Abstract
This article aims to evaluate “racial”, ethnic, and population diversity—or lack thereof—in psychosis research, with a particular focus on socio-environmental studies. Samples of psychosis research remain heavily biased toward Western, Educated, Industrialized, Rich, and Democratic (WEIRD) societies. Furthermore, we often fail to acknowledge the lack of diversity, thereby implying that our findings can be generalized to all populations regardless of their social, ethnic, and cultural background. This has major consequences. Clinical trials generate findings that are not generalizable across ethnicity. The genomic-based prediction models are far from being applicable to the “Majority World.” Socio-environmental theories of psychosis are solely based on findings of the empirical studies conducted in WEIRD populations. If and how these socio-environmental factors affect individuals in entirely different geographic locations, gene pools, social structures and norms, cultures, and potentially protective counter-factors remain unclear. How socio-environmental factors are assessed and studied is another major shortcoming. By embracing the complexity of environment, the exposome paradigm may facilitate the evaluation of interdependent exposures, which could explain how variations in socio-environmental factors across different social and geographical settings could contribute to divergent paths to psychosis. Testing these divergent paths to psychosis will however require increasing the diversity of study populations that could be achieved by establishing true partnerships between WEIRD societies and the Majority World with the support of funding agencies aspired to foster replicable research across diverse populations. The time has come to make diversity in psychosis research more than a buzzword.
Keywords: environment, diversity, ethnicity, race, population, genetics, exposome, health disparities, schizophrenia
Our ability to reach unity in diversity will be the beauty and the test of our civilization. (Mahatma Gandhi, Young India, January 8, 1925)
The biased sampling in mental health research has been a persistent issue over decades. It is striking that the majority of psychological theories are based on empirical studies representing only 12% of the world population and are biased toward Western, Educated, Industrialized, Rich, and Democratic (WEIRD) populations.1 Consequently, the current state of psychological science fails to adequately account for cultural and contextual differences that would increase our understanding of human behavior. Furthermore, these studies fail to acknowledge the lack of diversity, thereby implying that their findings can be generalized to all populations regardless of their social, ethnic, and cultural background. The failure to account for diversity, such as in genomic research, implies that insights, theories, and interventions are only applicable to and benefitting “the privileged few.” 2 Biased sampling not only leads to detrimental shortcomings for the applicability of research findings but also exacerbates already existing global health disparities.3
Evidence suggests that the prevalence and incidence of schizophrenia vary remarkably across social groups and geographical areas.4,5 It is an urgent matter to identify risk factors for psychosis spectrum disorder and test interventions in diverse populations beyond WEIRD societies. In this viewpoint, we attempt to review “racial”, ethnic, and population diversity—or lack thereof—in psychosis research, with a particular focus on socio-environmental studies.
Representation of Diversity in Clinical Trials
Although clinical mental health research has arguably advanced over the past half-century, leading to a better understanding of underlying mechanisms of mental disorders and evidence-informed treatments, the lack of diversity has been a major barrier for further progress.6 Therefore, the National Institutes of Health (NIH) instituted a regulatory guideline more than two decades ago but has yet to achieve its goals of increasing diversity and better reporting of ethnic characteristics in the NIH-funded clinical trials.7
The varying degrees of diversity are noticeable in clinical trials of psychosis conducted in North America. The North American Prodrome Longitudinal Study (NAPLS), aimed at identifying individuals with clinical high risk to prevent transition to psychosis, consisted of only 15.5% African Americans.8 In comparison, the NIMH RAISE First Episode Psychosis Program enrolled 28% African Americans for the active intervention group (the NAVIGATE arm), which was nonetheless much lower than the frequency of African Americans (49%) observed in the community care comparison group.9 Consistent with this trend, the sample of the long-acting injectable risperidone trial, aimed at improving adherence to treatment and outcomes in schizophrenia, consisted of 49% African Americans.10 In the RAISE-ETP trial, the improvement with NAVIGATE, the coordinated specialty care intervention, on the outcome measures, ie, quality of life and psychosis severity, was significant for patients in the highest quartile of socioeconomic status, but the results in the remaining 75% of patients were small and statistically insignificant.11 African American and Latin American first-episode psychosis patients have also been shown to use behavioral services less compared with European American patients.12 There may be various reasons for these differences, such as structural challenges to accessing care, divergent pathways to care, a greater use of community mental health centers, attitudinal barriers such as mistrust of research, and socioeconomic and health disparities experienced by African Americans.13,14 However, there is a single take-home message. Early intervention research—as well as “at-risk clinics” that offer comprehensive services such as individual therapies and family psychoeducation—should aim for increasing inclusion of African Americans to achieve a proportionally representative sample to the urban population drawn from. The enrollment of Asian Americans with psychotic disorders in clinical trials was even lower than those of other ethnic minority populations in the United States.15 Compared with the United States, neither the European Union nor the United Kingdom has yet established a strong policy to stipulate the enrollment of minority populations to clinical trials; and therefore, the representation of ethnic diversity should presumably be even lower than in the United States. The paucity of data and the absence of rigorous early detection and intervention clinical trials in the “Majority World” is another important issue and underscores the need for greater diversity and inclusiveness in research.
