Abstract
Operative treatment of osteoporosis-associated fragility fractures of the pelvis (FFP) and the sacrum is advocated with immobilizing or longstanding pain, fracture progression and displacement. We analyzed clinical outcomes regarding mobility, quality of life, and mortality of patients with FFP treated with trans-sacral bar (TB) osteosynthesis through S1. Demographics, clinical data, and operation-related data of patients with an FFP treated with TB were acquired from chart review. We assessed mortality, quality of life (EQ-5D), mobility, and residential status at follow-up. Seventy-nine females and six males with a median age of 78.0 years (IQR 73–84) were included, median follow-up was 3.2 years. Medical complications during hospitalization occurred in 28%. Operative revision was carried out in 15% of patients. One-year survival was 90.4%, this was associated with shorter preoperative and total length of stay in hospital (p 0.006 and 0.025, respectively). At follow-up, 85% lived at home and 82% walked with or without walking aid. Higher EQ-5D was reached with higher mobility status and living at home (p < 0.001 and < 0.001, respectively). TB osteosynthesis is an adequate and reliable method for fixation of FFP in the posterior pelvic ring to ensure timely mobilization. Shorter preoperative and total length of stay had lower mortality rates, advocating a standardized management protocol to limit time delay to operative therapy. Patients treated with TB osteosynthesis had low 1-year mortality of less than 10%.
Subject terms: Outcomes research, Trauma, Osteoporosis
Introduction
Fragility fractures of the pelvis (FFP) often lead to decreased mobility1, loss of independence and institutionalization2. Especially patients undergoing surgery had delayed presentation with a median of 14 days3. There is an excessive mortality4 with a 1-year mortality is as high as 17–30%1,4–6, similar to the 1-year mortality in hip fractures in elderly (19–33%)7,8. Surgically treated patients with an FFP had a lower mortality5.
Fractures of the posterior pelvic ring are found in 82% of FFP, mostly localized in the sacrum9. Surgical fixation of sacral fractures is usually performed by minimal-invasive iliosacral (IS) screws. Due to decreased bone mass in elderly and patients with a fragility fracture of the sacrum10,11, implant loosening with backing out is seen in 14–20% with 18% necessitating operative revision12,13. Alternatively, trans-sacral bar (TB) using washer and nuts on both sides14, augmented IS screws15, transiliac internal fixator16, or spinopelvic stabilization are used. Lower rates of implant loosening have been demonstrated when using trans-sacral implants13, confirmed by higher biomechanical strength compared to bilateral IS screws17. The shape and size of the upper sacrum limit safe trans-sacral implant positioning in half of patients18,19.
We retrospectively studied patients suffering from an FFP treated with minimal-invasive TB osteosynthesis through S1. By assessing medical and implant-related complications as well as mortality and functional outcome, our assumption was that TB osteosynthesis is a reliable and stable osteosynthesis of the posterior pelvic ring which lowers mortality due to better mobilisation.
Materials and methods
We retrospectively reviewed medical charts of adult patients with a pelvic fracture after low-energy trauma admitted at our center from 2005 to 2017. Low-energy fractures of the posterior pelvic ring were stabilized in 85 patients with TB (Fig. 1). Demographic and surgery-related data were collected: FFP classification according to Rommens and Hofmann9, operative details, length of stay (LOS), medical and implant-related complications, American Society of Anesthesiologists (ASA) physical status, medication, and following comorbidities: dementia, diabetes mellitus, cardiovascular disease, pulmonary disease, rheumatoid arthritis, and known malignancy. Symptomatic medical complications included: deep venous thrombosis, pulmonary embolism, cardiovascular events, urinary tract infections, pneumonia, and skin ulcer. Delayed presentation was defined as ≥ 7 days after trauma. Images were assessed for hip replacement or lumbar spine fusion.
Figure 1.

Flow diagram with patient inclusion and follow-up. FFP fragility fracture of the pelvis, FU follow-up. Graphic produced with draw.io (accessed 10.04.2020).
Treatment protocol
Patients with a FFP are admitted after complete diagnostics with conventional radiograph and CT scan. Isolated anterior fractures (FFP type 1) and non-displaced posterior lesions (FFP type 2) are treated conservatively with analgesics and physiotherapy-assisted mobilization. If these patients suffer immobilizing pain or prolonged pain without adequate mobilization after 5 to 7 days or if patients present posterior displaced fractures (FFP types 3 and 4, Fig. 2a,b), we recommend operative stabilization.
Figure 2.
