Abstract
Background
The first wave of COVID-19 in South Africa peaked in July, 2020, and a larger second wave peaked in January, 2021, in which the SARS-CoV-2 501Y.V2 (Beta) lineage predominated. We aimed to compare in-hospital mortality and other patient characteristics between the first and second waves.
Methods
In this prospective cohort study, we analysed data from the DATCOV national active surveillance system for COVID-19 admissions to hospital from March 5, 2020, to March 27, 2021. The system contained data from all hospitals in South Africa that have admitted a patient with COVID-19. We used incidence risk for admission to hospital and determined cutoff dates to define five wave periods: pre-wave 1, wave 1, post-wave 1, wave 2, and post-wave 2. We compared the characteristics of patients with COVID-19 who were admitted to hospital in wave 1 and wave 2, and risk factors for in-hospital mortality accounting for wave period using random-effect multivariable logistic regression.
Findings
Peak rates of COVID-19 cases, admissions, and in-hospital deaths in the second wave exceeded rates in the first wave: COVID-19 cases, 240·4 cases per 100 000 people vs 136·0 cases per 100 000 people; admissions, 27·9 admissions per 100 000 people vs 16·1 admissions per 100 000 people; deaths, 8·3 deaths per 100 000 people vs 3·6 deaths per 100 000 people. The weekly average growth rate in hospital admissions was 20% in wave 1 and 43% in wave 2 (ratio of growth rate in wave 2 compared with wave 1 was 1·19, 95% CI 1·18–1·20). Compared with the first wave, individuals admitted to hospital in the second wave were more likely to be age 40–64 years (adjusted odds ratio [aOR] 1·22, 95% CI 1·14–1·31), and older than 65 years (aOR 1·38, 1·25–1·52), compared with younger than 40 years; of Mixed race (aOR 1·21, 1·06–1·38) compared with White race; and admitted in the public sector (aOR 1·65, 1·41–1·92); and less likely to be Black (aOR 0·53, 0·47–0·60) and Indian (aOR 0·77, 0·66–0·91), compared with White; and have a comorbid condition (aOR 0·60, 0·55–0·67). For multivariable analysis, after adjusting for weekly COVID-19 hospital admissions, there was a 31% increased risk of in-hospital mortality in the second wave (aOR 1·31, 95% CI 1·28–1·35). In-hospital case-fatality risk increased from 17·7% in weeks of low admission (<3500 admissions) to 26·9% in weeks of very high admission (>8000 admissions; aOR 1·24, 1·17–1·32).
Interpretation
In South Africa, the second wave was associated with higher incidence of COVID-19, more rapid increase in admissions to hospital, and increased in-hospital mortality. Although some of the increased mortality can be explained by admissions in the second wave being more likely in older individuals, in the public sector, and by the increased health system pressure, a residual increase in mortality of patients admitted to hospital could be related to the new Beta lineage.
Funding
DATCOV as a national surveillance system is funded by the National Institute for Communicable Diseases and the South African National Government.
Introduction
South Africa, a temperate country in the southern hemisphere, had recorded the most COVID-19 cases in Africa as of June, 2021.1 The country has a high burden of non-communicable diseases and obesity, HIV, and tuberculosis. According to the 2016 Demographic and Health Survey, 41% of adult women and 11% of men had obesity, 46% of women and 44% of men had hypertension, and 13% of women and 8% of men had diabetes.2 In 2019, 7·5 million people were estimated to be living with HIV in South Africa, of whom 2·3 million (31%) were not receiving treatment.3 In 2018, 301 000 new cases of tuberculosis were diagnosed in South Africa.4 South Africa has a dual health system with a publicly funded district health system that serves about 84% of the population, and a private health system largely funded by private health insurance schemes.5
South Africa reported its first case of PCR-confirmed SARS-CoV-2 infection on March 5, 2020, and since then has experienced a first wave, which peaked in July, 2020, a larger second wave, which peaked in January, 2021,6 and from June, 2021, has entered the third wave. A new lineage of SARS-CoV-2 detected in Eastern Cape province in September, 2020,7 was reported to be the predominant lineage of initially tested samples in each of the Eastern Cape (154 of 157, 98%), Western Cape (137 of 174, 79%), KwaZulu-Natal (244 of 252, 97%), and Gauteng (126 of 150, 84%) provinces between December, 2020, and February, 2021.8, 9 This lineage, named 501Y.V2 or Beta, contains several mutations that were not identified in SARS-CoV-2 viruses from South Africa before September, 2020. Two of these mutations are within the receptor-binding domain, shown to enhance binding to the human ACE2 receptor.10
Research in context.
Evidence before this study
Most countries have reported higher numbers of COVID-19 cases in the second wave but lower case-fatality risk, in part due to new therapeutic interventions, increased testing, and better prepared health systems. South Africa experienced its second wave, which peaked in January, 2021, in which the variant of concern, SARS-CoV-2 501Y.V2 (Beta), predominated. New variants have been shown to be more transmissible and, in the UK, to be associated with increased admission to hospital and mortality rates in people infected with variant B.1.1.7 (Alpha) compared with infection with non-Alpha viruses. There are currently limited data on the severity of lineage Beta. We did separate literature searches on PubMed using the following terms: “COVID-19”, “wave”, and “mortality”; “COVID-19”, “variant”, and “mortality”; and “COVID-19”, “mortality”, and “trend”. All searches included publications from Dec 1, 2019, to May 5, 2021, without language restrictions. Additionally, we did two literature searches on MedRxiv using the terms “COVID-19”, “wave”, and “mortality”; and “COVID-19”, “variant”, and “mortality” from April 25, 2020, to May 5, 2021, without language restrictions.
Added value of this study
We analysed data from the DATCOV national active surveillance system for COVID-19 admissions to hospital, comparing in-hospital mortality and other patient characteristics between the first and second waves of COVID-19. The study revealed that after adjusting for age, sex, race, comorbidities, health sector, province, and weekly COVID-19 hospital admissions, there was a 31% increased risk of in-hospital mortality in the second wave. Our study also describes the demographic shift from the first to the second wave of COVID-19 in South Africa and quantifies the impact of overwhelmed hospital capacity on in-hospital mortality.
Implications of all the available evidence
Our data suggest that the new lineage (Beta) in South Africa might be associated with increased in-hospital mortality during the second wave. However, the findings should be interpreted with caution because our analysis is based on a comparison of mortality in the first and second wave as a proxy for dominant lineage and we did not have individual-level data on lineage. Individual-level studies comparing outcomes of people with and without the new lineage on the basis of sequencing data are required. We need to conduct surveillance and studies of new lineages to monitor their transmissibility and severity. Our data also suggest that overwhelmed hospital capacity was associated with increased in-hospital mortality during the first and second waves. With South Africa having entered the third wave of the pandemic in June, 2021, we require a combination of strategies to prevent high mortality, to slow the transmission of SARS-CoV-2, and to spread out the peak of the epidemic, which would prevent hospital capacity from being breached, as well as to increase access to vaccination.
Preliminary data suggest that SARS-CoV-2 Beta might be more transmissible than other lineages7, 11 and escape the immune response from preceding infection with earlier SARS-CoV-2 lineages.12, 13 The UK reported increased admission to hospital and mortality rates in people infected with variant B.1.1.7 (Alpha) compared with infection with non-Alpha viruses.14, 15 Data on the severity of lineage Beta are few. Determining the severity of disease during South Africa's second wave with Beta lineage predominance is important to better understand the burden of COVID-19 mortality and effect on health-care services.
We aimed to describe the demographic and clinical characteristics of individuals admitted to hospital with laboratory-confirmed COVID-19 throughout South Africa in the first and second waves, and assess risk factors for in-hospital mortality.
Methods
Study design and participants
We did a prospective cohort analysis of COVID-19 hospital surveillance data in South Africa. We accessed summary data on SARS-CoV-2 cases from national epidemiological reports.16 A secondary data analysis was done of the DATCOV national hospital surveillance database between March 5, 2020, and March 27, 2021. DATCOV is an active surveillance system for COVID-19 admissions, established in March, 2020, which has achieved comprehensive coverage of all hospitals in South Africa that have admitted a patient with COVID-19. As of March 27, 2021, a total of 644 facilities had submitted data on COVID-19 patients admitted to hospital: 393 from the public sector and 251 from the private sector. DATCOV contains data on all individuals who had a positive real-time RT-PCR assay for SARS-CoV-2 or a person who had a positive SARS-CoV-2 antigen test, with a confirmed duration of stay in hospital of one full day or longer, regardless of age or reason for admission. This included patients who had COVID-19 symptoms, were admitted for isolation, acquired nosocomial COVID-19 infection, or tested positive incidentally when admitted for other reasons. The case reporting form was adapted from the WHO COVID-19 case reporting tool and contains the following variables: basic demographic data (age, sex, and race which was self-defined by the patient as Black African, White, Mixed or Indian); exposures such as occupation; and potential risk factors such as obesity, comorbid diseases, and pregnancy status. Socioeconomic variables are not collected. Additional variables included data on level of treatment (ward, high dependency, or intensive care unit), complications, treatment, and outcomes of hospital admission (discharged, transferred to another hospital, or died).
The Human Research Ethics Committee (Medical), University of the Witwatersrand, approved the project protocol as part of a national surveillance programme (M160667).
Procedures
Data collection was either through direct entry onto the DATCOV online platform, or through import of electronic data from health information systems into the database. Data imports contained validation checks to identify data errors. Data management described were done routinely and not for this study.
Case-fatality risk was calculated among individuals with in-hospital outcome (ie, COVID-19 deaths divided by COVID-19 deaths plus COVID-19 discharges, excluding individuals who were still admitted to hospital at the time of analysis).
The wave periods were determined using national hospital admission data. Using the admission date, we defined the incidence risk of admissions as the total number of new admissions divided by the population at risk at the beginning of the observation period (Statistics South Africa mid-year population estimates for 2020 were used).17 The wave periods were defined from the time the country recorded a weekly incidence risk of 5 admissions per 100 000 people at the start of the wave to the same incidence risk at the end of the wave. For the analysis of factors associated with in-hospital mortality, the COVID-19 epidemic was divided into five periods. The first was pre-wave 1 (weeks 10–23 of 2020; March 5–June 6, 2020); the second was wave 1 (weeks 24–34 of 2020; June 7–Aug 22, 2020); the third was post-wave 1 (weeks 35–46 of 2020; Aug 23–Nov 14, 2020); the fourth was wave 2 (week 47 of 2020–week 5 of 2021; Nov 15, 2020–Feb 6, 2021); and the fifth was post-wave 2 (weeks 6–12 of 2021; Feb 7–March 27, 2021). Pre-wave 1 was the period from the start of the epidemic to the start of wave 1, post-wave 1 was the period from the end of wave 1 to the start of wave 2, and post-wave 2 was the time from the end of wave 2 to the end of the analysis period.
The primary outcome was risk factors for mortality, investigating whether wave period was associated with mortality; and the secondary outcome was wave period, exploring the changes in demographic and other characteristics between wave 1 and wave 2.
Statistical analysis
We implemented post-imputation random-effect (on admission facility) multivariable logistic regression models to compare the characteristics of COVID-19 patients admitted to hospital in wave 1 and wave 2, and assess risk factors for in-hospital mortality accounting for wave period. Covariates included were chosen on the basis of biological plausibility and evidence from previous analysis. For the multivariable model comparing wave 1 and wave 2 as outcomes, covariates included were age, sex, race, health sector, and presence of comorbidity, also adjusting for weekly national COVID-19 admissions. The analysis included only data from wave 1 and wave 2, and not the other wave periods. For the multivariable model assessing risk factors for mortality, covariates included were age, sex, race, public or private health sector, and presence of comorbidity, including the wave period, and adjusting for weekly national COVID-19 admissions. In the mortality model, we included all five wave periods (pre-wave 1, wave 1, post-wave 1, wave 2, and post-wave 2). Weekly national COVID-19 numbers of admissions were used as a proxy of burden of COVID-19 cases on the health-care system and divided into four categories: low (<3500), medium (3500–5749), high (5750–7999), and very high (>8000) admissions. Only COVID-19 admissions were included because data on patients admitted with other illnesses were not available.
