Abstract
Background:
An alarming cerebro/cardiovascular collateral damage, reflected by a decline in admissions for acute stroke (AS) and acute coronary syndrome (ACS), was observed during the initial phase of the COVID-19 pandemic, thereby leading to a re-design of public campaigns. However, there are limited data regarding the AS and ACS hospitalization rates during the second wave of the pandemic, which was followed by re-imposition of lockdowns.
Methods:
We calculated the rate of AS and ACS hospitalizations from three representative tertiary care hospitals in Greece during a 2-month period (November–December 2020) of the second wave of the COVID-19 pandemic compared with the corresponding control period in 2019 from three representative tertiary care hospitals in Greece. This was a follow-up study with identical design to our previous report evaluating AS and ACS hospitalizations during the first wave of the pandemic (March–April 2020).
Results:
Compared with 2019, there was a 34% relative reduction of AS hospitalizations [incidence rate ratio (IRR): 0.66, 95% confidence interval (CI): 0.48–0.92, p = 0.013] and 33% relative reduction of ACS hospitalizations (IRR: 0.67, 95% CI: 0.54–0.83, p < 0.001) during the second wave of the COVID-19 pandemic. The relative reduction was smaller and did not reach the level of statistical significance for the respective syndromes (haemorrhagic stroke: IRR 0.87, 95% CI: 0.41–1.82, p = 0.71; ST-elevation myocardial infarction: IRR 0.81, 95% CI: 0.57–1.14, p = 0.22).
Conclusion:
AS and ACS hospitalizations were persistently reduced during the second wave of the COVID-19 pandemic compared with 2019 in Greece. This decline was similar to the observations during the first wave despite the large differences in the epidemiological COVID-19 burden. Lockdowns, a common characteristic in both waves, appear to have a detrimental indirect impact on cerebro/cardiovascular diseases in the general population.
Keywords: acute coronary syndromes, admissions, COVID-19, Greece, intracerebral haemorrhage, ischaemic stroke, stroke
Introduction
Since January 2020 and as of 23 March 2021 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 123,000,000 people globally, while 2,727,640 deaths due to coronavirus disease – 19 (COVID-19) have been recorded. 1
During the initial phase of the pandemic (‘first wave’), most countries rapidly re-designed their health services on a large scale for treating patients with COVID-19. Moreover, many national authorities instituted lockdowns (mandatory to stay at home, work from home, school closures and business closure orders) to slow the rapid spread of the virus. At the same time, numerous regional and national reports suggested a significant decline in acute stroke (AS)2–11 and acute coronary syndrome (ACS) admissions.12–16 Therefore, strict social measures and fear of exposure to SARS-CoV-2 could have inadvertently discouraged patients from seeking medical care. Since then, the scientific community systematically urged people with cardiovascular symptoms not to avoid referring to hospitals out of fear of being infected with SARS-CoV-2.17,18
After May 2020, strict social measures were partially lifted and life in many countries was gradually restored to ‘normality’. However, during the last months of 2020 the number of patients with COVID-19 increased and many countries re-introduced restrictive measures. Only limited data exist regarding the cardiovascular ‘collateral damage’ during the ‘second wave’ of COVID-19, and especially during the national lockdowns. 19
Our national collaborative group has previously investigated the rate of AS and ACS admissions in neurological and cardiological departments of three tertiary hospitals in Greece during the first wave of the pandemic (March–April 2020). We further evaluated these rates during the second national lockdown due to COVID-19 pandemic.
Methods
Study design
We conducted an observational study including patients admitted with AS or ACS to three tertiary care university hospitals of different geographic and epidemiologic regions of Greece (southern: Athens; northern: Thessaloniki; western: Ioannina). 10 The methodology of our study has previously been published. 10 In brief, all consecutive patients who were admitted with a confirmed diagnosis of AS or ACS were included in this study. Stroke patients were categorized in acute ischaemic stroke and acute haemorrhagic stroke subgroups. ACS included both ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation ACS (NSTE-ACS) (i.e. non-STEMI and unstable angina). Data were prospectively collected during a 2-month period from 1 November to 31 December 2020 and the corresponding 2-month control period in 2019 (1 November to 31 December 2019). The study complies with the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board of the University Hospital of Ioannina with protocol number 7/21-4-2020 (θ19) and was adopted by the other hospitals. The patients gave written consent for the anonymous use of their data.