Active Noninclusion of “Racial” and Ethnic Diversity in Genomic Research
The lack of sample diversity in genomic research and its consequences are out in the open. By 2009, 96% of participants in the genome-wide association studies (GWAS) were of European descent.3 By active noninclusion of African, Latin American, and Indigenous populations, the GWAS have been missing out on a broad proportion of the world population, implicating that genomics only benefit the privileged few.2 This connotes that researching, and ultimately helping and curing, people of European ancestry is the first and only concern. “The genomics of inequality” has consequences that further exacerbate disparities in global health care.16
It has long been known that population stratification is a major confounder in genetic research—fundamentally limiting the usefulness of measures such as polygenic risk score (PRS). Therefore, populations in genomic studies are commonly stratified based on their ancestry; and only the largest population, which is European ancestry unfailingly, is included in the analysis.17 For instance, a recent study investigating the association of PRS with the transition to psychosis in individuals at risk showed that transition to psychosis was associated with PRS only in those of European ancestry, whereas the predictive performance of PRS for non-Europeans was considerably low and nonsignificant.18 Emerging evidence also suggests that the genetic architecture of schizophrenia may be different in non-European populations.19
Although these limitations have been well known by the research community for many years, the first genomic study of schizophrenia in an African population was only published in 2020.20 The findings of this analysis, conducted by the Human Heredity and Health in Africa (H3Africa), support relevant insights about the underlying biological mechanisms associated with schizophrenia.20 As the majority of human evolution happened in Africa, the vast genetic diversity found in African populations provides a unique opportunity to understand the evolutionary underpinnings of schizophrenia.
Furthermore, genomic research in diverse settings, such as Latin America, may provide valuable cues to the etiology.21 Considering that the etiology of psychosis spectrum disorder involves genetics, environment, and their interaction, it is crucial to investigate how specific environmental exposures, such as high levels of poverty, unregulated urbanization, crime, violence, and limited access to healthcare assistance, which are over proportionately present in Latin America, interact with the genetic liability to schizophrenia.21,22
We undeniably need diverse populations to test whether the discovery of novel genetic variants and the genomic-based prediction models are applicable to the Majority World. It is encouraging to see that after a strong call to action, the Schizophrenia Working Group of the Psychiatric Genomics Consortium has at last made an active effort to increase diversity.
The Lack of Population Diversity in Socio-Environmental Research
To examine the population diversity in socio-environmental research of psychosis, we retrieved information from the most recent meta-analyses and umbrella reviews of risk and protective factors for psychosis spectrum disorder.23,24 The methods and the complete results are found in the supplementary material. Our analysis revealed that the majority of studies cited in the meta-analyses of the most relevant socio-environmental factors associated with psychosis were conducted in WEIRD societies. Although there was some empirical evidence from Asian (Japan and India) and South American (Surinam and Brazil) countries, a large proportion of the world population was not addressed. Most strikingly, not a single study was conducted in Africa or the Middle East region.
Consequently, the lack of diversity in socio-environmental research leaves an enormous knowledge gap that could further advance our understanding of psychosis. If and how these socio-environmental factors affect individuals in entirely different geographic locations, gene pools, social structures and norms, cultures, and potentially protective counter-factors remain unclear. Meanwhile, middle-class European and European American experiences are treated as the norm and used for theory-building.25
Psychosocial Stressors: Urbanicity, Migration, and Childhood Adversity
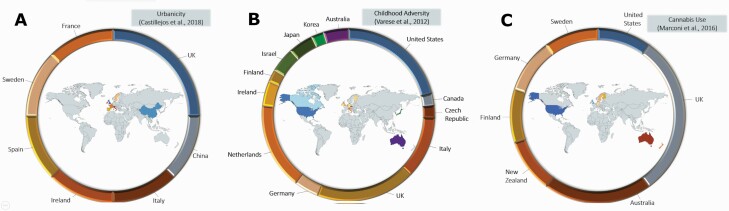
Living in urban areas was associated with higher stress levels and psychosis.26 However, the measurement and the definition of urbanicity vary between studies, resulting in the absence of a unified concept that is necessary to measure how spatial and social variations interact and pose a risk (figure 1A). The effect of urban living on mental well-being seems to be dependent on the social and structural conditions of the community per se. The contrasting impact of urban living on psychosis liability was apparent in the recent findings showing that urbanicity seemed to have an opposite effect in cities of the Netherlands and the United Kingdom vs those in Italy, Spain, and France.27 Although the source of these contrasting findings is yet to be found, it is difficult to argue that urbanicity is a universal risk factor for psychosis across Europe, let alone the world.
