Abstract
To improve the diagnostic efficiency of prostate cancer (PCa) and reduce unnecessary biopsies, we defined and analyzed the diagnostic efficiency of peripheral zone prostate-specific antigen (PSA) density (PZ-PSAD). Patients who underwent systematic 12-core prostate biopsies in Shanghai General Hospital (Shanghai, China) between January 2012 and January 2018 were retrospectively identified (n = 529). Another group of patients with benign prostatic hyperplasia (n = 100) were randomly preselected to obtain the PSA density of the non-PCa cohort (N-PSAD). Prostate volumes and transition zone volumes were measured using multiparameter magnetic resonance imaging (mpMRI) and were combined with PSA and N-PSAD to obtain the PZ-PSAD from a specific algorithm. Receiver operating characteristic (ROC) curve analysis was used to assess the PCa detection efficiency in patients stratified by PSA level, and the area under the ROC curve (AUC) of PZ-PSAD was higher than that of PSA, PSA density (PSAD), and transition zone PSA density (TZ-PSAD). PZ-PSAD could amend the diagnosis for more than half of the patients with inaccurate transrectal ultrasonography (TRUS) and mpMRI results. When TRUS and mpMRI findings were ambiguous to predict PCa (PIRADS score ≤3), PZ-PSAD could increase the positive rate of biopsy from 21.7% to 54.7%, and help 63.8% (150/235) of patients avoid unnecessary prostate biopsy. In patients whose PSA was 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, the ideal PZ-PSAD cut-off value for predicting clinically significant PCa was 0.019 ng ml−2, 0.297 ng ml−2, and 1.180 ng ml−2, respectively (sensitivity >90%). Compared with PSA, PSAD, and TZ-PSAD, the efficiency of PZ-PSAD for predicting PCa is the highest, leading to fewer missed diagnoses and unnecessary biopsies.
Keywords: benign prostate hyperplasia, detection efficiency, peripheral zone prostate-specific antigen density, prostate biopsy, prostate-specific antigen, prostatic neoplasm
INTRODUCTION
Prostate cancer (PCa) is one of the most common malignancies among men worldwide.1,2 With the aging of populations and changes in dietary and environmental factors, the incidence of prostate cancer has significantly increased.3 PCa patients in which the disease is detected late and those with a high degree of malignancy have a poor prognosis. Despite the effectiveness of androgen deprivation therapy (ADT) in the early stages of the disease, almost all patients deteriorate to castration-resistant prostate cancer (CRPC), which eventually leads to death.4 Therefore, early effective prostate cancer screening strategies are urgently needed to enable the identification of patients with PCa.
Prostate-specific antigen (PSA) has been an important screening indicator for prostate cancer in clinical practice.5 However, its main drawback is the lack of specificity and low diagnostic efficacy.6 Age-related benign prostatic hyperplasia (BPH) and prostatitis may also alter PSA values.7 Prostate volume (PV) is another strong predictor, and research into a volume-based prostate cancer identification strategy is worth exploring.8 One study reported that PSA density (PSAD), the ratio of PSA to PV, could increase the detection efficiency of PCa.9 Furthermore, another study extracted transition zone volume (TZV) from the PV and defined the ratio of total prostate-specific antigen (tPSA) to TZV as the transition zone of PSA density (TZ-PSAD), which improved the PCa detection efficiency for the PSA “gray zone”.10 However, these indicators preliminarily combine volume with PSA and require further precise quantification.
It is generally known that PCa mainly originates from the peripheral zone (PZ). Although a small portion of PCa originates from the transition zone (TZ), the degree of cell differentiation and disease prognosis are significantly better than those of prostate cancer originating from the PZ.11 This suggests that peripheral zone PSA density (PZ-PSAD) is more representative and targeted in predicting PCa. In order to define and calculate PZ-PSAD, we extracted the volume of the PZ (PZV) and the PSA values corresponding to the PZ and proposed a precise formula for PZ-PSAD. We compared the diagnostic efficacies of PZ-PSAD, PSA, PSAD, and TZ-PSAD and sought a better indicator to provide guidance for the diagnosis and screening of PCa.
PATIENTS AND METHODS
Patients
From January 2012 to January 2018, 529 males with suspected PCa underwent transrectal ultrasound-guided 12-core systematic prostatic biopsy in Shanghai General Hospital (Shanghai, China). The criteria for prostate biopsy were PSA level >4 ng ml−1 and/or abnormal findings on digital rectal examination (DRE), transrectal ultrasound (TRUS), or prostatic multiparameter magnetic resonance imaging (mpMRI). Those with an unclear history of prior medications and those with a history of 5α-reductase inhibitor treatment were excluded from the study cohort. After biopsy, patients with a pathological diagnosis of prostatic intraepithelial neoplasia or atypical small acinar proliferation were also excluded. Another 100 patients with BPH, who underwent prostatic hyperplasia surgery in Shanghai General Hospital and who had benign pathology with no malignant tumors, were randomly preselected. Their average PSA density served as the prostate-specific antigen density of the non-PCa cohort (N-PSAD), a parameter in the range of PSA density in the non-PCa cohort. This study was approved by the Ethics Committees of Shanghai General Hospital (2014KY054). All patients enrolled in the study provided informed consent and demonstrated good compliance.
Clinical data
Patients' baseline data, including age, PSA value, PV, TZV, and DRE; and TRUS and mpMRI findings, were collected. For patients with PCa, we obtained the Gleason score of the biopsy specimen, the number of positive cores after biopsy, and clinical tumor stage after radical surgery for PCa. In the mpMRI results, those with abnormal heterogeneous nodules in the mpMRI images and a Prostate Imaging Reporting and Data System (PIRADS) score >3 were registered as “positive,” and those without suspicious nodules or a PIRADS score ≤3 were registered as “negative.” The mpMRI was also used to measure the length, width, and height of the entire prostate and TZ by a radiologist. In the mpMRI image (Supplementary Figure 1 (224.2KB, tif) ), the transverse diameter (A), anteroposterior diameter (B) of the transition zone and the transverse diameter (C), and anteroposterior diameter (D) of the entire prostate are measured on a horizontal section. The superoinferior diameter of the transition zone (E) and that of the entire prostate (F) were measured on the sagittal plane. The PV was measured at the boundary of the prostate capsule, and the TZV was measured at the boundary of the fibrous layer of the TZ. The PV and TZV were calculated using the following ellipsoid volume formula: volume (ml) = (π/6) × anteroposterior diameter (cm) × transverse diameter (cm) × superoinferior diameter (cm).
