Abstract
Introduction:
Female veterans smoke cigarettes at high rates compared with both male veterans and nonveteran women. Proactive outreach (PRO) to smokers may reduce gender disparities in cessation care. The objectives of this study were to compare baseline experiences with VA smoking cessation care for men and women and to assess for gender differences in response to a PRO intervention.
Methods:
We conducted a post hoc subgroup analysis of a pragmatic, multisite randomized, controlled trial comparing PRO with usual care (UC). Baseline experiences included physician advice to quit, satisfaction with care, and past-year treatment use. At the 1-year follow-up, treatment use, quit attempts, and 6-month prolonged abstinence for women and men randomized to PRO versus UC were compared using logistic regression.
Results:
Baseline and follow-up surveys were returned by 138 women and 2,516 men. At baseline, women were less likely than men to report being very or somewhat satisfied with the process of obtaining smoking cessation medications in the VA (47% of women vs. 62% of men), but no less likely to report having used cessation medications from the VA in the past year (39% of women vs. 34% of men). After the intervention, phone counseling and combined therapy increased among both women and men in PRO as compared with UC. At the 1-year follow-up, men in PRO were significantly more likely to report prolonged abstinence than those in UC (odds ratio, 1.65; 95% CI, 1.28–2.14); results for women were in the same direction but not statistically significant (odds ratio, 1.39; 95% CI, 0.48–3.99).
Conclusions:
Satisfaction with cessation care in VA remains low. PRO to smokers was associated with an increased use of cessation therapies, and increased odds of achieving prolonged abstinence. A subgroup analysis by gender did not reveal significant differences in the treatment effect.
Female smokers experience unique health consequences of tobacco use, including increased cardiovascular disease risk relative to male smokers (Huxley & Woodward, 2011), as well as pregnancy complications, lower bone density, and elevated cervical cancer risk (U.S. Department of Health and Human Services, 2001). Although women have historically smoked cigarettes less than men, the gap has narrowed in recent years due to a slower rate of decline in smoking prevalence for women than men (Jamal et al., 2016). In 2015, 13.6% of adult U.S. women smoked, compared with 16.7% of adult men (Jamal et al., 2016).
Women veterans are a unique population of women for whom the prevalence of smoking has remained persistently elevated over recent years, despite decreasing for nonveteran women and veteran and nonveteran men (Brown, 2010). A higher proportion of women veterans smoke than nonveteran women (Weinberger, Esan, Hunt, & Hoff, 2016), and among women veterans who use the Veterans Health Administration (VA), current smoking rates exceed those of male veterans (23%- 29% of women smoked vs. 19%−23% men; Duffy et al., 2012; Farmer, Rose, Riopelle, Lanto, & Yano, 2011). These differences are likely due, in part, to the younger mean age of women veterans as compared with male veterans (Barnett, Hamlett-Berry, Sung, & Max, 2015). The youngest cohort of women veterans (born 1985–1989) in a recent national survey reported an alarmingly high smoking rate (44% of women smoked vs. 40% of men) that portends a growing problem (Brown, 2010). In addition to age, significant correlates of smoking that are highly prevalent among women veterans include the presence of mental health problems (Davis, Bush, Kivlahan, Dobie, & Bradley, 2003), including post-traumatic stress disorder (Dobie et al., 2004) and a history of sexual assault (Frayne, Skinner, Sullivan, & Freund, 2003; Surís & Lind, 2008). Although women veterans make up only 7% of current VA users, they are the fastest growing population of patients accessing VA care (Frayne et al., 2014), and smoking-related health care costs for women veterans totaled $132 million in 2010 (Barnett et al., 2015). Consequently, decreasing the prevalence of smoking among women veterans should be a priority for VA policymakers and clinicians.
Both biological (sex) and sociocultural (gender) factors contribute to smoking’s slow decline among women, and women veterans in particular. According to the National Institute of Health’s socioecological model for understanding tobacco-related health disparities, tobacco use is interrelated with life circumstances at social, educational, health, and economic levels (National Cancer Institute, 2017). For example, women who have experienced intimate partner violence have a higher smoking prevalence, and this relationship is influenced by pregnancy, ethnicity, and socioeconomic status. Women smoke fewer cigarettes per day than men on average, yet experience a high degree of nicotine dependence (Smith et al., 2015), which may be partially explained by higher menthol cigarette use (National Cancer Institute, 2017).
Most health care-based smoking cessation interventions, including those used in the VA, do not account for the complex sex and gender differences in smoking. Traditional clinical interventions rely on a reactive model: patients present to clinic and the clinician provides a brief “5As” intervention: ask about smoking, advise the patient to quit, assess readiness to quit, assist with quitting, and arrange follow-up care (Fiore, 2008). An analysis of organizational features in the VA could not identify any VA facility characteristics or variations that influenced sex or gender disparities in receipt of the 5As (Farmer et al., 2011). Recent advances in gender-sensitive primary care provision for women veterans have improved but not eliminated sex and gender differences in experiences of care in the VA. Some women, particularly those with a history of military sexual trauma, still report an unwelcoming environment for women at VA facilities (Kehle-Forbes et al., 2017). A proactive outreach (PRO) approach to smoking cessation may overcome sex and gender barriers to in-person and group care by contacting all smokers by telephone and offering assistance with quitting, either through in-person or telephone counseling and/or with cessation medications.
In 2005, we published an analysis of baseline data from a multisite, randomized, quality improvement project (conducted in 2000) to implement national VA tobacco cessation guidelines, in which we found comparable rates of receipt of advice to quit among female (64%) and male (66%) veteran smokers (Sherman, Fu, Joseph, Lanto, & Yano, 2005). However, we found significantly lower rates of smoking cessation medication prescriptions for women (16%) as compared with men (27%; age-adjusted odds ratio [OR], 0.6; 95% CI, 0.4–0.9). At the 1-year follow-up, only 2.7% of women had successfully quit smoking, as compared with 9.5% of men (age-adjusted OR, 0.3; 95% CI, 0.07–1.20; Sherman et al., 2005).