Study periods
The first case of confirmed COVID-19 in Greece was identified on 26 February 2020. Starting from March 2020, progressive measures of social distancing were imposed by the Greek authorities: (1) 10 March 2020: all schools and universities were locked down and self-confinement behaviour was strongly recommended; (2) 16 March 2020: 80% of all business activities were halted; and, ultimately, (3) 23 March 2020: restricting measures of population movement were implemented and continued until 3 May 2020, when the country began to gradually lift restrictions. 15 During the first wave of the pandemic the incidence of new infections and fatalities was relatively small in the country and the Intensive Care Units (ICUs) were not overloaded (the maximum number of patients treated in ICUs was 93 on 5 April 2020). 20 During this period the main slogan was ‘stay at home’ and ‘we protect the people we love’ (elderly and patients with pre-existing cardiovascular disease). However, in Greece, and at the same time as both the European Society of Cardiology and American College of Cardiology urged patients to seek help if they had symptoms of heart diseases, the scientific community was sounding an alarm and new slogans featured prominently in television adverts (e.g. ‘even in the era of COVID, the infarction cannot be delayed’). Moreover, press releases from the Hellenic Societies of Cardiology and Neurology stressed the fact that ‘the stay-at-home order during COVID-19 does not apply to heart attacks and strokes’ and repeated messages were published such as that ‘we stay at home but we do not forget heart attacks and strokes’, while neurologists and cardiologists had frequent interviews in broadcast media. During the second wave of the pandemic, Greek authorities issued new local lockdowns on 29 October 2020, and a national lockdown was put in place on 7 November 2020. Kindergartens, elementary schools and special schools remained open, unlike the first lockdown in March, while middle and high schools as well as universities switched to distance learning. On 14 November 2020, all schools were closed and switched to distance learning. On 14 December 2020, shops opened (employing a click-away method: the customer ordered the product electronically and received it from an outdoor area), while schools and restaurants remained closed up to the end of the study period. During that period the national health system was overstressed, the number of reported infections and deaths due to COVID-19 was dramatically increased and ICUs were overloaded (the maximum number of patients treated in ICUs was 622 on 3 December 2020). 20
Comparative analyses were performed between the study period of the second-wave of COVID-19 (1 November to 31 December 2020) and a period prior to the COVID-19 pandemic: the corresponding period of the previous year (1 November to 31 December 2019).
Statistical analysis
Categorical variables are presented as absolute numbers with corresponding percentages, and odds ratios (ORs) with 95% confidence intervals (CIs). Comparisons between categorical variables were conducted using the chi-square or Fisher’s exact test for low expected frequencies. Continuous variables are presented as medians with interquartile range, and the Mann–Whitney test was used for comparisons. Incidence rate ratios (IRRs), comparing the admission rates during COVID-19 versus the control period, were calculated using the Poisson regression to model the number of admissions per day. An α level of 0.05 (two-tailed) was used as determinant of statistical significance. Stata 10.0 (StataCorp, College Station, TX, USA) and SPSS 17.0 (IBM, Armonk, NY, USA) were used for analyses.
Results
A total of 153 AS (study period: 61; control period: 92) and 345 ACS patients (study period: 138; control period: 207) were recorded. Table 1 shows the demographic and baseline clinical characteristics of the patients. There were no differences between baseline clinical characteristics between the two periods, excepting a lower percentage of female patients and a higher percentage of smokers for ACS hospitalizations during the COVID-19 period (p = 0.014 and p = 0.019, respectively).
Table 1.