Obesity was not included in the model due to the high proportion of missing data. As the data can be assumed to be missing at random, for the main analysis, to account for incomplete or missing data on selected variables, we used multivariate imputation by chained equation (MICE—using the mi impute chained command in Stata) and generated ten complete imputed datasets that were used for subsequent analyses. The procedure involves a series of regression models being run, whereby each variable with missing data is modelled conditional upon the other variables in the dataset. Incomplete variables included sex, race, month of admission, and comorbidities. Complete variables included in the imputation process were age, province, health sector (ie, public or private), and in-hospital outcome (ie, discharged alive, or died, with transferred patients excluded from analysis).
A random effect on admission facility was included for all analyses to account for potential differences in the population served and the quality of care at each facility. For each multivariable model we assessed all variables that were significant at p<0·2 on univariate analysis and dropped non-significant factors (p≥0·05) with manual backward elimination. Pairwise interactions were assessed by inclusion of product terms for all variables remaining in the final multivariable additive model. We did a sensitivity analysis to separately assess factors associated with in-hospital mortality among patients admitted in the private and public sectors on the imputed dataset; and a complete case analysis on the unimputed dataset for all variables included in both models. We used the χ2 test to assess the difference in case-fatality risk at the peak of the first and second wave. Additionally, we compared the exponential growth rate of the first and the second wave. We estimated the exponential growth rate (from 5 admissions per 100 000 people at the start of the wave to the wave peak) for each wave using Poisson regression on count of weekly COVID-19 admissions (outcome variable) over time (weekly increases, dependent variable) and assessed the difference in the estimated weekly growth rate through the inclusion of an interaction term of weeks and wave in the model. The statistical analysis was implemented using Stata 15.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
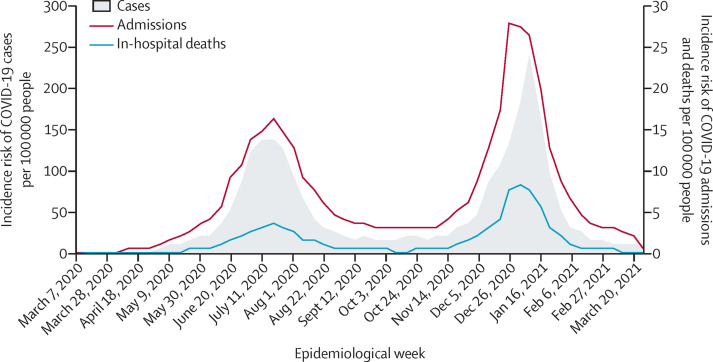
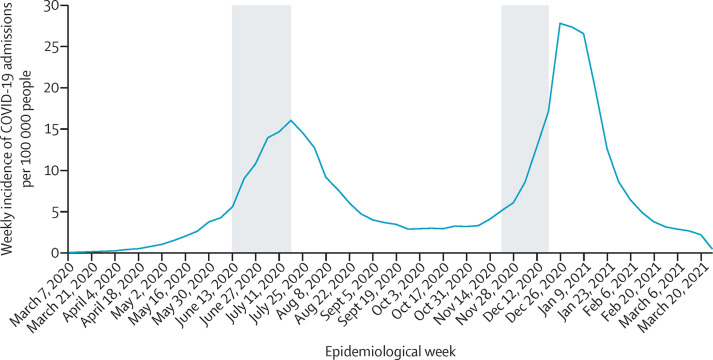
From March 5, 2020, to March 27, 2021, a total of 1 545 431 SARS-CoV-2 cases and 227 932 COVID-19 hospital admissions were reported in South Africa. Two wave periods were identified, and five wave periods defined: pre-wave 1, wave 1, post-wave 1, wave 2, and post-wave 2 (figure 1 ). Following the first wave peak in cases in epidemiological week 28, there was a resurgence beginning in the Eastern Cape province from week 40, followed by all other provinces subsequently, peaking in week 1 of 2021. Peak rates (per 100 000 people) of COVID-19 cases, admissions, and in-hospital deaths in the second wave exceeded the rates in the first wave (COVID-19 cases, 240·4 cases per 100 000 people vs 136·0 cases per 100 000 people; admissions, 27·9 admissions per 100 000 people vs 16·1 admissions per 100 000 people; deaths, 8·3 deaths per 100 000 people vs 3·6 deaths per 100 000 people; figure 2 ).
Figure 1.
Weekly incidence per 100 000 people of COVID-19 admissions by epidemiological week in South Africa, March 5, 2020–March 27, 2021
Dashed lines show the time periods of the first and second waves.
Figure 2.
Incidence of reported SARS-CoV-2 cases, COVID-19 admissions, and in-hospital deaths by epidemiological week of diagnosis in South Africa, March 5, 2020–March 27, 2021
Of the 219 265 COVID-19 patients nationally with a recorded in-hospital outcome (died or discharged), 51 037 died and the in-hospital case-fatality risk was 23·28% across the whole study period. The case-fatality risk at the peak of the second wave in January, 2021 (29·34%, 95% CI 28·95–29·74) was significantly higher than that at the peak of the first wave in July, 2020 (21·80%, 95% CI 21·39–22·22; p<0·0001; table 1 ).
Table 1.
COVID-19 in-hospital case-fatality risk reported by month of admission in South Africa, March 5, 2020–March 27, 2021
| Number who died | Total outcomes | Case-fatality risk (95% CI) | |
|---|---|---|---|
| 2020 | |||
| March | 45 | 400 | 11·25% (8·33–14·76) |
| April | 185 | 1449 | 12·77% (11·09–14·60) |
| May | 1072 | 5787 | 18·52% (17·53–19·55) |
| June | 3698 | 18 209 | 20·31% (19·73–20·90) |
| July | 8335 | 38 226 | 21·80% (21·39–22·22) |
| August | 3707 | 19 671 | 18·85% (18·30–19·40) |
| September | 1314 | 8851 | 14·85% (14·11–15·60) |
| October | 1167 | 7735 | 15·09% (14·30–15·90) |
| November | 2506 | 11 110 | 22·56% (21·78–23·35) |
| December | 10 621 | 39 582 | 26·83% (26·40–27·27) |
| 2021 | |||
| January | 15 264 | 52 019 | 29·34% (28·95–29·74) |
| February | 2380 | 11 940 | 19·93% (19·22–20·66) |
| March | 737 | 4235 | 17·40% (16·27–18·58) |
Data are absolute values (n), unless otherwise indicated.
The time it took from 5 admissions per 100 000 population to 15 admissions per 100 000 population in the first wave was 6 weeks and in the second wave was 5 weeks (figure 3 ). The estimated weekly growth rate from the start to the peak of the first wave was 1·20 (95% CI 1·19–1·20; 20% weekly average incidence risk increase from week to week); and in wave 2 was 1·43 (1·42–1·44; 43% weekly average incidence risk increase from week to week). There was a significantly higher rate of increase in wave 2 (ratio of growth rate in wave 2 compared with wave 1 was 1·19, 95% CI 1·18–1·20).
Figure 3.
Incidence per 100 000 people of COVID-19 admissions by epidemiological week in South Africa, March 5, 2020–March 27, 2021
Shading shows the time period from 5 admissions per 100 000 population to 15 admissions per 100 000 population in the first and second waves.
For multivariable analysis, after adjusting for weekly hospital admissions, the factors more common in individuals admitted to hospital in the second wave were age 40–64 years (adjusted odds ratio [aOR] 1·22, 95% CI 1·14–1·31), and age 65 years and older (aOR 1·38, 1·25–1·52), compared with younger than age 40 years; admissions in individuals of Mixed race (aOR 1·21, 1·06–1·38) compared with White individuals; admission in the public sector (aOR 1·65, 1·41–1·92); and very high weekly admissions (>8000 admissions; aOR 2·31, 1·81–2·95) compared with low weekly admissions (<3500 admissions). The factors less common in the second wave were admissions in Black individuals (aOR 0·53, 95% CI 0·47–0·60) and Indian individuals (aOR 0·77, 0·66–0·91) compared with White individuals; presence of a comorbid condition (aOR 0·60, 0·55–0·67); and medium level of weekly admissions (3500–5749 admissions; aOR 0·80, 0·66–0·96) compared with low weekly admissions (<3500 admissions). We also observed provincial differences between the first and second wave with admissions more likely in Limpopo and less likely in Free State, Gauteng, and North West provinces, compared with the Western Cape province (table 2 ). The sensitivity analysis using unimputed complete case data showed similar associations (appendix p 4).
Table 2.
Univariate and multivariate analysis of factors associated with admission to hospital in the first and second waves in South Africa, March 5, 2020–March 27, 2021
| Percentage of patients in first wave (95% CI) | Percentage of patients in second wave (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI)* | Adjusted OR (95% CI)† | |
|---|---|---|---|---|---|
| Age, years | |||||
| <40 | 24·3% (24·0–24·6) | 20·5% (20·3–20·8) | 1 (ref) | 1 (ref) | 1 (ref) |
| 40–64 | 51·2% (50·9–51·6) | 50·7% (50·4–51·1) | 1·17‡ (1·10–1·25) | 1·29‡ (1·21–1·38) | 1·22‡ (1·14–1·31) |
| ≥65 | 24·5% (24·2–24·8) | 28·7% (28·5–29·0) | 1·39‡ (1·26–1·53) | 1·46‡ (1·32–1·60) | 1·38‡ (1·25–1·52) |
| Sex | |||||
| Female | 55·8% (55·4–56·2) | 55·5% (55·2–55·8) | 1 (ref) | .. | .. |
| Male | 44·2% (43·8–44·6) | 44·5% (44·2–44·8) | 1·01 (0·98–1·05) | .. | .. |
| Race | |||||
| White | 9·2% (8·9–9·4) | 11·6% (11·2–11·9) | 1 (ref) | 1 (ref) | 1 (ref) |
| Black | 78·6% (78·2–79·0) | 68·1% (67·6–68·5) | 0·69‡ (0·61–0·77) | 0·56‡ (0·50–0·63) | 0·53‡ (0·47–0·60) |
| Mixed | 7·1% (6·8–7·3) | 13·6% (13·3–13·9) | 1·52‡ (1·29–1·80) | 1·22‡ (1·07–1·39) | 1·21‡ (1·06–1·38) |
| Indian | 5·2% (5·1–5·4) | 6·8% (6·6–7·0) | 1·03 (0·90–1·18) | 0·79‡ (0·67–0·93) | 0·77‡ (0·66–0·91) |
| Presence of comorbidities | |||||
| No | 39·3% (38·9–39·8) | 45·0% (44·6–45·3) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 60·7% (60·2–61·1) | 55·0% (54·7–55·4) | 0·79‡ (0·71–0·89) | 0·60‡ (0·55–0·66) | 0·60‡ (0·55–0·67) |
| Health sector | |||||
| Private sector | 51·6% (51·2–51·9) | 47·1% (46·8–47·4) | 1 (ref) | 1 (ref) | 1 (ref) |
| Public sector | 48·4% (48·1–48·8) | 52·9% (52·6–53·2) | 1·20‡ (1·02–1·40) | 1·63‡ (1·40–1·89) | 1·65‡ (1·41–1·92) |
| Province | |||||
| Western Cape | 16·5% (16·2–16·8) | 22·4% (22·2–22·7) | 1 (ref) | 1 (ref) | 1 (ref) |
| Eastern Cape | 12·4% (12·2–12·6) | 13·4% (13·2–13·6) | 0·79 (0·59–1·06) | 0·90 (0·66–1·24) | 0·97 (0·71–1·34) |
| Free State | 6·3% (6·1–6·5) | 3·3% (3·2–3·5) | 0·39‡ (0·28–0·55) | 0·49‡ (0·34–0·70) | 0·49‡ (0·34–0·70) |
| Gauteng | 34·9% (34·5–35·2) | 23·3% (23·0–23·5) | 0·49‡ (0·37–0·64) | 0·59‡ (0·44–0·78) | 0·55‡ (0·41–0·74) |
| KwaZulu-Natal | 18·1% (17·8–18·3) | 23·5% (23·3–23·8) | 0·96 (0·72–1·28) | 1·21 (0·89–1·65) | 1·14 (0·83–1·55) |
| Limpopo | 1·9% (1·8–2·0) | 5·2% (5·1–5·4) | 2·00‡ (1·42–2·83) | 2·60‡ (1·87–3·63) | 2·41‡ (1·74–3·34) |
| Mpumalanga | 3·0% (2·8–3·1) | 3·9% (3·8–4·1) | 0·97 (0·66–1·44) | 1·32 (0·91–1·92) | 1·30 (0·89–1·90) |
| North West | 5·6% (5·4–5·7) | 3·8% (3·6–3·9) | 0·49‡ (0·33–0·73) | 0·65‡ (0·43–0·99) | 0·62‡ (0·41–0·95) |
| Northern Cape | 1·4% (1·3–1·5) | 1·1% (1·1–1·2) | 0·59 (0·33–1·06) | 0·60 (0·35–1·04) | 0·62 (0·35–1·07) |
| Weekly national admission number | |||||
| Low (<3500) | 4·7% (4·5–4·9) | 3·0% (2·9–3·1) | 1 (ref) | .. | 1 (ref) |
| Medium (3500–5749) | 26·5% (26·2–26·8) | 13·4% (13·2–13·6) | 0·80‡ (0·65–0·97) | .. | 0·80‡ (0·66–0·96) |
| High (5750–7999) | 19·5% (19·2–19·8) | 14·7% (14·4–14·9) | 1·18 (0·94–1·48) | .. | 1·22 (0·98–1·52) |
| Very high (>8000) | 49·3% (48·9–49·6) | 68·9% (68·7–69·2) | 2·20‡ (1·71–2·85) | .. | 2·31‡ (1·81–2·95) |
For this analysis, the outcome variable was admission to hospital during wave 2 (event) versus admission to hospital during wave 1 (control), and the exposures were the characteristics of patients admitted to hospital. ORs represent the odds of being admitted to hospital in wave 2 among patients in the given exposure category versus the odds of being admitted to hospital in wave 2 among patients in the reference exposure category. OR=odds ratio.
