Abstract
Background:
Emotional disclosure is the therapeutic expression of emotion. It holds potential as a means of providing psychological support. However, evidence of its efficacy in palliative settings is mixed. This may be due to variation in intervention characteristics.
Aim:
To derive a greater understanding of the characteristics of potentially effective emotional disclosure-based interventions in palliative care by:
(1) Developing a taxonomy of emotional disclosure-based interventions tested in people with advanced disease and
(2) Mapping and linking objectives, outcomes, underlying mechanisms, and implementation factors.
Design:
A scoping review drawing on Intervention Component Analysis to combine evidence from studies’ methods, results, and discussion sections.
Data sources:
Six databases were searched to May 2020 including CINAHL, PsycINFO, and MEDLINE. Studies of emotional disclosure in adults with advanced disease were included. Study quality was appraised using an established tool.
Results:
Seven thousand seven hundred ninety-two unique records were screened, of which 25 primary studies were included. Intervention characteristics were grouped into classes within three domains: topic of disclosure, format, and dose. Evidence was not available to determine which, if any, of the characteristics is most effective. Thematic synthesis of evidence from methods and discussion sections identified factors to consider in tailoring an emotional disclosure-based intervention to this setting, including: population characteristics (e.g. time since diagnosis), providing a safe environment, and flexibility in format.
Conclusions:
This review approach facilitated a clearer understanding of factors that may be key in developing emotional disclosure-based interventions for palliative populations. Intervention Component Analysis has potential for application elsewhere to help develop evidence-based interventions.
Keywords: Palliative care, psychotherapy, emotions, mental health, scoping review, Intervention Component Analysis
What is already known about the topic?
Emotional disclosure-based interventions can improve psychological and physical wellbeing in general populations.
A range of emotional disclosure-based interventions exist, but evidence of their efficacy in palliative care is mixed; it is not clear in which forms they may be effective or most effective, and on which outcome measures.
Trials have been limited in the extent to which they have tailored the intervention for people with advanced disease.
What this paper adds
To our knowledge, this is the first scoping review to systematically map the characteristics of emotional disclosure-based interventions that have been tested in people with advanced disease.
By grouping intervention characteristics into classes within operative domains and mapping these to outcomes, we provide a picture of which intervention forms may be most promising to pursue in future research.
Disease stage, environment, flexibility in delivery and topic, clarity of instructions, and staff training are identified as important factors to consider when tailoring emotional disclosure-based interventions for people with advanced disease.
Implications for practice, theory or policy
The review provides an exemplar approach to scoping literature to inform complex intervention development and evaluation in cases where pre-existing findings are mixed.
The review highlights the need for researchers to report key facilitators and barriers they find in intervention implementation and efficacy when presenting results.
Researchers should consider the recommendations made in this review to inform development and evaluation of emotional disclosure-based interventions tailored for people with advanced disease.
Introduction
Psychological distress can be considerable for people living with advanced disease. For up to 50% of people receiving palliative care, this distress can develop into clinical anxiety or depression.1–4 In recognition of this, national and international clinical guidelines recommend that psychological support should form a crucial element of the holistic palliative care approach.5–9 However, research indicates current psychological service provision in palliative care is likely to be inadequate in the UK and globally.10–12 This can be partially attributed to limitations in funding for the end-of-life care sector.12–14 It is therefore important that palliative care services can access and implement cost-effective ways of providing psychological support for people in their care.
Certain forms of emotional disclosure-based interventions offer a potentially promising solution. For the purposes of this review, emotional disclosure is defined as techniques designed to encourage or facilitate the disclosure, expression or discussion of emotions or feelings. These therapies are based on the notion that expressing emotions can improve wellbeing. 15 The therapeutic potential of emotional disclosure has been recognized cross-culturally for centuries in the form of religious confessions and Freudian psychotherapeutic approaches. 15 For example, drawing on this long history, a simple expressive writing intervention was proposed in 1986. 16 In its most basic format, it involves writing down the facts and emotions about a trauma for 15–20 min per day over 3–4 consecutive days without the need for professional facilitation. 17 Hundreds of studies have since investigated expressive writing and emotional disclosure-based variations, with meta-analyses reporting small but positive effects on both physical and psychological health in various populations.18–21
Trials of emotional disclosure-based interventions in palliative populations, however, have had mixed-results.22–24 A recent meta-analysis of randomized controlled trials (RCTs) of expressive writing in people with advanced disease found, overall, it had no significant effect on the physical or psychological health measures investigated. 24 However, this evidence is weak; it is from four RCTs of limited quality, with only one of these using an intervention that had been specifically tailored to the unique needs of its population. 25 Whilst this study did individually report a positive effect of the intervention, it was a pilot with 13 participants, and thus was not designed to detect significance. 25 The importance of tailoring interventions to the target population is likely to be crucial, given the unique existential distress and physical challenges experienced by people at this stage of their illness. As a result, there is still a need for further, robustly designed trials of tailored emotional disclosure-based interventions.
In their guidelines for complex intervention development, the Medical Research Council outline the importance of having a clear theoretical rationale for an intervention and its component parts.26–28 A number of processes have been proposed to explain the potential effects of emotional disclosure, including emotion regulation and the psychosomatic theory of inhibition. 29 However, it is not clear to what extent existing interventions tested in palliative care draw on these processes to inform their design.29–31 Forming clearer links between underlying processes and intervention design may also help to inform outcome measure selection. Outside of advanced disease populations, reviews have found significant as well as null effects of emotional disclosure-based interventions on a range of psychological and physical symptoms.18,31,32 As such, it is not clear which outcome measures may be most appropriate for evaluating effectiveness.
Moreover, the content and structure of emotional disclosure-based interventions can vary widely, further complicating the evaluation process. For instance, session length, frequency of delivery, and the topic of the disclosure can vary. Emotional disclosure-based interventions also go beyond expressive writing and can include, for example, spoken disclosure, 33 poetry, 34 and narrative therapy. 35 There is often overlap between types of intervention (for example, written and spoken forms) and the language used to describe them. It is therefore challenging to understand which, if any, intervention components may potentially be most effective. To our knowledge, no review to date has explored the range of emotional disclosure-based interventions tested in palliative populations.
In summary, emotional disclosure-based interventions still appear to hold therapeutic potential for people with advanced disease. A lack of clarity on which emotional disclosure-based intervention characteristics may be optimal, their mechanisms of action and appropriate outcome measures, may limit our current understanding of how such interventions may be beneficial for palliative populations.26,36 This scoping review therefore aims to derive a greater understanding of the range of emotional disclosure-based interventions evaluated in palliative populations, looking beyond expressive writing, and to understand what a potentially effective one may look like.
The objectives of the review are to:
Develop a taxonomy of emotional disclosure-based interventions used for people with advanced disease. The taxonomy will identify, categorize, and define classes (i.e. types) of intervention that fall under the umbrella term “emotional disclosure.”
Map and identify any potential links between intervention characteristics, objectives, outcome measures, underlying mechanisms, facilitators and barriers, and efficacy of emotional disclosure-based interventions for people with advanced disease.
Methods
A scoping review is a suitable method for mapping out complex literature bases in a systematic manner. 37 This review was conducted in six key stages, guided by standard scoping review frameworks.38–40 The protocol guiding this scoping review is reported elsewhere. 41 In line with the iterative nature of scoping reviews, the protocol has been updated throughout the process, as documented in Supplemental File 1.
Stage 1. Defining the research question
The following research questions were defined:
Which psychotherapeutic interventions for patients with advanced disease are categorized as, or explicitly grounded in, emotional disclosure?
What are the primary objectives and characteristics of emotional disclosure-based interventions evaluated in this population?
What outcome measures are used to assess the efficacy of emotional disclosure-based interventions in this setting, and which of these captured significant effects?
What theoretical frameworks are used to explain the mechanisms underlying emotional disclosure-based interventions in this setting?
What are the facilitators and barriers to feasibility and efficacy of emotional disclosure-based interventions in this setting?
Stage 2. Identifying relevant studies
Eligibility criteria
All primary studies (irrespective of design) of emotional disclosure-based psychotherapeutic interventions were included, provided they:
a. Described the method of at least one task or exercise as part of the intervention that is designed to encourage or facilitate the disclosure, expression or discussion of emotions or feelings AND
b. Described emotional disclosure or expression of emotions as a key goal, rationale or functional mechanism of the intervention
Only studies testing interventions with adults (aged 18 and above) with a diagnosis of an advanced disease, such as metastatic cancer (or characterized as Stage III or IV), and/or being explicitly treated with a palliative intent were included. Advanced disease is a broad and commonly used term selected to capture the broad range of diagnoses that could fall under the remit of palliative care. Samples which included >50% patients with advanced disease were also included.
Exclusion criteria
Publications not in the English language, review articles, discussion pieces, book chapters, and dissertations/theses were excluded. Music, art, life review, dignity, and group therapies were excluded as distinct therapy types that have been reviewed elsewhere.42–48
Databases
Six databases were searched from inception to May 2020: CINAHL, Cochrane Central Register of Controlled Trials (CENTRAL), PsycINFO, Scopus, Web of Science, and MEDLINE. The European Union Clinical Trials Register, clinicaltrials.gov, the European Association for Palliative Care conference abstracts for the last 7 years (2012–2019) and reference lists of relevant studies, review articles, book chapters, and theses were also checked.
Search strategy
A combination of Medical Subject Headings (MeSH) and free-text search terms for emotional disclosure, advanced disease, and palliative care were used. The terms for emotional disclosure were based on earlier, related reviews, but adapted to capture a range of disclosure formats.22,24 The terms for advanced disease and palliative care were based on a previous review, 24 recommended by the Cochrane Palliative Care research group. An example of the search strategy string used for the Ovid PsycINFO database is shown in Table 1. The string was optimized for each database (see Supplemental File 2).
Table 1.
Search strategy string for PsycINFO database.
| exp Emotions/ OR emotion* OR feeling* AND Palliative Care/ OR (palliat* or terminal* or endstage or hospice* or metasta* or (end adj3 life) or (care adj3 dying) or ((advanced or late or last or end or final) adj3 (stage* or phase*))).tw. AND (disclos* or express* or communicat* or talk* or speak* or spoke* or writ* or draw* or sing*).mp. |
Filters applied: humans and adulthood (18+).
Stage 3. Study selection
Two reviewers independently screened titles and abstracts for inclusion to the full article review stage. Full article review was also conducted independently by two researchers. Unclear decisions were discussed between members of the review team.
Stage 4. Charting the data
A data extraction form was developed based on the variables most relevant to the research questions (see Supplemental File 3). Extraction was completed by one author and a sample of five studies checked by a second author.