Demographics, baseline clinical characteristics and presentation of patients admitted with stroke or ACS during the COVID-19 and control periods.
| Characteristic/parameter | Stroke admissions* (n = 153) | ACS admissions # (n = 345) | ||||
|---|---|---|---|---|---|---|
| COVID-19 (n = 61) | Control (n = 92) | p value | COVID-19 (n = 138) | Control (n = 207) | p value | |
| Demographics | ||||||
| Age [years, median (IQR)] | 63 (54.5–70.1) | 61 (51.7–67) | 0.153 | 63.7 (53.5–73) | 64 (56–73.6) | 0.449 |
| Female gender, n (%) | 27 (44.3) | 31 (33.7) | 0.187 | 18 (13) | 49 (23.7) | 0.014 |
| Baseline characteristics | ||||||
| Diabetes, n (%) | 14 (23) | 19 (20.7) | 0.735 | 41 (29.7) | 55 (26.7) | 0.542 |
| Hypertension, n (%) | 38 (62.3) | 67 (72.8) | 0.169 | 93 (67.4) | 129 (62.6) | 0.365 |
| Hypercholesterolaemia, n (%) | 46 (75.4) | 71 (77.2) | 0.801 | 75 (54.3) | 102 (49.5) | 0.379 |
| Smoking, n (%) | 22 (36.1) | 45 (48.9) | 0.117 | 71 (51.4) | 80 (38.6) | 0.019 |
| Chronic kidney disease, n (%) | 0 (0) | 2 (5.3) | 0.495 | 10 (7.2) | 14 (6.8) | 0.882 |
| Peripheral arterial disease, n (%) | 1 (1.6) | 4 (4.3) | 0.649 | 6 (4.3) | 14 (6.8) | 0.342 |
| Previous stroke, n (%) | 1 (1.6) | 4 (4.3) | 0.649 | 3 (2.2) | 12 (5.8) | 0.104 |
| Previous myocardial infarction, n (%) | 1 (1.6) | 9 (9.8) | 0.052 | 20 (14.5) | 36 (17.5) | 0.463 |
| Previous PCI, n (%) | 1 (1.6) | 6 (6.5) | 0.244 | 22 (15.9) | 41 (19.8) | 0.363 |
| Previous CABG, n (%) | 0 (0) | 4 (4.3) | 0.151 | 9 (6.5) | 11 (5.3) | 0.638 |
| Presentation | ||||||
| Stroke presentation | 0.433 | – | – | |||
| Ischaemic, n (%) | 48 (78.7) | 77 (83.7) | ||||
| Haemorrhagic, n (%) | 13 (21.3) | 15 (16.3) | ||||
| NIHSS, median (IQR) | 4 ([1–9.5) | 4 (1–6.8) | 0.738 | – | – | |
| ACS presentation | – | – | 0.161 | |||
| STEMI, n (%) | 59 (42.8) | 73 (35.3) | ||||
| NSTE-ACS, n (%) | 79 (57.2) | 134 (64.7) | ||||
| Ejection fraction [%, median (IQR)] | – | – | 50 (45–55) | 50 (45–55) | 0.937 | |
Stroke patients – percentage of missing data per characteristic/parameter: chronic kidney disease 53.6%.
ACS patients – percentage of missing data per characteristic/parameter: diabetes 0.3%; hypertension 0.3%; hypercholesterolaemia 0.3%; chronic kidney disease 0.6%; peripheral arterial disease 0.3%; previous stroke0.3%; previous myocardial infarction 0.3%; ejection fraction 0.9%.
ACS, acute coronary syndrome; CABG, coronary artery bypass grafting; IQR, interquartile range: NIHSS, National Institutes of Health Stroke Scale/Score; NSTE-ACS, non-ST-segment elevation ACS; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.
