Abstract
This study sought to validate the applicability of the mandarin Tinnitus Evaluation Questionnaire (TEQ), a brief score method administered by clinicians to quantify the tinnitus severity.
A descriptive observational questionnaire study in regard to psychometric properties and practicability was conducted with a total of 414 primary tinnitus outpatients, in which 173 of 414 patients completed the follow-up after receiving an intervention based on the tinnitus educational counseling and the life-style adjustment guidance. For quantifying the tinnitus severity, the TEQ and other 2 self-report questionnaires, Tinnitus Handicap Inventory and visual analog scale, were administered on patients’ first-visit and follow-up. With the psychometric analysis, we evaluated the performance of TEQ in tinnitus management, including distinguishing patients with varying severity and detecting the treatment-related outcome.
At the first visit, the TEQ showed an excellent inter-rater reliability (Pearson correlation, 0.97, P < .01), a good internal consistency reliability (Cronbach's α, 0.79), and an acceptable convergent validity (Pearson correlation, 0.78 with the Tinnitus Handicap Inventory; 0.62 with a single-question visual analog scale, P < .01). In detecting the treatment-related change, a large effect size of TEQ verified a sensitive responsiveness. After estimating the test-error, a 2-point reduction (2/21) of the TEQ was recommend to be considered a reference outcome indicator for the effective intervention.
Even though the TEQ is scored by clinician, it can reflect the clinical features of tinnitus patient. Flexible and simple assessing process makes it a practical tool for patient intake, intervention selection, and outcome measurement.
Keywords: clinician-administered, outcome measurement, psychometric properties, self-report, tinnitus assessment
1. Introduction
Tinnitus is the perception of sound in the absence of an external sound source.[1] Studies in various areas have shown that the prevalence of tinnitus lasting more than 5 minutes is approximately 11.9% to 30.3%.[2] At present, China lacks a nationwide epidemiological survey of tinnitus. Reports for local areas have revealed that the prevalence of tinnitus is approximately 14.5%.[3] Despite the high prevalence of this disorder, tinnitus patients often accompany with different subjective experiences and cognitions, and not all patients whose quality of life is affected by tinnitus will seek the same medical intervention.[4,5] Therefore, current studies suggest that tinnitus classification and individualized tinnitus management are essential.[4] However, as is the case for many subjective symptoms, tinnitus treatment-related studies lack an objective method to quantify outcome.[1,6,7]
Self-report questionnaires are now commonly used as tinnitus assessment tools.[1,8] The score of scale provides researchers with a quantified reference for the patient's intake evaluation and the outcome measurement, which is helpful for individualized interventions.[6] In the past decades, several dozens of self-report questionnaires in different languages are available[7]; however, at present, there is no single questionnaire that is widely accepted as a standardized instrument to quantify tinnitus.[1,7] In China, tinnitus patients usually tend to seek for medical interventions from otologists. The large number of tinnitus patients makes it hard to implement the individualized intervention. Patient-doctor interviews, containing the history-taking and the questionnaire assessment, are time-consuming in the management of outpatients. Simple and reliable assessment tools are needed for screening and enrolling patients, for developing individualized management, and for measuring treatment-related outcomes.[6,7,9,10]
The Tinnitus Handicap Inventory (THI) and the Tinnitus Questionnaire (TQ) were validated with good reliability, validity, which were used to tinnitus assessment by patients themselves for several years in China.[11–14] In the clinical reception of outpatient department, even both were translated and published normatively at our center,[11,14] however in our daily work, we still found that some practical problems exist. It is nearly half of the patients (44.4%, as reported by our team) claimed that some items of these questionnaires seems too ambiguous and away from their lives, which is hard to score by patients themselves.[15] A similar observation was also reported in another French study in 2003.[16] It cannot be denied that these self-report scales are validated statistically and translated accurately with standardized translating and back-translating strategies, but cultural differences still emerge and may take responsibility for the practical problem.[15,16] Influence factors as the education level, the knowledge of tinnitus and the attitude to the tinnitus assessment may cause the bias of the self-report result.[15] Considering the cultural adaptation, we introduced a new clinician-administered scoring method, the mandarin Tinnitus Evaluation Questionnaire (TEQ) as a simple screening tool and an outcome measurement in our tinnitus management.
The TEQ (mandarin version) was published by Liu in China.[17] Based on a face-to-face interview, it is aimed to assess the impression of clinicians toward the patients’ tinnitus severity in a brief score sheet. Based on the TEQ score, researchers hope to achieve the following objectives: to screen out patients who need interventions, to differentiate patients who need active attention of clinicians, to reflect the treatment-related change. The TEQ includes a total of 6 items that cover 3 aspects: the patient's awareness of tinnitus, the patient's reaction to the negative effects of tinnitus, and the overall impression of tinnitus annoyance and their desire for intervention.[17,18] All 6 items and their grading standards come from the clinical observation and an expert panel discussion.[19] And, TEQ has improved the traditional clinician-rated tinnitus grade classification (Feldmann,5 grades; Biesinger, 4 grades).[20–22] In the initial study, TEQ was reported by the developer with good reliability and validity.[18]
However, the psychometric properties of TEQ should be tested with more patients in more centers, and the quantified outcome measures need to be explored, such as the responsiveness and the effective criterion. In this study, we analyzed the difference between the clinician rating questionnaire and the self-report questionnaire. The self-report mandarin THI, translated by our center, was adopted as the control. Moreover, based on the conclusion, we try to raise concern about the clinician's role in the comprehensive assessment of tinnitus.
