Abstract
Background: Health inequities are among debatable and challenging aspects of health systems. Achieving equity through social determinants of health approach has been mentioned in most upstream national plans and acts in Iran. This paper reports the findings of a systematic review of the current synthesized evidence on health equity in Iran.
Methods: This is a narrative systematic review. The relevant concepts and terminology in health equity was found through MeSH. We retrieved the relevant studies from PubMed/MedLine, Social Sciences Database, and Google Scholar in English, plus the Jihad University Database (SID), and Google Scholar in Farsi databases from 1979 until the end of January 2018. The retrieved evidence has been assessed primarily based on PICOS criteria and then Ottawa-Newcastle Scale, and CASP for qualitative studies. We used PRISMA flow diagram and a narrative approach for synthesizing the evidence.
Results: We retrieved 172 455 studies. Following the primary and quality appraisal process, 114 studies were entered in the final phase of the analysis. The main part (approximately 95%) of the final phase included cross-sectional studies that had been analyzed through current descriptive inequality analysis indicators, analytical regression, or decomposition-based approaches. The studies were categorized within 3 main groups: health outcomes (40.3%), health utilization (32%), and health expenditures (27%).
Conclusion: As a part of understanding the current situation of health equity in the policymakers’ need to refer the retrieved evidence in this study, they need more inputs specially regarding the social determinants of health approach. It seems that health equity research plan in Iran needs to be redirected in new paths that give appropriate weights to biological, gene-based, environmental and contextbased, economic, social, and political aspects of health as well. We advocate addressing the aspects of Social Determinant of Health (SDH) in analyzing health inequalities.
Keywords: Health Equity, Health Inequality, Health Care Disparity, Health Care Inequality, Health Social Determinants, Health Care Availability, Health Care Accessibility, Health Disparity, Health Care Utilization
↑ What is “already known” in this topic:
Health inequalities are evident in Iran. Despite various theoretical concepts, measurement methods and hypothetical approaches available to tackle the problem in the country, a comprehensive and national review on the status of health equity is still lacking in Iran.
→ What this article adds:
This study systematically synthesizes the existing evidence to assist policymakers understand and realize the dimensions of health equity. Iran needs more efforts toward redirecting the agenda setting for both investigation and action regarding health equity.
Introduction
Health equity and equal access to health services for various socioeconomic groups are among ultimate goals of any health system. Nonetheless, the concept of health equity has been contr oversial, rendering an ongoing debate among health policymakers and planners over the past decades (1). Significant inequities in various aspects of health, ie, health outcomes, utilization of health services, and health financing (2), are major concerns in all contexts, ie, low, middle- and high-income countries. The publication of a series of regular reports began by Black in the 1980s in England, which was followed by other countries, including the United States (3). This was a global turning point in health inequity analysis. Ever since, many studies have focused on the impact of socioeconomic factors on the health status of the community. In addition, health equity has been the subject of many studies from different aspects, ie, availability, accessibility, utilization, healthcare payment and financing, morbidity, and mortality, while studies have focused on children, adolescents and young adults, elderly, women, and different ethnicities across various settings (3-7).
Given the key role of equity in improving community health, a number of international and national organizations have made continuous efforts to reduce health inequities. For instance, during the last 2 decades, the World Bank (WB), in cooperation with other agencies, eg, the World Health Organization (WHO), have worked with member states to improve the health and nutrition status and demographic indicators as well as protecting the population against the consequences of illness, malnutrition, and high fertility (5). Health equity and equitable access to healthcare services are also strongly endorsed by the Iranian constitution and other upstream policies, eg, various national development plans. Nonetheless, achieving these objectives still remains a big challenge (8-10). Health equity analysis has been a popular research topic at the provincial and national levels during the recent decades in Iran, eg, the 2 rounds of Urban HEART (Health Equity Assessment Research Tool) project in the capital city of Tehran, a collaboration among WHO, Tehran Municipality, and the Ministry of Health and Medical Education (MOHME) (11), Iran's Multiple Indicator Demographic and Health Survey (IrMIDHS) (12), and the Urban and Rural Expenditure-Income Survey (13). These efforts alongside a relative rich body of health equity analysis in the country show us the importance of health equity as a main concern for both academicians and government. Anyway, we need to monitor the trend of health equity researches in the country through a comprehensive lens. This implies on answering the following question:
- What are the main methodological approaches in health equity analysis in the country?
