Abstract
Background
Examining the analytical worth of the preoperative hemoglobin, albumin, lymphocyte, platelet (HALP) score and lymphocyte-to-monocyte ratio (LMR) within diseased persons having non-small cell lung cancer (NSCLC) after radical lung cancer surgery.
Methods
Clinical data concerning 238 diseased persons with NSCLC who underwent radical lung cancer resection within Nantong Cancer Hospital between January 2009 and October 2015 had been looking back studied. ROC curve had been employed in regulating optimal critical worth of HALP and LMR that had been 48.00 and 6.30 singly. A 5-year amplification observed survival concerning diseased persons, and clinicopathological stuff assessed using statistics procedure. Kaplan Meier method, log rank test had been exploited from the point of view to analyze for surviving, and Cox regression analysis had been exploited for univariate and multivariate analysis. Eventually, a nomogram had been produced to examine the confirmation internally.
Results
Kaplan Meier survival assessment revealed top HALP class’s overall survival (OS) was significantly higher than below HALP class’s (P<0.001), and high LMR group’s OS was also greater than below LMR class’s (P=0.001). Patients possessing average continuance period of 4 years. Further stratified study revealed high HALP class possessed notable OS as compared below HALP class (P=0.0002), and top LMR class possessed considerable OS as compared to below LMR class (P=0.003) in lung adenocarcinoma. In non-adenocarcinoma, there was no substantial difference in OS between two classes (P>0.05). Preoperative HALP and LMR remained independent risk constituents for tumor progression (P=0.005, P=0.028), lymph node metastasis and level of differentiation also had a certain effect on tumor progression (P<0.05), according to Cox multivariate analysis. Rise in HALP and LMR will help diseased persons having NSCLC live longer. The nomogram’s c-index in inside validation was 0.672 (95% confidence interval: 0.626–0.718).
Conclusions
Preoperative HALP versus LMR are independent predictive aspect within NSCLC diseased persons linked to clinicopathological features, and has a particular value in determining bodement.
Keywords: Non-small cell lung cancer (NSCLC); hemoglobin, albumin, lymphocytes, platelet score (HALP score); lymphocyte-to-monocyte ratio (LMR); overall survival (OS); prognosis; nomogram; risk factors
Introduction
Lung cancer seems to lead the large number of diseased persons to the valleys of death and morbidity alongside the most lethal malignant tumor (1,2). Despite the fact that non-small cell lung cancer (NSCLC) is responsible of 85% lung cancers (3), diseased persons having operable lesions have a highly variable. Diseased persons concerning level Ia non-small lung cancer have 73 percent 5-year survival rate, whereas those with stage IIIa have only a 24 percent 5-year survival rate (4). Furthermore, even though the pathological stage is the same and patients receive postoperative adjuvant chemotherapy, the prognosis remains uncertain. As a result, it’s important to screen non-small lung cancer diseased persons suffering the weak prognosis and treat them more vigorously in order to achieve the best outcomes. While a number of clinicopathological indicators, such as tumor size, lymph node metastasis (5), positive margin (6), can predict the prognosis of patients with NSCLC, more simple and precise biomarkers are needed to predict the disease’s prognosis.
Increasing record suggests the systemic inflammatory response is related to tumor characteristics such as proliferation, invasion, metastasis, and that its part is considerable within tumor occurrence and growth (7,8). Changes in tumor-related inflammatory cells show the degree of inflammatory response to tumors, and a higher inflammatory response often indicates a worse prognosis (9,10). Blood cells help tumor cells in the adaptive immune response by secreting a variety of cytokines that aid in various inflammatory processes (11). Recent research has shown that certain blood markers, such as the proportion concerning neutrophils to lymphocytes (NLR), platelets to lymphocytes (PLR), and the proportion lymphocytes to monocytes (LMR), all represent inflammatory changes in the tumor microenvironment (12-14). Further research has shown that a combination of these parameters can better predict a patient’s prognosis than a single index. The HALP amalgamated index, which is measured as haemoglobin (g/L) albumin (g/L) lymphocyte (/L)/platelet (/L), is linked to the survival rate of gastric cancer patients (15). However, no research on continuance, foretelling relating diseased persons possessed HALP and NSCLC have been conducted to date. As a result, function of undertaken article seems joining preoperative HALP and LMR to assess foretelling relating diseased persons suffering NSCLC.
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/atm-21-2120).
Methods
Clinical data
The Tumor Hospital Affiliated to Nantong University (Nantong, China) Ethics Committee (No.: LW2021003) approved the study, and all individual participants provided written informed consent. This research was carried out in conjunction with the Helsinki Declaration (as revised in 2013).
Experimental material 238 NSCLC diseased persons had radical resection at Nantong Cancer Hospital between January 2009 and October 2015 were chosen. The succeeding remained the conditions for inclusion: (I) patients were diagnosed with NSCLC in the beginning by receiving surgery; (II) no upper respiratory tract infection, urinary tract infection, malaise, several constituents create impacts outcomes concerning plasma repetitive inspection 30 days previously surgery; (III) routine plasma tests performed prior to surgery included lymphocyte, monocyte, hemoglobin, albumin, and platelet levels, and HALP and LMR were shaped; (IV) There was full clinical, pathological, and follow-up indication. All of the succeeding remained as prohibiting surroundings: diseased persons suffering positive pathological margin after surgery; diseased persons having antiquity of hematologic structure, autoimmune disease, or spiteful tumours; diseased persons having continuing uncooperative respiratory ailment, heart disaster, and several issues upsetting postoperative improvement; diseased persons suffering from many years preoperative radioactivity acquaintance Finally, 238 patients encompassed within report, having normal life of (62.3±8.4) years and 150 males and 88 females.
Research methods
Our hospital’s medical record management system was used to capture routine blood tests and the related clinicopathological results. The HALP and LMR were measured using lymphocyte, monocyte, haemoglobin, albumin, and platelet counts from routine blood and biochemical studies. The Youden index was determined using ROC curves affiliation among HALP, LMR, postoperative tumour movement in NSCLC patients. Owing to HALP and LMR values corresponding to the maximum value were chosen. Diseased persons remained then alienated among four classes: top HALP, below HALP, top LMR, and below LMR. clinicopathological stuff, continuance discrepancies within 2 classes were compared, and postoperative OS was used as the index of survival analysis. Instantaneously, single scalar and several scalar foretelling assessment had been run using expansion nomogram for producing foretelling scale to assess.