Fig. 1.
Population diversity of studies investigating the association of schizophrenia spectrum disorder with urbanicity (A), childhood adversity (B), and cannabis use (C).
A recent study investigating the association between urbanicity and psychosis in low- and middle-income countries (LMIC) reported similarly varying findings across countries.28 A positive association between urban living and psychotic experiences was present in Laos, Mexico, Estonia, and Morocco, whereas a negative association was identified in Nepal, Vietnam, Hungary, and South Africa.28 Pooled results showed no evidence for an association between urbanicity and psychosis in LMIC. Potential mechanisms have been speculated to be the patterns of cannabis use, lack of urban-rural disparities, and social isolation, as affluent and less affluent individuals tend to populate in the same areas of cities of LMIC.29 Moreover, social and familial cohesion seems to be stronger in some countries, thereby potentially buffering psychosis development.30
Both migration and immigrant status have been considered risk factors for psychosis, but most studies have focused on external migration solely. Migration is strongly associated with social defeat, discrimination, and isolation that are related to psychosis liability. However, no association between internal migration and psychosis was found in Brazil.31 Possible explanations might be lower social adversity levels and higher ethnic density that buffer the social risk factors implicated in external migration.32 Furthermore, the increased psychosis risk among migrants was not generalizable to all settings, such as people of Turkish descent in the Netherlands, Indian origin in the United Kingdom, European descent minority in South Africa, and Latin Americans in the United States.33 These findings converge on the hypothesis that it might be the size and quality of an individual’s social network that moderates the risk of psychosis,34 and urbanicity and immigration are more distant proxy measures.35 Testing this hypothesis will however require studies across different countries with uniquely different social network structures.
Another stressor associated with psychosis is childhood adversity, which is experienced by children worldwide, regardless of ethnicity, country of origin, and social status. In comparison with other socio-environmental factors associated with psychosis, childhood adversities have been studied more extensively across different nations, which are nonetheless mainly restricted to the North American and European regions (figure 1B),36 and thereby disregarding differences in cultures and social systems that evoke both risk and protective factors such as resilience.37
Physiological Stressors: Cannabis and Tobacco Smoking, and Season of Birth
Although converging evidence from observational and experimental studies suggests cannabis use may be a causal factor for psychosis,38 the study populations were mainly limited to men from WEIRD populations (figure 1C).39,40 In Asian countries, lower cannabis use rates may be motivated by stricter legislation and cultural norms.41 Furthermore, the varying degrees of access to high-potency cannabis may contribute to the variation in the incidence of psychotic disorders across different countries.42 The association between tobacco smoking and psychosis has only been demonstrated in a few European countries and Israel, where smoking rates have declined sharply in the 21st century.43
The risk of winter- and spring-birth on psychosis is proposed to be due to mothers being more exposed to viruses and infections during pregnancy.44 Although most studies conducted in the Northern Hemisphere reported consistent findings,45 a few studies from the Southern Hemisphere yielded somewhat conflicting results. For instance, an association between psychosis and the season of birth (May-July) was demonstrated in Northeast Brazil,45 whereas this association was not replicated in Singapore, which is one degree above the equator line and with minimal temperature variation like Brazil.46 In this regard, it is speculated that the higher rainfall variations in Brazil may be the underlying factor for the seasonality of schizophrenia births, as the rainfall season is associated with respiratory viruses and influenza. Although the underlying processes seem similar, an attribution of risk to winter births can be misleading, as the causal mechanism might not necessarily be related to the season but rather to the frequency of viral infections.44
The Game Plan: Embrace the Complexity, Increase the Diversity
In addition to the lack of diversity, how socio-environmental factors are assessed and studied has been a major shortcoming, as studies investigate the impact of a single exposure on a single outcome.35,47 This approach, however, does not reflect the complex network of various exposures, a multitude of genetic variations underlying a web of correlated behavioral phenotypes, including psychosis, and their interaction.48–50 This dense network of exposures is called the “exposome,” which is the entirety of exposures for an individual from conception to death. The exposome framework enables the evaluation of varying exposure rates across populations and their interdependence, which could explain how variations in socio-environmental factors across different social and geographical settings could contribute to divergent paths to psychosis development.35 For instance, the inconsistency in findings related to urbanicity may be explained by the population-level differences of the components of urbanicity, such as ethnic density, substance use, and pollution.
