Abstract
Background
Studies indicate that onion supplementation may be effective in the treatment of dyslipidemia; however, the results remain controversial. This meta‐analysis was conducted to evaluate potential benefits of onion on lipid profile.
Methods
Up to 12 October 2020, PubMed, Cochrane Library, Web of Science, and Scopus were searched for randomized controlled trials evaluating the effects of onion on lipid profile. Mean differences (MD) and 95% confidence intervals (CI) were calculated. Meta‐analysis was conducted using the fixed‐effects model.
Results
Ten trials with 446 participants in total were included in the meta‐analysis. The pooled findings of 10 studies suggested that onion supplementation significantly improved high‐density lipoprotein cholesterol (HDL) (MD: 2.29 mg/dl; 95% CI: 0.87, 3.72; I 2 = 0%) and low‐density lipoprotein cholesterol (LDL) (MD: −6.64 mg/dl; 95% CI: −10.91, −2.36; I 2 = 32%),while onion supplementation did not significantly lower triglycerides (TG) (MD: −6.55 mg/dl; 95% CI: −15.64, 2.53; I 2 = 45%). Analysis of nine trials showed a significant reduction in total cholesterol (TC) (MD: −5.39 mg/dl; 95% CI: −10.68, −0.09; I 2 = 49%) in patients with onion supplementation compared to the control group.
Conclusion
In summary, supplementation of onion was beneficial to control dyslipidemia, including improving levels of HDL, LDL, and TC, but could not reduce TG level. The therapeutic benefits of onion for dyslipidemia need to be treated with caution considering that some of the results are not robust.
Keywords: cholesterol, lipid profiles, meta‐analysis, onion, triglycerides
Cardiovascular diseases are, currently, the leading cause of death globally, accounting for about one third of all deaths. Controlling blood lipids can effectively reduce the risk of cardiovascular diseases. Onion supplementation was beneficial for blood lipids, including improving plasma levels of HDL, LDL, and TC.

1. INTRODUCTION
Cardiovascular diseases are currently the leading cause of death globally, accounting for about one‐third of all deaths (Hadjiphilippou & Ray, 2019; Yusuf et al., 2020). Dyslipidemia is a major risk factor for the development and progression of cardiovascular diseases (Kopin & Lowenstein, 2017; Pan et al., 2016). Dyslipidemia is an incurable but controllable condition characterized by elevated plasma triglycerides (TG), total cholesterol (TC), or low‐density lipoprotein cholesterol (LDL) concentrations and decreased plasma high‐density lipoprotein cholesterol (HDL) concentrations (Hedayatnia et al., 2020; Heshmat‐Ghahdarijani et al., 2020). Previous studies have shown that controlling blood lipids can effectively reduce the risk of cardiovascular diseases (Ida et al., 2019). Therefore, the treatment of dyslipidemia is one of the keys to prevent cardiovascular diseases (Yandrapalli et al., 2019). Statins, the main lipid‐lowering agents, are effective in improving blood lipids, but they are associated with many side effects that affect patient compliance (Karr, 2017). Furthermore, the reduction of drug efficacy is also a problem that cannot be ignored when statins are used for a long‐term (Shekarchizadeh‐Esfahani et al., 2020). Therefore, it is urgent to find a safe and effective supplementary treatment.
Alternatives based on natural products are of great interest because of their safety and potential effectiveness (Georgia‐Eirini et al., 2019; Yarla et al., 2016). Onion (Allium Cepa L.) is a perennial plant, belonging to Family Amaryllidaceae, one of the most widely consumed vegetables in the world (Khajah et al., 2019; Li et al., 2020). Onions are rich in sulfur compounds and Flavonoids (Chiu et al., 2016), and have traditionally been used to treat asthma, coughs, high blood pressure, ulcer wounds, and other ailments (Khajah et al., 2019). In recent years, onion has been found to have many kinds of biological activities, including anti‐inflammatory, anti‐oxidant, anticancer, anti‐diabetes, Immunoprotective, wound healing, anti‐scar and, anti‐obesity, and widely used in medicine (Khajah et al., 2019; Teshika et al., 2019). Recently, several studies have examined the effects of onion on blood lipids, but the results are contradictory. Lee et al. (2011) found that supplementation with 228 mg onion skin extract for 10 weeks significantly improved TC, LDL, and HDL levels in healthy subjects, but in Kim et al.'s study (2015), there was no significant difference in lipid profile after 12 weeks of administration of onion peel extract of 100 mg/day compared with placebo.
Therefore, it is necessary to summarize the evidence of the effects of onion on blood lipids. Unfortunately, there has been no systematic review or meta‐analysis in this area. The purpose of this study was to comprehensively review randomized controlled trials to evaluate the effects of onion on lipid profile.
2. METHODS AND MATERIALS
2.1. Search strategy
Two authors (Tang and Tao) independently searched the literature through PubMed, Cochrane Library, Web of Science, and Scopus from inception to 12 October 2020. Search strategy (Table 1): (Allium Cepa OR onion) AND (lipid OR lipids OR hyperlipidemic OR hyperlipidemia OR dyslipidemic OR dyslipidemia OR cholesterol OR hypercholesterolemic OR hypercholesterolemia OR triglycerides OR Triacylglycerol OR hypotriglyceridemic OR hypertriglyceridemia OR lipoprotein OR lipoproteins OR TG OR TC OR LDL OR HDL). Furthermore, references of the included studies were searched to reduce possible omissions.
TABLE 1.