Follow-up
Outpatient reviews, re-admission medical records, and cell phone conferences employed to get feedback from diseased persons until October 2020. Chest CT, abdominal CT, tumour markers, blood cell examination, and liver and kidney function were among the follow-up products, and OS had been identified the disease’s finding to death of many reasons to deadline.
Statistical analysis
Stuff seemed to process through SPSS 22.0 statistical software. The best cut-off value had been calculated exploiting ROC curve, the measurement data had been expressed in and equated via a t-test. The chi-square test or Fisher’s exact probability test were used measuring count data, and the K.M method and log rank test organized for assessing effect on OS. A multivariate Cox comparative risks deterioration archetypal followed for integrating components that had statistical consequence within univariate scrutiny. Lastly, nomogram had been drawn and the prediction model was built using the R programming language. When (P<0.05), the difference was statistically important.
Results
The relationship between HALP, LMR, and tumor progression
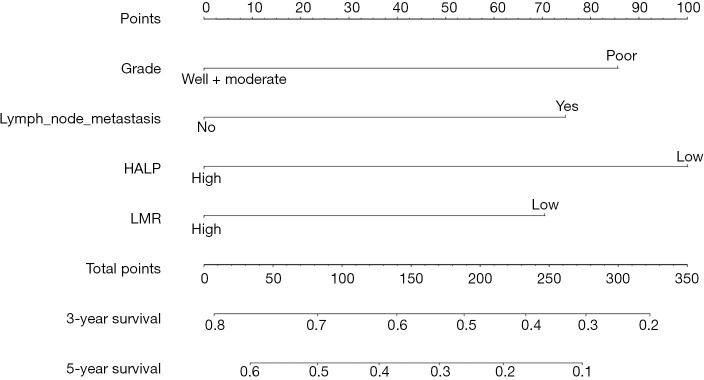
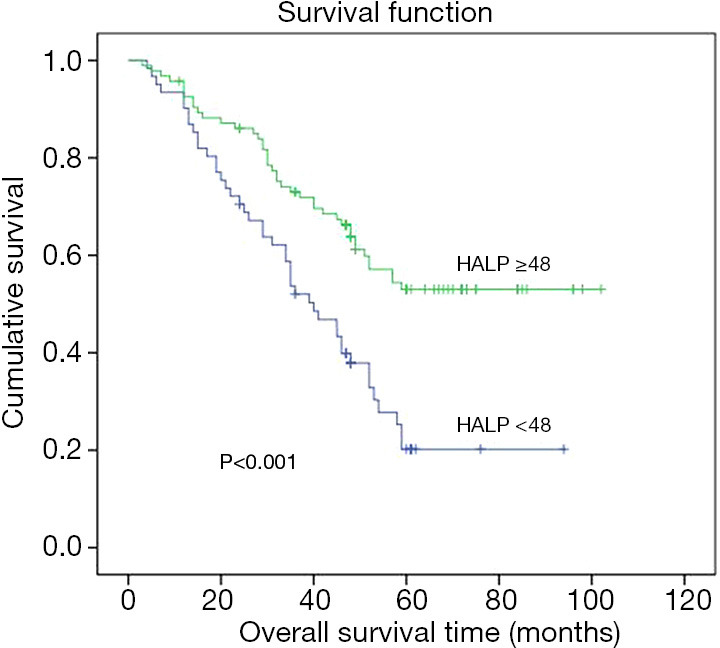
Figure 1 depicts the ROC curve for the relationship between HALP, LMR, and tumour movement within 238 diseased persons suffering from non-small lung cancer. ROC curve calculated that 48.0 was outstanding worth for HALP. Dividing diseased persons within 2 classes grounded upon whether their preoperative HALP was greater than 48.0: high HALP (n=139) and low HALP (n=99). The best LMR cut-off value was 6.3, and diseased persons had been categorized within 2 classes grounded upon whether their LMR was 6.3 or higher (n=63) or lower (n=175).
Figure 1.
Cutoff values for HALP and LMR as determined by the ROC curve. HALP, hemoglobin, albumin, lymphocyte, and platelet; LMR, lymphocyte-to-monocyte ratio.
Comparison of OS between the two groups
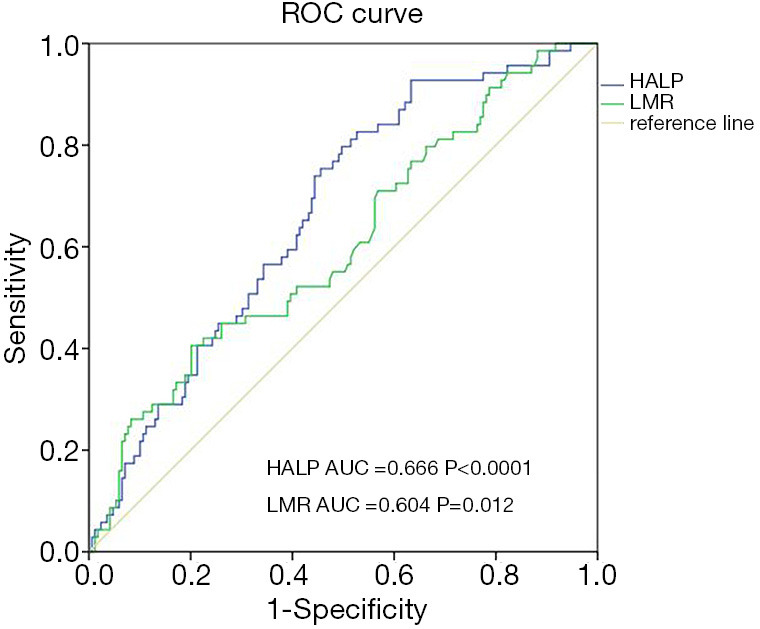
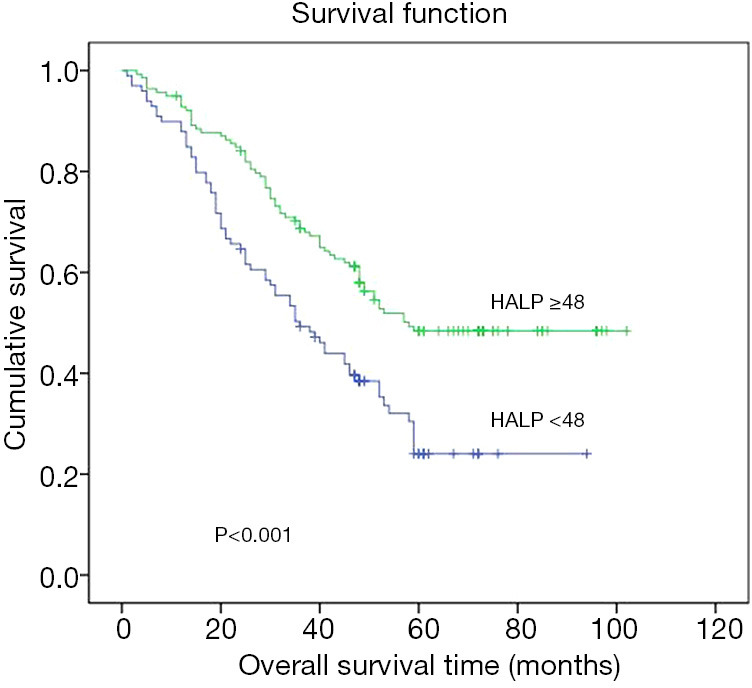
Related PFS information of the two groups was not perfect because certain patients did not receive the next phase of care in this hospital as their disease progressed. The findings of the K-Meier continuance work revealed that diseased persons within top HALP class had a notably better OS as compared to below HALP class (P<0.001), and diseased persons within top LMR class possessed considerable OS as compared to below LMR class (P=0.001). Average measurement break had been 4 years. Simultaneously, we discovered that, as shown in Figures 2-6, the earlier the pathological stage, the higher the gradation concerning discrepancy, and the absence of lymph node metastasis, the longer the patient’s OS.
