Abstract
We provide one of the first national longitudinal studies of the association between trajectories of marital quality and cognitive functioning among older adults, with close attention paid to gender differences. Data were drawn from the Health and Retirement Study (HRS) 2006-2016. Marital quality trajectories were assessed at three waves: 2006/2008, 2010/2012, and 2014/2016. Cognitive trajectories were assessed at five waves: 2008, 2010, 2012, 2014, and 2016. The final analytic sample included 7,901 respondents age 50 and older (4,334 men and 3,567 women) who were either married or cohabiting during the study period. Results from parallel linear growth curve models suggest that among older adults, initial positive marital quality was associated with better initial cognition, and initial negative marital quality was associated with worse initial cognition. Results from multiple group analysis further suggest that marital quality was significantly associated with men’s cognitive trajectories but not women’s. Among men, an increase in positive marital quality was associated with a slower rate of cognitive decline, whereas an increase in negative marital quality was associated with a faster rate of cognitive decline. These findings suggest that older men who experience a decline in marital quality may be vulnerable to cognitive decline and that reducing marital strain and improving marital quality may protect men’s cognitive health in later life.
Keywords: Marital quality, Cognitive function, Aging, Gender
Introduction
With the rapid aging of the U.S. population, cognitive decline has emerged as a serious and growing public health concern (Jessen et al., 2014). Cognitive decline can range from mild cognitive impairment to dementia, a severe condition associated with disability, increased need for medical and personal care, and premature death (Centers for Disease Control and Prevention, 2019). Today, more than 16 million older Americans are living with either a slight or a severe decline in cognitive abilities (Centers for Disease Control and Prevention, 2011). Research has been devoted to identifying primarily biological and behavioral risk factors of cognitive decline and dementia to inform the design of protective intervention strategies. An important next step is to identify social, life-course contexts that contribute to cognitive decline. In this study, we examine marital quality as an underexplored social risk/protective factor for cognitive decline among older adults in the United States.
It has long been recognized that married people are healthier (both mentally and physically) and longer-lived than unmarried people (Liu & Waite, 2014; Zhang & Hayward, 2006). Recent research also finds evidence of this marital advantage for cognitive health: The risk of cognitive impairment and dementia is lower among married people than among their unmarried peers (Liu et al., 2019; Liu et al., 2020). At the same time, family scholars argue that it is not the case that any marriage is better than none, pointing to marital quality—defined as spouses’ subjective appraisal of the marital relationship, including satisfaction, happiness, strain, and conflict—as more salient than marital status for health (Liu & Waite, 2014; Umberson et al., 2006). Marital quality has a profound influence on each partner’s life context and thus on his or her health risk (Carr et al., 2016; Umberson et al., 2006). However, few studies have examined how marital quality is related to the risk of cognitive decline.
To help fill this gap, we analyzed nationally representative longitudinal data from the Health and Retirement Study (HRS) 2006-2016 to assess how positive and negative aspects of marital quality shape trajectories of cognitive decline among older Americans. Given the longstanding literature on gender differences in marriage links to general health and well-being (Carr & Springer, 2010; Hughes & Waite, 2009; Liu & Waite, 2014; Zhang & Hayward, 2006), we further considered whether the relationship between marital quality and cognitive decline varies by gender. Guided by the gendered life course perspective, we used growth curve analyses to examine cognitive decline as a continuous process in response to marital quality change over time. Our findings will help health policy makers and practitioners design effective groupspecific intervention strategies to protect against cognitive decline.
Previous Empirical Studies of Marital Quality and Cognitive Health
A number of studies have examined the relationship between marital quality and various health outcomes, including self-rated health, psychological well-being, heart disease, diabetes, inflammation, salivary telomere length, and mortality, and have found that better marital quality is generally associated with better health outcomes (Bulanda et al., 2016; Carr et al., 2014; Carr et al., 2016; Eaker et al., 2007; Kiecolt-Glaser & Newton, 2001; Liu & Waite, 2014; Liu et al., 2016; Robles et al., 2014; Umberson et al., 2006; Yu & Liu, 2020). However, research on the linkage between marital quality and cognitive health, especially based on U.S. data, is rare and provides inconsistent evidence. For example, a study of 841 older, married respondents to the Americans’ Changing Lives survey found that negative marital quality was associated with a slower rate of increase in cognitive limitations over time, a finding inconsistent with the broad literature on marital quality linking to health (Xu et al., 2016). In contrast, a recent analysis of data from the Health and Retirement Study found no evidence of a relationship between marital strain and subsequent rates of memory change, although marital strain was negatively associated with baseline levels of memory (Zahodne et al., 2019). Neither study found evidence that positive marital quality is linked to either cognitive limitations (Xu et al., 2016) or memory decline (Zahodne et al., 2019). Other than these conflicting studies, empirical data about potential links between marital quality and cognitive decline is extremely limited, and the question clearly warrants more research.
A Life Course Perspective on the Link Between Marital Quality and Cognitive Trajectories
Recent research develops a life course perspective on the link between marital quality and general health (e.g., Liu & Waite, 2014; Umberson et al., 2006), which may extend to cognitive health. The life course perspective maintains that marital quality holds significant meaning for individuals and shapes life context, which in turn affects health outcomes (Liu & Waite, 2014; Umberson et al., 2006). Glymour and Manly (2008) argue that a life course approach to studying cognitive health is important because “cognitive function is a developmental trajectory, and harmful exposures may influence the likelihood of impairments in old age by derailing the maturation trajectory, promoting pathological processes, or restricting compensation or resilience after pathological events” (2008: p. 224). Involvement in a high-conflict marriage is one specific type of “harmful exposure” that can create a significant source of stress and result in elevated levels of stress over the life course (Carr et al., 2016; Glymour & Manly, 2008; Kiecolt-Glaser et al., 2005). Marital stress is one of the most frequently encountered and disturbing forms of human stress for most adults. Elevated stress, in general, is pathogenic and can raise individuals’ vulnerability to cognitive decline (Rothman & Mattson, 2010; Johansson et al., 2013), although mild stress does not necessarily harm and may actually bolster cognitive health (Thomas & Umberson, 2018). Marital stress can intensify the process of cognitive decline by causing the sympathetic nervous system to induce the release of stress hormones (e.g., catecholamines, cortisol), which can trigger physiological responses, damage brain cells, and impair memory and other cognitive functions (Kuhlmann et al., 2005; Henckens et al., 2009; Oei et al., 2007). Moreover, elevated stress from a high-conflict marriage may cause detrimental neurobiological changes and emotional and behavioral problems, such as feeling depressed, smoking, and drinking (Hayes et al., 2016; Swan & Lessov-Schlaggar, 2007). These emotional and behavioral problems, in turn, may be detrimental to cognitive function and accelerate cognitive decline in later life.
