Abstract
The Coronavirus disease 2019 (COVID-19) has been spreading worldwide with rapidly increased number of deaths. Hyperinflammation mediated by dysregulated monocyte/macrophage function is considered to be the key factor that triggers severe illness in COVID-19. However, no specific targeting molecule has been identified for detecting or treating hyperinflammation related to dysregulated macrophages in severe COVID-19. In this study, previously published single-cell RNA-sequencing data of bronchoalveolar lavage fluid cells from thirteen COVID-19 patients were analyzed with publicly available databases for surface and imageable targets. Immune cell composition according to the severity was estimated with the clustering of gene expression data. Expression levels of imaging target molecules for inflammation were evaluated in macrophage clusters from single-cell RNA-sequencing data. In addition, candidate targetable molecules enriched in severe COVID-19 associated with hyperinflammation were filtered. We found that expression of SLC2A3, which can be imaged by [18F]fluorodeoxyglucose, was higher in macrophages from severe COVID-19 patients. Furthermore, by integrating the surface target and drug-target binding databases with RNA-sequencing data of severe COVID-19, we identified candidate surface and druggable targets including CCR1 and FPR1 for drug delivery as well as molecular imaging. Our results provide a resource in the development of specific imaging and therapy for COVID-19-related hyperinflammation.
Subject terms: Infectious diseases, Inflammation, Diagnostics, Target identification, Diagnostic markers, Infectious diseases
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection has led to over 1,100,000 deaths worldwide as of October 18, 20201. The Chinese Centers for Disease Control and Prevention analyzed the characteristics of 72,314 cases of COVID-19 and reported that disease severity varies widely, with 81% of patients experiencing mild disease, 14% developing severe disease, and 5% developing critical disease that is characterized by respiratory and/or multiorgan failure2, 3. In most cases, severe/critical disease develops within 2 weeks after symptom onset4, and in a recent study, it was reported that the mortality of patients undergoing mechanical ventilation was 88.1%4, 5. Therefore, efforts to identify and manage patients who are at high risk of developing severe illness are urgently needed.
Hyperinflammation mediated by dysregulated macrophages is considered to be the key factor causing severe disease in patients with severe COVID-19 based on observations of macrophages in the alveolar lumina and increased cytokine levels in severe COVID-19 patients6, 7. Recently, targeted probes based on small molecules and antibodies have contributed to precise diagnosis and treatment in various inflammatory and infectious diseases8,9. Nonetheless, which molecular targets might be utilized in imaging and drug delivery for hyperinflammation in severe COVID-19 has not been investigated. Molecular imaging to detect characteristic hyperinflammation by a dysregulated immune response has the potential to predict the progression of severe COVID-19. Furthermore, a drug delivery system to target specific immune cells that cause hyperinflammation in severe COVID-19 might allow precise immune modulation and greatly impact patient survival.
In this study, we employed previously published single-cell RNA-sequencing (scRNA-seq) data based on bronchoalveolar lavage (BAL) fluid cells of healthy controls and COVID-19 patients for a data-mining study. It was analyzed along with three different databases, the Surfaceome database10, the Database of Imaging Radiolabeled Compounds (DIRAC)11, and BindingDB12, to identify feasible targets for molecular imaging and therapy in severe COVID-19.
Materials and methods
Preprocessing scRNA-seq data
scRNA-seq data for BAL fluid were downloaded from the Gene Expression Omnibus database (GSE145926). Patient data we used were acquired by a publicly available dataset that removed patient identifiers. The original datasets were approval-free to use based on public databases. The scRNA-seq data of each sample were preprocessed to exclude low-quality cells and check the mitochondrial genome using the PercentageFeatureSet function of the Seurat package. The cells were filtered for the analysis with cut-off values: expression of at least 200 genes and at most 6000 genes to exclude cell duplets, total counts more than 1000 counts, and less than 10% of transcripts of mitochondrial genes. Data were then scaled by log-normalization after the read counts were divided by the total number of transcripts and multiplied by 10,000. Highly variable 2,000 genes were selected using the FindVariableFeatures function of the Seurat package (version 3.0)13. Subsequently, the data of each sample were integrated using the FindIntegrationAnchors and IntegrateData function of the Seurat package. Data were then scaled to z-scores with regression of total cellular read counts and mitochondrial read counts. Cell types were determined by the graph-based clustering approach implemented by the FindClusters function of the Seurat package. Before clustering, dimension reduction was performed by principal component analysis, and 50 dimensions were used for clustering. The conservative resolution was set to 1.2.