- What dimensions and scopes of health equity have been more addressed, and which ones need to be a part of research agenda for helping policymakers?
To achieve the objectives of health equity, it is pivotal to determine the current status and document the existing studies, plans, and synthesized knowledge about health equity. Nevertheless, comprehensive and national reviews with consistent evidence on health equity status is still lacking in Iran. This study aims to provide the current gap in conducting health equity studies in Iran through a systematic review approach. This implies on synthesizing the evidence for Iranian health policymakers to realize in which dimensions of the health equity the country needs more efforts, and then redirecting the research policy agenda to them.
Methods
Search Strategy
This was a systematic review of the literature on health inequity in Iran between 1979 (the beginning of the Islamic revolution) until 01/31/2018. We used the PRISMA flow diagram and a narrative approach for synthesizing the evidence. We searched PubMed/MedLine, Cochrane Library, and Google Scholar in English as well as the Jihad University Database (SID) and Google Scholar in Farsi. Because of the nature of health equity analysis, it can be considered as an interdisciplinary field between health and medical sciences and social sciences. This means that health equity encompasses the health, medical, social, economic, political, environmental, philosophical, religious, and criminal dimensions. Therefore, we approached our search strategies through seeking PubMed/Medline, and Social Sciences Databases, the first of which is a biological, health and medical sciences database, and the second contains all aspects of the social sciences.
We found the MeSH terms for various terms and expressions as presented below:
Health Care Equality, Health Care Fairness, Health Care Utilization, Health Care Accessibility, Health Care Availability, Health Care Affordability, Horizontal Equity in Health Care, Vertical Equity in Health Care, Health Services Equality, Health Services Fairness, Health Services Accessibility, Health Services Availability, Health Services Affordability, Horizontal Equity in Health Services, Vertical Equity in Health Services, Inequality in Health, Disparity in Healthcare, Health Care Inequalities, Inequalities, Healthcare Disparity, Financial Protection in Health, Catastrophic and Impoverishing in Health Services, Fairness in Financial Contribution in Health, Gender Inequality in Health. Appendix presents the search strategy by databases.
Studies Primary Assessment
Two team members (H.G.H. and E.M.) were responsible for the primary assessment of the studies, and in case of any disagreement, a third person (A.T.) was involved.
The details are provided as follows:
P (Health Problem): Studies that address all aspects of health equity (as mentioned in search strategy keywords above) in Iran.
I (Intervention): No restriction for this criterion. All clinical, social, economic, and cultural interventions in clinical, individual, social, national and macro contextual context were considered.
C (Comparator): This criterion was also is in line with the intervention and there was no restriction on comparators.
O (Outcomes): Biological, health-related measures, morality, morbidity, quality of life, and wider consequences in the social context of Iran were considered.
S (Study Design): All studies that assessed various aspects of socioeconomic inequalities through descriptive analysis, calculation of regression coefficient for different inequality indicators as well as qualitative, longitudinal, case-control, cohort, and cross-sectional studies were included.
Exclusion Criteria: We excluded the Iranian immigrants living in other countries. In addition, we excluded protocol studies during the final phase. As some national research projects and studies were conducted through collaborations between the international agencies, eg, the World Health Organization, with the Iranian national authorities, eg, the Ministry of Health and Medical Education (MoHME), Tehran Municipality, etc., in both Persian and English, we considered them as primary, and if qualified, appraised them qualitatively.
Data Extraction and Study Quality Assessment: We used the Newcastle-Ottawa Scale for the critical appraisal of the remained studies from the primary screening stage. All studies in this stage were nonrandomized controlled trials (non RCTs); thus, we used Newcastle-Ottawa Scale for assessing their quality (14).
In addition, for the critical appraisal of the qualitative studies, a systematic review was done using Cambridge Quality Appraisal tools (15, 16).
Critical appraisal was done by B.A. and M.M.K., and any discrepancies were discussed with E.M. The results of the quality appraisal of the studies are included in various tables of summary of articles.