Taken together, there is a pressing need to achieve “racial”, ethnic, and sociocultural diversity at all levels of psychosis research. For instance, three-fourths of the original research articles published in the Schizophrenia Bulletin in 2020 investigated samples of WEIRD populations (supplementary table S1). Future research should aim to diversify samples and enable studies conducted in diverse social and geographical settings to increase our understanding of the pathoetiology of psychosis. Furthermore, these studies should be inclusive of individuals who do not identify with current schemes of “categorizations,” such as multiethnic, multiracial, and gender nonconforming. Researchers should campaign for diversity individually and collectively as professional organization affiliates (eg, Schizophrenia International Research Society) and lobby for financing diversity through funding agencies. Instead of the colonial approach to research, which unfortunately still exists to date,51 true partnerships between WEIRD societies and the Majority World should be established. To overthrow the legacies of colonialism, these collaborative initiatives should always involve local scientists with equal say on the project design—not just a means to an end. The research teams must be diverse and appropriate to the setting in which research is conducted to ensure that the social, historical, and cultural contexts are acknowledged. These partnerships should aim for building research capacities, such as training staff and making knowledge transfer possible to sustain long-term benefits and greater diversity in psychosis research. Although we are a long way from achieving diversity in psychosis research, it is encouraging to see the development of global mental health research collaborations such as the INTREPID II that aims to study psychosis in India, Nigeria, and Trinidad.52 Another example is NeuroGAP-Psychosis, an initiative by Broad Institute to expand GWAS of psychosis to African countries.53 Although funding agencies such as Wellcome Trust and the NIH Fogarty program include funding opportunities for scientists in the Majority World, these represent a fraction of the total schizophrenia research funding. The NIH’s new UNITE initiative “established to identify and address structural racism within the NIH-supported and the greater scientific community” is a step in the right direction. The burden thus lies with funding agencies to foster replicable research across diverse populations and help the field move away from “WEIRD”ness.
Conclusion
Psychosis research at all levels is still lagging behind when it comes to the diversity of study populations, research settings, and funding priorities. Although the main goals of mental health research are to understand human behavior, identify underpinnings of mental health problems, and find remedies for suffering, these goals are currently achieved in an inequitable manner. Accordingly, we as the scientific community are not only disregarding relevant human and contextual variations that would provide novel insights into psychosis spectrum disorder but also perpetuating already existing health care disparities by constantly prioritizing certain populations in our studies, and consequently, our theories, interventions, and treatments. The time has come to make diversity in psychosis research more than a buzzword.
Funding
Dr S.G. is supported by the Ophelia research project, The Netherlands Organization for Health Research and Development (ZonMw) grant number (636340001). Dr R.R. is supported by grants from the National Institute of Mental Health (NIMH) and the National Center for Complementary and Integrative Health (NCCIH). Dr R.B. is supported by the National Institute of Mental Health (NIMH) grant (K23MH120437).
Supplementary Material
Acknowledgments
Dr R.B. serves on the scientific board and reports stock ownership in “Taliaz Health,” with no conflict of interest relevant to this work. All other authors have no conflicts of interest to disclose.