92 year old female patient presenting 1 week after fall from standing height with immobilizing pain at lower lumbar spine. (a) Axial CT demonstrating slightly displacement of bilateral sacral fracture; (b) sagittal CT with displaced transversal fracture at S1/S2 level. The fracture was classified as FFP type IVb. (c) Lateral fluoroscopic image orientated in direction of the patient (bottom anterior, left cranial) showing overlapping of iliocortical densities and ischial notch. The drill guide is placed centrally in S1 corridor caudal to the iliocortical densities. (d) Oblique obturator view to assess the abutment of the washer on the iliac cortex. Postoperative control at discharge, patient is mobile with a walker ((e) anterior–posterior, (f) inlet, and (g) outlet view).
Trans-sacral bar osteosynthesis
Similar to IS screw, the TB crosses the vertical sacral fracture perpendicularly. Tightening of the nuts exerts slight interfragmentary compression. It is blocked bilaterally with locknuts; thus TB can be used in uni- and bilateral sacral fractures. The implant is load sharing, positioned in the center of weight transmission in S1: it transfers load from the spine to the posterior ilium. The strength of TB does not depend on the screw purchase in the reduced bone mass of the sacrum10,11, but on cortical bone of the posterior ilium.
Preoperative planning is mandatory19: the corridor’s dimension is evaluated in a coronal and axial view (according to the axis of the sacrum). Trans-sacral fixation should be avoided in dysmorphic sacra lacking safe space, the corridor’s dimension should be at least twice the TB’s diameter18. In these cases, a transiliac internal fixator or spinopelvic fixation is used. Bowel is prepped with purgatives the day before surgery for better intraoperative visualization.
The patient is placed prone on a radiolucent table. Fracture reduction is not carried out in posterior lesions of osteoporotic FFP. A strict lateral view is obtained using fluoroscopy, confirmed by overlapping of the sciatic notches and the iliocortical densities (ICD). The fluoroscopic image is orientated in the same direction as the patient (Fig. 2c). The S1 corridor is located caudally to the ICD, which marks the inner cortical layer of the iliac fossa near the IS joint. Subcutaneous tissue and muscles are split bluntly after skin incision. A 2.8 mm guide wire with drill bit is positioned centrally in the S1 corridor. With slight mallet blows, the first cortex is perforated. Using inlet and outlet projection, correct positioning is controlled and drilling is continued until it becomes palpable on the contralateral side. The anteroposterior position is confirmed with inlet view, the outlet view is used to assure position above the S1 sacral foramina. After contralateral skin incision the wire is held with a clamp. The wire is overdrilled with a 4.5 mm cannulated drill, leaving the 2.8 mm wire in place. A 6.0 mm non-cannulated sacral bar (Depuy Synthes, Oberdorf, Switzerland) mounted on a power drill is inserted in the prepared 4.5 mm canal. Under fluoroscopic control, the bar is inserted from one side to the other, while retracting the 2.8 mm drill from the other side tapping slightly against the tip of the sacral bar (kissing technique). After a washer and two nuts are placed and tightened contralaterally, the bar is retracted using backward drilling until the washer hits the lateral cortex of the ilium visible in the fluoroscope—tilted perpendicular to the posterior ilium (Fig. 2d). A washer and two nuts are inserted and slightly tightened. The overlapping part of the bar is cut with a bolt cutter. The TB is augmented with an IS screw on the fractured side to increase rotational stability. In cases of additional anterior stabilization, the patient is turned to supine position and again prepped. Conventional intraoperative fluoroscopy without navigation or 3D-imaging was used due to good experience in posterior pelvic fixation20. If possible, patients are mobilized with weight-bearing as tolerated. Routine postoperative imaging consisted of conventional X-rays with anteroposterior, inlet, and outlet view (Fig. 2e,f).
Follow-up (FU)
Patients or their relatives were contacted by phone21. If not possible, their general practitioner or the bureau of vital statistics was contacted to ask about vital status. Quality of life (QoL) was assessed by EuroQol 5D (EQ-5D) 5 level questionnaire, scores range from − 0.205 to 1.0 (higher indicates better QoL)22. The actual place of living and mobility status was asked, the mobility specified by Parker Mobility Score (PMS), ranging from 0 to 9 (higher indicates better mobility)23. Numeric pain score (NRS) and subsequent osteoporotic fractures were questioned.
Statistics
Normal distribution was assessed with Kolmogorov–Smirnov test. Descriptive statistics were described as mean and standard deviation in normally distributed data and as median and interquartile range (IQR) for non-normally distributed data. Groups were compared using the nonpaired Students t-test (normally distributed data) and the Mann–Whitney-U test (non-normally distributed data). Nominal groups were compared using the chi-square test, odds ratio (OR) and 95% confidence interval (CI) was calculated. Survival analysis was computed according to Kaplan–Meier. A p-value of ≤ 0.05 was considered significant. Statistical analysis was performed using SPSS software (IBM SPSS Statistics, Version 23; IBM Corp, Armonk, NY, USA).
