Background:
Despite being a common procedure, there are no standard protocols for postoperative immobilization and rehabilitation following reconstructive hip surgery in children with cerebral palsy (CP). The purpose of this study was to investigate variability in postoperative management and physical therapy (PT) recommendations among orthopaedic surgeons treating hip displacement in children with CP.
Methods:
An invitation to participate in an anonymous, online survey was sent to 44 pediatric orthopaedic surgeons. The case of a child undergoing bilateral femoral varus derotation osteotomies and adductor tenotomies was presented. Surgeons were asked to consider their typical practice and the case scenario when answering questions related to immobilization, weight-bearing, and rehabilitation. Recommendations with increasingly complex surgical interventions and different age or level of motor function were also assessed.
Results:
Twenty-eight orthopaedic surgeons from 9 countries with a mean 21.3 years (range: 5 to 40 y) of experience completed the survey. Postoperative immobilization was recommended by 86% (24/28) of respondents with 7 different methods of immobilization identified. All but 1 (23/24) reported immobilizing full time. Most (20/23) reported using immobilization for 4 to 6 weeks. Return to weight-bearing varied from 0 to 6 weeks for partial weight-bearing and 0 to 12 weeks for full weight-bearing. PT in the first 1 to 2 weeks postoperatively was reported as unnecessary by 29% (8/28) of surgeons. PT for range of motion, strengthening, and return to function was recommended by 96% (27/28) of surgeons, starting at a mean of 2.6 weeks postoperatively (range: 0 to 16 wk). Only 48% (13/27) reported all of their patients would receive PT for these goals in their practice setting. Inpatient rehabilitation was available for 75% (21/28) but most surgeons (17/21) reported this was accessed by 20% or fewer of their patients.
Conclusions:
Postoperative immobilization and PT recommendations were highly variable among surgeons. This variability may influence surgical outcomes and complication rates and should be considered when evaluating procedures. Further study into the impact of postoperative immobilization and rehabilitation is warranted.
Key Words: cerebral palsy, hip, surgery, physical therapy, immobilization, rehabilitation
Reconstructive hip surgery for children with cerebral palsy (CP) is an effective treatment for progressive hip displacement.1 Surgery typically includes a proximal femoral varus derotation osteotomy (VDRO) to correct coxa valga and increased femoral anteversion, a pelvic osteotomy (PO) to correct acetabular dysplasia or a combination of both.2 The ideal age and dose of surgical intervention used to treat hip displacement remain unclear. It has been suggested that successful outcomes may be impacted by age at surgery, preoperative migration percentage (MP), Gross Motor Function Classification System (GMFCS) level, and surgeon experience.3–5 The impact of postoperative care on surgical outcomes has been poorly evaluated.
Various methods of postoperative immobilization following reconstructive hip surgery have been described. Historically, the most common method reported in the literature has been a hip spica cast.1,4,6–8 The use of bilateral knee immobilizers with an abduction wedge, abduction brace, and abduction Petrie cast have also been described.3,9,10 A recent review of immobilization following reconstructive hip surgery enrolled in the Cerebral Palsy Hip Outcomes Project (CHOP), an international multicenter prospective study, found that removable immobilization at the hip alone, which included pillows, abduction wedge, or hip abduction brace, was the most frequently used method of immobilization postreconstructive surgery.11 The length of immobilization also varies widely, often reported between 2 and 8 weeks.1 Alternatively, Miller et al12 have reported using no postoperative immobilization. The impact of different immobilization methods on outcomes is unknown.
Postoperative protocols related to physical therapy (PT) are poorly described in the literature. Some study authors may report children receive PT postoperatively but details, such as frequency and intensity, are rarely provided.8,9,12,13 In a systematic review of hip osteotomies in children with CP, Bouwhuis et al1 reported that cointerventions, including PT, were comparable between outcome studies despite protocols being minimally described or not reported at all. We are unaware of any studies investigating the impact of postoperative PT on surgical outcomes or return to function.
The purpose of this study was to investigate variability in postoperative immobilization and PT recommendations among orthopaedic surgeons treating hip displacement in nonambulatory children with CP. Given the lack of literature on best practices in postoperative care following reconstructive hip surgery, we hypothesized that there would be significant variability. In addition, we aimed to learn about current practice models and which health care team members were involved in postoperative management.
