Abstract
Despite the accepted link between childhood abuse and positive psychotic symptoms, findings between other adversities, such as neglect, and the remaining dimensions in people with psychosis have been inconsistent, with evidence not yet reviewed quantitatively. The aim of this study was to systematically examine quantitatively the association between broadly defined childhood adversity (CA), abuse (sexual/physical/emotional), and neglect (physical/emotional) subtypes, with positive, negative, depressive, manic, and disorganized dimensions in those with psychosis. A search was conducted across EMBASE, MEDLINE, PsychINFO, and Cochrane Libraries using search terms related to psychosis population, CA, and psychopathological dimensions. After reviewing for relevance, data were extracted, synthesized, and meta-analyzed. Forty-seven papers were identified, including 7379 cases across 40 studies examining positive, 37 negative, 20 depressive, 9 disorganized, and 13 manic dimensions. After adjustment for publication bias, general adversity was positively associated with all dimensions (ranging from r = 0.08 to r = 0.24). Most forms of abuse were associated with depressive (ranging from r = 0.16 to r = 0.32), positive (ranging from r = 0.14 to r = 0.16), manic (r = 0.13), and negative dimensions (ranging from r = 0.05 to r = 0.09), while neglect was only associated with negative (r = 0.13) and depressive dimensions (ranging from r = 0.16 to r = 0.20). When heterogeneity was found, it tended to be explained by one specific study. The depressive dimension was influenced by percentage of women (ranging from r = 0.83 to r = 1.36) and poor-quality scores (ranging from r = −0.21 and r = −0.059). Quality was judged as fair overall. Broadly defined adversity and forms of abuse increase transdimensional severity. Being exposed to neglect during childhood seems to be exclusively related to negative and depressive dimensions suggesting specific effects.
Keywords: childhood trauma/psychosis/dimensions/meta-analysis
Introduction
Exposure to adversities, such as abuse and neglect, during childhood and adolescence is associated with psychotic disorders.1 Abundant research has shown that individuals with a psychotic disorder who are exposed to such experiences have a higher severity of hallucinations and delusions,2,3 as well as other clinical outcomes, such as depressive, manic, and disorganized symptoms.4,5 Understanding the nature of the association between such environmental risk factors and each of the psychopathological domains is important in subsequently understanding potential causative mediating mechanisms. This may help to detect individuals at risk of poorer psychopathological profile and enable specific interventions to be tailored accordingly.6
Childhood adversity (CA) is a construct that, in the field of psychosis, usually refers to being exposed to potentially traumatic events, such as abuse (sexual, physical, and emotional), neglect (physical and emotional), bullying or early separation,5 usually before age 16 or 18. It can be measured by using a cumulative score, which adds the number of different exposures, or individually by examining specific adversities in isolation. Evidence suggests that CA, broadly defined by a total cumulative score, may be transsymptomatic and leads to an admixture of constellations of symptom domains rather than in isolation.7,8 On the other hand, there is evidence on some specific links between adversities and symptoms.2,5,9 Regarding negative symptoms of psychosis, the evidence is less clear, with multiple inconsistent reports using general measures of CA,10–12 and some meta-analytic evidence (including 9 studies concerning abuse and 8 with neglect) suggesting a specific link with neglect only.2 Our understanding of the link between adversity, broadly defined or by specific subtypes, and the remaining fundamental psychopathological domains, such as manic, depressive, and disorganized dimensions, is less clear, with sparser evidence and no consensus so far.
Current literature on the specific effects between CA and individual symptoms is mainly limited to the effects on auditory perceptions or delusional ideas.3,5 However, studying single symptoms in isolation is far from being representative of real-life clinical settings as symptoms rarely occur in isolation and often co-occur and cluster. Thus, examining the psychopathological dimensions (the positive, negative, disorganized, depressive, and manic/excited) rather than single symptoms may be more representative to the clinical reality.13,14
To the best of our knowledge, only one meta-analysis has explored the links between abuse and neglect with the positive and negative dimensions in psychotic populations.2 This high-quality piece of work found that, whilst abuse may affect instinctively both dimensions, supporting the presence of general effects, neglect was only associated with the negative symptoms, supporting some evidence of specific effects.2 However, Bailey et al’s2 literature search in this study did not include the term “dimensions,” which may have led to missing relevant papers. Second, the authors did not explore depressive, disorganized, and manic/excited symptom dimensions. Third, their search was until December 2014, thus excluding the abundance of research that has been conducted since. Lastly, they did not take into account the potential bias led by different instruments used.
Based on these elements, we planned to replicate and update their findings and, extending their work, also cover the disorganized, depressive, and manic/exited dimensions in people with a psychotic disorder and thus provide a more comprehensive synthesis of the different adversities and psychotic dimensions.
Methods
The study protocol was registered on PROSPERO (CRD42019129193) and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses15 guidelines and Moose16 (see supplementary tables S1 and S2).
Search Strategy and Selection Criteria
The main electronic search was conducted on MEDLINE, EMBASE, and PsycINFO, through Ovid provider, and on Cochrane Libraries, up to May 2019. We searched Medical Subject Headings and keywords related to: (1) psychosis; (2) childhood adversity; and (3) clinical dimensions using the Boolean operator “AND” (full list of search terms provided in the supplementary material—Search Terms). Titles and abstracts, and subsequently selected eligible full texts of articles were screened independently by 2 reviewers (L.A. and M.T.) with 85% agreement. Titles and abstract discrepancies were resolved through discussion at a project group meeting, while full-text discrepancies were screened by a third independent reviewer (M.R.V.). A cross-reference search extracted titles/abstracts from identified reviews, and a full-text check of potentially eligible studies from these reviews was performed by one author (A.C.) and checked in duplicate by another author (L.A.). When data extraction was conducted and new potentially eligible studies were detected from included studies, these were also considered for inclusion.