Ethics
Approval for this retrospective study has been granted by the local ethics committee (837.140.17 (10974); Ethics Commission of the State Chamber of Medicine of Rhineland-Palatinate, Germany). Patients confirmed voluntary participation with the study, informed consent was obtained by living patients or their legal guardian. This study was conducted in accordance with Good Clinical Practice Guidelines.
Results
We included 85 patients treated with TB osteosynthesis (Table 1). Seventy-nine were females (92.9%) and six males (7.1%). The median age was 78.0 years (IQR 73–84, 50–95; median for males 85, and females 77, p 0.358). Time from trauma or begin of symptoms to presentation was at median 15 days (IQR 4–81, 0–863), two patients could not specify.
Table 1.
Fracture-related information and medical history.
| Number (total = 85) | Percentage | ||
|---|---|---|---|
| Trauma mechanism | |||
| Fall from standing height | 53 | 63% | |
| No trauma memorable | 30 | 35% | |
| Recurrent falls | 2 | 2% | |
| FFP classification | |||
| FFP 2 (posterior non-displaced) | 31 | 36% | |
| 2a | 6 | ||
| 2b | 16 | ||
| 2c | 9 | ||
| FFP3 (posterior unilateral displaced, all 3c) | 3 | 4% | |
| FFP4 (posterior bilateral displaced) | 51 | 60% | |
| 4b | 46 | ||
| 4c(1) | 5 | ||
| Concomitant fracture anterior pelvis | |||
| None | 22 | 26% | |
| Unilateral | 45 | 53% | |
| Bilateral | 18 | 21% | |
| ASA | |||
| ASA 2 | 24 | 28% | |
| ASA 3 | 57 | 67% | |
| ASA 4 | 4 | 5% | |
| Comorbidities | |||
| Dementia | 6 | 7% | |
| Cardiovascular disease | 68 | 80% | |
| Pulmonary disease | 11 | 13% | |
| Diabetes mellitus | 13 | 15% | |
| Rheumatoid arthritis | 6 | 7% | |
| Known malignancy | 25 | 29% | |
| Preexisting osteoporosis | 63 | 74% | |
| Number or comorbidities (2) | |||
| 0 | 7 | 8% | |
| 1 | 38 | 45% | |
| 2 | 29 | 34% | |
| 3 | 11 | 13% | |
| Medication | |||
| Corticosteroids | 8 | 9% | |
| Anticoagulation | 15 | 18% | |
| Antithrombotics | 21 | 25% | |
| Previous hip replacement | 17 | 20% | |
| Previous lumbar fusion | 4 | 5% | |
(1) All with sacral fracture and contralateral crescent fracture of the ilium.
(2) Counting: Dementia, cerebrovascular disease, pulmonary disease, diabetes mellitus, rheumatoid arthritis, known malignancy.
Surgery
Operation was carried out at a median of 5 days after admission (IQR 2–8.5, 0–26). Fifty-two patients (61%) had additional posterior implants; anterior instability was addressed in 38 patients (Table 2).
Table 2.
Detailed operative treatment of posterior and anterior pelvis.
| Number | % | |
|---|---|---|
| Posterior implants | 85 | |
| TB alone | 33 | 39% |
| TB + unilateral IS screw | 16 | 19% |
| TB + bilateral IS screws (3 patients with cement augmentation) | 31 | 36% |
| TB + anterior plate iliac plate trough 1st window of ilioninguinal approach | 4 | 5% |
| TB + spinopelvic fixation | 1 | 1% |
| Anterior instability | 63 | |
| No anterior stabilization | 15 | 24% |
| Plate osteosynthesis via modified Stoppa approach | 21 | 33% |
| Unilateral retrograde transpubic screw | 23 | 37% |
| Bilateral retrograde transpubic screw | 3 | 5% |
| Unilateral retrograde transpubic screw + plate osteosynthesis via modified Stoppa approach | 1 | 1% |
TB trans-sacral bar; IS ilio-sacral.
There were no serious vascular or neurologic complications, no fracture progression occurred in the posterior pelvis. Thirteen patients (15.3%) underwent revision surgery related to TB:
Four patients had revision for a loosened TB (all without additional IS screws and all with delayed presentation, two with persisting anterior instability and one with non-union of the sacral fracture); two of these patients developed peri-implant infection after the revision operation needing operative debridement.
Four hematomas required operative debridement (one with additional interventional coiling). One infected hematoma was debrided. One peri-implant infection with an epidural abscess was debrided.
