Abstract
The COVID-19 pandemic has taken a toll on people’s mental health. Besides the indirect impact of the pandemic, a diagnosis of COVID-19 is itself associated with a greater risk of subsequent mental illness. Conversely, people with an existing psychiatric diagnosis are at an increased risk of getting COVID-19. Here, we discuss why this is the case.
The COVID-19 pandemic has taken a toll on people’s mental health. Besides the indirect impact of the pandemic, a diagnosis of COVID-19 is itself associated with a greater risk of subsequent mental illness. Conversely, people with an existing psychiatric diagnosis are at an increased risk of getting COVID-19. Here, we discuss why this is the case.
Main text
We start this discussion by reviewing the evidence for bidirectional associations between coronavirus disease 2019 (COVID-19) and mental illness that has emerged from interrogation of large-scale electronic health records (EHRs) data. We then outline what studies of this kind can and cannot tell us and discuss approaches that could be used to identify the mechanisms underpinning the bidirectional associations between COVID-19 and mental illness.
Evidence for a link between COVID-19 infection and subsequent mental illness
The first robust evidence for a link between COVID-19 and subsequent mental illness emerged from a cohort study based on an EHR network that, at the time, included over 62,000 patients diagnosed with COVID-19.1 This study showed that within the first 3 months after a diagnosis of COVID-19, 18% of patients receive a psychiatric diagnosis (mostly anxiety disorder and depressive disorder), which was significantly more than in matched cohorts of patients with other contemporaneous health events (such as influenza or other respiratory tract infections). These risks were not limited to patients with known prior mental illnesses: 5.8% of people received their first such diagnosis over the same period, again significantly higher than after other health events.
This study also showed that patients diagnosed with a mental illness in the year before the COVID-19 pandemic were at a 65% increased risk of being diagnosed with COVID-19, even after matching cohorts for known risk factors for COVID-19 (including age, sex, race, BMI, and physical comorbidities). This was the case across the three categories of mental illness investigated: mood disorders, anxiety disorders, and psychotic disorders. In another study, patients with existing mental illness were found to be at an increased risk of hospitalization and mortality from COVID-19.2
In a follow-up study based on over 236,000 patients diagnosed with COVID-19 from the same network, the incidence of mental illness 6 months after a diagnosis of COVID-19 continued to be elevated and extended to include psychotic and substance use disorders, as well as a range of neurological conditions.3 In this study, the more severely affected patients with COVID-19 (i.e., those requiring hospitalization, admission to intensive care, or those who developed encephalopathy while acutely ill) were found to be at a higher risk of developing mental illness. However, an increased rate of mental illness was also observed in patients who did not require hospitalization at the time of their COVID-19 illness.
What EHR data can and cannot tell us
Live EHR networks have become a new key resource to answer pressing epidemiological questions during the COVID-19 pandemic. While we have used TriNetX Analytics (EHRs from 81 million patients, mostly in the USA), others have used IBM Watson Health Explorys2 (a similarly large EHR network in the USA) or OpenSAFELY4 (an EHR network of 57 million patients in the UK).
EHRs reflect clinical practice. When a patient sees a healthcare professional, the latter adds an entry in their EHR and also indicates any new diagnosis they make and any medication they prescribe. As such, they reflect the actual utilization of healthcare resources (to some extent), which can help in planning service provision. However, they also reflect the imperfections of clinical practice, from misdiagnosis (giving the wrong diagnosis to a patient) to miscoding (incorrectly encoding a diagnosis in the EHR).
EHR networks have other limitations too.5 , 6 Patients might receive part of their care from a healthcare organization that is not contributing data to the EHR; this might include COVID-19 testing and could lead to under-recording or delayed recording of COVID-19 status in the EHRs being analyzed. Estimates of relative risks associated with COVID-19 are confounded by the fact that some people in the control cohorts will have had undiagnosed COVID-19 infection. From a global perspective, EHRs are limited to relatively few countries, with significant underrepresentation of many regions, precluding generalization of findings and preventing comparable studies in many locations, notably low- and middle-income countries. Finally, some variables are often missing from EHRs such as contextual socioeconomic data and lifestyle factors. Because these factors are likely to influence the association between COVID-19 infection and mental illness, EHR-based cohort studies cannot on their own assess causality nor therefore explain why COVID-19 is associated with mental illness. In the next two sections, we explore the ways in which this question can be answered.
