Supplemental Digital Content is available in the text.
Key Words: transphyseal screw, guided growth, hemiepiphysiodesis, femoral angular deformity
Background:
We modified the original technique for percutaneous transphyseal screw which was described in 1998 by Metaizeau and colleagues for distal femoral coronal angular deformity correction; the modification is related to the screw direction, whereas the screw is administered in a retrograde pattern, starting from the epiphysis and directed toward the metaphysis. This technique opposes the original technique that was started with a metaphyseal entry point which aimed toward the epiphysis. This study evaluates the efficacy of the newly suggested surgical technique regarding the rate of correction and growth resumption after screw removal.
Methods:
This prospective study looked at 40 patients (65 distal femoral physes), who underwent a percutaneous retrograde transphyseal guided growth screw procedure, from October 2017 to September 2019. All the patients included had distal femoral coronal angular deformities; 52 in valgus and 13 in varus deformities. The study included 17 females with an average age of 11.75 (range: 8.4 to 14.5 y) for 29 femurs and 23 males with an average age of 13.75 (range: 11.75 to 15.6 y) for 36 femurs. The mechanical lateral distal femoral angle was measured initially, and then again was measured after reaching the desired corrected orientation. The patients were then followed up after the screw removal and followed up to maturity, if the physis had continued to grow postcorrection. The degree of correction per month was calculated, and the consequence of screw removal was detected. Follow-up average time was 12.6 months (range: 30 to 6 mo).
Results:
The average correction in the distal femur was 1.3 degrees per month (range: 0.5 to 1.857 degrees/mo). In all of the 65 segments (61 femurs had significant growth remaining and 4 femurs had reached skeletal maturity with suboptimal mechanical lateral distal femoral angle correction), the screws were removed at the time of angular correction. Rebound growth was observed in 15 physes with an average of 1.8 degrees (range: 2 to 3 degrees); they were stable in 42 physes and progressed in 4 physes with an average of 1.6 degrees (range: 1 to 2 degrees). Complications were minor and related to entrapment of soft tissue under the screw washer.
Conclusion:
Percutaneous retrograde transphyseal guided growth screw for distal femur coronal angular deformity is a minimally invasive procedure, with a statistically significant correction rate when compared with the original transphyseal screw technique. The new technique has proven to have growth resumption after screw removal with minimal complication risk.
Level of Evidence:
Level III—prospective observational study.
Coronal angular deformities in the skeletally immature bone are a common problem in adolescents.1 Early detection and adequate intervention is a key in achieving optimal deformity correction. Guided growth using percutaneous transphyseal screw was first described in 1998 by Metaizeau et al,2 and became popular in treating knee angular deformities in the premature bone stage. A small number of studies evaluated the rate of correction for distal femoral deformity using a single percutaneous transphyseal screw with a metaphyseal entry that approaches the epiphysis. This rate of correction had an average of 0.92 degrees per month,3 which might not be a sufficient rate to achieve full correction especially in a significant degree of angular deformities or when the patients are close to skeletal maturity.
In this study, the authors modified the original transphyseal screw technique to reverse the direction of the screw from the initial technique. The authors hypothesized that the modification would therefore start from the epiphysis and move toward the metaphysis. This would provide a better tethering effect for the screw function and subsequent temporary inhibition of the regional physeal growth for the selected region.4,5 That means if the mechanical tethering effect of the screw was improved, the rate of deformity correction would improve as well, albeit achieving full deformity correction before physeal closure.
This study used a new modified screw technique in the adolescent age group in both females and males. The aim of this study was to present the newly guided growth modulation technique with evaluation to correction rate. It also aimed to investigate reversibility of the physeal growth after the removal of the retrograde screw.
METHODS
The study was conducted following approval of the regional ethics committee (reference number 2017/908), and included 40 patients (65 femoral physes), who underwent a percutaneous retrograde transphyseal guided growth screw surgical correction from October 2017 to September 2019 for distal femoral angular deformities (52 femurs in valgus and 13 femurs in varus deformities). Written informed consent was obtained from all the patients’ legal guardians. The study included 17 females with an average age of 11.75 (range: 8.4 to 14.5 y) for 29 femurs and 23 males with an average age of 13.75 (range: 11.75 to 15.6 y) for 36 femurs. All affected femurs were measured for the mechanical lateral distal femoral angle (mLDFA) as described by Paley6; <85 degrees was considered a valgus deformity and >90 degrees was considered a varus deformity. Measurements were recorded during presurgical and postsurgical intervention. Patients’ mean follow-up was 12.6 months (range: 30 to 6 mo).