Two TB were removed due to pain (one non-specific pelvic pain, one with pain in S1 dermatome due to malpositioning).
One malpositioned TB was removed and changed to a transiliac internal fixator.
Revision for TB did not correlate with age (p 0.490), nor with number of comorbidities (p 0.277) or grading of FFP (p 0.105). In two patients, a plate osteosynthesis of the anterior pelvic ring loosened over time and was revised.
Fifteen patients were admitted postoperatively to the ICU for 1 to 4 days (18%). The median total LOS was 18 days (IQR 14–24, 6–92), the postoperative LOS was 12 days (IQR 9–15.5, 3–74).
Medical complications occurred in 24 patients (28%) during hospitalization: 15 urinary tract infections, 4 pneumonias, 4 skin ulcers, 3 deep venous thromboses, one of those had a pulmonary embolism, and one cardiovascular event. Complications correlated with larger total (p 0.003, median 24 vs 17 days) and preoperative LOS (p 0.007, median 4 vs 7 days), there was no correlation with patient’s age (p 0.685), ASA (p 0.744), number of comorbidities (p 0.958), postoperative LOS (p 0.252) or presentation with delay (p 0.268). Mobility and residential status at discharge and FU are depicted in Table 3.
Table 3.
Mobility and residential status at discharge and time of follow up.
| At discharge | At follow-up | % | |||
|---|---|---|---|---|---|
| Mobility | |||||
| Mobile on ward | 34 | 40% | Walking without aid | 10 | 18% |
| Mobile in room | 12 | 14% | Walking with aid | 35 | 64% |
| Transfer bed—wheelchair | 34 | 40% | Transfer bed—wheelchair | 8 | 14% |
| Bedridden | 4 | 5% | Bedridden | 2 | 4% |
| Unknown | 1 | 1% | |||
| Residential status | |||||
| Home independent with aid | 21 | 25% | 46 | 84% | |
| Nursing home | 14 | 17% | 3 | 5% | |
| Rehabilitation | 24 | 28% | 1 | 2% | |
| Geriatric ward | 20 | 23% | 5 | 9% | |
| Other hospital | 5 | 6% | |||
| Unknown | 1 | 1% | |||
Follow-up
Overall, median FU was 166.9 weeks (IQR 82–259, 2–663). Twenty-nine patients were reported dead (35%) during complete FU (four died later than FU interview), the status of one was unknown (Fig. 1). They died at a mean of 148.8 weeks after admission (± 121, 4.6–469). Cumulative survival rate according to Kaplan–Meier was 90.4% after 1 year, 86.3% after 2 years, and 57.4% after 5 years (Fig. 3).
Figure 3.
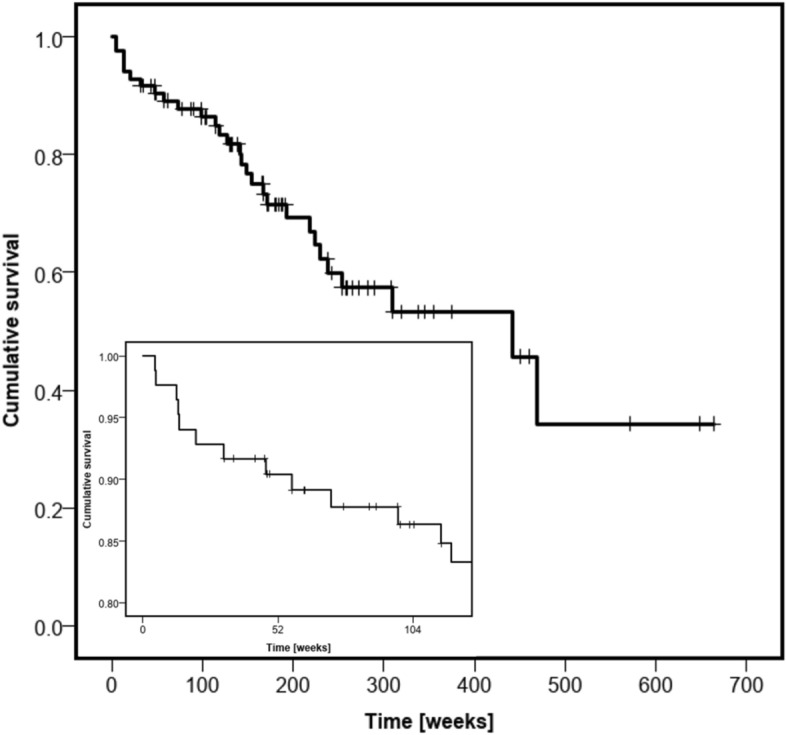
Kaplan–Meier survival analysis. Insert highlights survival in first 2 years of follow-up.
