Current guidelines recommend implantable cardioverter-defibrillator (ICD) implantation for prevention of sudden death in patients with heart failure (HF) and reduced ejection fraction (EF) and EF ≤35% after at least 3 months of optimized HF therapy.1 The angiotensin receptor–neprilysin inhibitor sacubitril/valsartan induces favorable ventricular remodeling2 and improves clinical outcomes in patients with HF with reduced EF (HFrEF) compared to enalapril.3 We investigated the impact of sacubitril/valsartan initiation on ICD eligibility in patients enrolled in the PROVE-HF study (Prospective Study of Biomarkers, Symptom Improvement, and Ventricular Remodeling During Sacubitril/Valsartan Therapy for Heart Failure) (URL: http://www.clinicaltrials.gov. Unique identifier: NCT02887183).
PROVE-HF was a 52-week, multicenter, open-label, single-arm study that enrolled 794 patients with chronic HFrEF and left ventricular ejection fraction ≤40% who were then initiated and titrated on sacubitril/valsartan.2 Echocardiographic assessments were performed at baseline and 6 and 12 months and were interpreted at a core laboratory that was blinded to the sequence of echocardiograms. The protocol was approved by the institutional review board at each participating center, and all participants provided informed consent before enrollment in the study. The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results.
For this study, patients with a baseline EF >35% or for whom EF at baseline was missing were excluded (N = 133). Longitudinal change in EF was estimated using latent growth curve modeling4 and missingness was handled using maximum likelihood. Groups (improved >35% vs remained ≤35%) were determined using fitted EF values; predictors of grouping at month 12 were subsequently evaluated using multivariable logistic regression.
Mean age of the study population was 65 years and 27% were women. The geometric mean for NT-proBNP (N-terminal pro-B-type natriuretic peptide) was 889 pg/mL. Patients were generally well-treated: 76% were taking an angiotensin coverting enzyme inhibitor/angiotensin II receptor blocker before enrollment, 97% were receiving a beta blocker, and 44% were taking a mineralocorticoid receptor antagonist. Median baseline EF was 27% and mean time since HF diagnosis was 6.4 years. At baseline, 31% had an ICD alone and 15% had a cardiac resynchronization therapy defibrillator device.
Histograms of changes in EF at each time point after initiation of sacubitril/valsartan are shown (Figure). The median absolute EF change from baseline was 4.8 points (IQR, 4.5–5.1) at 6 months and 9.6 points (IQR, 9.0–10.2) at 12 months. Six months after initiation of sacubitril/valsartan, 214 of 661 patients (32%) who were ICD-eligible at baseline had improved EF to >35%. By 12 months, this number increased to 407 of 661 (62%). A sensitivity analysis excluding patients with an implanted device at baseline produced similar findings, with 138 of 356 (39%) showing improvements in EF to >35% by 6 months, and 266 of 256 (75%) showing this level of improvement at 12 months. Significant baseline predictors of improving EF to >35% during follow-up included lower NT-proBNP, shorter duration of HF, higher baseline EF, and non-Hispanic White race (vs. non-Hispanic Black race). There were 23 deaths during follow-up: 8 in the group with improved EF and 15 in the group that did not improve EF. Five of 23 deaths were sudden, all occurring in the group with improved EF.
Figure.
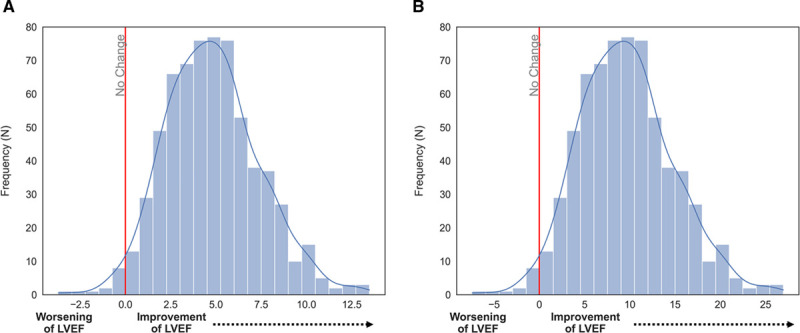
Absolute changes in ejection fraction over time. A, At month 6 and month 12 (B). LVEF indicates left ventricular ejection fraction.
The primary finding of the present study was that among a cohort of patients with HFrEF who met primary prevention ICD eligibility criteria at baseline, 32% improved their EF to >35% by 6 months and 62% to >35% by 12 months after initiation of sacubitril/valsartan therapy. These improvements occurred despite excellent background medical therapy, and were consistent whether or not patients with implanted devices at baseline were excluded. These findings have potential clinical implications for the care of patients with HFrEF: (1) in patients without ICD at the time of sacubitril/valsartan initiation, a substantial proportion of patients may have sufficient favorable ventricular remodeling to no longer qualify for primary prevention ICD therapy; and (2) the time course of favorable improvements in left ventricular EF may continue for at least 12 months. Although there is a potential concern that sudden death could still occur during this window of reassessment for improvements in EF, the risk of sudden death in HFrEF patients treated with sacubitril/valsartan is low (≈2% within 6 months in the PARADIGM trial [Prospective Comparison of ARNI with ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure])5 and <1% at 1 year (5 of 661) in the present study.
Our study has important limitations. Our analysis focused on the use of ICDs for primary prevention of sudden death in patients with HFrEF, and considerations may differ for secondary prevention or for patients with recent myocardial infarction. PROVE-HF was a single-arm study without a concurrent control arm. Although our study was designed to mirror real-world clinical use, the achieved doses of sacubitril/valsartan may be higher than in routine practice. These findings could be confirmed prospectively in appropriately designed clinical trials.