2. Materials and methods
2.1. Subjects
All data were collected from outpatients diagnosed with primary tinnitus by an otologist at the outpatient service of the Hearing Center, Department of Otolaryngology Head and Neck Surgery in West China Hospital between 2015 and 2018. Only adult (age > 18 years) patients with tinnitus as the main complaint were enrolled. Before enrollment, subjects provided informed consent for making sure the use of their clinical data voluntarily. In consideration of the probationary period of the TEQ, this study excluded subjects whose tinnitus durations from tinnitus onset to seeking intervention were less than 1 month to facilitate the stable description of patients with the frequency of tinnitus awareness and the degree of tinnitus annoyance. And subjects who could not complete any one test (TEQ or THI) due to visual impairment, severe hearing loss, cognitive and communication disorders, or mental diseases were excluded. In addition, patients confused about the purpose of assessment were also excluded. Finally, a total of 414 patients were included, of whom 173 (173/414) subjects completed 1 follow-up 2 months later. When first-visit, except for the questionnaire assessment, patients received a tinnitus educational counseling, including the knowledge of tinnitus and coping strategies. Between the first visit and the follow-up, the lifestyle modification advices (regular and enough sleep, health diet, and proper relaxation exercises) were proposed for all patients.[23]
2.2. TEQ
The TEQ contains 6 scoring items (as shown in Table 1).[17,18] The first 5 items are worth 3 points each, and the sixth item is worth 6 points, for a total of 21 points. The 6 items are listed in Table 1. In essential, the evaluation objective of each item is as follows: to understand the degree of awareness about tinnitus perception, that is “where and when”, to quantify the negative impact of tinnitus on the patient's functions (sleep, emotion, and concentration, respectively), to realize the reduction of the life quality and the urgency of patient desire in seeking for tinnitus interventions. All 6 items are scored by the professional evaluator through a face-to-face interview, in which some relevant and targeted questions in regard to patient's awareness and experience of tinnitus are inquired. According to the description of patients, 1 evaluator scores each item and then gets a total score of TEQ by summing all 6 item scores.[18] Six scoring items of TEQ are fixed, but the content of interview and the order of questions are flexible in consideration of patients’ life experience and work situation. A higher score is related to a higher degree of the awareness, the bothersome, and the desire for intervention. Basically, the score of TEQ can reflect the evaluator's subjective impression in regard to patients’ tinnitus severity after an interview. To reflect the tinnitus severity of patients more intuitively, the developer divided the total TEQ score into a grading system (Grade I, 1–6 points, Grade II, 7–10 points, Grade III, 11–14 points, Grade IV, 15–18 points, and Grade V, 19–21 points).[18] According to the developer, patients with grade V (19–21 points) TEQ score need immediate comprehensive interventions, including the involvement of psychologists and the anxiety/depression assessment. While excessive interventions and complicated tinnitus assessments may be inappropriate for the Grade I patients.
Table 1.
Tinnitus evaluation questionnaire (TEQ).
| Items | Scores∗ |
| Acoustic environment where patients are aware of tinnitus | No tinnitus (0) |
| Quiet environment (1) | |
| General environment (2) | |
| Any environment (3) | |
| Intermittent or continuous tinnitus | No tinnitus (0) |
| Intermittent, time with tinnitus < time without tinnitus (1) | |
| Intermittent, time with tinnitus ≥ time without tinnitus (2) | |
| Continuous (3) | |
| Effects of tinnitus on sleep | No (0) |
| Sometimes (1) | |
| Often (2) | |
| Always (3) | |
| Effects of tinnitus on emotion | No (0) |
| Sometimes (1) | |
| Often (2) | |
| Always (3) | |
| Effects of tinnitus on concentration | No (0) |
| Sometimes (1) | |
| Often (2) | |
| Always (3) | |
| Overall impression of tinnitus annoyance | (0 1 2 3 4 5 6) |
Total Score: 21.
2.3. THI
The THI was published by Newman et al[13] in 1996. It contains 25 items, which can be divided into 3 subcategories (functional, catastrophic, and emotional), to quantify the degree of tinnitus handicap. All these items are closed-ended questions. Each question is responded as “yes,” “sometimes,” or “no.” These 3 responses are scored as 4 points, 2 points, or 0 points, correspondingly. And the maximum score of THI is 100 points.[13] The total score of THI can also be divided into 5 grades (Grade I, 0–16 points, Grade II, 18–36 points, Grade III, 38–56 points, Grade IV, 59–76 points, and Grade V, 78–100 points).[7] The THI used in our study was the Mandarin version published in 2012.[11] In addition to its good psychometric properties, it has already been used to outcome measurement in some clinical hearing centers of China. Considering these, we include the result of THI as a comparison.[11]
2.4. Procedures
After enrolling, patients accepted a face-to-face interview with 1 of 2 evaluators (A or B), which one was decided by a computer using a random number table. This evaluator scored the TEQ for the first time. Subsequently, the history taking was completed by an audiologist, and then patients were asked to complete the THI and a single-question visual analog scale (How severe your tinnitus was over the past week? Choose a score from 0–10, 0 represents “not tinnitus present,” 10 represents “the worst tinnitus you can imagine”).[6] Next, patients underwent a standard pure-tone audiometry that included frequencies from 0.25 to 8 kHz. After the audiometry, patients were assessed again with the TEQ by another evaluator (A or B). Finally, a counsellor met with each patient for tinnitus education, coping strategies guidance, and the life-style modification.[23] The entire assessment and consultation work were completed in 1 to 2 days, and the interval between 2 TEQ evaluations was at least half a day. Neither of evaluators (A or B) participated in the intervention process, and they were blind to each other's TEQ score or the THI score.