Figure 2.
Kaplan-Meier curves for overall survival in patients with non-small cell lung cancer according to HALP. HALP, hemoglobin, albumin, lymphocyte, and platelet.
Figure 3.
Kaplan-Meier curves for overall survival in patients with non-small cell lung cancer according to LMR. LMR, lymphocyte-to-monocyte ratio.
Figure 4.
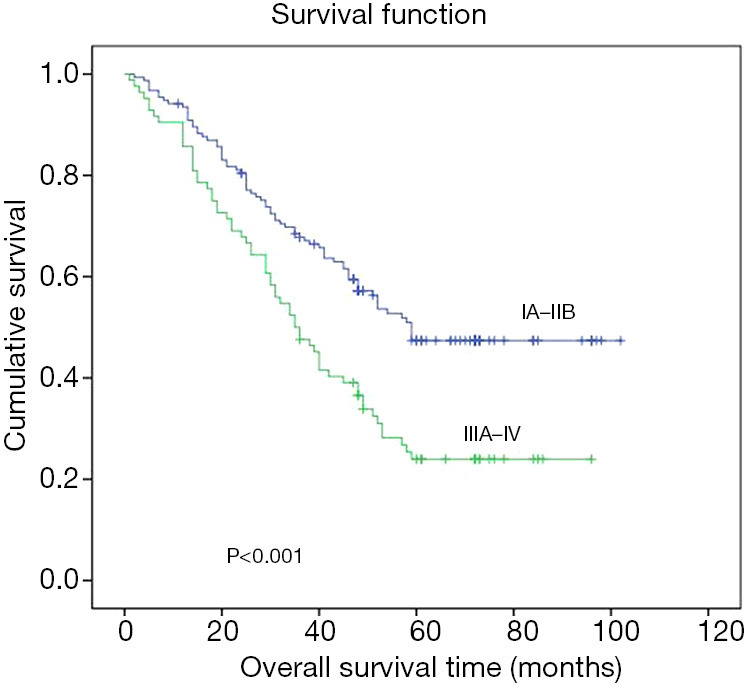
Kaplan-Meier curves for overall survival in patients with non-small cell lung cancer according to pathological stage.
Figure 5.
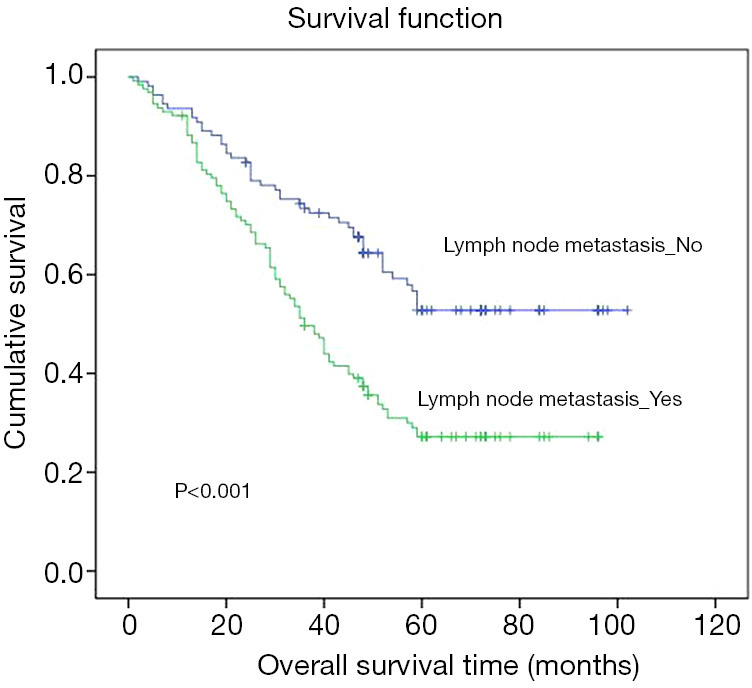
Kaplan-Meier curves for overall survival in patients with non-small cell lung cancer according to lymph node metastases.
Figure 6.