Unadjusted for weekly admissions.
Adjusted for weekly admissions.
Statistically significant estimates.
On multivariable analysis, after adjusting for weekly hospital admissions, we found an increased risk of in-hospital mortality in wave 2 (aOR 1·31, 95% CI 1·28–1·35) and decreased risk in the post-wave 1 period (aOR 0·85, 0·79–0·91), compared with wave 1. Other risk factors for in-hospital mortality included age 40–64 years (aOR 3·17, 95% CI 3·05–3·30), and age 65 years and older (aOR 7·89, 7·58–8·22), compared with younger than age 40 years; male sex (aOR 1·30, 1·27–1·33); Black race (aOR 1·18, 1·10–1·26), Mixed race (aOR 1·16, 1·07–1·26), and Indian race (aOR 1·30, 1·21–1·40) compared with White race; presence of a comorbid condition (aOR 1·67, 1·62–1·72); and admission in the public sector (aOR 1·39, 1·21–1·60). Compared with weeks with low numbers of national hospital admissions (<3500 admissions), there was an increased risk of mortality in weeks with high weekly admissions (5750–7999 admissions; aOR 1·08, 95% CI 1·01–1·15) and very high weekly admissions (>8000 admissions; aOR 1·24, 1·17–1·32). We also observed increased risk of mortality in Eastern Cape, KwaZulu-Natal, Limpopo, and Mpumalanga provinces, compared with the Western Cape province (table 3 ). The sensitivity analysis using unimputed data showed similar associations (appendix p 6).
Table 3.
Univariate and multivariate analysis of factors associated with in-hospital mortality in South Africa, March 5, 2020–March 27, 2021
| Case-fatality risk (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI)* | Adjusted OR (95% CI)† | |
|---|---|---|---|---|
| Age, years | ||||
| <40 | 7·2% (7·0–7·4) | 1 (ref) | 1 (ref) | 1 (ref) |
| 40–64 | 21·7% (21·5–22·0) | 3·75‡ (3·62–3·90) | 3·20‡ (3·08–3·32) | 3·17‡ (3·05–3·30) |
| ≥65 | 41·2% (40·8–41·6) | 9·38‡ (9·03–9·75) | 7·95‡ (7·63–8·28) | 7·89‡ (7·58–8·22) |
| Sex | ||||
| Female | 21·7% (21·5–21·9) | 1 (ref) | 1 (ref) | 1 (ref) |
| Male | 25·3% (25·0–25·5) | 1·32‡ (1·29–1·34) | 1·30‡ (1·27–1·33) | 1·30‡ (1·27–1·33) |
| Race | ||||
| White | 21·6% (20·8–22·3) | 1 (ref) | 1 (ref) | 1 (ref) |
| Black | 23·6% (23·4–23·8) | 0·79‡ (0·74–0·84) | 1·19‡ (1·11–1·27) | 1·18‡ (1·10–1·26) |
| Mixed | 22·6% (21·9–23·3) | 0·89‡ (0·83–0·96) | 1·17‡ (1·08–1·27) | 1·16‡ (1·07–1·26) |
| Indian | 23·9% (22·9–24·8) | 1·07 (0·99–1·14) | 1·31‡ (1·22–1·41) | 1·30‡ (1·21–1·40) |
| Presence of comorbidities | ||||
| No | 15·7% (15·4–15·9) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 28·9% (28·6–29·1) | 2·23‡ (2·17–2·30) | 1·67‡ (1·62–1·72) | 1·67‡ (1·62–1·72) |
| Health sector | ||||
| Private sector | 18·7% (18·5–19·0) | 1 (ref) | 1 (ref) | 1 (ref) |
| Public sector | 27·5% (27·2–27·7) | 1·99‡ (1·70–2·33) | 1·39‡ (1·21–1·60) | 1·39‡ (1·21–1·60) |
| Province | ||||
| Western Cape | 21·5% (21·1–21·9) | 1 (ref) | 1 (ref) | 1 (ref) |
| Eastern Cape | 32·6% (32·0–33·1) | 2·32‡ (1·79–3·01) | 2·14‡ (1·70–2·69) | 2·16‡ (1·72–2·71) |
| Free State | 22·3% (21·6–23·1) | 1·14 (0·83–1·56) | 1·29 (0·98–1·70) | 1·29 (0·98–1·69) |
| Gauteng | 20·0% (19·7–20·4) | 0·76‡ (0·60–0·98) | 1·08 (0·87–1·34) | 1·07 (0·86–1·33) |
| KwaZulu-Natal | 24·4% (24·0–24·8) | 1·45‡ (1·13–1·86) | 1·50‡ (1·21–1·87) | 1·48‡ (1·19–1·84) |
| Limpopo | 30·0% (29·0–31·0) | 1·98‡ (1·44–2·72) | 1·78‡ (1·34–2·35) | 1·74‡ (1·32–2·30) |
| Mpumalanga | 26·7% (25·7–27·6) | 2·27‡ (1·62–3·20) | 2·16‡ (1·61–2·92) | 2·14‡ (1·59–2·86) |
| North West | 14·6% (13·9–15·2) | 0·73 (0·49–1·09) | 0·93 (0·66–1·30) | 0·92 (0·65–1·30) |
| Northern Cape | 19·9% (18·6–21·3) | 1·32 (0·84–2·08) | 1·48 (0·99–2·21) | 1·48 (0·99–2·20) |
| Wave period | ||||
| Pre-wave 1 | 18·0% (17·2–18·7) | 0·79‡ (0·75–0·84) | 0·88‡ (0·83–0·93) | 0·99 (0·91–1·07) |
| Wave 1 | 20·8% (20·5–21·1) | 1 (ref) | 1 (ref) | 1 (ref) |
| Pre-wave 2 | 16·4% (16·0–16·9) | 0·70‡ (0·68–0·73) | 0·76‡ (0·73–0·79) | 0·85‡ (0·79–0·91) |
| Wave 2 | 27·8% (27·5–28·1) | 1·34‡ (1·31–1·37) | 1·37‡ (1·33–1·40) | 1·31‡ (1·28–1·35) |
| Post-wave 2 | 18·6% (17·9–19·2) | 0·80‡ (0·76–0·84) | 0·90‡ (0·85–0·95) | 1·02 (0·95–1·09) |
| Weekly national admission number | ||||
| Low (<3500) | 17·7% (17·3–18·0) | 1 (ref) | .. | 1 (ref) |
| Medium (3500–5749) | 21·0% (20·6–21·5) | 1·25‡ (1·20–1·29) | .. | 0·99 (0·93–1·05) |
| High (5750–7999) | 23·0% (22·5–23·5) | 1·44‡ (1·39–1·50) | .. | 1·08‡ (1·01–1·15) |
| Very high (>8000) | 26·9% (26·6–27·1) | 1·74‡ (1·69–1·79) | .. | 1·24‡ (1·17–1·32) |
OR=odds ratio.
Adjusted OR including wave periods.
Adjusted for weekly admissions.
Statistically significant estimates.
In the sensitivity analyses, we also separately analysed predictors of in-hospital death in the private sector and public sector (appendix p 8). Both analyses showed increased mortality in the second wave compared with the first wave, and similar trends and associations to those seen in the main combined analyses.
Discussion
The incidences of COVID-19 cases, admissions, and in-hospital deaths in the second wave exceeded the incidences in the first wave in South Africa. The weekly incidence of COVID-19 admissions also increased at a faster rate. Additionally, we found increased mortality in the second wave, partly explained by more admissions in older individuals and in the public sector, and by higher volumes of hospital admissions. Although we did not have individual-level data on infecting lineage for cases included in this analysis, the fact that Beta has been the predominant lineage in the second wave8, 9 suggests that the residual 31% increased mortality could possibly be associated with the new lineage. Preliminary findings in the UK show increased case-fatality risk for individuals infected with variant Alpha, with mortality hazard ratio estimates ranging from 1·35 to 1·91.18 However, these were a series of matched case-control and population cohort studies comparing variant and non-variant cases,18 while ours was an unmatched analysis with wave as a proxy for lineage.
On the basis of global trends, in-hospital COVID-19 mortality in South Africa might have been expected to decrease in the second wave. In most countries, the second wave of COVID-19 had a higher number of cases but lower mortality.19, 20, 21, 22, 23, 24 Improved outcomes during the second wave in these countries were probably a result of introduction of interventions such as remdesivir,25 dexamethasone,26 high-flow oxygen,27 and increased use of thromboprophylaxis,28 as well as non-pharmacological treatments such as placing the patient in the prone position.20 Other possible suggestions for the lower case-fatality risk observed in the second wave in many countries are changes in demographic characteristics of cases, and the cohort or harvest effect whereby a large number of older people and those with health conditions (the clinically vulnerable groups) are likely to have died in the first wave.22, 29, 30 Additionally, improved testing capacities in the second wave could have resulted in more mild cases being identified;22, 23, 31, 32 and health-care systems in many countries might have been better prepared in the second wave, offering timely treatment of severe cases.20, 22, 30
The shifts in trend of admissions and deaths between the first and second wave in South Africa could also be explained by the different context of the epidemic when compared with other countries. South Africa experienced the first wave 2 months later than did other countries and benefited from time for hospital preparedness and learning from other countries' experiences and the use of steroids, which were shown to improve clinical outcomes.33 The country was less well prepared for the second wave, which was not predicted to have started as early as it did.