Electronic search strategy
| Database | Search term (establish to 12 October 2020) | Number |
|---|---|---|
|
PubMed (All fields) |
#1: Allium Cepa OR onion | #1: 7,887 |
| #2: lipid OR lipids OR hyperlipidemic OR hyperlipidemia OR dyslipidemic OR dyslipidemia OR cholesterol OR hypercholesterolemic OR hypercholesterolemia OR triglycerides OR Triacylglycerol OR hypotriglyceridemic OR hypertriglyceridemia OR lipoprotein OR lipoproteins OR TG OR TC OR LDL OR HDL | #2: 1,685,442 | |
| #3: #1 AND #2 | #3: 783 | |
| Scopus (TITLE‐ABS‐KEY) | #1: Allium Cepa OR onion | #1: 23,917 |
| #2: lipid OR lipids OR hyperlipidemic OR hyperlipidemia OR dyslipidemic OR dyslipidemia OR cholesterol OR hypercholesterolemic OR hypercholesterolemia OR triglycerides OR Triacylglycerol OR hypotriglyceridemic OR hypertriglyceridemia OR lipoprotein OR lipoproteins OR TG OR TC OR LDL OR HDL | #2: 1,668,539 | |
| #3: #1 AND #2 | #3: 1,010 | |
|
Cochrane Library Trials (Title Abstract keyword) |
#1: Allium Cepa OR onion | #1: 240 |
| #2: lipid OR lipids OR hyperlipidemic OR hyperlipidemia OR dyslipidemic OR dyslipidemia OR cholesterol OR hypercholesterolemic OR hypercholesterolemia OR triglycerides OR Triacylglycerol OR hypotriglyceridemic OR hypertriglyceridemia OR lipoprotein OR lipoproteins OR TG OR TC OR LDL OR HDL | #2: 78,607 | |
| #3: #1 AND #2 | #3: 41 | |
|
Web of Science (Topic) |
#1: Allium Cepa OR onion | #1: 21,518 |
| #2: lipid OR lipids OR hyperlipidemic OR hyperlipidemia OR dyslipidemic OR dyslipidemia OR cholesterol OR hypercholesterolemic OR hypercholesterolemia OR triglycerides OR Triacylglycerol OR hypotriglyceridemic OR hypertriglyceridemia OR lipoprotein OR lipoproteins OR TG OR TC OR LDL OR HDL | #2: 1,971,491 | |
| #3: #1 AND #2 | #3: 1,529 |
2.2. Study selection
Trials meeting the following criteria were included: (a) Participants with dyslipidemia or without dyslipidemia; (b) Intervention were onion or products of onion; (c) The control group was placebo; (d) Outcomes assessed at least one of LDL, HDL, TG, or TC; (e) The study was designed as a randomized controlled trial. Exclusion criteria are as follows: (a) non‐human studies; (b) reviews, conference abstracts, case reports, letters to the editor, or technical reports; (c) reported on observational studies; (d) duplicate studies; (e) onion in combination with other drugs.
2.3. Data extraction
Characteristics of the included study were extracted, including first author, publication year, location, age, sample size, baseline body mass index (BMI), state of health, type of study, intervention, duration, outcomes. In addition, the mean changes of TG, TC, HDL, and LDL from baseline to the end of the study and their standard deviations (SDs) were also extracted. When data in the literature was not available, we contacted the corresponding author and attempt to obtain the data.
2.4. Quality assessment
The whole process of literature search, screening, data extraction, and quality assessment was conducted by two authors (Tang and Tao) independently, and all inconsistencies were discussed with the third author (Zhang) and resolved. Cochrane Collaboration's tool was used to conduct quality assessments, including the following seven domains: (a) random sequence generation; (b) allocation concealment; (c) blinding of participants and personnel; (d) blinding of outcome assessment; (e) incomplete outcome data; (f) selective reporting; (g) other sources of bias. Each domain was classified as high bias risk, low bias risk, and unclear bias risk. Based on the domains mentioned, the overall quality of each study was assessed as good (more than two domains were assessed as low risk), fair (two domains were assessed as low risk), or weak (less than two domains were assessed as low risk).
2.5. Statistical analysis
All concentration units were converted to mg/dl before the total effect is calculated. Effect size was defined as mean difference (MD) and 95% confidence interval (CI) (Higgins & Green, 2011. Available from www.cochrane‐handbook.org). When no net change in the outcomes (TG, TC, LDL, and HDL) was provided, the difference between baseline and end is calculated as the effect size. The following formula was used to calculate standard deviations (SDs) of the mean changes: SD = square root [(SDpretreatment)2 + (SDposttreatment)2 ‐ 2r × SDpretreatment × SDposttreatment], correlation coefficient (r) = .5. When standard error (SE) was reported, the following formula is used to calculate SD: SD = SE × √n (n = number of subjects). I 2 statistics were used to assess the size of heterogeneity. When I 2 > 50 was significant heterogeneity, and the random‐effect model was selected, whereas the fixed‐effect model was selected (Higgins et al., 2003). We separately excluded each study to explore the robustness of our results. Begg's rank correlation and Egger's weighted regression were used to examine potential publication bias. Subgroup analysis was performed based on the type of participants (dyslipidemia or without dyslipidemia) and period of treatment (>10 weeks or ≤10 weeks). All statistical analyses were performed using Review Manager 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration 2014; Copenhagen, Denmark) and Stata 12.0 (Stata Corp.). Moreover, statistically significant is defined as p < .05.
3. RESULTS
3.1. Identification and selection of studies
Of the 3,365 related literatures, 1,242 duplicates were excluded. Next, 2,096 literatures that did not meet the inclusion criteria were excluded by reviewing the title and abstract. Then, we evaluated the remaining 27 articles, and finally, 10 articles were included (Figure 1).
FIGURE. 1.