Does COVID-19 cause mental illness?
COVID-19 could be associated with mental illness because it is a causal factor, or because COVID-19 and mental illness are linked by other factors not accounted for in the studies mentioned above. One way to identify the existence of a causal link between the two would be to conduct an intervention study. While human challenges of COVID-19 have been approved in the UK for specific purposes,7 they are unlikely to be approved, well controlled, and sufficiently powered to assess a link between COVID-19 and mental illness. But there is an alternative: interventions that reliably decrease the risk of COVID-19 can be used to estimate the causal effect on subsequent mental illness (insofar as the only way by which this intervention can modify the risk of mental illness is via it modifying the risk of COVID-19). This could be achieved, for instance, if it was possible to know the mental health outcomes (besides the COVID-19 infection status) of patients who were randomly allocated to the active vaccine group versus the control arm of the COVID-19 vaccine trials.
If intervention studies are not available, then sophisticated observational studies and instrumental variables can be used to provide evidence for a causal link—even if the evidence is not necessarily conclusive.8 If an instrumental variable can be reliably identified in EHR data, then EHRs might be used in these sophisticated study designs. However, if no instrumental variable (and no intervention study) is available, then we will likely need to resort to carefully controlled studies with thorough sensitivity analyses to provide evidence for or against a causal link between COVID-19 and mental illness. In particular, these studies will need to have data on all relevant covariates. Given that EHR data and other retrospective analyses lack data on many factors that are likely to confound the association (e.g., lifestyle factors), such an approach will best be implemented using dedicated prospective cohort studies.
If COVID-19 causes mental illness, how does it do so?
Let us assume that indeed there is a causal link between a diagnosis of COVID-19 and subsequent mental illness, the question remains: how is one causing the other? Understanding the mechanisms at play might pave the way to identifying or designing optimal interventions to mitigate the impact of COVID-19 on mental health. But answering this question is as challenging as it is important.
One place to start is to recognize that mental illnesses have biological, psychological, and social factors in the complex causal web from which they emerge. It is not difficult to imagine plausible mechanisms along all three of these dimensions. Biologically, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can enter the brain,9 the immune response triggered by COVID-19 might have neural effects,10 and the hypercoagulable state of COVID-1911 might impair brain structure and function via cerebrovascular effects. Psychologically, a diagnosis of COVID-19 might trigger fear of death or other serious consequences, which materializes in some patients as a mental illness. Socially, the need to self-isolate as a result of a diagnosis of COVID-19 might result in loss of status at work, loss of income, and loss of social support, providing the stressors which result in psychiatric disorder in some people.
Mechanisms are neither mutually exclusive nor are they necessarily the same for different categories of mental illness. For instance, we found a steep gradient of incidence of psychotic disorders after COVID-19 from patients not requiring hospitalization (lowest incidence) to patients admitted to intensive care or having encephalopathy at the time of their COVID-19 illness (highest incidence). The gradient was much less marked for mood and anxiety disorders. Specifically, the incidence of a first mood or anxiety disorder after COVID-19 was about twice as high among patients with encephalopathy at the time of their COVID-19 illness compared with those without, whereas the incidence of a first psychotic disorder was almost 6 times higher in those with versus without encephalopathy. Insomnia and dementia presented a similarly steep gradient. These observations suggest that different mechanisms might underpin the emergence of mood and anxiety disorders compared with psychosis, insomnia, and dementia post-COVID-19.