Conversely, involvement in a happy marriage modifies one’s life context by increasing access to social support (e.g., emotional support, availability and perception of help, assistance and advice), social participation (e.g., engagement in community or social activities), and social controls (e.g., partners regulating each other’s health behaviors), all of which promote health (Dehle et al., 2001; Liu & Waite, 2014; Umberson et al., 2018) and may also protect against cognitive decline (Costa-Cordella et al., 2021; Pillai & Verghese, 2009; Shankar et al., 2013; Zunzunegui et al., 2003). For example, a spouse, especially in a happy relationship, is usually one’s primary confidant and provides a key source of companionship and social support (Dehle et al., 2001; Waite & Gallagher, 2000). Social support alleviates cardiovascular reactivity to stress, a precursor to the development of heart disease that can also negatively affect cognition (Hughes & Ganguli, 2009). Social support may also protect cognitive functioning via its buffering effect on stress: such support dampens the hypothalamic-pituitary-adrenocortical (HPA) axis response and promotes resilience (Costa-Cordella et al., 2021; Kelly et al., 2017; Ozbay et al., 2007). Additionally, a supportive spouse may enlarge an individual’s networks and increase social participation by establishing connections with the spouse’s friends and family (Waite & Gallagher, 2000). Growing evidence from both cross-sectional and longitudinal studies indicates that an active and socially engaged lifestyle is related to improved cognitive function in later life (Kelly et al., 2017; Litwin & Stoeckel, 2016; Newson & Kemps, 2005; Wang et al., 2013). Social participation and larger network size may reduce cognitive decline by improving cognitive reserves, which strengthen the ability to cope with neuropathological damage via compensatory cognitive strategies (Giles et al., 2012; Sommerlad et al., 2018; Zunzunegui et al., 2003). Also, daily communication with a spouse, perhaps especially while in a positive mood, provides cognitive stimulation and may increase neural plasticity, thereby maintaining and improving cognitive reserves (Giles et al., 2012). Moreover, in a supportive relationship, a spouse may remind the partner to develop healthy habits such as quitting smoking and reducing drinking (Umberson et al., 2018), which may, in turn, protect against cognitive decline, since both smoking and heavy drinking can damage cognitive function, for example by triggering oxidative stress and inflammation (Hayes et al., 2016; Swan & Lessov-Schlaggar, 2007). Taking this evidence together, we hypothesize that greater positive marital quality (i.e., marital support) is associated with better cognitive function and slower cognitive decline, while greater negative marital quality (i.e., marital stress) is associated with worse cognitive function andfaster cognitive decline (Hypothesis 1).
Gender Difference
Gender is a fundamental determinant of life course context and has been a central focus of research on links between marriage and health. Scholars argue that men tend to receive more health benefits from marriage than women and that women are more psychologically and physiologically vulnerable to marital strain than men (Bernard, 1972; Simon, 2002). Previous studies have provided mixed empirical evidence on these gender differences. For example, some studies find that marital strain has stronger harmful effects on women’s physiological functioning (Kiecolt-Glaser & Newton, 2001), cardiovascular risk (Liu & Waite, 2014), and longevity (Bulanda et al., 2016) than on men’s, while others find no evidence of gender differences in marital quality links to self-rated health (Umberson et al., 2006) or mental health (Carr et al., 2014).
Empirical research on gender differences in links between marital quality and cognitive function is rare. The only study we know of that has tested gender differences in marital quality links to cognition found no evidence of gender difference in the association between marital quality and cognitive limitations (Xu et al., 2016). A few other studies have examined gender variations in marital status links to cognition. For example, a study in Sweden found no gender differences in the association of marital status with dementia (Sundström et al., 2016), whereas another study found that never-married and widowed Chinese men had greater odds of being cognitively impaired than married Chinese men, yet no such associations were found in Chinese women (Feng et al., 2014). A recent study in the United States also found that divorce and widowhood had stronger effects on men’s risk of developing dementia than on women’s (Liu et al., 2020). Nevertheless, little is known about how marital quality may shape the process of cognitive decline similarly or differently for men and women. Given the paucity of previous research as well as the mixed evidence on gender differences in marital quality links to other health outcomes, we conduct an exploratory analysis rather than a hypothesis-driven analysis of gender difference in the association between marital quality and cognitive trajectories.
Data
We used data from the Health and Retirement Study (HRS) 2006-2016. The HRS is a longitudinal study of nationally representative samples of Americans age 50 and older and their spouses or partners, conducted by the Institute for Social Research at the University of Michigan. The survey oversamples Blacks and Hispanics and collects (by telephone or in person) detailed information on health behaviors and cognitive, physical, economic, work, and family conditions approximately every two years. In addition to the biennially longitudinal surveys, HRS respondents have been asked about psychosocial characteristics every four years: a random half of respondents have been asked these questions since 2006 (i.e., 2006, 2010, 2014), while the other half have been asked since 2008 (i.e., 2008, 2012, 2016). This information includes respondents’ assessments of the supportive and unsupportive behaviors of their spouses or unmarried cohabiting partners (Smith et al., 2017). Because the marital quality data were only collected every four years, we assessed marital quality trajectories based on three waves: 2006/2008, 2010/2012, and 2014/2016. To make full use of the data, we assessed cognitive trajectories based on five waves: 2008, 2010, 2012, 2014, and 2016. We excluded the cognitive measure in the 2006 wave due to concerns about time order between the dependent (cognition) and independent (marital quality) variables.