The PZ-PSAD was calculated using the following formula: PZ-PSAD=  The numerator “PSA – (N – PSAD × TZV)” is the PSA value corresponding to the PZ, which was obtained by subtracting the PSA corresponding to the TZ from the total PSA. The denominator “PV-TZV” is the volume of the PZ. N-PSAD is the average PSA density obtained from the standardized BPH patients (n = 100).
The numerator “PSA – (N – PSAD × TZV)” is the PSA value corresponding to the PZ, which was obtained by subtracting the PSA corresponding to the TZ from the total PSA. The denominator “PV-TZV” is the volume of the PZ. N-PSAD is the average PSA density obtained from the standardized BPH patients (n = 100).
Biopsy procedure and pathological diagnosis
The transrectal systematic 12-core prostate biopsy was performed in patients with left lateral decubitus and local infiltration of mucosa; lidocaine gel (Kangye, Handan, China) was administered. Two experienced urologists performed the TRUS-guided biopsies and used the tips of the BARD MAGNUM instrument (Bard, Covington, GA, USA) with a penetration depth of 22 mm. Oral antibiotics, such as cephalosporin, quinolone, or metronidazole (Xinyi, Shanghai, China), and hemostatic agents, such as amino cyclic acid (Tiancheng, Changchun, China) or hemocoagulase (Aohong, Jinzhou, China), were administered immediately after the transrectal prostate biopsy for 3 days. After formalin fixation and paraffin embedding, the pathological sections were examined by two independent pathologists. The final pathological report included a gross description, site localization, pathological diagnosis, the number of positive cores, and Gleason score.
Statistical analyses
Mann–Whitney U test was used to compare the differences in age, PSA, PV, PSAD, TZ-PSAD, and PZ-PSAD between the PCa and non-PCa groups. Pearson's Chi-square (χ2) test or Fisher's exact test was used to compare DRE, TRUS, and mpMRI findings and the PCa detection rates between the groups. The Kruskal–Wallis test was used to compare Gleason scores and clinical tumor stages between the groups with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1. Analysis of variance (ANOVA) was used to compare differences in age, PSA, PV, PSAD, TZ-PSAD, PZ-PSAD, and the number of positive cores between the groups with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1. Area under the receiver operating characteristic (ROC) curves (AUCs) were used to calculate the efficacy of PZ-PSAD, PSA, PSAD, and TZ-PSAD for detecting PCa. The diagnostic efficacy for PCa was also assessed using different PZ-PSAD, PSA, PSAD, and TZ-PSAD cutoff values in men with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, 4.0–20.0 ng ml−1, and >20.0 ng ml−1. The following formula can be used to evaluate the efficiency of PCa diagnosis at different cutoff points for each volume-adjusted PSA parameter: total efficiency = sensitivity × specificity. The cutoff point with the greatest efficiency is considered the optimal threshold for diagnosing PCa.
All statistical analyses were performed using IBM SPSS version 23.0 (IBM Co., Armonk, NY, USA) and MedCalc version 11.6 (MedCalc software, Acacialaan, Ostend, Belgium). Data were presented as mean ± standard deviation (s.d.) or median (interquartile range [IQR]) for continuous proportional and categorical variables, respectively. All statistical tests were two sided, and statistical significance was set at P < 0.05.
RESULTS
Comparisons of the clinical characteristics between PCa and non-PCa patients in the study cohort are shown in Table 1. Overall, 44.6% (236/529) of the patients were histologically diagnosed with PCa. The differences in age, PSA, PV, PSAD, TZ-PSAD, and PZ-PSAD and DRE, TRUS, and mpMRI findings in patients with and without PCa were all significantly different (all P < 0.01). Patients with PCa were older and had higher values of PZ-PSAD, PSA, PSAD, and TZ-PSAD and positive findings on DRE, TRUS, and mpMRI than did patients with benign pathology. The mean value of PZ-PSAD between PCa and non-PCa groups differed the most (29.10 times), compared with PSA (5.24 times), PSAD (6.23 times), and TZ-PSAD (4.84 times). Similarly, the median value of PZ-PSAD between the two groups differed the most (7.08 times) among the four parameters, and the quartile interval of PZ-PSAD did not overlap between the two groups. This indicates that PCa and non-PCa patients have different ranges of PZ-PSAD data sets, and that PZ-PSAD best reflects the difference between the PCa and non-PCa groups.
Table 1.