Since our prior study, the VA has taken steps to comprehensively address smoking cessation among veterans, including sponsoring a conference of national experts in 2004 to identify best practices for smoking cessation policy development in VA. In 2003, 2008, and 2014, the VA revised national policy directives to expand access to smoking cessation medications and counseling, and to designate a lead smoking cessation clinician at each VA facility (Institute of Medicine, 2009). Although these efforts have not been specifically tailored to women veterans, we hypothesize that this population-based approach has improved smoking cessation care for both women and men.
The objective of the current study was to determine whether sex and gender (hereafter, gender) differences in smoking cessation care at VA that we observed in 2000 persisted in 2009 and 2010, and to test whether a PRO intervention affected female and male smokers differently. Specifically, we used baseline data from a multisite, randomized trial of proactive tobacco cessation outreach (conducted in 2009 and 2010) to describe female and male smokers’ experiences with smoking cessation recommendations (physician advice to quit) and treatment (use of cessation medications and counseling, and satisfaction with treatment) in the year before study enrollment. We hypothesized that, unlike in our previous study using data from 2000, smoking cessation recommendations and treatment within the VA would no longer vary by gender. We then assessed for a differential response to PRO by gender. This aim was exploratory, to inform future research.
Methods
Study Design and Participants
Study participants were drawn from a multisite, prospective, randomized, controlled trial studying the effect of a PRO intervention versus usual care (UC) on smoking abstinence rates and use of cessation treatments. A sample of 6,400 current smokers (age 18–80 years) was identified via the VA electronic medical record at four VA medical centers (New York City, Jackson, Tampa, and Minneapolis). Sampling was stratified by site to include 1,600 participants per site, randomized 1:1 into the two study arms (randomized complete block [site] with subsampling study design). A baseline survey was sent to 6,400 potential participants, of whom 5,123 participants were included in the final study population and were also sent a follow-up survey 1 year later. Participants were recruited from October 2009 to September 2010; the study was completed in November 2011. For the current article, we performed a complete case analysis including the 2,654 (138 female and 2,516 male) veterans who returned both baseline and follow-up surveys. This study received ethical approval from the institutional review boards of all participating sites. More details on this study design and methods are available elsewhere (Fu et al., 2012).
Treatment
The PRO intervention combined counselor-initiated contact (mailed materials followed by telephone outreach) with an offer of telephone smoking cessation counseling or referral to in-person counseling. Telephone care included proactive calls from counselors at the Minneapolis VA who were trained in motivational interviewing. Counselors also facilitated access to smoking cessation pharmacotherapy through the participant’s VA primary care provider. The UC group did not receive PRO, but did have access to smoking cessation services through their local VA and state (or insurance-based) telephone quitline.
Measures
Pre-intervention
The first objective of this analysis was to describe female and male veteran smokers’ experiences with smoking cessation recommendations and treatment in the year before enrollment (2009–2010) in this pragmatic trial. We focused on three experience domains related to successful smoking cessation that are susceptible to changes at the health care system level: VA physician advice, use of cessation treatments inside or outside the VA, and satisfaction with VA cessation care.
VA physician advice.
Physician advice to quit is a core component of the 5A’s brief smoking cessation treatment model (i.e., ask, advise, assess, assist, arrange; Abrams et al., 2003), which has been included in VA guidance to providers. VA physician advice questions, adapted from standardized HEDIS measures (Davis, 1997), asked participants about advise/assist care received during at least one visit in the previous 12 months: “Did your VA doctor or health care provider say you should try to quit smoking? Did your VA doctor or health care provider talk about ways (other than medication) to help you with quitting smoking? Was medication talked about to help you quit smoking (for example: nicotine gum, patch, nasal spray, inhaler, prescription medication)?”
Use of cessation treatments.
Smokers were asked if they had used behavioral counseling (in person or telephone) or smoking cessation medications to try to quit smoking in the previous 12 months, either inside or outside the VA. Survey questions about prior treatment were adapted from the California Tobacco Surveys (California Department of Public Health) and the Centers for Disease Control and Prevention (2017) Behavioral Risk Factor Surveillance Survey.
Satisfaction with VA care.
Patient satisfaction with care is a multidimensional concept, influenced by patient, provider, and health care system characteristics, as well as patient expectations and preferences (Ware, Snyder, Wright, & Davies, 1983). Satisfaction with VA cessation care questions were designed to assess overall satisfaction with care, as well as practical concerns specific to obtaining smoking cessation care: “How satisfied were you with help received from your VA doctor or health care provider about quitting smoking? How satisfied were you with the process of obtaining medications from the VA to help you quit smoking?” The proportion of smokers who reported being very or somewhat satisfied was reported; patients who responded, “I never received help,” were not included in the denominator.
Baseline Demographic and Smoking Characteristics
Additional measures described patient personal and smoking characteristics. Standardized sociodemographic questions were asked at baseline and covered race, ethnicity, marital status, education level, employment status, and income (Fu et al., 2012). We assessed nicotine dependence with the two-item Heaviness of Smoking Index (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989) and asked participants whether they had made at least one quit attempt (lasting at least 24 hours) in the previous year. Cognitive factors included self-efficacy to quit (Baldwin et al., 2006; Dijkstra & Vries, 2000), readiness to quit (Abrams et al., 2003; Biener & Abrams, 1991), and attitudes toward nicotine replacement therapy (Etter & Perneger, 2001). Environmental factors included whether smoking was allowed at home, whether the participant lived with other smokers, and/or perceived external pressure to quit from “people close to me.” We obtained information on age, gender, and comorbid mental health conditions (using International Classification of Diseases 9the edition, codes) from VA administrative data sources.
Postintervention
Six-month prolonged abstinence.
The primary postintervention outcome for this analysis was self-reported 6-month prolonged abstinence at the 1-year follow-up, and was assessed among all randomized, included participants, regardless of treatment use during the study. Quit attempts were self-reported intentional cessation for more than 24 hours. Use of smoking cessation therapies was self-reported use of any cessation medications, telephone counseling, or a combination of medication and counseling, including therapies from within the VA or from outside sources.