At follow-up (2 months later), patients first accepted the TEQ assessment. And then, they were asked to described their subjective global impression of tinnitus change (worsening, unchanged, slightly improved, significantly improved).[6,7] Subsequently, after the audiological test, patients completed the THI by themselves again based on their experience of tinnitus in the latest week. The data collection was approved by the ethics committee of our hospital, and all procedures complied with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Patients can quit the tinnitus assessment or the intervention process at any time. Besides, the research team consists of medical staffs in Table 2.
Table 2.
Research team.
| Research team member | Duty |
| An ENT doctor | Patient enrolling |
| An information processing specialist | Registration and arranging the follow up |
| An Audiologist | Audiological tests |
| Two evaluators (A and B) | TEQ evaluation |
| A counsellor | Patient education in regard to tinnitus, Counselling and life-style guidance |
2.5. Data analysis and statistics
Measurement data were presented as mean value and standard deviation (mean ± SD), and enumeration data were expressed as the proportion. In this study, correlation analysis was performed using the Pearson correlation test, and internal consistency reliability analysis was performed by calculating the Cronbach's α coefficient.[7] The total score, the grade, and the cumulative percentage distribution were employed to reflect patient's severity of tinnitus, respectively.[24] In addition, we set the THI score as a reference to calculate the sensitivity, specificity, total consistent rate, and Kappa value of the TEQ for screening severe tinnitus (Grades IV–V) and for determining whether a tinnitus patient required interventions (Grades II–V).
For assessing the performance of TEQ in treatment-related outcomes measurement, the responsiveness and the minimum clinically meaningful change score (MCMCS) were reported. Grouping was performed according to the patient's subjective impression of tinnitus change after the intervention, and the effect size (ES) of TEQ score change was calculated for each group[25,26] (the worsening group, the unchanged group, the slightly improved group, and the significantly improved group). The larger the ES, the greater the improvement of score is after treatment. Ideally, if a test tool shows good responsiveness, the magnitude of the ES for each group should sensitively reflect patients’ subjective impressions of tinnitus changes; that is, the group with a significant improvement in tinnitus would demonstrate a greater ES. The formula used to calculate ES and the criterion for determining the magnitude of ES are based on Cohen's calculation.[25,27–29] At last, we calculated the MCMCS for estimating the evaluation criteria of intervention-related outcome measurement with Demorest's and Norman's method, separately. The MCMCS is a minimum reduction of TEQ score, which indicates that the patient's tinnitus may have undergone a meaningful change.[25,30–34] Data entry and statistical analysis were performed using SPSS 24.0 (SPSS, IBM Corp, Armonk, NY), and P < .05 was considered statistically significant.
3. Results
The demographic characteristics of 414 patients and 173 follow-up patients are shown in Table 3. Since all the patients came from a large teaching hospital with a chief complaint of tinnitus, patients with TEQ grade II–IV accounted for 91.30% of the sample at the first visit, while 74.15% of patients reported their THI score in grades II–IV.
Table 3.
Subjects characteristics.
| Total subjects (N = 414) | Follow-up subjects (N = 173) | |
| Age, years | ||
| Average (SD) | 43.93 (13.70) | 45.24 (13.59) |
| Range | 16–78 | 18–76 |
| Tinnitus duration, months | ||
| Average (SD) | 34.61 (52.62) | 35.39 (57.75) |
| Range | 1–312 | 1–264 |
| Gender, N (%) | ||
| Male | 192 (46.38%) | 77 (44.51%) |
| Female | 222 (53.62%) | 96 (55.49%) |
| Hearing loss, N (%) | ||
| No | 190 (45.89%) | 67 (38.73%) |
| Yes | 224 (54.11%) | 106 (61.27%) |
| Tinnitus location, N (%) | ||
| Left ear | 125 (30.19%) | 55 (31.79%) |
| Right ear | 78 (18.84%) | 30 (17.34%) |
| Bilateral ear | 172 (41.55%) | 71 (41.04%) |
| Inner head | 14 (3.38%) | 6 (3.47%) |
| Unable to describe | 25 (6.04%) | 11 (6.36%) |
| Tinnitus sound characteristics, N (%) | ||
| Cicadas | 227 (54.83%) | 85 (49.13%) |
| Others | 152 (36.71%) | 74 (42.77%) |
| Unable to describe | 35 (8.45%) | 14 (8.09%) |
| Education level | ||
| Without a college degree | 186 (44.93%) | 79 (45.66%) |
| With a college degree | 228 (55.07%) | 94 (54.34%) |
SD = standard deviation.