Comparison of clinical characteristics between prostate cancer and nonprostate cancer patients in the study cohort
| Group | PCa | Non-PCa | P |
|---|---|---|---|
| Cases, n (%) | 236 (44.6) | 293 (55.4) | |
| Age (year) | |||
| Median (IQR) | 70 (66–77) | 66 (62–70) | |
| Mean±s.d. | 71.26±7.46 | 66.71±6.72 | <0.001a |
| PSA value (ng ml−1) | |||
| Median (IQR) | 15.68 (8.49–36.79) | 8.32 (5.82–12.41) | |
| Mean±s.d. | 56.51±158.17 | 10.79±9.75 | <0.001a |
| Prostate volume (ml) | |||
| Median (IQR) | 40.13 (30.99–61.77) | 45.79 (61.78–82.00) | |
| Mean±s.d. | 49.64±28.56 | 67.09±32.96 | <0.001a |
| PSAD (ng ml−2) | |||
| Median (IQR) | 0.389 (0.198–0.987) | 0.141 (0.098–0.198) | |
| Mean±s.d. | 1.209±3.243 | 0.194±0.233 | <0.001a |
| TZ-PSAD (ng ml−2) | |||
| Median (IQR) | 0.716 (0.394–1.659) | 0.255 (0.149–0.385) | |
| Mean±s.d. | 1.853±4.258 | 0.383±0.523 | <0.001a |
| PZ-PSAD (ng ml−2) | |||
| Median (IQR) | 0.659 (0.235–2.274) | 0.093 (-0.044–0.228) | |
| Mean±s.d. | 6.053±31.264 | 0.208±0.984 | <0.001a |
| DRE (n) | |||
| Normal | 112 | 265 | |
| Positive | 124 | 28 | <0.001b |
| TRUS findings (n) | |||
| Normal | 87 | 252 | |
| Positive | 149 | 41 | <0.001b |
| mpMRI findings (n) | |||
| Normal | 57 | 215 | |
| Positive | 179 | 78 | <0.001b |
aMann-Whitney U test; bχ2 analysis. PCa: prostate cancer; IQR: interquartile range; s.d.: standard deviation; PSA: prostate-specific antigen; PSAD: prostate-specific antigen density; TZ-PSAD: transition zone prostate-specific antigen density; PZ-PSAD: peripheral zone prostate-specific antigen density; DRE: digital rectal examination; TRUS: transrectal ultrasound; mpMRI: multiparameter magnetic resonance imaging
The clinical characteristics of patients stratified according to different PSA levels are compared in Supplementary Table 1. In all, 254, 173, and 102 patients had PSA values of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, respectively. The rates of PCa detection were significantly different in men with PSA values of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1 (29.5%, 44.5%, and 82.4%, respectively; P < 0.01). The age, PZ-PSAD, PSAD, and TZ-PSAD and DRE, TRUS, and mpMRI findings of patients stratified according to the three different PSA levels were significantly different (all P < 0.01). Compared with patients with lower levels of PSA, those with higher levels of PSA were older and had higher PZ-PSAD, PSAD, and TZ-PSAD values and rates of positive findings on DRE, TRUS, and mpMRI (all P < 0.01).
Supplementary Table 1.
Clinical characteristics in men with prostate-specific antigen levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20 ng ml−1
| Group | PSA 4.0 – 10.0 ng ml−1 | PSA 10.1 – 20.0 ng ml−1 | PSA >20.0 ng ml−1 | P |
|---|---|---|---|---|
| Case number, n (%) | 254 (48.0) | 173 (32.7) | 102 (19.3) | |
| Positive detection rate | 75 (29.5%) | 77 (44.5%) | 84 (82.4%) | <0.001a |
| Age (year) | ||||
| Median (IQR) | 67 (62–72) | 68 (63.5–72) | 73.5 (65–79) | |
| Mean±s.d. | 67.37±7.01 | 68.40±6.79 | 72.72±8.00 | <0.001b |
| PSA value (ng ml−1) | 6.70±1.60 | 14.02±2.86 | 121.28±225.74 | <0.001b |
| PV value (ml) | 55.99±26.92 | 63.25±36.25 | 60.87±36.36 | 0.063b |
| PSAD value (ng ml−2) | 0.150±0.092 | 0.298±0.192 | 2.477±4.655 | <0.001b |
| TZ-PSAD value (ng ml−2) | 0.309±0.226 | 0.571±0.458 | 3.706±6.063 | <0.001b |
| PZ-PSAD value (ng ml−2) | 0.091±0.367 | 0.455±0.548 | 13.607±46.633 | <0.001b |
| DRE (+) | 50 | 41 | 61 | <0.001a |
| TRUS findings (+) | 69 | 53 | 68 | <0.001a |
| mpMRI (+) | 100 | 86 | 71 | <0.001a |
aχ2 analysis; bANOVA. PCa: prostate cancer; IQR: interquartile range; s.d.: standard deviation; PSA: prostate-specific antigen; PSAD: prostate-specific antigen density; TZ-PSAD: transition zone prostate-specific antigen density; PZ-PSAD: peripheral zone prostate-specific antigen density; DRE: digital rectal examination; TRUS: transrectal ultrasound; mpMRI: multiparameter magnetic resonance imaging; ANOVA: analysis of variance
The clinical tumor characteristics, such as the Gleason score, clinical tumor stage, number of positive cores, and the DRE and TRUS findings in PCa patients with different PSA levels were significantly different, as shown in Table 2 (all P < 0.05). The clinical characteristics of the 100 patients with BPH are shown in Supplementary Table 2. The average PSA density of these standardized BPH patients was 0.182 ± 0.177 ng ml−2 (N-PSAD).
Table 2.
Clinical tumor characteristics in men with prostate-specific antigen levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20 ng ml−1
| Group | PSA 4.0–10.0 ng ml−1 | PSA 10.1–20.0 ng ml−1 | PSA >20.0 ng ml−1 | P |
|---|---|---|---|---|
| Case, n (%) | 75 (29.5) | 77 (44.5) | 84 (82.4) | |
| Gleason score, n (%) | ||||
| ≤6 | 35 (46.7) | 30 (39.0) | 19 (22.6) | <0.001a |
| 7 | 36 (48.0) | 32 (41.6) | 31 (36.9) | |
| ≥8 | 4 (5.3) | 15 (19.5) | 34 (40.5) | |
| Clinical tumor stage, n (%) | ||||
| T1c–T2a | 37 (49.3) | 23 (29.9) | 16 (19.0) | <0.001a |
| T2b | 24 (32.0) | 30 (39.0) | 38 (45.2) | |
| T2c–T4 | 14 (18.7) | 24 (31.2) | 30 (35.7) | |
| Number of positive cores, mean±s.d. | 4.32±2.78 | 5.51±3.39 | 7.06±3.30 | <0.001b |
| DRE (+), n (%) | 31 (41.3) | 33 (42.9) | 60 (71.4) | <0.001c |
| TRUS findings (+), n (%) | 40 (53.3) | 44 (57.1) | 65 (77.4) | 0.003c |
| mpMRI (+), n (%) | 52 (69.3) | 57 (74.0) | 70 (83.3) | 0.108c |
aKruskal-Wallis test; bANOVA; cχ2 analysis. PSA: prostate-specific antigen; DRE: digital rectal examination; TRUS: transrectal ultrasound; mpMRI: multiparameter magnetic resonance imaging; s.d.: standard deviation; ANOVA: analysis of variance; DRE (+): touch hard or suspicious nodules in the prostate; TRUS findings (+): find suspicious nodules in the image; mpMRI (+): with a PIRADS score > 3
Supplementary Table 2.