Stage 5. Collating, summarizing, and reporting the results
Synthesis was based on Intervention Component Analysis, which is a pragmatic approach to identifying which characteristics of an intervention, from a group of similar interventions, are potentially important in terms of outcomes. 49 Intervention Component Analysis uses qualitative thematic techniques to analyze intervention descriptions to identify and group core characteristics of an intervention. Parallel to this, experience-based evidence from study methods and discussion sections is thematically analyzed; this evidence captures authors’ descriptions of their experience developing and implementing the intervention. Whilst Intervention Component Analysis is designed to review interventions reported in trials that aim to influence the same outcome, this scoping review includes a range of study designs using a number of outcome measures. The principles of Intervention Component Analysis were therefore used but the approach was modified to suit the available evidence and meet the review objectives.
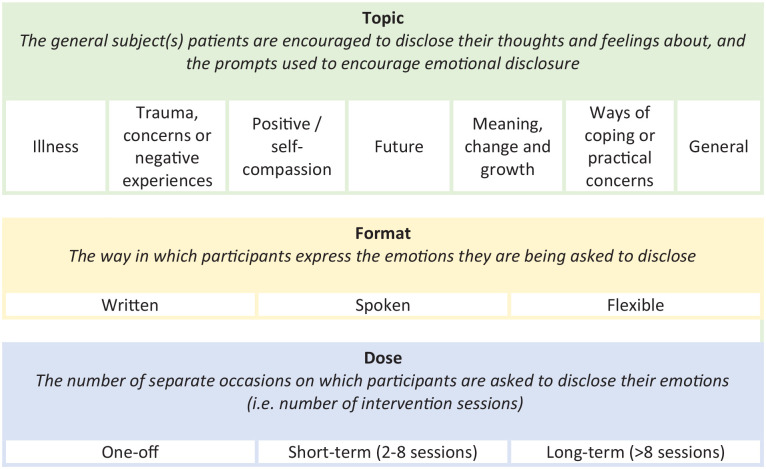
After extracting intervention descriptions, through iterative comparison and discussion, three operative domains were identified (i.e. overarching categories within which interventions varied). These were used as a framework for further exploration. Firstly, to form a multi-level taxonomy; using thematic analysis intervention descriptions were coded and similar characteristics grouped into classes (i.e. types) within each of the identified domains (Figure 2). Intervention objectives were then coded and grouped, and these were mapped to the outcome measures being used to assess them (Table 3). Thirdly, intervention classes in the multi-level taxonomy were mapped to the reported efficacy of interventions within them (Table 4). The underlying mechanisms that studies proposed were then grouped into theoretical classes (Table 5). Finally, in parallel to these processes, the facilitators and barriers extracted from discussion sections and methodological descriptions were analyzed using thematic analysis (Figure 3). One author (DM) led the analysis, with themes and conclusions discussed with the research team and updated throughout.
Figure 2.
Proposed multi-level taxonomy of ED-based intervention features.
Table 3.
Classification of intervention objectives and outcome measures in RCTs.
| Class of intervention objective | Primary outcome measures to evaluate objective* | Qualitative assessment methods |
|---|---|---|
| Quality of life | Global suffering VAS, QUAL-E, FACT-G, FACT-B, SDS, MDASI-BT/LC | n/a |
| Care quality and access | Use of mental health services measure | Interview |
| Case report | ||
| Psychological wellbeing | General: DT, ETS, POMS, POMSSF, composite measure, SDHS | Analysis of expression texts |
| Depression: CES-D, CES-D short version, PHQ-9, BDI | ||
| Anxiety: HADS-A, POMS Anxiety sub-scale, STAI | Interview | |
| Trauma and stress: IES | Case report | |
| Stress: PSS | ||
| Self-compassion: SCS | ||
| Other: FSCRS, SISE, FACT-G (emotional wellbeing subscale); CAR; MAAS | ||
| Physical wellbeing | Symptom scales: SSS, MSAS, ADLS, IADLS, ESAS | Analysis of expression texts |
| Existential and spiritual wellbeing | Spiritual: FACT-Sp, DSES, SHI | Analysis of expression texts |
| Preparation and completion: QUAL-E—preparation and completion sub-scale | Interviews | |
| Sleep and fatigue | Sleep: PSQI | n/a |
| Fatigue: FACT-F | ||
| Interpersonal | Romantic relationships: MSIS, QMI, PAIRI | n/a |
| Social support: brief family social support measure |
BDI: beck depression inventory; CAR: concerns about recurrence subscale; CES-D: center for epidemiological studies depression scale; DSES: daily spiritual experience scale; DT: distress thermometer; ETS: emotion thermometer scale; ESAS: Edmonton symptom assessment scale; FACT: functional assessment of cancer therapy; FACT-B: FACT-breast cancer; FACT-E: FACT-existential; FACT-G: FACT-general; FACT-Sp: FACT-spiritual; FSCRS: forms of self-criticizing and -reassuring scale; HADS: hospital anxiety and depression scale-anxiety; (I)ADLS: (instrumental) activities of daily living scale; IES: impact of events scale; MAAS: mindful-attention awareness scale; MSAS: memorial symptom assessment scale; MSIS: miller social intimacy scale; MDASI-BT: MD Anderson symptom inventory-brain tumor; MDSAI-LC: MD Anderson symptom inventory-lung cancer; PAIRI: personal assessment of intimacy in relationships inventory; PHQ-9: personal health questionnaire-9; POMS: profile of moods scale; POMSSF: POMS short form; PSQI: Pittsburgh sleep quality index; PSS: perceived stress scale; QMI: quality of marriage index; QUAL-E: quality of life at the end of life; SCS: self compassion scale; SDHS: short depression-happiness scale; SDS: symptom distress scale; SHI: self harm inventory; SISE: single item self-esteem scale; SSS: somatic symptom scale; STAI: state trait anxiety inventory; VAS: visual analog scale.
Some studies’ primary objective were grouped under more than one theme and therefore feature in more than one class.
Table 4.
Mapping intervention domains and classes to study outcomes.
| Intervention characteristics | Impact of intervention in controlled studies on:* | Summary of qualitative evidence on acceptability and experience | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Domain | Class | Quality of life | Psychological wellbeing | Physical wellbeing | Care quality/access | Existential/spiritual wellbeing | Sleep/fatigue | Social | |
| Outcome measures for which significant positive effects reported (follow up time-point post-intervention, weeks) | |||||||||
| Topic | Illness | + | +++ OOOOO | + | + | O | + O - ** | + | • One qualitative study reported the intervention was well-received and helped patient feel more cared for 54 |
| FACT-G (12) | Composite (12) IES (12) BDI (36) |
SSS (12) | Uptake MHS (8) | PSQI (up to 10) | MSIS, QMI (0) | ||||
| Trauma | OO | OO | O | +O | • One study reported participants found the intervention “overwhelmingly” helpful and could relate as a whole person.
63
• Two case studies reported positive feedback from participants, including better symptom control, improved communication, reduced distress and promoted dignity and self-esteem 52 and a sense of release, closure and distraction, as well as facilitating patients entering into therapy. 53 |
||||
| QUAL-E (5) | |||||||||
| Positive | +OOO | ++OO | O | +OOO | O | + | • One study reported participants found the intervention “overwhelmingly” helpful and could “relate as a whole person” (i.e. more than just their condition). 63 | ||
| MDASI (2-8) | CES-D, IES (4-12) SCS (2-8) |
QUAL-E (5) | PAIRI (2-8) | ||||||
| Future | + | O | • One case study reported positive feedback from participants including a sense of release, closure and distraction, and facilitated patients entering into therapy. 53 | ||||||
| FACT-G (12) | |||||||||
| Growth | +OOOO | +++OOO | + OO | + OO | OOO | + | • One study reported participants found the intervention “overwhelmingly” helpful and could “relate as a whole person” (i.e. more than just their condition). 63 | ||
| MDASI (2-8) | PHQ-9 (6) CES-D, IES (4-12) SCS (2-8) |
ESAS-pain (8) | QUAL-E (5) | PAIRI (2-8) | |||||
| Ways of coping | O | + O | + O | OO | • One qualitative study reported the interventions were well-received and helped patient feel more cared for 54 | ||||
| PHQ-9 (6) | ESAS-pain (8) | ||||||||
| General | +O | +++ | O | O | + | None reported | |||
| MDASI (2-8) | CES-D, IES (4-12) SCS (2-8) ETS—anxiety (0) |
PAIRI (2-8) | |||||||
| Format | Spoken | +OOOO | ++++ OOOOO | +OOO | + OO | OOO | ++ | • One study reported participants found intervention “overwhelmingly” helpful
63
and another reported the interventions were well-received and helped patient feel more cared for
54
• Two case studies reported positive feedback from participants, including better symptom control, improved communication, reduced distress and promoted dignity and self-esteem 52 and a sense of release, closure and distraction, as well as facilitating patients entering into therapy. 53 |
|
| MDASI (2-8) | PHQ-9 (6) BDI (36) CES-D, IES (4-12) SCS (2-8) |
ESAS-pain (8) | QUAL-E (5) | PAIRI (2-8) MSIS, QMI (0) |
|||||
| Written | + | ++ OOO | + | + | O | + O - ** | None reported | ||
| FACT-G (12) | IES (12) ETS—anxiety (0) |
SSS (12) | Uptake MHS (12) | PSQI (up to 10) | |||||
| Flexible | + | None reported | |||||||
| Composite measure (12) | |||||||||
| Dose | One-off | O | + O | + O | OO | • One qualitative study reported the interventions were well-received and helped patient feel more cared for 54 | |||
| PHQ-9 (6) | ESAS-pain (8) | ||||||||
| Short term | ++ OOO | ++++++OOOOOOO | +O | + | + OOO | + OO - ** | ++ | • One study reported participants found intervention “overwhelmingly” helpful and could “relate as a whole person” (i.e. more than just their condition)
63
• One case study reported positive feedback from participants: a sense of release, closure and distraction, facilitation to enter therapy. 53 |
|
| FACT-G (12) MDASI (2-8) |
Composite measure(12) IES (12) BDI (36) CES-D, IES (4-12) SCS (2-8) ETS—anxiety (0) |
SSS (12) | Uptake MHS (8) | QUAL-E (5) | PSQI (up to 10) | PAIRI (2-8) MSIS, QMI (0) |
|||
| Long-Term | • One case study reported positive feedback from participant, including better symptom control, improved communication, reduced distress, and promoted dignity and self-esteem 52 | ||||||||
Key: +Study reported a significant difference between intervention and control group in favor of intervention on at least one measure in class.
−Study reported a significant difference between intervention and control group in favor of control on at least one measure in class.
O study reported no significant difference between intervention and control group on any measure in class.
The number of +/− in each column indicates the total number of studies that reported a significant difference between the intervention and control group in each class. For measures where a significant difference was identified in favor of the intervention (+), the outcome measures for which those differences were identified are listed. Measures used in the same study are separated by commas. Measures used in different studies are on separate lines.