Surgical Technique
The patients were placed in a supine position, on a radiolucent table under general anesthesia without a tourniquet. The guide wire was placed over the deformed knee, and the planned trajectory of the screw was mimicked through fluoroscopy assistance. It was necessary to have true anteroposterior and lateral radiographic projections in 45 degrees flexion position for the affected knee. The intersection of the 2 perpendicular lines drawn on the radiographic projections formed the dermal entry point for the screw. A 1 cm incision was made in this location. A guide wire was inserted into the distal epiphysis in a small groove just distal to the medial epicondyle (in valgus deformity) or lateral epicondyle (in varus deformity) of the femur under fluoroscopic control. The flexed knee fulfills the posterior translation for collateral ligaments to be away from the screw entry.
The wire was then directed obliquely across the physis with a projection of 60 to 70 degrees in relation to the physeal plane. The guide wire was further advanced at the junction of the central two-thirds and the peripheral third of the medial or lateral femoral condylar physis. This was done based on the anteroposterior view ending in the junctional area between the metaphyseal and diaphyseal segments. On the lateral view, careful care and considerations were taken to ensure that the screws cross the center of the physis (Fig. 1).
FIGURE 1.
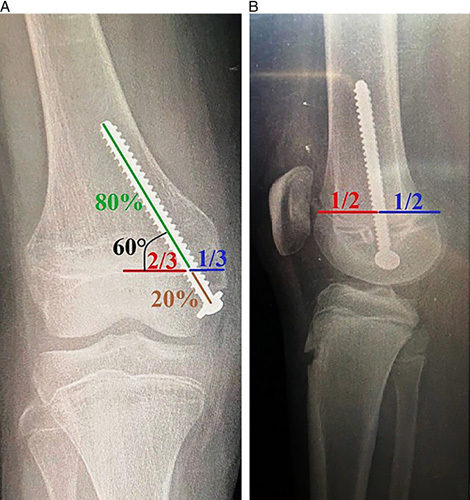
Retrograde transphyseal guided growth in a distal femur. A, Anteroposterior view, the screw entered from the epiphysis and directed toward the metaphysis with a 60-degree inclination to the physeal line at the junctional point between the medial one-third and central two-third of the medial femoral condyle, with a ratio of 2:8 of the screw length in epiphyseal and metaphyseal areas, respectively. B, Lateral view, the screw position in the central point of the physis.
A cannulated drill (5.2 mm) was used to drill the entry point at the cortex, up to the area just below the physis. Drilling across the physis was completely avoided. A cannulated stainless steel fully threaded 7 mm screw was inserted over the wire, with a washer using a screwdriver for manual insertion technique by hand; power insertion technique was avoided.7,8
The length of the screw was intended to cover 20% in length in epiphysis and 80% in metaphysis to achieve maximum bone grip in both physeal sides. Passive knee manipulation with full flexion and extension was done to release the soft tissue entrapped under the screw washer. Local anesthesia infiltration through the surgical wound was used before skin closure with a single subcuticular stitch.
Follow-up
The mLDFA measurements were taken in 2 to 3 consecutive months and compared with the preoperative measurements. The screws were removed when the normal range of mLDFA was between 85 and 90 degrees. This was the desired angular range for the mLDFA compared with its counterpart’s medial proximal tibial angle. These measurements in turn ensure the passage of the mechanical axis through the central portion of the knee (Fig. 2). Follow-up after the removal of the femoral screw was essential up to skeletal maturity. If the physis continued to grow after full correction, the consequences of screw removal were noted.
FIGURE 2.
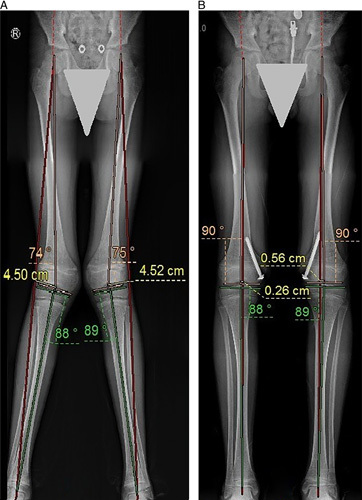
Bilateral genu valgus; femoral origin. A, Long-standing radiograph scanogram of a skeletally immature patient. B, The same patient after using the retrograde transphyseal guided growth technique with optimal bilateral deformity correction.