Clinical characteristics in 100 patients with benign prostate hyperplasia who were selected to obtain the average prostate-specific antigen density in the nonprostate cancer cohort
| Parameter | BPH |
|---|---|
| Age (year) | |
| Median (IQR) | 65 (61–73.75) |
| Mean±s.d. | 66.74±8.30 |
| PSA value (ng ml−1) | |
| Median (IQR) | 6.15 (2.68–13.89) |
| Mean±s.d. | 9.08±8.25 |
| Prostate volume (ml) | |
| Median (IQR) | 50.30 (36.29–71.99) |
| Mean±s.d. | 57.91±33.95 |
| PZ-PSAD (ng ml−2) | |
| Median (IQR) | 0.137 (0.058–0.210) |
| Mean±s.d. | 0.182±0.177 |
BPH: benign prostate hyperplasia; PSA: prostate-specific antigen; N-PSAD: prostate-specific antigen density in the non-PCa cohort; PZ-PSAD: peripheral zone prostate-specific antigen density; s.d.: standard deviation; IQR: interquartile range
The ROC analyses of parameters for the detection of PCa are shown in Supplementary Table 3 and Figure 1. Clearly, PZ-PSAD had the largest AUC and the greatest accuracy for discriminating PCa from non-PCa, followed by TZ-PSAD, PSAD, and PSA. In men with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, the ideal PZ-PSAD cutoff values for predicting PCa were 0.105 ng ml−2, 0.436 ng ml−2, and 1.803 ng ml−2, respectively. Among the PCa patients, 197 patients had a Gleason score ≥7 or a pathological grade ≥T2b, and we designated these patients to have clinically significant PCa. When a sensitivity of at least 90% is required, in men with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, the ideal PZ-PSAD cutoff values for predicting clinically significant PCa were 0.019 ng ml−2, 0.297 ng ml−2, and 1.180 ng ml−2, respectively (Table 3).
Supplementary Table 3.
Sensitivity, specificity, and area under the receiver operating characteristic curve of peripheral zone prostate-specific antigen density, prostate-specific antigen, prostate-specific antigen density, and transition zone prostate-specific antigen density for predicting prostate cancer
| PSA (ng ml−1) | Variable | Best cutoff | Sensitivity (%) | Specificity (%) | AUC-ROC |
|---|---|---|---|---|---|
| 4.0–10.0 | PZ-PSAD | 0.105 | 70.7 | 72.1 | 0.770 |
| PSA | 6.455 | 68.0 | 53.1 | 0.592 | |
| PSAD | 0.142 | 69.3 | 69.3 | 0.730 | |
| TZ-PSAD | 0.289 | 74.7 | 73.2 | 0.766 | |
| 10.1–20.0 | PZ-PSAD | 0.436 | 68.8 | 86.5 | 0.823 |
| PSA | 14.05 | 58.5 | 67.7 | 0.621 | |
| PSAD | 0.298 | 67.5 | 84.4 | 0.799 | |
| TZ-PSAD | 0.844 | 84.4 | 63.5 | 0.769 | |
| 4.0–20.0 | PZ-PSAD | 0.258 | 59.2 | 83.3 | 0.785 |
| PSA | 7.895 | 67.1 | 52.0 | 0.630 | |
| PSAD | 0.208 | 61.8 | 82.2 | 0.762 | |
| TZ-PSAD | 0.302 | 81.6 | 66.2 | 0.775 | |
| >20.0 | PZ-PSAD | 1.803 | 84.5 | 77.8 | 0.870 |
| PSA | 39.21 | 67.9 | 77.8 | 0.750 | |
| PSAD | 0.801 | 76.2 | 77.8 | 0.797 | |
| TZ-PSAD | 0.685 | 90.5 | 61.1 | 0.728 |
PSA: prostate-specific antigen; PSAD: prostate-specific antigen density; TZ-PSAD: transition zone prostate-specific antigen density; PZ-PSAD: peripheral zone prostate-specific antigen density; ROC: receiver operating characteristic; AUC-ROC: area under the ROC curve-ROC
Figure 1.
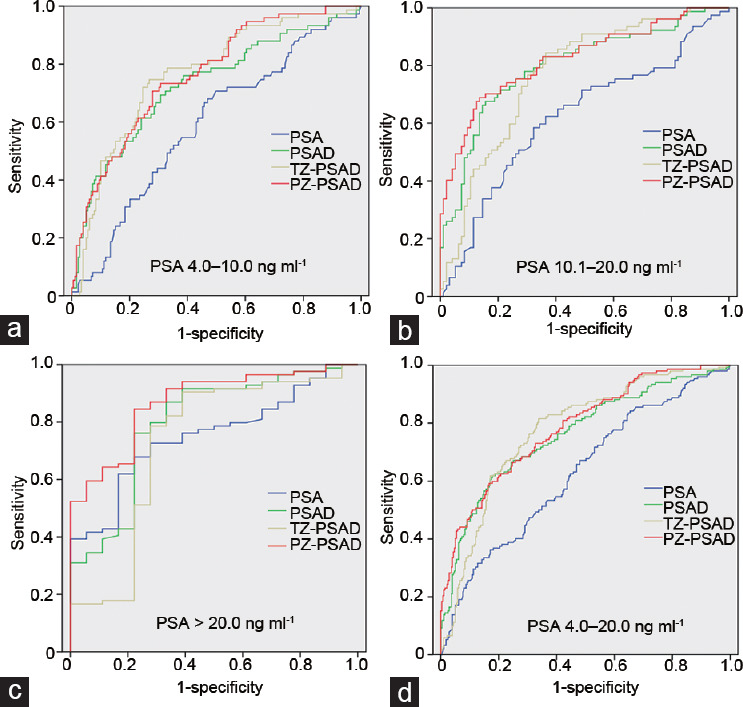
Receiver operating characteristic curve analyses of PSA, PSAD, TZ-PSAD, and PZ-PSAD in detecting prostate cancer in patients with PSA levels of (a) 4.0–10.0 ng ml−1, (b) 10.1–20.0 ng ml−1, (c) >20.0 ng ml−1, and (d) 4.0–20.0 ng ml−1. PSA: prostate-specific antigen; PSAD: PSA density; TZ-PSAD: transition zone PSAD; PZ-PSAD: peripheral zone PSAD.