BDI: beck depression inventory; CES-D: center for epidemiological studies depression scale; ESAS: Edmonton symptom assessment scale; ETS: emotion thermometer scale; FACT-G: functional assessment of cancer therapy- general; IES: impact of events scale; MDASI: MD Anderson symptom inventory; MHS: mental health services; MSIS: miller social intimacy scale; PAIRI: personal assessment of intimacy in relationships inventory; PHQ-9: personal health questionnaire-9; PSQI: Pittsburgh sleep quality index; QMI: quality of marriage index; QUAL-E: quality of life at the end of life; SCS: self-compassion scale; SSS: somatic symptom scale.
We describe results as effective based on statistical significance reported in the study, although we recognize that this is limited in that it provides no indication of the size or importance of an effect. Detailed results on the nature of the effect reported in each study are reported in Supplemental File 5. Only studies that were designed to evaluate efficacy were included in this part of the table.
EW participants with a longer duration of time since diagnosis exhibited increases in sleep disturbances.
Table 5.
Theoretical frameworks and underlying mechanisms of emotional disclosure-based interventions.
| Theories | Models and/or mechanisms |
|---|---|
| Communication | Patient–clinician communication models54,55 |
| Social and interpersonal | Social constraints inhibiting social-cognitive processing 78 and communication 68 |
| Social integration and interaction models33,60,57,68 | |
| Therapeutic value of game play 53 | |
| Supportive-expressive models52 | |
| Interdependence theory 33 | |
| Intimacy and relationship satisfaction62,67 | |
| Psychoanalytic | Inhibition and catharsis53,55,79 |
| Cognitive | Cognitive-processing mediation model and reappraisal models25,78 |
| Social constraints inhibiting social-cognitive processing 78 | |
| Emotion regulation 57 | |
| Emotional processing and awareness59,76,77 | |
| Information processing theories69,71 | |
| Cognitive-behavioral models 52 | |
| Life-stage and developmental | Continuity in chaotic illness model 78 |
| Biographical disruption model/reconstruction of personal narrative63,72,73,78 | |
| Health within illness model 78 | |
| Self | Self-compassion25,67,74 |
| Self-regulation of attention 67 | |
| Self-efficacy and enablement54,60,69,71 | |
| Non-directed client-centered approach69,71,75 | |
| Ego-functioning, self-esteem, and tolerance of negative affect 59 |
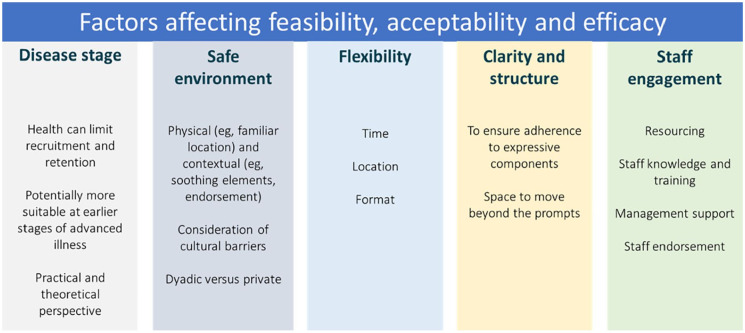
Figure 3.
Results of thematic analysis of implementation factors.
Quality appraisal
Study quality was graded by one author using the Hawker tool 50 and a subset of five was checked by another. Differences were resolved through discussion, and scoring amended as appropriate. In line with the grading used in prior reviews, scores ⩽18 are rated “poor,” scores from 19 to 27 “fair,” and ⩾28 “good.” 51 Quality appraisal is not a required component of scoping review methodology. 40 However, as one objective of this review was to map intervention characteristics to their reported efficacy, we recognized a value in assessing the quality of included studies to gauge the reliability of any links drawn from them.
Stage 6. Consultation
The scoping review was conducted collaboratively at all stages with the core research team, involving a palliative care consultant, a psychiatrist, health psychologist and researchers with expertise in emotional disclosure, palliative care research, and systematic reviewing. Clinical psychologists and a Patient and Public Involvement (PPI) representative were also consulted at key points.
Results
Characteristics of included studies
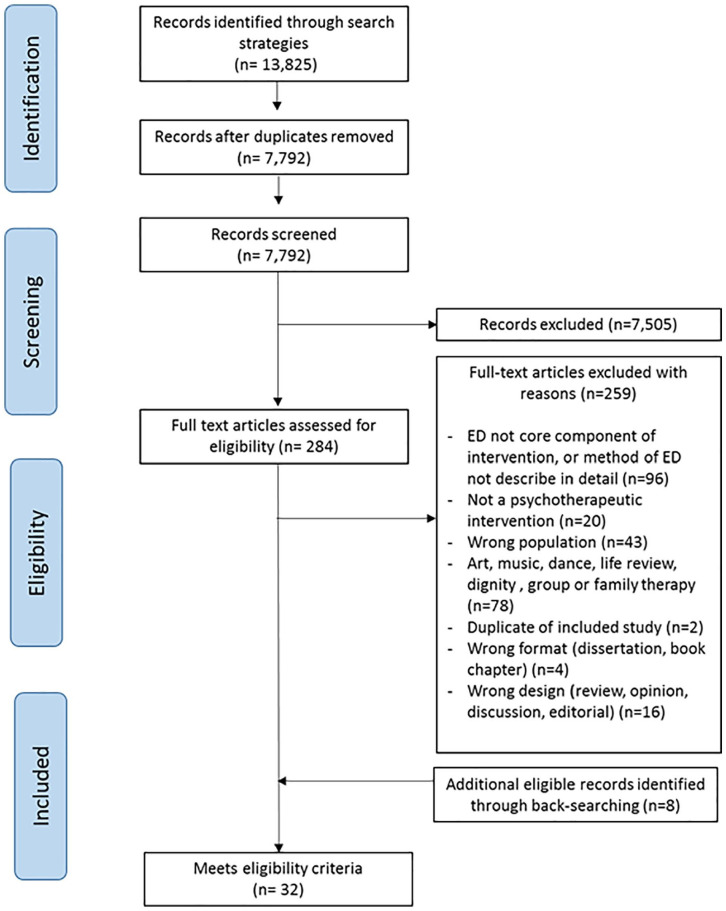
The literature search identified 7792 unique citations. Of these, 25 primary studies reported in 32 papers met the inclusion criteria (17 RCTs, 3 other studies reporting preliminary, secondary, or qualitative analyses of data from RCTs, and 5 other studies of different designs). Figure 1 presents a PRISMA flow diagram of study selection. Of the five studies using different designs,52–56 three used qualitative methods52–54 of which two were case studies;52,53 and two used mixed methods.55,56 Studies were conducted in four countries: USA (n = 18), UK (n = 5), China (n = 1), and Uruguay (n = 1). Most studies tested the intervention in people with advanced or incurable cancer (n = 19); other populations were people with amyotrophic lateral sclerosis (ALS) (n = 2), end stage renal disease (ESRD) (n = 1), and mixed terminal diagnoses (n = 3).
Figure 1.
PRISMA diagram of study selection.
Population and intervention characteristics are detailed in Table 2. More detailed study summaries are reported in Supplemental File 4.
Table 2.
Study and intervention characteristics.
| Reference | Description of intervention | Process of development |
|---|---|---|
| RCTs | ||
|
Arden-Close et al.
60
102 women at all stages of ovarian cancer (>50% at Stage III or IV) and their partners recruited via ovarian cancer charity UK |
Expressive writing (for couples)—based on Guided Disclosure Protocol (GDP)—instructions sent by post, and participant telephoned at designated time to instruct them to start writing, and again 15 min later telling them to stop Where: At home Dose: 15 min per day over 3 days within the same week (preferably consecutively). Patients and partners could write at the same or different times Topic: Patient’s diagnosis and treatment. Day 1: chronological description of event; Day 2: thoughts and feelings at the time of the event; Day 3: how they currently think and feel about the event, and reflections on future coping with a similar event. Who: Single researcher |
The intervention was based on GDP, a protocol developed by Duncan and Gidron
85
based on the cognitive processing hypothesis of trauma and tested in rheumatoid arthritis
86
and fibromyalgia.
87
Consultation with stakeholders not reported. |
|
Averill et al.
33
33 males and 15 females with amyotrophic lateral sclerosis (ALS) likely to survive for at least 6 months with good psychological health recruited via ALS registries US |
Written or spoken emotional disclosure—provided with written instructions for how to complete the exercise, suggestions (e.g. find a quiet place where you can write undisturbed) and paper on which to write and asked to either write (N = 10) or talk into a tape recorder (N = 8) Where: At home Dose: 20 min per day for 3 days over the period of a week Topic: Deepest feelings and thoughts related to their experience with ALS Who: Research nurse |
The development process was not reported; a range of EW interventions were cited in background (e.g. 16,61,87–89). Consultation with stakeholders not reported. |
|
Bruera et al.
66
15 females and 9 males with advanced gynecological and prostate cancer referred to palliative care or inpatient unit US |
Expressive writing—typed or handwritten Where: Remote (via phone call) but exact location not reported Dose: 20-min writing sessions, twice per week, for 2 weeks Topic: Their most upsetting experiences, important things about which they had the deepest feelings and thoughts about their cancer, and an event or experience that they had not talked about with others in detail Who: Research nurse |
The development process was not reported; cited EW interventions in the background.
61
Consultation with stakeholders not reported. |
|
De Moor et al.
61
36 males and 6 females with metastatic Stage IV Renal Cell Carcinoma recruited from a Phase II tumor vaccine trial with life expectancy more than 4 months US |
Expressive writing
Where: At each of the first four clinic visits while the patients waited to receive their vaccine treatment. Dose: 20 min session once a week for 4 weeks (first four clinic visits as part of trial) Topic: To write their deepest thoughts and feelings about their cancer. Specific prompts varied slightly from one session to the next but remained essentially the same. Who: Not reported |
Writing exercises followed the model developed by Pennebaker and Beall.
16
Consultation with stakeholders not reported. |
|
Imrie and Troop
13
8 females and 5 males with life-limiting illness or secondary cancer recruited from a Day Hospice UK |
Compassion-focussed expressive writing (CFEW) compared to expressive writing about stress without compassion instruction (control) Where: In a quiet room in the Day Hospice, at the same time as 1–6 other participants Dose: Two 20-min sessions, 1 week apart Topic: • Control condition—something they found stressful in the last week • Experimental condition—Stress + self-compassion—10 min writing on the stressful event, 10 writing with compassion to the self Who: Not reported |
Stakeholders involved in development: Day Hospice management informed the study design including the spacing of the writing sessions, the writing instructions, the support provided (e.g. pastoral support, informing care staff) and the measures used. This is the reason behind control group task (stress-only): the team felt writing about a neutral topic would be inappropriate. |
|
Lloyd Williams et al.
64
68 females and 32 males with advanced metastatic cancer (range of primary sites) at the end stage of their diseases recruited from hospice day units. UK |
Focussed narrative interview. A random selection were audio-recorded. Where: Not reported Dose: One off interview delivered at randomization or a few days later if requested. Length of interview not reported. Topic: Reflection on sense of meaning, wellbeing and suffering, what they believe to be the main cause of their suffering and any resources they use or professional care provided to maintain their wellbeing. Emphasis on allowing patients to “tell their story.” Who: Researcher delivers; training not reported but discussion notes intervention could be delivered by healthcare professionals with “training and supervision” |
Narrative therapy, dignity therapy, and supportive-expressive group therapy cited as background.90–93
Consultation with stakeholders not reported. |
|
Lloyd Williams et al.