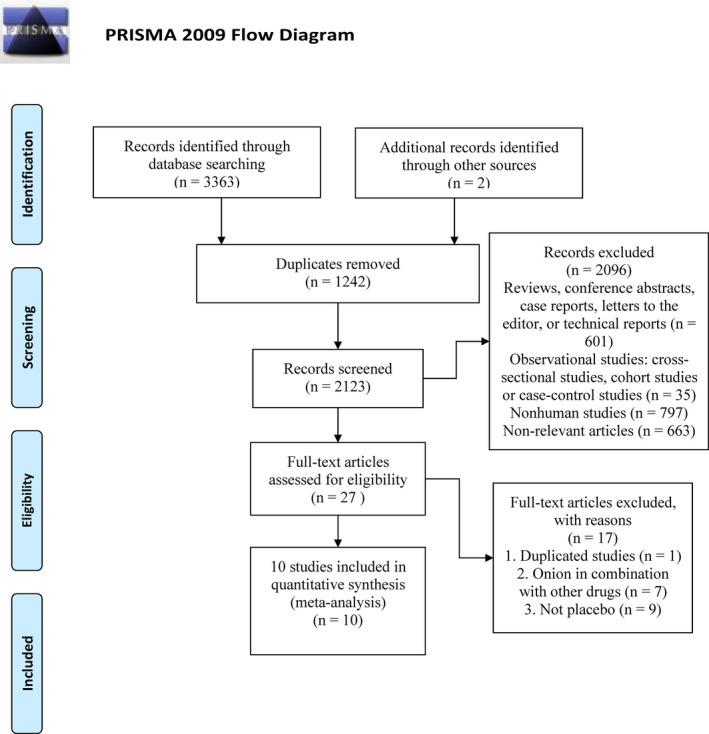
PRISMA flow diagram of the literature retrieval process
3.2. Study characteristics
A total of 446 participants in the 10 included studies were randomly assigned to either the placebo group or the onion group. The number of participants in each study ranged from 12 to 92. Two studies (Kim et al., 2013; Lee et al., 2011) involved healthy adult, three studies involved hyperlipidemia subjects (Kyung Huil et al., 2007; Lee et al., 2010; Lu et al., 2015), and five studies involved Overweight and/or obesity subjects (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim & Yim, 2015; Park et al., 2016). All the studies were published between 2007 and 2019. Eight trails (Choi et al., 2015; Jeong et al., 2019; Kim et al., 2013; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Park et al., 2016) were conducted in Korea, one (Lu et al., 2015) in China and one (Bruell et al., 2016) in Germany. The duration of intervention in the included studies ranged from 2 to 12 weeks. Seven trials (Choi et al., 2015; Jeong et al., 2019; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) were designed in parallel and three (Bruell et al., 2016; Kim et al., 2013; Lee et al., 2010) in a cross‐over design. Characteristics of the included study are summarized in Table 2.
TABLE 2.
Characteristics of all eligible studies
| First author, publication year | Location | Age | Sample size | BMI | Subjects | Type of study | Intervention | Duration | outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Kyung Hui (2007) | Korea | 47.1 | 43 | 25.6 | Patients with hypercholesterolemia | Randomized placebo‐controlled parallel trial | 200 ml/day onion extract | 8 weeks | TG, TC, HDL, LDL |
| Lee (2010) | Korea | 45.9 | 27 | 24.6 | borderline hypercholesterolemic subjects | Randomized single blind placebo‐controlled crossover trial | 150 ml/day onion extract | 10 weeks | TG, TC, HDL, LDL |
| Lee (2011) | Korea | 44.4 | 92 | 24.9 | Healthy male smokers | Randomized, Double blinded placebo‐controlled parallel trial | 1,000 mg/day OPE | 10 weeks | TG, TC, HDL, LDL |
| Kim (2013) | Korea | N | 12 | 20.2 | healthy young women | Randomized double‐blind placebo‐controlled crossover trial | 1,000 mg/day OPE | 2 weeks | TG, HDL, LDL |
| Kim (2015) | Korea | 45 | 37 | 26.3 | Obese women | Randomized double‐blind placebo controlled parallel trial | 100 mg/day OPE | 12 weeks | TG, TC, HDL, LDL |
| Choi (2015) | Korea | 43.1 | 62 | 26.2 | Overweight and obese subjects | Randomized double‐blind placebo‐controlled parallel trial | 1,000 mg/day OPE | 12 weeks | TG, TC, HDL, LDL |
| Lu (2015) | China | N | 23 | 25.2 | Mild hypercholesterolemic adults | Randomized placebo‐controlled parallel trial | 100 ml/day onion juice | 8 weeks | TG, TC, HDL, LDL |
| Brüll (2016) | Germany | 48.1 | 22 | 30.9 | Overweight‐to‐obese adults with hypertension | Randomized double‐blinded placebo‐controlled crossover trial | 396 mg/day OPE | 6 weeks | TG, TC, HDL, LDL |
| Park (2016) | Korea | 43.3 | 72 | 26.6 | Overweight and obese subjects | Randomized double‐blind, placebo‐controlled parallel trial | 340 mg/day OPE | 12 weeks | TG, TC, HDL, LDL |
| Jeong (2019) | Korea | 42.0 | 56 | 27.2 | Overweight Subjects | Randomized double‐blind placebo‐controlled parallel trial | 900 mg/day steamed onion | 12 weeks | TG, TC, HDL, LDL |
Abbreviations: HDL, high‐density lipoprotein cholesterol; LDL, low‐density lipoprotein cholesterol; N, not available; OPE, onion peel extract; TG, Triglyceride; TC, total cholesterol.
3.3. Quality assessment
All of the included studies mentioned randomization, but only five (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim & Yim, 2015; Kyung Huil et al., 2007) provided specific methods for randomization. Two studies (Bruell et al., 2016; Jeong et al., 2019) adequately concealed the randomization scheme. A double‐blind design was used in seven studies (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim et al., 2013; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016), blinding of outcome assessment in nine studies (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) were considered as low risk of bias. Incomplete outcome data in nine studies (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim et al., 2013; Kim & Yim, 2015; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) were judged as low risk of bias. Selective reporting and other biases were assessed as low risk of bias in all studies. The risk of bias is shown in Figure 2.
FIGURE. 2.