Analysis
Because the study design involved stratified sampling across four study sites, our estimations, testing, and modeling procedures are stratified analyses. A complete case analysis included only available survey responses. Baseline characteristics for women and men were compared using the Wald χ2 test for categorical variables and the Wald F test for continuous variables. Because randomization was not stratified by gender, we tested for differences in baseline characteristics between treatment arms within each gender, to include imbalanced covariates in later models. Logistic regression analyses, taking into account the sampling design and imbalanced covariates (i.e., age), were conducted to test the effect of gender on baseline experiences with smoking cessation recommendations and treatment. We then used logistic regression modeling to test for an interaction of Gender × Treatment (PRO vs. UC) with respect to prolonged abstinence at follow-up, again taking into account the sampling design and imbalanced covariates. The proportion of participants who used cessation treatments, as well as the proportion abstinent and treatment arm effect sizes (odds ratios [ORs] with 95% CI) were obtained separately for women and men in subgroup analyses.
Results
Of the 5,123 randomized veterans, baseline and follow-up surveys were returned by 138 women and 2,516 men (51.8% response rate). There was a differential response rate by gender in the PRO arm, but not in the UC arm. Among smokers randomized to PRO, women were less likely than men to complete both baseline and follow-up surveys (response rate 36.5% for women vs. 51.1% for men). In UC, the response rates did not differ by gender: 56.4% for women and 53% for men. Women comprised 5.2% of the study sample, proportionate to their representation in the VA at the time of enrollment (6%; Frayne et al., 2014). Age was the only covariate found to be imbalanced between treatment arms for any gender and, therefore, was included in subsequent models.
Pre-intervention
Baseline characteristics by gender
Compared with male smokers, female smokers were younger, less likely to be married, and were more likely to be employed (Table 1 ). Cigarettes per day and time to first cigarette did not differ significantly between women and men. Women began smoking at a slightly older age and were much more likely to smoke menthol cigarettes. Men were more likely than women to use tobacco products other than cigarettes in addition to smoking cigarettes. Female and male smokers were equally likely to have tried to quit in the previous year and reported similar confidence and self-efficacy to quit, similar perceptions of the advantages and disadvantages of nicotine replacement therapy, and similar environmental pressures to quit (smoking allowed in the home or living with another smoker). Women were significantly more likely than men to strongly agree that “people important to me want me to quit smoking.” Administrative data revealed significantly higher rates of depression and anxiety among female smokers, and higher rates of substance use disorder among male smokers. Post-traumatic stress disorder diagnoses did not differ by gender.
Table 1.
Baseline Sample Characteristics by Gender*
| Female Smokers, n (%) or Mean (SE) | Male Smokers, n (%) or Mean (SE) | p Value | |
|---|---|---|---|
| All participants | 138 | 2,516 | — |
| Treatment group | |||
| Usual care | 88 | 1,298 | — |
| Proactive outreach | 50 | 1,218 | |
| Sociodemographic characteristics | |||
| Age (y) | 51.2 (0.9) | 59.0 (0.2) | <.01 |
| Race | |||
| White | 72 (57%) | 1,533 (67%) | .17 |
| Black | 48 (32%) | 672 (23%) | |
| Hispanic | 8(5%) | 158 (5%) | |
| Other | 10(7%) | 153 (6%) | |
| Married or cohabiting | 46 (36%) | 1,245 (52%) | <.01 |
| Currently employed | 61 (46%) | 715(29%) | <.01 |
| Annual income ≤$20k | 56 (40%) | 1,172 (48%) | .06 |
| Smoking behaviors | |||
| Cigarettes per day | |||
| ≤10 | 61 (40%) | 877 (32%) | .12 |
| 11–20 | 54 (42%) | 1,049 (44%) | |
| ≥21 | 23(18%) | 546 (24%) | |
| Time to first cigarette (min) | |||
| >31 | 39 (29%) | 689 (26%) | .27 |
| 6–30 | 66 (47%) | 1,308 (54%) | |
| <5 | 33(25%) | 499 (20%) | |
| Age of smoking initiation (y) | 18.8 (0.5) | 17.2 (0.1) | <.01 |
| Menthol cigarette user | 81 (56%) | 881 (31%) | <.01 |
| Use other tobacco products | 28(21%) | 1,124 (47%) | <.01 |
| Cessation attitudes and attempts | |||
| Quit attempt in past 12 mo | 78 (56%) | 1,392 (54%) | .73 |
| Readiness to quit | 5.8 (0.2) | 5.7 (0.0) | .55 |
| Global confidence to quit (0–5) | 2.2 (0.1) | 2.3 (0.0) | .24 |
| Self-efficacy to quit | |||
| Emotional subscale | −0.7 (0.2) | −0.4 (0.0) | .06 |
| Skill subscale | 0.4 (0.1) | 0.1 (0.0) | .06 |
| Social subscale | −0.2 (0.2) | −0.2 (0.0) | .94 |
| Perceptions of NRT | |||
| Advantages subscale | 29.1 (0.5) | 28.4 (0.1) | .16 |
| Disadvantages subscale | 11.6 (0.3) | 11.9 (0.1) | .49 |
| Smoking not allowed in home | 48 (37%) | 937 (41%) | .44 |
| Another smoker lives in home | 60 (44%) | 1,043 (42%) | .69 |
| People important to me want me to quit smoking | |||
| Strongly disagree to neutral | 22 (16%) | 493 (22%) | <.01 |
| Somewhat agree | 19(15%) | 554 (24%) | |
| Strongly agree | 88 (68%) | 1,309 (55%) | |
| Mental health diagnoses | |||
| Depression | 53 (40%) | 493 (19%) | <.01 |
| Anxiety | 21 (16%) | 219 (9%) | .03 |
| PTSD | 12 (9%) | 200 (7%) | .46 |
| Substance use disorder | 17 (12%) | 499 (19%) | .02 |
Abbreviations: NRT, nicotine replacement therapy; PTSD, Post-traumatic stress disorder; SE, standard error.
Summary statistics adjust for study design with stratified sampling by site.