METHODS
Purposive sampling was used to identify participants. An invitation to complete an anonymous online survey was sent to 44 pediatric orthopaedic surgeons with expertise in the treatment of children with CP. This included surgeons contributing to an existing prospective, multicenter database studying hip outcomes in patients with CP (CHOP, https://clinicaltrials.gov/ct2/show/NCT01987882), and surgeons known to the study authors. Research ethics board approval was received. Participants were advised that, by completing the study, they were consenting to participation. Study data was collected and managed using the secure web application, Research Electronic Data Capture (REDCap) hosted at BC Children’s Hospital Research Institute.14,15
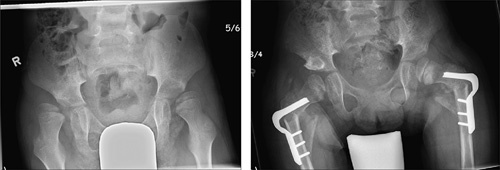
Participants were asked questions related to their experience, practice setting, and caseload. To further understand the roles of health care team members, surgeons identified which team members were involved in different stages of postoperative care. Two main case scenarios with clinical findings and surgical intervention performed were described. Preoperative and postoperative images were provided. In case 1, a 5-year-old girl with spastic quadriplegia, GMFCS level IV, with preoperative MPs of 77% for the right hip and 73% for the left hip, underwent bilateral VDROs and bilateral adductor tenotomises (Fig. 1). Surgeons were asked to consider their typical practice and the case scenario while answering questions related to immobilization, weight-bearing, and rehabilitation. Subsequently, surgeons were asked how management would differ if the scenario was altered such that only a unilateral VDRO was completed, the patient was 15 years old, or had different levels of mobility (GMFCS III or V).
FIGURE 1.

Preoperative and postoperative radiographs for case 1.
A second case was presented and respondents were again asked to identify differences in management. In case 2, a 6-year-old boy at GMFCS level V, with preoperative MPs of 90% for the right hip and 58% for the left hip, had bilateral VDROs plus a PO (Fig. 2). Increasingly complex surgical scenarios (an open reduction and bilateral pelvic osteotomies) were then added to this scenario.
FIGURE 2.
Preoperative and postoperative radiographs for case 2.
Descriptive statistics were used. Categorical variables were described with frequencies and percentages. Continuous variables were described with means, where appropriate.
RESULTS
The survey was completed by 28 orthopaedic surgeons from 9 countries, for a response rate of 28/44 (64%). Responses related to clinical experience and practice settings are shown in Table 1. Table 2 lists health care team members involved in aspects of postoperative care.
TABLE 1.
Surgeon Demographics, Practice Data, and Health Care Team Members
| Responses (N=28) [n (%)] | |
|---|---|
| Years in practice [mean (range)] | 21.3 (5-40) |
| Approximate patient visits per year [mean (range)] | 1350 (100-4500) |
| Approximate percentage of practice devoted to children with cerebral palsy [mean (range)] | 58 (20-100) |
| Country | |
| United States | 13 (46) |
| Canada | 4 (14) |
| Sweden | 3 (11) |
| UK | 2 (7) |
| Australia | 2 (7) |
| Denmark | 1 (4) |
| India | 1 (4) |
| Israel | 1 (4) |
| New Zealand | 1 (4) |
| Hospital setting | |
| Pediatric specialty hospital | 20 (71) |
| Tertiary care hospital (adult and pediatric hospital) | 7 (25) |
| General hospital (adult and pediatric hospital) | 1 (4) |
| Medical systems | |
| Publicly funded | 14 (50) |
| Mixed public/private | 12 (43) |
| Private | 2 (7) |
| Model of care | |
| Interdisciplinary | 19 (68) |
| Transdisciplinary | 6 (21) |
| Multidisciplinary | 3 (11) |
| Part of the CHOP (Cerebral Palsy Hip Outcomes Project) International Multicentre Study | 21 (75) |
TABLE 2.
