Abstract
Acute and chronic kidney failure is common in hospitalized patients with COVID-19, yet the mechanism of injury and predisposing factors remain poorly understood. We investigated the role of complement activation by determining the levels of deposited complement components (C1q, C3, FH, C5b-9) and immunoglobulin along with the expression levels of the injury-associated molecules spleen tyrosine kinase (Syk), mucin-1 (MUC1) and calcium/calmodulin-dependent protein kinase IV (CaMK4) in the kidney tissues of people who succumbed to COVID-19. We report increased deposition of C1q, C3, C5b-9, total immunoglobulin, and high expression levels of Syk, MUC1 and CaMK4 in the kidneys of COVID-19 patients. Our study provides strong rationale for the expansion of trials involving the use of inhibitors of these molecules, in particular C1q, C3, Syk, MUC1 and CaMK4 to treat patients with COVID-19.
Keywords: COVID-19, SARS-CoV-2, Kidney injury, Complement activation, Immune complexes, Syk, MUC1, CaMK4
1. Introduction
Coronavirus disease 2019 (COVID-19), a pandemic caused by coronavirus 2 (SARS-CoV-2) has affected the globe with devastating societal and economic consequences [1,2]. Severe COVID-19 symptoms include respiratory distress, venous thrombosis, and failure of vital organs [[3], [4], [5], [6], [7]]. In particular, renal failure is especially common and associated with high mortality rates among hospitalized patients [8]. Acute kidney injury (AKI) has been reported in 24% to 57% of hospitalized patients and in 61% to 78% of those in the intensive care units [[9], [10], [11], [12]]. COVID-19 patients who develop severe AKI, have greater dialysis requirements, experience less in-hospital recovery [10] and have a higher risk to develop chronic kidney disease [13]. Most patients with COVID-19-related AKI who recover continue to have low renal function after discharge from the hospital [14].
SARS-CoV-2 RNA has not been detected in the kidneys of COVID-19 patients [15], and it is likely that the renal failure is secondary to a number of mechanisms including immune dysregulation and inflammation, endothelial damage, thrombophilia, thrombotic microangiopathy, and complement activation [[16], [17], [18]]. Even though complement is a central driver of COVID-19 immunopathology [[19], [20], [21], [22], [23], [24]], the pathways underlining the direct or indirect activation of the complement system in the kidney tissue have not been studied.
Systemic inflammation can trigger uncontrolled activation of complement and platelets. Additionally, tissue hypoxia can cause the destabilization of endothelial function. Several key proteins may contribute to the development of injury. In response to ischemia, mucin-1 (MUC1) levels increase and stabilize both HIF-1α and β-catenin to potentiate downstream protective pathways, while the prolonged up-regulation of MUC1 in the injured kidney leads to chronic kidney disease through either of the pathways [25]. Our recent collaborative study confirmed that inhibition of spleen tyrosine kinase (Syk) using fostamatinib (a Syk inhibitor molecule- R406 or R788) reduces the expression of MUC1 in lung epithelial cells in a mouse model of acute lung injury [26]. Syk inhibition suppresses both local and remote organ injury [27,28], blocks Fc receptor signalling and reduces immune complex-mediated inflammation [29]. Syk, a non-receptor tyrosine kinase, is expressed on both hematopoietic cells and non-hematopoietic cells with a variety of functional effects including mitosis, differentiation, cellular adhesion, motility [30] and has a key role in adaptive immunity [31].
Several reports have provided insight into the role of Syk in COVID-19-related infection and lung injury [26,32]. Both Syk and MUC1 have a major role in the pathogenesis of disease through the hypoxia pathway [[33], [34], [35]]. SARS-CoV-2 causes hypoxia [36] and it is also known that hypoxia leads to modulation of calcium cell signalling [37]. Calcium/calmodulin-dependent protein kinase IV (CaMK4) depends on calcium signalling and is essential for the activation of transcription factors downstream of T-cell receptor (TCR) signalling [38,39]. Calcium signalling is essential for podocyte injury [40,41], but the role of CaMK4-dependent signalling in SARS-CoV-2 related kidney injury has not been addressed.
A single-cell atlas of postmortem kidney tissue samples from 16 patients who succumbed to COVID-19 failed to detect viral RNA in the kidney [15]. The non-viral mechanisms which account for the AKI in COVID-19 patients [10,11] remain poorly understood. In this communication we determined the deposition levels of complement components (C1q, C3, FH, C5b-9), Syk, MUC1 and CaMK4 along with immunoglobulin in the kidney tissues of people who succumbed to COVID-19.
2. Materials and methods
We included kidney tissue samples from three COVID-19 patients, two female and one male (ages 82, 58 and 75 years) who expired between April 22 and May 6, 2020 at the Beth Israel Deaconess Medical Center (BIDMC), Boston, United States. Kidney tissues were collected by minimally invasive ultrasound-guided autopsy within 3 h of death to maintain tissue viability. Detailed description of the sample acquisition technique, pathology and molecular findings have been presented previously [42]. Kidney tissues were also collected from autopsy material of two subjects, one male and one female, 65 and 59 years of age, who had expired in the pre-COVID-19 period (one who had suffered a middle cerebral artery syndrome stroke and another who had a diagnosis of Type I diabetes mellitus) to serve as controls. Family members were consented for limited autopsies by a pathologist during a witnessed phone call immediately after the death and after referral from the intensive care unit team. Research using autopsy tissue for this project was approved by the institutional review board (IRB) of BIDMC. A Health Insurance Portability and Accountability Act (HIPAA) waiver was granted by the IRB for access to the charts of the patients for each project using the tissue. Tissue was provided to research teams per previously IRB-approved research protocols.