The efficacy of the procedure was then evaluated by calculating the degrees of correction per month and data were statistically described in terms of mean±standard deviation and range, or frequencies (number of cases) and percentages when appropriate. Numerical data were tested for the normal assumption using the Kolmogorov Smirnov test. Comparison of numerical variables between the study groups (varus and valgus groups or female and male groups) was done using Student t test for independent samples. Two side P<0.05 was considered statistically significant. All statistical calculations were done using the computer program, IBM SPSS (Statistical Package for the Social Sciences; IBM Corp, Armonk, NY) release 22 for Microsoft Windows.
RESULTS
There were a total of 40 patients: 17 females (29 physes) and 23 males (36 physes); the average chronological age at surgery for females was 11.75 (range: 8.4 to 14.5 y) and for males was 13.75 (range, 11.75 to 15.6 y). The average total correction rate for mLDFA was 1.3 degrees per month (range, 0.5 to 1.857 degrees) postsurgical intervention [Table 1 (Supplementary Material, Supplemental Digital Content 1, http://links.lww.com/BPO/A351)].
TABLE 1.
Descriptive Statistics for All Study Cohorts
| n | Minimum | Maximum | Mean | Standard Deviation | |
|---|---|---|---|---|---|
| Age (y) | 40 | 8.4 | 15.75 | 12.9 | 1.6087 |
| Initial mLDFA (deg.) | 65 | 74 | 100 | 83.02 | 6.719 |
| Duration of correction (mo) | 65 | 4 | 11 | 5.9 | 2.393 |
| Final mLDFA (deg.) | 65 | 83 | 92 | 87.9 | 1.785 |
| Amount of correction (deg.) | 65 | 3 | 16 | 7.6 | 2.431 |
| Rate of correction (deg./mo) | 65 | 0.5 | 1.857 | 1.3 | 0.3468 |
In the female group, the average correction rate was 1.2 degrees per month whereas in the male group, the average rate was 1.35 degrees per month, with a P<0.05 (Table 2).
TABLE 2.
Rate of Correction Per Month Related to Sex and Deformity Type
| Sex | Mean | No. Patients | No. Femurs | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Female | 1.2 | 17 | 29 | 0.3353 | 0.5 | 1.666 |
| Male | 1.35 | 23 | 36 | 0.3596 | 0.857 | 1.857 |
| P | 0.012 | |||||
| Total | 1.3 | 40 | 65 | 0.3468 | 0.5 | 1.857 |
| Valgus | 1.25 | 32 | 52 | 0.3505 | 0.5 | 1.777 |
| Varus | 1.4 | 10 | 13 | 0.3455 | 1.0 | 1.857 |
| P | 0.025 | |||||
| Total | 1.3 | 40* | 65 | 0.3468 | 0.5 | 1.857 |
Two patients had windswept deformities.
In the group with distal femoral valgus deformity, the average correction rate was 1.25 degrees per month. However, in the group with distal femoral varus deformity, the average rate was 1.4 degrees per month, with a P<0.05 (Table 2).
In 61 physes, screws were removed before skeletal maturity, at the time of deformity correction or slight overcorrection (mechanical axis deviation 4 to 6 mm) in preparation for recurrence and related to the remaining growth activity. In 15 of these physes, there was a rebound effect with an average of 1.8 degrees ranging from 1 to 3 degrees. In 42 physes, there was no change in angular measurements during the remaining years of growth. There was progression after screw removal in 4 physes with an average of 1.6 degrees ranging from 1 to 2 degrees (Table 3). In summary, there is sufficient evidence that growth resumes in the portion of the physis traversed by the screw after screw removal in most cases. In 4 physes the screw was removed at skeletal maturity with a suboptimal measurement for the mLDFA, despite the notable improvement in comparison to the initial measurement.
TABLE 3.