Inclusion Criteria
Included studies were those that (1) examine the relationship between CA and psychopathological dimensions in individuals with psychosis; (2) were performed in humans; (3) included only psychotic patients with the following diagnoses: schizophrenia, schizophreniform/brief psychotic episode, bipolar disorder with psychotic features, schizoaffective disorder, major depression with psychotic features, and psychosis not otherwise specified; (4) defined diagnoses according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-III, DSM-III-R, DSM-IV, and DSM-IV-TR17), Research Diagnostic Criteria, or International Classification of Diseases, 9th or 10th Revision (ICD-9 or ICD-10, respectively18; see supplementary table S3 for full list with respective codes); (5) includes CA occurring before age 18 and involving exposure to CA measured as follows: by a (a) general measure of adversity (GA) broadly defined by a composite measure that includes either cumulative scores of different traumas, or use a binary measure that select patients having been exposed to any of the subtypes; (b) SA, (c) physical abuse (PA), (d) emotional abuse (EA), (e) physical neglect (PN), and (f) emotional neglect (EN), (g) bullying, and (h) household discord or equivalent experiences; (6) examine the positive, negative, disorganized, depressive, and manic/excited symptom dimensions13,14 and are measured using a well-validated instrument (see supplementary table S4 for full list of included instruments); and (7) studies with sufficient information to determine the presence of a statistically positive, negative, or nonsignificant association between any form of CA and each of the dimensions.
Exclusion Criteria
(1) Not being published in the English language; (2) included more than 20% of participants aged 65 years or over in accord with other studies6,19; (3) being performed in samples of specific populations, such as pregnant women or samples from forensic settings (to avoid potential confounding by other variables, such as hormonal changes or antisocial traits); (4) being published before 1979 according to others1 and because the first known empirical study on CA and psychosis was published around that time20 and the DSM-III21 was released in 1980, improving diagnostic consistency.
Quality Assessment and Data Extraction Procedures
Quality assessment was carried out using the Newcastle–Ottawa Scale22 (NOS) for cohort studies by 2 independent reviewers (Y.S. and A.C.). Details on the instrument items and quality assessment procedures can be found in the supplementary material (“quality assessment procedures”).
We extracted all the relevant data of each included study, providing full details on each included paper in supplementary table S5. In order to allow comparisons with the previous meta-analysis in the field,2 we extracted information on correlation coefficients and 95% confidence intervals (CIs), when possible. When associations were provided in other formats (mean differences, standardized β coefficients, or unstandardized regression coefficients), data were transformed using previously proposed procedures.23,24 To combine Person and Spearman’s correlations, Comprehensive Meta-Analysis version v.3 (CMA25) transforms them to Fisher’s Z, and then transforms those values back to correlations and uses the transformed values for the analyses.
As a predominance of the analyses were conducted using correlations and were not adjusted, unadjusted results were extracted. In order to account for the possible influence of confounders, the following meta-regressions were carried out: (1) age (mean age), (2) sex (percentage of females), (3) quality of the studies included (based on the NOS scores), and (4) variability in instruments used (based on whether they used Positive and Negative Syndrome Scale [PANSS] and Childhood Trauma Questionnaire [CTQ] or not; see details in Data Analysis). The choice of these instruments is because they are the most commonly used in this set of literature, ensuring some methodological homogeneity. When results were given separately between men and women, effects were pooled into one single category. When different time points were reported, we included only measures at baseline to permit comparison between all the studies, but results on prospective analyses were also reported in the detailed tables (supplementary table S5).
Data Analysis
We performed a set of meta-analyses, when data were available, for 6 types of CA in each of the 5 dimensions of interests. The CA categories were (1) GA, (2) SA, (3) PA, (4) EA, (5) PN, (6) EN, (7) bullying, and (8) household discord and, for each of the dimensions, meta-analyses were conducted when a minimum of 3 studies was available. Papers that used a general composite category of abuse or neglect (by aggregating each subtype) could not be included in the quantitative analyses per specific adversities, but results were extracted and presented in supplementary table S5.
The meta-analysis was conducted using CMA.25 Random effects models approach was used since we assume differences in measures, clinical features, and demographics between studies. To assess between-study heterogeneity, we looked at the I2 index and conducted the Q test. Serious heterogeneity was considered when I2 > 50% and Q-test P-value was <.05 according to others.26 In line with the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria, we explored the potential bias related to heterogeneity found in our analyses by exploring the forest plots and researching the presence of potential outliers that could explain the heterogeneity (eg, one individual study going in a different direction to all the others according to others26).