3.1. Reliability and convergent validity of the TEQ
The average TEQ scores of these 414 patients assessed by evaluators A and B in the first visit were 11.89 ± 3.78 points and 11.99 ± 3.74 points, respectively. Pearson's correlation coefficient between results assessed by the 2 evaluators was 0.97, beyond 0.8, suggesting an excellent inter-rater reliability of TEQ. The Cronbach's alpha coefficient of TEQ was 0.79 when assessed by evaluator A in the first visit (0.78, by evaluator B). Both were greater than 0.7, which demonstrated a good internal consistency reliability of TEQ. In addition, the mean TEQ total score of 414 patients at the initial visit was 11.89 ± 3.78 points, the mean THI total score was 47.36 ± 24.15 points, and the mean visual analog scale (VAS) score was 5.80 ± 2.49 points. The Pearson's correlation coefficient of the total score between TEQ and THI was 0.78 (P < .01) and that between TEQ and VAS was 0.62 (P < .01). It indicated a good convergent validity between the TEQ and 2 common self-reported tinnitus scales in China. Finally, the average time required to administer the TEQ assessment was 3.65 ± 0.99 minutes (ranging between 2 and 7 minutes), whereas the average time consumption for THI was 8.43 ± 2.12 minutes (ranging between 3 and 15 minutes). Thus, the TEQ assessment required less time than the THI assessment (P < .01).
3.2. Comparison of the TEQ and THI results for assessing tinnitus severity
One of the most important goals of TEQ is to assess the severity of tinnitus. Figure 1 shows the cumulative percentage distribution of patients[24] with different TEQ scores. For example, if patients with an TEQ total score less than or equal to 11 points accounted for 51.2% of the total sample, then the cumulative distribution percentage of patients with 11 points was 51.2%. Namely, we could preliminarily estimate that 1 patient with 11 points of TEQ had a moderate tinnitus. Similarly, Figure 1 shows the cumulative distribution percentage of the THI score.
Figure 1.
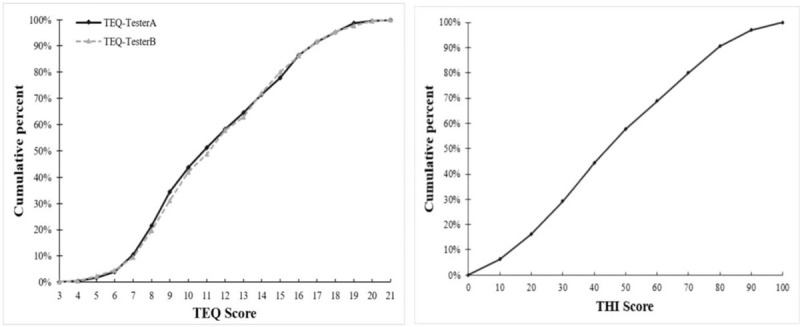
Cumulative percent distribution of responses on TEQ score and THI score.
In addition, to exhibit tinnitus severity, the developer of THI and TEQ reported methods more intuitively with the classification, respectively.[7,18,35] According to the opinion of developer, a THI ≥ 58 points, and an TEQ ≥ 15 points (grade IV and V patients) indicate severe tinnitus. In our study, a THI ≥ 58 points was used as a reference standard to evaluate the utility of the TEQ for diagnosing severe tinnitus. For this purpose, TEQ showed a moderate sensitivity (66.00%), a good specificity (92.80%), a total consistent rate of 83.09%, and a significant kappa value of 0.62 (P < .001). In addition, when we considered a THI ≥ 18 points and a TEQ ≥ 7 points as indexes to determine whether a patient required treatment, the sensitivity of TEQ was 98.92%, the specificity was 26.67%, the total consistent rate was 91.06%, and the kappa value was 0.36 (P < .001).
3.3. Responsiveness of the TEQ
Among all the subjects in this study, 173 completed 1 follow-up evaluation. According to patients’ subjective description about their tinnitus changes after the intervention, we divided these subjects into 4 groups: the worsening group, the unchanged group, the slightly improved group, and the significantly improved group, grouping method (PGIC) reported as Newman and Meikle.[6,7] The ES of the TEQ and THI score changes for each group is shown in Table 4. A greater ES indicates a more significant score reduction after intervention, and a negative ES indicates that the scale score increased after intervention.[7] The result of TEQ and THI suggested that the ESs gradually increased from the worsening group to the significantly improved group (ESs of TEQ for the 4 groups were −0.48, 0.02, 0.60, and 1.90, respectively; those of THI were 0.13, 0.27, 0.69, 1.30, respectively). Both increasing trends of the TEQ and THI corresponded to patients’ subjective impression. However, it is also worth noting that, in the significantly improved group, the ES was 1.90 for the TEQ and 1.30 for the THI. The ES of the TEQ was greater than that of the THI, which indicated that the decrease trend of TEQ score was more significant than that of THI score after intervention. In the worsening group, the TEQ score increased after intervention; therefore, its ES was −0.48, which was more consistent with the patients’ subjective impression of tinnitus deterioration. However, the THI score for this group after the intervention still showed a slight decrease, and its ES was 0.13, which was not in accordance with the subjective impression of these patients.
Table 4.