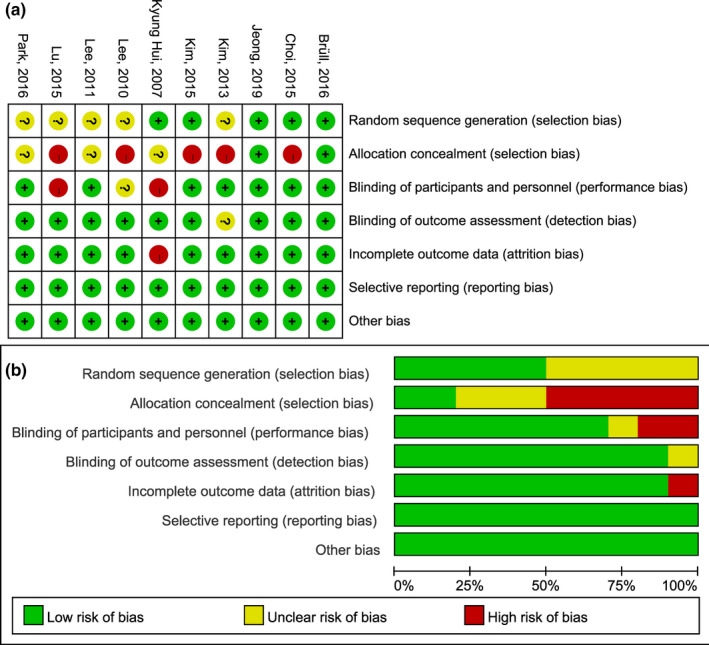
Risk of bias for each included study. (a) risk of bias summary; (b) risk of bias graph
3.4. Meta‐analysis
Ten studies (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim et al., 2013; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) reported the effect of onion supplementation on lipid profiles. Pooled evaluation of the included trials (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim et al., 2013; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) indicated that onion supplementation significantly improved HDL (MD: 2.29 mg/dl; 95% CI: 0.87, 3.72; I 2 = 0%; Figure 3), LDL (MD: −6.64 mg/dl; 95% CI: −10.91, −2.36; I 2 = 32%; Figure 4), but no significant lowering in TG (MD: −6.55 mg/dl; 95% CI: −15.64, 2.53; I 2 = 45%; Figure 5). Moreover, and meta‐analysis of nine studies (Bruell et al., 2016; Choi et al., 2015; Jeong et al., 2019; Kim & Yim, 2015; Kyung Huil et al., 2007; Lee et al., 2010; Lee et al., 2011; Lu et al., 2015; Park et al., 2016) showed a significant effect on lowering TC (MD: −5.39 mg/dl; 95% CI: −10.68, −0.09; I 2 = 49%; Figure 6), as compared to the placebo group.
FIGURE. 3.
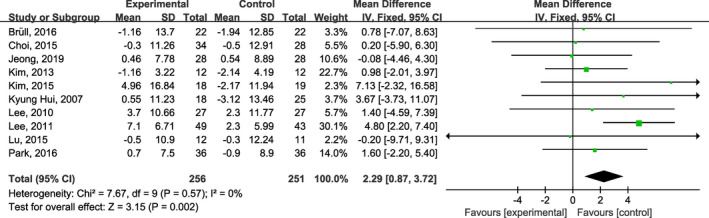
Forest plots of the effect of onion on plasma high‐density lipoprotein cholesterol concentrations
FIGURE. 4.
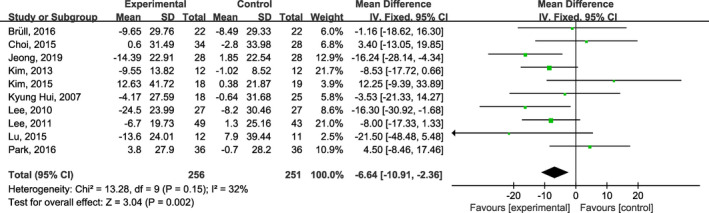
Forest plots of the effect of onion on plasma low‐density lipoprotein cholesterol concentrations
FIGURE. 5.
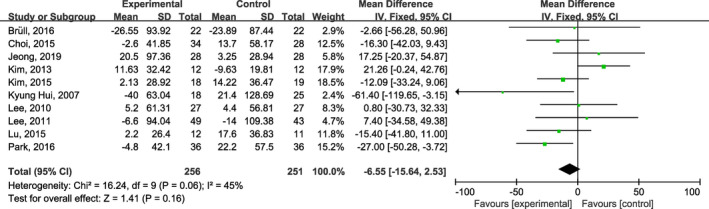
Forest plots of the effect of onion on plasma triglycerides concentrations
FIGURE. 6.
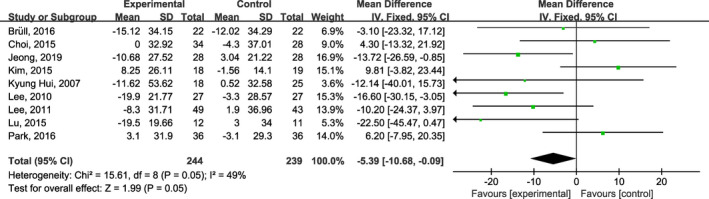
Forest plots of the effect of onion on plasma total cholesterol concentrations
3.5. Subgroup analysis
Notably, the subgroup analysis showed that in the subgroup of subjects with dyslipidemia, onion intake appeared to show a greater benefit in lowering TC (MD: −17.23 mg/dl; 95% CI: −27.99, −6.47; I 2 = 8%) and LDL (MD: −12.70 mg/dl; 95% CI: −23.12, −2.27; I 2 = 0%). However, onion supplementation did not improve TG in either subjects with (MD: −14.4 mg/dl; 95% CI: −33.52, 4.72; I 2 = 41%) or without dyslipidemia (MD: −4.27 mg/dl; 95% CI: −14.59, 6.06; I 2 = 50%). In addition, we observed more increases in HDL concentrations (MD: 2.81 mg/dl; 95% CI: 1.08, 5.54; I 2 = 17%) in the subgroup with onion intake longer than 10 weeks. The results of subgroup analysis are summarized in Table 3.
TABLE 3.