One-year mortality correlated with a longer total (p 0.006, median 24 vs 17 days) and preoperative LOS (p 0.025, median 10 vs 4 days), however postoperative LOS did not (p 0.337, median 14 vs 12 days). Patients did not differ in age (p 0.94, median 78.0 for dead vs 78.5), ASA score (p 0.62, median 3.0 for dead vs 3.0), number of comorbidities (p 0.47, median 2.0 for dead vs 1.0) or gender (p 0.42, all females). There was a higher risk of 1-year mortality in patients with a medical complication (OR 8.44, 95% CI 1.49–47.70, p 0.006). No statistical difference was found for patients walking at discharge (OR 0.37, 95% CI 0.07–2.02, p 0.234), presenting > 1 week after trauma (OR 1.04, 95% CI 0.19–5.82, p 0.963), or undergoing revision surgery (OR 2.15, 95% CI 0.37–12.50, p 0.387).
Median FU of the 55 living patients was 173.4 weeks (IQR 99–282, 31–663; Table 3). Twenty patients (36%) sustained another osteoporotic fracture during FU at a mean of 122.9 weeks (± 91.8, 5.3–369.7). The mean EQ5D-index was 0.527 (± 0.30, − 0.205 to 1.0). It correlated with mobility (PMS, R 0.660, p < 0.001) and pain (NRS, R − 0.433, p 0.001), there was no correlation with age (R 0.031, p 0.823), ASA (R − 0.108, p 0.433), and number of comorbidities (R 0.017, p 0.903). There was a higher EQ5D with walking at FU (0.60 vs 0.21, p < 0.001) and living at home at FU (0.59 vs 0.20, p < 0.001). No correlation was found to mobility at discharge (walking 0.54 vs 0.51, p 0.722). The median PMS was 5.0 (IQR 3–6, 0–9), it was higher in patients living at home at FU (median 6 vs. 0, p < 0.001). Age (R − 0.237, p 0.081), pain-level (NRS, R 0.027, p 0.844), and walking at discharge from hospital (median 5 for both, p 0.72) did not correlate. Twenty-eight patients (51%) did take some kind of anti-osteoporotic medication at follow-up.
Discussion
We reported 85 patients suffering from an FFP treated with TB. The 28% medical complication rate and 18 days median LOS represent the frail, multimorbid patient collective. Revision surgery for surgery-related complications was necessary in 15%. There was a high 1-year survival rate of 90%. After a mean follow-up of more than 3 years, 84% of surviving patients were living at home and 82% were walking. However, one-third did suffer another osteoporotic fracture during follow-up.
The patients requiring surgery for FFP are geriatric patients with a median age of 78 years, they were mostly frail, often reported a fall from standing height, and presented with multiple comorbidities. Seventy-two percent had an ASA of 3 or higher, which is more than in previous studies with 49–68%1,13,24. Half of the patients had two or more comorbidities. A median LOS of 18 days could be explained by failed trial of conservative treatment, preoperative conditioning, medical complications, or operative revisions. In literature, there is a range of LOS from 4.5 days up to 39 days, probably due to different local medical structures as co-geriatric management1,25. Risk factors for prolonged hospital admission include combined posterior and anterior pelvic ring injuries1 and operative management5.
The golden standard for FFP is conservative treatment. Patients with immobilizing or prolonged pain, displaced fractures or fracture progression3 may profit from surgical stabilization. In conservative treatment, the rate of medical complications is 20–53%1,26,27. Operatively treated patients tend to have less medical complications (13–28%)16,24,28,29. We confirmed lower complication rates with surgery (28%). Longer total and preoperative LOS in hospital correlated with medical complications. This advocates a timely decision for surgery, if necessary.
In our series, we did not have serious vascular or neurologic complications. Operative revision was required in 15% of our patients, other case series mentioned 6–16%13,16,28,29. All loosened implants (4.7%) were in patients with delayed presentation and without additional posterior osteosynthesis13. This supports a prompt operative intervention if conservative treatment fails. We suppose that bilateral locking with locknuts prevent loosening compared to 9% loosening in trans-sacral fixation using conventional screws. We changed our practice to augment TB with an additional IS screw on the fractured side. This may decrease rotation around the axis of the TB30. Less loosening and backing out in IS screw fixation in elderly was shown by using multiple posterior implants13. Anterior fixation, whenever possible minimally invasive using retrograde trans-pubic screws31 or alternatively using plate osteosynthesis32, is important to allow immediate mobilization if there is a concomitant anterior instability. Half of the loosened TB were observed in patients with persistent anterior instability3.