Clustering cells into each immune cell type
The FindAllMarkers function of the Seurat package was used to identify marker genes of the clusters, and high-ranked marker genes according to the fold-change were identified for each cluster with Wilcoxon rank sum test and likelihood-ratio test. For data visualization, the scRNA-seq data were embedded into two-dimensional projection, t-stochastic neighborhood embedding (t-SNE). The expression levels of known marker genes, CD68, FCGR3B, CD79A, LILRA4, KLRD1, CD3D, KRT18, and CD1C (Supplementary Fig. S1), were assessed to identify cell types, and each cluster was classified into nine cell types based on the expression level: T-cell, B-cell, natural killer (NK) T-cell, epithelial cell, neutrophil, myeloid dendritic cell, plasmacytoid dendritic cell, and macrophage.
Evaluating expression of alleged imaging targets
We selected molecular targets and matched imaging tracers among metabolism-related tracers: glucose transporters (GLUT)/2-[18F]-fluoro-2-deoxy-d-glucose ([18F]FDG)14, monocarboxylate transporters (MCT)/[11C]-acetate15, folate receptors (FOLR)/[18F]-labeled folic acid derivatives16, and L-type amino acid transporter 1/[11C]-methionine17. Furthermore, target molecules for macrophage imaging and matched imaging tracers were selected: translocator protein (TSPO)/[11C]-PBR2818 and mannose receptor 1 (MRC1)/2-deoxy-2-[18F]-fluoro-D-mannose19. The expression levels of other imaging target molecules were also examined: somatostatin receptor subtype-2 (SSTR2)/[68Ga]-DOTA-TATE20, fibroblast-activated protein (FAP)/[68Ga]-fibroblast-associated protein inhibitor21 considering pulmonary fibrosis of COVID-1922, alpha-v-beta-3 integrin (ITGAV)/arginylglycylaspartic acid (RGD)23, CD8 + T-cells/[89Zr]-radiolabeled human CD8-specific minibody24, and granzyme B (GZMB)/[68Ga]-NOTA-GZP25. We obtained expression level of selected imaging targets.
Additionally, we used Reactome to select genes of glycolysis and oxidative phosphorylation (OXPHOS) pathways to examine the overall activity of metabolic pathways26. The metabolic enrichment scores of each cell were estimated by the AddModuleScore function of the curated gene sets of both pathways to define the metabolic profiles of each sample. t-SNE plots and violin plots were generated using Seurat. Expression of imaging targets and enrichment scores of metabolic pathways were compared using a Kruskal–Wallis test. For each cluster of cells, feature scores of severe, moderate COVID-19 and healthy controls were compared. A p-value < 0.05 was considered significant (two tailed).
Exploration of target molecules in open access databases
We hypothesized that an ideal target for imaging and targeted therapy of COVID-19 would have the following characteristics: (1) highly expressed in severe COVID-19, (2) expressed on the cell surface, and (3) the existence of binding molecules. Thus, we utilized three different databases: the Surfaceome database10, the DIRAC11, and BindingDB12. The Surfaceome database was constructed using publicly available data on genes to catalog all those known to (or likely to) encode cell surface proteins (www.rdm.ox.ac.uk/research/rabbitts-group); because they can be targeted by ligands or antibodies, surface proteins associated with severe COVID-19 hyperinflammation may be candidates for imaging and therapy targets. DIRAC is an open-access positron emission tomography (PET) radiotracer database that provides [18F]-radiolabeled compounds with associated specific molecules (http://www.iphc.cnrs.fr/dirac/). BindingDB is a database of drug targets with small molecules binding to specific proteins (https://www.bindingdb.org/).
Venn diagrams were used to display the numbers of marker genes enriched in the specific macrophage subtypes, surface protein-encoding mRNA from the Surfaceome database, and target proteins from the DIRAC. Among markers of each cell cluster, surface markers were selected by Surfaceome, and the top 10 surface targets according to the fold change were selected. The surface markers between different clusters were then compared.
Additional study in supplementary datasets
Two other datasets were employed for validation study, GSE147143 and GSE149689. The former dataset contains scRNA-seq of BAL fluid from three severe COVID-19 patients27. The latter dataset contains scRNA-seq of peripheral blood mononuclear cells (PMBCs) from four healthy donors, five influenza patients, and eight COVID-19 patients28. Among the latter dataset, scRNA-seq from healthy donors and COVID-19 patients were selected. Pre-processing was performed in the same way as described above, except that the resolution was set to 0.3. The resolution was set as lower value to obtain appropriate number of clusters to characterize each cluster. In the former dataset, six markers were used to cluster immune cells and epithelial cells: CD68, FCGR3B, KLRD1, CD3D, KRT7, and TPPP3 (Supplementary Fig. S2a). In the latter dataset, six markers were used to cluster immune cells, platelet, and erythrocyte: CD68, CD6, HBB, KLRD1, PPBP, and MS4A1 (Supplementary Fig. S3a). Expression of candidate proteins for imaging and therapeutic targets were evaluated in each dataset. All statistical analyses were performed using the R program (v 3.6.1).