To assess publication bias, we looked for asymmetry in the funnel plots and conducted the Egger’s test27 (P < .05 might indicate potential publication bias). Whenever the latter was significant, we employed Duval and Tweedie’s trim-and-fill method.28 This not only assessed the statistical likelihood of publication bias but also provides the adjusted summary effect. When Egger’s test was significant, and inspection of the funnel plots suggested potential small-effect bias, the trim-and-fill method was carried. Analyses did not “survive” publication bias adjustment if the 95% CI crossed 0 following the trim-and-fill procedure according to others.26 For those analyses with at least 6 studies per analysis, we conducted meta-regressions by the risk of bias scores, age, and gender and variability in instruments used (whether or not they used the CTQ and PANSS as instruments, which allowed us to estimate potential biases related to studies that used other instruments) and quality assessment scores based on the NOS. To further account for the potential biases due to the heterogeneity of measures measuring CA and symptoms (considering that CTQ and PANSS are the most commonly used), we also conducted sensitivity analyses stratifying analyses based on whether they used CTQ/PANSS or not, considering that other instruments may have led to important heterogeneity. Statistical significance was set at P < .05 (2-tailed). Interpretation of correlation coefficients was based on predefined cutoffs as follows: values between 0 and 0.3 indicate a weak positive effect: between 0.3 and 0.7, a moderate positive effect and, above 0.7, a strong positive effect.29
Results
Database
Overall, 6845 records were identified, 294 full texts were screened and 47 articles were eligible for inclusion (supplementary figure 1). The 47 included articles were published between 1979 and May 2019 (see supplementary table S5).
Study sample sizes ranged from 20 to 1119; the mean age of the entire sample was 30.7 and the proportion of women was 35.31% overall. These studies included both cross-sectional and prospective investigations. However, only 11 studies used the latter, with follow-up periods ranging from 1 week to 5 years; thus, we could not meta-analyze prospective data given the very small number of papers in each subanalysis category. All the studies measured CA retrospectively. Studies were conducted predominantly in Europe (23), Australia (7) the United States, and Canada (8), followed by Turkey (4), Eastern Asia (3), Iran (1), and India (1).
Measures of CA
Details of the instruments used are detailed in supplementary table S5. Overall, GA was the most examined measure among studies, being utilized in 82.9% (n = 39) of the studies included, while 47% (n = 22) examined SA, 38.3% (n = 18) PA, 34% (n = 16) EA, 27.6% (13) PN, and 31.9% (15) EN. The CTQ30 is the most used composite instrument (46.8%; n = 22 studies). GA was measured based on a cumulative measure of different adversities; however, a small proportion used a binary measure based on predefined thresholds (3/18 of those using CTQ). None of the studies examined the association between bullying or household discord and symptom dimensions; so, no meta-analyses could be conducted for those adversities.
Measures Used for the Outcomes (Psychopathological Dimensions)
Details on the instruments used as well as items included in each outcome dimension are detailed in supplementary table S6. PANSS31 was the most utilized measure of symptom severity amongst all dimensions. High heterogeneity of measures was found for the depressive domain, which used 10 instruments as compared to 5 for the positive and negative, 2 for the disorganized, and 4 for the manic. Considerable overlap of symptoms assessed was found within the clinical domains across instruments. Details can be found in the supplementary material table S6.
Meta-Analytic Results
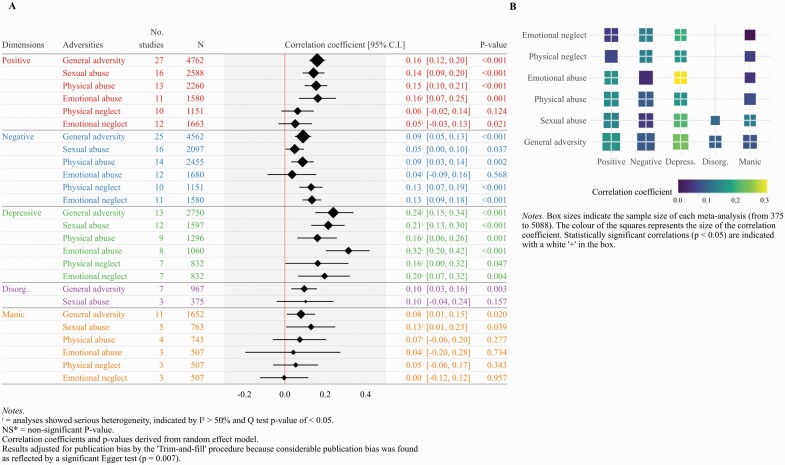
Results on the direction and magnitude of the meta-analytic evidence are reported in table 1 and illustrated in figure 1A and 1B. Forest plots of each analysis can be found in supplementary figures 2–27. As a whole, effect sizes found in this review were generally weak for all dimensions (0–0.3) or moderate at best for some of the analyses in the depressive domain (0.3–0.7). GA was positively associated with all dimensions. All abuse categories were positively associated with the depressive and positive dimensions. PA and SA, but not EA, were positively associated with the negative dimension, while only SA was associated with mania. PN and EN were positively associated with the negative and depressive dimensions and not with the others.
Table 1.