We confirmed the low 1-year mortality after surgical treatment of FFP (10–12%)13,29 compared to conservative treatment (17–23%)1,4,6,25,27,33. Elderly with a pelvic fracture show an increased mortality4. The 1-year mortality after surgical treatment of proximal femur fracture is higher with 19–33%7,8. This study showed increased mortality at 1 year if a medical complication occurred. Interestingly, there was no correlation to age, ASA, number of comorbidities, or with reduced mobility at discharge.
At a follow-up of more than 3 years, patients were living at home in 84% with 16% being institutionalized at that moment. A similar institutionalization rate of 9–13% 6 months after a pelvic fracture in elderly was observed in an insurance-based study from Germany2. Markedly higher institutional rates at follow-up were reported in literature with 25–51%1,13,25–27. Only 25% of our patients were primarily discharged home, more than half went to a rehabilitation or geriatric unit. Patients may benefit from more intensive rehabilitation in such institutions after surgical fixation with a high number returning to their home during follow-up. The same may apply for the high rate of 82% mobilization.
The QoL was reduced to a certain extent with an EQ-5D index of 0.53. Normative data in Germany in a cohort of > 75 years was 0.771–0.88234. A similarly low index of 0.51 was described in patients with femoral neck fractures (mean age 80 years)35 and 0.61 in such with hip fractures (mean age 81 years)36, both exhibited significantly lower values at follow up as before the injury. With a median PMS of 5, the mobility was slightly more limited compared to proximal femur fractures with a mean of 5.8 after 12 months37.
As medical complications and 1-year mortality were increased in patients with longer total and preoperative LOS, a shorter preoperative time and hence shorter stay at the hospital may be beneficial. In geriatric hip fractures, a delay in surgery increased risk for mortality as well as for complications38. A standardized management protocol of analgetic medication and early assisted mobilization may be beneficial together with geriatric co-management.
To our best knowledge, this study represents the largest cohort of patients with trans-sacral fixation as well as operative treatment of FFP. Our study was limited by the large range of FU time with up to 5 years. We suppose a surgery-related difference in mortality and QoL is possible in the first months, however, once the fracture is healed, outcomes may be more dependent on comorbidities. The preoperative quality of life was not assessed, as large follow-up times and increasing age may lead to inconsistent answers. The duration of operation was not evaluated because of different anterior osteosynthesis techniques and change from prone to supine position in case of additional anterior stabilization. The same accounts for intraoperative blood loss. With minimal-invasive technique the blood loss is not collected and thus not measurable. Another limitation is the lack of control group using alternative surgical treatment methods. Although following our protocol to recommend operative treatment for patients with displaced posterior pelvic ring fractures (FFP types 3 and 4) and in non-displaced fractures (FFP type 2) after failed conservative treatment, there may be a selection bias due to the operative expertise in our centre. Suffering from a pelvic fracture after none or a low-energy trauma was defined as fragility fracture, although osteoporosis was not formally assessed by bone mineral density measurement39.
Conclusion
Trans-sacral bar osteosynthesis is a safe and effective technique to mobilize patients with FFP. We recommend a standardized management protocol and, if necessary, timely operative fixation in patients with FFP to lower LOS, increase QoL, and decrease mortality. Posterior augmentation with IS screw and concomitant anterior fixation of instability is recommended.
Acknowledgements
The data collection which forms the base of this original work, has been possible by means of an educational grant of the Zimmer Biomet Company, Sulzerallee 8, P.o. Box CH-8404, Winterthur, Switzerland, IRE2017-56CH. We sincerely thank Ms. Kirsten Schuelke for meticulous data collection. The study includes data from the doctoral thesis of two of the authors (GP and SK).