Regarding the multivariable analysis, an increased risk of mortality with admission load in South Africa was observed. In weeks with very high weekly admissions (>8000 admissions), mortality increased by 24%, compared with weeks with low weekly national admissions (<3500 admissions). The observed increase in mortality of patients admitted to hospital at the peaks of the first and second waves reflects in part increasing pressure on the health system. In South Africa, the rising number of hospital admissions in the second wave required care to be rationed to those patients highest on triage lists.1 Studies have shown that a strain on hospital capacity has been associated with increased mortality in non-pandemic settings.34 COVID-19 mortality in hospitals appeared to be higher when the incidence of COVID-19 in the community was high or increasing35, 36 and when the number of hospital admissions were highest.19 Additionally, the rapid escalation in cases resulted in hospital resource constraints affecting outcomes.37 Furthermore, strains on critical care capacity were associated with increased COVID-19 mortality.37, 38 In Brazil, a strained health-care system with regional differences in access to resources, compounded by overburdened hospital systems, contributed to greater in-hospital mortality.39 Even the perception of a strained health system can lead to excess mortality from COVID-19 and other conditions, because individuals might avoid seeking care until their clinical condition has deteriorated or might die at home.40 Although we reported 51 037 in-hospital COVID-19 deaths, in the same time period the South African Medical Research Council reported 151 963 excess deaths above the numbers of deaths reported in previous years, estimating that at least 85% of the excess natural deaths are attributable to COVID-19.41 These data suggest that there might have been large numbers of individuals not accessing health care and dying at home. An important focus of the COVID-19 response in preparation for future waves should be efforts to strengthen health system readiness and prepare hospitals and critical care services with additional surge capacity.
In the second wave, individuals who had comorbidities and were of Black or Indian race were less likely to be admitted to hospital than they were during the first wave; while individuals who were older, of Mixed race, and presenting in public health-care facilities were more likely to be admitted. Similar findings of more admissions in older individuals less likely to have comorbidities in the second wave were reported from analysis of an individual hospital in the Eastern Cape.42 These differences observed between the first and second waves could have contradictory effects on mortality, with more admissions in older people and the public sector likely to result in increased mortality, and less admissions in individuals with comorbidities and of Black, Mixed, and Indian race (who have higher mortality) likely to result in reduced mortality.
The higher proportion of older people admitted in the second wave in South Africa could be due to changes in preventive behaviour and transmission dynamics or increased susceptibility to the new lineage. Across Europe, North America, the Middle East, and southeast Asia, a shift towards younger cases with fewer comorbidities and less severe disease has been observed and was considered to be due to public health measures to reduce transmission in clinically vulnerable groups.22, 23, 30, 43, 44, 45 The lower proportion of reported comorbidities in the second wave, even accounting for the age distribution of patients, could reflect differences in clinician practice, survival bias, or changing manifestation in individuals without underlying illness. It could also be due to variation in reporting of comorbidities, with underascertainment of other medical conditions at the peak of the wave more likely when hospitals were busy.
Differences in race could reflect Black individuals being more greatly affected in the first wave due to historical differences in socioeconomic status and housing conditions, which is supported by data showing higher seroprevalence in Black individuals than in other race groups in South Africa.46 It could also be due to greater aversion to seeking health care by Black, Mixed, and Indian groups in the second wave, as described in other settings during the pandemic.47 Some explanations for higher transmission and mortality in Black and Asian people have been suggested in the literature, including their over-representation in front-line occupations; higher incidences of multigenerational households; differences in access to health care; and public health messaging regarding prevention, early diagnosis, and treatment of COVID-19 being less effective in these groups, resulting in later presentation.19
The increased COVID-19 mortality in the public sector is in keeping with well described differences in the level of resourcing, standard of care, and outcomes between the public and private health sectors in South Africa.48 Provincial-level differences might reflect differences in testing, health seeking behaviour, health systems, clinical practice, and underlying population characteristics. Such regional differences have also been observed in other countries such as Brazil.39 The findings identify provinces less likely to have admissions in the second wave (Free State, Gauteng, and North West), suggesting that they might have earlier resurgences or larger third waves. Before the country entered the third wave, these provinces were prioritised for support by the national government, to be on alert and to ensure strong prevention and control responses.
Notably, even after adjusting for older age, higher admissions in the public sector, and higher hospital loads, a significant independent residual increase in in-hospital COVID-19 mortality was observed in wave 2, which was not accounted for by other factors.
Strengths of this study include the use of comprehensive electronic health record data on all COVID-19 hospital admissions at all 644 public and private hospitals in the country, thus minimising selection or surveillance bias and maximising generalisability. The study includes a diverse patient population, complete study outcomes, and a lengthy period of investigation of 13 months, with in-hospital follow-up until occurrence of discharge or death.
The allocation of wave time periods, categorisation of weekly hospital admissions, and risk factor analyses were performed at a national level. However, the timing of the waves differed by provinces and districts within provinces, and the national categories might not fit all provinces perfectly. Sensitivity analyses by sector found similar results to the national-level analysis, and analyses at provincial and district level in the Western Cape (unpublished) and at individual hospital level42 have confirmed moderately increased mortality in the second wave.
The high proportion of missing data, particularly for fields such as race (32%) and comorbidities (22%) is a limitation of a routine national surveillance system. Obesity was excluded from the analysis due to 75% of individuals having missing data. There are also no routine data available on socioeconomic status because this is not collected in DATCOV.
Additional limitations of this analysis were the lack of individual-level lineage type data, and possible residual confounding because we could not adjust for several factors. We adjusted for COVID-19 admissions but were not able to adjust for weekly hospital admission volumes for people under investigation and non-COVID-19 admissions. We were not able to adjust for differences between the first and second wave related to the level of national restrictions or lockdowns, and to individual preventive behaviours. The analysis includes only in-hospital deaths and any differences between the two waves in the proportions of patients who did not or could not access care and those who died outside of hospital are not accounted for in the analysis. There have been changes in treatment protocols with better COVID-19 treatment regimens including steroid use and high-flow oxygen. These have probably decreased mortality rates as the epidemic progressed. The numbers of hospitals reporting to DATCOV increased in October, 2020, and while all hospitals were required to back-capture historic admissions, they might not have done this completely, leading to reporting bias with possible under-reporting in the first wave. The characteristics of those patients who died in the first wave (such as old age, comorbidities, and obesity) might have differed from the survivors and those who were not infected with SARS-CoV-2. Therefore, the characteristics of patients admitted to hospital in the second wave might be different to those of the first wave as a result of survival bias. Thresholds for hospital admission might also have changed over time.
Although much of the increased mortality in the second wave was explained by more admissions in older individuals and in the public sector, and by increasing pressure on the health system, the finding of a residual 31% increase in mortality even after accounting for these factors suggests that the new lineage (Beta) might have contributed to increased in-hospital mortality during the second wave. However, the findings should be interpreted with caution because our analysis is based on a comparison of mortality in the first and second wave as a proxy for dominant lineage and we did not have individual-level data on lineage. Individual-level studies comparing outcomes of people with and without the new lineage on the basis of sequencing data are needed. As new variants continue to emerge across the globe, surveillance to identify them and studies to determine their transmissibility and severity are important. To prevent high mortality in the third wave, we advocate a so-called flattening the curve approach, which requires a combination of strategies to slow the spread of COVID-19, to spread out the peak of the epidemic, which would prevent hospital capacity from being breached.31
Data sharing
The dataset analysed for the manuscript is available upon reasonable request. The data dictionary is available on request to the corresponding author: waasilaj@nicd.ac.za
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
We thank the National Department of Health for implementation support, the National Institute for Communicable Diseases for support and oversight, and the DATCOV team. We also acknowledge the Network for Genomics Surveillance in South Africa for sequence frequencies, and laboratories and clinicians throughout the country reporting cases and hospitalisation data. We also thank the health professionals in all public and private sector hospitals and hospital groups submitting data to DATCOV, who are acknowledged and listed as the DATCOV author group. DATCOV as a national surveillance system, is funded by the National Institute for Communicable Diseases and the South African National Government. No additional funding was obtained towards the completion of this analysis and the development of this manuscript.
Contributors
WJ and LO contributed to the literature search. WJ, CC, M-AD, LO, and CM contributed to the study design and refining the methods of analysis. CM, ST, CC, and WJ contributed to data analysis, and creation of tables and figures. WJ, CC, ST, and CM contributed to data interpretation and initial drafting of the manuscript. WJ drafted the initial manuscript and all other coauthors contributed scientific inputs equally towards the interpretation of the findings and the final draft of the manuscript. WJ, CM, LO, and ST have verified the underlying data. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication.