Because the focus of our study was marital quality, we excluded unmarried respondents (i.e., divorced/separated, widowed, or never married) at each wave. Additional analyses (results not shown but available upon request) suggested that those who were unmarried and thus excluded from the analysis had poorer cognition. In this sense, we excluded a more vulnerable group and our findings may be conservative. We further excluded respondents who were younger than age 50 in 2006 and those who had missing data on key covariates such as education, race-ethnicity, and baseline marital status. Missing values on marital quality factors and cognitive scores (about 5%) were handled using the Full Information Maximum Likelihood (FIML) estimation approach in Mplus (Muthén & Muthén, 1998-2015). The final analytic sample included 7,901 respondents (4,334 men and 3,567 women) who were either married (n = 7,611) or cohabiting (n = 290). We included both married and cohabiting respondents because previous studies suggest that marriage and cohabitation tend to be similar among older couples (King & Scott, 2005; Brown & Wright, 2017). Findings of additional analyses (results not shown but available upon request) that excluded cohabitors were similar to those reported.
Measures
Cognition.
The HRS assessed cognitive function via the modified version of the Telephone Interview for Cognitive Status (TICS). A small percentage of respondents (0.8–3.1%) refused to participate in tests of immediate and delayed recall and serial 7s; the HRS has developed an imputation strategy for cognitive variables for all waves (Servais, 2010). We followed previous studies in calculating a final summary score by summing the following cognitive items: immediate and delayed recall of a list of 10 words (1 point for each), five trials of serial 7s (i.e., subtract 7 from 100, and continue subtracting 7 from each subsequent number for a total of five trials; 1 point for each trial), and backward counting (2 points). The final summary score ranges from 0 (severely impaired) to 27 (high functioning) (Crimmins et al., 2016).
Marital quality.
Marital quality comprises both positive and negative dimensions, which are not opposite ends of a single spectrum but distinct constructs (Umberson et al., 2006). The marital quality measures are composed of 8 items: (1) “How much does your spouse/partner really understand the way you feel about things?” (2) “How much can you rely on your spouse/partner if you have a serious problem?” (3) “How much can you open up to your spouse/partner if you need to talk about your worries?” (4) “How close is your relationship with your partner or spouse?” (5) “How much does your spouse/partner make too many demands on you?” (6) “How much does your spouse/partner criticize you?” (7) “How much does your spouse/partner let you down when you are counting on them?” (8) “How much does your spouse/partner get on your nerves?” Responses to these eight questions ranged from 1 (a lot) to 4 (not at all). Scores were recoded to obtain consistent response categories across all items. Results from exploratory factor analyses suggested that these eight items form two different dimensions. We followed prior research and distinguished between these two dimensions (Umberson et al., 2006; Liu & Waite, 2014), which we referred to as positive and negative marital quality, respectively. We used maximum-likelihood factor analyses and orthogonal varimax rotation to create these two dimensions of marital quality, with higher values indicating higher positive or negative marital quality. Table 1 shows the factor loadings of each item used to generate the factor scores for positive and negative marital quality. Cronbach’s alpha for positive and negative items across all waves ranges from 0.78 to 0.84, indicating a sufficient level of internal consistency.
Table 1.
Factor Loadings for Marital Quality
| 2006/08 | 2010/12 | 2014/16 | |
|---|---|---|---|
| Positive Marital Quality | |||
| 1. How much does your partner/spouse really understand the way you feel about things? | 0.77 | 0.77 | 0.76 |
| 2. How much can you rely on your partner/spouse if you have a serious problem? | 0.70 | 0.70 | 0.70 |
| 3. How much can you open up to your partner/spouse if you need to talk about your worries? | 0.83 | 0.83 | 0.84 |
| 4. How close is your relationship with your partner or spouse? | 0.73 | 0.70 | 0.72 |
| Negative Marital Quality | |||
| 5. How much does your partner/spouse make too many demands on you | 0.67 | 0.67 | 0.67 |
| 6. How much does your partner/spouse criticize you? | 0.67 | 0.71 | 0.70 |
| 7. How much does your partner/spouse let you down when you are counting on them? | 0.68 | 0.68 | 0.68 |
| 8. How much does your partner/spouse get on your nerves? | 0.73 | 0.74 | 0.74 |
Sociodemographic covariates.
We controlled for basic sociodemographic covariates at the baseline, including gender (0 = male, 1 = female), age (in years), race-ethnicity (non-Hispanic white [reference], non-Hispanic black, non-Hispanic other race, and Hispanic), education (less than high school [reference], high school graduate, some college, and college graduate or above), marital status (0 = married, 1 = cohabiting), order of marriage (0, 1st, 2nd, 3rd and higher-order marriage), parental status (0 = childless, 1 = at least one child), and having living siblings (0 = no living sibling, 1 = at least one living sibling). Because the marital quality measures were collected every four years, with a random half of the sample starting in 2006 and the other random half starting in 2008, we also controlled for an indicator of starting survey year for marital quality measures (0 = starting in 2006, 1 = starting in 2008).
Statistical Methods
To take advantage of the longitudinal data from the HRS, we used growth curve modeling to assess the effect of marital quality on the initial level of cognition (i.e., latent intercept) and change (i.e., latent slope) in cognition over the study period. Because respondents entered the HRS study period with different initial levels of both marital quality and cognition and experienced different changes in marital quality and cognition over time, we modelled marital quality as parallel growth trajectories to predict growth trajectories of cognition. The parallel linear growth curve model employed in this study can be specified as:
Cij is the ith individual’s cognitive function at time j. π0i and π1i are the latent intercept and slope of the cognitive trajectory for the ith individual across waves. Qij is the ith individual’s marital quality score at time j. Note that j in the cognitive trajectory indicates five waves, while j in the marital quality trajectory indicates three waves, θ0i and θ1i are the latent intercept and slope of the marital quality trajectory for the ith individual across waves. Tii denotes analysis time. X is the vector of covariates, and A1-A4 are vectors of corresponding coefficients, εij, vij, and δ1i-δ4i represent residual terms. The parameters λ00, λ10, and λ11 are the focus of the interpretation: they describe the effects of marital quality trajectories on cognitive trajectories. Figure 1 illustrates the structural model of parallel linear growth curve analysis employed in this study. Following previous studies (e.g., Umberson et al., 2006; Xu et al., 2016), we estimated positive and negative marital quality trajectories separately. We started with a general model followed by multiple group analysis to examine potential gender differences. We conducted t-tests to compare individual coefficients between men and women; results (not shown but available upon request) suggested that all key gender differences were statistically significant (p < .05) in the multiple group analysis. The growth curve models were estimated using Mplus 8.3 (Muthén & Muthén, 1998-2015).
Figure 1.