For immunofluorescence studies, formalin-fixed paraffin-embedded tissue sections were deparaffinized, dehydrated and followed by heat-induced epitope retrieval in sodium citrate buffer (10 mM Sodium citrate, 0.05% Tween 20, pH 6.0). The sections were then blocked with 3% bovine serum albumin (BP1600–100, Thermo Fisher) and 5% goat (50-062Z, Thermo Fisher) or donkey (S30-100ML, Sigma-Aldrich) serum for 1 h and incubated with the primary antibody overnight. Next day, the sections were washed, incubated with the secondary antibody for 90 min washed again and stained with DAPI (S36973, Thermo Fisher). Primary antibodies used in this study included antibodies to complement molecules [C1q (A201), FH (A229) (all from Quidel), C5b-9 (ab55811, Abcam), C3 (204,869, Calbiochem)], CaMK4 (ab3557, Abcam), MUC1 (ab80952, Abcam), human IgG + IgM + IgA (ab8512, Abcam), Syk (626,202, Biolegend) and synaptopodin (SC21537, Santa Cruz Biotechnology) to detect podocytes. Secondary antibodies were donkey anti-mouse (A10037), donkey anti-goat (A11055), goat anti-rabbit (A11011) (all from Life Technologies), and goat anti-hamster (127,545,160, Jackson immune research) conjugated with Texas red or fluorescein. Images were captured by BZ-X800E Fluorescence Microscope, KEYENCE and analyzed by the BZ-X 800 software ver. 1.1.1.8, KEYENCE. Quantitative fluorescence intensity measurements were performed with ImageJ (version 1.53).
Numerical data are expressed as mean fluorescence intensity per cell. Analysis was performed using statistical software (Graphpad Prism, USA). Comparisons among groups were performed by Mann-Whitney U test or one-way ANOVA, followed by Bonferroni's multiple comparison test. Statistical significance was accepted at p < 0.05. Experiments were performed in triplicate or quadruplicate.
3. Results and discussion
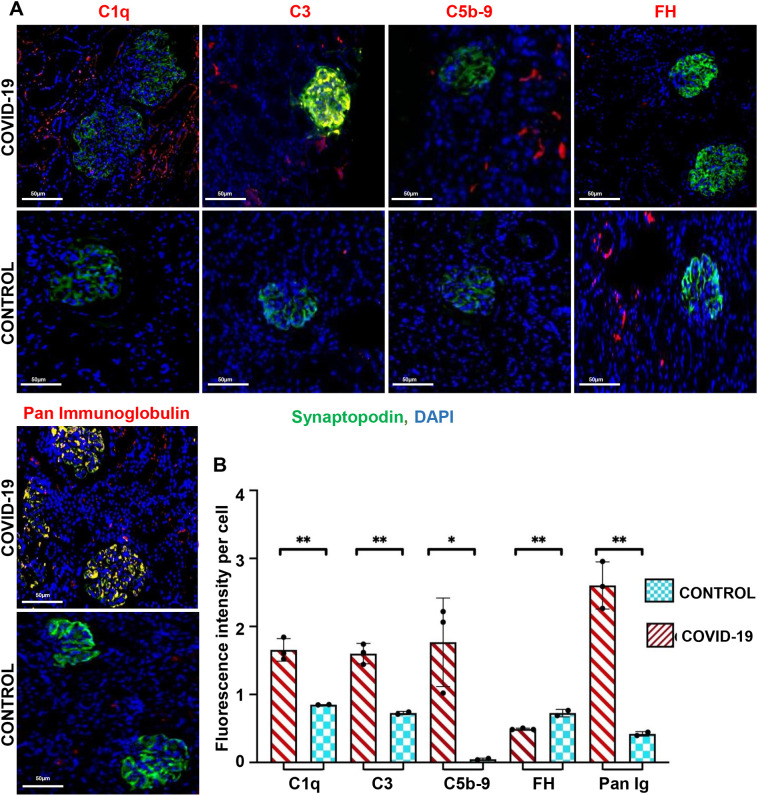
Analysis of immunohistochemical images (Fig. 1A) obtained from sections of formalin-fixed paraffin-embedded kidney tissues demonstrated that SARS-CoV-2 infection instigated the deposition of C1q of the classical pathway, C3, the central molecule of all pathways, and C5b-9, the membrane attack complex. We observed increased C1q and C3 deposition in tubules and glomeruli in all COVID-19 samples. C5b-9 deposition was absent in control kidney tissues and was primarily deposited in tubular basement membranes of COVID-19 samples (Fig. 1A, Supplementary Fig. 1). In accordance with our previous study [20] in COVID-19 infected lung tissues, we observed reduced expression of complement factor H (FH), a key inhibitor of the activation of the alternative complement pathway, in the kidney samples of COVID-19 patients compared with the control tissues. In addition, we found immunoglobulin deposited at increased levels in the kidney tissues of individuals with COVID-19 (Fig. 1A). Quantitative image analysis of kidney tissues further confirmed significantly higher deposition of the C1q, C3 and C5b-9 and total immunoglobulin with decreased expression of FH (Fig. 1B).
Fig. 1.
Deposition of complement components and immunoglobulin in the kidneys of COVID-19 patients. (A). Representative immunofluorescence staining (merged images) of kidney sections for complement molecules (C1q, C3, C5b-9 and FH), pan-immunoglobulin (all red) and synaptopodin (green) for podocyte detection. Nuclei are stained with DAPI (blue). Monochromatic (red) images of the studied proteins in COVID-19 samples are shown in Supplementary Fig. 1. Scale bar, 50 μm. (B). Mean fluorescence intensity per cell in COVID-19 and control samples (*Statistical significance was accepted at p < 0.05). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Complement activation has been associated with ischemia, trauma and sepsis and is linked with disease severity and poor clinical outcome [[43], [44], [45], [46]]. Activation of the complement system in patients with SARS-CoV-2 infection may initiate major complications in the kidney that lead to AKI. Although, clinical evidence has demonstrated increased prevalence of AKI in patients with SARS-CoV-2 infection [[9], [10], [11], [12]], SARS–CoV-2 virus was not detected in the kidney tissues that were collected for this study [42]. In agreement, previous studies also did not report robust signals of SARS-CoV-2 mRNA copies in the kidneys of COVID-19 patients [15,20,[47], [48], [49]].
The results of this work confirmed that infection with COVID-19 induces the deposition of C1q and C3 in kidney tissue that clearly implies the activation of the classical complement pathway, and this is further supported by the enhanced deposition of immunoglobulin. It is not yet clear whether the deposited immunoglobulin represents specific antibody against SARS-CoV-2 or naturally occurring antibodies which are present in normal individuals and are known to be deposited to injured tissues [50]. A recent study revealed the generation of autoantibodies in people with COVID-19 [51] which may be deposited in tissues and activate complement. Our finding revealed, like in the lung tissues infected with SARS-CoV-2 [52], decreased deposition of the regulatory complement component FH in the kidney tissues of COVID-19 patients, which may have enabled uncontrolled complement activation and deposition. Recently, variants of the FH gene were reported to be associated with severe clinical outcome in COVID-19 patients [53]. This implies that certain individuals have limited ability to control complement activation and accordingly they are more susceptible to severe disease. In another study complement FH gene polymorphisms and haplotypes were reported to provide protection against severe dengue virus-caused disease [54]. We also noted deposition of C5b–9 in tubular cells which is apparently responsible for cell destruction.