Results
Composition of immune cells in BAL fluid
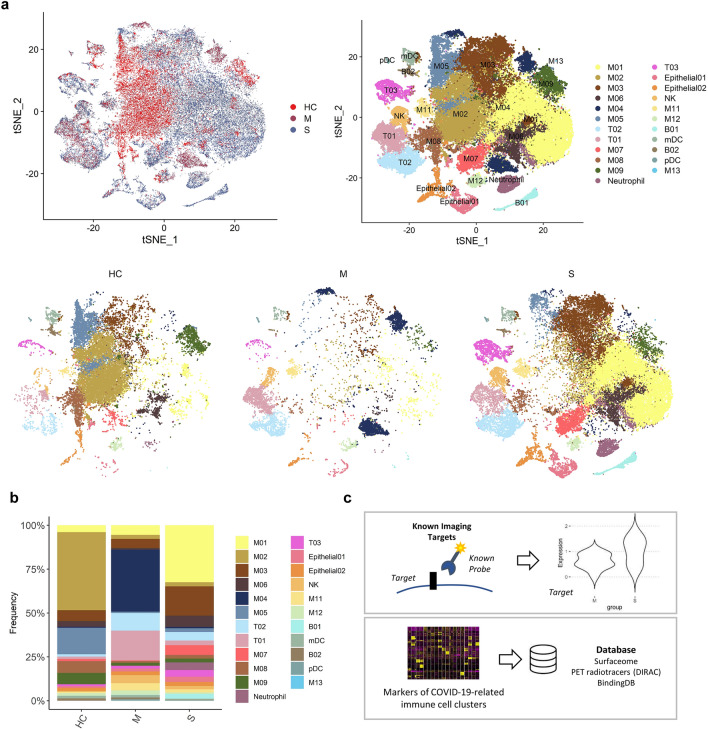
scRNA-seq data of BAL fluid cells were obtained from three patients with moderate COVID-19, six patients with severe/critical COVID-19, and four healthy controls (Gene Expression Omnibus database, accession number GSE145926)29. BAL fluid cells were classified into 21 clusters according to expression of cell-type specific marker genes (Fig. 1a, Supplementary Fig. S1). We explored the cell subpopulation of each group and identified a substantial difference in the composition of immune cells between the three groups (Fig. 1b). The majority of cells in BAL fluid were composed of different types of macrophages in the three groups. T-cells were more abundant in the moderate COVID-19 group than in the severe COVID-19 group. In contrast, neutrophils, NK T-cells, and plasma cells were more abundant in the severe COVID-19 group than in the moderate COVID-19 group. The composition of macrophage subpopulations differed between the three groups: 1) in the healthy control group, a cluster of macrophages, M02, was the most abundant subpopulation; 2) in moderate COVID-19, M04 was the most abundant cluster; and 3) in severe COVID-19, M01 and M03 were the two most dominant cell types.
Figure 1.
Bronchoalveolar immune landscape of COVID-19 patients and overview of the study design. (a) t-SNE projection of major cell type clusters in BAL fluid according to the severity of COVID-19 infection. Each point represents a single cell, and color coding of each patient group (upper left) and cell type population (upper right) are shown adjacent (HC = healthy control; M = moderate COVID-19 infection; S = severe COVID-19 infection). (b) The composition of major cell types per patient group. (c) Workflow for targetable molecule discovery in severe COVID-19 patients. We analyzed the expression level of potential imaging targets for COVID-19 patients. Additionally, we explored the marker genes of COVID-19-related immune cell clusters from three public databases (Surfaceome database, PET tracer database, and BindingDB).
We utilized the following two different approaches to discover potential targets to image and/or modulate the dysregulated immune system in severe COVID-19: 1) evaluating the expression levels of alleged imaging targets for inflammation and 2) exploring markers filtered by targetable molecules based on publicly available databases (Fig. 1c).