Association between adversities and symptoms dimensions, heterogeneity and publication bias
| Studies | Sample size | Samples | Correlation coefficient | Heterogeneity | Publication bias | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Values | 95% CI | P | I 2 | P | Funnel Plot Asymmetry |
Trim & Fill imputed studies |
Trim & Fill Adjusted R coeff (95% CI) | Egger’s P |
||||
| General adversity POSITIVE |
27 | 4762 | 27 | 0.16 | 0.12; 0.20 | .000 | 39.14 | .021 | No | 0 | NA | .726 |
| Sexual abuse POSITIVE |
16 | 2588 | 16 | 0.14 | 0.08; 0.19 | .000 | 41.98 | .035 | Possible left | 2 | 0.12 (0.05; 0.18) | .224 |
| Physical abuse POSITIVE |
13 | 2260 | 13 | 0.15 | 0.09; 0.21 | .000 | 40.54 | .064 | Yes left | 2 | 0.13 (0.07; 0.19) | .21 |
| Emotional abuse POSITIVE |
11 | 1580 | 11 | 0.16 | 0.07; 0.25 | .001 | 69.93 | .000 | No | 0 | NA | .021 |
| Physical neglect POSITIVE |
10 | 1151 | 10 | 0.06 | –0.01; 0.14 | .124 | 44.00 | .065 | No | 0 | NA | .216 |
| Emotional neglect POSITIVEa |
12 | 1663 | 12 | 0.10 | 0.01; 0.18 | .021 | 66.47 | .001 | Yes left | 3 | 0.05 (–0.03; 0.13) | .007 |
| General Adversity NEGATIVE |
25 | 4562 | 25 | 0.09 | 0.05; 0.13 | .000 | 34.32 | .049 | No | 0 | NA | .460 |
| Sexual abuse NEGATIVE |
16 | 2097 | 16 | 0.04 | 0.00; 0.09 | .037 | 24.96 | .172 | No | 0 | NA | .111 |
| Physical abuse NEGATIVE |
14 | 2455 | 14 | 0.08 | 0.03; 0.14 | .002 | 43.55 | .041 | No | 0 | NA | .137 |
| Emotional abuse NEGATIVE |
12 | 1680 | 12 | 0.03 | –0.08; 0.15 | .568 | 83.91 | .000 | No | 0 | NA | .744 |
| Physical neglect NEGATIVE |
10 | 1151 | 10 | 0.13 | 0.07; 0.18 | .000 | 0 | .78 | Yes left | 2 | 0.11 (0.05; 0.16) | .545 |
| Emotional neglect NEGATIVE |
11 | 1580 | 11 | 0.13 | 0.08; 0.18 | .000 | 0 | .972 | No | 0 | NA | .694 |
| General Adversity DEPRESSION |
13 | 2750 | 13 | 0.24 | 0.15; 0.34 | .000 | 81.62 | .000 | Yes left | 5 | 0.12 (0.01; 0.23) | .150 |
| Sexual abuse DEPRESSION |
12 | 1597 | 12 | 0.21 | 0.13; 0.29 | .000 | 63.66 | .001 | Yes left | 2 | 0.17 (0.07; 0.26) | .398 |
| Physical abuse DEPRESSION |
9 | 1296 | 9 | 0.16 | 0.06; 0.25 | .001 | 63.35 | .001 | No | 0 | NA | .050 |
| Emotional abuse DEPRESSION |
8 | 1060 | 8 | 0.31 | 0.20; 0.41 | .000 | 73.33 | .000 | Yes left | 3 | 0.23 (0.11; 0.34) | .316 |
| Physical neglect DEPRESSION |
7 | 832 | 7 | 0.16 | 0.00; 0.31 | .047 | 81.24 | .000 | Yes left | 2 | 0.08 (–0.08; 0.23) | .100 |
| Emotional neglect DEPRESSION |
7 | 832 | 7 | 0.19 | 0.06; 0.32 | .004 | 72.67 | .001 | Yes left | 3 | 0.08 (–0.06; 0.22) | .068 |
| General Adversity MANIA |
11 | 652 | 11 | 0.08 | 0.01–0.15 |
.020 |
44.25 | .056 |
Possible left | 2 | 0.06 (–0.00; 0.13) | .217 |
| Sexual abuse MANIA |
5 | 763 | 5 | 0.13 | 0.00; 0.24 | .039 | 60.60 | .038 | Possible left | 1 | 0.11 (–0.00; 0.23) | .228 |
| Physical abuse MANIA |
4 | 743 | 4 | 0.07 | –0.05–0.20 | .277 | 69.10 |
.021 | Possible left | 1 | 0.03 (–0.08; 0.16) | .620 |
| Emotional abuse MANIA |
3 | 507 | 3 | 0.04 | –0.19; 0.27 | .734 | 85.80 | .001 | No | NA | NA | .296 |
| Physical neglect MANIA |
3 | 507 | 3 | 0.05 | –0.05; 0.16 | .343 | 35.60 | .211 | No | NA | NA | .888 |
| Emotional neglect MANIA |
3 | 507 | 3 | –0.00 | –0.12; 0.11 | .957 | 43.70 | .169 | No | NA | NA | .007 |
| General adversity DISORGANIZATION |
7 | 967 | 7 | 0.09 | 0.03; 0.15 | .003 | 0 | .679 | No | NA | NA | .845 |
| Sexual abuse DISORGANIZATION |
3 | 375 | 3 | 0.10 | –0.04; 0.24 | .157 | 38.52 | .197 | No | NA | NA | .428 |
afor emotional neglect in the positive dimension analysis, substantial publication bias was found (with an Egger test = 0.007) and thus results after adjustment for Duval and Tweedie's trim-and-fill were considered for interpretation and for Figure 1.
Fig. 1.
(A) Summary of the meta-analyses conducted by type of adversity in each of the clinical dimensions. (B) Graphic representation summarizing the direction of the evidence, the magnitude, and the presence of significant associations among the 26 meta-analyses conducted.
Positive Dimension
Forty studies were included concerning this dimension, including 6500 subjects. Data on 2 studies could not be included in analyses because of incompatibility,32,33 (see supplementary table S7). Positive associations, with correlation coefficients between 0.142 and 0.163, indicating weak effect, were found for analyses with general measure of CA (27 studies; r = 0.16, 95% CI = [0.12, 0.20], P < .001), SA (16 studies; r = 0.14, 95% CI = [0.08, 0.19], P < .001), PA (13 studies; r = 0.15, 95% CI = [0.09, 0.21], P < .001), and EA (11 studies; r = 0.16, 95% CI = [0.07, 0.25], P = .001). Smaller correlation coefficients were found for PN and EN at 0.06 and 0.050 respectively, whose CI crossed 0 (the latter corresponds to the coefficient after adjustment for Duval and Tweedie’s trim-and-fill method given the presence of substantial publication bias with an Egger test = 0.007).