35
39 females and 18 males with advanced cancer receiving palliative care from a hospice day care service with a prognosis between 6 weeks and 12 months, with clinical depression UK |
Focussed narrative semi-structured interview. A random selection were audio-recorded. Where: In hospice or patient’s home Dose: One off 25–60 min interview delivered within one week of randomization Topic: Sense of meaning regarding distress/depression and physical, psychological and spiritual well-being; what they felt had been the main factor contributing to depression/distress, the resources they had employed, and any medical/professional care received. Emphasis on reflection on inner resources and coping methods. Who: Trained researchers with a health background and experience in research with patients with advanced illness |
Developed from literature reviews, expert clinician consensus, and pilot work. Drew on Medical Research Council (MRC) framework for the development and evaluation of complex interventions. 26 |
|
Low et al.
58
62 women with stage IV metastatic breast cancer receiving any form of treatment, recruited from larger study from oncology clinics, community practices, and online mBC website US |
Expressive writing—After receiving the written materials, participants call the research office to schedule writing sessions. A trained research assistant telephones the woman at the start of each writing session to read the instructions to the participant, then calls again 20 min later to ask the participant to stop writing. Where: At home Dose: Four 20-min sessions within a 3-week interval at participant’s convenience Topic: Writing about cancer-related emotions Who: Trained research assistant |
Instructions were adapted from Pennebaker and Beall
16
and Stanton et al.
94
The research assistant telephone procedure was based on a protocol followed in previous expressive writing research with cancer patients and loved ones.95,96
Consultation with stakeholders not reported. |
|
Manne et al.
59
253 women with gynecological cancer (>50% advanced) recruited from cancer centers and hospitals US |
Spoken disclosure in Supportive Counselling—therapist using active but non-directive and non-interpretive techniques to facilitate emotional expression Where—At the oncology offices of the study site Dose—6 h-long sessions and a phone booster session 1 week after final session Topic—Reactions to their cancer Who—Trained social workers or psychologists with 5–15 years therapy experience |
Components of the Supportive Counselling intervention included those commonly used in Supportive Counselling and Emotion-Focused Therapy techniques. Consultation with stakeholders not reported. |
|
Manne et al.
75
; Manne et al.
76
; Virtue et al.
77
; Virtue et al.
80
252 women with gynecological cancer (>50% advanced) recruited from cancer centers and hospitals US |
Spoken disclosure in supportive counselling—as per Manne et al.
59
but “bolstered by training therapists to facilitate expression of emotional reactions and understanding them” and an additional session Where—At the oncology offices of the study site Dose—Seven hour-long sessions and a phone booster session 2–3 weeks after final session Topic—Experiences with and reactions to their cancer Who—Trained social workers, master-level or doctoral-level psychologists, or psychiatrists who were practicing in the community or employees of each cancer centre with between one and 34 years of therapy experience |
Components drawn from supportive counselling and emotion-focused therapy, intervention based on SC in Manne et al.
59
but with adaptations to facilitate emotional expression. Consultation with stakeholders not reported. |
|
Milbury et al.
68,74
38 females and 37 males with metastatic lung cancer (and their partners) recruited from a cancer centre US |
Online couple-based meditation with spoken emotional disclosure
Where—Session 1 is completed face-to-face or online via videoconferences depending on the participants’ availability. Sessions 2–4 are delivered via videoconferencing Dose—4 h long sessions over 4 weeks. Additional home materials (CDs, printed materials, exercises) and guidance to disclosure reflections to partner. At least one booster telephone call per week over the 4-week intervention period. The phone call is intended as a homework reminder and addresses any questions regarding the homework. Topic—Session 1: Mindful meditation focus (not emotional sharing focus); Session 2: Compassion and positive emotions and emotional disclosure task; Session 3: Gratitude and emotional disclosure; Session 4: Purpose and value-based living Who—A trained master’s level mind-body intervention specialist who is experienced in working with cancer patients and their families |
Based on mindfulness-based intervention literature for cancer and previous work in patients with stage I–III lung cancer and their partners
97
and integrating partner-assisted emotional disclosure, citing Porter et al.
62
Consultation with stakeholders not reported. Authors have conducted pilot work with metastatic lung cancer patients to inform and refine content. 56 |
|
Milbury et al.
67
16 females and 18 males with primary or metastatic brain tumors (>50% advanced) recruited from clinics US |
Online couple-based meditation with spoken emotional disclosure—sessions with therapist over FaceTime
Where—remote (online), exact location not reported Dose—Four weekly (60 min each) sessions. One third of each session dedicated to disclosure/reflection. Topic—Session 1: Mindful awareness of experiences; Session 2: Interconnectedness and feelings of compassion to themselves and their partner; Session 3: Things, events and people for which they are grateful; Session4: Value-based living (“What do you want your life to be about?”) Who—masters level licensed psychological counsellor intern |
Intervention was developed “building on existing evidence”; the emotional disclosure elements based on Porter et al.
62
partner-assisted emotional disclosure. Consultation with stakeholders not reported. |
|
Mosher et al.
57
87 women with metastatic (Stage IV) breast cancer attending comprehensive cancer centre with clinically elevated distress US |
Expressive writing—participants receive written instructions by post and are telephoned by research fellow prior to each session, then phoned back immediately after session. Overview of exercise provided before Session 1. Participants return essays to research team by post. Where: At home Dose: 20 min of writing, four sessions, over 4–7 weeks Topic: Deepest thoughts and feelings regarding the cancer Who: Research fellow |
Participants followed the protocol used by Zakowski et al.
98
for written emotional disclosure in cancer patients. Consultation with stakeholders not reported. |
|
Porter et al.
62
92 males and 38 females with gastrointestinal cancer (>50% advanced) (and their partners) recruited from hospital oncology clinics US |
Partner-assisted emotional disclosure—participants attend sessions with a trained therapist who guides the patient to describe the events and their feelings about a cancer-related experience that caused strong emotions; the partner is trained to listen supportively and receptively. Where: At the medical centre (although encouraged to continue the discussions at home) Dose: Four weekly sessions (session 1, 75 min; sessions 2–4, 45 min) spread over up to 8 weeks Topic: The events and feelings about cancer-related experiences that caused strong emotions Who: Trained master’s level therapist (social worker or psychologist) |
A novel intervention building on private emotional disclosure and the cognitive-behavioral marital literature. Consultation with stakeholders not reported. |
|
Steinhauser et al.
72,73
38 female and 44 male hospice patients with varying diagnoses and a prognosis of less than 6 months to live, recruited from inpatient and outpatient hospital, palliative care, and hospice settings 18 took part in qualitative interviews (2009). US |
Spoken disclosure (Outlook intervention) in semi-structured, audio-recorded interview. At the end of each session, participants were given a handout, printed on cardstock, which explored the session content to seed further reflection Where: In participants’ homes Dose: Three 45 min–1 h interviews, 1 week apart Topic: Issues related to life completion and preparation: Session 1: life review, accomplishments, proudest moments, and cherished times Session 2: issues of forgiveness, things they would have done differently, things left unsaid or undone. Session 3: lessons learned, heritage, and legacy Who: Research assistant trained not to give implicit or explicit messages or agenda of specific content/emotional disclosure |
Linking life review, emotional self-disclosure, and social gerontology literatures to inform development. A team of clinician and non-clinician researchers developed and refined Outlook’s content and structure. |
|
Steinhauser et al.
63
212 male and 9 female hospice ineligible advanced disease patients (to understand benefits in early palliative care context) recruited from outpatient clinics US |
Spoken disclosure (Outlook intervention)—as in Steinhauser 2008; 2009 Where: Not reported Dose: 3 interviews over the space of 1 month (typically 1 week apart). Topic: As in Steinhauser 2008; 2009 Who: Clinical social worker following manualized script and receiving ongoing supervision |
As in Steinhauser 2008;2009 |
|
Zhu et al.
65
6 males and 10 females with incurable cancer recruited from cancer clinics US |
Written disclosure in Creative Writing Workshops (“Write from the heart”)
Where: Not reported Dose: 2-h long weekly CWW × 4 weeks Topic: Express their feelings about random things in life and was not restricted to cancer-related topics Who: Professional writer |
Not reported; cite creative writing studies and workshops in the background. Consultation with stakeholders not reported. |
| Secondary analyses of RCTs | ||
|
Laccetti et al.
79
Descriptive, correlational secondary analysis of RCT 68 women with metastatic breast cancer and life expectancy >6 months recruited from medical centers, community centers, and private clinic US |
Written disclosure
Where: Place and time of participant’s choosing Dose: Writing for 20–30 min a day for four consecutive days Topic: Writing about experiences with metastatic breast cancer, thoughts, and feelings related to not fully recovering from cancer and facing death, and any other traumatic and upsetting experiences in life that may or may not relate to breast cancer. Who: Not reported; alludes to being an intervention that can be prescribed and guided by nurses |
Based on Pennebaker’s expressive writing/facilitated disclosure and cite studies that have used EW in people with cancer (non-advanced).
16
Consultation with stakeholders not reported. |
|
Leal et al.
78
Qualitative evaluation of EW texts from RCT 16 females and 21 males with renal cell carcinoma recruited from RCT of EW in people with renal cell carcinoma of all stages US |
Written disclosure
Where: Participants’ home Dose: Four 20 min writing sessions over a 10 days period; between 1 and 4 days between sessions Topic: Writing about illness and other fears in response to four prompts: 1: First told you had cancer or about making decisions about your treatment 2: Adjusting to your cancer, how it has changed your life, or how it has affected your family 3: Fears, worries and concerns you may be experiencing 4: Thoughts and feelings about the future, or your fears and worries about the treatment not working Who: Research assistant (training not reported) |
Pennebaker and Beall’s intervention informed the general writing procedures.
16
Pilot work with cancer patients informed modifications of the intervention.61,98,99 |
|
Rose et al.69,71; Radziewicz
70
Evaluation of RCT 110 males and 51 females with advanced cancer (median life expectancy of one year or less) recruited from two ambulatory cancer clinics US |
Spoken disclosure via telephone-based Coping and Communication Support (CCS) intervention Where: Flexible as telephone-based Dose: Flexible and tailored to patient preference (all receive an initial phone call within 2 weeks of initial consultation; monthly calls recommended for those with high levels of distress; CCS Practitioners on call 24/7 to take calls) Topic: Patient concerns (psychological, existential, practical, symptoms, caregiver burden) and communication issues (family and friends, healthcare providers) Who: Advanced practice nurses with mental health training (CCS Practitioners) |
Based on review of psycho-oncology interventions, including SUPPORT intervention (nurse discussions with patients and families about care decisions) and the informing theoretical frameworks.