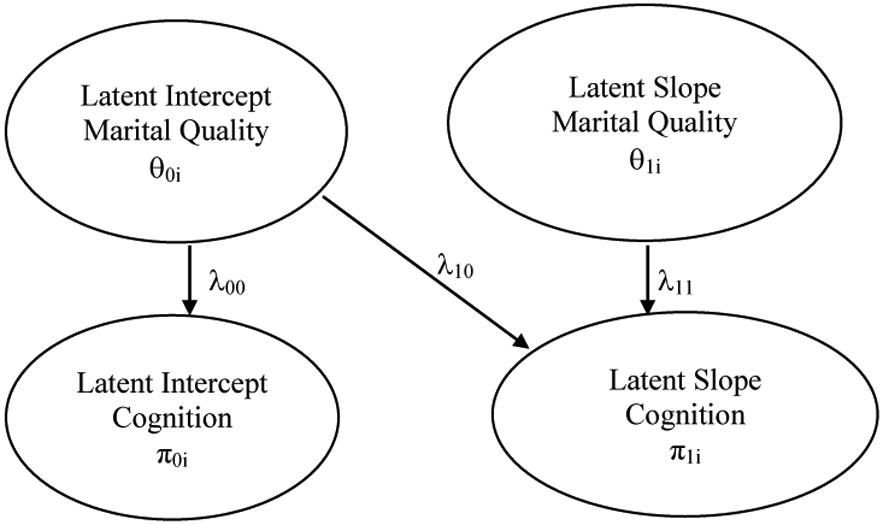
Structural Path Diagram of the Parallel Growth Curve Trajectories of Marital Quality and Cognition
Results
Table 2 displays the descriptive statistics of all analytical variables, both in the total sample as well as by gender. Generally, respondents’ cognitive function steadily decreased while the mean values of marital quality remained relatively stable across waves. Women showed significantly better cognitive functioning at each time point than men. Men tended to report higher positive marital quality and lower negative marital quality than women. On average, women were younger, less likely to be college graduates, more likely to be in their first marriages, and more likely to have living siblings than men.
Table 2.
Descriptive Statistics of Analytic Variables
| Mean (SD) or % | ||||
|---|---|---|---|---|
| Variables | Total (N=7,901) |
Men (n=4,334) |
Women (n=3,567) |
|
| Cognitive function 2008 | 15.74 (4.27) | 15.14 (4.15) | 16.43 (4.29) | * |
| Cognitive function 2010 | 15.51 (4.26) | 14.87 (4.19) | 16.22 (4.22) | * |
| Cognitive function 2012 | 15.29 (4.31) | 14.63 (4.20) | 16.01 (4.31) | * |
| Cognitive function 2014 | 15.45 (4.40) | 14.85 (4.27) | 16.09 (4.44) | * |
| Cognitive function 2016 | 15.22 (4.37) | 14.70 (4.30) | 15.74 (4.38) | * |
| Positive marital quality 2006/08 | 0.10 (0.83) | 0.21 (0.74) | −0.03 (0.91) | * |
| Positive marital quality 2010/12 | 0.09 (0.83) | 0.22 (0.73) | −0.05 (0.90) | * |
| Positive marital quality 2014/16 | 0.08 (0.84) | 0.21 (0.75) | −0.05 (0.91) | * |
| Negative marital quality 2006/08 | −0.05 (0.85) | −0.10 (0.81) | 0.01 (0.89) | * |
| Negative marital quality 2010/12 | −0.06 (0.84) | −0.12 (0.81) | 0.00 (0.86) | * |
| Negative marital quality 2014/16 | −0.05 (0.84) | −0.10 (0.81) | 0.01 (0.86) | * |
| Baseline Covariates | ||||
| Age (years) | 65.54 (8.86) | 67.05 (8.96) | 63.70 (8.35) | * |
| Race-ethnicity (%) | ||||
| Non-Hispanic White | 80.71 | 80.71 | 80.71 | |
| Non-Hispanic Black | 8.70 | 8.61 | 8.80 | |
| Hispanic | 5.95 | 5.95 | 5.94 | |
| Other | 4.64 | 4.73 | 4.54 | |
| Education (%) | ||||
| Less than high school | 17.93 | 19.73 | 15.76 | * |
| High school | 33.31 | 30.18 | 37.12 | * |
| Some college | 34.83 | 34.10 | 35.72 | |
| College graduate or above | 13.92 | 15.99 | 11.41 | * |
| Marital status (%) | ||||
| Married | 96.33 | 96.12 | 96.58 | |
| Cohabiting | 3.67 | 3.88 | 3.42 | |
| Order of Marriage | ||||
| 0 marriage | 0.46 | 0.48 | 0.42 | |
| 1st marriage | 68.37 | 66.77 | 70.31 | * |
| 2nd marriage | 23.10 | 24.57 | 21.31 | * |
| 3rd and higher-order | 8.07 | 8.17 | 7.96 | |
| Parental Status (%) | ||||
| Childless | 8.04 | 7.84 | 8.27 | |
| Having at least one child | 91.96 | 92.16 | 91.73 | |
| Sibling (%) | ||||
| No living sibling | 12.91 | 13.80 | 11.83 | * |
| Having at least one living sibling | 87.09 | 86.20 | 88.17 | * |
| MQ survey starting year (%) | ||||
| Since 2006 | 54.79 | 55.63 | 53.77 | |
| Since 2008 | 45.21 | 44.37 | 46.23 | |
Note:
Statistically significant difference by gender at the p < .01 level. SD: Standard Deviation
Table 3 presents the results from the growth curve models predicting the initial levels of cognitive function (latent intercept) and the rate of change (latent slope) in cognitive function. Panels A and B show the results of the models for positive and negative marital quality, respectively, predicting cognitive trajectories. Results in Table 3 suggest that higher initial levels of positive marital quality were associated with higher initial levels of cognitive function (Panel A: λ00 = 0.216, p < .01), and higher initial levels of negative marital quality were associated with lower initial levels of cognitive function (Panel B: λ00 = −0.271, p < .001). However, neither the initial levels nor the rate of change of either positive or negative marital quality were significantly associated with the rate of cognitive decline.
Table 3.