Contributor Information
DATCOV author group:
Shaina Abdullah, Fiona Abrahams, Vincentius Adams, FHIMA ADNANE, Sonia Adoni, Dieketso Melitta Adoons, Veronique Africa, Dr Aguinaga, Susan Akach, Prisha Alakram Khelawon, George Aldrich, Olatunde Alesinloye, Mathale Biniki Aletta, Mametja Alice, Tebogo Aphane, Moherndran Archary, Felicity Arends, Shireen Arends, Munonde Aser, T Asmal, Mohammed Asvat, Theunis Avenant, Muvhali Avhazwivhoni, Magnolia Azuike, Johanna Baartman, Dlava Babalwa, Johan Badenhorst, Miranda Badenhorst; Badenhorst, Bianca Badripersad (CEO), Lalihla Badul, M Bagananeng, Mncedisi Bahle, Liezl Balfour, Liezl Balfour, TC Baloyi, S Baloyi, Tinyiko Baloyi, Tshepo Mpho Baloyi, Thokozani Banda, Shimon Barit, Nicole Bartsch, Junaid Bayat, Siyabulela Bazana, Marlene Beetge, Marlene Beetge, Nosindiso Bekapezulu, Rammala Belebele, Phala Bella, Zanenkululeko Belot, Lindi Gladys Bembe, Sonja Bensch, Gishma Beukes, Karla Bezuidenhout, Themba Bhembe, N.A BIKISHA, Ben Bilenge, Leesa Bishop, Baphamandla Biyela, Cyntheola Blaauw, Mark Blaylock, Nicola Bodley, Power Bogale, Sibongile Bokolo, Stefan Bolon, Mary Booysen, Eldereze Booysen, Lia Boretti, Paula Borges, Millicent Boshoga, Natasha Bosman, Lucinda Bosvark, Nicky Botes, Adele Botha, CHANTALL BOTHA, Jana Botha, MANDLAKAYISE IRVIN BOTHA, Alet Botha, Janet Bradbury, Zandisile Breakfast, Maria Breed, Molele Brenda, Moshito Brice, Jolene Britz, Amanda brown, Ms T Buchanan, Thozama Bucwa, Crystelle Burger, Ziyanda Busakwe, Nosiviwe Bushula, Zinhle Buthelezi, Dumsile Buthelezi, Thubelihle Buthelezi, Mpumelelo Basil Buthelezi, Fundiswa Lidwina Buthelezi, Nadia Bux, Christoff Buys, Anneline Buys, Ernestina Caka, Armando Sanchez Canal, Sithole Caroline, Monrick Casper, Shannon Cawood, Oratile Cebisa, Nothando Cele, Sboniso Cele, Sthembile Goodness Cele, Mkhacani Chauke, Pinkie Chauke, Nevil Chelin, Xiaohui Chen, Venmalla Chetty, Kerisse Chetty, Christinah Cheu, Vindana Chibabhai, Takudzwa Chirima, Mantwa ChisaleMabotja, CHARITY CHIVENGE, Ngoasheng Choene, Mbali Nosisa Choko, Martin Choshi, Sabbir Chowdhury, Anastacia Christoforou, S.L.S Chuene, T.S Chueu, Dale Cilliers, Vanessa Cilliers, Marcel Claassen, Jeané Cloete, Chantelle Coelho, Chantelle Coelho, Carol Coetzee, Hans Jurgens Coetzee, Christine Coetzee, Marelize Coetzee, Dane Coetzer, Sizwe Coka, Mr M Colane, Herkulaas Combrink, Songezo Conjwa, Colleen Contrad, Faith Cornelissen, Leezelle Cronje, Christine Crouse, Moshai D.A, Ms Mahabane D.I, Tshidi Dabi, Ziyanda Dandala, Ziyaad Dangor, Gildenhuys Daniel, Ngwana Daniel, Alfred Daumas, Madelein Dauth, Mongalo David, Wayne Davids, Nozuko Daweti, Halima Dawood, Wandisa Dayile, B DE BRUIN, Karin De Klerk, Tanya De la Rosa, Marice de Nysschen, Marie De vos, Darien De Wet, Mohith Debising, Darshan Deenadayalu, Babalwa Dekeda, Mofokeng Desiree, Annelise Deysel, Abram Dhlamini, Makgethwa Dhlala Diala, Mathapelo Diale, Bella Diketane, Nosisa Dingani, Siyabonga Diniso, Lesego Diphatse, Anele Diya, Zihloniphile Dladla, Nompumelelo Dladla, Mlungisi Dladla, Patience Dladla, Baphilie Dlamini, NONHLANHLA DLAMINI, Linda Dlamini, Nonzwakazi Dlamini, Wendy Dlamini, Ncomeka Dlamini, Siyabonga Dlamini, Nicodemus Dlamini, Lebohang Dlamini, Motshedise Dlamini, Babalwa Christine Dlava, Phikiwe Dlova, Lindiwe Dlozi, Maenetja Doreen, Vumile Doyi, Athini Doyi, Belinda Du Plessis, Johanna Aletta du Plessis, Mr. Eddie du Plessis, Nicolette du Plessis, Karin du Plessis, Briette du Toit, Narissa du Toit, Jabulile Dube, Athayanda Dubula, Msomi Duduzile, Sechaba Duiker, Unati Bongile Duma, Kholiwe Duma, Kella Dunne, Kholeka Dyantyi, Avile Dyantyi, Simphiwe Dyasi, CHAUKE DYONDZO, Phelisa Dyubhele, B.J Dywili, Letitia Edwards Edwards, Madie Eksteen, Tersia Ellis, Tia Ellis, Glenda Emmerson, Theusia Enslin, ODIMULA EPULE, Lana Erasmus, Mathonsi Erick, Lerato Etsane, Shimange Eunice, Zanele Fani, Mariette Ferreira, K.L Finger-Motsepe, Fabion Floris, Tseko Fobo, Keresemetse Fokotsane, Duduzile Emmelda Fokwana, Genevieve Marion Fords, Juanita Fortein, Christine Fouche, Rulandi Fourie, Andrew Frean, Ludwig Fredericks, Wandile Funda, Kabelo Funjwa, Martha Futhane, Amanda Futuse, Dora Gabaediwe, Nonhlanhla Gabuza, Janycke Galant, Zanele Gama, Thobile Gano, Emma Cora Gardiner, Henri Gastrow, Kelly Gate, Ben Gaunt, Rikhotso Gavaza, Thapelo Gayi, Nkosinathi Gcakasi, Nomusa Gcobo, Leon Geffen, S Geldenhuys, Jenny George, Martha Gerber, Zolisa Getyengana, Nkululo Gigi, Radha Gihwala, Mitchell Gilliland, Zandile Gloria, Elitia Glover, Ellen Gokailemang, Suseth Goosen, Maria Gopane, Thandazile Gosa - Lufuta, Bernadett Gosnell, Sharleen Gouws, Christina Govender, Raksha Govender, Pearl Govender, Sally Govender, Christina Govender, Roxanne Govender, K Govender, Mrs Savie Govender, Rashika Govinden, Luphumlo Gqabuza, Nomthandazo Gqaji, Maneo Gqetywa, Caroline Green, Nathan Green, Neera Green, Hendrik Grobler, Pamela Groenwald, Daniel Grootboom, Beatrice Gumede, Nomonde Gumede, Simphiwe Gumede, Simphiwe Gumede, Slindile Gumede, Ntombikayise Gumede, Zenande Gumede, Thandiswa Gxotiwe, Makhubela H.L, Nonhlanhla Hadebe, Skhumbuzo Hadebe, Christos Halkas, Ansie Hamer, Ebrahim Hamida, Juan Hammond, Sumayia Haniff, Annelise Hare, lorinda Hattingh, Thenjiwe Hendricks, Philip-George Henecke, Brends Henly-Smith, Glynis Herselman, Ansie Heymans, Chantel Heyns, Golekane Hlabahlaba, Lucky Hlabangwane, Simango Hlamarisa, Ntokozo Hlanzi, Hlengiwe Hlela, Katlego Hlokwe, Thembinkosi hlongwa, Anele Hlongwana, Themba Hlubi, Tozama Hobo, Nare Nathaniel Hopane, Mariska House, Catharina Hudson, Marinda Huysamen, Jezreen Indheren, Samantha Ingle, Gavin Isaacs, TS Thekiso Isaacs, Maringa Itumeleng, Karien J van Rensburg, Saloshni Jackson, Neziswa Jacob, Burton Jacobs, Tshireletso Jacobs, Gugulethu Jacobs, Mesadi Jaftha, Zimkhitha Jaji, Sibusiso Jali, Gcobisa James, Gillian January, Andiswa Jeke, Laurent Jeremiah, LS Jeremiah, Mubeen Jhetam, Maureen John, Chuene John, Thandiwe Jola, Yolande Jonas, Anovick Jonas, Amilcar Juggernath, eileen kaba, Venetia Kabo, Disebo Kadi, Karabo Kaizer, Moshaya Peter Kambule, Lorraine Kapp, Tshepo Kau, Nchabeleng Keneth, O Kgabi, Tebogo Audrey Kgafela, Vincent Kgakgadi, Isabella Kgaswe, Tsholofelo Kgathlane, Vuyelwa Julia Kgetha, Mmaselloane Kgomojoo, MR B Kgoro, Christinah Kgosiemang, Gloria Kgosiencho, Stephen Khambula, Ariffa Khan, Refemetswe Khanare, Ncamsile Khanyase, Nokwethemba Khanyile(Data Capturer), Fillip Kharatsi, Simangele Khawula, Themba Khohlakala, Letitia Khomo, Isabel khoza, Sinethemba Khoza, Nombulelo Khukule, Busisiwe Khumalo, Tracy Khumalo, Zinhle khumalo, Vuyelwa Khumalo, Delisile Khumalo, Lebohang Khumalo, Boitumelo Khumalo, Thuli Khumalo, Gugu Khumalo, Bongiwe Khuzwayo, Thembhelihle Khuzwayo, Hennie Kidson, Jesne Kistan, Gugu Klaas, Marilyn Klassen, Josehine Koeberg, Marizel Koen, Simphiwe Koena, Ina Kok, Imraan Kola, Karabo Kolokoto, Ramachandra Konar, Dr Kotsedi, Jaline Kotze, MARTINS KOUPIS CDS, Sr Helen Kritzinger, Marlize Kruger, Henk Kruger, Tlangelani Kubayi, Thabisile Kubeka, Nonjabulo Kubheka, Melusi Kubheka, Sibusiso Clifford Kubheka, Erol Kubheka, Monica Kumalo, Thulani Kunene, Siphilile Candy Kunene, Yvette Kunneke, R.P KUPA, Rachel Kutama, Nompumelelo Kwakwazi, Lwanele Kweyama, Maureen Labuschagne, Marina Labuschagne, Prabha Lakshman, Prabha Lakshman, Lungelo Lamani, Thembela Lamani, Naomi Langa, Khangelani Langeni, Aphelele Langeni, Nwabisa Hazel Langeni, Gena Langeveldt, Anchen Laubscher, Laetitia Le Roux, Magagane Leah, Collen Lebea, Sello Lebea, Viyella Phumla Cynthia Lebenya, Lorraine lebogang, PK LEBOHO, Chantel Lee, Kelebogile Rejoice Lefakane, Zandile Legoabe, Patrick Lekala, Motsitsi Lekhoaba, Tanki Shadrack Lekunutu, Galaletsang Lerefolo, Mrs N Letebele, Tsepo Patric Lethoba, Emission Letlalo, Ofentse Letlhage, D.S.V Letshufi, Dineo Fiona Letsoalo, Seleka Jones Letsoalo, Pennelope Letsoalo, Getrude Letwaba, Sobekwa Linda, Katleho Lipholo, Sabata Litabe, Harsha Lochan, Linda Lomax, Francina Lombaard, Elmarie Loots, Ariana Lourens, Ariana Lourens, Celeste Louw, Rianna Louw, Zikhona Lubambo, Msebenzi Moises Lubambo, Gregory Ludada, Michael Lukas, Thembela Lungu, Nomvume Lupindo, Emmah Lusenga, Happiness Luthuli, Zoleka Sylvia Luvuno, Sr Gwangwa M.H, Mustafa Maarman, Buyisiwe Mabaso, Cynthia Mabaso, Morena Mabitle, Grace Mabogoane, Kgakgamatso Mabone, Rueben Mabuza, Velaphi Mabuza, Mogantla Madiseng, Thobile Madlala, Mashooase Madolo, Thabiso Madonsela, Lesetsa Madubanya, Amukelani Maepa, Namhla Mafumana, Caroline Mafumo, Pumeza Magadla, Viscah Magale, Nompumelelo Magaqa, Oberholzer Magda, Rakgoale Magdeline, Tswai Maggie, Bongeka Maginxa, Cathrine Maite Magoba, Caroline Magongwa, AGRETIA MAGUBANE, Agretia Ntombizodwa Magubane, R Magwai, Padmini Mahabeer, Elsie Mahadulula, Lungiswa Mahanjana, Amy Maharaj, Qedusiza Mahlambi, Yvonne Mahlangu, Lerato Mahlangu, Ntombifikile Mahlangu, Makhosazana Mahlangu, Mahlatsi Mahlangu, Penelope Mahlasela, Thosago Mahlatse, Regina Mahlobo, Dikhing Mahole, Adam Mahomed, Mapeu Debora Mahubane, Peter Mahume, Lehlogonolo Maifo, Vincent Maimane, Petunia Maimele, Phakoe Maine, Patricia Senyanyathi Mainongwane, Nomalungisa Majamani, Amahle Majozini, Noluthando Makalima, Nomfundo Makam, Khanyisa Makamba, R