting of noninferiority and equivalence randomized trials: Extension of the CONSORT 2010 Statement. JAMA, 308(24), 2594–2604. doi: 10.1001/jama.2012.87802 [DOI] [PubMed] [Google Scholar]
- Riber, K. (2016). Attachment organization in Arabic-speaking refugees with posttraumatic stress disorder. Attachment & Human Development, 18(2), 154–175. doi: 10.1080/14616734.2015.1124442 [DOI] [PubMed] [Google Scholar]
- Ripardo, R., Ferreira, J., & Howat-Rodrigues, A. (2019). Collins and Read Revised Adult Attachment Scale (RAAS) validity evidences. Psico Porto Alegre, 50(2), e29567. DOI: 10.15448/1980-8623.2019.2.29567 [DOI] [Google Scholar]
- Rudstam, G., Elofsson, U., Søndergaard, H. P., Bonde, L. O., & Beck, B. D. (2017). Trauma-focused group music and imagery with women suffering from PTSD/complex PTSD: A feasibility study. Approaches, Special Issue, 9(2), 202–216. http://approaches.gr/wp-content/uploads/2017/12/2-Approaches-9-2-2017-rudstam-a20171222.pdf [Google Scholar]
- Satinsky, E., Fuhr, D., Woodward, A., Sondorp, E., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy, 123(9), 851–863. doi: 10.1016/j.healthpol.2019.02.007 [DOI] [PubMed] [Google Scholar]
- Schulz, P. M., Resick, P. A., Huber, L. C., & Griffin, M. G. (2006). The effectiveness of cognitive processing therapy for PTSD with refugees in a community setting. Cognitive and Behavioral Practice, 13(4), 322–331. doi: 10.1016/j.cbpra.2006.04.011 [DOI] [Google Scholar]
- Schumi, J., & Wittes, J. T. (2011). Through the looking glass: Understanding non-inferiority. Trials, 12(1), 106. doi: 10.1186/1745-6215-12-106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonne, C., Lohmann, J. M. C., Bech, P., Elklit, A., & Mortensen, E. L. (2016). Treatment of trauma-affected refugees with venlafaxine versus sertraline combined with psychotherapy: A randomised study. BMC Psychiatry, 16(1), 383. doi: 10.1186/s12888-016-1081-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story, M., & Beck, B. D. (2017). Guided Imagery and Music with female military veterans: An intervention development study. The Arts in Psychotherapy, 55, 93–102. doi: 10.1016/j.aip.2017.05.003 [DOI] [Google Scholar]
- Suhaiban, H. A., Grasser, L. A., & Javanbakht, A. (2019). Mental health of refugees and torture survivors: A critical review of prevalence, predictors, and integrated care. International Journal of Environmental Research and Public Health, 16(13), 2309. doi: 10.3390/ijerph16132309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, C. T., Vidgen, A., & Roberts, N. P. (2018). Psychological interventions for post-traumatic stress disorder in refugees and asylum seekers: A systematic review and meta-analysis. Clinical Psychology Review, 63, 66–79. doi: 10.1016/j.cpr.2018.06.006 [DOI] [PubMed] [Google Scholar]
- Tinghög, P., Malm, A., Arwidson, C., Sigvardsdotter, E., Lundin, A., & Saboonchi, F. (2017). Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: A population- based survey. BMJ Open, 7(12), e018899. doi: 10.1136/bmjopen-2017-018899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp, C. W., Østergaard, S. D., Søndergaard, S., & Bech, P. (2015). The WHO-5 Well-Being Index: A systematic review of the literature. Psychotherapy and Psychosomatics, 84(3), 167–176. doi: 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- Turrini, G., Purgato, M., Acarturk, C., & Anttila, M. (2019). Efficacy and acceptability of psychosocial interventions in asylum seekers and refugees: Systematic review and meta-analysis. Epidemiology and Psychiatric Sciences, 28(4), 376–388. doi: 10.1017/S2045796019000027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk, J., Bosman, L., Hoekstra, T., Rijnhart, J., Welten, M., & Heymans, M. (2018). Different ways to estimate treatment effects in randomised controlled trials. Contemporary Clinical Trials Communications, 10, 80–85. doi: 10.1016/j.conctc.2018.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uphoff, E., Purgato, M., Churchill, R., & Barbui, C. (2019). An overview of systematic reviews on mental health promotion, prevention, and treatment of common mental disorders for refugees, asylum seekers, and internally displaced persons. Cochrane Database of Systematic Reviews, (10). doi: 10.1002/14651858.CD013458 [DOI] [PMC free article] [PubMed]
- Uygun, E. (2020). The relationship between the types of traumatic events and well-being, Post-Traumatic Stress levels and gender differences in Syrian patients: A cross-sectional controlled study. Journal of Immigrant and Minority Health. doi: 10.1007/s10903-020-01097-0 [DOI] [PubMed]
- Van Ee, E., Kleber, R. J., & Jongmans, M. J. (2016). Parental PTSD, adverse parenting and child attachment in a refugee sample. Attachment & Human Development, 18(3), 273–291. doi: 10.1080/14616734.2016.1148748 [DOI] [PubMed] [Google Scholar]
- WFMT (World Federation of Music Therapy) . (2011). Retrieved from https://wfmt.info/wfmt-new-home/about-wfmt/
- WHO . (n.d.). Process of translation and adaptation of instruments. Retrieved from https://www.who.int/substance_abuse/research_tools/translation/en/
- World Health Organization (WHO) . (1993). The ICD-10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated by the study will not be publicly available due to the rules of the Danish Data Protection Agency, but will be available from the corresponding author, after publication, on reasonable request and following signed confidentiality agreement with PI and the Danish Data Protection Agency Region Zealand.