Data Extraction and Synthesis: Data on the included studies were extracted by E.M. and M.M.K. through a checklist that included the author(s) names, year of publication, title of the study, aim(s), study type, sample size, data gathering tools and methods, main results, and conclusions. All data were used to present the results of the current study thorough a narrative synthetic approach.
We categorized the included studies based on 5 characteristics: study design; outcome variables; method of analysis; level of study; and the publication year, as described in Table 1. Most studies were analytical, analyzed service variables (hospitalization, outpatient, paraclinical, pharmacy, etc.), and used concentration index (CI) as a main indicator (Table 1). Because some papers used more than 1 tool in the analysis, the total number of included articles in the Data analysis categorywas 147 (instead of 114 actual papers included in this review). We present our findings based on the 3 dimensions of equity: health outcomes, utilization, and financing. As previously mentioned, we were faced with a wide range of topics as our main outcomes, and grouping them was a major challenge, so we used the World Bank health equity researchers approach to summarize and present the results in an organized fashion (7).
Table 1. Descriptive characteristics of the 114 selected articles .
| Characteristics | Number | Proportion (%) | |
| Study design | Case-control | 2 | 1.75 |
| Case study | 2 | 1.75 | |
| Descriptive | 27 | 23.68 | |
| Analytical | 74 | 64.91 | |
| Qualitative | 5 | 4.39 | |
| Mix methods | 4 | 3.51 | |
| Outcome variables | Health status, diseases, disorders and illness | 24 | 21.1 |
| Resources (bed, medicine, equipment, human and financial resources) | 26 | 22.8 | |
| Risky behavior | 2 | 1.8 | |
| Risk Factors in Health | 9 | 7.9 | |
| Mortality (by age) | 10 | 8.8 | |
| Services (inpatient, outpatient, para clinical, pharmacy, etc.) | 34 | 29.8 | |
| Others (pregnancy, inequality, attitudes, health literacy, etc.) Others (pregnancy, inequality, attitudes, health literacy, etc.) | 9 | 7.9 | |
| Data analysis method/ tool/ indicator | Concentration Index (CI) | 42 | 28.6 |
| Gini Coefficient (GC) | 20 | 13.6 | |
| The decomposition of inequality | 27 | 18.4 | |
| Catastrophic health expenditure | 23 | 15.6 | |
| GIS | 4 | 2.7 | |
| Other (gradient inequality, Robin Hood, Kakwani, dissimilarity, disparity) | 24 | 16.3 | |
| Qualitative, Combined | 7 | 4.8 | |
| Study Level | Local | 30 | 26.3 |
| Provincial | 31 | 27.2 | |
| National | 53 | 46.5 | |
| Year of publication | 2000-2005 | 3 | 2.6 |
| 2006-2010 | 9 | 7.9 | |
| 2011-2015 | 65 | 57.0 | |
| 2016-2018 | 37 | 32.5 |
Results
Figure 1 summarizes the flowchart of our literature review and data extraction process, based on PRISMA protocol (Fig. 1).
Fig. 1.
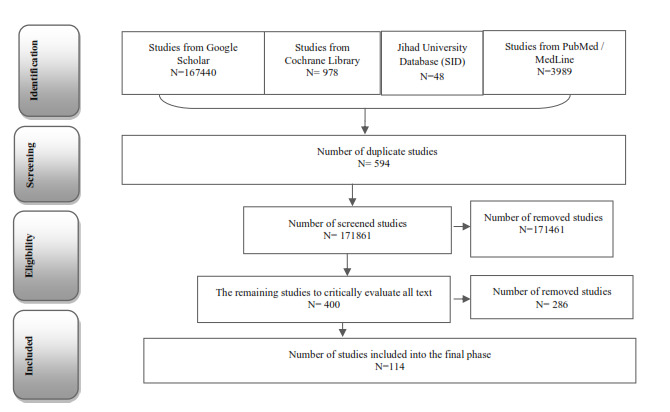
Data extraction process.