Table 3.
The optimal cutoff value of peripheral zone prostate-specific antigen density, prostate-specific antigen, prostate-specific antigen density, and transition zone prostate-specific antigen density for predicting clinically significant prostate cancer
| PSA (ng ml−1) | Variable | Best cutoff | Sensitivity (%) | Specificity (%) | AUC-ROC |
|---|---|---|---|---|---|
| 4.0–10.0 | PZ-PSAD | 0.019 | 92.6 | 43.5 | 0.403 |
| PSA | 4.895 | 90.7 | 16.0 | 0.145 | |
| PSAD | 0.095 | 94.4 | 34.0 | 0.321 | |
| TZ-PSAD | 0.195 | 92.6 | 44.0 | 0.407 | |
| 10.1–20.0 | PZ-PSAD | 0.297 | 90.6 | 71.6 | 0.649 |
| PSA | 10.885 | 90.6 | 18.3 | 0.166 | |
| PSAD | 0.225 | 90.6 | 71.6 | 0.649 | |
| TZ-PSAD | 0.335 | 92.2 | 58.7 | 0.541 | |
| >20.0 | PZ-PSAD | 1.180 | 92.3 | 54.2 | 0.500 |
| PSA | 25.00 | 91.0 | 25.0 | 0.228 | |
| PSAD | 0.470 | 91.0 | 54.2 | 0.493 | |
| TZ-PSAD | 0.720 | 91.0 | 54.2 | 0.493 |
PSA: prostate-specific antigen; PSAD: prostate-specific antigen density; TZ-PSAD: transition zone prostate-specific antigen density; PZ-PSAD: peripheral zone prostate-specific antigen density; ROC: receiver operating characteristic; AUC-ROC: area under the ROC curve
We further compared the diagnostic efficiency between PSA and PZ-PSAD in the group with PSA levels that ranged from 4.0 ng ml−1 to 20.0 ng ml−1. The optimal cutoff values of PSA and PZ-PSAD to predict PCa were 7.895 ng ml−1 and 0.258 ng ml−2, respectively. Compared with PSA, PZ-PSAD could increase the positive rate of biopsy from 43.5% to 65.7%, and help 68.9% (91/132) of the patients avoid unnecessary prostate biopsy.
We evaluated the efficacy of PZ-PSAD as a diagnostic aid in patients with inaccurate TRUS and mpMRI results (Figure 2). In 427 patients with PSA levels that ranged from 4.0 ng ml−1 to 20.0 ng ml−1, 77 patients in the non-PCa group had positive mpMRI findings (Figure 2b). Among them, 66 (85.7%) patients with PZ-PSAD values <0.258 ng ml−2 (diagnostic cutoff value) could avoid unnecessary biopsies by screening of PZ-PSAD. Similarly, 43 PCa patients had negative mpMRI findings, of which 22 (51.2%) with PZ-PSAD values ≥0.258 ng ml−2 could avoid a missed diagnosis by screening of PZ-PSAD. On TRUS examination (Figure 2a), it was found that PZ-PSAD could help 32 (84.2%) patients avoid unnecessary biopsies and 39 (57.4%) patients avoid a missed diagnosis.
Figure 2.
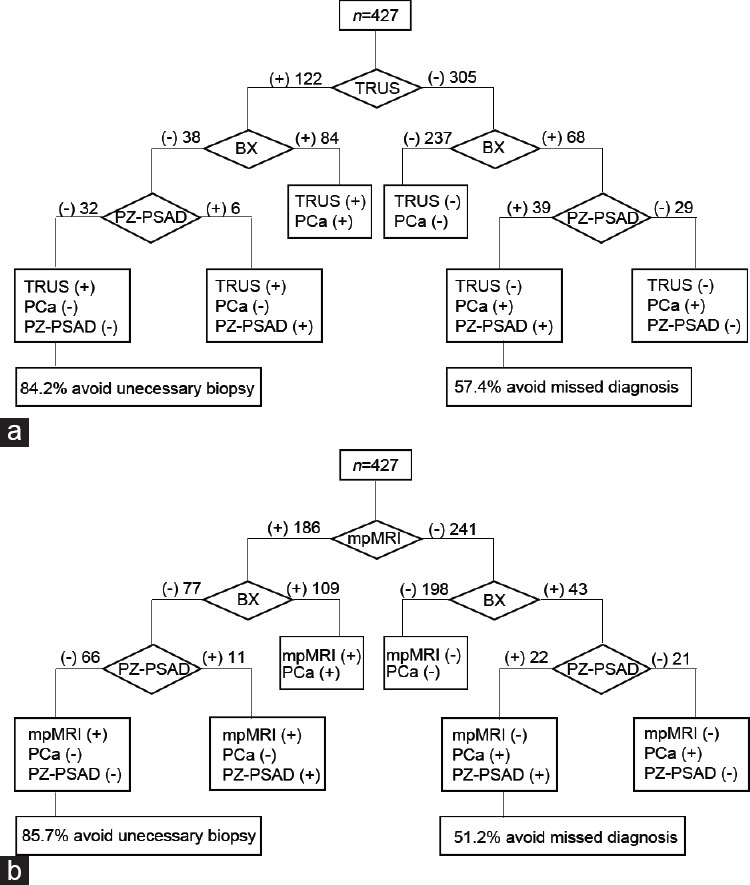
Combined with PZ-PSAD, (a) TRUS and (b) mpMRI can be more efficient in PCa diagnosis and help patients avoid unnecessary prostate biopsy and missed diagnosis. TRUS: transrectal ultrasound; mpMRI: multiparameter magnetic resonance imaging; PZ-PSAD: peripheral zone prostate-specific antigen density; PCa: prostate cancer; Bx: transrectal systematic 12-core prostate biopsy; (−): negative; (+): positive; PZ-PSAD (−): PZ-PSAD <0.258 ng ml−2; PZ-PSAD (+): PZ-PSAD ≥0.258 ng ml−2.