100
Stakeholder consultation not reported |
| Non-RCTs | ||
|
Garcia Perez and Dapueto
52
Case study Female with advanced ALS Uruguay |
Spoken disclosure via computer-assisted psychotherapy
Where: Initially psychologist’s office, moving to patient’s home after 3 months Dose: Around 1 h, once a week, starting 4 months after diagnosis Topic: General trauma, client’s choice Who: Psychotherapist |
This psychotherapeutic approach was based on cognitive-behavioral and expressive supportive models and techniques. The technology is an adaptation of augmentative-alternative communication technologies to enhance patient’s speaking capabilities to facilitate psychotherapy. Stakeholder consultation not reported |
|
Milbury et al.
56
5 women and 8 men with primary or metastatic non-small cell lung cancer recruited from clinics US |
Couple-based meditation with spoken emotional disclosure
Where—Clinical consultation room in cancer centre Dose—Four hour long sessions over 2 weeks. Additional home materials (CDs, printed materials, exercises) also provided. Topic—Session 1: Mindful meditation focus (not emotional sharing focus); Session 2: Connection and loving-kindness for positive emotions; Session 3: Gratitude; Session 4: Purpose and value-based living Who—Master-level mind body specialist |
Based on principles of interdependence theory, mindfulness-based intervention literature, and related interventions developed for people with stage I–III lung cancer.
97
Intervention content evaluation part of study used to refine intervention based on participants’ written and oral feedback. |
|
Pon et al.
53
Case studies 5 hospice patients with terminal stage cancer with <6 months to live recruited from a hospice program China |
Spoken disclosure in context of playing “My Wonderful Life” (MWL) board game—participant moves along game board performing acts or picking an “Honest expression” card Where: Not reported Dose: Three sessions, each session 60–90 min long Topic: Life review and death preparation components: Making plans for leaving family members, saying final farewells, asking for forgiveness, showing appreciation for and leaving messages for others, recollections of personal contributions, strengths and wisdom, and contextualized perceived failures. Who: Therapist/facilitator |
Adapted from communication games used in other settings (trauma, pediatric populations).101,102
Stakeholder consultation not reported |
|
Taylor et al.
54
Qualitative evaluation 24 male and 12 female patients with end-stage renal disease recruited from routine outpatient clinic UK |
Spoken disclosure in response to either:
a. Patient Issues Sheet (n = 21) for participants to circle 2–3 main issues to discuss during consultation (Intervention 1) or b. Direct well-being question adapted from PHQ-9 (n = 20) (Intervention 2) Where: During consultations Dose: Single consultation Topic: Intervention 1: Emotional concerns related to illness that they would most like to talk about Intervention 2: Issues experience during the last week Who: Renal consultants who have completed training with renal psychologists covering motivational interviewing, open questions, affirmation and reflection, and three stage model of counselling |
Development process not reported. Consultation with stakeholders not reported. |
|
Tuck et al.
55
Mixed methods 4 male and 3 females with a diagnosis of terminal cancer recruited from palliative care unit US |
Narrative storytelling (spoken, audio-recorded and transcribed) through the PATS (Presence, Active Listening, Touch, Sacred story) intervention. Where: Private room in the palliative care unit or at home Dose: One interview spread over several 20–30 min sessions over 8–24 h (flexible depending of patient schedule and health) Topic: Experience of finding out they have cancer and there is no treatment or cure. If the following topics are not covered in the resulting story, probes were used exploring spirituality, sacred stories, healing, and change and growth Who: Initially by the principal investigator at the palliative care unit and latterly by a doctoral student trained in the protocol |
Developed by the first author/principal investigator based on spirituality and healing literature. Consultation with stakeholders not reported. |
CCS: coping and communication support; CFEW: compassion-focused expressive writing; EMO: emotional writing condition; EW: expressive writing; GDP: guided disclosure protocol; mBC: metastatic breast cancer; MWL: my wonderful life; NW: neutral writing; PATS: presence, active listening, touch, sacred story; PCU: palliative care unit; RCT: randomized controlled trial; RM: relaxation meditation; UC: usual care.
Quality appraisal
Of the 32 included papers, 20 were rated as “Good” and 10 as “Fair”; two were not in appropriate formats for quality appraisal (one protocol and one abstract). Supplemental File 5 presents a summary of ratings.
Multi-level taxonomy of emotional disclosure-based interventions
A multi-level taxonomy of emotional disclosure-based interventions is presented in Figure 2. Through iterative discussion and comparison, topic of disclosure, format of disclosure, and dose were identified as operative domains. Classes are proposed within each domain.
Primary objectives and outcome measures
Intervention objectives were grouped into the following classes (see Table 3): quality of life, care quality and access, psychological wellbeing, physical wellbeing, existential and spiritual wellbeing, sleep and fatigue, and interpersonal. In cases where studies did not explicitly state primary intervention objectives, the stated aim of the study was used. Classes were then mapped to study primary outcome measures. The most commonly explored class of primary objective (in 14 of 17 RCTs) was psychological wellbeing. Within that class, objectives and outcome measures varied, including a range of anxiety, depression, and overall distress measures. Across the studies, 41 different outcome measures were used to evaluate primary intervention objectives, and follow-up time-points ranged from immediately to 18 months post-intervention.
Significant positive effects were reported in RCTs for 17 different outcome measures (summarized in Table 4); at least one measure within each objective class reported a significant positive effect. However, results using each measure were not consistent across studies. Results are described as “effective” based on statistical significance, although it is recognized that this is limited in that it provides no indication of study quality or effect size. However, what is sought is consistency in findings across studies to guide the direction of future research, rather than making clinical recommendations. All study results are summarized in Supplemental File 4.
Mapping intervention classes to efficacy
Table 4 shows the mapping of classes within each domain in the taxonomy to study outcomes.
Topic of disclosure
In the majority of studies, participants were directed to express their feelings about their illness as at least one of the disclosure topics (n = 14). Of these, nine were trials, of which six reported significant positive effects on at least one outcome compared to control, including accessing mental health services, 57 psychological wellbeing,33,58,59 quality of life, 60 sleep, 61 physical symptoms, 61 and interpersonal relationships. 62 One RCT reported a significant negative effect of the intervention which directed people to express emotions about their illness. 58 This study found that there was a significant interaction between time since diagnosis and group: women in the intervention group with a longer time since diagnosis were more likely to report increased sleep disturbances at 3 months follow-up compared to those in the control group.
Six trials investigated interventions using general trauma or negative experiences as at least one of the disclosure topics. Of these, studies reported a significant improvement in existential and spiritual wellbeing, 63 pain, 64 depressive symptoms, and anxiety 65 compared to control. Two did not find any significant effects on any measure (although they were not powered to do so).25,66 Some interventions also asked people to express feelings on growth, ways of coping or positive emotions. Of these, significant positive effects versus control were reported on measures of quality of life,60,67 psychological wellbeing,35,67,68 physical wellbeing 64 and existential wellbeing, 63 as well as interpersonal relationships. 67 Most interventions asked participants to express feelings about a combination of different topics. In sum, no single topic or combination of topics was consistently related to a positive effect on any particular outcome.
Format of disclosure
Most studies (n = 15) investigated interventions asking people to express thoughts and feelings through spoken disclosure.35,52–56,59,62,63,67–77 Eight studies investigated written disclosure.57,58,60,61,65,66,78,79 Two studies explored flexible interventions, which gave participants the option of whether to speak or write,25,33 Table 2 gives a description of the nature of these interventions.
RCTs testing spoken interventions reported significant effects on quality of life, 67 depression, 35 cancer-related distress, 68 pain, 64 self-compassion, 67 existential/spiritual wellbeing, 63 and interpersonal relationships.62,67 Five RCTs investigating written interventions also reported significant effects compared to control on anxiety, 65 sleep, 61 uptake of mental health services, 57 intrusive thoughts, 58 somatic symptoms, 58 and quality of life. 60 Of the two RCTs that investigated a flexible intervention, one reported a significant improvement in psychological wellbeing 3 months post-intervention. 33 The other was a feasibility study not designed to evaluate efficacy. 25 In sum, there were no obvious patterns: all formats resulted in benefits in some outcomes.
Dose of disclosure
The majority of studies (n = 19) investigated short-term interventions (classified as 2–8 sessions) delivered over a time period of up to 2 months.25,33,53,56–63,65–68,72,73,75,78,79 Four studies investigated one-off interventions, two of which were RCTs that reported significant improvements in the emotional disclosure group compared to control (one on pain and one on depression).35,64 The other two studies (one case study, and one that did not report on efficacy) investigated longer term interventions delivered on an ongoing weekly or monthly basis and no defined number of sessions.52,69–71 Session length as well as the interval between sessions varied considerably (see Table 2). In sum, no links could be made between intervention dose and effectiveness. However, some studies did suggest that for interventions linking emotional processing and awareness to outcomes, more sessions over a longer time period may be needed to produce long-term effects.59,76,77
Overview of underlying mechanisms
The theories and models used to inform intervention development and explain potential effects are summarized in Table 5. Studies drew on a range of communication, social, psychoanalytic, cognitive, developmental and self-compassion theories, but rarely provided a full theoretical justification for each intervention characteristic. One found that low levels of emotional support and more recent diagnoses were associated with better responses to the intervention. 58 Another found that emotional disclosure increased quality of life only if illness-related couples’ communication also improved. 60 Studies reported contrasting findings relating to the role of natural expressivity. One study found high levels of baseline emotional expressivity were associated with a larger effect on depressive symptoms. 59 Others found high levels of holding back, 62 and ambivalence over emotional expression 33 were associated with larger effects. In sum, a number of studies investigated moderators of intervention effects to explore underlying mechanisms, with overall mixed findings.
Facilitators and barriers to feasibility and efficacy
This section reports the results of the thematic analysis of experience-based evidence where authors discuss their findings in relation to their intervention design and implementation. We identified five inter-related themes as important factors to consider in development of emotional disclosure-based interventions for palliative populations. These are summarized in Figure 3 and described below.