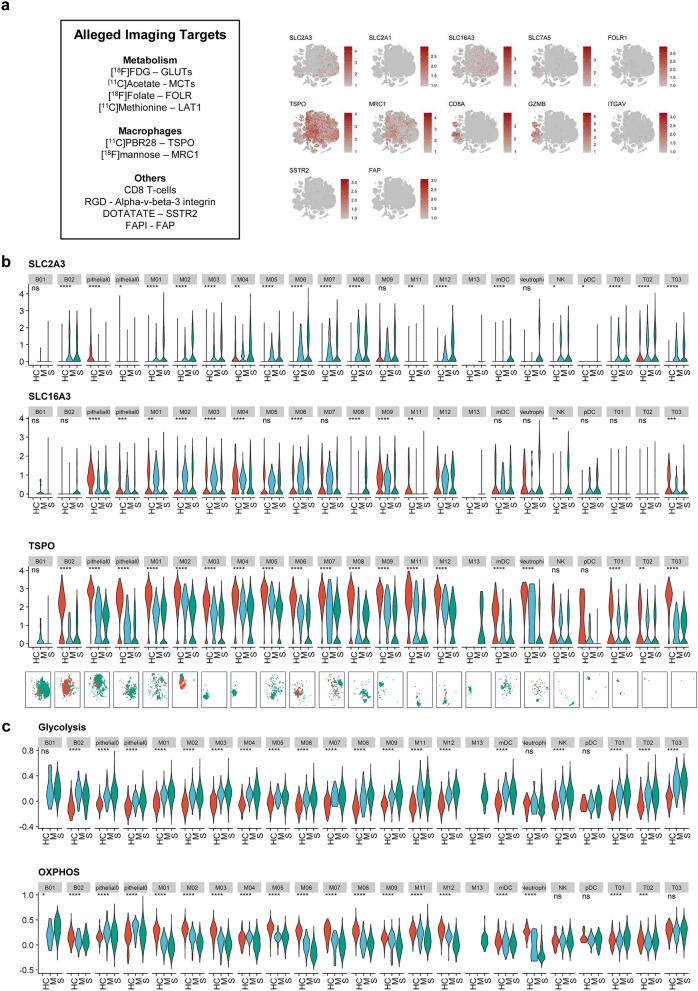
Evaluating expression levels of alleged imaging targets
All selected molecular targets were projected onto a t-distributed stochastic neighbor embedding (t-SNE) plot depicting 21 immune cell clusters of all patients, and macrophages enriched in severe COVID-19 patients were marked separately (Fig. 2a). The expression levels of molecular targets were scattered separately for cells from healthy controls, moderate COVID-19, and severe COVID-19 for each immune cell cluster. SLC2A1 (GLUT1) showed low expression across the immune cell clusters, whereas SLC16A3 (MCT4) was highly expressed in macrophage clusters. To analyze whether molecular targets are able to distinguish the severity of COVID-19 infection, we compared the expression level of each target between the groups (Fig. 2b, Supplementary Fig. S4). We found that SLC2A3 (GLUT3) was increased in macrophage clusters enriched in severe COVID-19 patients. TSPO and MRC1 were highly expressed in macrophage clusters enriched in healthy controls and moderate COVID-19 patients. GZMB was highly expressed in CD8 + T-cells and NK T-cells of the severe COVID-19 group. As we found that GLUT3 was associated with M01 and M03 clusters, two dominant macrophage subtypes in severe COVID-19, we further analyzed enrichment scores for glycolysis and OXPHOS pathways to explore the characteristics of glucose utilization in severe COVID-19 (Fig. 2c). Interestingly, in most immune cells, including T-cells and macrophages, enrichment scores of glycolysis were higher in the severe COVID-19 group than in the moderate and healthy control groups. In neutrophil and macrophage clusters, scores of OXPHOS were lower in the severe group than in the moderate and healthy control groups. As [18F]FDG uptake is determined by expression levels of GLUTs and hexokinase, the initial enzyme of glycolysis, we assume that [18F]FDG PET can be used for the identification of immune cells associated with severe COVID-19.
Figure 2.
Potentially alleged imaging marker molecules of COVID-19 and metabolic pathways. (a) t-SNE plots showing the expression of several potentially alleged imaging targets on BAL fluid immune cells. The markers indicate the heterogeneous pattern of expression across the immune cells. The last panel indicates subtypes of macrophages abundant in severe COVID-19 patients. (b) Expression levels of SLC2A3, SLC16A3, and TSPO across cell clusters of three groups. (ns: p > 0.05; *p < = 0.05; **p < = 0.01; ***p < = 0.001; ****p < = 0.0001) (HC = healthy control; M = moderate COVID-19; S = severe COVID-19) t-SNE plots on the bottom panels show the distribution of each immune cell cluster. (red dot = HC; blue dot = M; green dot = S) (c) Enrichment scores of glycolysis and oxidative phosphorylation (OXPHOS) pathways across cell clusters of three groups.
Exploration of ideal targets of severe COVID-19 hyperinflammation
Based on the proportions of immune cells within each group (Fig. 1b), we considered M01/M03, M04, and M02 as specific macrophage subtypes for the severe COVID-19, moderate COVID-19, and healthy control groups, respectively. Targetable marker proteins of the M01, M02, M03, and M04 clusters were explored with two different methods, Wilcoxon rank sum test and likelihood-ratio test. Subsequently, we identified specific targetable proteins included in both the Surfaceome and PET tracer databases. SLC3A2 and SLC2A3 in the M01 cluster and FOLR2 in the M03 cluster were identified in results from both methods, indicating that [18F]FDG and [18F]-labeled folic acid derivatives may be useful for imaging severe COVID-19 (Fig. 3a).
Figure 3.