Comparing effect sizes of the self-report significantly improved, slightly improved, unchanged or worsening group on overall change scores for TEQ and THI.
| TEQ | THI | ||||||
| Group | N | Change Scores after intervention | SDpooled | ES | Change Scores after intervention | SDpooled | ES |
| Worsening | 16 | −1.63 | 3.42 | −0.48 | 2.75 | 21.17 | 0.13 |
| Unchanged | 50 | 0.08 | 3.67 | 0.02 | 7.12 | 24.31 | 0.29 |
| Slightly improved | 40 | 2.15 | 3.58 | 0.60 | 16.45 | 23.79 | 0.69 |
| Significantly improved | 67 | 5.79 | 3.04 | 1.90 | 26.96 | 20.75 | 1.30 |
ES = effect size, SDpooled = the pooled standard deviation, Xaverage is in short for mean scores. ES < 0.2 indicates no effect size, 0.2–0.5, a small ES, 0.5–0.8, a medium ES, and ≥ 0.8, a large ES.
3.4. Minimum clinically meaningful change score of TEQ
How much of a reduction in TEQ points can be considered a criterion of tinnitus improvement is a key point for postintervention studies. In this study, we introduced the standard error of the retest difference and calculated the 95% confidence interval to estimate whether a truly meaningful score change occurred.[33] The calculation result is shown in Table 5. The MCMCS of TEQ was estimated to be 2 by the 95% CI (1.85). In addition, we used the half SD of TEQ score at the first visit to roughly estimate the MCMCS. This approach stemmed from Norman's systematic review,[32] which noted that in most circumstances, the threshold of discrimination for changes in health-related quality of life for chronic diseases appears to be approximately half of the SD. In this study, we found that the SD of score on the initial visit was 3.77 and that half of the SD was 1.88. Since the TEQ score can only be an integer, the estimated MCMCS was still 2 (as Table 5). Considering the results of both methods, when the TEQ score is reduced by more than or equal to 2 points after the intervention, the patient's tinnitus can be considered improved; thus, we can use this as an outcome standard for effective intervention.
Table 5.
The minimum clinically meaningful change scores (MCMCS) of TEQ.
| Evaluator | Mean ± SD | Rinter-rater | Se | 95% CI | 0.5SDbaseline | MCMCS∗ |
| A | 11.90 ± 3.77 | 0.97 | 0.65 | 1.85 | 1.88 | 2 |
| B | 11.99 ± 3.74 |
The total score of TEQ should be integer, so we estimate reduced 2 scores after intervention as the MCMCS of TEQ.
If this 2-point reduction in TEQ score was used as a criterion indicating an effective intervention, then among the 173 patients in this study, 97 showed tinnitus improvement at follow-up, with an effective rate of 56.07%. In addition, 107 patients reported slight and significant improvement of tinnitus, for an effective rate of 61.85%; therefore, the effective rates indicated by the TEQ standard and the patients’ subjective impression of tinnitus improvement were similar. When a 20-point reduction in the THI score was used as the standard for an effective intervention,[33] 57 patients showed effective improvement, and the effective rate was 32.95%, which is lower than the effective rate indicated by the patients’ subjective impression of tinnitus improvement.
4. Discussion
According to our experience, in our center, clinicians usually play a guiding role in the decision-making of treatment implementation. Especially in outpatient's department of Chinese hospitals, patients often expect clinicians to have a preliminary understanding of the patient's condition after medical history-taking and physical examination, and to provide the next step of treatment in a short time, such as referral or rehabilitation.[15] The subjective impression of clinician will have an impact on the intervention process of tinnitus. Previous researches have already been conducted regarding the tinnitus assessment based on the clinician-rating. For example, Feldman et al proposed a 5-level classification method for the severity of tinnitus.[22] However, in practice, the actual situation of a single patient's tinnitus is difficult to fully match all classification descriptions of a certain level, which makes this classification method difficult to apply.[7] Different from the traditional method of clinician-rating, there is a score system in TEQ in addition to the classification method, which makes it more discriminative. At the same time, clinician rating eases the burden of patients for completing the questionnaire, and also avoids the probable error in understanding the written expression items of self-report quesionnaire.[15]
A good psychometric property is a prerequisite for the clinical application of measurement tools.[6,7] In this study, the inter-rater correlation trend for the total TEQ score was very good, with a correlation coefficient of 0.97 (> 0.80). It was very close to 0.94, the value reported by the TEQ developer,[18] suggesting that difference in evaluators does not have a significant impact on the result. Apart from its external reliability, the TEQ also showed a good internal consistency reliability. Cronbach's coefficient was 0.79 (> 0.70), which was also close to the coefficient of 0.76 reported by the developer,[18] indicating that a correlation exists in these 6 TEQ items. However, the Cronbach's coefficient of TEQ was lower than that of THI.[11] Reasons for this observation may be those as follows: the number of TEQ items is smaller, and each item of TEQ is for evaluating one aspect of tinnitus.