Negative Dimension
Thirty-seven studies were included concerning this dimension, including 6053 subjects. Data on 4 studies could not be meta-analyzed because of incompatible data format32,34–36supplementary table S7. Positive associations with weak effects were found for analyses with GA (25 studies; r = 0.09, 95% CI = [0.05, 0.13], P < .001), SA (16 studies; r = 0.04, 95% CI = [0.00, 0.09], P = .037), and PA (14 studies; r = 0.08, 95% CI = [0.03, 0.14], P = .002), while no association was found for EA whose CI crossed 0 (12 studies; r = 0.03, 95% CI = [−0.08, 0.15], P = .0568. However, and contrary to the finding concerning positive dimension, positive significant associations with greater (but still weak) effects were found for PN (10 studies; r = 0.13, 95% CI = [0.07, 0.18], P < .001) and EN (11 studies; r = 0.13, 95% CI = [0.08, 0.18], P < .001).
Depressive Dimension
Data on the 20 studies including this dimension could be meta-analyzed, including 3753 subjects. One study could not be included in analyses by subtype because of incompatible data32 (supplementary table S7). Meta-analyses revealed that all categories were positively associated with the depressive dimensions with weak and moderate effects ranging from 0.16 to 0.32. GA (13 studies; r = 0.24, 95% CI = [0.15, 0.34], P < .001), SA (12 studies; r = 0.21, 95% CI = [0.23, 0.29], P < .001), PA (9 studies; r = 0.16, 95% CI = [0.06, 0.25], P < .001), EA (8 studies; r = 0.31, 95% CI = [0.20, 0.41], P = .001), PN (7 studies; r = 0.16, 95% CI = [0.00, 0.31], P = .047), and EN (7 studies; r = 0.19, 95% CI = [0.06, 0.32], P = .004).
Disorganized Dimension
Data on the 9 studies including this dimension could be meta-analyzed, including 1246 subjects. Disorganized symptoms were associated with GA (7 studies; r = 0.09, 95% CI = [0.03, 0.15], P = .003) and with SA (3 studies; r = 0.10, 95% CI = [−0.04, 0.24], P = .157) with weak effects. No quantitative analyses could be conducted for the remaining subtypes
Manic Dimension
Data on the 13 studies including this dimension could be meta-analyzed, including 2021 subjects. Mania was positively (with weak effect sizes) associated with GA (11 studies; r = 0.08, 95% CI = [0.01, 0.15], P = .020) and with SA (5 studies; r = 0.13, 95% CI = [0.00, 0.24], P = 0.039) but not with the other subtypes.
Bias Assessment, Heterogeneity, and Meta-Regressions
The overall quality of included studies was rated as “fair,” ranging from 4 to 7 and with a mean of 4.97. The agreed quality grades of each study are presented in supplementary tables S8, and each general score of each study is also reported in supplementary table S5.
Following GRADE criteria, we conducted the exploration of forest plots (see supplementary figures 2–27), with all 12 analyses revealing serious heterogeneity, which were: EA (I2 = 69.93; P = .000) and EN (I2 = 66.47; P = .001) in the positive dimension; EA in the negative dimension (I2 = 83.91; P = .000); GA (I2 = 34.32; P = .049), SA (I2 = 63.66; P = .001), PA (I2 = 63.35; P = .001), EA (I2 = 73.33; P = .000), PN (I2 = 81.24; P = .000), and EN (I2 = 72.67; P = .001) in the depressive dimension; SA (I2 = 60.60; P = .038), PA (I2 = 69.10; P = .021), and EA (I2 = 85.80; P = .001) for the manic dimension. Details are provided in the supplementary material. Exploration of the forest plots revealed that the heterogeneity of the majority of analyses could be explained either by one specific study with small effect going in the opposite direction of all the others or because of a combination of studies with small and large effects sizes going in the same direction; thus, this heterogeneity was considered of little importance. However, this was not the case for EN (positive dimension) and EA (negative dimension), where the dispersion was considerable with studies that showed relatively high effect sizes going in the opposite direction.
We conducted meta-regressions using as covariates the proportion of women, mean age, use of CTQ vs PANSS, and the NOS scores. Results are presented in supplementary table S9 and detailed narratively in the SM. As a whole, all the analyses between CA with the depressive dimension were influenced by the proportion of women (GA r = 1.02, P = .036; SA r = 1.03, P = .005; PA r = 0.99, P = .019; EA r = 0.83, P = .105; PN r = 1.35, P = .033; EN r = 1.31, P = .003), suggesting that women exposed to trauma tended to show higher severity of depression.
Using CTQ and PANSS, as compared to studies that used other instruments did not affect the results. Higher scores on the NOS were negatively associated with depression scores for SA (r = −0.14, P < .001); PA (r = −0.13, P = .004) all the subtypes except for EA, PN (r = −0.21, P = .001), EN (r = −0.19, P < .001), meaning that better quality studies tended to show lower scores in the depressive dimension.
Sensitivity Analyses
We conducted sensitivity analyses with at least 8 studies based on whether they used CTQ/PANSS or not, considering that other instruments may have led to important heterogeneity. Given the low number of studies for the manic, disorganized, and depressive dimensions using CTQ and PANSS, we alternatively categorized them according to whether they used CTQ or not and PANSS or not. None of the analyses revealed a clear difference between studies using this methodology and those that did not. Our results did not change notably when we excluded 6 papers whose composite score of GA also included some experiences that were not in our inclusion criteria.12,37–41 Results can be seen in supplementary table S10 and the Sensitivity Analyses section in the supplementary material.