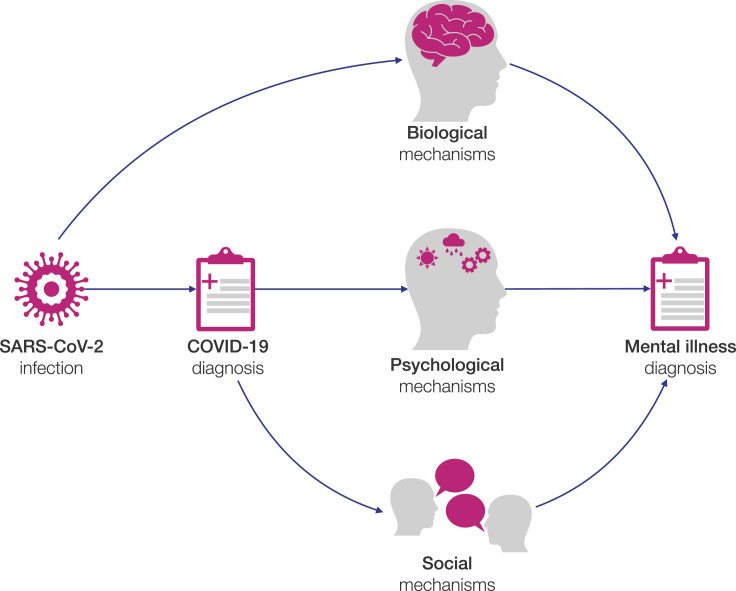
If we draw the possible causal relationships between the different elements at play (what is called, in causal inference parlance, a directed acyclic graph; Figure 1 ), something important emerges: biological mechanisms (if they are present) are triggered by infection with SARS-CoV-2 itself whereas psychological and social mechanisms (if they are present) are triggered by a diagnosis of COVID-19. Indeed, if the virus (or the immune response to it) has biological effects on the brain, then these effects will be present whether or not a diagnosis of COVID-19 has been made. Moreover, if a patient has been infected with the virus but does not have a diagnosis (e.g., because they were asymptomatic and did not get tested or because the test resulted in a false negative), then they won’t suffer the psychological and social consequences. We should qualify further what we mean by “diagnosis of COVID-19.” Obviously, if one develops symptoms of COVID-19 but does not get tested, the person might still believe they have caught COVID-19 despite the absence of a confirmed diagnosis. So “COVID-19 diagnosis” could be understood as a spectrum from “I know I had COVID-19” to “I am pretty certain I did not have COVID-19,” with “I think I had COVID-19” sitting somewhere between these extremes. This is important because “self-diagnosis” might trigger the same psychological and social cascade of effects as medically confirmed diagnoses.
Figure 1.
Possible causal mechanisms linking COVID-19 to mental illness
Direct acyclic graph illustrating how SARS-CoV-2 infection and COVID-19 diagnosis might be causally related to mental illness via biological, psychological, and social mechanisms.
The distinction between infection and diagnosis provides an opportunity to distinguish the biological effect from the psychological and social mechanisms. Indeed, it might be possible to detect retrospectively those patients who have been infected with SARS-CoV-2 without a diagnosis of COVID-19 being made at that time, by measuring the antibody levels in their blood. Many of these patients will have been unaware that they had COVID-19, and hence the biological mechanisms would have been activated but not the psychological and social ones. However, this approach would preferentially be focused on asymptomatic or mild COVID-19 infection, and results might not generalize to those who had experienced moderate or severe illness.
Finally, we might also be able to tell apart the psychological and social mechanisms (if we assume the latter are largely if not entirely mediated by the need to self-isolate). The mental health outcomes could be observed in people who have had to self-isolate without being infected with SARS-Cov-2 nor diagnosed with COVID-19 (e.g., pupils from school where there has been an outbreak; parents of a child whose nursery has had to close, etc). In such a study, particular attention would need to be paid to the absence of activated psychological mechanisms (e.g., if a pupil who had to self-isolate becomes fearful that they might have caught COVID-19 from their school friends).
Why are patients with mental illness at an increased risk of COVID-19?
The previous two sections have focused on how COVID-19 might be associated with subsequent mental illness. But, as noted above, a relationship in the opposite direction has also been observed: patients with mental illness (specifically a mood disorder, anxiety disorder, or psychotic disorder, corresponding to ICD-10 codes F20-F48) are at a 65% increased risk of getting COVID-19,1 even after adjusting for all other established risk factors for COVID-19 that were available in EHRs. The same issues apply to this relationship: is it causal, and if so, what might the mechanisms be?
This association might not be causal: a third factor (e.g., lifestyle factors) not available in EHRs might be causing both mental illness and COVID-19. But even if this is so, the finding remains clinically useful. Indeed, whatever that third factor might be, it does not appear to be routinely recorded in patients’ EHRs. As a result, such a hypothetical third factor might not be available to clinicians making a judgement about the risk of COVID-19 for an individual patient. In contrast, diagnoses of mental illness are readily available to all clinicians. A diagnosis of mental illness, in this case, can help assess the individual risk of COVID-19.