One main purpose for tinnitus questionnaire is intake assessment,[6] including subject enrollment, patient classification, and patient referrals. “How bad is my tinnitus?” is one of the most urgent questions that patients care about in our center. Therefore, the result of assessment should demonstrate a good interpretability,[7] which can be used to instruct the management. This study included a large sample size comprised of outpatients. We calculated the cumulative percentages of patients with different scores and plotted the cumulative distribution percentage graph of patients with different scores, referring to the method reported by Kuk et al.[24] With this graph, we can roughly explain the degree of tinnitus severity to patients. For example, if a patient's TEQ score at the first visit is 14 points, we can explain that “your tinnitus is more severe than that of 70% of patients who seek treatment in our center,” rather than simply saying “your tinnitus scale score is 14 points.” In addition, this method can also be used to compare the severity of tinnitus in patients from different sources. If the enrolled patients come from the community in one study and from hospitals in another study, the community patients may have relatively milder tinnitus, and the steep ascending section of the percentage distribution graph should be closer to the low-score area on the left side of the abscissa.
The second purpose of the TEQ is outcome assessment; that is, to detect tinnitus changes and to evaluate the efficacy of an intervention. Indeed, researchers suggest that responsiveness may be one essential psychometric property for this type of tool.[5,7,25,36] In this study, greater ES represented more significant score reduction after intervention. The TEQ and THI have been set with different maximum scores; however, the pooled SD was used in the calculation of ES, which made the score change of TEQ and THI comparable by a single value.[7,25,27,37] Regardless of whether the TEQ or THI was used, the score showed a trend that the more significant the patient's impression of improvement was, the larger the ES was. However, differences still existed between these 2 scales. Compared with the THI, the reduction trend of TEQ score after intervention could more sensitively reflect improvement, and the score change of TEQ was more in line with patients’ impressions as tinnitus worsens. In addition to responsiveness, the outcome assessment criterion is another core component in the intervention study. For the TEQ, the MCMCS calculated with 2 methods were consistent in that both were equal to 2 points. Namely, a 2-point or more obvious reduction in TEQ score after intervention can be interpreted as the tinnitus improvement. In this sample, the calculated effective rate of the TEQ (56.07%) was close to the effective rate (61.85%) indicated by the patients’ subjective impression of improvement.
Although TEQ includes fewer scoring items than other questionnaires, its application is flexible. For example, when examining concentration, patients’ complaints may be diverse. Some patients suggest that tinnitus affected their concentration when reading, some patients suggest that tinnitus affected their ability to follow a speaker/teacher in a meeting/class, and some patients point out the distraction during the communication. Including all these problems would greatly increase the number of items on a scale. Furthermore, some patients do not have a habit of reading in their daily lives, some do not attend meetings, and some live by themselves or rarely participate in social activities, so the corresponding questions would not be relevant to them. It has been reported that too many questions not only increase the burden of completing a scale for tinnitus patient but also lead to a poor responsiveness, as Tyler.[38]
In 2001, a framework, the International Classification of Functioning, Disability and Health (ICFDH), was proposed by WHO to provide domains of tinnitus assessment with regard to the health-related quality of life.[7,38,39] It suggested that both eliminating or habituating the tinnitus sound and alleviating the adverse impact of tinnitus in activity limitation should be the aim of tinnitus management.[7] Researchers have undertaken considerable in-depth exploration in previous studies. Tyler et al[38] suggested that if a questionnaire includes too many secondary area questions, the scale's responsiveness may be affected; furthermore, a patient's daily activities may interfere with the scoring of these secondary area questions. Henry et al[4] proposed that tinnitus assessment should adhere closely to the tinnitus itself and should not consider the patient's distress as a result of hyperacusis or hearing loss. In addition, Langguth et al[40] noted that repeated questions regarding whether tinnitus caused patients to feel a loss of control, to consider committing suicide, to feel a lack of security, or to feel loneliness in social relationships would induce them to blame tinnitus for various unhappiness, thereby wasting excessive attentions to the tinnitus and increasing the difficulty of rehabilitation. Considering the practicability, 3 items including sleep, concentration, and emotion in TEQ were also generally adopted in other tinnitus assessments.[34,38]
In terms of the test content, the difference between TEQ and THI lies in whether patients’ awareness of tinnitus is considered. Although psychoacoustic studies of tinnitus suggest that loudness matching is unrelated to the patient's subjective impression of tinnitus severity, this may be related to the measurement method itself.[5–7] But at follow-up, what patients often described first to clinicians was changes in the awareness and attention of tinnitus. Unlike loudness matching of psychoacoustic tests and the VAS used to assess the loudness of tinnitus,[7] the TEQ requires patients to list the environment in which he or she may be aware of tinnitus in daily life, which is easier for patients to describe how much patients’ life is disturbed by tinnitus.
However, for this study, some potential biases still exist in the TEQ implementation and the subjects. Due to the clinician-reported frame, medical staffs who evaluate the TEQ should accept training to make sure a uniform assessment criterion. And the preliminary is work consuming. Besides, to ensure a face-to-face interview and a long interval (2 months) for the follow-up TEQ test, patients with the telephone follow-up were excluded, the number of follow-up subjects decreased. So, the effect of subjects’ compliance on the correlation between the clinician-reported outcome and the self-reported outcome is unclear. In consideration of different evaluation systems, it is improper to estimate whether the clinician-administered TEQ is superior to other self-reported scales. In contrast, TEQ does have practical advantages over traditional clinician-reported grade systems, and can be used in patients unable to complete the self-report questionnaire. According to our recommendation, it is necessary to evaluate the severity of tinnitus by comprehensively considering the impression of the physician and the patient's self-perception. Also, to educate patients with the correct knowledge of tinnitus should precede any tinnitus assessments.