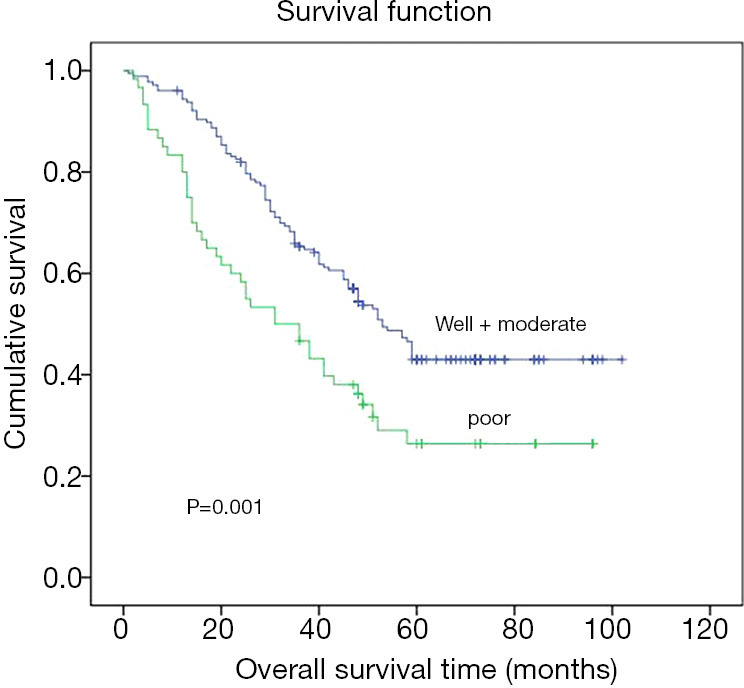
Kaplan-Meier curves for overall survival in patients with non-small cell lung cancer according to degree of differentiation.
Results of further stratified analysis
Further stratified study proved top HALP class possessed considerable OS as compared to below HALP class (P<0.001), and top LMR class possessed considerable OS as compared to below LMR class (P=0.003) in lung adenocarcinoma. In non-adenocarcinoma, there was no substantial difference in OS between two classes (P>0.05), as shown in Figures 7-10.
Figure 7.
Kaplan-Meier curves for overall survival in patients with lung adenocarcinoma according to HALP. HALP, hemoglobin, albumin, lymphocyte, and platelet.
Figure 8.
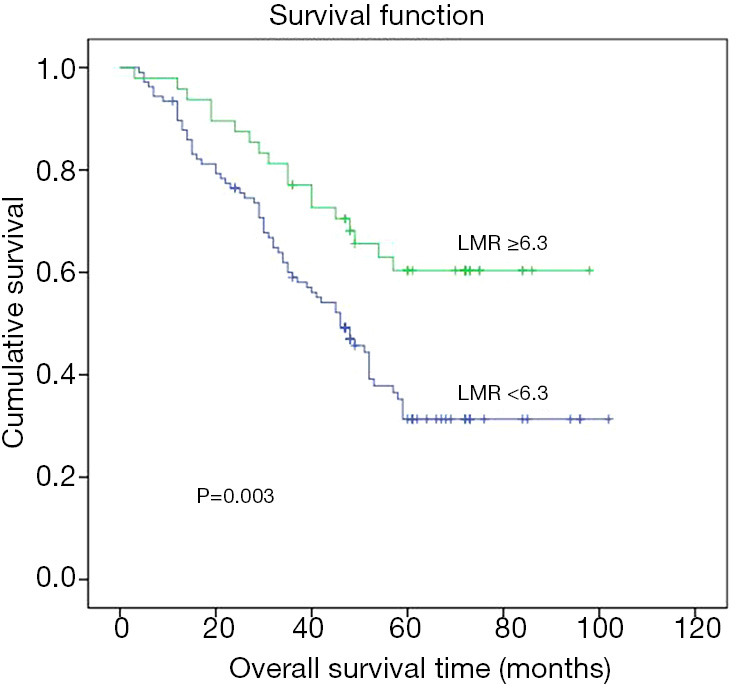
Kaplan-Meier curves for overall survival in patients with lung adenocarcinoma according to LMR. LMR, lymphocyte-to-monocyte ratio.
Figure 9.
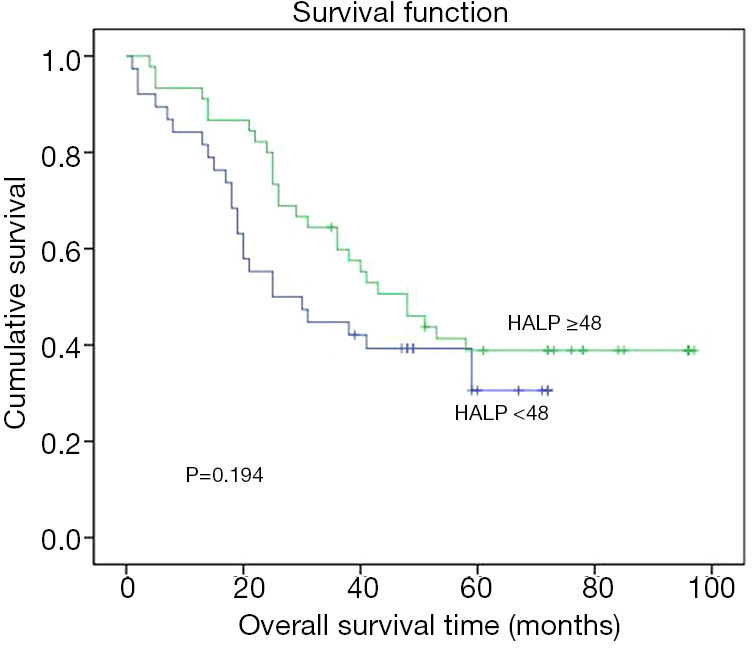
Kaplan-Meier curves for overall survival in patients with non-lung adenocarcinoma according to HALP. HALP, hemoglobin, albumin, lymphocyte, and platelet.
Figure 10.
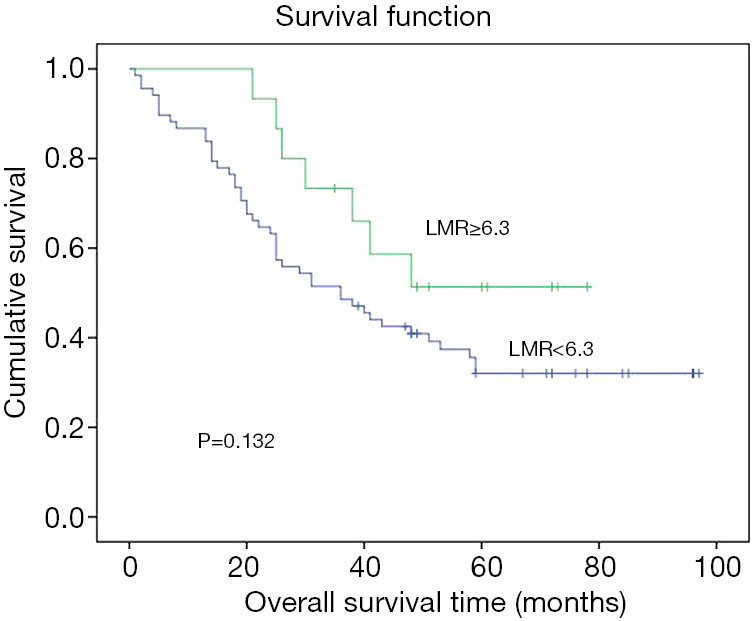
Kaplan-Meier curves for overall survival in patients with non-lung adenocarcinoma according to LMR. LMR, lymphocyte-to-monocyte ratio.