Effects of Marital Quality on Cognition from Latent Growth Curve Models, HRS 2006-2016, Total Sample (N=7,901)
| A. Positive Marital Quality |
B. Negative Marital Quality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Latent Intercept | Latent Slope | Latent Intercept | Latent Slope | |||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Marital quality intercept | 0.216** | 0.066 | −0.010 | 0.011 | −0.271*** | 0.069 | 0.009 | 0.011 |
| Marital quality slope | 0.724 | 0.494 | −1.054 | 0.842 | ||||
| Baseline Covariates | ||||||||
| Age (centered at mean) | −0.144*** | 0.005 | −0.011*** | 0.001 | −0.144*** | 0.005 | −0.011*** | 0.001 |
| Gender (ref: male) | ||||||||
| Female | 0.992*** | 0.079 | −0.033** | 0.012 | 0.970*** | 0.077 | −0.036** | 0.012 |
| Race-ethnicity (ref: non-Hispanic White) | ||||||||
| non-Hispanic Black | −2.318*** | 0.138 | 0.002 | 0.021 | −2.299*** | 0.138 | 0.003 | 0.021 |
| Hispanic | −1.221*** | 0.168 | 0.012 | 0.026 | −1.201*** | 0.169 | 0.018 | 0.026 |
| Other | −1.960*** | 0.181 | −0.011 | 0.027 | −1.920*** | 0.182 | −0.023 | 0.031 |
| Education (ref: less than high school) | ||||||||
| High school | 2.196*** | 0.118 | 0.007 | 0.019 | 2.195*** | 0.118 | 0.016 | 0.020 |
| Some college | 3.493*** | 0.119 | −0.009 | 0.019 | 3.494*** | 0.118 | −0.004 | 0.019 |
| College above | 4.708*** | 0.143 | 0.018 | 0.022 | 4.718*** | 0.142 | 0.021 | 0.022 |
| Marital Status (ref: married) | ||||||||
| Cohabiting | −0.633** | 0.213 | 0.018 | 0.034 | −0.675** | 0.213 | 0.046 | 0.042 |
| Order of Marriage (ref: 0 marriage) | ||||||||
| 1st marriage | 0.217 | 0.584 | −0.039 | 0.089 | 0.158 | 0.584 | −0.010 | 0.090 |
| 2nd marriage | 0.295 | 0.585 | −0.058 | 0.090 | 0.220 | 0.585 | −0.021 | 0.090 |
| 3rd and higher-order | 0.234 | 0.595 | −0.075 | 0.090 | 0.168 | 0.595 | −0.046 | 0.092 |
| Having at least one child | 0.120 | 0.140 | −0.004 | 0.021 | 0.128 | 0.140 | −0.004 | 0.022 |
| Having at least one living sibling | 0.189 | 0.118 | 0.027 | 0.019 | 0.201 | 0.118 | 0.024 | 0.019 |
| MQ survey starting year (ref: 2006) | ||||||||
| 2008 | −0.010 | 0.075 | −0.001 | 0.011 | −0.023 | 0.075 | 0.009 | 0.014 |
| Means of growth parameters | 12.392*** | 0.602 | −0.141 | 0.094 | 12.458*** | 0.603 | −0.183* | 0.093 |
| Variances in growth parameters | 6.159*** | 0.192 | 0.012** | 0.005 | 6.148*** | 0.192 | 0.012* | 0.005 |
| Model fit index | CFI=0.992 | TLI=0.985 | RMSEA=0.018 | CFI=0.991 | TLI=0.984 | RMSEA=0.019 | ||
p<0.001
p<0.01
p<0.05
Table 4 shows the results from multiple group analysis for men and women; these results suggest that marital quality shaped cognitive trajectories only of men but not of women. For men, higher initial levels of positive marital quality were associated with higher initial levels of cognitive function (Panel A: λ00 = 0.363, p < .001), and a more rapid increase in positive marital quality was associated with a slower rate of cognitive decline (Panel A: λ11 = 1.607, p < .01). Moreover, among men, higher initial levels of negative marital quality were associated with lower initial levels of cognitive function (Panel B: λ00 = −0.425, p < .001), and a more rapid increase in negative marital quality was associated with a faster rate of cognitive decline (Panel B: λ11 = −1.366, p < .05). Neither positive nor negative marital quality was significantly associated with the cognitive trajectories of women.
Table 4.
Effects of Marital Quality on Cognition from Multiple Group Analysis of Latent Growth Curve Models by Gender, HRS 2006-2016, N=7,901
| A. Positive Marital Quality | B. Negative Marital Quality | |||||||
|---|---|---|---|---|---|---|---|---|
| Latent Intercept | Latent Slope | Latent Intercept | Latent Slope | |||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Men (n=4,334) | ||||||||
| Marital quality intercept | 0.363*** | 0.104 | 0.010 | 0.016 | −0.425*** | 0.098 | 0.008 | 0.016 |
| Marital quality slope | 1.607** | 0.612 | −1.366* | 0.653 | ||||
| Means of growth parameters | 12.410*** | 0.777 | −0.133 | 0.125 | 12.574*** | 0.777 | −0.200 | 0.127 |
| Variances in growth parameters | 6.172*** | 0.244 | 0.012 | 0.000 | 6.131*** | 0.243 | 0.012 | 0.000 |
| Women (n=3,567) | ||||||||
| Marital quality intercept | 0.119 | 0.085 | −0.020 | 0.014 | −0.129 | 0.097 | 0.007 | 0.016 |
| Marital quality slope | −0.332 | 0.965 | 0.275 | 1.078 | ||||
| Means of growth parameters | 13.406*** | 0.945 | −0.250 | 0.156 | 13.402*** | 0.945 | −0.233 | 0.139 |
| Variances in growth parameters | 6.090*** | 0.270 | 0.012 | 0.000 | 6.086*** | 0.270 | 0.012 | 0.000 |
| Model fit index | CFI=0.991 | TLI=0.984 | RMSEA=0.019 | CFI=0.990 | TLI=0.983 | RMSEA=0.019 | ||
p<0.001
p<0.01
p<0.05
Sensitivity analysis for reverse causality.
We work from a causal framework to develop our hypothesis that marital quality may affect cognitive trajectories. However, declines in cognitive function are also likely to lead to declines in marital quality. To address this possibility of reverse causality, we conducted additional analyses by running cross-lagged parallel models using the intercept of marital quality to predict the slope of cognition and using the intercept of cognition to predict the slope of marital quality. The results (reported in Appendix A) suggest that initial levels (i.e., intercept) of positive marital quality predict a later change (i.e., slope) in cognition (in particular for men), but initial levels of cognition did not predict a later change in marital quality. These results support our hypothesis that marital quality affects trajectories of cognition instead of vice versa. Nevertheless, we acknowledge that if the respondent was at a later stage of dementia and in need of significant care, marital quality could change in response to cognitive decline. In HRS, these respondents usually had proxy respondents to answer the questions and were not included in our analytic sample.