References
- 1. Rad MS, Martingano AJ, Ginges J. Toward a psychology of Homo sapiens: making psychological science more representative of the human population. Proc Natl Acad Sci USA. 2018;115(45):11401–11405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bustamante CD, Burchard EG, De la Vega FM. Genomics for the world. Nature. 2011;475(7355):163–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Popejoy AB, Fullerton SM. Genomics is failing on diversity. Nature. 2016;538(7624):161–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosmarin DH. Diversity science: new dawn in a golden age. Clin Psychol Sci. 2016;4(4):701–703. [Google Scholar]
- 7. Mendoza DB, Williams MT, Chapman LK, Powers M. Minority inclusion in randomized clinical trials of panic disorder. J Anxiety Disord. 2012;26(5):574–582. [DOI] [PubMed] [Google Scholar]
- 8. Addington J, Liu L, Buchy L, et al. . North American Prodrome Longitudinal Study (NAPLS 2): the prodromal symptoms. J Nerv Ment Dis. 2015;203(5):328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kane JM, Robinson DG, Schooler NR, et al. . Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry. 2016;173(4):362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rosenheck RA, Krystal JH, Lew R, et al. ; CSP555 Research Group . Long-acting risperidone and oral antipsychotics in unstable schizophrenia. N Engl J Med. 2011;364(9):842–851. [DOI] [PubMed] [Google Scholar]
- 11. Bennett D, Rosenheck R. Socioeconomic status and the effectiveness of treatment for first-episode psychosis [published online ahead of print November 24, 2020]. Health Serv Res. doi: 10.1111/1475-6773.13606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heun-Johnson H, Menchine M, Axeen S, et al. . Association between race/ethnicity and disparities in health care use before first-episode psychosis among privately insured young patients. JAMA Psychiatry. 2021;78(3):311–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. [DOI] [PubMed] [Google Scholar]
- 14. Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21(3):879–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lim C, Hernandez M, Gaona L, Barrio C. Recruitment of Asian Americans with schizophrenia spectrum disorder for research participation: barriers, strategies, and outcomes. Community Ment Health J. 2021;57(3):490–501. [DOI] [PubMed] [Google Scholar]
- 16. Need AC, Goldstein DB. Next generation disparities in human genomics: concerns and remedies. Trends Genet. 2009;25(11):489–494. [DOI] [PubMed] [Google Scholar]
- 17. Popejoy AB. Diversity in precision medicine and pharmacogenetics: methodological and conceptual considerations for broadening participation. Pharmgenomics Pers Med. 2019;12:257–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perkins DO, Olde Loohuis L, Barbee J, et al. . Polygenic risk score contribution to psychosis prediction in a target population of persons at clinical high risk. Am J Psychiatry. 2020;177(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Periyasamy S, John S, Padmavati R, et al. . Association of schizophrenia risk with disordered niacin metabolism in an Indian genome-wide association study. JAMA Psychiatry. 2019;76(10):1026–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gulsuner S, Stein DJ, Susser ES, et al. . Genetics of schizophrenia in the South African Xhosa. Science. 2020;367(6477):569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fonseca L, Sena BF, Crossley N, et al. . Diversity matters: opportunities in the study of the genetics of psychotic disorders in low- and middle-income countries in Latin America [published online ahead of print November 23, 2020]. Braz J Psychiatry. doi: 10.1590/1516-4446-2020-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–950. [DOI] [PubMed] [Google Scholar]
- 23. Belbasis L, Köhler CA, Stefanis N, et al. . Risk factors and peripheral biomarkers for schizophrenia spectrum disorders: an umbrella review of meta-analyses. Acta Psychiatr Scand. 2018;137(2):88–97. [DOI] [PubMed] [Google Scholar]
- 24. Radua J, Ramella-Cravaro V, Ioannidis JPA, et al. . What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. 2018;17(1):49–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Medin D, Bennis W, Chandler M. Culture and the home-field disadvantage. Perspect Psychol Sci. 2010;5(6):708–713. [DOI] [PubMed] [Google Scholar]
- 26. Castillejos M, Martín-Pérez C, Moreno-Küstner B. A systematic review and meta-analysis of the incidence of psychotic disorders: the distribution of rates and the influence of gender, urbanicity, immigration and socio-economic level. Psychol Med. 2018;48(13):2101–2115. [DOI] [PubMed] [Google Scholar]
- 27. Jongsma HE, Gayer-Anderson C, Lasalvia A, et al. ; European Network of National Schizophrenia Networks Studying Gene-Environment Interactions Work Package 2 (EU-GEI WP2) Group . Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry. 2018;75(1):36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. DeVylder JE, Kelleher I, Lalane M, Oh H, Link BG, Koyanagi A. Association of urbanicity with psychosis in low- and middle-income countries. JAMA Psychiatry. 2018;75(7):678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Padhy SK, Sarkar S, Davuluri T, Patra BN. Urban living and psychosis – an overview. Asian J Psychiatr. 2014;12:17–22. [DOI] [PubMed] [Google Scholar]