We further evaluated the efficacy of PZ-PSAD to diagnose PCa when TRUS and mpMRI findings were ambiguous to diagnose PCa (Table 4). Among 235 patients with negative mpMRI and TRUS findings, 51 (21.7%) patients were histologically diagnosed with PCa. The optimal cutoff value of PZ-PSAD obtained by ROC curve analysis was used to screen patients. Only 31.9% (75/235) of the patients with PZ-PSAD (+) required a biopsy and 80.4% (41/51) of the PCa patients could be detected. Among the 10 PCa patients with PZ-PSAD (−), three patients had a Gleason score of 7 and seven patients had a Gleason score of 6; all patients were medium- and low-risk PCa patients. PZ-PSAD could increase the positive rate of biopsy from 21.7% to 54.7% and help 63.8% (150/235) of the patients avoid unnecessary prostate biopsy.
Table 4.
The efficacy of peripheral zone prostate-specific antigen density to diagnose prostate cancer in patients with negative multiparameter magnetic resonance imaging and transrectal ultrasound results (prostate imaging reporting and data system ≤3)
| Group | PSA 4.0–10.0 ng ml−1 | PSA 10.1–20.0 ng ml−1 | PSA >20.0 ng ml−1 | Total |
|---|---|---|---|---|
| TRUS/MRI (−), n | 135 | 78 | 22 | 235 |
| Pathology (+), n (%) | 22 (16.3) | 18 (23.1) | 11 (50.0) | 51 (21.7) |
| PZ-PSAD cutoff value (ng ml−2) | 0.105 | 0.436 | 1.803 | |
| PZ-PSAD (+), n (%) | 45 (33.3) | 19 (24.4) | 11 (50.0) | 75 (31.9) |
| PZ-PSAD (+) pathology (+), n | 17 | 14 | 10 | 41 |
PSA: prostate-specific antigen; PZ-PSAD: peripheral zone prostate-specific antigen density; PCa: prostate cancer; TRUS: transrectal ultrasound; mpMRI: multiparameter magnetic resonance imaging; PIRADS: Prostate Imaging Reporting and Data System; TRUS/MRI (-): without suspicious nodules or a PIRADS score ≤ 3; pathology (+): prostate cancer; PZ-PSAD (+): PZ-PSAD > cut-off value
DISCUSSION
This project was undertaken to propose a “rigorous,” “efficient,” and “practical” index to diagnose PCa. We designed a “rigorous” formula for PZ-PSAD by combining the PSA value with TZV, PZV, and the baseline N-PSAD. Our findings indicate that PZ-PSAD is “efficient” and has a diagnostic efficacy superior to that of PSA, PSAD, and TZ-PSAD for predicting PCa. PZ-PSAD is “practical” in that we can improve the diagnostic accuracy of mpMRI and TRUS, and indicate the need for a prostate biopsy when TRUS and mpMRI findings are ambiguous to diagnose PCa (PIRADS score ≤3). Subsequently, through the ROC curve analysis of a large dataset, this study recommended individual PZ-PSAD screening criteria for men to improve the diagnostic efficiency for PCa.
As a “rigorous” parameter, PZ-PSAD is calculated according to a comprehensive formula that includes the PSA, TZV, PZV, and baseline N-PSAD. In contrast, previous volume-adjusted PSA densities, such as PSAD and TZ-PSAD, are the ratio of PSA to PV or TZV and require precise quantification. This formula divides the tPSA into two parts, with PZ and TZ each taking part. The PSA of TZ is calculated by the product of N-PSAD and TZV, and the PSA of PZ is divided by PZV to obtain PZ-PSAD. This method is concise, and the data needed are economical and easy to obtain in clinical practice. To obtain the N-PSAD, we preselected 100 standardized BPH patients from our center rather than extracting this information from a database. These BPH patients are similar in age, diet, ethnicity, and living environment to the patients with suspected PCa who were enrolled in this study, which can reduce the experimental error and heterogeneity in different populations. Subsequently, the mean PSAD of 0.18 ng ml−2 in the standardized BPH patients was defined as the N-PSAD. Bazinet et al.12 reported that the optimal cutoff value of PSAD in early prostate cancer was 0.15 ng ml−2. Yue13 reported that the value of PSAD in patients with BPH was 0.17 ng ml−2. Zhao et al.14 reported that PSAD in the negative prostate puncture group was 0.19 ng ml−2. The value of N-PSAD in this study is representative and similar to the data reported above in Asian and Western cohorts.
PZ-PSAD is “efficient” and has higher diagnostic efficiency than PSA, PSAD, and TZ-PSAD. In recent years, PSA has been the most commonly utilized tool for the diagnosis of PCa. But in the PSA “gray zone” (4.0–10.0 ng ml−1), the diagnostic specificity of PSA is relatively low and without effective threshold values.15 So the Chinese Urological Association recommends that men with PSA levels >10 ng ml−1 undergo prostate biopsy.16 The American Urological Association (AUA) guidelines recommend not merely using the PSA threshold to indicate the need for a prostate biopsy, and that multiple factors should be considered, including PSA density, free PSA/total PSA, molecular subtype, PSA kinetics, patient age, PSA doubling speed, and family history.17,18,19 PSAD and TZ-PSAD have been reported to improve the prostate cancer detection rate with PSA levels of 2.5–20.0 ng ml−1 and 4.0–20.0 ng ml−1, respectively.20,21 Our study attempted to enhance the predictive performance of PSA utilizing capacity-adjusted parameters and defined a new parameter, PZ-PSAD. Clearly, PZ-PSAD had the largest AUC and total efficiency for discriminating PCa, followed by TZ-PSAD, PSAD, and PSA. PZ-PSAD is efficient for PCa screening and has high specificity to identify confounding factors that affect PSA values, such as BPH and prostatitis.