Discovery of targetable marker protein of severe COVID-19. (a) Venn diagrams representing intersection between markers for specific subtype of macrophages of each patient group (M01 and M03 for severe COVID-19, M04 for moderate COVID-19, and M02 for healthy control), the Surfaceome database, and the PET tracer database. In DEG analysis by both Wilcoxon test and likelihood-ratio test, the targetable surface proteins were SLC43A2 and SLC2A3 for M01 and FOLR2 for M03. HRH2 was selected as a targetable surface protein in DEG analysis by Wilcoxon test. On the contrary, FLT1 was selected in DEG analysis by likelihood-ratio test. (b) A dot plot representing expression of the top 10 surface markers in specific macrophage subtypes. The dot size represents the fraction of cells expressing a specific marker in a particular cluster, and the intensity of color indicates the average expression in that cluster. (c) FPR1, which is mostly expressed in the M01 cluster, is suggested as an example of a potential imaging and surface target for severe COVID-19 patients. For the left panel, t-SNE plots represent cells acquired from healthy controls and moderate and severe COVID-19 patients, respectively.
Additionally, the top 10 surface markers of M01, M02, M03, and M04 selected by fold-changes were visualized by the average expression level and proportions of transcripts-expressing cells (Fig. 3b). Notably, a few surface molecules enriched in M01/M03 among the top 10 surface markers correspond to drug targets in the BindingDB, including CCR1, FPR1, and GPR183. FPR1 was higher in the severe COVID-19 group than in the healthy control and moderate groups (Fig. 3c). The specific peptide ligand of FPR1, cinnamoyl-F-(D)L-F-(D)L-F (cFLFLF), has been used for imaging inflammation30 and targeted drug delivery conjugated with nanoparticles31 (Fig. 3c). Thus, we suggest that cFLFLF-based imaging or drug delivery systems can be utilized for imaging and therapy of severe COVID-19. Additionally, there are 1155 and 22 ligand candidates for CCR1 and GPR183, surface targets enriched in severe COVID-19, in BindingDB, respectively. All markers of M01, M02, M03, and M04 with surface targets, PET database and targeting drug candidates are summarized in Supplementary Table S1. Accordingly, for M01/M03 subtypes, 154 surface target candidates, nine [18F]-labeled radiotracers, and 132 molecules associated with drug targets were identified, warranting further evaluation for utilization in imaging and therapy of severe COVID-19.
Additional study in supplementary datasets
Among markers suggested above, five markers were selected for additional study: SLC2A3, FOLR2, CCR1, FPR1, and GPR183. In scRNA-seq data from GSE147143 dataset (BAL fluid of severe COVID-19 patients), SLC2A3, CCR1, and FPR1 were highly expressed in the macrophage and neutrophil clusters. GPR183 was highly expressed in the macrophage cluster (Supplementary Fig. S2b). In scRNA-seq data from GSE149689 dataset (PBMCs of COVID-19 patients), there was a specific myeloid cell cluster (My04) was identified in severe COVID-19 patients (Supplementary Fig. S3b). Especially, SLC2A3 and FPR1 were expressed highly in the My04 cluster (Supplementary Fig. S3c).
Discussion
COVID-19 is a novel viral infection disease of which the most representative manifestation is severe pulmonary inflammation4. An excessive inflammatory process is known as a main factor that leads to pulmonary destruction and even death32. Many approaches to treating patients with severe COVID-19 by controlling the immune response using immunomodulators such as dexamethasone, interleukin-6 inhibitors or tumor necrosis factor blockers have been reported33, 34. Currently, COVID-19 patients can be classified into mild, moderate, severe/critical diseases based on clinical symptoms according to the National Health Commission of China guidelines35, and the classification of disease severity in COVID-19 is critical for the grading treatment of patients. Indeed, evaluation of the severity of the immune response is needed to select patients who urgently need anti-inflammatory treatment if the immune modulation strategy becomes an important treatment option for severe COVID-19. Moreover, it might be useful in optimizing the allocation of medical resources and preventing the occurrence of overtreatment and undertreatment in the outbreak of an epidemic. However, to the best of our knowledge, efficient indicators for the severity of COVID-19, therapeutic response, and outcome have not been fully elucidated. Some previous studies have proposed clinical symptoms, laboratory, and radiologic findings as diagnostic tools for the classification of COVID-19 severity36. Our study suggests targetable molecules reflecting the different compositions of immune cells according to the severity of COVID-19, indicating that imaging and therapeutic targeting of specific molecules of hyperinflammation in severe COVID-19 may provide a new feasible strategy of stratification and precision immune modulation in COVID-19.
