Abstract
These initial data suggest that with prenatal vitamins and choline supplements, we might decrease one risk factor associated with poorer health outcomes disproportionally affecting Black families, ie, preterm birth. Dissemination of this research fulfills the principle of Justice in the Belmont Report, to ensure that participants from different racial, ethnic and socioeconomic groups receive benefits from research directed to their specific problems.
Keywords: phosphatidylcholine, infant preterm, fetal development, African American, child development, schizophrenia
We appreciate the opportunity to discuss our study in the context of demographics in health disparities. The study was designed to assess prenatal stress and possible interactions with maternal choline plasma concentration on the early development of cerebral inhibition, behavior, and temperament in the offspring. Over the past decade, we have investigated interactions between maternal plasma choline and gestational exposure to infection and other factors linked in the scientific literature with poorer child outcomes, especially those associated with increased risk for later mental illness. The women who enroll are asked to self-identify their race and ethnicity in accordance with NIH guidelines.
In this study, we investigated a number of maternal variables, including age, race and ethnicity, BMI, and polymorphic variation in genes involved in choline metabolism, to assess if any were associated with maternal choline concentration. Grouping together as Black the participants who self-identified as Black or African American or predominantly Black or African American multiethnic ancestry is consistent with current NIH-defined categories. The finding that this group of women had the lowest choline concentration of any group while controlling for other maternal variables was unexpected. We examined possible reasons for the finding. Women who self-identified as White from the same neighborhoods with the same access to grocery stores as Black women had higher choline concentrations. Black women in this cohort were less likely to be obese, use marijuana, tobacco, or alcohol, and had similar years of education compared to White women. There were no significant genetic associations with ancestry and choline concentration. Pregnant women in rural Uganda had choline concentrations significantly higher than Black American women in our study. Finally, we assayed levels of cortisol in the women’s hair, which were significantly higher in Black women and related to a number of stressors, as described in the paper.1 Higher cortisol levels were associated with lower choline levels, possibly because cortisol causes the mother’s liver to sequester choline in early gestation, thereby restricting its availability to the fetus.
We do not know all the reasons for elevated hair cortisol observed in the Black women in this study. Our study included comprehensive self-ratings of mood, anxiety, and stress, but it was not designed to assess systemic racism or other contributors to health disparities. Despite no differences between the groups in terms of prenatal and pediatric care or prenatal vitamins and folic acid, babies born to Black women were more likely to be preterm. The infants’ lower gestational age at birth was related to lower maternal choline concentrations in early gestation. Lower gestational age at birth has adverse effects on the development of cognition and behavior throughout childhood.
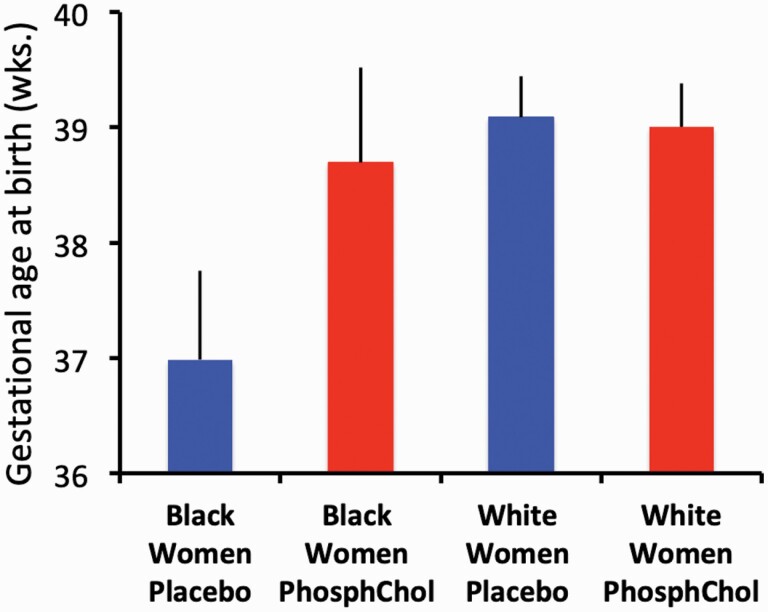
We re-examined gestational age at birth in our earlier clinical trial of phosphatidylcholine supplementation. The FDA recommends at least 550 mg choline from diet or supplements for pregnant women. It approved our administering 900 mg as phosphatidylcholine, randomized with placebo. All women received intensive dietary instruction to help them eat more choline-containing food. However, other investigators have subsequently found that variance in diet has minimal effects on choline concentrations, particularly in Black women. We found that the mean gestational age of babies born to Black mothers who received phosphatidylcholine supplementation approached that of babies born to White women (figure 1). The mean gestational age for babies of Black mothers who received placebo was 3 weeks preterm.
Fig. 1.
Gestational age at birth in a randomized clinical trial of Phosphatidylcholine supplementation. All women received guidance for adequate dietary choline intake. Details are in the full report.1
Maternal choline supplements are not a panacea for the myriad factors that contribute to the disparities in health and access to health care, including the effects of systemic racism encountered by these mothers; nor can it protect children from the impact of discrimination as they enter life. These initial data suggest that with prenatal vitamins and choline supplements, we might decrease one risk factor associated with poorer health outcomes disproportionally affecting Black families, ie, preterm birth. Dissemination of this research fulfills the principle of Justice in the Belmont Report, to ensure that participants from different racial, ethnic and socioeconomic groups receive benefits from research directed to their specific problems. The NIH Office of Behavioral Health and Social Sciences Research featured the paper in its December 2020 Research Spotlights.2
The number of individuals in the 2 studies is small, 40 Black women. This limitation and others are discussed in the paper. Larger studies designed to address the multidimensionality in participant characteristics are needed to fully understand the utility of choline in addressing prenatal health disparities.
The American Medical Association recommends that all prenatal vitamin regimens contain evidence-based amounts of choline.3 The pure phosphatidylcholine we study costs over $800 per pregnancy, and other choline supplements cost nearly $100. Savings from preterm neonatal care as well as later behavioral health care could balance a modest investment in supplements during gestation. Otherwise, cost is a barrier for the women who most need supplements. Raising awareness of the benefits of choline supplements and adding prenatal choline supplements to formularies could benefit all families. Dialogues about the causes and potential interventions for early health disparities are helpful in this effort.
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Funding
This work was supported by the National Institute of Child Health and Human Development (K12HD001271-11 to M.C.H.); National Center for Advancing Translational Sciences (UL1 TR001082); National Institute of Diabetes and Digestive and Kidney Diseases (R01DK56350 to S.Z.); The Institute for Children’s Mental Health; and the Anschutz Foundation.
References
- 1.Hunter SK, Hoffman MC, McCarthy L, et al. . Black American maternal prenatal choline, offspring gestational age at birth, and developmental predisposition to mental illness Schizophr Bull. 2021;47(4):896–905. doi: 10.1093/schbul/sbaa171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NIH Office of Behavioral and Social Science Research. Research Spotlights December 2020. https://obssr.od.nih.gov/research-spotlights-december-2020/. Accessed January 15, 2021.
- 3.AMA. Proceedings of the 2017 Annual Meeting House of Delegates. https://www.ama-assn.org/about/proceedings-2017-annual-meetinghouse-delegates. Accessed November 27, 2017.