PZ-PSAD is “practical” to aid mpMRI and TRUS in predicting PCa and indicating the need for a prostate biopsy in clinical practice (Figure 2 and Table 4). The results show that in 427 patients with PSA levels of 4.0–20.0 ng ml−1, PZ-PSAD can amend the diagnosis in patients with inaccurate TRUS and mpMRI results and help more than half of the patients avoid unnecessary biopsies and missed diagnosis. Therefore, we can combine the results of TRUS and mpMRI with PZ-PSAD to assess the need for a prostate biopsy. Furthermore, in the clinical diagnosis strategy, for suspected PCa patients with elevated PSA and abnormal TRUS and mpMRI findings (PIRADS >3), prostate biopsy is recommended; if the TRUS and mpMRI results are negative with PIRADS ≤3, it is difficult to decide whether a prostate biopsy should be performed. Among suspected PCa patients with negative mpMRI and TRUS results, if patients with positive PZ-PSAD result (31.9%) are recommended for a biopsy, 80.4% of PCa patients will be detected. PZ-PSAD increased the positive rate of biopsy from 21.7% to 54.7%, and helped 150 (63.8%) patients avoid unnecessary prostate biopsy. Moreover, ten PCa patients with PZ-PSAD (−) were medium- and low-risk patients, and 7 of them had a Gleason score ≤6. This reveals that PZ-PSAD helps to screen clinically significant PCa effectively when TRUS and mpMRI findings were negative or ambiguous to diagnose PCa.
When using PZ-PSAD for PCa diagnosis, stratified screening for patients with PSA values of different levels is more targeted and efficient. In the current study, we discovered that patients with different PSA levels have different detection rates of PCa and tumor characteristics, as shown in Table 2. Moreover, the detection rate of PCa in Chinese men is much lower than that in other reports.22,23 We added groups with PSA levels of 10–20 ng ml−1 and >20 ng ml−1 to supplement the deficiency of PSA “gray area” coverage and conducted a stratified analysis based on PSA levels. In men with PSA levels that ranged from 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, the ideal PZ-PSAD cutoff values for predicting PCa were 0.105 ng ml−2, 0.436 ng ml−2, and 1.803 ng ml−2, respectively. In clinical practice, there is more demand for the screening of clinically significant PCa (Gleason ≥7 or pathological grade ≥T2b) and, thus, higher sensitivity is required. When a sensitivity of at least 90% is required, in men with PSA levels of 4.0–10.0 ng ml−1, 10.1–20.0 ng ml−1, and >20.0 ng ml−1, the ideal PZ-PSAD cutoff values for predicting clinically significant PCa were 0.019 ng ml−2, 0.297 ng ml−2, and 1.180 ng ml−2, respectively. The development of individual screening criteria can increase the efficiency of PZ-PSAD in diagnosing PCa in more scenarios.
In clinical practice, to screen for PCa, the first examinations are PSA detection, DRE, and TRUS. For cases of suspected PCa after the above-mentioned examinations, mpMRI is performed because the cost of MRI is higher than that of TRUS. In this study, the PV and TZV are measured by mpMRI to calculate PZ-PSAD because of its accuracy. It will be more practical to use TRUS for PZ-PSAD calculation in clinical practice. Therefore, this study compared the PZ-PSAD data measured by mpMRI and TRUS. It revealed that the PZ-PSAD data measured by mpMRI and TRUS were not statistically different (P = 0.172). This suggests that the PV and TZV measured by TRUS can be used to calculate PZ-PSAD in clinical applications, which improves the convenience and popularity of this index.
In order to advance the application and generalization of these experimental findings, some problems require further investigation. The clinical data were obtained from a single hospital, which leads to a selection bias. In addition, different cores, biopsy schemes, and operating techniques may lead to different detection rates of PCa, and prostate systematic multipoint biopsy may also fail to detect a part of the prostate cancer.24,25,26 To confirm our findings, larger prospective randomized studies are needed.
CONCLUSION
In the diagnosis of PCa, PZ-PSAD, PSA, PSAD, and TZ-PSAD have certain diagnostic value for patients with PSA values of different levels, but the accuracy of PZ-PSAD to predict PCa is the highest, which means a lower missed diagnosis rate and more patients can avoid unnecessary biopsy. PZ-PSAD can amend the diagnosis in patients with inaccurate TRUS and mpMRI results, and indicate the need for a prostate biopsy when TRUS and mpMRI findings were negative or ambiguous to diagnose PCa.
AUTHOR CONTRIBUTIONS
CW and YYW conceived the study, collected data, performed the statistical analysis, and drafted the manuscript. SYW, JXD, and MD helped to collect data and performed the statistical analysis. YR, XHW, YFJ, BMH, and SJX participated in design and coordination of the study. CYJ and FJZ conceived the study, participated in its design and coordination, and helped to draft the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing interests.
Measurement of the prostate and transition zone volumes. (a) Measurement of the transverse diameter and anteroposterior diameter on horizontal plane. (b) Measurement of the superoinferior diameter on sagittal plane. A: transverse diameter of the transition zone; B: anteroposterior diameter of the transition zone; C: transverse diameter of the entire prostate; D: anteroposterior diameter of the entire prostate; E: superoinferior diameter of the transition zone; F: superoinferior diameter of the entire prostate.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No. 81772746; No. 81870516) and Natural Science Foundation of Xinjiang Province (2019D01C091).