Author contributions
D.W.: initiation and concept of the project; data acquisition, processing and analysis; writing and revision of the manuscript. M.K.: concept of the project, data collection, processing and analysis, critical revision of the manuscript. G.P.: data collection and processing. S.K.: data collection and processing. I.M.: data collection and processing; revision of the manuscript. A.H.: concept of the project, data collection and processing. P.M.R.: concept of the project, data analysis, critical revision of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Loggers SAI, Joosse P, Jan PK. Outcome of pubic rami fractures with or without concomitant involvement of the posterior ring in elderly patients. Eur. J. Trauma Emerg. Surg. 2019;45(6):1021–1029. doi: 10.1007/s00068-018-0971-2. [DOI] [PubMed] [Google Scholar]
- 2.Benzinger P, Riem S, Bauer J, et al. Risk of institutionalization following fragility fractures in older people. Osteoporos. Int. 2019;30(7):1363–1370. doi: 10.1007/s00198-019-04922-x. [DOI] [PubMed] [Google Scholar]
- 3.Rommens PM, Arand C, Hopf JC, Mehling I, Dietz SO, Wagner D. Progress of instability in fragility fractures of the pelvis: An observational study. Injury. 2019;50(11):1966–1973. doi: 10.1016/j.injury.2019.08.038. [DOI] [PubMed] [Google Scholar]
- 4.Andrich S, Haastert B, Neuhaus E, et al. Excess mortality after pelvic fractures among older people. J. Bone Miner. Res. 2017;32(9):1789–1801. doi: 10.1002/jbmr.3116. [DOI] [PubMed] [Google Scholar]
- 5.Höch A, Özkurtul O, Pieroh P, Josten C, Böhme J. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr. Orthop. Surg. Rehabil. 2017;8(1):3–9. doi: 10.1177/2151458516681142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rommens PM, Hopf JC, Herteleer M, Devlieger B, Hofmann A, Wagner D. Isolated pubic ramus fractures are serious adverse events for elderly persons: An observational study on 138 patients with fragility fractures of the pelvis type I (FFP type I) J. Clin. Med. 2020;9(8):2498. doi: 10.3390/jcm9082498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, et al. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. 2019;14(1):203. doi: 10.1186/s13018-019-1226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mariconda M, Costa GG, Cerbasi S, et al. The determinants of mortality and morbidity during the year following fracture of the hip: A prospective study. Bone Jt. J. 2015;97:383–390. doi: 10.1302/0301-620X.97B3.34504. [DOI] [PubMed] [Google Scholar]
- 9.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 2013;44(12):1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 10.Wagner D, Hofmann A, Kamer L, et al. Fragility fractures of the sacrum occur in elderly patients with severe loss of sacral bone mass. Arch. Orthop. Trauma Surg. 2018;138(7):971–977. doi: 10.1007/s00402-018-2938-5. [DOI] [PubMed] [Google Scholar]
- 11.Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM. Sacral bone mass distribution assessed by averaged three-dimensional CT models: Implications for pathogenesis and treatment of fragility fractures of the sacrum. J. Bone Jt. Surg. Am. 2016;98(7):584–590. doi: 10.2106/JBJS.15.00726. [DOI] [PubMed] [Google Scholar]
- 12.Reuther G, Röhner U, Will T, Dehne I, Petereit U. CT-guided screw fixation of vertical sacral fractures in local anaesthesia using a standard CT. RöFo Fortschritte Auf Dem Geb Röntgenstrahlen Nukl. 2014;186(12):1134–1139. doi: 10.1055/s-0034-1366605. [DOI] [PubMed] [Google Scholar]
- 13.Eckardt H, Egger A, Hasler RM, et al. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: Assessment of complications and factors influencing failure. Injury. 2017;48(12):2717–2723. doi: 10.1016/j.injury.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury. 2012;43(4):446–451. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Suero EM, Greiner A, Becker CA, et al. Biomechanical stability of sacroiliac screw osteosynthesis with and without cement augmentation. Injury. 2020 doi: 10.1016/j.injury.2020.01.043. [DOI] [PubMed] [Google Scholar]
- 16.Schmitz P, Baumann F, Acklin YP, et al. Clinical application of a minimally invasive cement-augmentable Schanz screw rod system to treat pelvic ring fractures. Int. Orthop. 2019;43(3):697–703. doi: 10.1007/s00264-018-3988-6. [DOI] [PubMed] [Google Scholar]
- 17.Zhao Y, Li J, Wang D, Liu Y, Tan J, Zhang S. Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury. 2012;43(4):490–494. doi: 10.1016/j.injury.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 18.Wagner D, Kamer L, Sawaguchi T, et al. Space available for trans-sacral implants to treat fractures of the pelvis assessed by virtual implant positioning. Arch. Orthop. Trauma Surg. 2019 doi: 10.1007/s00402-019-03204-9. [DOI] [PubMed] [Google Scholar]
