The COVID-19 pandemic has catalyzed rapid innovation for healthcare delivery models that maintain provision of high-quality medical care while preserving physical distancing measures and balancing the supply of clinical services with surge in demand. Many of these solutions involve uptake of existing care models that previously had low utilization rates.1 One example is Hospital at Home (HaH), the outpatient provision of acute services traditionally provided in an inpatient setting.2 This care model has multiple potential advantages in a pandemic setting, such as limiting nosocomial spread and helping to reduce inpatient capacity strain.3 Additionally, HaH has potential to reduce healthcare spending through reducing direct cost of the acute care episode,4–6 which appeals to the economic uncertainty of many healthcare systems during and beyond the pandemic.7
Indeed, reduced spending is posited as one of HaH’s primary benefits. Hospitalizations are expensive and represent the largest contributor to overall healthcare spending.8 Because providing advanced interventions in an outpatient setting may be less expensive than equivalent inpatient care, substituting HaH for inpatient care has promise to decrease spending. However, the true effect of HaH on spending will depend on how HaH is implemented. Healthcare innovations are frequently promoted as cost-saving solutions, yet examples such as robotic-assisted surgery,9 transcatheter aortic valve replacement,10 and telehealth services11 suggest that innovations must be carefully applied in order to ensure that they are provided to the intended population, resulting in true cost savings along with high quality. Once the medical community shifts from crisis mode back into sustainable operations, it will be important to re-evaluate whether stopgap care models ultimately demonstrate effectiveness and/or reduce spending before permanent integration into healthcare systems. To help guide decisions regarding implementation or de-implementation of HaH after the COVID-19 pandemic, we describe 3 key factors that are necessary for the accurate evaluation of HaH programs’ effect on healthcare spending, following a similar approach as described for telehealth services.12
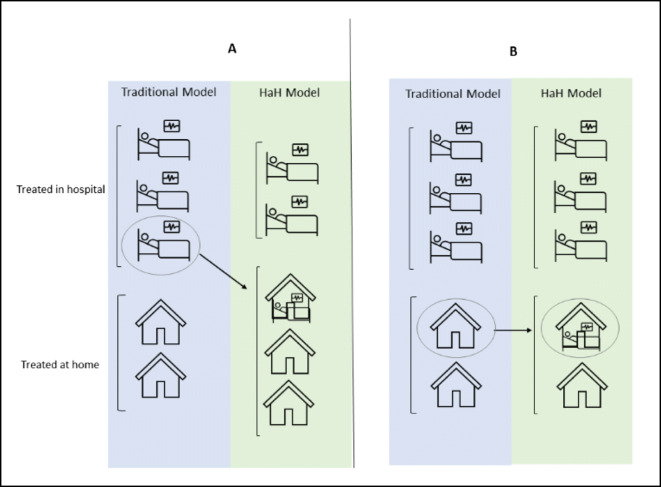
First, the effect of HaH on spending will depend on the proportion of HaH utilization that is substitutive versus additive. HaH programs are designed to substitute a lower-cost outpatient care setting for an expensive inpatient setting. For example, patients who previously would have been admitted to the hospital to receive intravenous antibiotics could now receive intravenous antibiotics at home. However, a potential unintended consequence is that HaH programs might promote new use of advanced interventions (treatments or intensive monitoring) in patients who otherwise would have been discharged home without advanced interventions (e.g., oral antibiotics). The discretionary nature of decisions to use advanced interventions increases the likelihood that HaH will result in additive utilization. Current data suggest that physicians already overuse advanced interventions such as intravenous route of administration, urinary catheters, and telemetry monitoring.13–15 It is plausible that removing the inconvenience of hospitalization could further increase overutilization (Fig. 1). To promote substitutive use rather than additive, independent panels composed of expert professionals without conflicts of interest could create point-of-care tools that take advantage of risk models and appropriateness criteria to provide patient-specific risk profiles useful in decision-making for individual patients.
Figure 1.
Panel A: In a substitutive model of Hospital at Home, selected patients who would have received advanced therapies in hospital under a traditional model are instead provided advanced therapies at home. Panel B: In an additive model, patients who would have not received advanced therapies at all are instead provided advanced therapies at home.
The extent to which HaH provides additive or low-value utilization as HaH accessibility expands introduces the concern of demand elasticity. Demand elasticity refers to how sensitive the demand for a good or service is to changes in other economic variables. It is typically applied in terms of price; but can also describe supply-induced demand—i.e., “if you build it they will come”.16 The concern for supply-induced demand has been well-described for intensive care unit beds.17 Similarly, HaH implementation must safeguard against allowing improved accessibility of advanced interventions to create their own demand.
Existing studies of HaH have design features that preclude assessment of substitutive versus additive utilization because patients are not eligible to be considered for enrollment until after a physician has independently determined need for hospitalization to deliver advanced therapies. Foreseeably, in actual practice, knowledge of the availability of HaH services may influence the judgment of necessity of advanced therapies. Confirmation of additive utilization through pragmatic or implementation studies would have major implications for healthcare delivery and financing. For example, constraining supply of HaH services, perhaps through certificate of need laws or other legislation, may help ensure patients who are unlikely to benefit from advanced therapies are not receiving them.