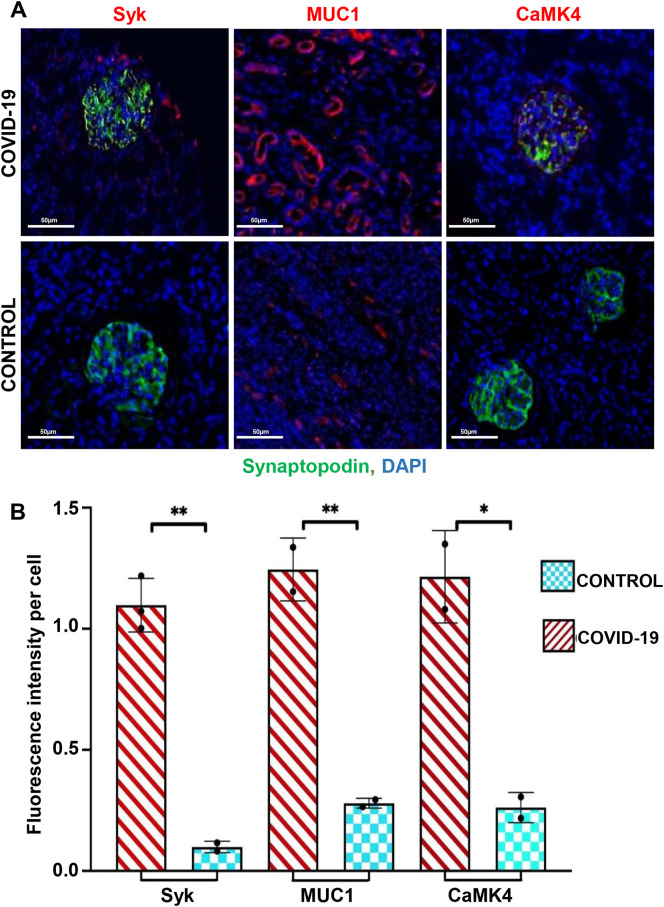
A number of molecules have been shown to be involved in organ injury including Syk [27,28], MUC1 [25,55,56] and CaMK4 [40,41,57]. Accordingly, we determined the expression levels of these molecules in kidney tissues from patients with COVID-19. Immunohistochemical images and quantitative image analysis established the extensive expression of Syk, MUC1 and CaMK4 in the kidney tissues of all three COVID-19 patients compared to controls (Fig. 2A and B).
Fig. 2.
Expression of CaMK4, Syk and MUC1 in the kidney of COVID-19 patients. (A). Representative immunofluorescence staining (merged images) of kidney sections for Syk, MUC1, CaMK4 (all red), synaptopodin (green). and nucleus (blue, DAPI). Monochromatic (red) images of the studied proteins in COVID-19 samples are shown in Supplementary Fig. 1. Scale bar, 50 μm. (B). Mean fluorescence intensity per cell in COVID-19 and control samples (*Statistical significance was accepted at p < 0.05). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Syk actively participates in many cell processes including adhesion, platelet activation, and innate immune recognition. These biological processes in which Syk participates has made Syk a convincing target for therapeutic strategies and approximately 70 patents have been filed using molecules to inhibit Syk for the treatment of a multitude of diseases [58]. Previously, our laboratory demonstrated that inhibition of Syk activity by the Syk inhibitor fostamatinib abolished intestinal (local) and lung (remote) tissue damage after mesenteric ischemia reperfusion [27]. Fostamatinib was approved in April 2018 by the FDA for the treatment of chronic immune thrombocytopenia. Moreover, fostamatinib is effective in limiting kidney injury in experimental animal models of glomerulonephritis [59], vasculitis [60] and proliferative immunoglobulin A (IgA) nephropathy [61]. Syk inhibition effectively inhibits IgE- and IgG-mediated activation of Fc receptor signalling and reduces immune complex-mediated inflammation [29]. Syk is also required for pathogen engulfment in complement-mediated phagocytosis [62]. These reports and our results suggest that Syk inhibitors may have a strong potential to treat COVID-19-related kidney injury.
MUC1, besides being involved in the development of tissue injury, is important in the defense against pathogen invasion [25,56]. MUC1 localizes to distal convoluted tubules and collecting ducts [63] in the kidney, however, under ischemic conditions MUC1 is localized in the proximal tubule [25,55,56]. We found higher expression of MUC1 in the kidney tissues of COVID-19 patients compared to controls. Our reported collaborative study showed that Syk inhibition may provide a beneficial effect in COVID-19-associatd acute lung injury by reducing the expression of MUC1 in lung epithelial cells [26]. A recent study suggested that the levels of KL-6/MUC1 may serve as a good prognostic biomarker of disease severity in hospitalized COVID-19 patients [64]. MUC1 defines both protective and harmful effects. The dual character of MUC1 has been established in many diseases including - kidney ischemia-reperfusion injury [55] and cancer metastasis [65].
Calcium signalling is involved in many pathways and regulates the expression of complement components, Syk, MUC-1 and NF-kB pathways [[66], [67], [68], [69], [70]]. In this study we found increased expression of CaMK4 in the kidney tissues of COVID-19 patients compared to controls. CaMK4 plays a role in kidney resident cell malfunction and injury including mesangial cells, podocytes and tubular epithelial cells. CaMK4 has a crucial role in controlling the structure and function of podocytes and proliferation of mesangial cells [71]. It was shown that CaMK4 hampers liver cell viability and proliferation and drives apoptosis [72]. Our group has explored tdelivery of KN-93 to inhibit CaMK4 in a cell-targeted manner in T cells [57] and podocytes [41] in lupus-prone mice. CaMK4 inhibition prevents podocyte injury, decreases mesangial IL-6 production and prevents kidney damage and interstitial inflammation [41,57]. We propose that targeted delivery of a CaMK4 inhibitor to resident kidney cells may have a promising therapeutic potential in COVID-19 related AKI. Novel in vitro culture platforms of podocytes [73] may also be utilized to study the pathobiology of COVID-19 related kidney injury and drug toxicity.