Summary of results from all subgroup analyses
| ‐ | Subgrouped by | The number of studies | Effect size | 95% CI | I 2 (%) | p for between subgroup heterogeneity |
|---|---|---|---|---|---|---|
| HDL | Type of participants | – | – | – | – | .81 |
| dyslipidemia | 3 | 1.82 | −2.37, 6.00 | 0 | – | |
| without dyslipidemia | 7 | 2.35 | 0.84, 3.87 | 16 | – | |
| period of treatment | – | – | – | – | .30 | |
| >10 weeks | 6 | 2.81 | 1.08, 4.54 | 17 | – | |
| ≤10 weeks | 4 | 1.19 | −1.33, 3.71 | 0 | – | |
| LDL | Type of participants | – | – | – | – | .21 |
| dyslipidemia | 3 | −12.70 | −23.12, −2.27 | 0 | – | |
| without dyslipidemia | 7 | −5.41 | −10.10, −0.72 | 40 | – | |
| period of treatment | – | – | – | – | .79 | |
| >10 weeks | 6 | −6.20 | −11.55, −0.86 | 56 | – | |
| ≤10 weeks | 4 | −7.40 | −14.54, −0.27 | 0 | – | |
| TG | Type of participants | – | – | – | – | .36 |
| dyslipidemia | 3 | −14.40 | −33.52, 4.72 | 41 | – | |
| without dyslipidemia | 7 | −4.27 | −14.59, 6.06 | 50 | – | |
| period of treatment | – | – | – | – | .22 | |
| >10 weeks | 6 | −10.71 | −21.98, 0.56 | 8 | – | |
| ≤10 weeks | 4 | −1.15 | −14.20, 16.51 | 68 | – | |
| TC | Type of participants | – | – | – | – | .01 |
| dyslipidemia | 3 | −17.23 | −27.99, −6.47 | 8 | ||
| without dyslipidemia | 6 | −1.61 | −7.69, 4.47 | 45 | – | |
| period of treatment | – | – | – | – | .31 | |
| >10 weeks | 6 | −4.20 | −9.97, 1.56 | 62 | – | |
| ≤10 weeks | 3 | −11.70 | −25.03, 1.63 | 0 | – |
Abbreviations: HDL, high‐density lipoprotein cholesterol; LDL, low‐density lipoprotein cholesterol; TC, total cholesterol; TG, Triglyceride.
3.6. Sensitivity analysis
Found of sensitivity analysis suggested that the pooled effect size of LDL was not affected by any of the studies. However, the effect of onion on level of TC was sensitive to the trials by Lu et al. (2015) (MD: −4.43; 95% CI: −9.87, 1.01), Lee et al. (2011) (MD: −4.61; 95% CI: −10.31, 1.10), Lee et al. (2010) (MD: −3.37; 95% CI: −9.12, 2.38), Kyung Hui et al. (2007) (MD: −5.13; 95% CI: −10.52, 0.26) and Jeong et al. (2019) (MD: −3.69; 95% CI: −9.50, 2.12), and Kim et al.’s study (2013) markedly affected the total effect size of TG (MD: −12.60; 95% CI: −22.63, −2.58). Sensitivity analysis indicated that the overall effect size of HDL was changed by excluding Lee et al.'s (2011) study (MD: 1.21; 95% CI: −0.49, 2.92).
3.7. Publication bias
There was no evidence of publication bias for TG (Begg's = 1.000, Egger's = 0.749), TC (Begg's = 0.917, Egger's = 0.703), LDL (Begg's = 0.592, Egger's = 0.481), and HDL (Begg's = 0.271, Egger's = 0.509).
4. DISCUSSION
To our knowledge, this is the first meta‐analysis to assess the impact of onion on blood lipids. Our results showed that onion could not reduce plasma TG levels, but onion administration did improve plasma HDL, TC, and LDL levels. In particular, for subjects with dyslipidemia, onion intake appeared to show a greater benefit in reducing TC and LDL. Our findings have important clinical implications because the benefits of onion on blood lipids can effectively reduce the risk of cardiovascular disease (Mattiuzzi et al., 2020; Rader & Hovingh, 2014).
Onions are rich in flavonoids and dietary fiber, which epidemiology has shown can reduce the risk of cardiovascular disease (Hamauzu et al., 2011). However, the clinical evidence for the efficacy of onion on blood lipids is not uniform. Some studies have shown that onion consumption is effective in improving blood lipid levels in both patients with hyperlipidemia and healthy subjects (Louria et al., 1985; Vidyashankar et al., 2010). Chiu et al. (Chiu et al., 2016) found that red wine onion extract showed additional lipid‐lowering effects compared with red wine after supplementing red wine onion extract at 250 ml/day for 10 weeks for hyperlipidemia patients. Lee et al. showed that with the intake of frozen onion powder, the subjects' plasma HDL level increased, levels of plasma TC, plasma LDL, and atherosclerosis index significantly decreased (Lee et al., 2008), which was similar to our results. In addition to the changes in experimental indicators, a questionnaire for participants showed that most patients with hyperlipidemia thought onion intake was good for their health (Lee et al., 2008). However, Arora's study (Arora & Arora, 1981) did not observe the benefit of onion supplementation on dyslipidemia. Similarly, Ebrahimi‐Mamaghani et al. found that eating raw red onion did not improve HDL and TG levels in patients with polycystic ovary syndrome (Ebrahimi‐Mamaghani et al., 2014). Different characteristics of the subjects (healthy subjects, hyperlipidemia subjects), different onion products (onion skin extract, raw onion, onion juice), and Inconsistency in the duration of onion supplementation may lead to inconsistent results. As the results of the subgroup analysis showed, onion appeared to be more beneficial for subjects with dyslipidemia, and onion supplementation for longer than 10 weeks may be more beneficial for improving HDL. Since eight studies used onion extract, one used red onion, and one used onion juice, subgroup analysis based on different onion products was not feasible.
Although a large number of studies have investigated the effects of onion on blood lipids, the mechanism of onion improving blood lipids is still unclear and may be related to the following aspects. On the one hand, onion can activate lecithin‐cholesterol Acyltransferase by enhancing the action of insulin, so as to promote the conversion of LDL into HDL (Ige & Akhigbe, 2013). On the other hand, onion can promote the excretion of bile acids and inhibit the absorption of cholesterol to reduce plasma cholesterol (Guan et al., 2010). In addition, the anti‐lipid effect of onion may be related to reducing lipid hydroperoxide and lipoperoxide concentrations (Campos et al., 2003; Guan et al., 2010).