Patient and tumor characteristics
No substantial variation within the two classes within footings gender, smoking, drinking, category 2 diabetes, hypertension, lymph node metastasis, pathological type, differentiation degree, or clinical stage (P>0.05). Table 1 shows that major modifications within phase, gender, tumour size, and pathological type within top and below LMR classes (P<0.05).
Table 1. Relationship between preoperative HALP and LMR and the clinical-pathological data of patients.
| Characteristic | Total number, N (%) | HALP, N (%) | LMR, N (%) | |||||
|---|---|---|---|---|---|---|---|---|
| <48 | ≥48 | P | <6.3 | ≥6.3 | P | |||
| Age | 0.023 | 0.008 | ||||||
| ≥65 | 102 (42.0) | 51 (21.4) | 51 (21.4) | 84 (35.3) | 18 (7.6) | |||
| <65 | 136 (57.1) | 48 (20.2) | 88 (37.0) | 91 (38.2) | 45 (18.9) | |||
| Gender | 0.072 | <0.001 | ||||||
| Male | 150 (63.0) | 69 (29.0) | 81 (34.0) | 122 (51.3) | 28 (11.8) | |||
| Female | 88 (37.0) | 30 (12.6) | 58 (24.4) | 53 (22.3) | 35 (14.7) | |||
| Smoking history | 0.745 | 0.536 | ||||||
| Yes | 87 (36.6) | 35 (14.7) | 52 (21.8) | 66 (27.7) | 21 (8.8) | |||
| No | 151 (63.4) | 64 (26.9) | 87 (36.6) | 109 (45.8) | 42 (17.6) | |||
| Drinking history | 0.562 | 0.243 | ||||||
| Yes | 50 (21.0) | 19 (8.0) | 31 (13.0) | 40 (16.8) | 10 (4.2) | |||
| No | 188 (79.0) | 80 (33.6) | 108 (45.4) | 135 (56.7) | 53 (22.3) | |||
| Type 2 diabetes | 0.226 | 0.220 | ||||||
| Yes | 15 (6.3) | 4 (1.7) | 11 (4.6) | 9 (3.8) | 6 (2.5) | |||
| No | 223 (93.7) | 95 (39.9) | 128 (53.8) | 166 (69.7) | 57 (23.9) | |||
| Hypertension | 0.116 | 0.212 | ||||||
| Yes | 58 (24.4) | 19 (8.0) | 39 (16.4) | 39 (16.4) | 19 (8.0) | |||
| No | 180 (75.6) | 80 (33.6) | 100 (42.0) | 136 (57.1) | 44 (18.5) | |||
| Tumor size | 0.020 | 0.024 | ||||||
| ≥3 cm | 163 (68.5) | 76 (31.9) | 87 (36.6) | 127 (53.4) | 36 (15.1) | |||
| <3 cm | 75 (31.5) | 23 (9.7) | 52 (21.8) | 48 (20.2) | 27 (11.3) | |||
| Lymph node metastasis | 0.743 | 0.150 | ||||||
| Yes | 128 (53.8) | 52 (21.8) | 76 (31.9) | 99 (41.6) | 29 (12.2) | |||
| No | 110 (46.2) | 47(19.7) | 63 (26.5) | 76 (31.9) | 34 (14.3) | |||
| Pathological type | 0.338 | 0.032 | ||||||
| Adenocarcinoma | 155 (65.1) | 61 (25.6) | 94 (39.5) | 107 (45.0) | 48 (20.2) | |||
| Non-adenocarcinoma | 83 (34.9) | 38 (16.0) | 45 (18.9) | 68 (28.6) | 15 (6.3) | |||
| Degree of differentiation | 0.357 | 0.099 | ||||||
| Well + moderate | 178 (74.8) | 71 (29.8) | 107 (45.0) | 126 (52.9) | 52 (21.8) | |||
| Poor | 60 (25.2) | 28 (11.8) | 32 (13.4) | 49 (20.6) | 11 (4.6) | |||
| Pathological stage | 0.400 | 0.320 | ||||||
| IA–IIB | 154 (64.7) | 61 (25.6) | 93 (39.1) | 110 (46.2) | 44 (18.5) | |||
| IIIA–IV | 84 (35.3) | 38 (16.0) | 46(19.3) | 65 (27.3) | 19 (8.0) | |||
P<0.05 was statistically significant. HALP, hemoglobin, albumin, lymphocyte, and platelet; LMR, lymphocyte-to-monocyte ratio.
Univariate and multivariate analysis results
The influencing factors of OS (P<0.05) were lymph node metastasis, gradation of differentiation, pathological level, HALP, and LMR, according to univariate study. As shown in Tables 2 and 3, preoperative HALP and LMR remained independent risk aspects for tumor progression (P=0.005, P=0.028), while lymph node metastasis and degree of differentiation also had a certain effect on tumor progression (P<0.05).