Impact of disease stage and type
Whilst all studies recruited people with advanced disease, the stage ranged from pre-palliative 63 to people receiving inpatient hospice care with less than 6 months to live.53,72,73 Participant health was often noted by authors as a factor limiting recruitment, retention, and adherence.25,33,35,55,60–62,64,66,72,73 Some suggested that emotional disclosure-based interventions may be more suitable for people at the earlier stages of advanced illness, as they may be more physically able to complete the intervention.25,66,72,73 Some study authors also suggested that emotional disclosure-based interventions may be more suitable for people who have not yet processed the trauma they are being asked to disclose; for example, those who had been relatively recently diagnosed, 58 who had experienced an acute stressor,33,57 or who had exhibited higher baseline levels of distress.57,61,63 However, others noted that short-term emotional disclosure-based interventions may not produce enduring effects due to the evolving nature of advanced illness, suggesting booster sessions as a possible solution. 75 And others suggested that the increased patient contact for people at an advanced stage of illness may in fact increase retention compared to those at an earlier stage of disease. 65
Ensuring a safe environment for disclosure
The importance of creating an environment where people feel comfortable to share difficult feelings was frequently highlighted.25,53–55,75,78,80 This related to the physical environment; for example, setting the intervention in a safe space, such as the participant’s home, or a private room. 25 It also referred to contextual factors, such as incorporating other soothing or positive elements that facilitate feelings of comfort53,55 and healthcare professionals endorsing the intervention and framing it as safe and trustworthy. 54 The importance of creating a safe environment extended to ensuring that family carers felt comfortable with the participant taking part in the intervention;33,55 this can be particularly salient in non-Western countries, such as China, where there are cultural barriers to expressing emotions. 53 Some noted that partner-based interventions improved retention and feasibility over private interventions,62,67 suggesting the presence of a partner may contribute to feeling safe and supported. However, challenges associated with dyads were also reported, such as inhibitions around disclosing emotions to a partner or worry about burdening them. 62
Flexibility of intervention
Flexibility in format and delivery was often noted as a facilitator. This is partially related to the variable health of participants and location of where people were receiving care; where expression sessions were held at structured times and places, participants were often not able to attend or complete the intervention due to illness or other appointments.25,63 Likewise, if the intervention was only delivered in a specific room at the hospice, it became less accessible for people who were unable to leave their home, or bed.25,55,66 The place where people feel most safe to disclose their emotions can also vary between individuals; thus it is important to provide flexibility about the intervention location. 25 Likewise, authors noted that there were individual differences in the format with which people felt comfortable disclosing their emotions, related to factors such as stage of disease,33,52 differences in education, or simply personal preference.25,54,66
Clarity and structure of instructions
A number of authors commented on clarity of instructions as an important factor in ensuring adherence to the core expressive components of the intervention, particularly for self-directed interventions.33,58,63,66 In one study it was noted that despite instructions asking participants to focus on their feelings, the tendency was to describe a factual account of their illness journey, undermining the emotional expression objective of the intervention. 66 Whilst a certain amount of structure and guidance on disclosure topics was highlighted as important, opportunity to move beyond the prompts and experience self-revelation was also highlighted as valuable.53,63 Another study highlighted that interventions with an unstructured format may be better suited to those with higher baseline emotional expressivity. 59 It was also suggested that building in additional supportive components, such as coping skills training, may help to optimally manage distress.59,75
Staff engagement and training
The importance of staff endorsement to build trust, staff knowledge, and management support were noted as key for successful implementation.54,55 Providing staff with information about the intervention was also noted to help allay their fears around how to respond to patients bringing up emotional concerns.54,69 Others highlighted that when delivering the intervention in the palliative care unit or hospice, there were interruptions from staff, and that there could be difficulties in finding an appropriate space, which may require management support.27,30 Finally, one study noted the importance of clear communication during the consent process, as some participants declined taking part because they did not feel entitled to further treatment for their mental wellbeing, since they were already receiving holistic care from their hospice team. 35
Discussion
Main findings
This scoping review developed a multi-level taxonomy, grouping emotional disclosure-based interventions for people with advanced disease into three operative domains: topic, format, and dose of disclosure. Within each domain, intervention characteristics were grouped into classes, and each class mapped to reported efficacy. An earlier systematic review already showed that the overall evidence of expressive writing efficacy is mixed. 24 The present review unpicked a broader range of emotional disclosure-based interventions to determine if there is any indication of which characteristic, or combination of characteristics, may hold the most therapeutic potential. Whilst there were no clear patterns in terms of which intervention characteristics in any domain were most effective, it was possible to identify a framework of potential key characteristics to guide further research.
Objectives and outcome measures
The objectives of emotional disclosure-based interventions varied, and included improvement of quality of life, as well as psychological, physical, and existential wellbeing. Most studies described the improvement of some aspect of psychological wellbeing as a primary objective. Many, though, provided vague descriptions of objectives. A range of outcome measures were employed to evaluate intervention efficacy, and follow-up time-points also varied. This reflects the uncertainty within the emotional disclosure and psychological intervention literature as a whole, on how best to evaluate such interventions.30,81 That said, these are holistic interventions and thereby impact is likely to be broad in terms of benefit.
Theoretical mechanisms
Authors drew on a wide range of psychological and social theories to inform and explain emotional disclosure-based intervention development and effect; this is similar to other reviews.29–31 However, these were rarely fully developed into causal mechanisms. Medical Research Council guidelines suggest that effective intervention development should be based on a clear understanding of its causal mechanisms.26,36 As emotional disclosure-based interventions vary across a number of domains, a single, cohesive theoretical framework to fit all emotional disclosure-based interventions is unlikely to be suitable. Rather, when developing interventions, researchers should focus on proposing theoretical accounts to justify the intervention design. Some studies in this review harnessed the potential of qualitative or linguistic analysis of disclosure texts to explore underlying mechanisms;25,55,76–79,80 this represents a potentially fruitful direction for future research. Such theoretical work can in turn inform appropriate outcome measure selection. In line with the wider psychosocial intervention literature, 82 findings highlight that there are likely to be individual differences in response to emotional disclosure. Clarifying the underlying mechanisms and individual differences in response to emotional disclosure-based intervention will ultimately help clinicians to decide which, if any, forms of emotional disclosure-based interventions are likely to work for which people.
Facilitators and barriers
The review identified five themes relating to facilitators of and barriers to emotional disclosure-based intervention implementation and efficacy: impact of disease stage; ensuring a safe environment; flexibility; clarity and structure of instructions; and staff engagement and training. When developing interventions for people with advanced disease, it is crucial to understand the specific environment where these interventions will be implemented, and to adjust them accordingly.26,36 Unless an intervention can be effectively implemented, it will not be effective on a wide scale. As such, it is recommended that future research developing emotional disclosure-based interventions for the palliative care setting should pay attention to the themes highlighted here, in combination with appropriate co-design work to develop practically implementable interventions. 83
Strengths and limitations
A systematic, six-stage process based on scoping review guidelines was undertaken to capture and map a broad body of literature. This review applied a pragmatic, novel approach (modified Intervention Component Analysis) to synthesize insights into intervention characteristics, evaluation approaches, theoretical frameworks, and implementation factors, including studies that used a range of study designs. By including studies that were not designed to assess efficacy (such as feasibility and pilot studies), it was also possible to capture information about acceptability and feasibility. However, this limited the possibility of drawing clear links between intervention characteristics and efficacy. Regardless of this decision, the heterogeneity of intervention objectives and outcome measures made efficacy synthesis challenging. In light of this, one core strength of the review was the capture and analysis of experience-based evidence. This provided important insights into key implementation factors that should be considered in the design of interventions, but which are often overlooked in more traditional evidence syntheses. As all papers were graded as “Good” or “Fair” quality, this lends a certain degree of credibility to this evidence. However, due caution should still be applied when considering its strength since much of this data is based on informal author reflections.
Studies evaluated interventions in a range of palliative settings and populations. This strengthens the generalizability and relevance of findings to palliative care services, which usually provide care for people with a range of diagnoses. However, whilst people living with advanced disease do share common experiences, some physical and psychological challenges are uniquely associated with specific conditions. Should researchers use insights from this review to inform intervention development, it would be important to consult with relevant stakeholders to ensure they address population and setting-specific factors on a more granular level. The majority of included studies were conducted in Western countries (US and UK). There can be significant cultural differences in the ways death, disease, and emotional expression are viewed.15,84 It is critical researchers consider this when interpreting or applying the results of this review in non-Western countries, or areas with multi-cultural populations.
Since emotional disclosure is a component of many formats of psychological therapy, there was sometimes a lack of clarity over what constitutes an emotional disclosure-based intervention. Despite employing a rigorous, discursive process to determine eligibility, some level of subjectivity about the selection of papers remained. However, the review was not designed to exhaustively capture every study that has ever been conducted in the field. Rather, it was designed to identify different types of intervention that could be classified as “emotional disclosure-based,” to systematically assess their characteristics and to identify the reasons why they may or may not be effective in palliative populations.
What this review adds
This review maps the range of emotional disclosure-based interventions tested in people with advanced disease and proposes a multi-level taxonomy classifying their core characteristics. This is important as these low-cost interventions have therapeutic potential in palliative care settings. The review could help researchers adopt a common language to describe emotional disclosure-based interventions for people with advanced disease (and perhaps beyond) and inform design of future research, including systematic reviews and meta-analyses. This paper describes paths for researchers to move forward with the development of interventions that can be practically implemented, drawing on key facilitators and barriers. It also provides recommendations into promising avenues for future intervention evaluation to help guide selection of appropriate outcome measures. Additionally, the paper acts as an exemplar of a review approach that may be used to inform development and evaluation of complex, multi-component interventions where pre-existing evidence is mixed.
Conclusion
Based on a systematic scoping of a diverse literature, this review has mapped and drawn links between emotional disclosure-based intervention characteristics, objectives, outcome measures, efficacy, and implementation factors. By drawing on the Intervention Component Analysis method, it was possible to integrate information not usually considered in traditional reviews of intervention efficacy. This has allowed the proposal of novel evidence-based recommendations for future research aiming to develop and evaluate emotional disclosure-based interventions in palliative populations.
Supplemental Material
Supplemental material, sj-docx-1-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-2-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-3-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-4-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-5-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-6-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Acknowledgments
The authors would like to thank Mr Peter Buckle and Dr Penny Rapaport for their thoughtful contributions to the review design. We would also like to thank the following people for their responses to requests for further information about their work: Dr Michael Antoni, Dr Linda Carlson, Dr Janine Giese-Davis, Dr Anna Gustafsson, Dr Monika Joshi, Dr Stuart McClean, Dr Judith Paice, Dr Laurie Rosen, Dr Friedrich Stiefel, Dr Sampoornam Webster, and Dr Joseph Winger.
Footnotes
Author contributions: All authors contributed to study and search strategy design and refinement of study selection criteria. DM, BC, NK, JC, and KA screened all records and full-texts. DM and BC developed the data extraction tool. DM extracted all data, and BC checked extraction of a subset. DM assessed the quality of included studies, and JC checked a subset. DM led data analysis. All authors were involved in checking and refining the analysis, writing the manuscript, and revising the final submission.
Data management and sharing: This review reports on data that already exists within the public domain and appropriate references are provided throughout the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The time spent on this review by author DM was supported by a Marie Curie and Economic and Social Research Council collaborative grant (grant number: ES/P000592/1). The time spent on the review by authors BC and PS comes from core funding of the research department by Marie Curie (grant number: MCCCFPO-16-U) and an Alzheimer’s Society (AS) funded fellowship awarded to NK (grant number: 399 AS-JF-17b-016). The time spent on the review by author KA comes from a grant provided by Faculty of Medicine, Prince of Songkla University, Thailand. The time spent on the review by author JC comes from a Marie Curie Chair’s Grant (grant number: 509537). The work of DM, BC, PS, NK, KA, and JC is also supported by the UCLH NIHR Biomedical Research Centre.