Discussion
A rich literature has shown that marital quality is significantly associated with a variety of health outcomes, including mental health, physical health, and mortality (Bookwala, 2005; Bulanda et al., 2016; Choi et al., 2016; Liu & Waite, 2014; Robles et al., 2014). Yet few studies have examined the link between marital quality and cognitive health. Using a nationally representative sample of older adults over a period of ten years, our study investigated how positive and negative aspects of marital quality were related to cognitive trajectories. We also explored whether these associations varied by gender. Our findings advance the limited research on marital quality and cognitive health in several respects.
First, consistent with the general literature on marital quality and health outcomes in later life, we found some support for our hypothesis that higher initial levels of positive marital quality would be significantly associated with better initial cognition and that higher initial levels of negative marital quality would be associated with worse initial cognition among these older adults. The life course approach emphasizes the importance of context when considering the links between health and the social world (Dannefer, 2003). Marital quality is one of the key factors that define life course contexts. Our results suggest that both the stress and the support processes operating within marriage are related to individuals’ cognitive health. However, neither initial levels of positive marital quality nor initial levels of negative marital quality were associated with the rate of cognitive decline over time in our sample. This is consistent with the findings in a recent study by Zahodne and colleagues (2019) showing no evidence that baseline marital quality shapes subsequent memory decline.
Second, we went beyond baseline marital quality to examine changes in marital quality over time in relation to cognitive trajectories; we found that the association between marital quality and cognitive trajectories varied by gender. Specifically, we found that the marital quality trajectory was significantly associated with men’s cognitive trajectories but not women’s. Among men, an increase in positive marital quality was associated with a slower rate of cognitive decline, while an increase in negative marital quality was associated with a faster rate of cognitive decline. This finding among men is consistent with the general literature on marital quality and health as well as our hypothesis that positive marital quality is conducive to health and negative marital quality undermines health. Yet, it is puzzling that such an association is absent among women. Previous empirical research on marital quality, gender, and health has been mixed: some studies have reported that women were more sensitive to marital strain and that their health was also more negatively impacted by low marital quality (Bulanda et al., 2016; Kiecolt-Glaser & Newton, 2001), while others have found that marital quality affected health similarly for men and women (Robles et al., 2014; Umberson et al., 2006). Only one previous study has examined gender differences in cognitive health in relation to marital quality, and no gender difference was found (Xu et al., 2016). Such limited and mixed findings call for more research in this important area.
Why does marital quality matter to older men’s cognition but not older women’s? A possible explanation is that men’s well-being relies more on wives’ support while women’s well-being mainly benefits from a larger network outside of marriage (Bernard, 1972; Simon, 2002). A growing body of literature has found that marital loss (divorce and widowhood) has more negative effects on dementia risk for men than for women (Liu et al., 2020; Feng et al., 2014). Researchers suggest that in traditional marriages, women are usually the kin-keepers in the family, offer emotional support to their husbands, and also often monitor their husbands’ health, and thus the loss of a spouse is more damaging to men’s social networks and social support; such damage is associated with risk of cognitive impairment and dementia (Liu et al., 2020). A similar argument can be made to explain the gendered effects of marital quality on cognitive decline. It is possible that in later life, older men may rely more on their spouses for emotional support and cognitive stimulation due to their small circle of intimate ties, while women usually have larger social networks and rely less on their spouses. Therefore, low marital quality may be more consequential for men’s cognitive health, because if men do not receive emotional support from their spouse, they may not have another source of such support. On the other hand, women in low-quality marriages may still have access to a large network of family and friends for social support and social interactions that protect their cognition and compensate for the negative effects of low marital quality.
Our study has several limitations. First, our data were constrained by the way marital quality measures were collected in the HRS. Unlike cognitive measures, which were collected every two years, marital quality was measured only every four years. Therefore, we only had three waves of data on marital quality during our study period. A longer follow-up would lead to better modeling of marital quality trajectories over time. Second, our sample is selective of older adults who remained married during the study period. Those who experienced worse marital quality are more likely to have become divorced or widowed and thus be excluded from the analysis. In this sense, our sample is selective of relatively higher-quality marriages and may have excluded vulnerable respondents, and the results may underestimate the potential negative effects of marital strain on cognitive health. Because women are more likely to initiate divorce (Kalmijn & Poortman, 2006), especially in cases of gray divorce, women in extremely low-quality marriages were more likely to be excluded from our sample. This selection effect may bias our findings to some extent, especially for women. Despite these limitations, our study has notable strengths. We used a large national sample of older adults and a relatively long follow-up study of cognition and marital quality. We also examined both positive and negative marital quality and found gender differences in the link between marital quality and cognitive decline.
Conclusions
A substantial body of literature suggests that marital quality matters for a variety of health outcomes, including mental health, physical health, and mortality (Bulanda et al., 2016; Kiecolt-Glaser et al., 2005; Robles et al., 2014). Our study extends this literature by showing that both positive and negative dimensions of marital quality were associated with trajectories of cognitive function for men but not for women in later life in a large, nationally representative sample of older adults. This finding suggests that older men who experience a decline in marital quality may be at comparatively high risk of cognitive decline. It also suggests that reducing marital strain and improving marital quality may protect cognitive health in later life, especially for older men. Future studies should further explore specific mechanisms underlying the association between marital quality and cognitive health with attention to gender variations.
Marital quality is associated with men’s cognitive trajectories but not women’s.
An increase in positive marital quality is associated with slower cognitive decline for older men.
An increase in negative marital quality is associated with faster cognitive decline for older men.
Older men with a decline in marital quality may be a vulnerable group for cognitive decline.
Acknowledgments
This study was supported by the National Institute on Aging, Grants R01AG061118 and R03AG062936.
Appendix A.
Table A1.