Table 2. Univariate Cox regression analyses of prognosis of OS.
| Characteristic | HR (95% CI) | P |
|---|---|---|
| Age (<65, ≥65) | 1.119 (0.799–1.569) | 0.512 |
| Gender (male, female) | 1.367 (0.956–1.952) | 0.086 |
| Smoking history (no, yes) | 1.245 (0.883–1.754) | 0.211 |
| Drinking history (no, yes) | 1.308 (0.880–1.943) | 0.184 |
| Type 2 diabetes (no, yes) | 0.930 (0.473–1.829) | 0.833 |
| Hypertension (no, yes) | 0.807 (0.541–1.204) | 0.293 |
| Tumor size (<3 cm, ≥3 cm) | 1.249 (0.864–1.806) | 0.237 |
| Lymph node metastasis (no, yes) | 2.098 (1.473–2.990) | 0.00004 |
| Pathological type (adenocarcinoma, non-adenocarcinoma) | 1.293 (0.915–1.826) | 0.145 |
| Degree of differentiation (well + moderate, poor) | 1.816 (1.261–2.615) | 0.001 |
| Pathological stage (IA–IIB, IIIA–IV) | 1.871 (1.336–2.622) | 0.0003 |
| HALP (<48.0, ≥48.0) | 0.531 (0.379–0.744) | 0.0002 |
| LMR (<6.3, ≥6.3) | 0.482 (0.312–0.744) | 0.001 |
P<0.05 was statistically significant. OS, overall survival; HALP, hemoglobin, albumin, lymphocyte, and platelet; LMR, lymphocyte-to-monocyte ratio.
Table 3. Multivariate Cox regression analyses of prognosis of OS.
| Characteristic | HR (95% CI) | P |
|---|---|---|
| Degree of differentiation (well + moderate, poor) | 1.532 (1.059–2.215) | 0.023 |
| Lymph node metastasis (no, yes) | 1.905 (1.332–2.725) | 0.0004 |
| HALP (<48.0, ≥48.0) | 0.610 (0.433–0.860) | 0.005 |
| LMR (<6.3, ≥6.3) | 0.607 (0.389–0.947) | 0.028 |
P<0.05 was statistically significant. OS, overall survival; HALP, hemoglobin, albumin, lymphocyte, and platelet; LMR, lymphocyte-to-monocyte ratio.
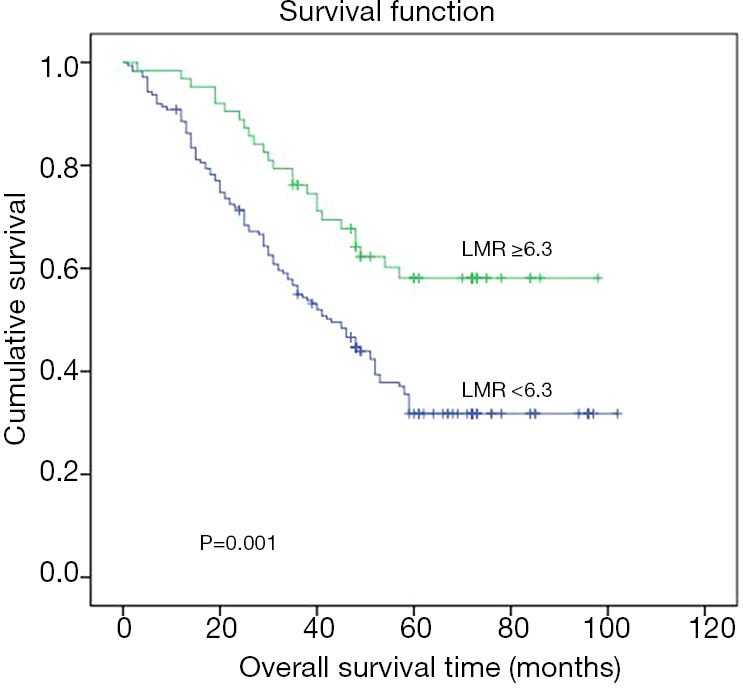
R language draws nomograms and builds predictive models
A nomogram could reliably forecast 3- and 5-year continuance charges relating diseased persons having HALP, LMR, lymph node metastasis, gradation relating distinction grounded upon outcomes relating Cox regression analysis. Furthermore, the nomogram’s c-index in internal endorsement remained 0.672 (95% CI: 0.626–0.718), suggesting that the prediction model had good prediction accuracy, as shown in Figure 11.
Figure 11.
Kaplan-Meier curves for overall survival in patients with non-lung adenocarcinoma according to LMR. LMR, lymphocyte-to-monocyte ratio.
Discussion
According to a global cancer epidemiological survey, lung cancer is the major reason that leads the diseased persons to morbidity and mortality. It has high occurrence rate concerning cancer-related death in the world (1,2,16). Lung cancer is classified into two types grounded upon pathological cataloguing: NSCLC and small cell lung cancer (SCLC). Adenocarcinoma (60%), sarcomatoid carcinoma, squamous cell carcinoma, and large cell lung cancer (17,18) are among 81 percent to 85 percent of lung cancers (3). Because of its large number, high degree of malignancy, and complex distribution of pathological forms, NSCLC seems the burning issue in clinical and scientific research (19-21).
We demonstrated that preoperative HALP and LMR are linked foretelling relating non-small lung cancer diseased persons after radical lung cancer surgery and are independent risk factors for non-small lung cancer foretelling within research. Developed nomogram can assist clinicians in identifying high-risk patients after surgery in a timely and accurate manner, as well as providing appropriate care options.
Many studies have found a connection between inflammation and nutritional status-related factors and cancer patient prognosis (22-24). Serum albumin degree can be used humble proxy indicator in examining the quantity of protein, a nutritional status gauge, and it has been linked to cancer survival in some studies (25,26). Below albumin levels (3.50 g/dL) were found in 16.5 percent relating bladder cancer patients subsequently deep-seated cystectomy, were significantly accompanying relating augmented hazard concerning demise (HR =1.76, P=0.04), according to Lambert et al. (27). A tumour, particularly one with a high degree of malignancy, is a chronic wasting disease. Anemia caused by cancer is another common complication among cancer patients. Iron deficiency, vitamin deficiency, and an increase in interleukins and tumour necrosis factor, both of which result in an inflammation imbalance, are common causes. Hemoglobin levels in cancer patients have been shown to be directly linked to survival and tumour development in studies (28). Anemia seems free foretelling component regarding cancer suffering people, stating by Caro et al. (29) who found that the risk of anemia-related death within prostate cancer sufferer augmented by 47 percent. Lympopenia is also common in advanced cancer patients and can hasten the disease’s progression (8,30). Platelet stimulation is linked to metastasis, and platelets can also protect cancer cells from immune attack (31).