- 19.Wagner D, Kamer L, Sawaguchi T, et al. Critical dimensions of trans-sacral corridors assessed by 3D CT models: Relevance for implant positioning in fractures of the sacrum. J. Orthop. Res. 2017;35(11):2577–2584. doi: 10.1002/jor.23554. [DOI] [PubMed] [Google Scholar]
- 20.Rommens PM, Nolte EM, Hopf J, Wagner D, Hofmann A, Hessmann M. Safety and efficacy of 2D-fluoroscopy-based iliosacral screw osteosynthesis: Results of a retrospective monocentric study. Eur. J. Trauma Emerg. Surg. 2020 doi: 10.1007/s00068-020-01362-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Devine A, Taylor SJC, Spencer A, Diaz-Ordaz K, Eldridge S, Underwood M. The agreement between proxy and self-completed EQ-5D for care home residents was better for index scores than individual domains. J. Clin. Epidemiol. 2014;67(9):1035–1043. doi: 10.1016/j.jclinepi.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Hout B, Janssen MF, Feng Y-S, et al. Interim scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–715. doi: 10.1016/j.jval.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Parker M, Palmer C. A new mobility score for predicting mortality after hip fracture. J. Bone Jt. Surg. Br. 1993;75:797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 24.Osterhoff G, Noser J, Held U, Werner CML, Pape H-C, Dietrich M. Early operative versus nonoperative treatment of fragility fractures of the pelvis: A propensity-matched multicenter study. J. Orthop. Trauma. 2019;33(11):e410–e415. doi: 10.1097/BOT.0000000000001584. [DOI] [PubMed] [Google Scholar]
- 25.Studer P, Suhm N, Zappe B, Bless N, Jakob M. Pubic rami fractures in the elderly—A neglected injury? Swiss Med. Wkly. 2013;143:w13859. doi: 10.4414/smw.2013.13859. [DOI] [PubMed] [Google Scholar]
- 26.Breuil V, Roux CH, Testa J, et al. Outcome of osteoporotic pelvic fractures: An underestimated severity. Survey of 60 cases. Jt. Bone Spine. 2008;75(5):585–588. doi: 10.1016/j.jbspin.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 27.Mears SC, Berry DJ. Outcomes of displaced and nondisplaced pelvic and sacral fractures in elderly adults. J. Am. Geriatr. Soc. 2011;59(7):1309–1312. doi: 10.1111/j.1532-5415.2011.03455.x. [DOI] [PubMed] [Google Scholar]
- 28.Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury. 2015;46(8):1631–1636. doi: 10.1016/j.injury.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 29.Höch A, Pieroh P, Henkelmann R, Josten C, Böhme J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: A prospective, observational study with 1-year follow-up. BMC Surg. 2017;17(1):132. doi: 10.1186/s12893-017-0330-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hammer N, Steinke H, Lingslebe U, et al. Ligamentous influence in pelvic load distribution. Spine J. 2013;13(10):1321–1330. doi: 10.1016/j.spinee.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 31.Rommens PM, Graafen M, Arand C, Mehling I, Hofmann A, Wagner D. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury. 2020;51(2):340–346. doi: 10.1016/j.injury.2019.12.018. [DOI] [PubMed] [Google Scholar]
- 32.Herteleer M, Boudissa M, Hofmann A, Wagner D, Rommens PM. Plate fixation of the anterior pelvic ring in patients with fragility fractures of the pelvis. Eur. J. Trauma Emerg. Surg. 2021 doi: 10.1007/s00068-021-01625-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park J-W, Park S-M, Lee HJ, Lee C-K, Chang B-S, Kim H. Mortality following benign sacral insufficiency fracture and associated risk factors. Arch. Osteoporos. 2017;12(1):100. doi: 10.1007/s11657-017-0395-3. [DOI] [PubMed] [Google Scholar]
- 34.Szende A, Janssen B, Cabases J, editors. Self-Reported Population Health: An International Perspective Based on EQ-5D. Springer; 2014. [PubMed] [Google Scholar]
- 35.Tidermark J, Zethraeus N, Svensson O, Törnkvist H, Ponzer S. Femoral neck fractures in the elderly: Functional outcome and quality of life according to EuroQol. Qual. Life Res. 2002;11(5):473–481. doi: 10.1023/a:1015632114068. [DOI] [PubMed] [Google Scholar]
- 36.Hack J, Buecking B, Aigner R, et al. What are the influencing factors in self-rated health status after hip fracture? A prospective study on 402 patients. Arch. Osteoporos. 2019;14(1):92. doi: 10.1007/s11657-019-0642-x. [DOI] [PubMed] [Google Scholar]
- 37.Kammerlander C, Hem ES, Klopfer T, et al. Cement augmentation of the proximal femoral nail antirotation (PFNA)—A multicentre randomized controlled trial. Injury. 2018;49(8):1436–1444. doi: 10.1016/j.injury.2018.04.022. [DOI] [PubMed] [Google Scholar]
- 38.Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318(20):1994. doi: 10.1001/jama.2017.17606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rommens PM, Drees P, Thomczyk S, Betz U, Wagner D, Hofmann A. Die Fragilitätsfraktur des Beckens ist eine Indikatorfraktur der osteoporose. Osteologie. 2018;27(03):144–153. doi: 10.1055/s-0038-1673536. [DOI] [Google Scholar]