Makan, Mashiane Makarapa, Malesela Makgahlela, Mogoiwa David Makgisa, Makgoba Makgomo, MA Makgopa, Mabone Makhalema, Lindokuhle Lizo Makhanya, Philile Valentia Makhanya, Tolerance Makharaedzha, Nathi Makhathini, Elizabeth Makhesi, Cinile Makhubela, Nkululeko Freedom Makhunga, Nomalinge Makhupula, RR Makhura, Rangwato Makola, Zingisa Makuba, Asanda Makubalo, Lonwabo Makumsha, George Makuya, Levy Mmachuene Malaka, Themba Malangeni, ML MALATJI, Pelonomi Malebana-Metsing, Malek Malek, Luthando Malevu, Luthando Malevu, Juanita Malgas, Dimakatso Malgas, Paul Makgasane Malope, Monyeki Malose, Katekani Maluleke, Kato Mambane, Nthabiseng Mamorobela, Kukami Manamela, Tshepo Manana, Sathiel Maneto, Aron Kabelo Manganye, Pheto Mangena, Anna Mangoale, TINOTENDA FLORENCE MANGOZHO, Pariva Manickchund, Zandisile Mankayi, Arthur Manning, Kelebogile Manyaapelo Manyaapelo, Tabea Manyane, Zoliswa Manzana, Milton Manzini, Busisiwe Mapasa-Dube, Siboniso Maphumulo, Ntombifuthi Maphumulo, Sindy Maponya, Khomotso Mumsy Maponya, Napjadi Maponya, Lami Maqubela, Lizeka Maqubela, Vuyo Maqungo, Marisa Marais, Chantal Marais, Nondumiso Maramba, Annelize Mare, Madumetsa Maredi, Afikile Martins, Johanna Marule, Refilwe Marumo, NN Masakona, KEDIBONE VINCENTIA MASEHLA, Eric Maseko, Tshilidzi Maselesele, Mojalefa Maselo, M Maseloa, M.E Masemola, Thembi Masemola, Bella Mashaba, James Mashangwane, Mantebele Mashao, Shalom Mashego, Lerato Mashele, Ester Mashiane, Joyce Mashibini, J Mashilo, Tumi Mashiloane, Charity Mashishi, Ngazibini Mashiyi, Khomola Mashudu, aluwani masindi, Caroline Maslo, Nduduzo Masondo, Dumisile Masuku, Cry Matamela, Mirriam Matandela, Nontokozo Mathabela, T Mathabi, Keitumetse Mathe, Mathabo Mathebula, Catherine Mathebula, Mdungazi Andres Mathebula, Nqobizwe Mathenjwa, Jane Mathibe, Lebohang Mathibela, MAKWELA MATHILDA, Khakhu Mathiva, Mokgadi Alinah Mathobela, Fikile Pearl Mathonsi, KP Mathonsi, Katlego Mathosa, Noluvo Matiwane, Emma Matjeke, Bella Matjiane, Thabang Matjila, Sr Chidi Matlala, Petlo Matome, Nolusindiso Matoti, C. Matseliso, Dineo Matsemela, Phumeza Matsha, Gaalebale Prudence Matshediso, Motsumi Matshediso, Esther Matshela, Bongeka Mavuma, Pearl Mavundla, Nomthandazo Mavuso, Lovender Mawasha, Rebecca Mawelela, Nelisiwe Mazibuko, Phumlani Mazibuko, Lindiwe Mazubane, Bavumile Mbanjwa, Ayanda Mbasa, Nosimilo Mbatha, ZANELE MBATHA, Rudolph Zenzele Mbatha, Gift Mbedzi, Tatenda Trevor Mbizi, Khumbulani Mbonambi, Nondumiso Mboniswa, Nomfanelo Mbonisweni, Jody Mbuilu, Siyabonga Mbulawa, Zama Mbutho, Natasha Mbuzi, Nonkululeko Mchunu, Cyprian Mchunu, Nokuzola Mchunu, Masesi Thandeka Mchunu, Vuyokazi Mciteka, Solly Mdaka, Neho Mdakane, Siyabonga Mdediswa, Melusi Mdima, Nozipho Mdima Masondo, Siviwe Mdindana, Ntombizikhona Mdleleni, Sibusiso Mdletshe, Gcobisa Precious Mdoda, Ntombi Mdolo, Anele Mdontsane, Ruchikas Mehta, Philile Rittah Memela, Masande Methuse, Keatlaretse Metshile, Pheliswa Metuse, Anton Meyer, Gavin Meyer, Cameron Meyer, Sisonke Mfazwe, Andiswa Mfecane, Bongeka Mfecane, Nelisiwe Mfeka, Busisiwe Mgaga, Thandiwe Portia Mgauli, Thembekile Mgedezi, Vuyokazi Mgedezi, Kalipile Mgevane, Bongni Mgiba, Babalwa Mgoduka, PATRICK MHLABA, Zeldah Mhlaba, Ntombizodwa Mhlanga, Vangile Mhlinza, Nokuthula Mhlongo, sibongiseni Mhlongo, Unamandla Mhlotshana, Mabaso Mikateko, Helena Minnie, Karen Mintoor, Bongi Miyeni, Mabelane MJ, Rosy Mjethu, Gloria Mkhize, Mvuselelo Mkhize, Ntokozo Siyabonga Mkhize, Victoria Mkhize, Nomkhosi Mkhize, Nokuthula Mkhize, Mathini Mkhwanazi, Nolwandle Mkile, Kholofelo Mkise, Nokwandiso Mkiya, Pearl Mkongi, Pearl Mkongi, Mnonopheli Mkungeka, Hlomile Mlahleki, Nolukholo Mlibali, Sakhumzi mlungwana, Jonas Mmachele, Mashatole Mmateka, Molebatsi Mmokwa, Thembisa Mmutlane, Zanele Olive Mndebele, nonhlanhla mngomezulu, Noluthando Millicent Mnguni, Pumza Mngunyana, Nomxolisi Mngunyana, Ntombebongo Mngxekeza, ZENZELE MNISI, Hlengiwe Precious Mnqayi, PHUMZILE MNQAYI, Thabiso Mntungwa, Siya Mnyaka, Ntombikayise Mnyakeni, Vuyani Mnyamana, Nomzingisi Mnyipika, Koena Moabelo, Mmakgoshi Alseria Moatshe, Jennifer Mochaki-Senoge Mochaki-Senoge, Sharon Moche, Tebello Mocwagae, Koeikantse Modibane, Tebogo godfrey Modimoeng, Obakeng Modisa, Itumeleng Modisane, Olebogeng Modise, Makaepeaa Flovia Modjadji, Sharon Modupe, Maja Moeketsi, Ntswaki Moeketsi, Kereditse Kingsley Moeng, Naledi Nthabiseng Mofamere, Samuel Mofokeng, Thabo Mofokeng, Jonas Mofomme, VICKY MOGAKANE, Lehlohonolo Mogale, Audrey Mogapi, Thomas Mogashoa, Mphaka James Mogatla, Kgaladi Mogoale, Dikeledi Maggie Mohajane, Nkuba Mohapi, Mthoamihla Mohatsela, Irene Mohlala, Daphney Mohlala, Mpho Mohlamonyane, Bonolo Millord Mohutsiwa, Selemela Moipone, Tshepang Moisi, Nelly Mojalefa, Vuyo Moji, Buhle Mokangwana, Matloa Mokgabo, Manaka Mokgaetji, Jane Mokgaotsi, Neo Theodore Mokgoro, Thalitha Mokhatla, Lerato Lovedalia Mokhele, Sheila Mokhema, Mamoya Mokoena, Mojalefa Mokoena, Lleka Mokome, Cynthia Mokone, Ipeleng Mokono, Thabiso Mokonyama, Josiah Mokori, Dolores Mokuena, Danny Mokumo, Oddy Mokwena, Kgaogelo Mokwena, Kgantshi Sam Mokwena, Lebogang Mokwene, Thato Elliott Molate, Ditoche Molebalwa, Boingotlo Molefe, KGOPA STANLEY MOLEHE, Kgomotso Moleme, Sarah Moliane, FANYANA MOLOI, Retshepile Joseph Molorane, Glenda Tsholanang Molotsi, Lerato Molukanele, Joy Monareng, Thapelo Moncho, Modiadie Monica, Refilwe Monnane, Andile Monqo, Neo Montewa, Kgalalelo Montsioa, Reitumetse monyaki, Masekhobe Jeanett Monyane, Lipson Monyela, Yudeshan Moodley, Kriesen Moodley, Kaira Moodley, Boitumelo Donald Mooka, Prea Moonsamy, Simmi Moopanar, David Moore, Lineo Mophethe, Tshegohatso Moremedi, Kealeboga Moremong, nthangeni morgan, Egma Moripa, Lulamile Morris, Me. A.M. Mosala, Thabo Mosana, Alice Mosase, Yolanda Mose, Maponya Mosehlo, Mothusi Moseki, Mojalefa David Moshabe, Mbulelo Moshani, Pelisa Moshani, Ledwaba Mosima, Ezrom Mosima, M.P Mosoma, Lebohang Motaung, Mokete Motaung, Thozama Charmain Motaung Xhama, Purine Khethiwe Motha, Lerato Motimele, Boitumelo Motimeng, Shirley Motladiile, otsile Motlhabane, Joshua Motlhamme, Mandla Motloba, Kagiso Motse, Sophia Motshegoa, Edward Moutlana, Irma Mouton, Zanele Moya, Nomonde Moyake, Maja MP, Jenny Mpete, Luamba Meltha Mpfuni, Seputule Mphahlele Mphahlele, Mashadi Mphake, Ephraim Letlhogonolo Mphanya, Mashudu Mphaphuli, Tebogo Chwene Mphela, MS Mpontshane, Thabile Mqotyana, Babalwa Mqungquthu, Noluthando Busane Msane, Malusi Mseleku, Sibusiso Msibi, Mancele Msibi, Thulisile Msibi, Siyabonga Linda Msibi, Clement Nhlanhla Msiza, Lungelo Msomi, Mandlenkosi Mtatambi, Thembisa Mthathambi, December Mthembu, Nhlahla Mthembu, Fezile Mbali Mthembu, Lungiswa Mthembu, Nompumelelo Petunia Mthethwa, Khulekani Mthimkhulu, Lungani Percival Mthuli, Ashley Mthunzi, Xolani Sydney Mtolo, Nomonde Precious Mtolo, Linda Mtshali, Neliswa Mtwa, Fezeka Mtyobile, Kanyisa Mtyobile, Mpfariseni Mudau, Magwabeni Muemeleli, Isaac Mulaudzi, Rebecca Mulaudzi, Mhlelekedzeni Mulaudzi, Dakalo Rejoyce Muligwe, Blessing Muponda, Mmbangiseni Stella Mushadi, M Mushid, Konanani Muthaphuli, J Muthavhine, Mpho Muthika, Samkelisiwe Mvelase, Vusi Mvelase, LAURENT KAYUMBA MWEHU, Thabile Myaka, Magriet myburgh, Zimkhitha Mzamo, Fezeka Mzawuziwa, Mfundo Lunga Mzini, Oscar Mzizana, Ntokozo Mzobe, Thokozile Mzobe, Zamaswazi Mzobe, Mtimkulu Mzwandile, Fathima Naby, KESHNEE NAICKER, Pregashnie Naicker, Saroja Naicker, Pershen Naicker, Saiyen Virgil Naicker, RIA NAIDOO, Sam Naidoo, Mergan Naidoo, KAMALAMBAL NAIDOO, Aroomugam Naidoo, Sivuyile Naku, Firdose Nakwa, Masoga Nancy, Rita Nathan, Maritsa Naude, Gcobisa Ncaza, Aviwe Ncaza, Relebohile Ncha, Yanelisa Ncoyini, Snothile Ncube, Mrs Ndaba, VUSUMUZI NDABA, Mmapula Ndaba, Siziwe Ndawonde, Ziphozihle Ndevu, NONHLANHLA FAITH NDHLOVU, Simphiwe Ndima, Sindisiwe Ndlela, Thobsile P Ndlela, Nobuhle Ndlovu, Nwabisa Ndlovu, Virginia Dipuo Ndlovu, Sombekhaya Ndlumbini, Khululiwe Nduli, Priscilla Nontokozo Nduli, Michael Ndwambi, Jeremy Nel, Rina Nel, Lizelle Nel, Ntsundeni florah Nemanashi, Usinkhangwe Nyaphophi Nemudivhiso, Joyce Nemutavhanani Nemutavhanani, Jabu Nene, Xolani Nene, David Netshilonga, Rendani Netsianda, Charmaine Newton, Vuyo Leroy Ngalo, Ncumisa Ngani, Thabisa Monica Ngcakaza, Thamela Ngcobo, Trulove Nonhlanhla Ngcobo, Richards Ngcobo, Gcinile Ngcobo, Guguletu Ngcobo, Thozama Ngetu, Pinkie Ngewu, Tshepo Ngobeni, Providence Ngobeni, Khanyisile Ngobeni, Prudence Ngobeni, Thembisile Ngobese, Tracy Ngomane, Nolusindiso Ngondo, Nokukhanya Ngubane, Sithembiso Ngubane, Ntombizodwa Praxedise Nguse, Tholakele Ngwane, Elizabeth Ngwasheng, Siphamandla Ngwenya, Gugu Ngwenya, Nomthandazo Ngwenya, Themba Ngwenya, Eva Ngwenya, Zintlanu Ngxola, Tshegofatso Nhabe, Jabulile Nhlabathi, Ishmael Nhlangwana, Sithembile Nhlapo, Matlala nick, Vicky Niemand, Carina Nienaber, Louise Nix, Chumisa Njikelana, Masiza Njomi, Lucia Nkabinde, M NKABINDE, Boitumelo Nkabiti, Gugu Nkabule, Mankopodi Nkadimeng, Nonkanyiso Nkanjeni, Palesa Portia Nkatlo, Bongani Nkewana, Audrey Nkhwashu, Ngokoana Nkoana, Mmathapelo Nkoane, M Nkogatse, Fezile Nkomo, Ntando Nkomo, Nontobeko Nkonyane, Sydney Nkosi, Ntombikayise Nkosi, Phumzile Nkosi, Ntombifuthi Nkosi, TINTSWALO NKOSI, ML Nkosi, Godfrey Nkosi, Amukelani Nkosi, Fikile