Health Care Team Members Involved During Care
| n (%) | |||
|---|---|---|---|
| Health Care Team Members | Acute Postoperative | Discharge Planning | Orthopaedic Follow-up |
| Physical therapist | 22 (79) | 23 (82) | 22 (79) |
| Nurse practitioner | 17 (61) | 17 (61) | 15 (54) |
| Nurse | 15 (54) | 17 (61) | 15 (54) |
| Occupational therapist | 9 (32) | 13 (46) | 11 (39) |
| Pediatrician | 7 (25) | 5 (18) | 3 (11) |
| Complex care physician | 9 (32) | 5 (18) | 1 (4) |
| Physiatrist | 4 (14) | 2 (7) | 7 (25) |
| Anesthesiologist | 18 (64) | 2 (7) | 0 |
| Social worker | 6 (21) | 10 (36) | 7 (25) |
| Orthotist | 7 (25) | 5 (18) | 17 (61) |
| Respirologist | 5 (18) | 2 (7) | 1 (4) |
| Neurologist | 2 (7) | 1 (4) | 3 (11) |
Case 1, 5 Years Old, GMFCS Level IV, Bilateral VDROs
Seven different methods of postoperative immobilization were identified (Table 3). All but 1 surgeon reported using the immobilization full time. The remaining surgeon reported using an abduction wedge in sitting and lying. Length of immobilization, restrictions on the range of motion (ROM), and recommendations for continued splinting/positioning at night or portions of the day are shown in Table 3. Four surgeons reported they would not immobilize postoperatively. One of these reported using postural management to ensure adequate positioning, while 2 reported using knee immobilizers if the knees were prone to rest in flexion.
TABLE 3.
Type and Duration of Immobilization for Case 1 Reported by Surgeons
| Length of Immobilization (wk) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of Immobilization | No. Surgeons [n (%)] | Full Time Use | Full Time, off for Transport | Not Full Time | 3 | 3-4 | 4 | 4-6 | 6 | 12 | Continued Immobilization Recommended |
| Bilateral long leg splints (Zimmer splints) and abduction wedge | 9 (32) | 5 | 4 | 0 | 1 | 1 | 1 | 1 | 5 | 6 | |
| Abduction wedge only | 8 (29) | 2 | 5 | 1 | 3 | 3 | 1 | 6 | |||
| Hip spica cast | 2 (7) | 2 | NA | NA | 1 | 1 | 1 | ||||
| Petrie or Broomstick cast | 2 (7) | 2 | NA | NA | 2 | 2 | |||||
| Bilateral long leg splints (Zimmer splints) only (no wedge) | 1 (4) | 0 | 1 | 0 | 1 | 0 | |||||
| Bilateral short leg casts with derotation bar and knee immobilizers | 1 (4) | 0 | 1 | 0 | 1 | 1 | |||||
| Hip abduction orthosis and long leg casts | 1 (4) | 1 | 0 | 0 | 1 | 1 | |||||
| None | 4 (14) | NA | NA | NA | 1 | ||||||
| Length of restriction (wk) | |||||||||||
| Range of motion restrictions | 0-1 | 2-3 | 4-5 | 6-7 | 12 | ||||||
| Hip flexion | 7 (25) | Range: 30-90 degrees | 1 | 2 | 1 | 3 | |||||
| Hip adduction | 11 (40) | Range: 0-40 degrees abduction | 2 | 4 | 4 | 1 | |||||
| Time postoperative (wk) | |||||||||||
| Return to weight-bearing | 0-1 | 2-3 | 4-5 | 6-7 | 8 | 12 | |||||
| Partial | 7 | 8 | 7 | 6 | 0 | 0 | |||||
| Full | 5 | 3 | 4 | 14 | 1 | 1 | |||||
NA indicates not applicable.
Most surgeons recommended early mobilization to a wheelchair at postoperative day 0/1 (10/28; 36%), day 2/3 (14/28; 50%), or day 4/5 (2/28; 7%). Two surgeons reported mobilizing to a wheelchair at a much later time (day 30 and 6 wk). Upon discharge home, 79% (22/28) reported the child would be transported in their own car; 21% (6/28) reported the child would be transported via ambulance. When immobilization was removable, 58% (11/19) of surgeons allowed the immobilization to be removed for transport.
Recommendations for return to weight-bearing are shown in Table 3. PT recommendations and availability during the first 1 to 2 weeks following the procedure (before discharge from hospital) and for goals related to ROM, strengthening, and return to function are shown in Table 4. One surgeon who responded ‘sometimes’ recommending PT during the immediate postoperative period noted that PT services were limited so funding was better used after the acute period. Availability and recommendations for inpatient rehabilitation are shown in Table 4.