Natural products are increasingly popular because they are believed to have few side effects (Teshika et al., 2019). Onions as a common food have been the subject of numerous clinical trials, only few side‐effects have been reported. Nishimura et al. (Nishimura et al., 2019) reported four participants with mild gastrointestinal symptoms. In Song et al.'s study, two patients experienced transient itching after using the onion extract gel (Song et al., 2018). These suggest that onion administration is a safe and feasible alternative therapy.
Our study had several advantages. On the one hand, we strictly limited the inclusion criteria and only randomized placebo‐controlled trials were included. On the other hand, we conducted a comprehensive evidence search without language or time restrictions, reducing bias. Like all studies, our meta‐analysis has some limitations. First, most of the included studies were small sample studies, which may affect the reliability of the treatment effect. Second, most of the included studies were conducted in Korea, which makes it difficult to apply the results to other regions. Finally, the longest duration of onion supplementation was only 12 weeks, which may affect the true effect of onion on blood lipids.
5. CONCLUSIONS
In summary, onion supplementation was beneficial to control dyslipidemia, including improving plasma levels of HDL, LDL, and TC, but did not reduce plasma TG level. The therapeutic benefits of onion for dyslipidemia need to be treated with caution considering that some of the results are not robust. It is necessary to investigate the effect of long‐term onion supplementation on dyslipidemia through large‐sample, high‐quality studies. In addition, onion may be more effective in subjects with dyslipidemia, and future studies should focus on patients with hyperlipidemia to better assess the effect of onion on blood lipid.
CONFLICTS OF INTEREST
The authors declare that they do not have any conflict of interest.
AUTHOR CONTRIBUTIONS
Wang Huang: Conceptualization (equal); Investigation (equal); Methodology (equal); Software (equal); Writing‐original draft (equal); Writing‐review & editing (equal). gang tang: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Methodology (equal); Software (equal); Writing‐original draft (equal); Writing‐review & editing (equal). linyu zhang: Formal analysis (equal); Methodology (equal); Software (equal); Writing‐original draft (equal); Writing‐review & editing (equal). jie tao: Data curation (equal); Formal analysis (equal); Methodology (equal); Software (equal); Writing‐original draft (equal); Writing‐review & editing (equal). zhengqiang wei: Conceptualization (equal); Formal analysis (equal); Methodology (equal); Software (equal); Writing‐review & editing (lead).
ETHICAL APPROVAL
This study does not involve any human or animal testing.
ACKNOWLEDGMENTS
None declared.
Huang W, Tang G, Zhang L, Tao J, Wei Z. Effect of onion on blood lipid profile: A meta‐analysis of randomized controlled trials. Food Sci Nutr. 2021;9:3563–3572. 10.1002/fsn3.2309
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- Arora, R. C. , & Arora, S. (1981). Comparative effect of clofibrate, garlic and onion on alimentary hyperlipemia. Atherosclerosis, 39(4), 447–452. 10.1016/0021-9150(81)90002-2 [DOI] [PubMed] [Google Scholar]
- Brüll, V. , Burak, C. , Stoffel‐Wagner, B. , Wolffram, S. , Nickenig, G. , Müller, C. , Langguth, P. , Alteheld, B. , Fimmers, R. , Stehle, P. , & Egert, S. (2016). Acute intake of quercetin from onion skin extract does not influence postprandial blood pressure and endothelial function in overweight‐to‐obese adults with hypertension: A randomized, double‐blind, placebo‐controlled, crossover trial. European Journal of Nutrition, 56(3), 1347–1357. 10.1007/s00394-016-1185-1. [DOI] [PubMed] [Google Scholar]
- Campos, K. E. , Diniz, Y. S. , Cataneo, A. C. , Faine, L. A. , Alves, M. J. , & Novelli, E. L. (2003). Hypoglycaemic and antioxidant effects of onion, Allium cepa: Dietary onion addition, antioxidant activity and hypoglycaemic effects on diabetic rats. International Journal of Food Sciences and Nutrition, 54(3), 241–246. 10.1080/09637480120092062 [DOI] [PubMed] [Google Scholar]
- Chiu, H. F. , Shen, Y. C. , Huang, T. Y. , Venkatakrishnan, K. , & Wang, C. K. (2016). Cardioprotective efficacy of red wine extract of onion in healthy hypercholesterolemic subjects. Phytotherapy Research, 30(3), 380–385. 10.1002/ptr.5537 [DOI] [PubMed] [Google Scholar]
- Choi, E.‐Y. , Lee, H. , Woo, J. S. , Jang, H. H. , Hwang, S. J. , Kim, H. S. , Kim, W.‐S. , Kim, Y.‐S. , Choue, R. , Cha, Y.‐J. , Yim, J.‐E. , & Kim, W. (2015). Effect of onion peel extract on endothelial function and endothelial progenitor cells in overweight and obese individuals. Nutrition, 31(9), 1131–1135. 10.1016/j.nut.2015.04.020 [DOI] [PubMed] [Google Scholar]
- Ebrahimi‐Mamaghani, M. , Saghafi‐Asl, M. , Pirouzpanah, S. , & Asghari‐Jafarabadi, M. (2014). Effects of raw red onion consumption on metabolic features in overweight or obese women with polycystic ovary syndrome: A randomized controlled clinical trial. Journal of Obstetrics and Gynaecology Research, 40(4), 1067–1076. 10.1111/jog.12311 [DOI] [PubMed] [Google Scholar]