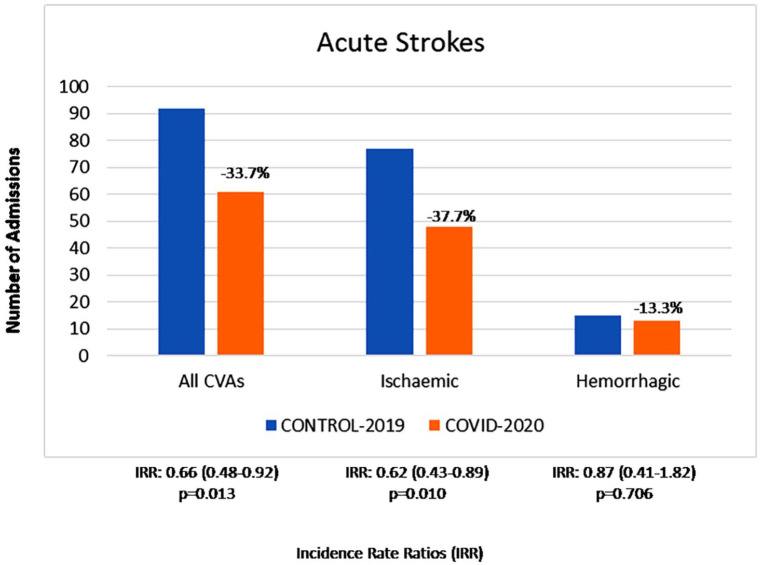
Compared with the control period, we observed an almost identical relative reduction of AS and ACS hospitalizations. There was an overall 34% relative reduction of AS admissions (IRR: 0.66, 95% CI: 0.48–0.92, p = 0.013; Figure 1) and a 33% relative reduction of ACS admissions (IRR: 0.67, 95% CI: 0.54–0.83, p < 0.001; Figure 2) during the COVID-19 pandemic. The relative reduction of ischaemic stroke admissions was 38% (IRR: 0.62, 95% CI: 0.43–0.89, p = 0.010), while the reduction of haemorrhagic stroke admissions (13%) was smaller and did not reach the level of statistical significance (IRR: 0.87, 95% CI: 0.41–1.82, p = 0.706). The percentage of admitted stroke patients ⩽65 years during the COVID-19 period tended to be lower compared with the control period (59.0% versus 71.7%, OR 0.57, 95% CI: 0.29–1.12, p = 0.102). Patients presenting with AS were managed either conservatively or by intravenous thrombolysis. The proportion of patients who were treated with intravenous thrombolysis was numerically lower during the COVID-19 period compared with the control period without, however, reaching statistical significance (8.2 versus 14.1%; OR 0.54, 95% CI: 0.18–1.61, p = 0.265).
Figure 1.
Number of acute stroke hospitalizations in three tertiary hospitals in Greece during the last 2 months of 2020 compared with the corresponding period in 2019. Relative (per cent) changes are presented for each stroke subtype.
CVA, cerebrovascular accident; IRR, incidence rate ratio.
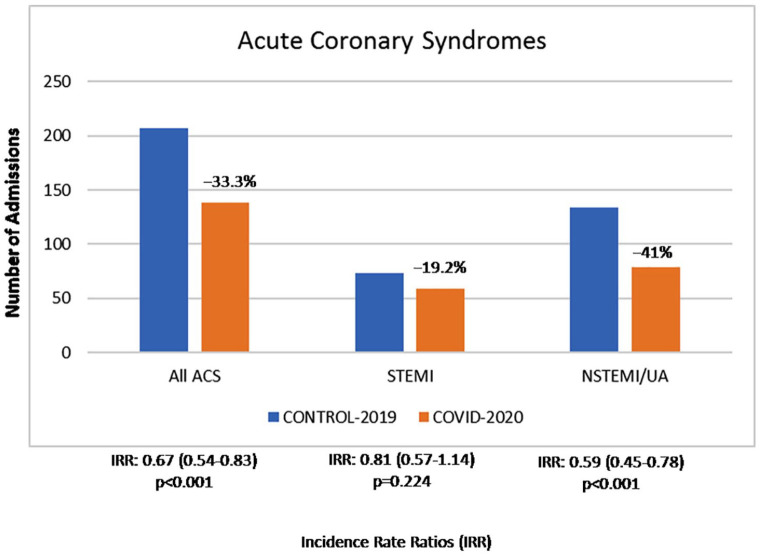
Figure 2.
Number of acute coronary syndrome (ACS) hospitalizations in three tertiary hospitals in Greece during the last 2 months of 2020 compared with the corresponding period in 2019. Relative (per cent) changes are presented for ACS subtype.
IRR, incidence rate ratio; NSTEMI, non-STEMI; STEMI, ST-segment elevation myocardial infarction; UA, unstable angina.