Studies’ Characteristics
A major part (approximately 65%) of the included studies were analytical that aimed to investigate the association between health outcome(s) inequality with socioeconomics and demographics determinants. Calculating and analyzing the health services (cares) inequality constructed about 30% of the interested outcomes by researchers. Also, 26.4% of the study have used Concentration index as their main inequality analysis indicator. About 46.5% of the studies are national level studies, which means they have used data extracted from national surveys for analyzing health inequality. The main part of the studies (57%) has been performed between 2011 through 2015. Details of the studies’ characteristics are available in Table 1.
1. Health Outcomes:Investigating the factors that affect health equity outcomes was the main focus in 36 articles (15-60 in Table 2). We included all studies whose focus were life expectancy, mortality, quality of life, and incidence of diseases and health disorders (both mental and physical) in this category. These articles documented that inequality in demographic variables can affect the health outcomes.
Table 2. Summary of articles focusing on equity in health outcomes .
| Author(s) | Aims | Study Design | Newcastle-Ottawa Scale** | Main outcome(s) |
| Emamian MH, Fateh M, Hosseinpoor AR, Alami A, Fotouhi A.(17) | To describe socio-economic inequality with obesity and its associated factors | A cross-sectional study through analyzing the national surveillance data for 2005 | Good |
Slop index of inequality Concentration Index Decomposition inequality in obesity |
| Farzadi F, Ahmadi B, Shariati B, Alimohamadian M, Mohamad K.(18) | Looks at the trend in the population gender ratio from 1956 to 2006, with a focus on analyzing mortality rates and hence the overall health of Iranian women | A cohort analysis on population censuses in Iran | Good | “Comparison of Mortality in the 25–34 years age group in 1956–1966 compared with subsequent decades. |
| Gooshki ES, Rezaei R, Wild V.(19) |
To shed light on the health of migrants in Iran from the perspective of social justice |
A systematic Review | Satisfactory | Adverse health consequences for population |
| Moradi-Lakeh M, Bijari B, Namiranian N, Olyaeemanesh A-R, Khosravi A. (20) | To assess the trend of geographical disparities between rural areas | A trend observational study | Good |
Crude Mortality Rate Neonatal Mortality rate Infant Mortality Rate Under Five Mortality Rate |
| Nedjat S, Hosseinpoor AR, Forouzanfar MH, Golestan B, Majdzadeh R. (21) | This study aims to estimate health inequality between different socioeconomic groups and its determinants | A cross-sectional study through a Population survey in Tehran | Good |
Concentration Index Decomposing socio-economic factors affecting the health status |
| Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Jafarzadehpur E, et al. (22) | To investigate economic inequality and its determinants in near vision, in a middle-aged population | A cross-sectional study | Good | The main contributors of gap between lower and higher socio-economic group through Oaxaca-Blinder Decomposition |
| Morasae EK, Forouzan AS, Majdzadeh R, Asadi-Lari M, Noorbala AA, Hosseinpoor AR. (23) | To measure socioeconomic inequality in mental health, and then to untangle and quantify the contributions of potential determinants of mental health to the measured socioeconomic inequality | A cross-sectional study through a Population survey in Tehran | Good | “The overall CI of mental health in Tehran was -0.0673 (95% CI = -0.070 - -0.057). Decomposition of the CI revealed that economic status made the largest contribution (44.7%) to socioeconomic inequality in mental health. Educational status (13.4%), age group (13.1%), district of residence (12.5%) and employment status (6.5%).” |
| Ramezani Doroh V, Vahedi S, Arefnezhad M, Kavosi Z, Mohammadbeigi A. (24) | To decompose the health inequality of people living in Shiraz | A cross-sectional study through a multistage-sample survey | Good |
Concentration Index for Mental and General Health Decomposing inequality |
| Veisani Y, Delpisheh A. (25) | To understand the determinants of socioeconomic inequality of mental health in the female-headed households | A cross-sectional study | Satisfactory |
Concentration Index Decomposing Inequality |