Prior Year Smoking Cessation Recommendations and Treatment
VA physician advice
Nearly all female (89%) and male (93%) smokers reported being advised to quit smoking by their primary care provider in the year before study enrollment (Table 2). There were no statistically significant differences in the proportions of women or men who reported that a VA provider discussed ways to quit other than medications (79% of women vs. 74% of men) or discussed medications to help with quitting (72% vs. 71%).
Table 2.
Baseline Experiences with Smoking Cessation Recommendations and Treatment, by Gender, Within the Past 12 Months
| Female Smokers, n (%)* | Male Smokers, n (%)* | Age-Adjusted Odds Ratio* (95% CI) | |
|---|---|---|---|
| N | 138 | 2,516 | |
| VA physician advice | |||
| VA provider advised to quit | 113 (89%) | 2,200 (93%) | 0.63 (0.36–1.13) |
| VA provider discussed nonmedical ways to quit | 100(79%) | 1,748 (74%) | 1.31 (0.84–2.05) |
| VA provider discussed medications to quit | 90(72%) | 1,669(71%) | 1.05 (0.71–1.56) |
| Use of cessation treatments | |||
| Behavioral counseling from VA, any | 16(12%) | 262 (10%) | 1.19 (0.69–2.07) |
| In-person counseling | 16(11%) | 240 (9%) | 1.26 (0.72–2.19) |
| Phone counseling | 0(0%) | 29(1%) | Not estimable |
| Behavioral counseling from outside VA, any | 15(12%) | 153 (6%) | 2.09 (1.17–3.73) |
| In-person counseling | 11 (8%) | 127 (5%) | 1.68 (0.87–3.27) |
| Phone counseling | 6 (5%) | 30(1%) | 5.23 (1.99–13.74) |
| Cessation medication use from VA | 52 (39%) | 867 (34%) | 1.22 (0.84–1.75) |
| Cessation medication use from outside VA | 16(11%) | 305(12%) | 0.96 (0.56–1.67) |
| Satisfaction with VA cessation care† | |||
| N | 96 | 1,787 | |
| Very or somewhat satisfied with help received to quit | 57 (62%) | 1,106 (62%) | 0.99 (0.65–1.52) |
| N | 75 | 1,401 | |
| Very or somewhat satisfied with process of obtaining meds to quit | 33 (47%) | 874 (62%) | 0.54 (0.33–0.87) |
Abbreviations: SE, standard error; VA, Veterans Health Administration.
Proportions and odds ratios are model based. The model adjusts for study design and age.
Denominator for satisfaction questions excludes participants who reported that they never received help with smoking cessation
Use of cessation treatments
Few smokers reported having used behavioral counseling, either in person or over the phone, in the past year, either within or outside the VA. Most use did not differ by gender, with one exception: female smokers were more likely to have used non-VA telephone counseling (e.g., state or insurance-based quitline support) than male smokers (5% vs. 1%). More smokers reported receiving cessation medications from the VA (39% of women and 34% of men) than from outside the VA (11% of women and 12% of men); these proportions were not significantly different bygender.
Satisfaction with VA cessation care
Sixty-two percent of female and male smokers reported being very or somewhat satisfied with the help they received with quitting. Women were significantly less likely than men to report being very or somewhat satisfied with the process of obtaining medications to quit (47% of women vs. 62% of men).
Postintervention
Six-month prolonged abstinence
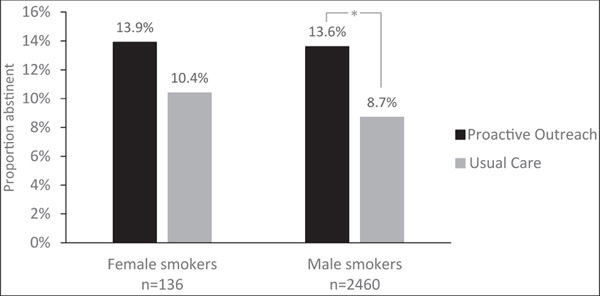
Overall, similar proportions of female and male smokers reported 6-month prolonged abstinence at the 1-year follow-up (12.3% and 10.9%, respectively; p = .61; Table 3; Figure 1). There was not a statistically significant interaction of Gender × Treatment (proactive vs. UC) with respect to smoking cessation (p = .75). Among 50 women randomized to proactive care, 7 quit smoking, as compared with 9 of the 88 randomized to UC (model-based prolonged abstinence estimates for women 13.9% in proactive care vs. 10.4% in UC; age-adjusted OR, 1.39; 95% CI, 0.48–3.99). Among 1,218 men randomized to proactive care, 161 quit, as compared with 110 of the 1,298 men in UC (13.6% in proactive care vs. 8.7% in UC; age-adjusted OR, 1.65; 95% CI, 1.28–2.14).
Table 3.
Postintervention Outcomes: Six-Month Prolonged Abstinence, Quit Attempts, and Treatment Use by Treatment Arm and Gender
| Proactive Outreach, n (%) | Usual Care (Ref), n (%)* | Age-Adjusted Odds Ratio* (95% Cl) | |
|---|---|---|---|
| N | 1,268 | 1,386 | |
| Six-month abstinence | |||
| Female smokers | 7 (13.9%) | 9 (10.4%) | 1.39 (0.48–3.99) |
| Male smokers | 161 (13.6%) | 110(8.7%) | 1.65 (1.28–2.14) |
| Quit attempts | |||
| Female smokers | 28 (54.6%) | 49 (54.6%) | 1.00 (0.45–2.21) |
| Male smokers | 667 (57.6%) | 699 (54.6%) | 1.13 (0.94–1.35) |
| Use of in-person counseling | |||
| Female smokers | 5 (14.3%) | 9(15.8%) | 0.89 (0.27–2.90) |
| Male smokers | 77 (9.2%) | 76 (8.4%) | 1.11 (0.80–1.55) |
| Use of phone counseling | |||
| Female smokers | 17 (57.2%) | 4 (10.5%) | 11.36 (3.42–37.66) |
| Male smokers | 174 (33.2%) | 29 (5.9%) | 7.92 (5.24–11.95) |
| Cessation medication use | |||
| Female smokers | 26 (52.5%) | 43 (55.7%) | 0.88 (0.40–1.94) |
| Male smokers | 528 (47.5%) | 510 (43.4%) | 1.18 (0.98–1.41) |
| Combined therapy | |||
| Female smokers | 13 (34.9%) | 9(15.7%) | 2.88 (1.10–7.58) |
| Male smokers | 174 (22.4%) | 70 (8.6%) | 3.08 (2.29–4.14) |
Proportions and odds ratios are model based. The model adjusts for study design and age, and baseline measures when applicable
Figure 1.