ACS admissions showed a reduction of 41% for NSTE-ACS (IRR: 0.59, 95% CI: 0.45–0.78, p < 0.001), while there was a smaller reduction of 19% for STEMI (IRR: 0.81, 95% CI: 0.57–1.14, p = 0.224). There was no difference regarding the percentage of younger (⩽65 years) patients admitted with ACS during the COVID-19 and pre-pandemic periods (67% for both periods, OR = 1.0, 95% CI: 0.65–1.54, p > 0.999). There was no significant difference in the proportion of patients presenting with ACS who underwent percutaneous coronary intervention in the COVID-19 period compared with the control period (75.4 versus 69.1% respectively; odds ratio: 1.37, 95% CI: 0.84–2.23, p = 0.205).
Discussion
Our results showed that the number of AS and ACS admissions during the second wave of the COVID-19 pandemic in academic hospitals in Greece was lower than that of the corresponding period in 2019. The relative reduction was almost identical regarding acute cerebrovascular and cardiovascular admissions. A lower decline in admissions was observed in patients with more clinically severe events (haemorrhagic stroke and STEMI). The relative reduction of admissions for AS was larger for younger patients, while no difference was noticed in ACS admissions.
Limited data exist regarding the cerebro/cardiovascular ‘collateral damage’ during the second phase of the COVID-19 pandemic, which was followed by new national lockdowns. Wu et al. 19 reported a decline in hospitalized patients with acute myocardial infarction by almost 34%, which pre-dated the onset of the second national lockdown in the United Kingdom. The second dip appeared to be similar to that of the first pandemic wave (32% during the first UK lockdown) and the rates of admissions declined even further after the beginning of both national lockdowns. 19 Likewise, the magnitude of reduction of ACS admissions in our study was similar to that of the first lockdown in Greece.10,15 Since, the results are comparable and originated from national health care systems with different characteristics, it is unlikely that the reduction of admissions during the pandemic merely reflects a local/national change in the quality of provided health care services. Moreover, these results show that community interventions to ensure that the general population, and especially people with cerebro/cardiovascular symptoms, will continue to seek appropriate medical care had no major effect on patient behaviour. However, this is not a rare phenomenon in recent medical history. Over the last decades many studies reported no reduction in pre-hospital time delay of patients diagnosed with ACS despite media and educational campaigns.20,21,22 In the COVID-19 era, we need clever campaign strategies. For example, a strategy, distributed by national digital media and designed with behavioural insights, was associated with improved self-reported personal hygiene and physical distancing in the Netherlands during the COVID-19 crisis. 23 However, several factors (age, gender, education level) affected the outcomes of this particular study. 23 In Greece, a telephone interview survey revealed significant lifestyle changes (passive smoking, working hours and alcohol consumption were reduced while sleeping hours were increased) in the general population during the first lockdown, and also showed that there was anxiety about the pandemic (45.1%), and lack of motivation and satisfaction (38.4%). Moreover, almost one out of four participants reported that if they had chest pain they would not seek medical attention. 24 It would be interesting to see in the future any association between lifestyle changes and hospital admissions from cardio/cerebrovascular events.
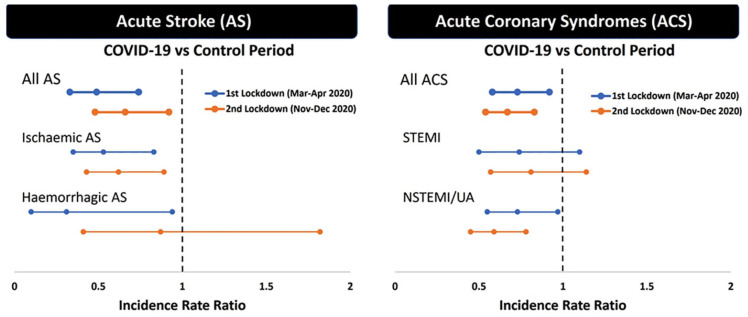
Using identical methodology, we have previously reported a greater reduction of AS (51%) compared with ACS admissions (27%) during the first wave of the COVID-19 pandemic and the first national lockdown in Greece. 10 The relative reduction of ischaemic stroke admissions was 47% and of haemorrhagic stroke admissions 69%. There was a similar relative reduction for STEMI and NSTEMI/UA admissions (26% versus 27%, respectively). Figure 3 shows the respective reductions in AS and ACS hospitalizations during the first and second waves of the pandemic.
Figure 3.