Sources of Funding
The PROVE-HF study (Prospective Study of Biomarkers, Symptom Improvement, and Ventricular Remodeling During Sacubitril/Valsartan Therapy for Heart Failure) was funded by Novartis Pharmaceuticals.
Disclosures
Dr Felker has received research grants from the National Heart, Lung, and Blood Institute, American Heart Association, Amgen, Bayer Merck, Cytokinetics, and Myokardia; has acted as a consultant to Novartis, Amgen, Bristol Myers Squibb, Cytokinetics, Medtronic, Cardionomic, Innolife, Boehringer-Ingelheim, Abbott, Eidos Therapeutics, Reprieve, and Sequana; and has served on clinical end point committees/data safety monitoring boards for Amgen, Merck, Medtronic, EBR Systems, V-Wave, LivaNova, and Rocket Pharma. Dr Butler has acted as a consultant to Abbott, Adrenomed, Amgen, Applied Therapeutics, Array, AstraZeneca, Bayer, Boehringer Ingelheim, CVRx, G3 Pharma, Impulse Dynamics, Innolife, Janssen, LivaNova, Luitpold, Medtronic, Merck, Novartis, NovoNordisk, Relypsa, Sequana Medical, V-Wave Limited, and Vifor; and served on speaker’s bureaus for Novartis, Boehringer Ingelheim–Lilly, AstraZeneca, and Janssen. Dr Ibrahim has received honoraria from Novartis and Roche. Dr Pina reports honoraria from Relypsa/Vifor, Novartis, and AstraZeneca. Dr Maisel has received consulting income from Abbott Vascular, Ortho Clinical Diagnostics, and Novartis. Drs Ward and Williamson are employees of Novartis Pharmaceuticals. Dr Solomon has received research grants from Alnylam, Amgen, AstraZeneca, Bellerophon, Bayer, Bristol Myers Squibb, Celladon, Cytokinetics, Eidos, Gilead, GlaxoSmithKline, Ionis, Lilly, Lone Star Heart, Mesoblast, MyoKardia, National Institutes of Health/National Heart, Lung, and Blood Institute, Neurotronik, Novartis, Respicardia, Sanofi Pasteur, Theracos, and has consulted for Abbott, Akros, Alnylam, Amgen, Arena, AstraZeneca, Bayer, Bristol Myers Squibb, Cardior, Cardurion, Corvia, Cytokinetics, Daiichi-Sankyo, Gilead, GlaxoSmithKline, Ironwood, Lilly, Merck, Myokardia, Novartis, Roche, Takeda, Theracos, Quantum Genetics, Cardurion, AoBiome, Janssen, Cardiac Dimensions, Tenaya, Sanofi-Pasteur, Dinaqor, Tremeau, CellProThera, and Moderna. Dr Januzzi is a trustee of the American College of Cardiology; has received grant support from Novartis Pharmaceuticals, Applied Therapeutics, Innolife, and Abbott Diagnostics; has received consulting income from Abbott Diagnostics, Janssen, Novartis, and Roche Diagnostics; and participates in clinical end point committees/data safety monitoring boards for Abbott, AbbVie, Amgen, Bayer, and Takeda.The other authors report no disclosures.
Footnotes
The podcast and transcript are available as a Data Supplement at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.121.054034.
For Sources of Funding and Disclosures, see page 181.
Contributor Information
Javed Butler, Email: jbutler4@umc.edu.
Nasiren E. Ibrahim, Email: drnasrien@gmail.com.
Ileana L. Piña, Email: ilppina@aol.com.
Alan Maisel, Email: asmaisel@gmail.com.
Devavrat Bapat, Email: DBAPAT@mgh.harvard.edu.
Alexander Camacho, Email: ACAMACHO2@mgh.harvard.edu.
Jonathan H. Ward, Email: jon.ward@novartis.com.
Kristin M. Williamson, Email: Kristin.williamson@novartis.com.
Scott D. Solomon, Email: ssolomon@rics.bwh.harvard.edu.
James L. Januzzi, Email: JJANUZZI@PARTNERS.ORG.
References
- 1.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–327. doi 10.1161/CIR.0b013e31829e8776 [DOI] [PubMed] [Google Scholar]
- 2.Januzzi JL, Jr., Prescott MF, Butler J, Felker GM, Maisel AS, McCague K, Camacho A, Pina IL, Rocha RA, Shah AM, et al. ; PROVE-Hf Investigators. Association of change in N-terminal pro-B-type natriuretic peptide following initiation of sacubitril-valsartan treatment with cardiac structure and function in patients with heart failure with reduced ejection fraction. JAMA. 2019;322:1085–1095. doi: 10.1001/jama.2019.12821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, et al. ; PARADIGM-HF Investigators and Committees. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004. doi: 10.1056/NEJMoa1409077 [DOI] [PubMed] [Google Scholar]
- 4.Felt JM, Depaoli S, Tiemensma J. Latent growth curve models for biomarkers of the stress response. Front Neurosci. 2017;11:315. doi: 10.3389/fnins.2017.00315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Desai AS, McMurray JJ, Packer M, Swedberg K, Rouleau JL, Chen F, Gong J, Rizkala AR, Brahimi A, Claggett B, et al. Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients. Eur Heart J. 2015;36:1990–1997. doi: 10.1093/eurheartj/ehv186 [DOI] [PubMed] [Google Scholar]