- Georgia‐Eirini, D. , Athina, S. , Wim, V. B. , Christos, K. , & Theodoros, C. (2019). Natural products from mediterranean diet: From anti‐hyperlipidemic agents to dietary epigenetic modulators. Current Pharmaceutical Biotechnology, 20(10), 825–844. 10.2174/1573407215666190628150921 [DOI] [PubMed] [Google Scholar]
- Guan, L. , Chung, H. Y. , Su, Y. , Jiao, R. , Peng, C. , & Chen, Z. Y. (2010). Hypocholesterolemic activity of onion is mediated by enhancing excretion of fecal sterols in hamsters. Food & Function, 1(1), 84–89. 10.1039/c0fo00036a [DOI] [PubMed] [Google Scholar]
- Hadjiphilippou, S. , & Ray, K. K. (2019). Cholesterol‐lowering agents. Circulation Research, 124(3), 354–363. 10.1161/circresaha.118.313245 [DOI] [PubMed] [Google Scholar]
- Hamauzu, Y. , Nosaka, T. , Ito, F. , Suzuki, T. , Torisu, S. , Hashida, M. , Fukuzawa, A. , Ohguchi, M. , & Yamanaka, S. (2011). Physicochemical characteristics of rapidly dried onion powder and its anti‐atherogenic effect on rats fed high‐fat diet. Food Chemistry, 129(3), 810–815. 10.1016/j.foodchem.2011.05.027 [DOI] [PubMed] [Google Scholar]
- Hedayatnia, M. , Asadi, Z. , Zare‐Feyzabadi, R. , Yaghooti‐Khorasani, M. , Ghazizadeh, H. , Ghaffarian‐Zirak, R. , Nosrati‐Tirkani, A. , Mohammadi‐Bajgiran, M. , Rohban, M. , Sadabadi, F. , Rahimi, H.‐R. , Ghalandari, M. , Ghaffari, M.‐S. , Yousefi, A. , Pouresmaeili, E. , Besharatlou, M.‐R. , Moohebati, M. , Ferns, G. A. , Esmaily, H. , & Ghayour‐Mobarhan, M. (2020). Dyslipidemia and cardiovascular disease risk among the MASHAD study population. Lipids in Health and Disease, 19(1), 42. 10.1186/s12944-020-01204-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heshmat‐Ghahdarijani, K. , Mashayekhiasl, N. , Amerizadeh, A. , Teimouri Jervekani, Z. , & Sadeghi, M. (2020). Effect of fenugreek consumption on serum lipid profile: A systematic review and meta‐analysis. Phytotherapy Research, 34(9), 2230–2245. 10.1002/ptr.6690 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T. , & Green, S. (Eds). (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Retrieved from www.cochrane‐handbook org [Google Scholar]
- Higgins, J. P. , Thompson, S. G. , Deeks, J. J. , & Altman, D. G. (2003). Measuring inconsistency in meta‐analyses. BMJ, 327(7414), 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ida, S. , Kaneko, R. , & Murata, K. (2019). Efficacy and safety of pemafibrate administration in patients with dyslipidemia: A systematic review and meta‐analysis. Cardiovascular Diabetology, 18(1), 38. 10.1186/s12933-019-0845-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ige, S. F. , & Akhigbe, R. E. (2013). Common onion (Allium cepa) extract reverses cadmium‐induced organ toxicity and dyslipidaemia via redox alteration in rats. Pathophysiology, 20(4), 269–274. 10.1016/j.pathophys.2013.04.002 [DOI] [PubMed] [Google Scholar]
- Jeong, S. , Chae, J. , Lee, G. , Shin, G. , Kwon, Y.‐I. , Oh, J.‐B. , Shin, D. Y.b , & Lee, Jong Ho (2020). Effect of Steamed Onion (ONIRO) consumption on body fat and metabolic profiles in overweight subjects: A 12‐week randomized, double‐blind, placebo‐controlled clinical trial. Journal of the American College of Nutrition, 39(3), 206–215. 10.1080/07315724.2019.1635052 [DOI] [PubMed] [Google Scholar]
- Karr, S. (2017). Epidemiology and management of hyperlipidemia. American Journal of Management Care, 23(9 Suppl), S139–S148. [PubMed] [Google Scholar]
- Khajah, M. A. , Orabi, K. Y. , Hawai, S. , Sary, H. G. , & El‐Hashim, A. Z. (2019). Onion bulb extract reduces colitis severity in mice via modulation of colonic inflammatory pathways and the apoptotic machinery. Journal of Ethnopharmacology, 241, 112008. 10.1016/j.jep.2019.112008 [DOI] [PubMed] [Google Scholar]
- Kim, J. , Cha, Y.‐J. , Lee, K.‐H. , & Park, E. (2013). Effect of onion peel extract supplementation on the lipid profile and antioxidative status of healthy young women: a randomized, placebo‐controlled, double‐blind, crossover trial. Nutrition Research and Practice, 7(5), 373–379. 10.4162/nrp.2013.7.5.373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, K. A. , & Yim, J. E. (2015). Antioxidative activity of onion peel extract in obese women: A randomized, double‐blind, placebo controlled study. Journal of Cancer Prevention, 20(3), 202–207. 10.15430/jcp.2015.20.3.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kopin, L. , & Lowenstein, C. (2017). Dyslipidemia. Annals of Internal Medicine, 167(11), Itc81‐itc96. 10.7326/aitc201712050 [DOI] [PubMed] [Google Scholar]
- Kyung Huil, N. , Hyun Wook, B. , Tae Youn, C. , Soon Gyu, Y. , Se Won, P. , & Hyoieels, J. (2007). Effects of ethanol extract of onion on the lipid profiles in patientswith hypercholesterolemia. [양파의 알코올 추출물이 고콜레스테롤혈증 환자의지질 성상에 미치는 영향]. Journal of Nutrition and Health, 40(3), 242‐248. [Google Scholar]
- Lee, H. J. , Lee, K. H. , Park, E. , & Chung, H. K. (2010). Effect of onion extracts on serum cholesterol in borderline hypercholesterolemic participants. [양파추출물 섭취가 경계역 고콜레스테롤혈증 대상자의 콜레스테롤 저하에 미치는 효과]. Journal of The Korean Society of Food Science and Nutrition, 39(12), 1783‐1789. [Google Scholar]