Discussion
This is the first meta-analysis examining the association between adversity, as a composite measure and by individual subtypes, and the severity of the main psychopathological dimensions in people with psychotic disorders. Three key findings steam from our results: (1) CA, measured as a composite broad category, as well as with most types of abuse, is associated with a range of psychopathological dimensions with weak effects, thus supporting evidence for general effects on psychosis. (2) Neglect is specifically related to the negative and depressive dimensions but not with the other dimensions, supporting the presence of some specific effects. (3) The depressive dimension seems to be the most affected by all forms of adversities with the greatest correlation coefficients ranging from weak to moderate effects, which highlights the importance to address the mood of traumatized individuals with psychosis.
Methodological Considerations
The findings of this review should be interpreted in the context of various methodological considerations.
In terms of limitations related to the included studies: (1) Although a major strength of our work is its large scale, the inclusion of 47 studies and 7379 subjects, enabling us to cover multiple subtypes of adversities across all the study dimensions, the disorganized dimension remained poorly covered: SA was the only subanalysis that we were able to conduct quantitatively; (2) there was a lack of studies examining bullying and household discord, suggesting a new avenue for further work; and (3) only 11 studies overall provided prospective data, hindering the conduction of informative prospective analyses per subtypes of adversities in all the dimensions and, therefore, not allowing comparisons with baseline data.
In terms of limitations of the current work itself: (4) although we tried our best to account for potential heterogeneity resulting from the different instruments used (conducting meta-regression analyses and sensitivity analyses according to studies that used CTQ and PANSS or not) and despite finding no evidence that they may have affected our results, it was impossible to account for all the possible variations across instruments utilized. For example, 6 of the 47 papers12, 37–39, 42, 43 included in their continuous cumulative scores of GA some other life events that were not among our inclusion criteria. Moreover, although most of the symptom clusters defined by the dimensions overlapped across scales, as shown in supplementary table S3, there was some unavoidable nonoverlap, and this needs to be considered when interpreting our data. (5) Adversities tend to co-occur and are highly correlated5; thus, the study of the individual impact of each one separately does not necessarily represent the real-life setting in patients who are exposed to multiple adversities. Thus, when we discuss the presence of specific pathways, the reader needs to consider that such pathways may operate simultaneously in polytraumatized individuals. (6) The effect sizes found in our analyses were generally weak or moderate at best (for the depressive domain). Thus, we need to consider that some of the significant results found in this review can be highly dependent on sample sizes bias and could be affected by other potential confounding variables that have not been systematically addressed by studies included in this work given a lack of data (such as years of education, duration of untreated psychosis, or the percentage of cannabis smokers).
Evidence for General Effects by CA Broadly Defined and Abuse
CA Broadly Defined (GA)
We found evidence for the general effects of overall adversity and all psychopathological dimensions. Our results are not in line with the only previous meta-analysis in the field, which found that a general measure of CA was associated with the positive but not the negative dimension.2 More precisely, that study found, on negative symptoms, a correlation coefficient of r = 0.04 (P = .095) with negative symptoms, whilst we observe a coefficient of r = 0.09 (P < .001) in our study. This discrepancy could be explained by our larger sample (15 studies and 3712 participants in Bailey et al2 compared to 25 studies and 4562 participants in the current work). In addition to the positive and negative dimensions, we further extended the association to the disorganized, depressive, and manic domains.
GA was measured mostly by adding different forms of traumas and creating a cumulative continuous score, so our results are capturing the presence of cumulative effects. Thus CA, measured by the cumulation of adversities, is transsymptomatic and leads to a more serious form of psychosis with higher severity of various symptoms that also co-occur.5,7 There is evidence that some symptoms, particularly low mood, anxiety,6 or dissociation44 may be sequentially related to psychosis in traumatized individuals. Thus, it is likely that, in individuals with various forms of abuse and neglect, multiple and dynamic noncompeting mediating mechanisms are operating simultaneously,6 adding complexity when trying to disentangle specific mediating pathways in polytraumatized individuals. On the other hand, this highlights the idea that people with psychosis and multiple traumas are severely impaired in a variety of psychopathological domains, which suggests that we should consider them as a particularly vulnerable population within the psychosis spectrum, requiring special attention in clinical settings.
Abuse
The positive association of abuse categories was consistent for the positive and depressive dimension, weaker for the negative, only tentatively for the manic, and absent for the disorganized. Nonetheless, we found very few studies in the latter 2 dimensions, suggesting that the lack of evidence may be caused by insufficient sample size.
In terms of the positive dimension, we replicated findings from Bailey et al,2 who found an association with SA, being the only subtype examined in their work. We extended their findings by showing that the association found with the positive dimension is also present for emotional and PA as well. This consolidates the evidence that abuse is not only associated with psychosis onset1 but also with higher severity of the positive dimension in those with the disorder.3,5,45
In terms of negative symptoms, against a quite widespread belief that the link between CA and negative symptoms is limited to neglect,46 and contrary to Bailey et al,2 we found some evidence of a week association between sexual (r = 0.05), physical (r = 0.09) but not EA and the negative dimension. The weak effects sizes do not allow us to draw conclusions about a possible differential impact between these abuse subtypes on the negative dimension, but, certainly, this needs to be addressed carefully in future research.