Vinoliah Nkosi, Mbali Nkosi, Nomcebo Lucia Nkosi, Siphokazi Nkosi, Amanda Nkuhlu, Phumzile Nkumane, Malebo Nkuna, Wendy Nkwakwha, Sesi Noge, Elizabeth Nolte, Peko Nomawabo, Malibongwe Nombita, Nandipha Nophale, Jeanetta Nothnagel, Bongiwe Novokoza, Zanele Nqaphi, Thobekile Nqondo, Siphokazi Nqwelo, Nkoana NS, Sindiswa Ntabeni, Mr Ntabeni, mawethu Ntampula, Mthutuzeli Ntebe, MOKWABO NTELA, Hezekiah Ntimbane, Xolisa Ntintsilana, Patrick Ntleki, Zanele Ntobela, Bandile Ntombela, Bandile Ntombela, Zamaswazi Ntombela, Khonelihle Zandile Ntombela, Praisegod Samkelo Thobani Ntombela, Lindiwe Ntonintshi, Dipuo Ntseane, Thobeka Ntseane, Xolelwa Ntsham, Mbalenhle Ntshele, Amanda Ntshewula, Zinzi Ntsoko, Athini Ntsoto, Nomsa Ntuli, Nokwazi Ntuli, Nomvula Ntuli, Andrew Diffar Ntuli, Faith Ntuli, Margrit Nurnberger, Ntsikelelo Nxala, Sithandiwe Nxasane, Mr Thanda Nxumalo, Xolani Nyathi, Nontobeko Nyawula, Nhlakanipho Nzama, Maila Nkuneng Obed, Florence Ogwal, Maureen Olifant, Mr B Oliphant, Monota Olive, Kagisho Olyn, Raymond Omoighe, Phumeza One, Ratombo Oscar, Nkuna Owen, Mailula P, Nalini Padayachee, Vasaily Padayachy, Ntombizakhe Pakade, Mosiuoa Palime, Jane Palisa, Arifa Parker, Lesenyeho Parkies, Andy Parrish, Nilesh Patel, Anastasia Pather, Mkhombo Tsakani Patience, Marisa Patzke, Akhumzi Pawuli, Ntandokazi Pelako, Phaswana Sibasa Penrose, Litha Peppeta, Santosh Pershad, Makheda Pertunia, Nkuna Pertunia, Dane Perumal, Mongameli Peter, Justin Peters, Vatiswa Petlane, Harideen Petrus, Kgomotso Phahladira, Matebesi John Phakisa, R Phale, Livhuwani Phathela, Sekate Daniel Phillip, Beverly Phiri, Mapule Precious Phiri, Thapelo Phokane, Frank Phokoane, Moele Pholosho, Sekoro Phooko, Sekodi Geoffrey Phooko, Maponya Phutiane, Faiza Pillay, Melanie Pillay, Sayuri Pillay, CR Pillay, Zikhona Plaatjie, James Pootona, Samantha Potgieter, Marius Potgieter, Mulaudzi Mulatedzi Precious, Paul Janus Pretorius, Hans Prozesky, Mokhethi Pule, Jayshina Punwasi, Dot Putzier, Lutho Qankqiso, Siphokazi Qebedu, Phozisa Qhola, Ntombesithathu Qotoyi, Sipho Victor Qotso, Zanele Qwabe, Helena Rabie, Phoebe Rabothata, Christina Rachoene, Mteteleli Radana, Maria Radebe, Dr. Valentino Radebe, Nonkululeko Radebe, Ella Radinne, Sherly Raduvha, Shamintha Raghunath, Claudine Rajagopaul, Mary Rakgwale, Malumbete Michael Ralethe, Kenneth ralimo, Motlalepule Ramafoko, Maduvhahafani Ramagoma, Charlotte Raman, Dr Ramavhuya, Molly Rambally, Nivasha Ramdeen, Tanusha Ramdin, Sharita Rameshwarnath, Yeishna Ramkillawan, Ramotlou, Faith Rampedi, Vijayluxmi Rampersad, Avhashoni Ramuima, Noluthando Ranone, Mabohlale Portia Rapasa, Mpharoane rapelang, Nika Raphaely, Lesiba Rashokeng, Caroline Rashopola, Tebogo Ratau, M RATAU, Mpfariseni David Ratshili, Elmari Rautenbach, Rofhiwa Ravele, Johannes Reachable, Peta Mmalahla Rebecca, Kessendri Reddy, Andrew Redfern, Robertha Reed, Mumsy Rees, Dr Reji, Gary Reubenson, Veena Rewthinarain, Paul Rheeder, Nkonayani Rhulani, Mufamadi Richard, J.S Rikhotso, Shatimone Beverley Rikhotso, Lavhelani Ndivhaleni Robert, Noncedo Roto, Gideon Ruder, Kapil Rugnath, Lizette Ruiters, Mina Ruiters, Sue Russell, Lynn Ruwiza, Molokoane RY, Mandy Saaiman, Emmanuel Sabela, Lerato Sadiq, Litha Saki, HYPPOLITE SALAMBWA, Menitha Samjowan, Nazlee Samodien, Rakgolele Samuel, Fakudze Sandile, Cekuse Sanelisiwe, Mandlankosi Sani, Simangele Sawuka, Lelani Schoeman, Magriet Scholts, Ronel Schroder, Mamotetekoane Sebalabala, Selwalenkwe Collet Sebati, Jacoline Seboko, Wilheminah Sebuthoma, Annah Segami, Ruth Segokotlo, MR Sehloho, Khutjo Seisa, Antony Sekgobela, Monica Sekhosana, John Sekonyela, Mpho Sekoto, Naledi Sekulisa, Mokgadi Vanessa Sekwadi, Lebogo Selaelo, Johannes Selatlha, Kgomotso Selekolo, William Selfridge, Lucy Semenya, Ivy Sengakane, Masabata Sengata, Petronella Sentle, Malebo Seoketsa, Pratheesha Seonandan, Thomas Mambushi Serumula, Nkululeko Setheni, Refiloe Setlale, Tumediso Setlhodi, Barbara Setlhodi, Robert Setloghele, Aarthi Sewpersad, Ryan Sewpersadh, Phumlile Shabalala, Owen Shabangu, Kungesihe Shabangu, Harriet Sbonangaye Shabangu, Doctor Thokozani Shabangu, Clifford Shadi, Hasifa Shaik, Tseliso Shale, Qedani Shandu, Nomvelo Shandu, Ntswaki Marcia Shange, Abongile Shenxane, A Sherriff, Sebenzile Shezi, Thenjiwe Shezi, Scally Shihangule, Cheyeza Shikwambana, Lungisani Shoba, Kamogelo shokane, Nora Sibande, Lydia Sibeko, Xolani Sibeko, Zanele Sibiya, Mncedisi Sibiya, Sphamandla Sibuta, Thembakazi Sifumba, Sipho Sigcau, Lutho Sigila, Kayakazi Sihentshe, Bongani Sihlangu, Daisy Sikhakhane, Shaun Nhlanhla Sikhakhane, Mbali Siko, Sipho Sikonje, Khumbulekile Simanga, Nomsa Simango, Thulisile Simela, Ntombikayise Simelane, Sashah Singh, Marjorie Singh, Mrs Ragani Singh, Shash Singh, Anita Singh, Hitekani Sithole, Senzekile Sithole, Ntokozo Danielle Sithole, Koketso Maxwell Sithole, Jonnie Situma, Annie Sivraman, Katekani Siwela, Nonqubela Siyewuyewu, Maweya Sizeka, Nonceba Siziba, Andrew Skhosana, Khanyisile Skhosana, RORISANG SKHOSANA, Tandiwe Skoko, Sunet Slabbert, Ntombela Smangaliso, Christine Smedley, Lydia Smit, Natassia Smit, Lizelle Smit, Michelle Smit, Fasie Smith, Lizzie Smith, Sunell Smith, Cassius Smith, Stefan Smuts, Ayanda Sofe, Khobane Solomon, LJ Solomon, chauke Sombani, RICHARD SONGCA, Anga Sontamo, Supriya Soorju, Zubenathi Sopazi, Brian Soqasha, Bongiwe Sosibo, Ntsika Sotsaka, Mandy Soula, Simon Spoor, Sarah Stacey, Asanda Stali, Mutele Mmboniseni Stephina, Myra Steup, Sinoxolo Steven, AW Stevens, Vincent Stevens, Dewald Steyn, Bianca Steyn, Pat Stocks, Henk Stolk, Alida Stoltz, Renate Strehlau, Anneke Stroebel, Loraine Strydom, Jean-Marie Strydom, Anton Strydom, Ursula Strydom, Midhu Sunnyraj, Nwabisa Swana, Winnie Swanepoel, Suzan Swanepoel, Elsie Swartbooi, Estley Swartz Swartz, Casandra Syce, Shihambi T.E, Joyce Tabane, NE Tabane, Mrs Tawana, Ntene Tebello, Siphosetu Wiseman Tembe, Samantha Terblanche, Ntombifuthi Thabede, Nkhumeleni Thabelo, Sibusiso Thabethe, Lekhanya Thabo George, Keorapetse Thare, Makofane Thebogo, Lerato Thekiso, Lloyd Theko, Celimphilo Zandi Themba, Danie Theron, Henda Theron, Ilze Theron, Thandiwe Thingathinga, M.M THLABADIRA, Dikeledi Thoka, Zanele Thokwana, Gustav Thom, Mamphot Joel Thubakgale, Theodora Thwala, P Thys, Monethi Tieho, Matodzi Timothy, Ndlovu Tintswalo, Babalwa Tivana, Molefi Tladi, Bongiwe Tokota, Simthandile Toni, Ariel Torres, Mande Toubkin, Marinda Tsatsi, Khanyisile Tshabalala, Nozibele Tshamase, Gontse Tshefu, Makgoga Tshegofatjo, Given Tshikomba, Thapelo Tshilo, Lerato Tshira, S.T Tshirado, Maipfi Tshisikule, G Tsoke, N TSOKE, Alatha Tsoko, Mosele Tsotetsi, SANDEVA TSUBELLA, Noxolo Tuswa, Maipato Tutse, Nomayenzeke Tutu, Sphephelo Twala, Nhlanhla Twala, Simphiwe Twala, John Ubisi, Tefo Unathi, A Van Aswegen, Marietjie van der Merwe, Trudie van der Merwe, Patience van der Plank, Elmarie van der Spuy, Linda Van Der Westhuizen, Adele Van Der Westhuizen, Talana van der Westhuizen, Mene van der Westhuyzen, Thea Van Dyk, Ingrid van Heerden, Ryno van Jaarsveld, Ryno van Jaarsveld, M Van Lill, Heidi van Niekerk, Ben van Niekerk, Amanda van Rensburg, Judy van Schallwyk, Zeitschke Yarnrich Van Sensie, Magda van Vuuren, Cloete van Vuuren, Olga Funiswa Vandu, Mandisa Vane, Lucia VanZyl, Ebrahim Variava, Mariam Veerus, Nokhwezi Velapi, Sebina Veleko, Z. Velezantsi, Retha Venter, Corlia Vergottini, Corlia Vergottini, Inga Vermeulen, Liabara Lufuluvhi Vidah, Bongani Vilakazi, Treasure N Vilakazi, Mbalenhle Precious Vilakazi, Karen Viljoen, Werner Viljoen, Karen Viljoen, Zuretha Volschenk, Angelo Vos, Matlala VV, Jacques Walters, Kate Webb, John Welsh, D WESSELS, Judy Wheller, Fundile White, Priscilla White, Carmen Whyte, Ansie Willemse, Sape William, Daniel Williams, Kamielah Williams, Mercia Williams, Anne Williamson, Cherade Wilson, Boipelo Wolff, Michelle Wray, Ntombizonke B Xaba, Thabang Jabulani Xaba, Thanks Xiniwe, Mtshali Xoliswa, Funokwakhe Xulu, Gibson Xulu, Sandlakazi Yam, NM Zakhura, Mashela Zareloa, Sive Zinto, Dyibeni Zinziswa, Lulamile Ziselo, Zakhele Zitha, Emmanuel Zitha, Anele Zokufa, Innocent Zondi, Sikhumbuzo Bernard Zondi, Sbuyi Zondi, Thulani Zondi, Wandiswa Zongola, Liesl Zühlke, Zandile Zulu, LUNGELO ZULU, Thandeka Zulu, Slindili Zulu, Nkosinathi Zulu, Angel Zuma, precious Zungu, Pamela Zungu, Melusi Zungu, Priscilla Zungu, Bongo Lihle Zwakala, Antonia Zwane, Promise Zwane, Muziwendoda Zwane, Hlengiwe Priscila Zwane, and Nomgcobo Zwane
Supplementary Material
References
- 1.Africa Center for Strategic Studies Analyzing Africa's second wave of COVID-19. 2021. http://africacenter.org/spotlight/analyzing-africas-second-wave-of-covid-19/
- 2.Statistics South Africa SADHS: South African Demographic and Health Survey 2016: Key Indicator Report. 2016. https://www.statssa.gov.za/publications/Report%2003-00-09/Report%2003-00-092016.pdf
- 3.UNAIDS Country Factsheet South Africa. 2019. https://www.unaids.org/en/regionscountries/countries/southafrica
- 4.WHO . World Health Organization; Geneva: 2019. Global tuberculosis report. [Google Scholar]
- 5.Maluleke R. Statistics South Africa; Pretoria: 2019. Inequality trends in South Africa. A multidimensional diagnostic of inequality. [Google Scholar]