In conclusion, we report increased deposition of components of the complement pathways and increased expression of Syk, MUC-1 and CaMK4 in kidney tissues of people who succumbed to COVID-19. The pattern of complement deposition indicates the activation of both classical and alternative pathways. Any of the molecular pathways, alone or in combination that participate in the interplay of these molecules, may activate the immune response in COVID-19-associated AKI. Selective inhibition of these molecules or pathways may advance the treatment strategy of COVID-19 patients. This study provides additional rationale for the expansion of clinical trials to include modulators of the expression of the involved molecules.
The following is the supplementary data related to this article.
Representative monochromatic (single red channel) images of the studied proteins in COVID-19 samples. Scale bar, 50μm.
Acknowledgments
Acknowledgement
This work was supported by National Institutes of Health (NIH), National Institute of Allergy and Infectious Diseases (NIAID), United States grant 1R21AI151367-01A1.
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gasmi A., Noor S., Tippairote T., Dadar M., Menzel A., Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin. Immunol. 2020;215:108409. doi: 10.1016/j.clim.2020.108409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Liu L., Shan H., Lei C.L., Hui D.S.C., Du B., Li L.J., Zeng G., Yuen K.Y., Chen R.C., Tang C.L., Wang T., Chen P.Y., Xiang J., Li S.Y., Wang J.L., Liang Z.J., Peng Y.X., Wei L., Liu Y., Hu Y.H., Peng P., Wang J.M., Liu J.Y., Chen Z., Li G., Zheng Z.J., Qiu S.Q., Luo J., Ye C.J., Zhu S.Y., Zhong N.S., C. China Medical Treatment Expert Group for Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., Cereda D., Coluccello A., Foti G., Fumagalli R., Iotti G., Latronico N., Lorini L., Merler S., Natalini G., Piatti A., Ranieri M.V., Scandroglio A.M., Storti E., Cecconi M., Pesenti A., Network C.-L.I. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goyal P., Choi J.J., Pinheiro L.C., Schenck E.J., Chen R., Jabri A., Satlin M.J., Campion T.R., Jr., Nahid M., Ringel J.B., Hoffman K.L., Alshak M.N., Li H.A., Wehmeyer G.T., Rajan M., Reshetnyak E., Hupert N., Horn E.M., Martinez F.J., Gulick R.M., Safford M.M. Clinical characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Llitjos J.F., Leclerc M., Chochois C., Monsallier J.M., Ramakers M., Auvray M., Merouani K. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J. Thromb. Haemost. 2020;18:1743–1746. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., Collange O., Boulay C., Fafi-Kremer S., Ohana M., Anheim M., Meziani F. Neurologic features in severe SARS-CoV-2 infection. N. Engl. J. Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fabrizi F., Alfieri C.M., Cerutti R., Lunghi G., Messa P. COVID-19 and acute kidney injury: a systematic review and meta-analysis. Pathogens. 2020;9 doi: 10.3390/pathogens9121052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Argenziano M.G., Bruce S.L., Slater C.L., Tiao J.R., Baldwin M.R., Barr R.G., Chang B.P., Chau K.H., Choi J.J., Gavin N., Goyal P., Mills A.M., Patel A.A., Romney M.-L.S., Safford M.M., Schluger N.W., Sengupta S., Sobieszczyk M.E., Zucker J.E., Asadourian P.A., Bell F.M., Boyd R., Cohen M.F., Colquhoun M.I., Colville L.A., de Jonge J.H., Dershowitz L.B., Dey S.A., Eiseman K.A., Girvin Z.P., Goni D.T., Harb A.A., Herzik N., Householder S., Karaaslan L.E., Lee H., Lieberman E., Ling A., Lu R., Shou A.Y., Sisti A.C., Snow Z.E., Sperring C.P., Xiong Y., Zhou H.W., Natarajan K., Hripcsak G., Chen R. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ (Clinical research ed.) 2020;369 doi: 10.1136/bmj.m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisher M., Neugarten J., Bellin E., Yunes M., Stahl L., Johns T.S., Abramowitz M.K., Levy R., Kumar N., Mokrzycki M.H., Coco M., Dominguez M., Prudhvi K., Golestaneh L. AKI in hospitalized patients with and without COVID-19: a comparison study. J. Am. Soc. Nephrol. 2020;31:2145–2157. doi: 10.1681/ASN.2020040509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirsch J.S., Ng J.H., Ross D.W., Sharma P., Shah H.H., Barnett R.L., Hazzan A.D., Fishbane S., Jhaveri K.D., Abate M., Andrade H.P., Barnett R.L., Bellucci A., Bhaskaran M.C., Corona A.G., Chang B.F., Finger M., Fishbane S., Gitman M., Halinski C., Hasan S., Hazzan A.D., Hirsch J.S., Hong S., Jhaveri K.D., Khanin Y., Kuan A., Madireddy V., Malieckal D., Muzib A., Nair G., Nair V.V., Ng J.H., Parikh R., Ross D.W., Sakhiya V., Sachdeva M., Schwarz R., Shah H.H., Sharma P., Singhal P.C., Uppal N.N., Wanchoo R., Flores C. Bessy Suyin, Ng J.H. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98:209–218. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan L., Chaudhary K., Saha A., Chauhan K., Vaid A., Zhao S., Paranjpe I., Somani S., Richter F., Miotto R., Lala A., Kia A., Timsina P., Li L., Freeman R., Chen R., Narula J., Just A.C., Horowitz C., Fayad Z., Cordon-Cardo C., Schadt E., Levin M.A., Reich D.L., Fuster V., Murphy B., He J.C., Charney A.W., Böttinger E.P., Glicksberg B.S., Coca S.G., Nadkarni G.N. AKI in hospitalized patients with COVID-19. J. Am. Soc. Nephrol. 2021;32:151–160. doi: 10.1681/ASN.2020050615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coca S.G., Singanamala S., Parikh C.R. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81:442–448. doi: 10.1038/ki.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nugent J., Aklilu A., Yamamoto Y., Simonov M., Li F., Biswas A., Ghazi L., Greenberg J., Mansour S., Moledina D., Wilson F.P. Assessment of acute kidney injury and longitudinal kidney function after hospital discharge among patients with and without COVID-19. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delorey T.M., Ziegler C.G.K., Heimberg G., Normand R., Yang Y., Segerstolpe Å., Abbondanza D., Fleming S.J., Subramanian A., Montoro D.T., Jagadeesh K.A., Dey K.K., Sen P., Slyper M., Pita-Juárez Y.H., Phillips D., Biermann J., Bloom-Ackermann Z., Barkas N., Ganna A., Gomez J., Melms J.C., Katsyv I., Normandin E., Naderi P., Popov Y.V., Raju S.S., Niezen S., Tsai L.T.Y., Siddle K.J., Sud M., Tran V.M., Vellarikkal S.K., Wang Y., Amir-Zilberstein L., Atri D.S., Beechem J., Brook O.R., Chen J., Divakar P., Dorceus P., Engreitz J.M., Essene A., Fitzgerald D.M., Fropf R., Gazal S., Gould J., Grzyb J., Harvey T., Hecht J., Hether T., Jané-Valbuena J., Leney-Greene M., Ma H., McCabe C., McLoughlin D.E., Miller E.M., Muus C., Niemi M., Padera R., Pan L., Pant D., Pe’er C., Pfiffner-Borges J., Pinto C.J., Plaisted J., Reeves J., Ross M., Rudy M., Rueckert E.H., Siciliano M., Sturm A., Todres E., Waghray A., Warren S., Zhang S., Zollinger D.R., Cosimi L., Gupta R.M., Hacohen N., Hibshoosh H., Hide W., Price A.L., Rajagopal J., Tata P.R., Riedel S., Szabo G., Tickle T.L., Ellinor P.T., Hung D., Sabeti P.C., Novak R., Rogers R., Ingber D.E., Jiang Z.G., Juric D., Babadi M., Farhi S.L., Izar B., Stone J.R., Vlachos I.S., Solomon I.H., Ashenberg O., Porter C.B.M., Li B., Shalek A.K., Villani A.-C., Rozenblatt-Rosen O., Regev A. COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature. 2021;595:107–113. doi: 10.1038/s41586-021-03570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gavriilaki E., Brodsky R.A. Severe COVID-19 infection and thrombotic microangiopathy: success does not come easily. Br. J. Haematol. 2020;189:e227–e230. doi: 10.1111/bjh.16783. [DOI] [PubMed] [Google Scholar]
- 17.Satyam A., Tsokos G.C. Curb complement to cure COVID-19. Clin. Immunol. 2020;221:108603. doi: 10.1016/j.clim.2020.108603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Song W.C., FitzGerald G.A. COVID-19, microangiopathy, hemostatic activation, and complement. J. Clin. Invest. 2020;130:3950–3953. doi: 10.1172/JCI140183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noris M., Benigni A., Remuzzi G. The case of complement activation in COVID-19 multiorgan impact. Kidney Int. 2020;98:314–322. doi: 10.1016/j.kint.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pfister F., Vonbrunn E., Ries T., Jack H.M., Uberla K., Lochnit G., Sheriff A., Herrmann M., Buttner-Herold M., Amann K., Daniel C. Complement activation in kidneys of patients with COVID-19. Front. Immunol. 2020;11:594849. doi: 10.3389/fimmu.2020.594849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Nooijer A.H., Grondman I., Janssen N.A.F., Netea M.G., Willems L., van de Veerdonk F.L., Giamarellos-Bourboulis E.J., Toonen E.J.M., Joosten L.A.B., R.-C.-s. group Complement activation in the disease course of coronavirus disease 2019 and its effects on clinical outcomes. J. Infect. Dis. 2021;223:214–224. doi: 10.1093/infdis/jiaa646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skendros P., Mitsios A., Chrysanthopoulou A., Mastellos D.C., Metallidis S., Rafailidis P., Ntinopoulou M., Sertaridou E., Tsironidou V., Tsigalou C., Tektonidou M., Konstantinidis T., Papagoras C., Mitroulis I., Germanidis G., Lambris J.D., Ritis K. Complement and tissue factor–enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Invest. 2020;130:6151–6157. doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mastaglio S., Ruggeri A., Risitano A.M., Angelillo P., Yancopoulou D., Mastellos D.C., Huber-Lang M., Piemontese S., Assanelli A., Garlanda C., Lambris J.D., Ciceri F. The first case of COVID-19 treated with the complement C3 inhibitor AMY-101. Clin. Immunol. 2020;215:108450. doi: 10.1016/j.clim.2020.108450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mastellos D.C., Pires da Silva B.G.P., Fonseca B.A.L., Fonseca N.P., Auxiliadora-Martins M., Mastaglio S., Ruggeri A., Sironi M., Radermacher P., Chrysanthopoulou A., Skendros P., Ritis K., Manfra I., Iacobelli S., Huber-Lang M., Nilsson B., Yancopoulou D., Connolly E.S., Garlanda C., Ciceri F., Risitano A.M., Calado R.T., Lambris J.D. Complement C3 vs C5 inhibition in severe COVID-19: early clinical findings reveal differential biological efficacy. Clin. Immunol. 2020;220:108598. doi: 10.1016/j.clim.2020.108598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Bataineh M.M., Sutton T.A., Hughey R.P. Novel roles for mucin 1 in the kidney. Curr. Opin. Nephrol. Hypertens. 2017;26:384–391. doi: 10.1097/MNH.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kost-Alimova M., Sidhom E.