Evidence for Specific Effects by Neglect
Neglect subtypes were exclusively related to the negative and depressive dimensions but not with the positive or manic, with not enough studies in the disorganized domain to draw conclusions. This differential impact of neglect on the positive and the negative dimensions replicates what was found by Bailey et al.2 Research understanding the pathways linking neglect and the negative symptoms is almost nonexistent. To the best of our knowledge, only one study conducted in clinical samples suggests a connecting role of mentalizing abilities and attention deficits.47 Thus, more research in this area is needed.
The Depressive Dimension is Affected by all Forms of CA
A consistent association between all categories with the depressive symptoms was found, with the stronger effects being present for EA (r = 0.32). This supports the view that the well-known link between trauma with depression48 also applies when depression is measured as an outcome in those with psychosis. Moreover, it highlights the importance of targeting mood in the treatment of people with psychosis and trauma; not only do those symptoms by themselves strongly impact on functioning and quality of life49 but also mood appears as a potential mediating mechanism connecting trauma with the positive symptoms as recently suggested.6
Conclusions
Our meta-analysis suggests that CA measured broadly is associated with greater severity of all main dimensions in psychosis; this is also the case for experiences of abuse, although more studies examining manic and disorganized dimensions are needed. We found evidence for some specific effects, such as the effect of neglect on the depressive and negative dimension exclusively, which opens a new avenue for future research investigating possible mediating pathways. Against previous reports,2 we found evidence that sexual and PA, but not EA, are associated with the negative dimension in those with psychosis, which also opens new avenues. The depressive dimension is the most severely affected by all forms of trauma with the strongest effects across all analyses conducted, showing the importance of treating depressive symptoms in traumatized patients with psychosis, given the supporting evidence of a partial mediation of mood-related symptoms in the adversity–psychosis association.6
Supplementary Material
Acknowledgments
We thank our funding bodies (Swiss National Science Foundation, the National Institute for Health Research, National Alliance for Research on Schizophrenia and Depression, and Economic and Social Research Council Centre for Society and Mental Health) for their support.
Funding
This work was supported by the Swiss National Science Foundation (grant P2LAP3_171804 to L.A.). This paper represents independent research part funded by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, South-Eastern Norway Health Authority (#2017060), and the National Alliance for Research on Schizophrenia and Depression Young Investigator Award to M.A. (#22388). G.S.P is supported by the Alicia Koplowitz Foundation. This paper represents an independent research part supported by the Economic and Social Research Council Centre for Society and Mental Health at King’s College London (ESRC reference: ES/S012567/1). The views expressed are those of the author(s) and not necessarily those of the Economic and Social Research Council Studentships, the NIHR, the National Health Service, the Department of Health and Social Care, or King’s College London.
References
- 1. Varese F, Smeets F, Drukker M, et al. . Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. 2018;44(5):1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bentall RP, de Sousa P, Varese F, et al. . From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc Psychiatry Psychiatr Epidemiol. 2014;49(7):1011–1022. [DOI] [PubMed] [Google Scholar]
- 4. Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112(5):330–350. [DOI] [PubMed] [Google Scholar]
- 5. Morgan C, Gayer-Anderson C. Childhood adversities and psychosis: evidence, challenges, implications. World Psychiatry. 2016;15(2):93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alameda L, Rodriguez V, Carr E, et al. . A systematic review on mediators between adversity and psychosis: potential targets for treatment. Psychol Med. 2020;50(12):1966–1976. [DOI] [PubMed] [Google Scholar]
- 7. van Nierop M, Viechtbauer W, Gunther N, et al. ; Genetic Risk and OUtcome of Psychosis investigators . Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. 2015;45(6):1277–1288. [DOI] [PubMed] [Google Scholar]
- 8. Bebbington P. Unravelling psychosis: psychosocial epidemiology, mechanism, and meaning. Shanghai Arch Psychiatry. 2015;27(2):70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bendall S, Jackson HJ, Hulbert CA. Childhood trauma and psychosis: review of the evidence and directions for psychological interventions. Aust Psychol. 2010;45(4):299–306. [Google Scholar]
- 10. Alameda L, Golay P, Baumann PS, Ferrari C, Do KQ, Conus P. Age at the time of exposure to trauma modulates the psychopathological profile in patients with early psychosis. J Clin Psychiatry. 2016;77(5):e612–e618. [DOI] [PubMed] [Google Scholar]
- 11. van Dam D, van Nierop M, Viechtbauer W, et al. . Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychol Med. 2015;45(7):1363–1377. [DOI] [PubMed] [Google Scholar]
- 12. Seidenfaden D, Knorr U, Soendergaard MG, et al. . The relationship between self-reported childhood adversities, adulthood psychopathology and psychological stress markers in patients with schizophrenia. Compr Psychiatry. 2017;72:48–55. [DOI] [PubMed] [Google Scholar]
- 13. van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Quattrone D, Di Forti M, Gayer-Anderson C, et al. . Transdiagnostic dimensions of psychopathology at first episode psychosis: findings from the multinational EU-GEI study. Psychol Med. 2019; 49(8):1378–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Stewart L, Shekelle P. Implementing PRISMA-P: recommendations for prospective authors. Syst Rev. 2016;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stroup DF, Berlin JA, Morton SC, et al. . Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 17. American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association;1994. [Google Scholar]