The incidence rate ratio (IRR) of admissions (i.e. relative change in COVID-19 compared with the control period). Blue and orange lines indicate IRR and 95% confidence intervals.
ACS, acute coronary syndrome; AS, acute stroke; NSTEMI, non-STEMI; STEMI, ST-segment elevation myocardial infarction; UA, unstable angina.
Notably, during the second wave of the pandemic we did not replicate the reduction in the admissions of younger patients that was documented during the first wave. This may be due to the fact that during the second wave in Greece, new infections, deaths, intubated patients, and the overall pressure on the health system were far higher than those of the first wave. Second, after the first wave, messages to the community focused mainly on the importance of swiftly transferring older people with vascular risk factors swiftly to the emergency room. Third, people with more severe symptoms (haemorrhagic stroke and STEMI in AS and ACS groups, respectively) may have fewer reservations to seek care in contrast to people with milder symptoms. Finally, the discrepant observation between the first and the second wave of the pandemic can be contributed to chance, since the number of admissions in some subgroups was relatively small in our study. However, our findings from two periods with different epidemiological characteristics in Greece (low versus high penetrance of the SARS-CoV-2 virus and limited versus increased healthcare burden) showed that lockdowns possibly have a negative impact on the cerebro/cardiovascular diseases regardless of the burden of COVID-19 in the community.
During the first wave of the pandemic, large-scale measures might have affected triggers for AS and ACS, resulting in a true incidence reduction and an ensuing relevant admission reduction. On the other hand, studies reported a dramatic increase in out-of-hospital cardiac arrest (OHCA) cases during the COVID-19 period.24,25 Only a minority of OHCA patients had either a confirmed diagnosis of SARS-CoV-2 infection or displayed clinical signs consistent with COVID-19.25,26 In Greece, a small study from a single hospital showed that the cases of OHCA transferred to the emergency room did not differ between the pre-pandemic and the COVID-19 era. 27 Consequently, we can hypothesize that many ACS patients did not reach emergency and hospital services. In addition, the number of deaths observed during 2020 (52 weeks) was higher than the previous year (130,288 versus 124,538; +4.62%). Interestingly, the p-score (deaths period 2020 – average deaths period 2015–2019/average deaths period 2015–2019) was high (7.25% corresponding to an excess of 8802 deaths). 28 Furthermore, only 4881 deaths were classified as COVID-19 related during 2020. In view of the former considerations, the excess mortality could be associated with potential misclassification of undiagnosed causes of death including fatal cerebro/cardiovascular accidents that did not reach emergency/hospital services. Notably, cerebro/cardiovascular diseases are by far the leading causes of death in Greece. 29
It is quite difficult to obtain accurate information regarding the exact reasons behind our findings in the two different waves retrospectively, since the bulk of the patients who actually avoided seeking medical care after having had symptoms is not known and these patients cannot be targeted for interviews; our questions and interviews address the hospitalized patients. Additionally, there are no validated questionnaires regarding the avoidance of medical care during pandemics. During the initial interview and medical assessment at the Emergency Room we have asked what the patients think about their cerebro/cardiovascular disease and the new virus. It is interesting that the majority of patients reported that they knew about the appeals of the scientific community to seek help if they had symptoms of cerebro/cardiovascular diseases. Approximately half of the hospitalized patients reported ‘not at all/a little worry’ about COVID-19. Only one in three patients reported no delay for seeking medical attention.
Our study is limited by the inherent disadvantages of observational registries and the relatively small sample size of each subgroup. Moreover, during the study period, the three University Hospitals which were included in the study did also serve as COVID reference-centres in Greece. Thus, the possibility that patients might have preferred an admission to another, non-COVID, hospital cannot be excluded.
In conclusion, the rate of AS and ACS admissions during the second wave of the COVID-19 pandemic in Greece was lower than that of the corresponding period in 2019. Lockdowns appear to have detrimental effects on the management of cerebro/cardiovascular diseases in the general population. More appropriate and aggressive strategies are urgently needed to mitigate this major collateral health system damage of the long-standing pandemic.
Footnotes
Author contributions: Concept and design: Christos Katsouras, Georgios Tsivgoulis, Lampros K. Michalis, Sotirios Giannopoulos.