We explored expression of alleged imaging targets to assess the feasibility of existing molecular imaging probes for inflammation. Notably, SLC2A3 (GLUT3) was highly expressed in macrophages enriched in severe COVID-19 patients. In addition, these macrophages showed enhanced glycolysis and relatively low OXPHOS. These findings support the evaluation of glucose metabolism in inflammatory lesions and can provide information on the immunologic response associated with severe COVID-19. Notably, by reflecting enhanced glucose metabolism in inflammatory cells, particularly macrophages, [18F]FDG PET has been commonly employed in clinical settings for identifying inflammatory or infection foci and evaluating the severity of inflammation37. A recent case series also showed increased FDG uptake in COVID-19-related inflammation in the lungs and lymph nodes38. Our results suggest that [18F]FDG PET can be utilized to stratify COVID-19 patients with severe pulmonary inflammation, as enhanced glucose uptake and glycolysis were found to be associated with subtypes of macrophages in severe COVID-19 compared with moderate disease. Imaging-based characterization has advantages in reflecting the metabolic aspects of macrophages related to severe COVID-19 and evaluating the whole body to localize hyperinflammation. In addition to the pulmonary system, other organs, such as the liver or kidney, can be affected by SARS-CoV-23. Considering the availability of [18F]FDG PET imaging and that can cover the whole body, it can be used for the diagnosis of systemic inflammation caused by SARS-CoV-2. Although further clinical validation is required, the degree of FDG uptake in inflammatory lesions in the lung can be used as a predictable finding of hyperinflammation by suggesting macrophage subtypes with enhanced glucose metabolism.
We further explored candidate molecules for imaging and druggable targets using databases. It is notable that SLC2A3 (GLUT3) was selected in this analysis, and this result indicates that it is a good candidate for targeted imaging reflecting immune cells in severe COVID-19 patients. Other surface molecules associated with druggable targets were also identified; FOLR2 was another candidate imaging target for the severe COVID-19 group. The folate receptor is a molecular target used to diagnose inflammatory diseases39. This result is consistent with a previous animal study that showed the possibility of imaging FOLR2-positive macrophages in acute lung inflammation40. In addition, we focused on surface targets that bind to druggable molecules. CCR1 and FPR1 were highly expressed in macrophages enriched in the severe COVID-19 group. Notably, these proteins were revealed to be highly expressed in myeloid clusters also in the validation studies. Specifically, a study originally published with GSE147143 data showed the neutrophil cluster was associated with severe COVID-19 compared with healthy controls27. The cluster showed high expression of our suggested markers, CCR1, FPR1 as well as SLC2A3. Among them, SLC2A3 and FPR1 demonstrated high expression in the severe COVID-19 in PBMC samples. Specific druggable molecules for these targets are indicated in BindingDB. In particular, FPR1 is a G protein-coupled receptor expressed in macrophages. There is a previous study reporting the feasibility of FPR1 targeted imaging to diagnose macrophage infiltration in inflammatory diseases41. As FPR1 is targeted by small peptides (cFLFLF), it can be applied to active targeting drug delivery systems as well as molecular imaging31. Furthermore, FPR1 is reported to have a role in regulating or modulating the immune response in cancer and inflammation42. As immunomodulation or immunoregulation has recently been emphasized as a treatment strategy in COVID-1943, FPR1 may be an appropriate target not only for assessing disease severity but also for delivering therapeutic drugs. We identified various druggable molecules specifically binding to markers of macrophages enriched in severe COVID-19 (Supplementary Table), and the findings may be used to develop an appropriate drug delivery and imaging platform for precise immune modulation strategies in COVID-19. In other words, the present results indicate that the target molecules explored can be applied to diagnose severe pulmonary inflammation due to SARS-CoV-2 shortly.
We explored candidates of surface target molecules from some subsets of macrophages. It is unclear that macrophages expressing the target protein specifically cause a hyperinflammatory response. However, numbers of M01/M03/M04, which were selected as specific macrophage subsets for the severe COVID-19 and moderate COVID-19 were occupied the majority in each group and patient (Fig. 1b, Supplementary Fig. S3). Thus, the suggested molecules may be useful to identify specific macrophages specifically presenting in COVID-19 patients with hyperinflammation. Additionally, the suggested targetable markers are overlapping with conventional markers such as SLC2A3 or FOLR2. They are expressed in immune cells of other inflammatory diseases. However, our point is not a differential diagnosis of severe COVID-19 from other disease entity but focusing on specific markers in severe inflammation among COVID-19 entity. COVID-19 is primarily diagnosed by PCR examination for viral genome. After identification of SARS-CoV-2, the suggested idea can be applied to stratification or early diagnosis of hyperinflammation.
There are limitations in the present study. Because we analyzed cells from BAL fluid, the results may not be entirely consistent with the immune cell composition or protein expression of the lung tissue itself. Nonetheless, the characteristics or composition of cells in BAL fluid reflect immune cells of the lung associated with inflammation. Thus, targeted imaging of the identified molecules can be applied to in vivo settings. Also, protein expression is not always correlated with level of mRNA transcripts. It is a limitation that this study cannot assure sufficient concentrations of protein expression. Nevertheless, in selection of target proteins, the specificity of protein and presence of targetable tracer are important as well as expression level of protein. If a protein is expressed a lot but non-specifically, it is not appropriate for a candidate of target protein. The significance of this study is that specificity of RNA expression was suggested as a basic knowledge for further development. Further study is warranted to validate protein expression with experimental methods such as flow cytometry.