-H., Satyam A., Chamberlain B.T., Dvela-Levitt M., Melanson M., Alper S.L., Santos J., Gutierrez J., Subramanian A., Byrne P.J., Grinkevich E., Reyes-Bricio E., Kim C., Clark A.R., Watts A.J.B., Thompson R., Marshall J., Pablo J.L., Coraor J., Roignot J., Vernon K.A., Keller K., Campbell A., Emani M., Racette M., Bazua-Valenti S., Padovano V., Weins A., McAdoo S.P., Tam F.W.K., Ronco L., Wagner F., Tsokos G.C., Shaw J.L., Greka A. A High-content screen for mucin-1-reducing compounds identifies fostamatinib as a candidate for rapid repurposing for acute lung injury. Cell Rep. Med. 2020;1:100137. doi: 10.1016/j.xcrm.2020.100137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pamuk O.N., Lapchak P.H., Rani P., Pine P., Lucca J.J.D., Tsokos G.C. Spleen tyrosine kinase inhibition prevents tissue damage after ischemia-reperfusion. Am. J. Physiol. Gastroint. Liver Physiol. 2010;299:G391–G399. doi: 10.1152/ajpgi.00198.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pamuk O.N., Can G., Ayvaz S., Karaca T., Pamuk G.E., Demirtas S., Tsokos G.C. Spleen tyrosine kinase (Syk) inhibitor fostamatinib limits tissue damage and fibrosis in a bleomycin-induced scleroderma mouse model. Clin. Exp. Rheumatol. 2015;33:S15–S22. [PubMed] [Google Scholar]
- 29.Braselmann S., Taylor V., Zhao H., Wang S., Sylvain C., Baluom M., Qu K., Herlaar E., Lau A., Young C., Wong B.R., Lovell S., Sun T., Park G., Argade A., Jurcevic S., Pine P., Singh R., Grossbard E.B., Payan D.G., Masuda E.S. R406, an orally available spleen tyrosine kinase inhibitor blocks fc receptor signaling and reduces immune complex-mediated inflammation. J. Pharmacol. Exp. Ther. 2006;319:998–1008. doi: 10.1124/jpet.106.109058. [DOI] [PubMed] [Google Scholar]
- 30.Antenucci L., Hytonen V.P., Ylanne J. Phosphorylated immunoreceptor tyrosine-based activation motifs and integrin cytoplasmic domains activate spleen tyrosine kinase via distinct mechanisms. J. Biol. Chem. 2018;293:4591–4602. doi: 10.1074/jbc.RA117.000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chauhan A.K., Moore T.L. Immune complexes and late complement proteins trigger activation of Syk tyrosine kinase in human CD4(+) T cells. Clin. Exp. Immunol. 2012;167:235–245. doi: 10.1111/j.1365-2249.2011.04505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Strich J.R., Ramos-Benitez M.J., Randazzo D., Stein S.R., Babyak A., Davey R.T., Suffredini A.F., Childs R.W., Chertow D.S. Fostamatinib inhibits neutrophils extracellular traps induced by COVID-19 patient plasma: a potential therapeutic. J. Infect. Dis. 2020;223:981–984. doi: 10.1093/infdis/jiaa789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kitamoto S., Yokoyama S., Higashi M., Yamada N., Takao S., Yonezawa S. MUC1 enhances hypoxia-driven angiogenesis through the regulation of multiple proangiogenic factors. Oncogene. 2013;32:4614–4621. doi: 10.1038/onc.2012.478. [DOI] [PubMed] [Google Scholar]
- 34.Chakraborty G., Rangaswami H., Jain S., Kundu G.C. Hypoxia regulates cross-talk between syk and lck leading to breast cancer progression and angiogenesis *. J. Biol. Chem. 2006;281:11322–11331. doi: 10.1074/jbc.M512546200. [DOI] [PubMed] [Google Scholar]
- 35.Jang J.W., Park S., Moon E.Y. Spleen tyrosine kinase regulates crosstalk of hypoxia-inducible factor-1α and nuclear factor (erythroid-derived2)-like 2 for B cell survival. Int. Immunopharmacol. 2021;95:107509. doi: 10.1016/j.intimp.2021.107509. [DOI] [PubMed] [Google Scholar]
- 36.Serebrovska Z.O., Chong E.Y., Serebrovska T.V., Tumanovska L.V., Xi L. Hypoxia, HIF-1α, and COVID-19: from pathogenic factors to potential therapeutic targets. Acta Pharmacol. Sin. 2020;41:1539–1546. doi: 10.1038/s41401-020-00554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gusarova G.A., Trejo H.E., Dada L.A., Briva A., Welch L.C., Hamanaka R.B., Mutlu G.M., Chandel N.S., Prakriya M., Sznajder J.I. Hypoxia leads to Na,K-ATPase downregulation via Ca(2+) release-activated Ca(2+) channels and AMPK activation. Mol. Cell. Biol. 2011;31:3546–3556. doi: 10.1128/MCB.05114-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Racioppi L., Means A.R. Calcium/calmodulin-dependent kinase IV in immune and inflammatory responses: novel routes for an ancient traveller. Trends Immunol. 2008;29:600–607. doi: 10.1016/j.it.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Greka A., Mundel P. Balancing calcium signals through TRPC5 and TRPC6 in podocytes. J. Am. Soc. Nephrol. 2011;22:1969–1980. doi: 10.1681/ASN.2011040370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ichinose K., Ushigusa T., Nishino A., Nakashima Y., Suzuki T., Horai Y., Koga T., Kawashiri S.-y., Iwamoto N., Tamai M., Arima K., Nakamura H., Obata Y., Yamamoto K., Origuchi T., Nishino T., Kawakami A., Tsokos G.C. Lupus nephritis IgG induction of calcium/calmodulin-dependent protein kinase IV expression in podocytes and alteration of their function. Arthritis Rheum. 2016;68:944–952. doi: 10.1002/art.39499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maeda K., Otomo K., Yoshida N., Abu-Asab M.S., Ichinose K., Nishino T., Kono M., Ferretti A., Bhargava R., Maruyama S., Bickerton S., Fahmy T.M., Tsokos M.G., Tsokos G.C. CaMK4 compromises podocyte function in autoimmune and nonautoimmune kidney disease. J. Clin. Invest. 2018;128:3445–3459. doi: 10.1172/JCI99507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brook O.R., Piper K.G., Mercado N.B., Gebre M.S., Barouch D.H., Busman-Sahay K., Starke C.E., Estes J.D., Martinot A.J., Wrijil L., Ducat S., Hecht J.L. Feasibility and safety of ultrasound-guided minimally invasive autopsy in COVID-19 patients. Abdominal Radiol. 