Writing of the manuscript: Christos Katsouras, Georgios Tsivgoulis, Michail Papafaklis, Lina Palaiodimou, Sotirios Giannopoulos.
Data collection: Michail Papafaklis, Theodore Karapanayiotides, Dimitrios Alexopoulos, Evangelos Ntais, Georgia Papagiannopoulou, Ioanna Koutroulou, Antonios Ziakas, Georgios Sianos, Antonios Kouparanis, Paraskevi Trivilou, Christos Ballas, Ioanna Samara, Maria Kosmidou, Lina Palaiodimou, Nikolaos Grigoriadis
Critical revision for important intellectual content: Theodore Karapanayiotides, Nikolaos Grigoriadis, Lampros K. Michalis
Availability of data: The data that support the findings of this study are available from the corresponding author (SG), upon reasonable request.
Conflict of interest statement: Georgios Tsivgoulis is Associate Editor at Therapeutic Advances in Neurological Disorders, therefore, the peer review process was managed by alternative members of the Board and the submitting Editor was not involved in the decision-making process.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iDs: Georgios Tsivgoulis  https://orcid.org/0000-0002-0640-3797
https://orcid.org/0000-0002-0640-3797
Ioanna Koutroulou  https://orcid.org/0000-0001-5043-6521
https://orcid.org/0000-0001-5043-6521
Lina Palaiodimou  https://orcid.org/0000-0001-7757-609X
https://orcid.org/0000-0001-7757-609X
Sotirios Giannopoulos  https://orcid.org/0000-0001-7443-5179
https://orcid.org/0000-0001-7443-5179
Contributor Information
Christos Katsouras, Second Department of Cardiology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Georgios Tsivgoulis, Second Department of Neurology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece.
Michail Papafaklis, Second Department of Cardiology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Theodore Karapanayiotides, Second Department of Neurology, Faculty of Health Sciences, School of Medicine, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Dimitrios Alexopoulos, Department of Cardiology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece.
Evangelos Ntais, Department of Neurology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Georgia Papagiannopoulou, Second Department of Neurology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece.
Ioanna Koutroulou, Second Department of Neurology, Faculty of Health Sciences, School of Medicine, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Antonios Ziakas, Department of Cardiology, Faculty of Medicine, School of Health Sciences, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Georgios Sianos, Department of Cardiology, Faculty of Medicine, School of Health Sciences, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Antonios Kouparanis, Department of Cardiology, Faculty of Medicine, School of Health Sciences, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Paraskevi Trivilou, Department of Cardiology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece.
Christos Ballas, Second Department of Cardiology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Ioanna Samara, Second Department of Cardiology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Maria Kosmidou, Department of Neurology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Lina Palaiodimou, Second Department of Neurology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece.
Nikolaos Grigoriadis, Second Department of Neurology, Faculty of Health Sciences, School of Medicine, AHEPA University Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece.
Lampros K. Michalis, Second Department of Cardiology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
Sotirios Giannopoulos, Second Department of Neurology, ATTIKON University Hospital, National and Kapodistrian University of Athens, Athens, Greece; Department of Neurology, University Hospital of Ioannina, University of Ioannina, Ioannina, Greece.
References
- 1. John Hopkins University & Medicine. Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), https://coronavirus.jhu.edu/map.html (accessed 23 March 2021).