Outcomes After Screw Removal; Follow-up in Months: Rebound, Stable, and Progression With the Percentages for Each Type of Deformity
| Types (%) | ||||||
|---|---|---|---|---|---|---|
| Follow-up (mo) Average (Range) | Valgus | Varus | Total (%) | |||
| Outcome | 15.5 (6-26) | Rebound 1.8 degrees (1-3 degrees) | Count | 14 | 1 | 15 |
| % Within outcome | 93.3 | 6.7 | 100 | |||
| % Within deformity | 26.9 | 7.7 | 24.6 | |||
| 12.6 (6-30) | Stable | Count | 33 | 9 | 42 | |
| % Within outcome | 78.6 | 21.4 | 100 | |||
| % Within deformity | 68.8 | 69.2 | 68.9 | |||
| 9.7 (6-12) | Progression 1.6 degrees (1-2 degrees) | Count | 1 | 3 | 4 | |
| % Within outcome | 25.0 | 75.0 | 100 | |||
| % Within deformity | 1.9 | 23.1 | 6.5 | |||
| Total | 12.6 (6-30) | Count | 48 | 13 | 61 | |
| % Within outcome | 80.0 | 20.0 | 100 | |||
| % Within deformity | 100 | 100 | 100 | |||
The first 7 patients in this study had minimal complications. These complications include painful flexion in early postoperative days. This was not recorded in subsequent cases after using the manipulation maneuver for the knee intraoperatively to release the soft tissue entrapped under the screw washer, before definitive screw tightening. There were no other screw-related complications, infections, fractures, or secondary deformities in all the study patients.
DISCUSSION
Physeal guided growth technique, also known as hemiepiphysiodesis, for angular deformities in growing children often eliminates the need for osteotomies.9,10 In 1949, Blount and Clarke described physeal stapling, which stopped growth rapidly and almost completely.11–13 Complications included superficial wound infections, staple malposition, extrusion, bending and breakage and difficulty in removing the staples.14,15 The staples used initially were made of stainless steel and were prone to breakage. However, the improved flat-profile Vitallium staples, reinforced at the shoulders, have proven to be more efficient.16 In particular, hemiepiphyseal stapling using the newer staples has been shown to be a safe and reliable method of correction of angular knee deformities. Nevertheless, the staples would extrude or migrate.17 Although growth should be expected to resume after staple removal, improper technique through the violation of periosteum, epiphyseal vessels, or physis either during insertion or removal may preclude growth resumption. Although the technique remains popular, it requires meticulous care to prevent disruption of the perichondral ring. Stevens et al18 presented a large series of hemiepiphyseal stapling performed for the treatment of genu valgum in 152 knees; the average correction rate in lateral distal femoral angle was 0.9 degrees per month.
In 1998 Métaizeau et al2 described the percutaneous epiphysiodesis transphyseal screws (PETS) technique that was with a metaphyseal entry approaching epiphysis. It was used as a hemiepiphysiodesis technique on 9 patients with angular deformities of the knee. This method of PETS had numerous advantages. The operative technique was straightforward and required a short learning curve; it took about 10 minutes to insert 2 femoral screws.2
Métaizeau and colleagues concluded that the screw did not destroy the growth potential of the physis from the outset. Further growth was still possible when the screws were removed before physeal closure. This feature provided a controlled manner of growth retardation and prevented overcorrection. The screws would begin to exert their effect on the growth plate soon after insertion.2 The rigidity of the screws was believed to be accountable for the speed of correction.2 A short time lag, nevertheless, exists to allow for bone with compressive forces to build up across the trabeculae. This time could be reduced by initial compression loading of the screws.2 However, compression cannot be achieved with the use of fully threaded screws, which is the current preferred medium to use, as it is easier to remove.2,19,20
Joseph and colleagues evaluated the PETS technique for 48 femoral physes with angular deformity regarding effectiveness, predictability, and reversibility. They concluded that PETS represents the best of both worlds.21–23 It combines the minimal invasiveness of a percutaneous technique with reversibility. Anecdotally, they have found that the patients had much less postoperative pain and swelling compared with those in their previous experience using the percutaneous physeal ablation techniques. In comparison with techniques requiring a staple or small plate, the incisions were much smaller and the patients reported a much more rapid return to function.21–24
In 2004 a new method emerged; an 8-plate system was designed (Orthofix, Verona, Italy).23 The results of this technique were published in 2008 by Burghardt and colleagues.23–26 The 8-plate is a 2-hole, nonlocking plate, with 2 screws used to perform temporary hemiepiphysiodesis; tension band plate (TBP) was thought to be an improvement over the Blount staple because it theoretically does not compress the growth plate as seen in the stapling method. So, it is a reversible technique and it is more resistant to spontaneous extrusion.26–28 Yeo et al29 investigated the 8-plate correction rate in 80 distal femoral physis that ranged from 0.40 to 1.15 degrees per month according to its pathologic cause. The 8-plate femoral correction rate was 0.77 degrees per month (0.14 to 1.42 degrees/mo) in the study by Danino et al,30 which included 444 patients.