- 30. Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry. 2010;52(2):113–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shuhama R, Carmo LSRD, Busatto Filho G, et al. . From where we came: absence of internal migration effect on psychosis in two case-control Brazilian samples. Schizophr Res. 2019;212:241–242. [DOI] [PubMed] [Google Scholar]
- 32. Oh H, Abe J, Negi N, DeVylder J. Immigration and psychotic experiences in the United States: another example of the epidemiological paradox? Psychiatry Res. 2015;229(3):784–790. [DOI] [PubMed] [Google Scholar]
- 33. Kirkbride JB. Migration and psychosis: our smoking lung? World Psychiatry. 2017;16(2):119–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Degnan A, Berry K, Sweet D, Abel K, Crossley N, Edge D. Social networks and symptomatic and functional outcomes in schizophrenia: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):873–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guloksuz S, Rutten BPF, Pries LK, et al. ; European Network of National Schizophrenia Networks Studying Gene-Environment Interactions Work Package 6 (EU-GEI WP6) Group . The complexities of evaluating the exposome in psychiatry: a data-driven illustration of challenges and some propositions for amendments. Schizophr Bull. 2018;44(6):1175–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Varese F, Smeets F, Drukker M, et al. . Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Noltemeyer AL, Bush KR. Adversity and resilience: a synthesis of international research. Sch Psychol Int. 2013;34(5):474–487. [Google Scholar]
- 38. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot – a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hamilton I, Monaghan M. Cannabis and psychosis: are we any closer to understanding the relationship? Curr Psychiatry Rep. 2019;21(7):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lee TY, Kwon JS. Psychosis research in Asia: advantage from low prevalence of cannabis use. NPJ Schizophr. 2016;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Di Forti M, Quattrone D, Freeman TP, et al. ; EU-GEI WP2 Group . The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. Lancet Psychiatry. 2019;6(5):427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hunter A, Murray R, Asher L, Leonardi-Bee J. The effects of tobacco smoking, and prenatal tobacco smoke exposure, on risk of schizophrenia: a systematic review and meta-analysis. Nicotine Tob Res. 2020;22(1):3–10. [DOI] [PubMed] [Google Scholar]
- 44. Ferreira FR, de Paula GC, de Carvalho RJV, Ribeiro-Barbosa ER, Spini VBMG. Impact of season of birth on psychiatric disorder susceptibility and drug abuse incidence in a population from the Köppen tropical savanna region of Brazil. Neuropsychobiology. 2020;79(2):131–140. [DOI] [PubMed] [Google Scholar]
- 45. Messias E, Mourao C, Maia J, et al. . Season of birth and schizophrenia in Northeast Brazil: relationship to rainfall. J Nerv Ment Dis. 2006;194(11):870–873. [DOI] [PubMed] [Google Scholar]
- 46. Parker G, Mahendran R, Koh ES, Machin D. Season of birth in schizophrenia: no latitude at the equator. Br J Psychiatry. 2000;176:68–71. [DOI] [PubMed] [Google Scholar]
- 47. Guloksuz S, van Os J, Rutten BPF. The exposome paradigm and the complexities of environmental research in psychiatry. JAMA Psychiatry. 2018;75(10):985–986. [DOI] [PubMed] [Google Scholar]
- 48. Guloksuz S, Pries LK, Delespaul P, et al. ; Genetic Risk and Outcome of Psychosis (GROUP) Investigators . Examining the independent and joint effects of molecular genetic liability and environmental exposures in schizophrenia: results from the EUGEI study. World Psychiatry. 2019;18(2):173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pries LK, Lage-Castellanos A, Delespaul P, et al. ; Genetic Risk and Outcome of Psychosis (GROUP) Investigators . Estimating exposome score for schizophrenia using predictive modeling approach in two independent samples: the results from the EUGEI study. Schizophr Bull. 2019;45(5):960–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Pries LK, van Os J, Ten Have M, et al. . Association of recent stressful life events with mental and physical health in the context of genomic and exposomic liability for schizophrenia. JAMA Psychiatry. 2020;77(12):1296–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Boshoff N. Neo-colonialism and research collaboration in Central Africa. Scientometrics. 2009;81(2):413–434. [Google Scholar]
- 52. Roberts T, Gureje O, Thara R, et al. . INTREPID II: protocol for a multistudy programme of research on untreated psychosis in India, Nigeria and Trinidad. BMJ Open. 2020;10(6):e039004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Stevenson A, Akena D, Stroud RE, et al. . Neuropsychiatric Genetics of African Populations-Psychosis (NeuroGAP-Psychosis): a case-control study protocol and GWAS in Ethiopia, Kenya, South Africa and Uganda. BMJ Open. 2019;9(2):e025469. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.