2021;46:1263–1271. doi: 10.1007/s00261-020-02753-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matsumoto N., Satyam A., Geha M., Lapchak P.H., Dalle Lucca J.J., Tsokos M.G., Tsokos G.C. C3a enhances the formation of intestinal organoids through C3aR1. Front. Immunol. 2017;8 doi: 10.3389/fimmu.2017.01046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Satyam A., Andreo K., Lapchak P.H., Dalle Lucca J.J., Davis R.B., Tsokos M.G., Shapiro N.I., Tsokos G.C. Complement deposition on the surface of RBC after trauma serves a biomarker of moderate trauma severity: a prospective study. Shock. 2020;53:16–23. doi: 10.1097/SHK.0000000000001348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Satyam A., Graef E.R., Lapchak P.H., Tsokos M.G., Dalle Lucca J.J., Tsokos G.C. Complement and coagulation cascades in trauma. Acute Med. Surgery. 2019;6:329–335. doi: 10.1002/ams2.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Satyam A., Kannan L., Matsumoto N., Geha M., Lapchak P.H., Bosse R., Shi G.-P., Dalle Lucca J.J., Tsokos M.G., Tsokos G.C. Intracellular activation of complement 3 is responsible for intestinal tissue damage during mesenteric ischemia. J. Immunol. 2017;198:788–797. doi: 10.4049/jimmunol.1502287. [DOI] [PubMed] [Google Scholar]
- 47.Kudose S., Batal I., Santoriello D., Xu K., Barasch J., Peleg Y., Canetta P., Ratner L.E., Marasa M., Gharavi A.G., Stokes M.B., Markowitz G.S., D’Agati V.D. Kidney biopsy findings in patients with COVID-19. J. Am. Soc. Nephrol. 2020;31:1959–1968. doi: 10.1681/ASN.2020060802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Golmai P., Larsen C.P., DeVita M.V., Wahl S.J., Weins A., Rennke H.G., Bijol V., Rosenstock J.L. Histopathologic and Ultrastructural findings in postmortem kidney biopsy material in 12 patients with AKI and COVID-19. J. Am. Soc. Nephrol. 2020;31:1944–1947. doi: 10.1681/ASN.2020050683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Santoriello D., Khairallah P., Bomback A.S., Xu K., Kudose S., Batal I., Barasch J., Radhakrishnan J., D’Agati V., Markowitz G. Postmortem kidney pathology findings in patients with COVID-19. J. Am. Soc. Nephrol. 2020;31:2158–2167. doi: 10.1681/ASN.2020050744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tsokos G.C., Fleming S.D. Autoimmunity, complement activation, tissue injury and reciprocal effects. Curr. Dir. Autoimmun. 2004;7:149–164. doi: 10.1159/000075691. [DOI] [PubMed] [Google Scholar]
- 51.Wang E.Y., Mao T., Klein J., Dai Y., Huck J.D., Jaycox J.R., Liu F., Zhou T., Israelow B., Wong P., Coppi A., Lucas C., Silva J., Oh J.E., Song E., Perotti E.S., Zheng N.S., Fischer S., Campbell M., Fournier J.B., Wyllie A.L., Vogels C.B.F., Ott I.M., Kalinich C.C., Petrone M.E., Watkins A.E., Obaid A., Moore A.J., Casanovas-Massana A., Lu-Culligan A., Nelson A., Nunez A., Martin A., Watkins A.E., Geng B., Odio C.D., Harden C.A., Todeasa C., Jensen C., Kim D., McDonald D., Shepard D., Courchaine E., White E.B., Silva E., Kudo E., DeIuliis G., Rahming H., Park H.-J., Matos I., Nouws J., Valdez J., Lim J., Rose K.-A., Anastasio K., Brower K., Glick L., Sharma L., Sewanan L., Knaggs L., Minasyan M., Batsu M., Kuang M., Nakahata M., Linehan M., Askenase M.H., Simonov M., Smolgovsky M., Sonnert N., Naushad N., Vijayakumar P., Martinello R., Datta R., Handoko R., Bermejo S., Prophet S., Bickerton S., Velazquez S., Rice T., Khoury-Hanold W., Peng X., Yang Y., Cao Y., Strong Y., Dela Cruz C., Farhadian S.F., Schulz W.L., Ma S., Grubaugh N.D., Ko A.I., Iwasaki A., Ring A.M. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595:283–288. doi: 10.1038/s41586-021-03631-y. [DOI] [PubMed] [Google Scholar]
- 52.Satyam A., Tsokos M.G., Brook O.R., Hecht J.L., Moulton V.R., Tsokos G.C. Activation of classical and alternative complement pathways in the pathogenesis of lung injury in COVID-19. Clin. Immunol. 2021;226:108716. doi: 10.1016/j.clim.2021.108716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gavriilaki E., Asteris P.G., Touloumenidou T., Koravou E.-E., Koutra M., Papayanni P.G., Karali V., Papalexandri A., Varelas C., Chatzopoulou F., Chatzidimitriou M., Chatzidimitriou D., Veleni A., Grigoriadis S., Rapti E., Chloros D., Kioumis I., Kaimakamis E., Bitzani M., Boumpas D., Tsantes A., Sotiropoulos D., Sakellari I., Kalantzis I.G., Parastatidis S.T., Koopialipoor M., Cavaleri L., Armaghani D.J., Papadopoulou A., Brodsky R.A., Kokoris S., Anagnostopoulos A. Genetic justification of severe COVID-19 using a rigorous algorithm. Clin. Immunol. 2021;226:108726. doi: 10.1016/j.clim.2021.108726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pastor A.F., Rodrigues Moura L., Neto J.W.D., Nascimento E.J.M., Calzavara-Silva C.E., Gomes A.L.V., Silva A.M.D., Cordeiro M.T., Braga-Neto U., Crovella S., Gil L.H.V.G., Marques E.T.A., Jr., Acioli-Santos B. Complement factor H gene (CFH) polymorphisms C-257T, G257A and haplotypes are associated with protection against severe dengue phenotype, possible related with high CFH expression. Hum. Immunol. 2013;74:1225–1230. doi: 10.1016/j.humimm.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gibier J.-B., Hémon B., Fanchon M., Gaudelot K., Pottier N., Ringot B., Van Seuningen I., Glowacki F., Cauffiez C., Blum D., Copin M.-C., Perrais M., Gnemmi V. Dual role of MUC1 mucin in kidney ischemia-reperfusion injury: Nephroprotector in early phase, but pro-fibrotic in late phase. Biochim. Biophys. Acta (BBA) - Mol. Basis Dis. 2017;1863:1336–1349. doi: 10.1016/j.bbadis.2017.03.023. [DOI] [PubMed] [Google Scholar]