A second factor influencing the effect of HaH on spending is how utilization of HaH affects subsequent health status and care. HaH may decrease spending if it is provided to patients in whom a costly adverse event of hospitalization, such as delirium or nosocomial infection, might be prevented. However, HaH may also increase downstream utilization, particularly if it is applied to patients in whom the risk-benefit ratio may favor traditional home-based care without advanced therapies. One reason for this is that standards for quality and safety like those that exist for traditional hospitals currently do not exist for HaH programs. Delivery of advanced medical therapies is associated with risk of complications which may be increased in a setting where routine safety practices have not been established. For example, complications of venous access devices such as peripherally inserted central catheters may be higher in a HaH setting, where rigorous safety standards such as those required by the Joint Commission18 are not in place. Currently, leaders of a consortium of hospital-at-home programs are working to create quality standards that could shape regulatory and reimbursement policies.19
Additionally, the “immersion” experience of hospitalization offers opportunities beyond simply the use of advanced interventions, such as providing a foundation for illness and treatment education and discussion of the risk factors for potential complications and long-term effects of the illness. Hospital days provide time for patients to begin to engage hospital physicians, nurses, and social workers to discuss the emotional and psychological ramifications of their illnesses. Hospital staff leverage the opportunity to discuss modifiable risk factors and provide motivational interviewing to promote lifestyle changes. Proper implementation of HaH should account for these “intangibles” of hospitalization to ensure that downstream health and healthcare utilization are not adversely affected.
The third factor is the relative cost difference between an HaH episode and an equivalent inpatient stay. Prior to the COVID-19 pandemic, reimbursement for HaH services was limited to select Medicare Advantage and commercial insurance plans. Responding to the urgent need to increase capacity of the US healthcare system during the COVID-19 pandemic, the Centers for Medicare and Medicaid (CMS) outlined steps for hospitals to acquire a waiver allowing reimbursement for the provision of acute care to patients outside a traditional hospital setting under the Hospitals Without Walls Program approved in March 2020.20 Building on the Hospitals Without Walls initiative and the expansion of telehealth, CMS expanded regulatory flexibilities for hospitals to treat eligible patients in their homes through telehealth and remote monitoring in the Acute Hospital Care At Home Program announced in November 2020. This program was developed to support HaH models that already have extensive experience providing acute hospital care at home. Six health systems were initially approved for the new waivers and CMS launched an online portal for additional health systems to submit waiver applications (https://aspe.hhs.gov/proposal-submissions-physician-focused-payment-model-technical-advisory-committee).
The cost savings of HaH depend on it being a lower cost service compared to inpatient care. Under the current waivers, Medicare inpatient payments to a hospital are the same as they would have been if the care was provided in a traditional inpatient setting. How HaH will be routinely reimbursed in the USA after the COVID-19 pandemic remains unknown. If HaH is reimbursed at a much lower rate than an equivalent inpatient stay, its use can increase additively and still be cost-saving. However, if high reimbursement is used to incentivize development of HaH programs (as is the case for the CMS Hospitals Without Walls Program), this could not only negate the desired cost savings but may also lead to overutilization in patients who would not have been hospitalized in the first place. Outside of the pandemic, the health authority in Australia pays for an HaH admission at the same rate as an inpatient admission, which has been a major incentive to increased utilization of HaH services.21 However, because patients selected for hospital at home services are often less complex than those selected for traditional inpatient treatment, lower reimbursement rates may be appropriate. Although fair reimbursement is important to incentivize adoption of HaH programs, high rates of reimbursement may undermine the potential of HaH to reduce spending or create artificial savings by shifting a higher proportion of costs to hospitals, as the DRG payment to hospitals may be inadequate if lower cost, less complex patients are removed from the average inpatient population. These economic disincentives would be mitigated by capitated or population-based payments in which accountability for resource utilization and cost is assumed.
Finally, because the true aim is improving value, not simply reducing cost, a comprehensive evaluation of the economic effect of HaH on healthcare systems must also incorporate assessments of overall value-add due to potential benefits such as improved health, better patient experience, reduction in caregiver stress, and better end-of-life care.22 Future studies should apply a value framework to comprehensively determine the incremental benefit of the program relative to its cost. Additionally, the impact of HaH on disparities in care for historically vulnerable populations should be incorporated into estimates of program value from a societal perspective.
While HaH is briskly adopted as an innovative response to COVID-19, we must re-evaluate this care delivery model’s effect on health outcomes and healthcare spending once the pandemic has stabilized. Whether HaH will live up to its promise of decreasing spending will depend on (i) the proportion of HaH utilization that is substitutive versus additive, (ii) the effect of HaH on downstream events, and (iii) the reimbursement models for HaH versus traditional inpatient care.