Proportion of female and male smokers who report 6-month prolonged abstinence at the 1-year follow-up, by treatment arm.
Quit attempts
More than one-half of female and male smokers made at least one quit attempt during the 1-year follow-up period, with no statistically significant difference by treatment arm or gender.
Use of smoking cessation therapies
Among women and men, randomization to the PRO intervention was associated with significantly higher use of telephone counseling (for women: 57.2% vs. 10.5%; OR, 11.36; 95% CI, 3.42–37.66; for men: 33.2% vs. 5.9%; OR, 7.92; 95% CI, 5.24–11.95) or combined therapy with counseling and medication (for women: 34.9% vs. 15.7%; OR, 2.88; 95% CI, 1.10–7.58; for men: 22.4% vs. 8.6%; OR, 3.08; 95% CI, 2.29–4.14), compared with UC. In contrast, PRO was not associated with significant increases in rates of in-person cessation counseling (for women: 14.3% vs. 15.8%; OR, 0.89; 95% CI, 0.27–2.90; for men: 9.2% vs. 8.4%; OR, 1.11; 95% CI, 0.80–1.55) or medication use (for women: 52.5% vs. 55.7%; OR, 0.88; 95% CI, 0.40–1.94; for men: 47.5% vs. 43.4%; OR, 1.18; 95% CI, 0.98–1.41).
Discussion
In a large, multisite, randomized trial of a PRO smoking cessation intervention, we analyzed baseline experiences of smoking cessation care in the VA as well as postintervention outcomes by gender. Baseline experiences did not vary significantly by gender with respect to advice to quit or use of cessation medications for recent quit attempts. However, women were less likely than men to be satisfied with the process of obtaining cessation medications. After a PRO intervention, female and male smokers were both more likely to use telephone counseling and combined therapy with counseling and medication, but only male smokers were significantly more likely to achieve prolonged abstinence if randomized to PRO rather than UC. Prolonged abstinence outcomes for women were of a similar magnitude and direction, but did not reach statistical significance.
Baseline Experiences with Smoking Cessation Recommendations and Treatment in VA
Compared with our parallel analysis, based on data from 2000, rates of advice to quit improved for both women and men in the VA from approximately two-thirds of women and men to approximately 90% of each a decade later. This rate is far higher than the range seen in surveys of nonprofit health maintenance organization or Medicare patients (71%–76%) (Shadel et al., 2015; Stevens et al., 2005; Quinn et al., 2005) and the range from national population-based surveys of smokers with a health care visit in the past 12 months (57%–66%; Babb, 2017; Kruger, O’Halloran, Rosenthal, Babb, & Fiore, 2016). Recommendations for medications and behavioral counseling to quit increased substantially for both women and men, and the gender disparity related to medication prescriptions that we previously identified was no longer evident. Our findings build on intervening work by Farmer et al. (2011), which revealed progressive improvement in levels of advice to quit (87% of women, 83% of men) and cessation assistance (63% and 62% with medications; 61% and 60% other treatments) for female and male smokers in the VA, respectively. Some credit for these improvements for both women and men over time may be attributable to VA policy directives that have made cessation medications and counseling more readily available to all patients, such as the elimination of copayments for individual or group cessation counseling sessions in 2005 (Petzel, 2014).
Despite these improvements in physician advice to quit, baseline satisfaction with cessation care was relatively low for both women and men. System-level changes to create a more streamlined, accessible process for obtaining cessation medications have been shown to increase use of cessation medications (Ku, Brantley, Bysshe, Steinmetz, & Bruen, 2016). Satisfaction with the process of obtaining cessation medications was significantly lower for women than men; the reason for this disparity was unclear from our data. No other studies have examined this specific disparity, but several surveys have compared female and male veterans’ satisfaction with VA pharmacy services more broadly, with mixed results. In a 2004 survey, women reported lower satisfaction than men with respect to VA pharmacy pickup and mail services in unadjusted analyses, but the differences became insignificant after accounting for demographic and health factors (Wright, Craig, Campbell, Schaefer, & Humble, 2006). In contrast, a more recent survey found very high satisfaction with pharmacy services for both female and male veterans, but described some disparities by race and gender for satisfaction with pharmacy services and related measures such as cost and respect (Zickmund et al., 2018). Future efforts to study and improve smoking cessation in VA should include attention to potential gender differences in experiences obtaining cessation medications.
At baseline, most smokers had not used behavioral counseling to try to quit smoking during the past year: 10%−12% of all smokers reported use of VA behavioral counseling, regardless of reporting a formal quit attempt. Population-based surveys show that relatively few U.S. smokers use behavioral counseling during a quit attempt (4%−9%; Curry, Sporer, Pugach, Campbell, & Emery, 2007; Shiffman, Brockwell, Pillitteri, & Gitchell, 2008). Although comparable data from other health care systems are lacking, rates in this study also exceeded behavioral counseling use by insurance status for privately insured (2.6%), Medicare (0.9%), and Medicaid (0.9%) populations (Cokkinides, Ward, Jemal, & Thun, 2005). Women were more likely than men to have used telephone counseling, although the absolute numbers were small. This finding is consistent with analyses of telephone quitlines worldwide, which universally demonstrate higher use by female smokers (Abdullah, Lam, Chan, & Hedley, 2004; Gilbert, Sutton, & Sutherland, 2005; Miller, Wakefield, & Roberts, 2003; Swartz, Cowan, Klayman, Welton, & Leonard, 2005). The rate of telephone counseling use among male veteran smokers at baseline mirrored the national average of 1% of smokers (Cummins, Bailey, Campbell, Koon-Kirby, & Zhu, 2007). Higher baseline use of phone counseling among female smokers highlights the potential of phone-based PRO interventions for women.