TABLE 4.
Surgeon Reports of Postoperative PT and Inpatient Rehabilitation Recommendations for Case 1
| % Actually Receiving | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Recommend | 0-25 | 26-50 | 51-75 | 76-99 | 100 | Time PT/Inpatient Rehabilitation Recommended to Start Postsurgery (wk) | Frequency/Length of Stay | |||
| Recommend PT immediately postsurgery (before discharge) | Yes 18 (64%) Sometimes 2 (8%) | 2 | 3 | 3 | 12 | NA | NA | |||
| Recommend PT for goals such as ROM, strength, and return to function | 27 (96%) | 4 | 3 | 1 | 7 | 13 | 0-1 wk: 11 | Daily: 1 | ||
| 2-3 wk: 6 | Daily by parent: 4 | |||||||||
| 4-5 wk: 6 | 2-3× per week: 14 | |||||||||
| 6-7 wk: 2 | 1× per week: 5 | |||||||||
| 8-12 wk: 0 | Rarely: 1 | |||||||||
| 12-16 wk: 1 | Incomplete response: 4 | |||||||||
| Access to inpatient rehabilitation | 21 (75%) | 18 | 1 | 2 | Upon discharge from acute care: 4 | <2 wk: 1 | ||||
| Once immobilization discharged: 6 | 2-4 wk: 9 | |||||||||
| Once weight-bearing as tolerated: 3 | 5-6 wk: 3 | |||||||||
| Location of PT within the first 6 mo postoperatively (select all that apply) | Acute care facility: 4 | |||||||||
| Inpatient rehabilitation facility: 6 | ||||||||||
| Outpatient rehabilitation facility: 16 | ||||||||||
| Within their own home: 11 | ||||||||||
| Private physical therapy clinic: 7 | ||||||||||
| School: 11 | ||||||||||
NA indicates not applicable; PT, physical therapy; ROM, range of motion.
Six different scenarios were then presented with surgeons only identifying differences in how their management would change from the original case 1 scenario. These differences are summarized in Table 5 and described below.
TABLE 5.
Summary of Changes to Postoperative Recommendations Reported for Different Case Scenarios Compared With the Postoperative Care Recommended for Case 1
| No. Surgeons | ||||||||
|---|---|---|---|---|---|---|---|---|
| Change to Case | Reported a Change [n (%)] | Increased Immobilization (Length or Type) | Decreased Immobilization (Length or Type) | Earlier Weight-bearing | Later Weight-bearing | Increased PT | Decreased PT | Increased Inpatient Rehabilitation |
| Case 1, unilateral VDRO | 1 (4) | 1 | ||||||
| Case 1, older age (15 y) | 10 (36) | 2 | 3 | 1 | 2 | 6 | 1 | 1 |
| Case 1, level GMFCS V | 5 (18) | 1 | 1 | 3 | ||||
| Case 1, level GMFCS III | 9 (32) | 1 | 2 | 1 | 9 | 4 | ||
| Case 2 | 5 (18) | 4 | 1 | |||||
| Case 2 with open reduction | 10 (36) | 7 | 3 | |||||
| Case 2 with bilateral pelvic osteotomies | 3 (11) | 3 | ||||||
GMFCS indicates Gross Motor Function Classification System; PT, physical therapy; VDRO, varus derotation osteotomy.
Case 1, 5 Years Old, GMFCS Level IV, Unilateral VDRO Only
Twelve surgeons (42%) reported they never complete a unilateral VDRO. Only 1 surgeon reported a change in recommendations with a unilateral VDRO with time to full weight-bearing reduced from 4 to 6 to 2 weeks.
Case 1, 15 Years Old, GMFCS Level IV, Bilateral VDROs
Ten surgeons (36%) reported a change in management had the child been 15 years old. Length of immobilization was increased by 2 surgeons. Two reduced immobilization from a hip spica for 4 to 6 weeks to no immobilization and 1 surgeon reported they would now allow the immobilization to come off for transport. Two surgeons increased the time to partial or full weight-bearing, while 1 reduced this time. Four surgeons who previously did not recommend PT recommended it for an older child (3 before hospital discharge; 1 postdischarge). Two surgeons recommended PT at a greater frequency after discharge from the hospital, while 1 would decrease it. One surgeon reported 80% of children at this age, up from 0% at age 5 years, would have inpatient rehabilitation.