Taken together, we demonstrate different compositions of immune cells in BAL fluid from healthy controls and COVID-19 patients. The subpopulations of macrophages differed among the three groups. Regarding alleged imaging markers, SLC2A3 was abundant in macrophage subtypes enriched in severe COVID-19 patients, and we identified SLC3A2, SLC2A3, and FOLR2 as candidate molecules as imaging targets. In addition, various molecular targets, including CCR1, FPR1, and GPR183, are suggested as candidates for drug delivery systems as well as imaging. This work provides a resource to develop targeted imaging and therapeutic strategies for severe pulmonary hyperinflammation related to COVID-19.
Supplementary Information
Acknowledgements
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Ministry of Science and ICT, Republic of Korea (No. 2020R1C1C1007105) and by grant no. 2620180060 from the Seoul National University Hospital (SNUH) Research Fund and a grant from the Korea Health Technology Research & Development Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI19C0339).
Author contributions
H.C., K.J.N. designed the study. H.L., J.P., K.J.N., and H.C. performed data analysis. H.J.I. interpreted and critically reviewed results. H.L. wrote the first draft. All authors wrote and revised the manuscript. All authors read and approved the final manuscript.
Data availability
The single-cell RNA-sequencing data can be downloaded from the Gene Expression Omnibus database (https://www.ncbi.nlm.nih.gov/geo/).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hongyoon Choi, Kwon Joong Na, Hyung-Jun Im.
Contributor Information
Hyung-Jun Im, Email: iiihjjj@gmail.com.
Kwon Joong Na, Email: kjna85@gmail.com.
Hongyoon Choi, Email: chy1000@snu.ac.kr.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-93743-2.
References
- 1.WHO. Coronavirus Disease (COVID-19) Weekly Epidemiological Update: 20 October 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed 24 October, 2020).
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages. Nat. Rev. Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson S, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luca C, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect. Dis. 2020;20:1135–1140. doi: 10.1016/S1473-3099(20)30434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diane Marie DV, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020;26:1636–1643. doi: 10.1038/s41591-020-1051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weissleder R, Nahrendorf M, Pittet MJ. Imaging macrophages with nanoparticles. Nat Mater. 2014;13:125–138. doi: 10.1038/nmat3780. [DOI] [PubMed] [Google Scholar]
- 9.Ikoba U, et al. Nanocarriers in therapy of infectious and inflammatory diseases. Nanoscale. 2015;7:4291–4305. doi: 10.1039/C4NR07682F. [DOI] [PubMed] [Google Scholar]
- 10.Bausch-Fluck D, et al. The in silico human surfaceome. Proc. Natl. Acad. Sci. USA. 2018;115:E10988–E10997. doi: 10.1073/pnas.1808790115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchand P, Bekaert V, Ouadi A, Laquerriere P, Brasse D. Forty years of F-18-labeled compound development in an open access database. J. Nucl. Med. 2013;54:15. [Google Scholar]
- 12.Liu T, Lin Y, Wen X, Jorissen RN, Gilson M. BindingDB: A web-accessible database of experimentally determined protein–ligand binding affinities. Nucleic Acids Res. 2007;35:D198–D201. doi: 10.1093/nar/gkl999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butler A, Hoffman P, Smibert P, Papalexi E, Satija R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat. Biotechnol. 2018;36:411–420. doi: 10.1038/nbt.4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mamede M, et al. [18F]FDG uptake and PCNA, Glut-1, and Hexokinase-II expressions in cancers and inflammatory lesions of the lung. Neoplasia. 2005;7:369–379. doi: 10.1593/neo.04577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Derlin T, et al. Feasibility of 11C-acetate PET/CT for imaging of fatty acid synthesis in the atherosclerotic vessel wall. J. Nucl. Med. 2011;52:1848–1854. doi: 10.2967/jnumed.111.095869. [DOI] [PubMed] [Google Scholar]
- 16.Low PS, Henne WA, Doorneweerd DD. Discovery and development of folic-acid-based receptor targeting for imaging and therapy of cancer and inflammatory diseases. Acc. Chem. Res. 2008;41:120–129. doi: 10.1021/ar7000815. [DOI] [PubMed] [Google Scholar]
- 17.Thackeray JT, Bankstahl JP, Wang Y, Wollert KC, Bengel FM. Targeting amino acid metabolism for molecular imaging of inflammation early after myocardial infarction. Theranostics. 2016;6:1768–1779. doi: 10.7150/thno.15929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu C, Li F, Niu G, Chen X. PET imaging of inflammation biomarkers. Theranostics. 2013;3:448–466. doi: 10.7150/thno.6592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tahara N, et al. 2-deoxy-2-[18F] fluoro-d-mannose positron emission tomography imaging in atherosclerosis. Nat. Med. 2014;20:215–219. doi: 10.1038/nm.3437. [DOI] [PubMed] [Google Scholar]