Gender Differences in Response to PRO
After PRO, both female and male smokers were more likely than those randomized to UC to use telephone counseling and combined therapy with counseling and medication. For male smokers, a small, statistically significant effect of PRO on prolonged abstinence was seen. This small effect of a population- level intervention could translate to a meaningful public health impact. A small effect on prolonged abstinence was also observed among women, but the confidence interval was wider and included 1. These post hoc subgroup findings add to the limited, mixed evidence on gender differences in response to proactive smoking cessation interventions.
Some prior research with female smokers has not demonstrated a significant benefit from PRO interventions. Several randomized trials proactively identified and recruited female smokers in specific populations, such as pregnant women (Rigotti et al., 2006; Solomon, Secker-Walker, Flynn, Skelly, & Capeless, 2000) or women with abnormal pap test results (McBride et al., 1999; McClure, Westbrook, Curry, & Wetter, 2005). Women in those trials were randomized to a proactive telephone counseling intervention or to a UC/best practice control. Three of four studies found no statistically significant improvement in abstinence rates at any time point for proactive counseling as compared with UC; one found short-term improvement at 6 months but not at 12 months. Compared with our study population, each of these women-only trials included more women (n = 151–580) with a younger mean age (23–36 years vs. 51 years in our study). A gender gap in long-term efficacy outcomes may not be specific to PRO interventions: a recent review of sex/gender differences in smoking cessation reported that, in general, women and men attempt to quit at similar rates, but women are less likely to maintain abstinence in studies with longer follow-up (Smith, Bessette, Weinberger, Sheffer, & McKee, 2016).
In contrast, several studies have shown a benefit of proactive cessation care for long-term abstinence in female smokers. Recently, Haas et al. (2015) conducted a randomized, controlled trial using interactive voice response technology to proactively offer cessation support to a group of low-income smokers. In a subgroup analysis, women had significantly higher odds of abstinence at the 9-month follow-up when randomized to PRO versus UC; the result for men was in the same direction but was not statistically significant. That study was smaller than ours overall (n = 707), but included many more women (68% female). Similarly, we recently completed a large trial of PRO to low- income (non-VA) smokers in Minnesota (Fu et al., 2016) and in an unpublished subgroup analysis found a statistically significant intervention effect among a large sample of female smokers (n = 1,250 women; 15.7% in PRO reported 6-month prolonged abstinence at the 1-year follow-up, compared with 11.9% in UC; p = .04), with results in the same direction but not statistically significant among a smaller sample of male smokers (n = 507 men; 18.3% vs. 12.4% reported prolonged abstinence in PRO vs. UC; p = .06; unpublished results provided via personal communication with Patrick Hammett, February 20, 2018). Compared with the smaller, women-only trials discussed, more recent studies likely benefit from increased availability of effective cessation medications and contemporaneous public health interventions (such as smoke-free policies). Taken together with our results, these larger, more recent trials suggest that PRO is an effective smoking cessation intervention for women.
Limitations
Women veterans are a unique subpopulation, and these results are not necessarily generalizable to other groups. The study sample, from four VA sites, was not designed to be representative of all VA smokers. Only current smokers were enrolled, so baseline experiences with smoking cessation recommendations and treatment in the VA were likely biased by the fact that participants had not achieved abstinence. Prolonged abstinence is a self-reported measure that may be subject to social desirability bias. Although multiple studies have validated smoking self-report (Patrick et al., 1994; Yeager & Krosnick, 2010), including among VA smokers (Noonan, Jiang, & Duffy, 2013), self-report may be less reliable among populations for whom smoking is particularly socially undesirable, such as pregnant women (Florescu et al., 2009). However, overall rates of smoking status misclassification by self-report do not seem to vary significantly by gender (Caraballo, Giovino, Pechacek, & Mowery, 2001).
Response rates were lower for women (but not men) assigned to PRO, as compared with UC. We doubt that this finding represents a negative reaction to the intervention by women because the difference in response rates was present at baseline, before receipt of any outreach. We suspect the differential response rate represents a combination of chance and a smaller sample size in the PRO arm. Randomization was not stratified by gender, which may have contributed to the lower number of women assigned to PRO rather than UC. Future trials should oversample women veterans, to increase sample size, and consider blocking randomization by sex, to ensure matched treatment groups.
Owing to the relatively small number of women enrolled, we lacked power to show an interaction between gender and treatment with respect to prolonged abstinence. Additionally, we report a complete case intent-to-treat analysis that is subject to bias from missing data that is not missing at random. Post hoc subgroup analyses provide descriptive data about experiences with PRO for female and male smokers separately, but results require replication in a larger sample to be conclusive.
Implications for Practice and/or Policy
VA providers and policymakers must address patient satisfaction with tobacco cessation care, particularly with respect to obtaining cessation medications. PRO to smokers helps to facilitate treatment use among female and male veterans and can be considered a tool for improving access to care. Future cessation trials should oversample women veteran smokers.
Conclusions
VA smoking cessation care has improved substantially in the past decade for both women and men. Research on smoking cessation interventions for women veterans remains limited despite high smoking rates among women veterans. This study adds to the evidence that PRO can be an effective intervention for both female and male smokers.
Acknowledgments
Dr. Danan had full access to all the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis.
Supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and Health Services Research and Development (IAB-05-303). The views expressed in this article are those of the authors and do not represent the views of the VA or the US Government. This trial is registered in clinicaltrials.gov (NCT00608426).
Footnotes
Conflict of interest statement: The authors declare they have no competing interests.
