Abstract
Purpose
Severe cardiogenic shock is the major driver of mortality on cardiologic intensive care units. Novel therapeutic options like extracorporeal membrane oxygenation (ECMO) or the combination of ECMO and a percutaneous microaxial pump like Impella CP (ECMELLA) are promising Options. Here we want to focus on the question what happens when left ventricular preload is too low to unload in cardiogenic shock in patients with ECMELLA and this aspect is illustrated by transesophageal echocardiography.
Methods
We detail a case of a 43‐year‐old active smoker who was admitted for acute myocardial infarction causing severe cardiogenic shock and who was finally treated with ECMELLA. Transesophageal echocardiography is used to illustrate what happens when left ventricle (LV) preload is too low to unload.
Results
Transesophageal echocardiography demonstrates complete collapse of LV and LA as consequence of increased but still low flow rate of the coaxial pump.
Conclusion
Novel therapeutic options like ECMO and percutaneous microaxial pumps like Impella CP, 5.0 or the combination of both (ECMELLA), are promising options. Whether these approaches reduce mortality has to be evaluated in urgently needed randomized trials but results will not be available in the next few years.
A 43‐year‐old active smoker was admitted for acute myocardial infarction (peak creatine kinase of 11 000 U/L) with thrombotic occlusion of dominant left circumflex and concomitant chronic occlusion of the left anterior descending causing severe cardiogenic shock (CS). After recanalization of the left circumflex a veno‐arterial extracorporeal membrane oxygenation (ECMO) was implanted due to progressive hemodynamic instability and high catecholamine dosages. The patient was transferred to our intensive care unit (ICU), specialized in ECMO treatment for CS. At admission on ICU severe pulmonary congestion was already present. Hence, a coaxial pump (Impella, Abiomed, Germany)—capable of pumping up to 3.5 L/min of blood—was implanted to unload the left ventricle (LV). 1 , 2 Unfortunately, even with a low flow Impella rate of 1.6 L/min, LV and left atrium (LA) were completely emptied (Figure 1) due to low LV filling, right ventricular failure and limited volume therapy as a consequence of severe pulmonary congestion with FiO2 of 100%. Consecutively the coaxial pump lowered flow automatically to 0.6 L/min and could not reduce pulmonary edema. 3
FIGURE 1.
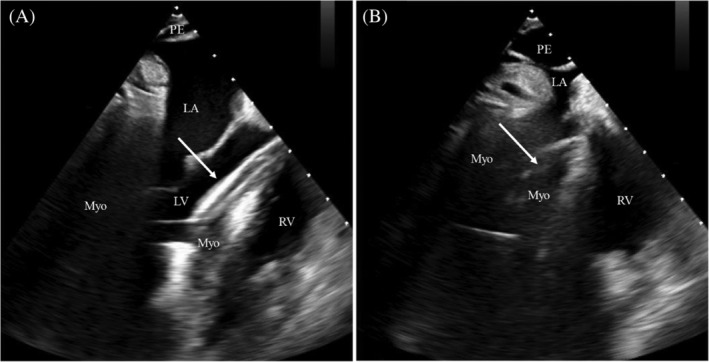
(A) Transesophageal echocardiography (long axis view) showing coaxial pump (Impella, Abiomed, Germany) (arrow) running from ascending aorta across aortic valve into the LV with minimal flow rate (0.6 L/min) and a concomitant VA‐ECMO blood flow of 3,8 L/min. (B) Same patient with transesophageal echocardiography (long axis view) demonstrating complete collapse of LV and LA as consequence of increased but still low flow rate (1.6 L/min) of the coaxial pump. LA, left atrium; LV, left ventricle; RV, right ventricle; Myo, myokardium; PE, pericardial effusion
Severe CS is the major driver of mortality on cardiologic ICUs. 4 , 5 Novel therapeutic options like ECMO and percutaneous microaxial pumps like Impella CP, 5.0 or the combination of both (ECMELLA), are promising options. Whether these approaches reduce mortality has to be evaluated in urgently needed randomized trials but results will not be available in the next few years. 3
CONFLICT OF INTEREST
Martin Orban has received speaker honoraria from Abbott Medical, AstraZeneca, Abiomed, Bayer vital, BIOTRONIK, Bristol‐Myers Squibb, CytoSorbents, Daiichi Sankyo Deutschland, Edwards Lifesciences Services, Sedana Medical, outside the submitted work without involvement. The other authors declare no conflicts of interest.
AUTHOR CONTRIBUTION
Conceptualization: Enzo Lüsebrink, Steffen Massberg, Martin Orban
Data curation: Enzo Lüsebrink, Martin Orban
Formal Analysis: Enzo Lüsebrink, Martin Orban
Funding acquisition: Enzo Lüsebrink, Martin Orban
Investigation: Enzo Lüsebrink, Martin Orban
Methodology: Enzo Lüsebrink, Martin Orban
Project administration: Enzo Lüsebrink, Martin Orban
Resources: Enzo Lüsebrink, Steffen Massberg, Martin Orban
Software: Enzo Lüsebrink, Martin Orban
Supervision: Enzo Lüsebrink, Martin Orban
Validation: Enzo Lüsebrink, Steffen Massberg, Martin Orban
Visualization: Enzo Lüsebrink, Martin Orban
Writing – Original Draft Preparation: Enzo Lüsebrink, Martin Orban
Writing – Review & Editing: Enzo Lüsebrink, Steffen Massberg, Martin Orban
All authors have read and approved the final version of the manuscript.
All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and the accuracy of the data analysis.
TRANSPARENCY STATEMENT
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
ETHICAL STANDARDS
All ethical standards were met in writing and submitting this article.
Lüsebrink E, Massberg S, Orban M. Combined extracorporeal membrane oxygenation and microaxial pump—when left ventricular preload is too low to unload in cardiogenic shock. Health Sci Rep. 2021;4:e321. 10.1002/hsr2.321
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article.
REFERENCES
- 1. Schäfer A, Werner N, Westenfeld R, et al. Clinical scenarios for use of transvalvular microaxial pumps in acute heart failure and cardiogenic shock ‐ a European experienced users working group opinion. Int J Cardiol. 2019;291:96‐104. 10.1016/j.ijcard.2019.05.044. [DOI] [PubMed] [Google Scholar]
- 2. Thiele H, Ohman EM, de Waha‐Thiele S, Zeymer U, Desch S. management of cardiogenic shock complicating myocardial infarction: an update 2019. Eur Heart J. 2019;40(32):2671‐2683. 10.1093/eurheartj/ehz363. [DOI] [PubMed] [Google Scholar]
- 3. Lüsebrink E, Orban M, Kupka D, et al. Prevention and treatment of pulmonary congestion in patients undergoing venoarterial extracorporeal membrane oxygenation for cardiogenic shock. Eur Heart J. 2020;41:3753‐3761. 10.1093/eurheartj/ehaa547. [DOI] [PubMed] [Google Scholar]
- 4. Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012;367:1287‐1296. 10.1056/NEJMoa1208410. [DOI] [PubMed] [Google Scholar]
- 5. Schrage B, Becher PM, Bernhardt A, et al. Left ventricular unloading is associated with lower mortality in patients with cardiogenic shock treated with Venoarterial extracorporeal membrane oxygenation: results from an international, multicenter cohort study. Circulation. 2020;142:2095‐2106. 10.1161/CIRCULATIONAHA.120.048792. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.