| Amirian H, Poorolajal J, Roshanaei G, Esmailnasab N, Moradi G. (26) | The effect of inequity on health outcomes was investigated via a three-stage procedure | A cross-sectional study through a multistage-sample survey | Good | Concentration Index |
| Khajavi A, Pishgar F, Dehghani M, Naderimagham S. (27) | To assess inequalities in infant mortality in rural regions | A trend analysis in national scale | satisfactory | Comparing the decreasing rate of mortality over the time |
| Alizadeh M, Laghousi D. (28) | To assess the trend of geographical disparities in child and maternal mortality rates | A population-based trend analysis | satisfactory | Index of Disparity in Neonatal, Infant and Under Five Mortality Rates between 1999 and 2013. |
| Rarani MA, Rashidian A, Arab M, Khosravi A, Abbasian E.(29) | To measured socioeconomic inequality in under-five mortality in Iran and across its provinces. | A cross-sectional study on multiple indicator demographic and health Survey | satisfactory | Concentration Index for Under Five Mortality Rate. |
| Kiadaliri AA. (30) | To assess gender and social disparities in Esophagus cancer incidence across Iran’s provinces through 2003-2009 | A trend analysis by Iran National Statistical Centre | Satisfactory | Rate ratios and Kunst and Mackenbach relative indices of inequality (RIIKM) were used to assess gender and social inequalities |
| Kiadaliri AA, Saadat S, Shahnavazi H, Haghparast-Bidgoli H. (31) | To assess overall, gender and social inequalities across Iran’s provinces during 2006–2010. | A time trend province-level study | Good | Rate ratio and Kunst and Mackenbach relative index of inequality were used to assess overall, gender and social inequalities, respectively. |
| Ghorbani Z, Ahmady AE, Ghasemi E, Zwi A. (32) | To identify the socioeconomic distribution of perceived oral health among adults | A cross-sectional population-based survey in Tehran | Good | Concentration Index of non-replaced extracted teeth (NRET), and m perceived dental health |
| Hosseinpoor AR, Mohammad K, Majdzadeh R, Naghavi M, Abolhassani F, Sousa A, et al. (33) | To measure the socioeconomic inequality in infant mortality in Iran | A cross-sectional study on Iran Demographic and Health Survey data | Good |
Concentration Index in Infant Mortality Decomposition Inequality |
| Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R, et al. (34) | To quantify the determinants' contributions of socioeconomic inequality in infant mortality | A cross-sectional study on Iran Demographic and Health Survey data | Good | Decomposing of Inequality |
| Almasi-Hashiani A, Sepidarkish M, Safiri S, Morasae EK, Shadi Y, Omani-Samani R.(35) | To determine the economic inequality in history of stillbirth and understanding determinants of unequal distribution of stillbirth in Tehran, Iran. | A population-based cross-sectional study | Good | “Decomposition of the Concentration Index of stillbirth |
| Rad EH, Khodaparast M. (36) | Taxation system and health insurance contribution of Iranians were assessed | A cross-sectional analysis on data obtained from Iran Statistical Center. | Satisfactory | Kakwani Index of health insurance contribution |
| Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. (37) | To report the status of the unmet refractive need and the role of economic inequality | A cross-sectional nested case-control | Good | Oaxaca-Blinder decomposition method of unmet refractive need |
| Hosseinkhani Z, Nedjat S, Aflatouni A, Mahram M, Majdzadeh R. (38) | To assess the association of child maltreatment with socioeconomic status among schoolchildren | A cross-sectional study | Satisfactory | Concentration Index of child maltreatment |
| Mansouri A, Rarani MA, Fallahi M, Alvandi I. (39) | To estimate and decompose educational inequalities in the prevalence of IBS | A cross-sectional study | Good | Concentration Index |
| Fateh M, Emamian MH, Asgari F, Alami A, Fotouhi A.(40) | To investigate the socioeconomic inequality of hypertension in Iran and to identify its influencing factors | A cross-sectional study | Good |
Slop index of inequality (SII) and concentration index (C) for hypertension. Oaxaca–Blinder decomposition |
| Moradi G, Ardakani HM, Majdzadeh R, Bidarpour F, Mohammad K, Holakouie-Naieni K. (41) | To determine the socioeconomic status (SES) of inequalities and the proportion of the determinants in nonuse of seat belts in cars and helmets on motorcycles | A cross-sectional study | Good | The concentration index, concentration curve, and comparison of Odds Ratio (OR) in different SES groups were used to measure the socioeconomic inequalities using logistic regression. |