- 2. Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 2020; 51: 2315–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoyer C, Ebert A, Huttner HB, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke 2020; 51: 2224–2227. [DOI] [PubMed] [Google Scholar]
- 4. Jasne AS, Chojecka P, Maran I, et al. Stroke code presentations, interventions, and outcomes before and during the COVID-19 pandemic. Stroke 2020; 51: 2664–2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Katsanos AH, Palaiodimou L, Zand R, et al. The impact of SARS-CoV-2 on stroke epidemiology and care: a meta-analysis. Ann Neurol 2021; 89: 380–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Montaner J, Barragán-Prieto A, Pérez-Sánchez S, et al. Break in the stroke chain of survival due to COVID-19. Stroke 2020; 51: 2307–2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Siegler JE, Heslin ME, Thau L, et al. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis 2020; 29: 104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tsivgoulis G, Palaiodimou L, Katsanos AH, et al. Neurological manifestations and implications of COVID-19 pandemic. Ther Adv Neurol Disord 2020; 13: 1756286420932036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tsivgoulis G, Palaiodimou L, Zand R, et al. COVID-19 and cerebrovascular diseases: a comprehensive overview. Ther Adv Neurol Disord 2020; 13: 1756286420978004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Katsouras C, Karapanayiotides T, Papafaklis M, et al. Greater decline of acute stroke admissions compared with acute coronary syndromes during COVID-19 outbreak in Greece: cerebro/cardiovascular implications amidst a second wave surge. Eur J Neurol. Epub ahead of print 8 December 2020. DOI: 10.1111/ene.14666. [DOI] [PubMed] [Google Scholar]
- 11. Richter D, Eyding J, Weber R, et al. Analysis of nationwide stroke patient care in times of COVID-19 pandemic in Germany. Stroke 2021; 52: 716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. New Engl J Med 2020; 383: 88–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020; 75: 2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mafham MM, Spata E, Goldacre R, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020; 396: 381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Papafaklis MI, Katsouras CS, Tsigkas G, et al. “Missing” acute coronary syndrome hospitalizations during the COVID-19 era in Greece: medical care avoidance combined with a true reduction in incidence? Clin Cardiol 2020; 43: 1142–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Østergaard L, Butt JH, Kragholm K, et al. Incidence of acute coronary syndrome during national lock-down: Insights from nationwide data during the Coronavirus disease 2019 (COVID-19) pandemic. Am Heart J 2021; 232: 146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. European Academy of Neurology. COVID-19: a message from those living with neurological disorders, https://www.efna.net/wp-content/uploads/2020/04/COVID-19_EFNA-message.pdf (2020, accessed 23 March 2021).
- 18. European Society of Cardiology. Appeals to “stay at home” during COVID-19 do not apply to heart attacks, https://www.escardio.org/The-ESC/Press-Office/Press-releases/Appeals-to-stay-at-home-during-COVID-19-do-not-apply-to-heart-attacks-bis (2020, accessed 23 March 2021).
- 19. Wu J, Mamas MA, de Belder MA, et al. Second decline in admissions with heart failure and myocardial infarction during the COVID-19 pandemic. J Am Coll Cardiol 2021; 77: 1141–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Public Health Organization. Current state of Covid-19 outbreak in Greece and timeline of key containment events, https://eody.gov.gr/en/current-state-of-covid-19-outbreak-in-greece-and-timeline-of-key-containment-events/ (accessed 23 March 2021).
- 21. Blohm MB, Hartford M, Karlson BW, et al. An evaluation of the results of media and educational campaigns designed to shorten the time taken by patients with acute myocardial infarction to decide to go to hospital. Heart (British Cardiac Society) 1996; 76: 430–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: the Rapid Early Action for Coronary Treatment (REACT) trial. JAMA 2000; 284: 60–67. [DOI] [PubMed] [Google Scholar]
- 23. Yousuf H, Corbin J, Sweep G, et al. Association of a public health campaign about coronavirus disease 2019 promoted by news media and a social influencer with self-reported personal hygiene and physical distancing in the Netherlands. JAMA Netw Open 2020; 3: e2014323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tsigkas G, Koufou EE, Katsanos K. Potential relationship between lifestyle changes and incidence of hospital admissions for acute coronary syndrome during the COVID-19 lockdown. Front Cardiovasc Med 2021; 8: 604374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baldi E, Sechi GM, Mare C, et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J 2020; 41: 3045–3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fothergill RT, Smith AL, Wrigley F, et al. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resuscitation Plus 2021; 5: 100066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kapelios CJ, Siafarikas C, Bonou M, et al. The effect of the COVID-19 pandemic on acute coronary syndrome hospitalizations and out-of-hospital cardiac arrest in Greece. Public Health 2021; 191: 17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hellenic Statistical Authority. Deaths/2020, https://www.statistics.gr/en/statistics/-/publication/SPO09/ (accessed 23 March 2021).
- 29. The Organisation for Economic Co-operation and Development. Greece: Country Health Profile 2019, https://www.oecd.org/greece/greece-country-health-profile-2019-d87da56a-en.htm (accessed 23 March 2021).