Park and colleagues compared the efficacy of PETS and TBP and this was the first comparative study between these techniques in patients with idiopathic genu valgum. There were significant differences in the rate of correction between the techniques. Although both PETS and TBP were capable of gradually correcting genu valgum deformities in skeletally immature patients, PETS proved to be faster in deformity correction rate with differences approaching statistical significance. The rate of correction at the distal femur averaged 0.92 degrees per month.3 These results were comparable with a study by Shin and colleagues, which also reported a similar rate of 0.92 degrees per month at the distal femur.30,31 Yet, in the TBP group, the rate of correction at the distal femur averaged at 0.64 degrees per month.3 These results were also similar with those presented by Gottliebsen et al32 at 0.58 degrees per month at distal femur. Although the TBP method has a longer lever arm, it takes a longer time to function as a hinge. To be more specific, the PETS holds the growth plate immediately after operation by means of mechanical compression, but the plate may not instantly restrain the physis, which requires tension to act as a TBP.3
Each technique has its advantages and disadvantages, which have been investigated in previous studies. In our study, we investigated the mechanical tethering effect of transphyseal screw in the reverse direction of the original Métaizeau technique, which was described with an epiphyseal entry point approaching the metaphysis. As with this orientation, the screw compression effect could be better in comparison of the screw of metaphyseal-epiphyseal direction, because the Métaizeau screw tethers the growth plate with the distal screw serrations only through the epiphysis.2 So, the screw failure with ongoing growth is anticipated as the screw pullout force in the same direction of metaphyseal growth direction (Fig. 3). However, when using the screw in the epiphyseal-metaphyseal direction the screw pullout force is in reverse direction to the metaphyseal growth direction. The screw tethers the physis with a screw head and washer which increase the surface area of the screw head. As 20% of screw length will cross through the epiphysis and 80% will cross in metaphysis it provides a firmer holding mechanism. It is known that the effect of a transphyseal screw is related to the angulation of the screw to the physis and to its distance from the center of the bone, the mean angle between the physes and screws was 52.4±5.9 degrees at the distal femurs in the original antegrade screw. The screw position is in a zone at one-third to one-fourth of the growth plate width,3 whereas in the retrograde screw, the authors aimed for a screw position to be at 60 to 70 degrees inclination with the physeal plane and projected at the lateral one-third of the growth plate. All these mechanical modifications were hypothesized to be responsible for the firming tethering screw effect.
FIGURE 3.
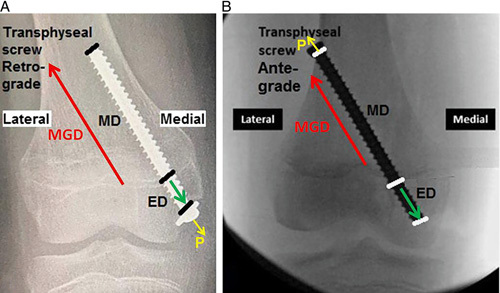
A comparison showing the main differences between retrograde transphyseal screw (P+ED against MGD) (A) and the standard antegrade transphyseal screw (P+MGD against ED) (B). ED indicates epiphyseal distance; MD, metaphyseal distance; MGD, metaphyseal growth direction; P, pullout.