- 20.Anzola LK, et al. Somatostatin receptor imaging by SPECT and PET in patients with chronic inflammatory disorders: A systematic review. Eur. J. Nucl. Med. Mol Imaging. 2019;46:2496–2513. doi: 10.1007/s00259-019-04489-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luo Y, Pan Q, Zhang W. IgG4-related disease revealed by 68Ga-FAPI and 18F-FDG PET/CT. Eur. J. Nucl. Med. Mol. Imaging. 2019;46:2625–2626. doi: 10.1007/s00259-019-04478-2. [DOI] [PubMed] [Google Scholar]
- 22.George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: The potential role for antifibrotic therapy. Lancet Respir Med. 2020;8:807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen H, Niu G, Wu H, Chen X. Clinical application of radiolabeled RGD peptides for PET imaging of integrin αvβ3. Theranostics. 2016;6:78–92. doi: 10.7150/thno.13242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griessinger CM, et al. The PET-tracer 89Zr-Df-IAB22M2C enables monitoring of intratumoral CD8 T cell infiltrates in tumor-bearing humanized mice after T cell bispecific antibody treatment. Cancer Res. 2020;80:2903–2913. doi: 10.1158/0008-5472.CAN-19-3269. [DOI] [PubMed] [Google Scholar]
- 25.Larimer BM, et al. Granzyme B PET imaging as a predictive biomarker of immunotherapy response. Cancer Res. 2017;77:2318–2327. doi: 10.1158/0008-5472.CAN-16-3346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Croft D, et al. The Reactome pathway knowledgebase. Nucleic Acids Res. 2014;42:D472–D477. doi: 10.1093/nar/gkt1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He J, et al. Single-cell analysis reveals bronchoalveolar epithelial dysfunction in COVID-19 patients. Protein Cell. 2020;11:680–687. doi: 10.1007/s13238-020-00752-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JS, et al. Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19. Sci. Immunol. 2020;5:1554. doi: 10.1126/sciimmunol.abd1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liao M, et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat. Med. 2020;26:842–844. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- 30.Locke LW, et al. A novel neutrophil-specific PET imaging agent: cFLFLFK-PEG-64Cu. J. Nucl. Med. 2009;50:790–797. doi: 10.2967/jnumed.108.056127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang J, Chen M, Li S, Ye RD. Targeted delivery of a ligand–drug conjugate via formyl peptide receptor 1 through cholesterol-dependent endocytosis. Mol. Pharm. 2019;16:2636–2647. doi: 10.1021/acs.molpharmaceut.9b00188. [DOI] [PubMed] [Google Scholar]
- 32.Zhang B, et al. Clinical characteristics of 82 death cases with COVID-19. PLoS ONE. 2020;15:e0235458. doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Russell B, et al. Associations between immune-suppressive and stimulating drugs and novel COVID-19: A systematic review of current evidence. Ecancermedicalscience. 2020;14:1022. doi: 10.3332/ecancer.2020.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Horby P, et al. Dexamethasone in hospitalized patients with covid-19: Preliminary report. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu Y, Chen Y, Tang X. Guidelines for the diagnosis and treatment of coronavirus disease 2019 (COVID-19) in China. Glob. Health Med. 2020;2:66–72. doi: 10.35772/ghm.2020.01015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adhikari SP, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: A scoping review. Infect. Dis. Poverty. 2020;9:29. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Love C, Tomas MB, Tronco GG, Palestro CJ. FDG PET of infection and inflammation. Radiographics. 2005;25:1357–1368. doi: 10.1148/rg.255045122. [DOI] [PubMed] [Google Scholar]
- 38.Zou S, Zhu X. FDG PET/CT of COVID-19. Radiology. 2020;296:E118. doi: 10.1148/radiol.2020200770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yi Y-S. Folate receptor-targeted diagnostics and therapeutics for inflammatory diseases. Immune Netw. 2016;16:337–343. doi: 10.4110/in.2016.16.6.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han W, et al. Molecular imaging of folate receptor β–positive macrophages during acute lung inflammation. Am. J. Respir. Cell Mol. Biol. 2015;53:50–59. doi: 10.1165/rcmb.2014-0289OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang Y, et al. PET imaging detection of macrophages with a formyl peptide receptor antagonist. Nucl. Med. Biol. 2015;42:381–386. doi: 10.1016/j.nucmedbio.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen K, et al. Regulation of inflammation by members of the formyl-peptide receptor family. J. Autoimmun. 2017;85:64–77. doi: 10.1016/j.jaut.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehta P, et al. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The single-cell RNA-sequencing data can be downloaded from the Gene Expression Omnibus database (https://www.ncbi.nlm.nih.gov/geo/).