Case 1, 5 Years Old, Bilateral VDROs, GMFCS Level III or V
Had the child’s motor function been classified at level V, 18% (5/28) of surgeons reported their management would differ. One surgeon reported they would now use a hip spica. Another surgeon noted they would now recommend PT during the acute period “sometimes” rather than always and 2 surgeons would recommend a decrease in the frequency of posthospital discharge. One surgeon recommended PT start immediately postsurgery rather than at 2 weeks postoperatively.
With a child at GMFCS level III, 32% (9/28) reported a change in recommendations. Two surgeons would no longer use full-time immobilization, with 1 also changing from a broomstick cast to a splint. One of these surgeons noted available daytime would be used for standing, walking, or hydrotherapy. Another surgeon noted they would now use splinting after full-time immobilization for a period of 3 months. All 9 surgeons reported changes in PT recommendations. Surgeons who did not previously recommend PT during the acute period in the hospital now reported they would recommend it always (2 surgeons) or sometimes (1 surgeon). Four reported increasing the recommended frequency of PT posthospital discharge and 3 surgeons recommended starting this PT earlier. One surgeon would reduce the time to full weight-bearing to 2 weeks. Four surgeons noted the percentage of children at GMFCS level III in their practice attending inpatient rehabilitation would increase.
Case 2, 6 Years Old, GMFCS Level V, Bilateral VDROs, Unilateral Pelvic Osteotomy
With this scenario, 5 (18%) surgeons reported a change in recommendations. Four surgeons reported they would now use a hip spica cast. One surgeon reported they would delay return to partial and full weight-bearing from week 0 to 6. One surgeon would now recommend hip flexion be limited to 90 degrees (Fig. 2).
Case 2, 6 Years Old, GMFCS Level V, Bilateral VDROs, Unilateral Pelvic Osteotomy With Open Reduction
With the addition of an open reduction to this scenario, 6 surgeons reported they would utilize a hip spica cast or Broomstick cast instead of bilateral long leg splints (zimmer splints) and abduction wedge or abduction wedge alone. One surgeon reported an abduction brace would be utilized rather than no immobilization. Three surgeons, who reported initiating an early return to partial and full weight-bearing in postoperative weeks 0 or 1 in the original scenario, would delay return to full weight-bearing to 6 weeks; one of these surgeons still reported they would permit early partial weight-bearing at week 0. One surgeon noted in open text comments that open reductions were never done.
Case 2, 6 Years Old, GMFCS Level V, Bilateral VDROs, Bilateral Pelvic Osteotomies
Three surgeons reported they would use a hip spica cast if bilateral pelvic osteotomies were completed. One surgeon reported never performing bilateral pelvic osteotomies.
DISCUSSION
This survey demonstrates high variability in postoperative immobilization and therapy recommendations amongst an international group of surgeons following reconstructive hip surgery in children with CP. The impact of this variability on surgical outcomes and patient satisfaction was not investigated and remains unclear. While some variability in practice is expected, high variability can impact the quality of care, patient safety, and the value of the care provided.16 Given the lack of consensus on optimal postoperative protocols, the care provided to children with CP following reconstructive hip surgery should be studied further and considered when evaluating surgical outcomes.
Together with improved fixation, the use of abduction pillows or knee immobilizers has become more common.3,11 It’s been suggested that hip spica casting be reserved for children with poor bone quality or those at risk of implant failure.3,7,17 Our findings are consistent with this as surgeons reported they would choose increased immobilization with increasing patient complexity, including surgery in children at GMFCS level V, bilateral surgery, and an open reduction. The use of a hip spica cast increased from 7% in case 1 to 21% in case 2 with the addition of a PO and/or an open reduction. Given the significant variability and lack of evidence on best practice for postoperative immobilization, patient and parent experience with no, or different, methods of immobilization should be evaluated. We are unaware of any literature investigating parent preference regarding different postoperative immobilization methods or factors such as postoperative pain control, ease of care, or return to function. Miller et al12 reported that 6 parents with children who had previously had casts preferred immediate mobilization following surgery, and that floor nurses found children who received no postoperative immobilization were more uncomfortable and more difficult to handle in the first 48 to 72 hours than when a cast was used. One surgeon commented in the survey responses that, “it is the surgeon’s responsibility to have a stable fixation for a VDRO and PO and to have no restrictions for the child and family.” This assumes no immobilization is the family preference but further evaluation of this is required. Study of patient-important outcomes, such as pain control, ease of care, and return to function, with different types of immobilization is warranted.