Conversely, the association between mental illness and increased risk of COVID-19 might be causal and might result from biological, psychological, and social mechanisms. Biologically, it might be that the pro-inflammatory state postulated to occur in some forms of psychiatric disorder predisposes to COVID-19, or that psychotropic medications increase the risk to COVID-19 (as it has been suggested for clozapine12). Psychologically, it might be that patients with mental illness depend on social interactions (both from healthcare professionals and from their support network) as part of their path to recovery, or it might be that impaired cognitive control affects patients’ ability to adhere to protective behaviors (e.g., social distancing). Socially, it might be that patients with mental illness have reduced access to relevant health information (e.g., because of smaller social networks) and have fewer opportunities to work from home (e.g., because of more precarious or manual jobs).
The mechanisms are likely to be varied and to form complex causal webs rather than simple causal links. Elaborate study designs are probably the only approach through which such a causal web can be analyzed and deciphered. If we assume that biological mechanisms are universal, whereas psychological and social mechanisms are (at least to some extent) culturally influenced, then comparing epidemiological studies from different areas of the world might be one place to start.
Conclusions
Large-scale EHR studies have established that there is an association between COVID-19 and subsequent mental illness but not why that is. To answer this question, we must first identify whether the association is causal and then reveal the mechanisms at play. The answers are needed if we are to devise effective and targeted interventions to mitigate the impact of COVID-19 on mental health and on patients with mental illness. Research of this kind may also reveal principles underlying links between infections in general (or even physical illness as a whole) and mental illness. As such, the COVID-19 pandemic creates a window of opportunity to understand better the profound and bidirectional connections between our physical and mental health.
Acknowledgments
Work supported by the National Institute for Health Research (NIHR) Oxford Health Biomedical Research Centre (grant BRC-1215-20005). M.T. is an NIHR Academic Clinical Fellow and an NIHR Oxford Health BRC Senior Research Fellow. The views expressed are those of the authors and not necessarily those of the UK National Health Service, NIHR, or the UK Department of Health.
Author contributions
M.T. and P.J.H. wrote the first draft, revised, and edited the manuscript.
Declaration of interests
M.T. is a clinical advisor to Akrivia Health which is unrelated to the work presented here. P.J.H. declares no competing interests.
References
- 1.Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson E.J., Walker A.J., Bhaskaran K., Bacon S., Bates C., Morton C.E., Curtis H.J., Mehrkar A., Evans D., Inglesby P., et al. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020;584:430. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casey J.A., Schwartz B.S., Stewart W.F., Adler N.E. Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annu. Rev. Public Health. 2016;37:61–81. doi: 10.1146/annurev-publhealth-032315-021353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon G.E. Big data from health records in mental health care: Hardly clairvoyant but already useful. JAMA Psychiatry. 2019;76:349–350. doi: 10.1001/jamapsychiatry.2018.4510. [DOI] [PubMed] [Google Scholar]
- 7.Callaway E. Dozens to be deliberately infected with coronavirus in UK ‘human challenge’ trials. Nature. 2020;586:651–652. doi: 10.1038/d41586-020-02821-4. [DOI] [PubMed] [Google Scholar]
- 8.VanderWeele T.J. Can sophisticated study designs with regression analyses of observational data provide causal inferences? JAMA Psychiatry. 2021;78:244–246. doi: 10.1001/jamapsychiatry.2020.2588. [DOI] [PubMed] [Google Scholar]
- 9.Meinhardt J., Radke J., Dittmayer C., Franz J., Thomas C., Mothes R., Laue M., Schneider J., Brünink S., Greuel S., et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat. Neurosci. 2021;24:168–175. doi: 10.1038/s41593-020-00758-5. [DOI] [PubMed] [Google Scholar]
- 10.Kreye J., Reincke S.M., Prüss H. Do cross-reactive antibodies cause neuropathology in COVID-19? Nat. Rev. Immunol. 2020;20:645–646. doi: 10.1038/s41577-020-00458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonaventura A., Vecchié A., Dagna L., Martinod K., Dixon D.L., Van Tassell B.W., Dentali F., Montecucco F., Massberg S., Levi M., Abbate A. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat. Rev. Immunol. 2021;21:319–329. doi: 10.1038/s41577-021-00536-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Govind R., Fonseca de Freitas D., Pritchard M., Hayes R.D., MacCabe J.H. Clozapine treatment and risk of COVID-19 infection: retrospective cohort study. Br. J. Psychiatry. 2020 doi: 10.1192/bjp.2020.151. Published online July 27, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]