The HALP score is a comprehensive index that measures a patient’s nutritional and immune health. In gastrointestinal cancer, esophageal squamous cell carcinoma (32), colorectal cancer (33), gastric cancer (15), and malignant tumours of the urinary system, it has been shown to have a prognostic impact (34,35). However, no fresh works looked into HALP score’s prognostic importance in victims having non-small lung cancer. It is proved by outcomes HALP is independent component prognostic factor for sufferers facing surgery of non-small lung cancer, and that an improvement in HALP can substantially improve NSCLC patients’ overall survival. Previous research has also shown that a decrease in HALP possessed weak foretelling within other tumors (32,35), which confirms our findings.
LMR has been shown to affect the postoperative foretelling concerning sufferers having non-small lung cancer during recent studies (36). Tumor cells’ immune microenvironment does the core part within the incidence and development relating tumours. Lymphocytes, especially T cells, have been shown to be important and linked to prognosis in studies. High levels of CD4+ T lymphocytes in the tumour stroma or tumour nests of NSCLC seem interrelated better OS, according to Geng et al. (37). This is consistent with Donnem et al. findings (38). Monocytes are also innate immune cells, as Olingy et al. (39) point out, and they do the core part within cancer movement. Monocytes can perform a variety of functions, including promoting blood vessel formation and secreting tumor-killing mediators, depending on which subgroup they belong to. Density of tumor-associated macrophages, which produces microenvironment conducive to cancer growth and is linked to weak prognosis, has been linked to the peripheral blood mononuclear cell count in other studies. As a result, in non-small lung cancer, LMR composed of two factors may have a better prognostic benefit.
Two measures were combined in this study to assess foretelling relating non-small lung cancer suffers and affiliation within preoperative HALP, LMR, OS. Lymph node metastasis, degree of differentiation, pathological level, HALP, and LMR were all found to be statistically significant using COX regression univariate analysis. Simultaneously, to avoid the effect of individual variables, we included all five in a multivariate study and discovered that preoperative HALP, LMR, lymph node metastasis, and degree of differentiation are independent prognostic factors of patients with NSCLC. The greater the HALP value, greater the LMR value, the higher the degree of differentiation, and the absence of lymph node metastasis in diseased persons relating non-small lung cancer, the longer the patient’s OS. At the same time, at least 50 patients in this study had one or more relapses, possibly indicating the potential for NSCLC to recur and develop, as well as the study’s positive clinical significance. We drew a nomogram and conducted internal verification based on the findings of the COX regression study to estimate the 3-year and 5-year survival rates concerning suffers having meagre lung cancer. C-index of the nomogram had been 0.672 (95% CI: 0.626–0.718) during internal verification, suggesting that the prediction model is accurate.
This research has some drawbacks, such as single-center design and a limited sample size. At same time, since this seems retrospective review, there may be biases in stuff collection and interpretation. Despite these flaws, this is the first research to show that HALP and LMR reductions indicate a poor prognosis within lung cancer victims.
Conclusions
For patients having non-small lung cancer, a decrease in preoperative HALP and LMR is an undesirable prognostic factor. To understand the exact mechanism of HALP and LMR in NSCLC, further multi-center, large-sample prospective studies are required.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: Jiangsu Province’s Scientific Research Project “333 Project” (BRA2019030), the Nantong Science and Technology Foundation grant (MS22019008), and the Nantong Science and Technology Plan Fund (MB2020016) provided assistance to carry out this research.
Ethical Statement: The writers are responsible for all aspects of the writing, including ensuring that any concerns about the work’s quality or credibility are thoroughly investigated and resolved. The Tumor Hospital Affiliated to Nantong University (Nantong, China) Ethics Committee (No.: LW2021003) approved the study, and all individual participants provided written informed consent. This research was carried out in conjunction with the Helsinki Declaration (as revised in 2013).
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/atm-21-2120
Data Sharing Statement: Available at https://dx.doi.org/10.21037/atm-21-2120
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/atm-21-2120). The authors have no conflicts of interest to declare.
(English Language Editor: B. Draper)
References
- 1.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. 10.3322/caac.21262 [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- 3.Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 2019;69:363-85. 10.3322/caac.21565 [DOI] [PubMed] [Google Scholar]
- 4.Wu GX, Raz DJ. Lung Cancer Screening. Cancer Treat Res 2016;170:1-23. 10.1007/978-3-319-40389-2_1 [DOI] [PubMed] [Google Scholar]
- 5.Li ZM, Ding ZP, Luo QQ, et al. Prognostic significance of the extent of lymph node involvement in stage II-N1 non-small cell lung cancer. Chest 2013;144:1253-60. 10.1378/chest.13-0073 [DOI] [PubMed] [Google Scholar]
- 6.Predina JD, Keating J, Patel N, et al. Clinical implications of positive margins following non-small cell lung cancer surgery. J Surg Oncol 2016;113:264-9. 10.1002/jso.24130 [DOI] [PubMed] [Google Scholar]
- 7.Colotta F, Allavena P, Sica A, et al. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis 2009;30:1073-81. 10.1093/carcin/bgp127 [DOI] [PubMed] [Google Scholar]
- 8.Mantovani A, Allavena P, Sica A, et al. Cancer-related inflammation. Nature 2008;454:436-44. 10.1038/nature07205 [DOI] [PubMed] [Google Scholar]
- 9.Jeong JH, Lim SM, Yun JY, et al. Comparison of two inflammation-based prognostic scores in patients with unresectable advanced gastric cancer. Oncology 2012;83:292-9. 10.1159/000342376 [DOI] [PubMed] [Google Scholar]
- 10.Proctor MJ, Morrison DS, Talwar D, et al. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 2011;47:2633-41. 10.1016/j.ejca.2011.03.028 [DOI] [PubMed] [Google Scholar]