Declarations
Conflict of Interest
ST receives grant funding from NIH, outside of the submitted work. LG has an unpaid position on the Board of Chancellors of the American College of Radiology.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wosik J, Fudim M, Cameron B, et al. Telehealth Transformation: COVID-19 and the rise of Virtual Care, J Am Med Inform Assoc. 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed]
- 2.Leff B. Defining and disseminating the hospital-at-home model. CMAJ. 2009;180(2):156–157. doi: 10.1503/cmaj.081891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sitammagari K, Murphy S, Kowalkowski M, et al. Insights From Rapid Deployment of a “Virtual Hospital” as Standard Care During the COVID-19 Pandemic. Ann Intern Med. 2020;11:M20–4076. doi: 10.7326/M20-4076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levine DM, Ouchi K, Blanchfield B, Saenz A, Burke K, Paz M, Diamond K, Pu CT, Schnipper JL. Hospital-Level Care at Home for Acutely Ill Adults: A Randomized Controlled Trial. Ann Intern Med. 2020;172(2):77–85. doi: 10.7326/M19-0600. [DOI] [PubMed] [Google Scholar]
- 5.Cryer L, Shannon SB, Van Amsterdam M, Leff B. Costs for ‘hospital at home’ patients were 19 percent lower, with equal or better outcomes compared to similar inpatients. Health Aff (Millwood). 2012;31(6):1237–1243. doi: 10.1377/hlthaff.2011.1132. [DOI] [PubMed] [Google Scholar]
- 6.Physician-Focused Payment Model Technical Advisory Committee. Report to the Secretary of Health and Human Services. Comments and Recommendation on “HaH-Plus” (Hospital at Home Plus) Provider-Focused Payment Model. 2017. https://aspe-hhs-gov.libproxy.lib.unc.edu/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf. Accessed 5 May 2020.
- 7.Khullar D, Bond AM, Schpero WL. COVID-19 and the Financial Health of US Hospitals. JAMA. 2020;323(21):2127–2128. doi: 10.1001/jama.2020.6269. [DOI] [PubMed] [Google Scholar]
- 8.https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet. Accessed 2 Feb 2021.
- 9.Gkegkes ID, Mamais IA, Iavazzo C. Robotics in general surgery: A systematic cost assessment. J Minim Access Surg. 2017;13(4):243–255. doi: 10.4103/0972-9941.195565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Modi PK, Sukul DA, Oerline M, Thompson MP, Nallamothu BK, Ellimoottil C, Shahinian VB, Hollenbeck BK. Episode Payments for Transcatheter and Surgical Aortic Valve Replacement. Circ Cardiovasc Qual Outcomes. 2019;12(12):e005781. doi: 10.1161/CIRCOUTCOMES.119.005781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ashwood JS, Mehrotra A, Cowling D, Uscher-Pines L. Direct-to-consumer telehealth may increase access to care but does not decrease spending. Health Aff (Millwood). 2017;36:485–91. doi: 10.1377/hlthaff.2016.1130. [DOI] [PubMed] [Google Scholar]
- 12.Licurse AM, Mehrotra A. The Effect of Telehealth on Spending: Thinking Through the Numbers. Ann Intern Med. 2018;168(10):737–738. doi: 10.7326/M17-3070. [DOI] [PubMed] [Google Scholar]
- 13.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–2. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 14.Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA. ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf. 2015;24:167–174. doi: 10.1136/bmjqs-2014-003821. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067–76. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rice TH, Labelle RJ. Do physicians induce demand for medical services? J Health Polit Policy Law. 1989;14(3):587–600. doi: 10.1215/03616878-14-3-587. [DOI] [PubMed] [Google Scholar]
- 17.Gooch RA, Kahn JM. ICU bed supply, utilization, and health care spending: an example of demand elasticity. JAMA. 2014;311:567–8. doi: 10.1001/jama.2013.283800. [DOI] [PubMed] [Google Scholar]
- 18.The Joint Commission. National Patient Safety Goals. Available at: https://www.jointcommission.org/assets/1/6/2015_NPSG_HAP.pdf. Accessed 29 Jan 2021.
- 19.https://hahusersgroup.org/about/. Accessed 2 Feb 2021.
- 20.https://www.cms.gov/files/document/covid-hospitals.pdf. Accessed 2 Feb 2021.
- 21.Montalto M. The 500-bed hospital that isn’t there: the Victorian Department of Health review of the Hospital in the Home program. Med J Aust. 2010;193(10):598–601. doi: 10.5694/j.1326-5377.2010.tb04070.x. [DOI] [PubMed] [Google Scholar]
- 22.Levine DM, Pian J, Mahendrakumar K, Patel A, Saenz A, Schnipper JL. Hospital-Level Care at Home for Acutely Ill Adults: a Qualitative Evaluation of a Randomized Controlled Trial. J Gen Intern Med. 2021. 10.1007/s11606-020-06416-7. [DOI] [PMC free article] [PubMed]