In our technique, we tried to acquire the advantage of previous procedures. It combines the minimal invasiveness of a percutaneous technique. It is a short and simple procedure with optimal transphyseal compression. It also allows early postoperative full weight-bearing mobilization and no perichondrial ring injury. It has potential growth reversibility after removal and the advantages of this cost-effective technique and performing the surgery under day case protocol. The main concern in our technique is that the epiphyseal entry point would slightly invade the intracapsular joint space although it is an extra-articular entry. Despite this, no complications were recorded in this study except in earlier 7 patients; there was painful flexion in early postoperative days, which was because of soft tissue entrapment under the screw washer. This complication was not recorded in subsequent cases after using the manipulation maneuver of the knee with full flexion and extension intraoperatively before definitive screw tightening. There were no other screw-related complications, infections, fractures, or secondary deformities in this group.
The rate of correction at the distal femur averaged 1.25 degrees per month in valgus deformities and 1.4 degrees per month in varus deformities in retrograde transphyseal guided growth screw technique, which provided accelerated rate in comparison to previous techniques to achieve the optimal correction within the remaining period of growth.
There were some limitations to our study. The relatively small number of cases may have decreased the power for statistical analysis. Further studies with a larger cohort are needed to fully evaluate the technique. Second, there was no control or comparative group to evaluate the new technique precisely. So, we relied on previous studies for various guided growth techniques to compare between the rates of correction for each procedure. However, the entire cohort of patients continued their follow-up until physeal closure even after the screw removal, so we could detect any rebound or progression of the deformities.
Finally, the concept of correction using percutaneous retrograde transphyseal guided growth screw had an efficient rate in skeletally immature femur for coronal angular deformities with expected potentiality of resuming physeal growth after screw removal.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.pedorthopaedics.com.
Footnotes
No funding sources.
The authors declare no conflicts of interest.
Contributor Information
Ahmed Abdelaziz, Email: ahmed_abdelaziz50@yahoo.com.
Sameeh M. ElAshry, Email: Sameeh76or@yahoo.com.
Mohammad M. Awadh, Email: egpinusa@yahoo.com.
Aliaa Khaja, Email: aliaa.khaja@gmail.com.
Saleh Alsaifi, Email: salsaifi@gmail.com.
REFERENCES
- 1. De Brauwer V, Moens P. Temporary hemiepiphysiodesis for idiopathic genua valga in adolescents: percutaneous transphyseal screws (PETS) versus stapling. J Pediatr Orthop. 2008;28:549–554. [DOI] [PubMed] [Google Scholar]
- 2. Metaizeau JP, Wong-Chung J, Bertrand H, et al. Percutaneous epiphysiodesis using transphyseal screws (PETS). J Pediatr Orthop. 1998;18:363–369. [PubMed] [Google Scholar]
- 3. Park H, Park M, Kim SM, et al. Hemiepiphysiodesis for idiopathic genu valgum: percutaneous transphyseal screw versus tension-band plate. J Pediatr Orthop. 2018;38:325–330. [DOI] [PubMed] [Google Scholar]
- 4. Kuzma AL, Luo TD, De Gregorio M, et al. Biomechanical evaluation of interfragmentary compression of lag screw versus positional screw at different angles of fixation. J Orthop Trauma. 2019;33:183–189. [DOI] [PubMed] [Google Scholar]
- 5. Carpenter RS, Galuppo LD, Stover SM. Effect of diameter of the drill hole on torque of screw insertion and pushout strength for headless tapered compression screws in simulated fractures of the lateral condyle of the equine third metacarpal bone. Am J Vet Res. 2006;67:895–900. [DOI] [PubMed] [Google Scholar]
- 6. Paley D. Normal lower limb alignment and joint orientation. Principles of Deformity Correction, 1st ed. Berlin, Germany: Springer-Verlag; 2005:11–17. [Google Scholar]
- 7. Zlowodzki MP, Wijdicks CA, Armitage BM, et al. Value of washers in internal fixation of femoral neck fractures with cancellous screws. J Orthop Trauma. 2015;29:e69–e72. [DOI] [PubMed] [Google Scholar]