Ethics and consent: Ethics approval is not required since the study involves only secondary analysis of data that has already been collected and published.
ORCID iDs: Daisy McInnerney  https://orcid.org/0000-0002-8921-2215
https://orcid.org/0000-0002-8921-2215
Nuriye Kupeli  https://orcid.org/0000-0001-6511-412X
https://orcid.org/0000-0001-6511-412X
Kanthee Anantapong  https://orcid.org/0000-0003-3190-4355
https://orcid.org/0000-0003-3190-4355
Kate Flemming  https://orcid.org/0000-0002-0795-8516
https://orcid.org/0000-0002-0795-8516
Bridget Candy  https://orcid.org/0000-0001-9935-7840
https://orcid.org/0000-0001-9935-7840
Supplemental material: Supplemental material for this article is available online.
References
- 1. Buzgova R, Jarosova D, Hajnova E. Assessing anxiety and depression with respect to the quality of life in cancer inpatients receiving palliative care. Eur J Oncol Nurs 2015; 19(6): 667–672. [DOI] [PubMed] [Google Scholar]
- 2. Chan KY, Chan ML, Yau TCC, et al. Quality of life for Hong Kong Chinese patients with advanced gynecological cancers in the palliative phase of care: a cross-sectional study. J Palliat Care 2012; 28(4): 259–266. [PubMed] [Google Scholar]
- 3. Kim HS, Kim M, Lee SH. Symptom clusters in Korean patients with metastatic cancer undergoing palliative chemotherapy. J Hosp Palliat Nurs 2018; 18(4): 292–299. [Google Scholar]
- 4. Leroy T, Fournier E, Penel N, et al. Crossed views of burden and emotional distress of cancer patients and family caregivers during palliative care. Psychooncology 2016; 25(11): 1278–1285. [DOI] [PubMed] [Google Scholar]
- 5. British Psychological Society. Psychological best practice in inpatient services for older people. Leicester, UK: British Psychological Society, 2017. [Google Scholar]
- 6. Kalus C, Beloff H, Brennan J, et al. The role of psychology in end of life care. Leicester: The Professional Board of the British Psychological Society, 2008. [Google Scholar]
- 7. American Psychological Association. Resolution on palliative care and end-of-life issues and justification, https://www.apa.org. https://www.apa.org/about/policy/palliative-care-eol (2017, accessed 26 December 2019)
- 8. Connor SR, Sepulveda Bermedo MC. Global atlas of palliative care at the end of life. Worldwide Palliative Care Alliance. Geneva, Switzerland: World Health Organization, 2014. [Google Scholar]
- 9. Cherny NI, on behalf of the ESMO Guidelines Working Group. ESMO clinical practice guidelines for the management of refractory symptoms at the end of life and the use of palliative sedation. Ann Oncol 2014; 25(suppl 3): iii143–iii152. [DOI] [PubMed] [Google Scholar]
- 10. Russell C, Fountain A. Role of clinical psychology in UK hospices. BMJ Support Palliat Care 2020; 10(2): 196–200. [DOI] [PubMed] [Google Scholar]
- 11. Atkin N, Vickerstaff V, Candy B. ‘Worried to death’: the assessment and management of anxiety in patients with advanced life-limiting disease, a national survey of palliative medicine physicians. BMC Palliat Care 2017; 16(1): 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. WHCPA. WHPCA annual report 2018/19, http://www.thewhpca.org/resources/item/annual-report-2018-19 (2019, accessed 20 April 2020).
- 13. Hospice UK. Hospice accounts: analysis of the accounts of the UK charitable hospices for the year ended 21 March 2016, https://www.hospiceuk.org/what-we-offer/hospice-finance/benchmarking (2017, accessed 20 April 2020).
- 14. Hospice UK. Impact of cost pressures - findings April 2019. Hospice UK, 2019. [Google Scholar]
- 15. Lepore SJ, Smyth JM. The writing cure: an overview. In: Lepore SJ, Smyth JM. (ed.) The writing cure: how expressive writing promotes health and emotional well-being. Washington, DC: American Psychological Association; 2002, pp.3–14. [Google Scholar]
- 16. Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abnorm Psychol 1986; 95: 274–281. [DOI] [PubMed] [Google Scholar]
- 17. Smyth JM, Pennebaker JW. Exploring the boundary conditions of expressive writing: in search of the right recipe. Br J Health Psychol 2008; 13(1): 1–7. [DOI] [PubMed] [Google Scholar]
- 18. Frattaroli J. Experimental disclosure and its moderators: a meta-analysis. Psychol Bull 2006; 132(6): 823–865. [DOI] [PubMed] [Google Scholar]
- 19. Frisina PG, Borod JC, Lepore SJ. A meta-analysis of the effects of written emotional disclosure on the health outcomes of clinical populations. J Nerv Ment Dis 2004; 192(9): 629–634. [DOI] [PubMed] [Google Scholar]
- 20. Reinhold M, Bürkner P-C, Holling H. Effects of expressive writing on depressive symptoms-a meta-analysis. Clin Psychol Sci Pract 2018; 25(1): e12224. [Google Scholar]
- 21. Pavlacic J, Buchana E, Maxwell N, et al. A meta-analysis of expressive writing on posttraumatic stress, posttraumatic growth, and quality of life. Rev Gen Psychol 2019; 23(2): 230–250. [Google Scholar]
- 22. Merz EL, Fox RS, Malcarne VL. Expressive writing interventions in cancer patients: a systematic review. Health Psychol Rev 2014; 8(3): 339–361. [DOI] [PubMed] [Google Scholar]
- 23. Zhou C, Wu Y, An S, et al. Effect of expressive writing intervention on health outcomes in breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Ozakinci G, editor. PLoS One 2015; 10(7): e0131802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kupeli N, Chatzitheodorou G, Troop NA, et al. Expressive writing as a therapeutic intervention for people with advanced disease: a systematic review. BMC Palliat Care 2019; 18(1): 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Imrie S, Troop NA. A pilot study on the effects and feasibility of compassion-focused expressive writing in Day Hospice patients. Palliat Support Care 2012; 10(2): 115–122. [DOI] [PubMed] [Google Scholar]
- 26. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: following considerable development in the field since 2006, MRC and NIHR have jointly commissioned an update of this guidance to be published in 2019, https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/ (2006, accessed 8 January 2019).
- 27. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. O’Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019; 9(8): e029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sloan DM, Marx BP. Taking pen to hand: evaluating theories underlying the written disclosure paradigm. Clin Psychol Sci Pract 2004; 11(2): 121–137. [Google Scholar]
- 30. Pennebaker JW. Theories, therapies, and taxpayers: on the complexities of the expressive writing paradigm. Clin Psychol Sci Pract 2004; 11(2): 138–142. [Google Scholar]
- 31. Baikie KA, Wilhelm K. Emotional and physical health benefits of expressive writing. Adv Psychiatr Treat 2005; 11(5): 338–346. [Google Scholar]
- 32. Oh P-J, Kim SH. The effects of expressive writing interventions for patients with cancer: a meta-analysis. Oncol Nurs Forum 2016; 43(4): 468–479. [DOI] [PubMed] [Google Scholar]
- 33. Averill AJ, Kasarskis EJ, Segerstrom SC. Expressive disclosure to improve well-being in patients with amyotrophic lateral sclerosis: a randomised, controlled trial. Psychol Health 2013; 28(6): 701–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Davies EA. Why we need more poetry in palliative care. BMJ Support Palliat Care 2018; 8(3): 266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lloyd-Williams M, Shiels C, Ellis J, et al. Pilot randomised controlled trial of focused narrative intervention for moderate to severe depression in palliative care patients: DISCERN trial. Palliat Med 2018; 32(1): 206–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Evans CJ, Harding R, Higginson IJ; on behalf of MORECare. ‘Best practice’ in developing and evaluating palliative and end-of-life care services: a meta-synthesis of research methods for the MORECare project. Palliat Med 2013; 27(10): 885–898. [DOI] [PubMed] [Google Scholar]
- 37. Munn Z, Stern C, Aromataris E, et al. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 2018; 18: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8(1): 19–32. [Google Scholar]
- 39. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5(1): 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The Joanna Briggs Institute. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. Adelaide, Australia: The Joanna Briggs Institute; 2015. [Google Scholar]
- 41. McInnerney D, Kupeli N, Stone P, et al. Emotional disclosure as a therapeutic intervention in palliative care: a scoping review protocol. BMJ Open 2019; 9(8): e031046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hilliard RE. Music therapy in hospice and palliative care: a review of the empirical data. Evid Based Complement Alternat Med 2005; 2(2): 173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McConnell T, Porter S. Music therapy for palliative care: a realist review. Palliat Support Care 2017; 15(4): 454–464. [DOI] [PubMed] [Google Scholar]
- 44. Boehm K, Cramer H, Staroszynski T, et al. Arts therapies for anxiety, depression, and quality of life in breast cancer patients: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2014; 2014: 103297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wood MJM, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the management of symptoms in adults with cancer? A systematic review. Psychooncology 2011; 20(2): 135–145. [DOI] [PubMed] [Google Scholar]
- 46. Martínez M, Arantzamendi M, Belar A, et al. ‘Dignity therapy’, a promising intervention in palliative care: a comprehensive systematic literature review. Palliat Med 2017; 31(6): 492–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Keall RM, Clayton JM, Butow PN. Therapeutic life review in palliative care: a systematic review of quantitative evaluations. J Pain Symptom Manage 2015; 49(4): 747–761. [DOI] [PubMed] [Google Scholar]
- 48. Boutin DL. Effectiveness of cognitive behavioral and supportive-expressive group therapy for women diagnosed with breast cancer: a review of the literature. J Spec Group Work 2007; 32(3): 267–284. [Google Scholar]
- 49. Sutcliffe K, Thomas J, Stokes G, et al. Intervention component analysis (ICA): a pragmatic approach for identifying the critical features of complex interventions. Syst Rev 2015; 4(1): 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hawker S, Payne S, Kerr C, et al. Appraising the evidence: reviewing disparate data systematically. Qual Health Res 2002; 12(9): 1284–1299. [DOI] [PubMed] [Google Scholar]
- 51. Den Boer K, De Veer AJE, Schoonmade LJ, et al. A systematic review of palliative care tools and interventions for people with severe mental illness. BMC Psychiatry 2019; 19(1): 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. García Pérez AI, Dapueto JJ. Case report of a computer-assisted psychotherapy of a patient with ALS. Int J Psychiatry Med 2014; 48(3): 229–233. [DOI] [PubMed] [Google Scholar]
- 53. Pon AKL. My wonderful life: a board game for patients with advanced cancer. Illn Crisis Loss 2010; 18(2): 147–161. [Google Scholar]