- 56.Pastor-Soler N.M., Sutton T.A., Mang H.E., Kinlough C.L., Gendler S.J., Madsen C.S., Bastacky S.I., Ho J., Al-bataineh M.M., Hallows K.R., Singh S., Monga S.P., Kobayashi H., Haase V.H., Hughey R.P. Muc1 is protective during kidney ischemia-reperfusion injury. Am. J. Physiol. Renal. Physiol. 2015;15(12):F1452–F1462. doi: 10.1152/ajprenal.00066.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Otomo K., Koga T., Mizui M., Yoshida N., Kriegel C., Bickerton S., Fahmy T.M., Tsokos G.C. Cutting edge: nanogel-based delivery of an inhibitor of CaMK4 to CD4+ T cells suppresses experimental autoimmune encephalomyelitis and lupus-like disease in mice. J. Immunol. 2015;195:5533–5537. doi: 10.4049/jimmunol.1501603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geahlen R.L. Getting Syk: spleen tyrosine kinase as a therapeutic target. Trends Pharmacol. Sci. 2014;35:414–422. doi: 10.1016/j.tips.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schuringa J.J., Timmer H., Luttickhuizen D., Vellenga E., Kruijer W. C-Jun and c-Fos cooperate with STAT3 in IL-6-induced transactivation of the IL-6 respone element (IRE) Cytokine. 2001;14:78–87. doi: 10.1006/cyto.2001.0856. [DOI] [PubMed] [Google Scholar]
- 60.McAdoo S.P., Prendecki M., Tanna A., Bhatt T., Bhangal G., McDaid J., Masuda E.S., Cook H.T., Tam F.W.K., Pusey C.D. Spleen tyrosine kinase inhibition is an effective treatment for established vasculitis in a pre-clinical model. Kidney Int. 2020;97:1196–1207. doi: 10.1016/j.kint.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McAdoo S., Tam F.W.K. Role of the spleen tyrosine kinase pathway in driving inflammation in IgA nephropathy. Semin. Nephrol. 2018;38:496–503. doi: 10.1016/j.semnephrol.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi Y., Tohyama Y., Kadono T., He J., Miah S.M., Hazama R., Tanaka C., Tohyama K., Yamamura H. Protein-tyrosine kinase Syk is required for pathogen engulfment in complement-mediated phagocytosis. Blood. 2006;107:4554–4562. doi: 10.1182/blood-2005-09-3616. [DOI] [PubMed] [Google Scholar]
- 63.Leroy X., Copin M.-C., Devisme L., Buisine M.-P., Aubert J.-P., Gosselin B., Porchet N. Expression of human mucin genes in normal kidney and renal cell carcinoma. Histopathology. 2002;40:450–457. doi: 10.1046/j.1365-2559.2002.01408.x. [DOI] [PubMed] [Google Scholar]
- 64.d’Alessandro M., Bergantini L., Cameli P., Lanzarone N., Antonietta Mazzei M., Alonzi V., Sestini P., Bargagli E. Serum KL-6 levels in pulmonary Langerhans’ cell histiocytosis. Eur. J. Clin. Investig. 2020;50 doi: 10.1111/eci.13242. [DOI] [PubMed] [Google Scholar]
- 65.Syrkina M.S., Maslakova A.A., Potashnikova D.M., Veiko V.P., Vassetzky Y.S., Rubtsov M.A. Dual role of the extracellular domain of human Mucin MUC1 in metastasis. J. Cell. Biochem. 2017;118:4002–4011. doi: 10.1002/jcb.26056. [DOI] [PubMed] [Google Scholar]
- 66.Merle N.S., Church S.E., Fremeaux-Bacchi V., Roumenina L.T. Complement system part I - molecular mechanisms of activation and regulation. Front. Immunol. 2015;6:262. doi: 10.3389/fimmu.2015.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elsner J., Oppermann M., Czech W., Dobos G., Schopf E., Norgauer J., Kapp A. C3a activates reactive oxygen radical species production and intracellular calcium transients in human eosinophils. Eur. J. Immunol. 1994;24:518–522. doi: 10.1002/eji.1830240304. [DOI] [PubMed] [Google Scholar]
- 68.Nie M., Bal M.S., Yang Z., Liu J., Rivera C., Wenzel A., Beck B.B., Sakhaee K., Marciano D.K., Wolf M.T. Mucin-1 increases renal TRPV5 activity in vitro, and urinary level associates with calcium nephrolithiasis in patients. J. Am. Soc. Nephrol. 2016;27:3447–3458. doi: 10.1681/ASN.2015101100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kulathu Y., Hobeika E., Turchinovich G., Reth M. The kinase Syk as an adaptor controlling sustained calcium signalling and B-cell development. EMBO J. 2008;27:1333–1344. doi: 10.1038/emboj.2008.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rao S., Liu X., Freedman B.D., Behrens E.M. Spleen tyrosine kinase (Syk)-dependent calcium signals mediate efficient CpG-induced exocytosis of tumor necrosis factor alpha (TNFalpha) in innate immune cells. J. Biol. Chem. 2013;288:12448–12458. doi: 10.1074/jbc.M113.454405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferretti A.P., Bhargava R., Dahan S., Tsokos M.G., Tsokos G.C. Calcium/Calmodulin kinase IV controls the function of both T cells and kidney resident cells. Front. Immunol. 2018;9:2113. doi: 10.3389/fimmu.2018.02113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li Z., Lu J., Zeng G., Pang J., Zheng X., Feng J., Zhang J. MiR-129-5p inhibits liver cancer growth by targeting calcium calmodulin-dependent protein kinase IV (CAMK4) Cell Death Dis. 2019;10:789. doi: 10.1038/s41419-019-1923-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Satyam A., Tsokos M.G., Tresback J.S., Zeugolis D.I., Tsokos G.C. Cell-derived extracellular matrix-rich biomimetic substrate supports podocyte proliferation, differentiation, and maintenance of native phenotype. Adv. Funct. Mater. 2020;30:1908752. doi: 10.1002/adfm.201908752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Representative monochromatic (single red channel) images of the studied proteins in COVID-19 samples. Scale bar, 50μm.