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
REFERENCES
- 1.Xia SJ, Cui D, Jiang Q. An overview of prostate diseases and their characteristics specific to Asian men. Asian J Androl. 2012;14:458–64. doi: 10.1038/aja.2010.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 3.Rebecca S, Jiemin GA, Zhao HZ. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. [Google Scholar]
- 4.Zong Y, Goldstein AS. Adaptation or selection--mechanisms of castration-resistant prostate cancer. Nat Rev Urol. 2013;10:90–8. doi: 10.1038/nrurol.2012.237. [DOI] [PubMed] [Google Scholar]
- 5.Tosoian J, Loeb S. PSA and beyond: the past, present, and future of investigative biomarkers for prostate cancer. ScientificWorldJournal. 2010;10:1919–31. doi: 10.1100/tsw.2010.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avery KN, Metcalfe C, Vedhara K, Lane JA, Davis M, et al. Predictors of attendance for prostate-specific antigen screening tests and prostate biopsy. Eur Urol. 2012;62:649–55. doi: 10.1016/j.eururo.2011.12.059. [DOI] [PubMed] [Google Scholar]
- 7.Stefano DL, Passera R, Fiori C, Bollito E, Cappia S, et al. Prostate health index and prostate cancer gene 3 score but not percent-free prostate specific antigen have a predictive role in differentiating histological prostatitis from PCa and other nonneoplastic lesions (BPH and HG-PIN) at repeat biopsy. Urol Oncol. 2015;33:424e17–23. doi: 10.1016/j.urolonc.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 8.Hermie I, Van Besien J, De Visschere P, Lumen N, Decaestecker K. Which clinical and radiological characteristics can predict clinically significant prostate cancer in PI-RADS 3 lesions? A retrospective study in a high-volume academic center. Eur J Radiol. 2019;114:92–8. doi: 10.1016/j.ejrad.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 9.Benson MC, Whang IS, Pantuck A, Ring K, Kaplan SA, et al. Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol. 1992;147:815–6. doi: 10.1016/s0022-5347(17)37393-7. [DOI] [PubMed] [Google Scholar]
- 10.Kalish J, Cooner WH, Graham SD., Jr Serum PSA adjusted for volume of transition zone (PSAT) is more accurate than PSA adjusted for total gland volume (PSAD) in detecting adenocarcinoma of the prostate. Urology. 1994;43:601–6. doi: 10.1016/0090-4295(94)90170-8. [DOI] [PubMed] [Google Scholar]
- 11.Xia SJ. Two-micron (thulium) laser resection of the prostate-tangerine technique: a new method for BPH treatment. Asian J Androl. 2009;11:277–81. doi: 10.1038/aja.2009.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bazinet M, Meshref AW, Trudel C, Aronson S, Péloquin F, et al. Prospective evaluation of prostate-specific antigen density and systemic biopsies for early detection of prostatic carcinoma. Urology. 1994;43:44–52. doi: 10.1016/s0090-4295(94)80260-2. [DOI] [PubMed] [Google Scholar]
- 13.Yue LX. Evaluating hypoechoic lesion in prostate and PSAD for the diagnosis of prostate cancer. J Clin Ultrasound. 1999;1:207–9. [Google Scholar]
- 14.Zhao YR, Xu Y, Zhang DJ, Chang JW, Zhang SM, et al. The predictive value of serum prostate specific antigen, prostate specific antigen density and prostate specific antigen transition zone density in prostate biopsy. Chin J Urol. 2005;26:622–5. Article in Chinese. [Google Scholar]
- 15.Kitagawa Y, Ueno S, Izumi K, Kadono Y, Konaka H, et al. Cumulative probability of prostate cancer detection in biopsy according to free/total PSA ratio in men with total PSA levels of 21–100 ng ml−1 at population screening. J Cancer Res Clin Oncol. 2014;140:53–9. doi: 10.1007/s00432-013-1543-9. [DOI] [PubMed] [Google Scholar]
- 16.Chinese guidelines for diagnosis and treatment of prostate cancer 2018 (English version) Chin J Cancer Res. 2019;31:67–83. doi: 10.21147/j.issn.1000-9604.2019.01.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol. 2017;71:618–29. doi: 10.1016/j.eururo.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Williams SB, Salami S, Regan MM, Ankerst DP, Wei JT, et al. Selective detection of histologically aggressive prostate cancer: an Early Detection Research Network Prediction model to reduce unnecessary prostate biopsies with validation in the Prostate Cancer Prevention Trial. Cancer. 2012;118:2651–8. doi: 10.1002/cncr.26396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Labbé DP, Sweeney CJ, Brown M, Galbo P, Rosario S, et al. TOP2A and EZH2 provide early detection of an aggressive prostate cancer subgroup. Clin Cancer Res. 2017;23:7072–83. doi: 10.1158/1078-0432.CCR-17-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin YR, Wei XH, Uhlman M, Lin XT, Wu SF, et al. PSA density improves the rate of prostate cancer detection in Chinese men with a PSA between 25–100 ng ml-1 and 101–200 ng ml-1: a multicenter study. Asian J Androl. 2015;17:503–7. doi: 10.4103/1008-682X.142129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang P, Du W, Xie KJ, Deng XR, Fu JG, et al. Transition zone PSA density improves the prostate cancer detection rate both in PSA 40–100 and 101–200 ng ml−1 in Chinese men. Urol Oncol. 2013;31:744–8. doi: 10.1016/j.urolonc.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 22.Chen R, Sjoberg DD, Huang YR, Xie LP, Zhou LQ, et al. Prostate-specific antigen and prostate cancer in Chinese men undergoing initial prostate biopsies in comparison with Western cohorts: data from the PBCG and CPCC. J Urol. 2017;197:90–6. doi: 10.1016/j.juro.2016.08.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsuda T, Saika K. Comparison of time trends in prostate cancer incidence (1973–2002) in Asia, from cancer incidence in five continents, Vols.IV–IX. Jpn J Clin Oncol. 2009;39:468–9. doi: 10.1093/jjco/hyp077. [DOI] [PubMed] [Google Scholar]
- 24.Kalish J, Cooner WH, Graham SD., Jr Serum PSA adjusted for volume of transition zone (PSAT) is more accurate than PSA adjusted for total gland volume (PSAD) in detecting adenocarcinoma of the prostate. Urology. 1994;43:601–6. doi: 10.1016/0090-4295(94)90170-8. [DOI] [PubMed] [Google Scholar]
- 25.Chun FK, Epstein JI, Ficarra V, Freedland SJ, Montironi R, et al. Optimizing performance and interpretation of prostate biopsy: a critical analysis of the literature. Eur Urol. 2010;58:851–4. doi: 10.1016/j.eururo.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 26.Jiang CY, Shen PF, Wang C, Gui HJ, Ruan Y, et al. Comparison of diagnostic efficacy between transrectal and transperineal prostate biopsy: a propensity score-matched study. Asian J Androl. 2019;21:612–7. doi: 10.4103/aja.aja_16_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Measurement of the prostate and transition zone volumes. (a) Measurement of the transverse diameter and anteroposterior diameter on horizontal plane. (b) Measurement of the superoinferior diameter on sagittal plane. A: transverse diameter of the transition zone; B: anteroposterior diameter of the transition zone; C: transverse diameter of the entire prostate; D: anteroposterior diameter of the entire prostate; E: superoinferior diameter of the transition zone; F: superoinferior diameter of the entire prostate.