- 11.Varga G, Foell D. Anti-inflammatory monocytes-interplay of innate and adaptive immunity. Mol Cell Pediatr 2018;5:5. 10.1186/s40348-018-0083-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong YF, Chen ZH, Wei L, et al. Identification of the prognostic value of lymphocyte-to-monocyte ratio in patients with HBV-associated advanced hepatocellular carcinoma. Oncol Lett 2017;14:2089-96. 10.3892/ol.2017.6420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magdy M, Hussein T, Ezzat A, et al. Pre-treatment Peripheral Neutrophil-Lymphocyte Ratio as a Prognostic Marker in Gastric Cancer. J Gastrointest Cancer 2019;50:763-8. 10.1007/s12029-018-0144-x [DOI] [PubMed] [Google Scholar]
- 14.Wang Y, Huang D, Xu WY, et al. Prognostic Value of Pretreatment Lymphocyte-to-Monocyte Ratio in Non-Small Cell Lung Cancer: A Meta-Analysis. Oncol Res Treat 2019;42:523-31. 10.1159/000501726 [DOI] [PubMed] [Google Scholar]
- 15.Chen XL, Xue L, Wang W, et al. Prognostic significance of the combination of preoperative hemoglobin, albumin, lymphocyte and platelet in patients with gastric carcinoma: a retrospective cohort study. Oncotarget 2015;6:41370-82. 10.18632/oncotarget.5629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1684-735. 10.1016/S0140-6736(18)31891-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inamura K. Lung Cancer: Understanding Its Molecular Pathology and the 2015 WHO Classification. Front Oncol 2017;7:193. 10.3389/fonc.2017.00193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen I, Warth A. Lung cancer: developments, concepts, and specific aspects of the new WHO classification. J Cancer Res Clin Oncol 2016;142:895-904. 10.1007/s00432-015-2004-4 [DOI] [PubMed] [Google Scholar]
- 19.Dy GK, Prasad D, Kumar P, et al. A Phase 2 Randomized, Double-Blind, Placebo-Controlled Study Evaluating Nintedanib Versus Placebo as Prophylaxis Against Radiation Pneumonitis in Patients With Unresectable NSCLC Undergoing Chemoradiation Therapy. J Thorac Oncol 2021;16:e19-20. 10.1016/j.jtho.2020.11.019 [DOI] [PubMed] [Google Scholar]
- 20.Remon J, Hendriks LEL. Osimertinib Should be the Standard of Care for the Adjuvant Therapy of Stage IB to IIIA EGFR-Mutant NSCLC. J Thorac Oncol 2021;16:368-70. 10.1016/j.jtho.2020.11.027 [DOI] [PubMed] [Google Scholar]
- 21.Song L, Xu Q, Lizaso A, et al. Brigatinib After Progression From Alectinib or Crizotinib: Paving the Way for Treatment Sequencing of ALK Inhibitors in ALK-Positive NSCLC. J Thorac Oncol 2021;16:349-51. 10.1016/j.jtho.2020.11.023 [DOI] [PubMed] [Google Scholar]
- 22.Lu H, Ouyang W, Huang C. Inflammation, a key event in cancer development. Mol Cancer Res 2006;4:221-33. 10.1158/1541-7786.MCR-05-0261 [DOI] [PubMed] [Google Scholar]
- 23.Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 2012;62:243-74. 10.3322/caac.21142 [DOI] [PubMed] [Google Scholar]
- 24.McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 2009;12:223-6. 10.1097/MCO.0b013e32832a7902 [DOI] [PubMed] [Google Scholar]
- 25.Liu X, Meng QH, Ye Y, et al. Prognostic significance of pretreatment serum levels of albumin, LDH and total bilirubin in patients with non-metastatic breast cancer. Carcinogenesis 2015;36:243-8. 10.1093/carcin/bgu247 [DOI] [PubMed] [Google Scholar]
- 26.Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 2010;9:69. 10.1186/1475-2891-9-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lambert JW, Ingham M, Gibbs BB, et al. Using preoperative albumin levels as a surrogate marker for outcomes after radical cystectomy for bladder cancer. Urology 2013;81:587-92. 10.1016/j.urology.2012.10.055 [DOI] [PubMed] [Google Scholar]
- 28.Belcher DA, Ju JA, Baek JH, et al. The quaternary state of polymerized human hemoglobin regulates oxygenation of breast cancer solid tumors: A theoretical and experimental study. PLoS One 2018;13:e0191275. 10.1371/journal.pone.0191275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caro JJ, Salas M, Ward A, et al. Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer 2001;91:2214-21. [DOI] [PubMed] [Google Scholar]
- 30.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 2016;66:271-89. 10.3322/caac.21349 [DOI] [PubMed] [Google Scholar]
- 31.Zhang GM, Zhu Y, Luo L, et al. Preoperative lymphocyte-monocyte and platelet-lymphocyte ratios as predictors of overall survival in patients with bladder cancer undergoing radical cystectomy. Tumour Biol 2015;36:8537-43. 10.1007/s13277-015-3613-x [DOI] [PubMed] [Google Scholar]
- 32.Cong L, Hu L. The value of the combination of hemoglobin, albumin, lymphocyte and platelet in predicting platinum-based chemoradiotherapy response in male patients with esophageal squamous cell carcinoma. Int Immunopharmacol 2017;46:75-9. 10.1016/j.intimp.2017.02.027 [DOI] [PubMed] [Google Scholar]
- 33.Jiang H, Li H, Li A, et al. Preoperative combined hemoglobin, albumin, lymphocyte and platelet levels predict survival in patients with locally advanced colorectal cancer. Oncotarget 2016;7:72076-83. 10.18632/oncotarget.12271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peng D, Zhang CJ, Tang Q, et al. Prognostic significance of the combination of preoperative hemoglobin and albumin levels and lymphocyte and platelet counts (HALP) in patients with renal cell carcinoma after nephrectomy. BMC Urol 2018;18:20. 10.1186/s12894-018-0333-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peng D, Zhang CJ, Gong YQ, et al. Prognostic significance of HALP (hemoglobin, albumin, lymphocyte and platelet) in patients with bladder cancer after radical cystectomy. Sci Rep 2018;8:794. 10.1038/s41598-018-19146-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mandaliya H, Jones M, Oldmeadow C, et al. Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl Lung Cancer Res 2019;8:886-94. 10.21037/tlcr.2019.11.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geng Y, Shao Y, He W, et al. Prognostic Role of Tumor-Infiltrating Lymphocytes in Lung Cancer: a Meta-Analysis. Cell Physiol Biochem 2015;37:1560-71. 10.1159/000438523 [DOI] [PubMed] [Google Scholar]
- 38.Donnem T, Hald SM, Paulsen EE, et al. Stromal CD8+ T-cell Density—A Promising Supplement to TNM Staging in Non-Small Cell Lung Cancer. Clin Cancer Res 2015;21:2635-43. 10.1158/1078-0432.CCR-14-1905 [DOI] [PubMed] [Google Scholar]
- 39.Olingy CE, Dinh HQ, Hedrick CC. Monocyte heterogeneity and functions in cancer. J Leukoc Biol 2019;106:309-22. 10.1002/JLB.4RI0818-311R [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as