All surgeons described team-based models of care (Table 2). Approximately 80% of respondents reported PTs were involved in acute postoperative management, discharge planning, and orthopaedic follow-up visits. During acute postoperative management, anesthesiology involvement, presumably for pain control, was common. At orthopaedic follow-up visits, an orthotist and a nurse and/or nurse practitioner were also often involved. These results suggest that pain relief, immobilization, and therapy are important in postoperative care.
Almost all surgeons reported they recommended PT for goals related to ROM, strengthening, and return to function. However, there was a wide range in when PT was initiated (0 to 16 wk) and in frequency (rarely to daily). Of concern, less than half of respondents who recommended PT reported that all of their patients would receive PT for these goals. Similarly, there was high variability for return to weight-bearing with recommendations ranging between 0 and 6 weeks for partial weight-bearing and 0 to 12 weeks for full weight-bearing. The impact of time to weight-bearing on return to function is unknown. While inpatient rehabilitation was often available most surgeons reported this was accessed by 20% or fewer of their patients. Children with greater independent baseline mobility (GMFCS level III) were more likely to have an inpatient rehabilitation stay.
This study did not explore the type of therapy or intensity of intervention recommended or provided. These details are not available in the literature. Future studies reporting surgical outcomes of reconstructive hip surgery should report postoperative therapy interventions to allow for comparison. Surgeons responding to this survey may not have been able to report what PT is provided to their patients and, therefore, the inclusion of physical therapists in future research in this area is advisable. In addition, the experiences of therapists, children, and families may provide valuable insights into the benefits and challenges associated with different postoperative protocols, including such factors as the timing of returning to weight-bearing. Determining optimal PT protocols utilizing patient-important outcomes is a key part of optimizing value in the care provided.16
As part of the CHOP, Kulkarni et al11 reported postoperative immobilization used in actual practice but that review compared a heterogenous patient population undergoing different reconstructive procedures with varying levels of complexity. The use of case scenarios in our survey allowed for direct comparison of responses and allowed surgeons to provide details related to their practice choices. This survey also collected additional information not collected in CHOP related to decision-making, access to rehabilitation, and postoperative PT. Furthermore, this study permitted the involvement of surgeons not participating in the CHOP. Additional surgeons were selected based on their known interest in treating children with CP. By utilizing purposive sampling, we aimed to identify surgeons who would be experienced and have established protocols for reconstructive hip surgery. Years of experience were similar between surgeons involved in CHOP (mean: 22.4 y, range: 5 to 40 y) and those not involved (mean: 18.0 y, range: 6 to 32 y). Despite this opportunity to include additional surgeons, almost all were from developed countries, and surgeons from low-income countries are not represented. The inclusion of these surgeons may further increase variability.
This study has limitations. The reason for the variability in postoperative care was not explored. Factors such as historical treatment practices, method of surgical fixation, surgeon preferences, access to funding, and available resources may influence how children are treated. We asked surgeons to recall their typical practice rather than prospectively collecting data on actual cases. This may lead to the generalization of reporting. Surgeons may customize their postoperative care to an individual child based on bone health, surgical fixation, and rate of healing. In addition, postoperative care may depend on environmental factors such as the distance required to travel or the home environment. Finally, this study focused mostly on the postoperative care of nonambulatory children with CP.
CONCLUSIONS
The findings of this survey demonstrate that among experienced CP surgeons, there is wide variation in the method of postoperative immobilization and regimes of PT following reconstructive hip surgery for children with CP. To improve the quality and value of the care provided and maximize patient safety, evaluation of the impact of different postoperative protocols to optimize patient outcomes and satisfaction is required. This evidence could be generated in clinical trials or large-scale prospective multi-centered observational studies such as the CHOP.
Footnotes
S.D.M., M.J., N.F., and K.M.: helped in the study design, survey development, data analysis, manuscript preparation. J.S.: helped in study design, survey development and distribution, data analysis. B.J.S. and U.G.N.: helped in survey development, data analysis, manuscript preparation.
The authors declare no conflicts of interest.