5. Conclusion
Scales based on clinician rating are widely used in the evaluation of subjective symptoms.[41] After training with the scoring criteria of the TEQ, clinicians, audiologists, psychologists, and counsellors can complete the assessment for different situations. It can be used as a consistent indicator between medical staffs when assessing tinnitus by medical staff. The result can be easily recorded and interpreted. In the outcome measurement, blind assessment should be considered, namely, the person who does not participate in treatment can administer the TEQ evaluation. Currently, the TEQ has only been studied in Chinese Mandarin-speaking outpatients at hospital. The application in community surveys and the validation of its English version need to be further studied.
Acknowledgment
The authors gratefully acknowledge Professor Peng Liu at the Department of Otorhinolaryngology, the First Affiliated Hospital of Guangzhou University of Traditional Chinese Medicine for his support in the implementation of TEQ.
Author contributions
Chen Zhiji, MD Experimental design, data analysis, writing manuscript
Fei Yingping, MD Project implementation
Wu Di, MD PhD Project implementation, data analysis
Yang Xiameng, MD Process control
Zheng Yun, MD PhD Modification, subject management, process control
Conceptualization: Yun Zheng.
Data curation: Zhiji Chen, Yingping Fei, Xiameng Yang.
Formal analysis: Zhiji Chen, Yingping Fei.
Funding acquisition: Yun Zheng.
Investigation: Yingping Fei, Di Wu.
Methodology: Zhiji Chen, Di Wu, Xiameng Yang.
Project administration: Zhiji Chen, Yun Zheng, Di Wu, Xiameng Yang.
Software: Zhiji Chen.
Supervision: Xiameng Yang.
Validation: Zhiji Chen.
Writing – original draft: Zhiji Chen.
Writing – review & editing: Yun Zheng.
Footnotes
Abbreviations: CI = confidence interval, ES = effect size, MCMCS = Minimum Clinically Meaningful Change Score, PGIC = Patient's Global Impression of Change, SD = standard deviation, TEQ = Tinnitus Evaluation Questionnaire, THI = Tinnitus Handicap Inventory, VAS = visual analog scale.
How to cite this article.: Chen Z, Zheng Y, Fei Y, Wu D, Yang X. Validation of the mandarin tinnitus evaluation questionnaire: a clinician-administered tool for tinnitus management. Medicine. 2021;100:27(e26490).
All data generated or analyzed during this study are included within the article.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: tinnitus executive summary. Otolaryngol Head Neck Surg 2014;151:533–41. [DOI] [PubMed] [Google Scholar]
- [2].McCormack A, Edmondson-Jones M, Somerset S, et al. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 2016;337:70–9. [DOI] [PubMed] [Google Scholar]
- [3].Xu X, Bu X, Zhou L, et al. An epidemiologic study of tinnitus in a population in Jiangsu Province, China. J Am Acad Audiol 2011;22:578–85. [DOI] [PubMed] [Google Scholar]
- [4].Henry JA, Griest S, Zaugg TL, et al. Tinnitus and hearing survey: a screening tool to differentiate bothersome tinnitus from hearing difficulties. Am J Audiol 2015;24:66–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Henry JA. Measurement” of Tinnitus. Otol Neurotol 2016;37:e276–85. [DOI] [PubMed] [Google Scholar]
- [6].Meikle MB, Stewart BJ, Griest SE, et al. Tinnitus outcomes assessment. Trends Amplif 2008;12:223–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Newman CW, Sandridge SA, Jacobson GP. Assessing outcomes of tinnitus intervention. J Am Acad Audiol 2014;25:76–105. [DOI] [PubMed] [Google Scholar]
- [8].Aazh H, Moore BCJ. Usefulness of self-report questionnaires for psychological assessment of patients with tinnitus and hyperacusis and patients’ views of the questionnaires. Int J Audiol 2017;56:489–98. [DOI] [PubMed] [Google Scholar]
- [9].Hiller W, Goebel G. Rapid assessment of tinnitus-related psychological distress using the Mini-TQ. Int J Audiol 2004;43:600–4. [DOI] [PubMed] [Google Scholar]
- [10].Hall DA, Haider H, Szczepek AJ, et al. Systematic review of outcome domains and instruments used in clinical trials of tinnitus treatments in adults. Trials 2016;17:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Meng Z, Zheng Y, Liu S, et al. Reliability and validity of the Chinese (Mandarin) tinnitus handicap inventory. Clin Exp Otorhinolaryngol 2012;5:10–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hallam RS, Jakes SC, Hinchcliffe R. Cognitive variables in tinnitus annoyance. Br J Clin Psychol 1988;27(pt 3):213–22. [DOI] [PubMed] [Google Scholar]
- [13].Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg 1996;122:143–8. [DOI] [PubMed] [Google Scholar]
- [14].Meng Z, Chen Z, Xu K, et al. Psychometric properties of a Mandarin version of the tinnitus questionnaire. Int J Audiol 2016;55:366–74. [DOI] [PubMed] [Google Scholar]
- [15].Wu D, Zheng Y, Chen Z, et al. Further validation of the Chinese (Mandarin) Tinnitus Handicap Inventory: comparison between patient-reported and clinician-interviewed outcomes. Int J Audiol 2018;57:440–8. [DOI] [PubMed] [Google Scholar]