- 18. World Health Organization The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines Geneva, switzerland: World Health Organization; 1992. [Google Scholar]
- 19. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. [DOI] [PubMed] [Google Scholar]
- 20. Friedman S, Harrison G. Sexual histories, attitudes, and behavior of schizophrenic and “normal” women. Arch Sex Behav. 1984;13(6):555–567. [DOI] [PubMed] [Google Scholar]
- 21. Pichot P. [DSM-III: the 3d edition of the diagnostic and statistical manual of mental disorders from the American Psychiatric Association]. Rev Neurol (Paris). 1986;142(5):489–499. [PubMed] [Google Scholar]
- 22. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. [DOI] [PubMed] [Google Scholar]
- 23. Lenhard W, Lenhard A.. Calculation of Effect Sizes. Dettelbach, Germany; 2016. [Google Scholar]
- 24. Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. J Appl Psychol. 2005;90(1):175–181. [DOI] [PubMed] [Google Scholar]
- 25. Borenstein M, Hedges L, Higgins J, Rothstein H.. Comprehensive Meta-Analysis Version 2. Englewood, NJ: Biostat; 2005. [Google Scholar]
- 26. Davies C, Segre G, Estradé A, et al. . Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(5):399–410. [DOI] [PubMed] [Google Scholar]
- 27. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. [DOI] [PubMed] [Google Scholar]
- 29. Ratner B. The correlation coefficient: Its values range between+ 1/− 1, or do they? J Target Meas Anal Market. 2009;17(2):139–142. [Google Scholar]
- 30. Bernstein DP, Stein JA, Newcomb MD, et al. . Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. [DOI] [PubMed] [Google Scholar]
- 31. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. [DOI] [PubMed] [Google Scholar]
- 32. Sayın A, Yüksel N, Konac E, et al. . Effects of the adverse life events and Disrupted in Schizophrenia-1 (DISC1) gene polymorphisms on acute symptoms of schizophrenia. DNA Cell Biol. 2013;32(2):73–80. [DOI] [PubMed] [Google Scholar]
- 33. Lysaker PH, Beattie NL, Strasburger AM, Davis LW. Reported history of child sexual abuse in schizophrenia: associations with heightened symptom levels and poorer participation over four months in vocational rehabilitation. J Nerv Ment Dis. 2005;193(12): 790–795. [DOI] [PubMed] [Google Scholar]
- 34. Ruby E, Rothman K, Corcoran C, Goetz RR, Malaspina D. Influence of early trauma on features of schizophrenia. Early Interv Psychiatry. 2017;11(4):322–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sahin S, Yüksel Ç, Güler J, et al. . The history of childhood trauma among individuals with ultra high risk for psychosis is as common as among patients with first-episode schizophrenia. Early Interv Psychiatry. 2013;7(4):414–420. [DOI] [PubMed] [Google Scholar]
- 36. Schalinski I, Teicher MH. Type and timing of childhood maltreatment and severity of shutdown dissociation in patients with schizophrenia spectrum disorder. PLoS One. 2015;10(5):e0127151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kilcommons AM, Morrison AP. Relationships between trauma and psychosis: an exploration of cognitive and dissociative factors. Acta Psychiatr Scand. 2005;112(5): 351–359. [DOI] [PubMed] [Google Scholar]
- 38. Kumari V, Gudjonsson GH, Raghuvanshi S, et al. . Reduced thalamic volume in men with antisocial personality disorder or schizophrenia and a history of serious violence and childhood abuse. Eur Psychiatry. 2013;28(4):225–234. [DOI] [PubMed] [Google Scholar]
- 39. Lindgren M, Mäntylä T, Rikandi E, et al. . Childhood adversities and clinical symptomatology in first-episode psychosis. Psychiatry Res. 2017;258:374–381. [DOI] [PubMed] [Google Scholar]
- 40. McCabe KL, Maloney EA, Stain HJ, Loughland CM, Carr VJ. Relationship between childhood adversity and clinical and cognitive features in schizophrenia. J Psychiatr Res. 2012;46(5):600–607. [DOI] [PubMed] [Google Scholar]
- 41. Stain HJ, Brønnick K, Hegelstad WT, et al. . Impact of interpersonal trauma on the social functioning of adults with first-episode psychosis. Schizophr Bull. 2014;40(6):1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McCabe KL, Maloney EA, Stain HJ, Loughland CM, Carr VJ. Relationship between childhood adversity and clinical and cognitive features in schizophrenia. J Psychiatr Res. 2012;46(5):600–607. [DOI] [PubMed] [Google Scholar]
- 43. Stain HJ, Brønnick K, Hegelstad WT, et al. . Impact of interpersonal trauma on the social functioning of adults with first-episode psychosis. Schizophr Bull. 2014;40(6):1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Longden E, Branitsky A, Moskowitz A, Berry K, Bucci S, Varese F. The relationship between dissociation and symptoms of psychosis: a meta-analysis. Schizophr Bull. 2020;46(5):1104–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Murray R, Mondelli V, Stilo S, et al. . The influence of risk factors on the onset and outcome of psychosis: what we learned from the GAP study. Schizophr Res. 2020;225:63–68. [DOI] [PubMed] [Google Scholar]
- 46. Ross CA, Anderson G, Clark P. Childhood abuse andthe positive symptoms of schizophrenia. Psychiatr Serv. 1994;45(5):489–491. [PubMed] [Google Scholar]
- 47. Mansueto G, Schruers K, Cosci F, van Os J; GROUP Investigators . Childhood adversities and psychotic symptoms: the potential mediating or moderating role of neurocognition and social cognition. Schizophr Res. 2019;206:183–193. [DOI] [PubMed] [Google Scholar]
- 48. Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: a meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. 2015;30(6):665–680. [DOI] [PubMed] [Google Scholar]
- 49. Alameda L, Golay P, Baumann PS, et al. . Mild depressive symptoms mediate the impact of childhood trauma on long-term functional outcome in early psychosis patients. Schizophr Bull. 2017;43(5):1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.