References
- Abdullah A, Lam T, Chan S, & Hedley A. (2004). Which smokers use the smoking cessation Quitline in Hong Kong, and how effective is the Quitline? Tobacco Control, 13(4), 415–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrams DB, Niaura RS, Brown RA, Emmons KM, Goldstein MG, & Monti PM (2003). The tobacco dependence treatment handbook. New York: The Guilford Press. [Google Scholar]
- Babb S. (2017). Quitting smoking among adults—United States, 2000–2015. MMWR Morbidity and Mortality Weekly Report, 65,1457–1464. [DOI] [PubMed] [Google Scholar]
- Baldwin AS, Rothman AJ, Hertel AW, Linde JA, Jeffery RW, Finch EA, & Lando HA (2006). Specifying the determinants of the initiation and maintenance of behavior change: An examination of self-efficacy, satisfaction, and smoking cessation. Health Psychology, 25(5), 626. [DOI] [PubMed] [Google Scholar]
- Barnett PG, Hamlett-Berry K, Sung H-Y, & Max W. (2015). Health care expenditures attributable to smoking in military veterans. Nicotine & Tobacco Research, 17(5), 586–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, & Abrams DB (1991). The contemplation ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology, 10(5), 360. [DOI] [PubMed] [Google Scholar]
- Brown DW (2010). Smoking prevalence among US Veterans. Journal of General Internal Medicine, 25(2), 147–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, & Mowery PD (2001). Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Epidemiology, 153(8), 807–814. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Behavioral Risk Factor Surveillance System Questionnaire. [Google Scholar]
- Cokkinides VE, Ward E, Jemal A, & Thun MJJ (2005). Under-use of smoking-cessation treatments: Results from the National Health Interview Survey, 2000. American Journal of Preventive Medicine, 28(1), 119–122. [DOI] [PubMed] [Google Scholar]
- Cummins SE, Bailey L, Campbell S, Koon-Kirby C, & Zhu S-H (2007). Tobacco cessation quitlines in North America: A descriptive study. Tobacco Control, 16(Suppl. 1), i9–i15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry SJ, Sporer AK, Pugach O, Campbell RT, & Emery SJ (2007). Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. American Journal of Public Health, 97(8), 1464–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis RM (1997). Healthcare report cards and tobacco measures. Tobacco Control, 6(Suppl. 1), S70–S77. [PubMed] [Google Scholar]
- Davis TM, Bush KR, Kivlahan DR, Dobie DJ, & Bradley KA (2003). Screening for substance abuse and psychiatric disorders among women patients in a VA Health Care System. Psychiatric Services, 54(2), 214–218. [DOI] [PubMed] [Google Scholar]
- Dijkstra A, & Vries HD (2000). Self-efficacy expectations with regard to different tasks in smoking cessation. Psychology and Health, 15(4), 501–511. [Google Scholar]
- Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, & Bradley KA (2004). Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment. Archives of Internal Medicine, 164(4), 394–400. [DOI] [PubMed] [Google Scholar]
- Duffy SA, Kilbourne AM, Austin KL, Dalack GW, Woltmann EM, Waxmonsky J, & Noonan D. (2012). Risk of smoking and receipt of cessation services among veterans with mental disorders. Psychiatric Services, 63(4), 325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etter JF, & Perneger TV (2001). Attitudes toward nicotine replacement therapy in smokers and ex-smokers in the general public. Clinical Pharmacology & Therapeutics, 69(3), 175–183. [DOI] [PubMed] [Google Scholar]
- Farmer MM, Rose DE, Riopelle D, Lanto AB, & Yano EM (2011). Gender differences in smoking and smoking cessation treatment: An examination of the organizational features related to care. Women’s Health Issues, 21(Suppl. 4), S182–S189. [DOI] [PubMed] [Google Scholar]
- Fiore M. (2008). Treating tobacco use and dependence: 2008 update: Clinical practice guideline. Collingdale, PA: Diane Publishing. [Google Scholar]
- Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, & Koren GJ (2009). Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: Focus on developmental toxicology. Therapeutic Drug Monitoring, 31(1), 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne S, Phibbs CS, Saechao F, Maisel NC, Friedman SA, & Finlay A. (2014). Sourcebook: Women Veterans in the Veterans Health Administration. Volume 3. Sociodemographics, Utilization, Costs of Care, and Health Profile. Washington, DC. [Google Scholar]
- Frayne SM, Skinner KM, Sullivan LM, & Freund KM (2003). Sexual assault while in the military: Violence as a predictor of cardiac risk? Violence and Victims, 18(2), 219. [DOI] [PubMed] [Google Scholar]
- Fu SS, van Ryn M, Nelson D, Burgess DJ, Thomas JL, Saul J, … Joseph AM(2016). Proactive tobacco treatment offering free nicotine replacement therapy and telephone counselling for socioeconomically disadvantaged smokers: A randomised clinical trial. Thorax, 71(5), 446–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu SS, van Ryn M, Sherman SE, Burgess DJ, Noorbaloochi S, Clothier B, & Joseph AM (2012). Population-based tobacco treatment: Study design of a randomized controlled trial. BMC Public Health, 12(1), 159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert H, Sutton S, & Sutherland G. (2005). Who Calls QUIT®? The characteristics of smokers seeking advice via a telephone helpline compared with smokers attending a clinic and those in the general population. Public Health, 119(10), 933–939. [DOI] [PubMed] [Google Scholar]
- Haas JS, Linder JA, Park ER, Gonzalez I, Rigotti NA, Klinger EV, . Marinacci LX (2015). Proactive tobacco cessation outreach to smokers of low socioeconomic status: A randomized clinical trial. JAMA Internal Medicine, 175(2), 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, & Robinson J. (1989). Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Addiction, 84(7), 791–800. [DOI] [PubMed] [Google Scholar]
- Huxley RR, & Woodward M. (2011). Cigarette smoking as a risk factor for coronary heart disease in women compared with men: A systematic review and meta-analysis of prospective cohort studies. Lancet, 378(9799), 1297–1305. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM). (2009). Combating tobacco use in military and veteran populations. Washington, DC: Author. [Google Scholar]