- Lee, K. H. , Kim, Y. H. , Park, E. J. , & Cho, S. R. (2008). Study on dietary habit and effect of onion powder supplementation on serum lipid levels in early diagnosed hyperlipidemic patients. Journal of the Korean Society of Food Ence & Nutrition, 37(5), 561–570. 10.3746/jkfn.2008.37.5.561 [DOI] [Google Scholar]
- Lee, K.‐H. , Park, E. , Lee, H.‐J. , Kim, M.‐O. , Cha, Y.‐J. , Kim, J.‐M. , Lee, H. , & Shin, M.‐J. (2011). Effects of daily quercetin‐rich supplementation on cardiometabolic risks in male smokers. Nutrition Research and Practice, 5(1), 28–33. 10.4162/nrp.2011.5.1.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Q. , Wang, Y. , Mai, Y. , Li, H. , Wang, Z. , Xu, J. , & He, X. (2020). Health benefits of the flavonoids from onion: Constituents and their pronounced antioxidant and anti‐neuroinflammatory capacities. Journal of Agriculture and Food Chemistry, 68(3), 799–807. 10.1021/acs.jafc.9b07418 [DOI] [PubMed] [Google Scholar]
- Louria, D. B. , McAnally, J. F. , & Lasser, N. (1985). Onion extract in treatment of hypertension and hyperlipidemia: A preliminary communication. Current Therapeutic Research ‐ Clinical and Experimental, 37, 127–131. [Google Scholar]
- Lu, T. M. , Chiu, H. F. , Shen, Y. C. , Chung, C. C. , Venkatakrishnan, K. , & Wang, C. K. (2015). Hypocholesterolemic efficacy of quercetin rich onion juice in healthy mild hypercholesterolemic adults: A pilot study. Plant Foods for Human Nutrition, 70(4), 395–400. 10.1007/s11130-015-0507-4 [DOI] [PubMed] [Google Scholar]
- Mattiuzzi, C. , Sanchis‐Gomar, F. , & Lippi, G. (2020). Worldwide burden of LDL cholesterol: Implications in cardiovascular disease. Nutrition, Metabolism and Cardiovascular Diseases, 30(2), 241–244. 10.1016/j.numecd.2019.09.008 [DOI] [PubMed] [Google Scholar]
- Nishimura, M. , Muro, T. , Kobori, M. , & Nishihira, J. (2019). Effect of daily ingestion of quercetin‐rich onion powder for 12 weeks on visceral fat: A randomised, double‐blind, placebo‐controlled, parallel‐group study. Nutrients, 12(1), 10.3390/nu12010091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, L. , Yang, Z. , Wu, Y. , Yin, R.‐X. , Liao, Y. , Wang, J. , Gao, B. , & Zhang, L. (2016). The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis, 248, 2–9. 10.1016/j.atherosclerosis.2016.02.006 [DOI] [PubMed] [Google Scholar]
- Park, J.‐S. , Cha, Y. J. , Lee, K. H. , & Yim, J. E. (2016). Onion peel extract reduces the percentage of body fat in overweight and obese subjects: A 12‐week, randomized, double‐blind, placebo‐controlled study. Nutrition Research and Practice, 10(2), 175–181. 10.4162/nrp.2016.10.2.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rader, D. J. , & Hovingh, G. K. (2014). HDL and cardiovascular disease. Lancet, 384(9943), 618–625. 10.1016/s0140-6736(14)61217-4 [DOI] [PubMed] [Google Scholar]
- Shekarchizadeh‐Esfahani, P. , Arab, A. , Ghaedi, E. , Hadi, A. , & Jalili, C. (2020). Effects of cardamom supplementation on lipid profile: A systematic review and meta‐analysis of randomized controlled clinical trials. Phytotherapy Research, 34(3), 475–485. 10.1002/ptr.6543 [DOI] [PubMed] [Google Scholar]
- Song, T. , Kim, K. H. , & Lee, K. W. (2018). Randomised comparison of silicone gel and onion extract gel for post‐surgical scars. Journal of Obstetrics and Gynaecology, 38(5), 702–707. 10.1080/01443615.2017.1400524 [DOI] [PubMed] [Google Scholar]
- Teshika, J. D. , Zakariyyah, A. M. , Zaynab, T. , Zengin, G. , Rengasamy, K. R. , Pandian, S. K. , & Fawzi, M. M. (2019). Traditional and modern uses of onion bulb (Allium cepa L.): A systematic review. Critical Reviews in Food Science and Nutrition, 59(sup1), S39–S70. 10.1080/10408398.2018.1499074 [DOI] [PubMed] [Google Scholar]
- Vidyashankar, S. , Sambaiah, K. , & Srinivasan, K. (2010). Regression of preestablished cholesterol gallstones by dietary garlic and onion in experimental mice. Metabolism: Clinical and Experimental, 59(10), 1402–1412. 10.1016/j.metabol.2009.12.032 [DOI] [PubMed] [Google Scholar]
- Yandrapalli, S. , Gupta, S. , Andries, G. , Cooper, H. A. , & Aronow, W. S. (2019). Drug therapy of dyslipidemia in the elderly. Drugs and Aging, 36(4), 321–340. 10.1007/s40266-018-00632-x [DOI] [PubMed] [Google Scholar]
- Yarla, N. S. , Bishayee, A. , Sethi, G. , Reddanna, P. , Kalle, A. M. , Dhananjaya, B. L. , Dowluru, K. S. V. G. K. , Chintala, R. , & Duddukuri, G. R. (2016). Targeting arachidonic acid pathway by natural products for cancer prevention and therapy. Seminars in Cancer Biology, 40–41, 48–81. 10.1016/j.semcancer.2016.02.001 [DOI] [PubMed] [Google Scholar]
- Yusuf, S. , Joseph, P. , Rangarajan, S. , Islam, S. , Mente, A. , Hystad, P. , Brauer, M. , Kutty, V. R. , Gupta, R. , Wielgosz, A. , AlHabib, K. F. , Dans, A. , Lopez‐Jaramillo, P. , Avezum, A. , Lanas, F. , Oguz, A. , Kruger, I. M. , Diaz, R. , Yusoff, K. , … Dagenais, G. (2020). Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high‐income, middle‐income, and low‐income countries (PURE): A prospective cohort study. Lancet, 395(10226), 795–808. 10.1016/s0140-6736(19)32008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