- 54. Taylor F, Combes G, Hare J. Improving clinical skills to support the emotional and psychological well-being of patients with end-stage renal disease: a qualitative evaluation of two interventions. Clin Kidney J 2016; 9(3): 516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Tuck I, Johnson SC, Kuznetsova MI, et al. Sacred healing stories told at the end of life. J Holist Nurs Off J Am Holist Nurses Assoc 2012; 30(2): 69–80. [DOI] [PubMed] [Google Scholar]
- 56. Milbury K, Engle R, Tsao A, et al. Pilot testing of a brief couple-based mind-body intervention for patients with metastatic non-small cell lung cancer and their partners. J Pain Symptom Manage 2018; 55(3): 953–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mosher CE, Duhamel KN, Lam J, et al. Randomised trial of expressive writing for distressed metastatic breast cancer patients. Psychol Health 2012; 27(1): 88–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Low CA, Stanton AL, Bower JE, et al. A randomized controlled trial of emotionally expressive writing for women with metastatic breast cancer. Health Psychol Off J Div Health Psychol Am Psychol Assoc 2010; 29(4): 460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Manne S, Rubin S, Edelson M, et al. Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. - PsycNET. J Consult Clin Psychol 2007; 75(4): 615–628. [DOI] [PubMed] [Google Scholar]
- 60. Arden-Close E, Gidron Y, Bayne L, et al. Written emotional disclosure for women with ovarian cancer and their partners: randomised controlled trial. Psychooncology 2013; 22(10): 2262–2269. [DOI] [PubMed] [Google Scholar]
- 61. De Moor C, Sterner J, Hall M, et al. A pilot study of the effects of expressive writing on psychological and behavioral adjustment in patients enrolled in a Phase II trial of vaccine therapy for metastatic renal cell carcinoma. Health Psychol 2002; 21(6): 615–619. [DOI] [PubMed] [Google Scholar]
- 62. Porter LS, Keefe FJ, Baucom DH, et al. Partner-assisted emotional disclosure for patients with gi cancer: results from a randomized controlled trial. Cancer 2009; 115(18 Suppl): 4326–4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Steinhauser KE, Alexander S, Olsen MK, et al. Addressing patient emotional and existential needs during serious illness: results of the outlook randomized controlled trial. J Pain Symptom Manage 2017; 54(6): 898–908. [DOI] [PubMed] [Google Scholar]
- 64. Lloyd-Williams M, Cobb M, O’Connor C, et al. A pilot randomised controlled trial to reduce suffering and emotional distress in patients with advanced cancer. J Affect Disord 2013; 148(1): 141–145. [DOI] [PubMed] [Google Scholar]
- 65. Zhu J, Hussain M, Joshi A, et al. Effect of creative writing on mood in patients with cancer. BMJ Support Palliat Care 2020; 10(1): 64–67. [DOI] [PubMed] [Google Scholar]
- 66. Bruera E, Willey J, Cohen M, et al. Expressive writing in patients receiving palliative care: a feasibility study. J Palliat Med 2008; 11(1): 15–19. [DOI] [PubMed] [Google Scholar]
- 67. Milbury K, Weathers S-P, Durrani S, et al. Online couple-based meditation intervention for patients with primary or metastatic brain tumors and their partners: results of a pilot randomized controlled trial. J Pain Symptom Manage 2020; 59(6): 1260–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Milbury K, Li Y, Durrani S, et al. Results of a pilot randomized controlled trial: a couple-based meditation intervention for patients with metastatic lung cancer and their partners. J Clin Oncol 2019; 37(31_suppl): 135–135.30457920 [Google Scholar]
- 69. Rose JH, Radziewicz R, Bowmans KF, et al. A coping and communication support intervention tailored to older patients diagnosed with late-stage cancer. Clin Interv Aging 2008; 3(1): 77–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Radziewicz RM, Rose JH, Bowman KF, et al. Establishing treatment fidelity in a coping and communication support telephone intervention for aging patients with advanced cancer and their family caregivers. Cancer Nurs 2009; 32(3): 193–202. [DOI] [PubMed] [Google Scholar]
- 71. Rose JH, Bowman KF, Radziewicz RM, et al. Predictors of engagement in a coping and communication support intervention for older patients with advanced cancer: patient engagement in a coping and communication support intervention. J Am Geriatr Soc 2009; 57: s296–s299. [DOI] [PubMed] [Google Scholar]
- 72. Steinhauser KE, Alexander SC, Byock IR, et al. Seriously ill patients’ discussions of preparation and life completion: an intervention to assist with transition at the end of life. Palliat Support Care 2009; 7(4): 393–404. [DOI] [PubMed] [Google Scholar]
- 73. Steinhauser KE, Alexander SC, Byock IR, et al. Do preparation and life completion discussions improve functioning and quality of life in seriously ill patients? Pilot randomized control trial. J Palliat Med 2008; 11(9): 1234–1240. [DOI] [PubMed] [Google Scholar]
- 74. Milbury K, Tsao AS, Liao Z, et al. A research protocol for a pilot randomized controlled trial designed to examine the feasibility of a couple-based mind-body intervention for patients with metastatic lung cancer and their partners. Pilot Feasibility Stud 2018; 4(1): 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Manne SL, Virtue SM, Ozga M, et al. A comparison of two psychological interventions for newly-diagnosed gynecological cancer patients. Gynecol Oncol 2017; 144(2): 354–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Manne SL, Myers-Virtue S, Darabos K, et al. Emotional processing during psychotherapy among women newly diagnosed with a gynecological cancer. Palliat Support Care 2017; 15(4): 405–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Virtue SM, Manne S, Criswell K, et al. Levels of emotional awareness during psychotherapy among gynecologic cancer patients. Palliat Support Care 2019; 17(1): 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Leal I, Milbury K, Engebretson J, et al. Interconnection: a qualitative analysis of adjusting to living with renal cell carcinoma. Palliat Support Care 2018; 16(2): 146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Laccetti M. Expressive writing in women with advanced breast cancer. Oncol Nurs Forum 2007; 34(5): 1019–1024. [DOI] [PubMed] [Google Scholar]
- 80. Myers Virtue S, Manne SL, Darabos K, et al. Emotion episodes during psychotherapy sessions among women newly diagnosed with gynecological cancers: emotion episodes during psychotherapy with cancer patients. Psychooncology 2015; 24(9): 1189–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Guidi J, Brakemeier E-L, Bockting CLH, et al. Methodological recommendations for trials of psychological interventions. Psychother Psychosom 2018; 87(5): 276–284. [DOI] [PubMed] [Google Scholar]
- 82. De Villiers B, Lionetti F, Pluess M. Vantage sensitivity: a framework for individual differences in response to psychological intervention. Soc Psychiatry Psychiatr Epidemiol 2018; 53(6): 545–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Donetto S, Tsianakas V, Robert G. Using experience-based co-design to improve the quality of healthcare: mapping where we are now and establishing future directions. London: Kings College London; 2014. [Google Scholar]
- 84. Givler A, Maani-Fogelman PA. The importance of cultural competence in pain and palliative care. StatPearls. Treasure Island, FL: StatPearls Publishing; 2019. [PubMed] [Google Scholar]
- 85. Duncan E, Gidron Y. Written emotional expression and health: evidence for a new guided disclosure technique. In: Proceedings of the British Psychological Society. 1999. 29. [Google Scholar]
- 86. Broderick J, Stone A, Smyth J. et al. The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Ann Behav Med 2004; 27(1): 50–59. [DOI] [PubMed] [Google Scholar]
- 87. Broderick JE, Junghaenel DU, Schwartz JE. Written emotional expression produces health benefits in fibromyalgia patients. Psychosom Med 2005; 67(2): 326–334. [DOI] [PubMed] [Google Scholar]
- 88. Mann T. Effects of future writing and optimism on health behaviors in HIV-infected women. Ann Behav Med 2001; 23(1): 26–33. [DOI] [PubMed] [Google Scholar]
- 89. Kelley J, Lumley M, Leisen J. Health effects of emotional disclosure in rheumatoid arthritis patients. Health Psychol 1997; 16(4): 331–340. [DOI] [PubMed] [Google Scholar]
- 90. Noble A, Jones C. Benefits of narrative therapy: holistic interventions at the end of life. Br J Nurs 2005; 14(6): 330–333. [DOI] [PubMed] [Google Scholar]
- 91. Kissane DW, Grabsch B, Clarke DM, et al. Supportive-expressive group therapy for women with metastatic breast cancer: survival and psychosocial outcome from a randomized controlled trial. Psychooncology 2007; 16(4): 277–286. [DOI] [PubMed] [Google Scholar]
- 92. Carlick A, Biley FC. Thoughts on the therapeutic use of narrative in the promotion of coping in cancer care. Eur J Cancer Care 2004; 13(4): 308–317. [DOI] [PubMed] [Google Scholar]
- 93. Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol 2005; 23(24): 5520–5525. [DOI] [PubMed] [Google Scholar]
- 94. Stanton AL, Danoff-Burg S, Sworowski LA, et al. Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients. J Clin Oncol 2002; 20(20): 4160–4168. [DOI] [PubMed] [Google Scholar]
- 95. Bishop M, Lee G, Stanton A, et al. A Phase I study of telephone-based expressive writing for spouse/partner caregivers of HSCT survivors. 2004. [Google Scholar]
- 96. Zakowski S, Ramati A, Morton C, et al. Written emotional disclosure buffers the effects of social constraints on distress among cancer patients. Health Psychol 2004; 23(6): 555–563. [DOI] [PubMed] [Google Scholar]
- 97. Carlson LE, Doll R, Stephen J, et al. Randomized controlled trial of Mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J Clin Oncol 2013; 31(25): 3119–3126. [DOI] [PubMed] [Google Scholar]
- 98. de Moor J, Moye L, Low M, et al. Expressive writing as a presurgical stress management intervention for breast cancer patients. J Soc Integr Oncol Spring 2008; 6(2): 59–66. [PubMed] [Google Scholar]
- 99. Milbury K, Lopez G, Spelman A, et al. Examination of moderators of expressive writing in patients with renal cell carcinoma: the role of depression and social support. Psychooncology 2017; 26(9): 1361–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Lynn J, DeVries KO, Arkes HR, et al. Ineffectiveness of the SUPPORT intervention: review of explanations. J Am Geriatr Soc 2000; 48(S1): S206–S213. [DOI] [PubMed] [Google Scholar]
- 101. Ward-Wimmer D. Introduction: The healing potential of adults at play. In: Schaefer CE. (ed.) Play therapy with adults. Hoboken, NJ: John Wiley & Sons; 2003. [Google Scholar]
- 102. Webb NB. Groups for children traumatically bereaved by the attacks of September 11, 2001. Int J Group Psychother 2005; 55(3): 355–374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-2-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-3-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-4-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-5-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine
Supplemental material, sj-docx-6-pmj-10.1177_02692163211013248 for Emotional disclosure in palliative care: A scoping review of intervention characteristics and implementation factors by Daisy McInnerney, Nuriye Kupeli, Paddy Stone, Kanthee Anantapong, Justin Chan, Kate Flemming, Nicholas Troop and Bridget Candy in Palliative Medicine