Results from Cross-Lagged Parallel Growth Curve Models of Marital Quality (MQ) and Cognition, HRS 2006-2016
| Positive Marital Quality | Negative Marital Quality | |||
|---|---|---|---|---|
| Cognition slope | MQ slope | Cognition slope | MQ slope | |
| Total sample (N=7,901) | ||||
| MQ intercept | 0.004 (0.010) | −0.008 (0.010) | ||
| Cognition intercept | 0.001 (0.001) | −0.001 (0.001) | ||
| Men (n=4,334) | ||||
| MQ intercept | 0.030* (0.015) | −0.016 (0.015) | ||
| Cognition intercept | 0.001 (0.001) | −0.002 (0.001) | ||
| Women (n=3,567) | ||||
| MQ intercept | −0.013 (0.013) | −0.001 (0.015) | ||
| Cognition intercept | 0.000 (0.001) | 0.000 (0.001) | ||
Note: Each model controls for all covariates. Standard errors in parenthesis.
p < .05
Footnotes
The Authors declared that there is no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bernard J (1972). The future of marriage. New York: World. [Google Scholar]
- Bookwala J (2005). The role of marital quality in physical health during the mature years. Journal of Aging and Health, 17(1), 85–104. doi: 10.1177/0898264304272794 [DOI] [PubMed] [Google Scholar]
- Brown SL, & Wright MR (2017). Marriage, cohabitation, and divorce in later life. Innovation in Aging, 1(2), igx015. doi: 10.1093/geroni/igx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulanda JR, Brown JS, & Yamashita T (2016). Marital quality, marital dissolution, and mortality risk during the later life course. Social Science & Medicine, 165, 119–127. doi: 10.1016/j.socscimed.2016.07.025 [DOI] [PubMed] [Google Scholar]
- Carr D, Cornman JC, & Freedman VA (2016). Marital quality and negative experienced well-being: An assessment of actor and partner effects among older married persons. The Journals of Gerontology: Series B, 71(1), 177–187. doi: 10.1093/geronb/gbv073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Freedman VA, Cornman JC, & Schwarz N (2014). Happy marriage, happy life? Marital quality and subjective well-being in later life. Journal of Marriage and the Family, 76(5), 930–948. doi: 10.1111/jomf.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, & Springer KW (2010). Advances in families and health research in the 21st century. Journal of Marriage and Family, 72(3), 743–761. doi: 10.1111/j.1741-3737.2010.00728.x [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2011). Cognitive impairment: A call for action, now! https://www.cdc.gov/aging/pdf/cognitive_impairment/cogimp_poilicy_final.pdf
- Centers for Disease Control and Prevention. (2019). Subjective cognitive decline—a public health issue. Retrieved from https://www.cdc.gov/aging/aginginfo/subjective-cognitive-decline-brief.html
- Choi H, Yorgason JB, & Johnson DR (2016). Marital quality and health in middle and later adulthood: Dyadic associations. The Journals of Gerontology: Series B, 71(1), 154–164. doi: 10.1093/geronb/gbu222 [DOI] [PubMed] [Google Scholar]
- Costa-Cordella S, Arevalo-Romero C, Parada FJ, & Rossi A (2021). Social Support and Cognition: A Systematic Review. Front Psychol, 12, 637060. doi: 10.3389/fpsyg.2021.637060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, & Kim JK (2016). Change in cognitively healthy and cognitively impaired life expectancy in the United States: 2000-2010. SSM-Population Health, 2, 793–797. doi: 10.1016/j.ssmph.2016.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannefer D (2003). Cumulative advantage/disadvantage, and the life course: Cross-fertilizing age and social science theory. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(6), S327–37. [DOI] [PubMed] [Google Scholar]
- Dehle C, Larsen D, & Landers JE (2001). Social support in marriage. American Journal of Family Therapy, 29(4), 307–324. [Google Scholar]
- Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB Sr, & Benjamin EJ (2007). Marital status, marital strain, and risk of coronary heart disease or total mortality: the Framingham Offspring Study. Psychosomatic Medicine, 69(6), 509–513. [DOI] [PubMed] [Google Scholar]
- Feng L, Ng XT, Yap P, Li J, Lee TS, Hakansson K, … & Ng TP (2014). Marital status and cognitive impairment among community-dwelling Chinese older adults: the role of gender and social engagement. Dementia and Geriatric Cognitive Disorders Extra, 4(3), 375–384. doi: 10.1159/000358584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles LC, Anstey KJ, Walker RB, & Luszcz MA (2012). Social networks and memory over 15 years of followup in a cohort of older Australians: results from the Australian longitudinal study of ageing. Journal of Aging Research, 2012. doi: 10.1155/2012/856048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glymour MM, & Manly JJ (2008). Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychology Review, 18(3), 223–254. doi: 10.1007/s11065-008-9064-z [DOI] [PubMed] [Google Scholar]
- Hughes TF, & Ganguli M (2009). Modifiable midlife risk factors for late-life cognitive impairment and dementia. Curr Psychiatry Rev, 5(2), 73–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessen F, Amariglio RE, Van Boxtel M, Breteler M, Ceccaldi M, Chételat G, … & Subjective Cognitive Decline Initiative. (2014). A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer's disease. Alzheimer's & Dementia, 10(6), 844–852. doi: 10.1016/j.jalz.2014.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson L, Guo X, Waern M, Östling S, Gustafson D, Bengtsson C, & Skoog I (2010). Midlife psychological stress and risk of dementia: a 35-year longitudinal population study. Brain, 133(8), 2217–2224. doi: 10.1093/brain/awq116 [DOI] [PubMed] [Google Scholar]
- Hayes V, Demirkol A, Ridley N, Withall A, & Draper B (2016). Alcohol-related cognitive impairment: Current trends and future perspectives. Neurodegenerative Disease Management, 6(6), 509–523. [DOI] [PubMed] [Google Scholar]
- Henckens MJ, Hermans EJ, Pu Z, Joëls M, & Fernández G (2009). Stressed memories: how acute stress affects memory formation in humans. Journal of Neuroscience, 29(32), 10111–10119. doi: 10.1523/JNEUROSCI.1184-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, & Waite LJ (2009). Marital biography and health at mid-life. Journal of Health and Social Behavior, 50(3), 344–358. doi: 10.1177/002214650905000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn M, & Poortman AR (2006). His or her divorce? The gendered nature of divorce and its determinants. European sociological review, 22(2), 201–214. [Google Scholar]
- Kelly ME, Duff H, Kelly S, Power JEM, Brennan S, Lawlor BA, & Loughrey DG (2017). The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Systematic reviews, 6(1), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, & Glaser R (2005). Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry, 62(12), 1377–1384. doi: 10.1001/archpsyc.62.12.1377 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, & Newton TL (2001). Marriage and health: His and hers. Psychological Bulletin, 127(4), 472–503. doi: 10.1037/0033-2909.127.4.472 [DOI] [PubMed] [Google Scholar]