Contributor Information
Stacey D. Miller, Email: smiller4@cw.bc.ca.
Maria Juricic, Email: mjuricic@cw.bc.ca.
Nandy Fajardo, Email: nandy.fajardo@cw.bc.ca.
Judy So, Email: judyyjso@student.ubc.ca.
Unni G. Narayanan, Email: unni.narayanan@sickkids.ca.
Kishore Mulpuri, Email: kmulpuri@cw.bc.ca.
REFERENCES
- 1. Bouwhuis CB, Van Der Heijden-Maessen HC, Boldingh EJK, et al. Effectiveness of preventive and corrective surgical intervention on hip disorders in severe cerebral palsy: a systematic review. Disabil Rehabil. 2015;37:97–105. [DOI] [PubMed] [Google Scholar]
- 2. Flynn JM, Miller F. Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg. 2002;10:198–209. [DOI] [PubMed] [Google Scholar]
- 3. Shore BJ, Zurakowski D, Dufreny C, et al. Proximal femoral varus derotation osteotomy in children with cerebral palsy: the effect of age, gross motor function classification system level, and surgeon volume on surgical success. J Bone Joint Surg Am. 2015;97:2024–2031. [DOI] [PubMed] [Google Scholar]
- 4. Rutz E, Vavken P, Camathias C, et al. Long-term results and outcome predictors in one-stage hip reconstruction in children with cerebral palsy. J Bone Joint Surg Am. 2015;97:500–506. [DOI] [PubMed] [Google Scholar]
- 5. Oh CW, Presedo A, Dabney KW, et al. Factors affecting femoral varus osteotomy in cerebral palsy: a long-term result over 10 years. J Pediatr Orthop B. 2007;16:23–30. [DOI] [PubMed] [Google Scholar]
- 6. Noonan KJ, Walker TL, Kayes KJ, et al. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in cerebral palsy: statistical analysis in 73 hips. J Pediatr Orthop B. 2001;10:279–286. [PubMed] [Google Scholar]
- 7. Root L, Laplaza FJ, Brourman SN, et al. The severely unstable hip in cerebral palsy. Treatment with open reduction, pelvic osteotomy, and femoral osteotomy with shortening. J Bone Joint Surg Am. 1995;77:703–712. [DOI] [PubMed] [Google Scholar]
- 8. Barakat MJ, While T, Pyman J, et al. Bilateral hip reconstruction in severe whole-body cerebral palsy: ten-year follow-up results. J Bone Joint Surg Br. 2007;89:1363–1368. [DOI] [PubMed] [Google Scholar]
- 9. Rutz E, Brunner R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop. 2010;30:726–731. [DOI] [PubMed] [Google Scholar]
- 10. Roposch A, Wedge JH. An incomplete periacetabular osteotomy for treatment of neuromuscular hip dysplasia. Clin Orthop Relat Res. 2005;431:166–175. [DOI] [PubMed] [Google Scholar]
- 11. Kulkarni VA Davids JR Ferkul A, et al. post-operative immobilization following hip reconstruction in children with cerebral palsy: practice patterns and associated complications from a prospective multi-center international cohort study [Conference presentation abstract]. Seventy-third Meeting of the American Academy for Cerebral Palsy and Developmental Medicine (AACPDM), Anaheim, CA; 2019. Available at: http://shrinerschildrens.org/wp-content/uploads/2019/08/T-I-SP12-Postop-Immob-Hip-Reconstruction.pdf. Accessed September 15, 2020.
- 12. Miller F, Girardi H, Lipton G, et al. Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop. 1997;17:592–602. [DOI] [PubMed] [Google Scholar]
- 13. Huh K, Rethlefsen SA, Wren TA, et al. Surgical management of hip subluxation and dislocation in children with cerebral palsy: isolated VDRO or combined surgery? J Pediatr Orthop. 2011;31:858–863. [DOI] [PubMed] [Google Scholar]
- 14. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shore BJ, Murphy RF, Hogue GD. Practice management. What should we measure? J Pediatr Orthop. 2015;35:S61–S66. [DOI] [PubMed] [Google Scholar]
- 17. Albrektson J, Kay RM, Tolo VT, et al. Abduction pillow immobilization following hip surgery: a welcome alternative for selected patients. J Child Orthop. 2007;1:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]