- 6.National Institute for Communicable Diseases COVID-19 sentinel hospital surveillance update, week 53. 2021. https://www.nicd.ac.za/wp-content/uploads/2021/01/NICD-COVID-19-Weekly-Sentinel-Hospital-Surveillnace-update-Week-53.pdf
- 7.Tegally H, Wilkinson E, Giovanetti M. Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. medRxiv. 2020 doi: 10.1101/2020.12.21.20248640. published online Dec 22. (preprint). [DOI] [Google Scholar]
- 8.National Institute for Communicable Diseases Dominance of the SARS-CoV-2 501Y.V2 lineage in Gauteng. 2021. https://www.nicd.ac.za/wp-content/uploads/2021/01/Dominance-of-the-SARS-CoV-2-501Y.V2-lineage-in-Gauteng-South-Africa-1.pdf
- 9.GISAID Network for Genomics Surveillance in South Africa sequence frequencies. https://www.gisaid.org/hcov19-variants/
- 10.Greaney AJ, Starr TN, Gilchuk P. Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell Host Microbe. 2021;29:44–57. doi: 10.1016/j.chom.2020.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearson CAB, Russell TW, Davies NG, Kucharski AJ, Edmunds WJ, Eggo RM. Estimates of severity and transmissibility of novel South Africa SARS-CoV-2 variant 501Y.V2. 2021. https://cmmid.github.io/topics/covid19/reports/sa-novel-variant/2021_01_11_Transmissibility_and_severity_of_501Y_V2_in_SA.pdf
- 12.Wibmer CK, Ayres F, Hermanus T. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. Nat Med. 2021;27:622–625. doi: 10.1038/s41591-021-01285-x. [DOI] [PubMed] [Google Scholar]
- 13.Cele S, Gazy I, Jackson L. 2021. Escape of SARS-CoV-2 501Y.V2 variants from neutralization by convalescent plasma. Nature. 2021;593:142–146. doi: 10.1038/s41586-021-03471-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davies NG, Jarvis CI, Edmunds WJ, Jewell NP, Diaz-Ordaz K, Keogh RH. Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7. Nature. 2021;593:270–274. doi: 10.1038/s41586-021-03426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iacobucci G. COVID-19: new UK variant may be linked to increased death rate, early data indicate. BMJ. 2021;372:n230. doi: 10.1136/bmj.n230. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Communicable Diseases COVID-19 Weekly Epidemiology Brief, week 12. 2021. https://www.nicd.ac.za/wp-content/uploads/2021/04/COVID-19-Weekly-Epidemiology-Brief-week-12-2021.pdf
- 17.Statistics South Africa Statistical release: mid-year population estimates 2020. 2021. http://www.statssa.gov.za/publications/P0302/P03022020.pdf
- 18.Horby P, Huntley C, Davies N. NERVTAG paper on B.1·1.7 severity. 2021. https://www.gov.uk/government/publications/nervtag-paper-on-covid-19-variant-of-concern-b117
- 19.Navaratnam AV, Gray WK, Day J, Wendon J, Briggs TWR. Patient factors and temporal trends associated with COVID-19 in-hospital mortality in England: an observational study using administrative data. Lancet Respir Med. 2021;9:397–406. doi: 10.1016/S2213-2600(20)30579-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Horwitz LI, Jones SA, Cerfolio RJ. Trends in COVID-19 risk-adjusted mortality rates. J Hosp Med. 2021;16:90–92. doi: 10.12788/jhm.3552. [DOI] [PubMed] [Google Scholar]
- 21.James N, Menzies M, Radchenko P. COVID-19 second wave mortality in Europe and the United States. Chaos. 2021;31 doi: 10.1063/5.0041569. [DOI] [PubMed] [Google Scholar]
- 22.Fan G, Yang Z, Lin Q, Zhao S, Yang L, He D. Decreased case fatality rate of COVID-19 in the second wave: a study in 53 countries or regions. Transbound Emerg Dis. 2021;68:213–215. doi: 10.1111/tbed.13819. [DOI] [PubMed] [Google Scholar]
- 23.Saito S, Asai Y, Matsunaga N, Hayakawa K, Terada M, Ohtsu H. First and second COVID-19 waves in Japan: a comparison of disease severity and characteristics. J Infect. 2021;82:84–123. doi: 10.1016/j.jinf.2020.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jalali SF, Ghassemzadeh M, Mouodi S. Epidemiologic comparison of the first and second waves of coronavirus disease epidemics in Babol, North of Iran. Caspian J Intern Med. 2020;11(suppl 1):S544–S550. doi: 10.22088/cjim.11.0.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beigel JH, Tomashek KM, Dodd LE. Remdesivir for the treatment of Covid-19—final report. N Engl J Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horby P, Lim WS, Emberson JR. Dexamethasone in hospitalized patients with Covid-19—preliminary report. N Engl J Med. 2020;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guy T, Creac'hcadec A, Ricordel C. High-flow nasal oxygen: a safe, efficient treatment for COVID-19 patients not in an ICU. Eur Respir J. 2020;56 doi: 10.1183/13993003.01154-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Contou D, Fraissé M, Pajot O, Tirolien J, Mentec H, Plantefève G. Comparison between first and second wave among critically ill COVID-19 patients admitted to a French ICU: no prognostic improvement during the second wave? Crit Care. 2021;25:3. doi: 10.1186/s13054-020-03449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG. Second versus first wave of COVID-19 deaths: shifts in age distribution and in nursing home fatalities. Environ Res. 2021;195 doi: 10.1016/j.envres.2021.110856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burgess S, Smith D, Kenyon JC, Gill D. Lightening the viral load to lessen COVID-19 severity. BMJ. 2020;371 doi: 10.1136/bmj.m4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iftimie S, López-Azcona AF, Vallverdú I. First and second waves of coronavirus disease-19: a comparative study in hospitalized patients in Reus, Spain. PLoS One. 2021;16 doi: 10.1371/journal.pone.0248029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates—an ecological analysis of 65 countries. J Inf Secur. 2020;81:e98–e99. doi: 10.1016/j.jinf.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mccarthy K, Tempia S, Kufa T. The importation and establishment of community transmission of SARS-CoV-2 during the first eight weeks of the South African COVID-19 epidemic. SSRN. 2021 doi: 10.2139/ssrn.3792114. published online Feb 26. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guise JM. The association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med. 2017;32:686–696. doi: 10.1007/s11606-016-3936-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asch D, Sheils NE, Islam MN. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181:471–478. doi: 10.1001/jamainternmed.2020.8193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8:e480. doi: 10.1016/S2214-109X(20)30068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bravata DM, Perkins AJ, Myers LJ. Association of intensive care unit patient load and demand with mortality rates in US department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Network Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gupta S, Hayek SS, Wang W. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180:1–12. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ranzani OT, Bastos LSL, Gelli JGM. Characterisation of the first 250 000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9:407–418. doi: 10.1016/S2213-2600(20)30560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madahar P, Wunsch H, Jha P, Slutsky AS, Brodie D. Trends in COVID-19-related in-hospital mortality: lessons learned from nationwide samples. Lancet Respir Med. 2021;9:322–324. doi: 10.1016/S2213-2600(21)00080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.South Africa Medical Research Council Report on weekly deaths in South Africa. 2021. https://www.samrc.ac.za/reports/report-weekly-deaths-south-africa
- 42.Maslo CI, Messina A, Laubscher A. COVID-19: a comparative study of severity of patients hospitalized during the first and the second wave in South Africa. medRxiv. 2021 doi: 10.1101/2021.05.11.21257033. published online May 11. (preprint). [DOI] [Google Scholar]
- 43.Boehmer TK, DeVies J, Caruso E. Changing age distribution of the COVID-19 pandemic—United States, May–August 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1404–1409. doi: 10.15585/mmwr.mm6939e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Doidge JC, Mouncey PR, Thomas K. Trends in intensive care for patients with COVID-19 in England, Wales, and Northern Ireland. Preprints. 2020 doi: 10.20944/preprints202008.0267.v1. published online Aug 11. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Venkatesan P. The changing demographics of COVID-19. Lancet Respir Med. 2020;8:e95. doi: 10.1016/S2213-2600(20)30461-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sykes W, Mhlanga L, Swanevelder R. Prevalence of anti-SARS-CoV-2 antibodies among blood donors in Northern Cape, KwaZulu-Natal, Eastern Cape, and Free State provinces of South Africa in January 2021. Res Sq. 2021. published online Feb 12. (preprint). [DOI]
- 47.Czeisler MÉ, Marynak K, Clarke KEN. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rispel L, Shisana O. In: South African Health Review 2019. Moeti T, Padarath A, editors. Health Systems Trust; Durban: 2019. Achieving high-quality and accountable universal health coverage in South Africa: a synopsis of the Lancet National Commission Report; pp. 69–80. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset analysed for the manuscript is available upon reasonable request. The data dictionary is available on request to the corresponding author: waasilaj@nicd.ac.za