- King V, & Scott ME (2005). A comparison of cohabiting relationships among older and younger adults. Journal of Marriage and Family, 67(2), 271–285. doi: 10.1111/j.0022-2445.2005.00115.x [DOI] [Google Scholar]
- Kuhlmann S, Piel M, & Wolf OT (2005). Impaired memory retrieval after psychosocial stress in healthy young men. Journal of Neuroscience, 25(11), 2977–2982. doi: 10.1523/JNEUROSCI.5139-04.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin H, & Stoeckel KJ (2016). Social network, activity participation, and cognition: A complex relationship. Research on aging, 38(1), 76–97. [DOI] [PubMed] [Google Scholar]
- Liu H, & Waite L (2014). Bad marriage, broken heart? Age and gender differences in the link between marital quality and cardiovascular risks among older adults. Journal of Health and Social Behavior, 55(4), 403–423. doi: 10.1177/0022146514556893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Waite L, & Shen S (2016). Diabetes risk and disease management in later life: A national longitudinal study of the role of marital quality. The Journals of Gerontology: Series B, 71(6), 1070–1080. doi: 10.1093/geronb/gbw061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Zhang Y, Burgard SA, & Needham BL (2019). Marital status and cognitive impairment in the United States: evidence from the National Health and Aging Trends Study. Annals of Epidemiology, 38, 28–34. doi: 10.1016/j.annepidem.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Zhang Z, Choi SW, & Langa KM (2020). Marital status and dementia: Evidence from the Health and Retirement Study. The Journals of Gerontology: Series B, 75(8), 1783–1795. doi: 10.1093/geronb/gbz087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2015). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Oei NY, Elzinga BM, Wolf OT, de Ruiter MB, Damoiseaux JS, Kuijer JP, Veltman DJ, Scheltens P, & Rombouts SA (2007). Glucocorticoids decrease hippocampal and prefrontal activation during declarative memory retrieval in young men. Brain Imaging and Behavior, 1(1-2), 31–41. doi: 10.1007/s11682-007-9003-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA III, Chamey D, & Southwick S (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont), 4(5), 35. [PMC free article] [PubMed] [Google Scholar]
- Pillai JA, & Verghese J (2009). Social networks and their role in preventing dementia. Indian Journal of Psychiatry, 51(Suppl1), S22. [PMC free article] [PubMed] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, & McGinn MM (2014). Marital quality and health: a meta-analytic review. Psychological Bulletin, 140 (1), 140. doi: 10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman SM, & Mattson MP (2010). Adverse stress, hippocampal networks, and Alzheimer’s disease. Neuromolecular Medicine, 12(1), 56–70. doi: 10.1007/s12017-009-8107-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servais M (2010). Overview of HRS public data files for cross-sectional and longitudinal analysis. Retrieved from Ann Arbor, Michigan: https://hrs.isr.umich.edu/sites/default/files/biblio/OverviewofHRSPublicData.pdf [Google Scholar]
- Simon RW (2002). Revisiting the relationships among gender, marital status, and mental health. American Journal of Sociology, 107(4), 1065–1096. doi: 10.1086/339225 [DOI] [PubMed] [Google Scholar]
- Shankar A, Hamer M, McMunn A, & Steptoe A (2013). Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosomatic Medicine, 75(2), 161–170. doi: 10.1097/PSY.0b013e31827f09cd [DOI] [PubMed] [Google Scholar]
- Smith J, Ryan L, Sonnega A, & Weir D (2017). Psychosocial and lifestyle questionnaire 2006–2016. Ann Arbor, MI: Survey Research Center, Institute for Social Research. [Google Scholar]
- Sommerlad A, Ruegger J, Singh-Manoux A, Lewis G, & Livingston G (2018). Marriage and risk of dementia: Systematic review and meta-analysis of observational studies. Journal of Neurology, Neurosurgery, and Psychiatry, 89, 231–238. doi: 10.1136/jnnp-2017-316274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundstrom A, Westerlund O, & Kotyrlo E (2016). Marital status and risk of dementia: A nationwide population-based prospective study from Sweden. BMJ Open, 6(1). doi: 10.1136/bmjopen-2015-008565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan GE, & Lessov-Schlaggar CN (2007). The effects of tobacco smoke and nicotine on cognition and the brain. Neuropsychology Review, 17(3), 259–273. [DOI] [PubMed] [Google Scholar]
- Thomas PA, & Umberson D (2018). Do older parents’ relationships with their adult children affect cognitive limitations, and does this differ for mothers and fathers? Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(6), 1133–1142. 10.1093/geronb/gbx009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Donnelly R, & Pollitt AM (2018). Marriage, social control, and health behavior: A dyadic analysis of same-sex and different-sex couples. Journal of health and social behavior, 59(3), 429–446. 10.1177/0022146518790560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, & Needham B (2006). You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior, 47(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite LJ, & Gallagher M (2000). The case for marriage: Why married people are happier, healthier, and better off financially. New York: Broadway Books. [Google Scholar]
- Xu M, Thomas PA, & Umberson D (2016). Marital quality and cognitive limitations in late life. The Journals of Gerontology: Series B, 71(1), 165–176. doi: 10.1093/geronb/gbv014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu YL, & Liu H (2020). Marital Quality and Salivary Telomere Length Among Older Men and Women in the United States. Journal of Aging and Health. doi: 10.1177/0898264320980250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne LB, Ajrouch KJ, Sharifian N, & Antonucci TC (2019). Social relations and age-related change in memory. Psychology and Aging, 34(6), 751. doi: 10.1037/pag0000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, & Hayward MD (2006). Gender, the marital life course, and cardiovascular disease in late midlife. Journal of Marriage and Family, 68(3), 639–657. doi: 10.1111/j.1741-3737.2006.00280.x [DOI] [Google Scholar]
- Zunzunegui MV, Alvarado BE, Del Ser T, & Otero A (2003). Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. The Journals of Gerontology: Series B, 58(2), S93–S100. doi: 10.1093/geronb/58.2.S93 [DOI] [PMC free article] [PubMed] [Google Scholar]