- Institute, U. S. N. C. (2017). A socioecological approach to addressing tobacco-related health disparities. Bethesda, MD. [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, & Graffunder CM (2016). Current cigarette smoking among adults—United States, 2005–2015. MMWR Morbidity and Mortality Weekly Report, 65, 1205–1211. [DOI] [PubMed] [Google Scholar]
- Kehle-Forbes SM, Harwood EM, Spoont MR, Sayer NA, Gerould H, & Murdoch M. (2017). Experiences with VHA care: A qualitative study of US women veterans with self-reported trauma histories. BMC Women’s Health, 17(1), 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger J, O’Halloran A, Rosenthal AC, Babb SD, & Fiore MC (2016). Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health, 16(1), 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku L, Brantley E, Bysshe T, Steinmetz E, & Bruen BK (2016). How Medicaid and other public policies affect use of tobacco cessation therapy, United States, 2010–2014. Preventing Chronic Disease, 13, E150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Scholes D, Grothaus LC, Curry SJ, Ludman E, & Albright J. (1999). Evaluation of a minimal self-help smoking cessation intervention following cervical cancer screening. Preventive Medicine, 29(2), 133–138. [DOI] [PubMed] [Google Scholar]
- McClure JB, Westbrook E, Curry SJ, & Wetter DW (2005). Proactive, motivationally enhanced smoking cessation counseling among women with elevated cervical cancer risk. Nicotine & Tobacco Research, 7(6), 881–889. [DOI] [PubMed] [Google Scholar]
- Miller C, Wakefield M, & Roberts L. (2003). Uptake and effectiveness of the Australian telephone Quitline service in the context of a mass media campaign. Tobacco Control, 12(Suppl. 2), ii53–ii58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noonan D, Jiang Y, & Duffy SA (2013). Utility of biochemical verification of tobacco cessation in the Department of Veterans Affairs. Addictive Behaviors, 38(3), 1792–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, & Kinne S. (1994). The validity of self-reported smoking: A review and meta-analysis. American Journal of Public Health, 84(7), 1086–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzel RA (2014). National Smoking and Tobacco Use Cessation Program. (1056). Washington, DC. [Google Scholar]
- Quinn VP, Stevens VJ, Hollis JF, Rigotti NA, Solberg LI, Gordon N, … Zapka J. (2005). Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. American Journal of Preventive Medicine, 29(2), 77–84. [DOI] [PubMed] [Google Scholar]
- Rigotti NA, Park ER, Regan S, Chang Y, Perry K, Loudin B, & Quinn V. (2006). Efficacy of telephone counseling for pregnant smokers: A randomized controlled trial. Obstetrics & Gynecology, 108(1), 83–92. [DOI] [PubMed] [Google Scholar]
- Shadel WG, Elliott MN, Haas AC, Haviland AM, Orr N, Farmer MM, . Cleary PD (2015). Clinician advice to quit smoking among seniors. Preventive Medicine, 70, 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SE, Fu SS, Joseph AM, Lanto AB, & Yano EM (2005). Gender differences in smoking cessation services received among veterans. Womens Health Issues, 15(3), 126–133. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, & Gitchell JG (2008). Use of smoking-cessation treatments in the United States. American Journal of Preventive Medicine, 34(2), 102–111. [DOI] [PubMed] [Google Scholar]
- Smith PH, Bessette AJ, Weinberger AH, Sheffer CE, & McKee SA (2016). Sex/genderdifferencesinsmokingcessation:Areview. PreventiveMedicine,92,135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PH, Kasza KA, Hyland A, Fong GT, Borland R, Brady K, . McKee, S. A. (2015). Gender differences in medication use and cigarette smoking cessation: Results from the International Tobacco Control Four Country Survey. Nicotine & Tobacco Research, 17(4), 463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon LJ, Secker-Walker RH, Flynn BS, Skelly JM, & Capeless EL (2000). Proactive telephone peer support to help pregnant women stop smoking. Tobacco Control, 9(Suppl. 3), iii72-iii74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens VJ, Solberg LI, Quinn VP, Rigotti NA, Hollis JA, Smith KS, . Boyle RG (2005). Relationship between tobacco control policies and the delivery of smoking cessation services in nonprofit HMOs. Journal of the National Cancer Institute Monographs, (35), 75–80. [DOI] [PubMed] [Google Scholar]
- Suris A, & Lind L. (2008). Military sexual trauma: A review of prevalence and associated health consequences in veterans. Trauma, Violence, &Abuse, 9(4), 250–269. [DOI] [PubMed] [Google Scholar]
- Swartz SH, Cowan TM, Klayman JE, Welton MT, & Leonard BA (2005). Use and effectiveness of tobacco telephone counseling and nicotine therapy in Maine. American Journal of Preventive Medicine, 29(4), 288–294. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2001). Women and smoking: A report of the Surgeon General. Rockville, MD: Author. [Google Scholar]
- Ware JE, Snyder MK, Wright WR, & Davies AR (1983). Defining and measuring patient satisfaction with medical care. Evaluation and Program Planning, 6(3–4), 247–263. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, Esan H, Hunt MG, & Hoff RA (2016). A review of research on smoking behavior in three demographic groups of veterans: Women, racial/ethnic minorities, and sexual orientation minorities. American Journal of Drug and Alcohol Abuse, 42(3), 254–268. [DOI] [PubMed] [Google Scholar]
- Wright SM, Craig T, Campbell S, Schaefer J, & Humble C. (2006). Patient satisfaction of female and male users of Veterans Health Administration services. Journal of General Internal Medicine, 21(Suppl. 3), S26–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, & Krosnick JA (2010). The validity of self-reported nicotine product use in the 2001 −2008 National Health and Nutrition Examination Survey. Medical Care, 48(12), 1128–1132. [DOI] [PubMed] [Google Scholar]
- Zickmund SL, Burkitt KH, Gao S, Stone RA, Jones AL, Hausmann LR, .Fine MJ (2018). Racial, ethnic, and gender equity in veteran satisfaction with health care in the Veterans Affairs Health Care System. Journal of General Internal Medicine, 33(3), 305–331. [DOI] [PMC free article] [PubMed] [Google Scholar]