- 8. Bishop JA, Behn AW, Castillo TN. The biomechanical significance of washer use with screw fixation. J Orthop Trauma. 2014;28:114–117. [DOI] [PubMed] [Google Scholar]
- 9. Stevens PM. Guided growth: 1933 to the present. Strategies Trauma Limb Reconstr. 2006;1:29–35. [Google Scholar]
- 10. Phemister DB. Operative arrestment of longitudinal growth of bones in the treatment of deformities. J Bone Joint Surg Am. 1933;15-A:1–15. [Google Scholar]
- 11. Phemister DB. Epiphysiodesis for equalizing the length of the lower extremities and for correcting other deformities of the skeleton. Mem Acad Chir (Paris). 1950;76:758–763. [PubMed] [Google Scholar]
- 12. Haas SL. Retardation of bone growth by a wire loop. J Bone Joint Surg. 1945;27:25–36. [Google Scholar]
- 13. Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling: a preliminary report. J Bone Joint Surg. 1949;31:464–478. [PubMed] [Google Scholar]
- 14. Blount WP. A mature look at epiphyseal stapling. Clin Orthop Relat Res. 1971;77:158–163. [PubMed] [Google Scholar]
- 15. Frantz CH. Epiphyseal stapling: a comprehensive review. Clin Orthop Relat Res. 1971;77:149–157. [PubMed] [Google Scholar]
- 16. Mielke CH, Stevens PM. Hemiepiphyseal stapling for knee deformities in children younger than 10 years: a preliminary report. J Pediatr Orthop. 1996;16:423–429. [DOI] [PubMed] [Google Scholar]
- 17. Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 18. Stevens PM, Maguire M, Dales MD, et al. Physeal stapling for idiopathic genu valgum. J Pediatr Orthop. 1999;19:645–649. [PubMed] [Google Scholar]
- 19. Bowen JR, Johnson WJ. Percutaneous epiphysiodesis. Clin Orthop. 1984;190:170–173. [PubMed] [Google Scholar]
- 20. Timperlake RW, Bowen JR, Guille JT, et al. Prospective evaluation of fifty three consecutive percutaneous epiphysiodeses of the distal femur and proximal tibia and fibula. J Pediatr Orthop. 1991;11:350–357. [PubMed] [Google Scholar]
- 21. Inan M, Chan G, Littleton AG, et al. Efficacy and safety of percutaneous epiphysiodesis. J Pediatr Orthop. 2008;28:648–651. [DOI] [PubMed] [Google Scholar]
- 22. Joseph G, Khoury, Joao O, et al. Results of screw epiphysiodesis for the treatment of limb length discrepancy and angular deformity. J Pediatr Orthop. 2007;27:623–628. [DOI] [PubMed] [Google Scholar]
- 23. Stevens PM. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27:253–259. [DOI] [PubMed] [Google Scholar]
- 24. Ogilvie JW, King K. Epiphysiodesis: two-year clinical results using a new technique. J Pediatr Orthop. 1990;10:809–811. [PubMed] [Google Scholar]
- 25. Canale ST, Christian CA. Techniques for epiphysiodesis about the knee. Clin Orthop. 1990;255:81–85. [PubMed] [Google Scholar]
- 26. Surdam JW, Morris CD, DeWeese JD, et al. Leg length inequality and epiphysiodesis: review of 96 cases. J Pediatr Orthop. 2003;23:381–384. [PubMed] [Google Scholar]
- 27. Burghardt RD, Herzenberg JE, Standard SC, et al. Temporary hemiepiphyseal arrest using a screw and plate device to treat knee and ankle deformities in children: a preliminary report. J Child Orthop. 2008;2:187–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burghardt RD, Herzenberg JE. Temporary hemiepiphysiodesis with the eight-plate for angular deformities: mid-term results. J Orthop Sci. 2010;15:699–704. [DOI] [PubMed] [Google Scholar]
- 29. Yeo A, Richards C, Eastwood DM. Rate of lower limb angular correction in 8-plate hemiepiphysiodesis in children with varying skeletal pathologies. Orthop Proc. 2015;97-B:9. [Google Scholar]
- 30. Danino B, Rödl R, Herzenberg JE, et al. Guided growth: preliminary results of a multinational study of 967 physes in 537 patients. J Child Orthop. 2018;12:91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shin SJ, Cho TJ, Park MS, et al. Angular deformity correction by asymmetrical physeal suppression in growing children: stapling versus percutaneous transphyseal screw. J Pediatr Orthop. 2010;30:588–593. [DOI] [PubMed] [Google Scholar]
- 32. Gottliebsen M, Rahbek O, Hvid I, et al. Hemiepiphysiodesis: similar treatment time for tension-band plating and for stapling: A randomized clinical trial on guided growth for idiopathic genu valgum. Acta Orthop. 2013;84:202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.pedorthopaedics.com.