- [16].Bouscau-Faure F, Keller P, Dauman R. Further validation of the Iowa tinnitus handicap questionnaire. Acta Otolaryngol 2003;123:227–31. [DOI] [PubMed] [Google Scholar]
- [17].Liu P, Li M. Communication evaluation of curative effect in tinnitus. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2008;43:710–3. [PubMed] [Google Scholar]
- [18].Liu P, Xu GL, Li M, et al. Study on reliability and validity of the Tinnitus Evaluation Questionnaire. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2012;47:716–9. [PubMed] [Google Scholar]
- [19].Neck S. Editorial Board of Chinese Journal of Otorhinolaryngology H. Interpretation of Chinese 2012 tinnitus experts consensus. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2012;47:709–12. [PubMed] [Google Scholar]
- [20].Cima RFF, Mazurek B, Haider H, et al. A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO 2019;67: suppl 1: 10–42. [DOI] [PubMed] [Google Scholar]
- [21].Baguley DM, Moffat DA, Hardy DG. What is the effect of translabyrinthine acoustic schwannoma removal upon tinnitus? J Laryngol Otol 1992;106:329–31. [DOI] [PubMed] [Google Scholar]
- [22].Feldmann H. Tinnitus. Dtsch Med Wochenschr 1992;117:480. [PubMed] [Google Scholar]
- [23].Liu YQ, Chen ZJ, Li G, et al. Effects of educational counseling as solitary therapy for chronic primary tinnitus and related problems. Biomed Res Int 2018;2018:6032525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kuk FK, Tyler RS, Russell D, et al. The psychometric properties of a tinnitus handicap questionnaire. Ear Hear 1990;11:434–45. [DOI] [PubMed] [Google Scholar]
- [25].Meikle MB, Henry JA, Griest SE, et al. The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear 2012;33:153–76. [DOI] [PubMed] [Google Scholar]
- [26].Henry JA, Griest S, Thielman E, et al. Tinnitus Functional Index: development, validation, outcomes research, and clinical application. Hear Res 2016;334:58–64. [DOI] [PubMed] [Google Scholar]
- [27].Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed.Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- [28].Adamchic I, Tass PA, Langguth B, et al. Linking the Tinnitus Questionnaire and the subjective Clinical Global Impression: which differences are clinically important? Health Qual Life Outcomes 2012;10:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Zeman F, Koller M, Figueiredo R, et al. Tinnitus handicap inventory for evaluating treatment effects: which changes are clinically relevant? Otolaryngol Head Neck Surg 2011;145:282–7. [DOI] [PubMed] [Google Scholar]
- [30].Newman CW, Wharton JA, Jacobson GP. Retest stability of the tinnitus handicap questionnaire. Ann Otol Rhinol Laryngol 1995;104(9 Pt 1):718–23. [DOI] [PubMed] [Google Scholar]
- [31].Demorest ME, Walden BE. Psychometric principles in the selection, interpretation, and evaluation of communication self-assessment inventories. J Speech Hear Disord 1984;49:226–40. [DOI] [PubMed] [Google Scholar]
- [32].Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582–92. [DOI] [PubMed] [Google Scholar]
- [33].Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol 1998;9:153–60. [PubMed] [Google Scholar]
- [34].Newman CW, Sandridge SA, Bolek L. Development and psychometric adequacy of the screening version of the tinnitus handicap inventory. Otol Neurotol 2008;29:276–81. [DOI] [PubMed] [Google Scholar]
- [35].McCombe A, Baguley D, Coles R, et al. Guidelines for the grading of tinnitus severity: the results of a working group commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999. Clin Otolaryngol Allied Sci 2001;26:388–93. [DOI] [PubMed] [Google Scholar]
- [36].Tyler RS, Oleson J, Noble W, et al. Clinical trials for tinnitus: study populations, designs, measurement variables, and data analysis. Prog Brain Res 2007;166:499–509. [DOI] [PubMed] [Google Scholar]
- [37].Zeman F, Koller M, Schecklmann M, et al. group TRIds. Tinnitus assessment by means of standardized self-report questionnaires: psychometric properties of the Tinnitus Questionnaire (TQ), the Tinnitus Handicap Inventory (THI), and their short versions in an international and multi-lingual sample. Health Qual Life Outcomes 2012;10:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Tyler R, Ji H, Perreau A, et al. Development and validation of the tinnitus primary function questionnaire. Am J Audiol 2014;23:260–72. [DOI] [PubMed] [Google Scholar]
- [39].WHO. International Classification of Functioning, Disability and Health: ICF. 2001; Available at: http://www.who.int/classifications/icf/en/. Accessed January 2, 2021 [Google Scholar]
- [40].Langguth B, Searchfield G, Biesinger E. Møller A, Langguth B, DeRidder D, Kleinjung T, et al. History and questionnaires. Textbook of Tinnitus.. New York: Springer; 2011. 338. [Google Scholar]
- [41].Gagliese L. Turk DC, MR. Assessment of pain in elderly people. Handbook of Pain Assessment. 2nd ed.. New York: Guilford; 2001. 119–33. [Google Scholar]