| Veisani Y, Delpisheh A, Moradi G, Hassanzadeh J, Sayehmiri K. (42) | To estimate the relationship between the socioeconomic status and addiction and mental disorders in suicide attempts | A cross-sectional study | Good | concentration index (CI) and decomposing contribution in inequality |
| Tourani S, Zarezadeh M, Raadabadi M, Pourshariati F.(43) | Determining regional disparity of obstetrics and gynecology services and its association with children and infant mortality rates | A cross-Sectional Study | Satisfactory | Gini Coefficient |
| Entezarmahdi R, Majdzadeh R, Foroushani AR, Nasehi M, Lameei A, Naieni KH.(44) | To measure inequality of disability in leprosy | A cross-sectional study | Satisfactory | extended concentration index decomposition |
| Moradi G, Mohammad K, Majdzadeh R, Ardakani HM, Naieni KH.(45) | To determine socioeconomic inequalities in risk factors for NCDs | A trend analysis of inequality | Good | Concentration Index |
| Naghdi S, Ghiasvand H, Zadeh NS, Azami S, Moradi T.(46) | To estimate the impact of some macro-economic factors specially inequality factors on the Iranian rural health status | A time trend ecological study | Satisfactory | Gini Coefficient |
| Kiadaliri AA.(47) | Investigating social disparities in breast cancer (BC) and ovarian cancer (OC) incidence rates among women | A time trend province-level study | Satisfactory | rate ratio and Kunst and Mackenbach relative index of inequality were used to assess social disparities |
| Kia AA, Rezapour A, Khosravi A, Abarghouei VA.(48) | To assess the socioeconomic inequality in malnutrition in under-5 children | A crosse-sectional study | Good | Concentration Index |
| Moradi G, Moinafshar A, Adabi H, Sharafi M, Mostafavi F, Bolbanabad AM. (49) | To evaluate socioeconomic inequalities in the oral health status | A crosse-sectional study | Satisfactory | Concentration Index |
| Kiadaliri AA, Asadi-Lari M, Kalantari N, Jafari M, Mahdavi MRV, Faghihzadeh S.(50) | To examine educational inequalities among adults | A population based cross-sectional study | Good | Slope Index of Inequality (SII) and the Relative Index of Inequality (RII) |
| Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A.(51) | To explore inequality in visual impairment | A cohort study | Good | Blinder-Oaxaca decomposition |
| Hosseini M, Olyaeemanesh A, Ahmadi B, Nedjat S, Farzadi F, Arab M, et al.(52) | To identify the state of gender equity in the health sector of the Islamic Republic of Iran | A mixed method | Satisfactory | Gender Inequality in different aspects of health indicators |
| Moradi G, Majdzadeh R, Mohammad K, Malekafzali H, Jafari S, Holakouie-Naieni K.51 | To determine the status of diabetes socioeconomic inequality and the share of determinants of inequalities | A time trend comparative study | Good |
Concentration Index Decomposition Inequality |
| Emamian MH, Fateh M, Gorgani N, Fotouhi A.(53) | To describe the socio-economic inequality in stunting and its determinants | A cross-sectional population-based | Good |
Concentration Index Oaxaca-Blinder Decomposition |
| Raeisi A, Mehboudi M, Darabi H, Nabipour I, Larijani B, Mehrdad N, et al.(54) | To investigate the socioeconomic inequality of overweight and obesity among the elderly | prospective cohort study | Good | Concentration Index and the Lorenz curve |
| Safiri S, Kelishadi R, Heshmat R, Rahimi A, Djalalinia S, Ghasemian A, et al.(55) | To describe the socioeconomic inequality associated with oral hygiene behavior | A cross-sectional Study | Good | Concentration Index (C) and the slope index of inequality (SII) |
| Peykari N, Djalalinia S, Qorbani M, Sobhani S, Farzadfar F, Larijani B. (56) | Summarizing evidences on associations between socioeconomic factors and diabetes in Iranian population | A systematic review | Good | The prevalence of diabetes among different socio-economic and demographic groups. |
| Ravaghi H, Goshtaei M, Olyaee Manesh A, Abolhassani N, Arabloo J (57) | Obtain a deeper understanding of the development of health equity indicators and identify their implementation challenges | A qualitative study | Satisfactory | Shaping the stakeholder’s perspective for different health inequality indicators |
| Zaboli R, Tourani S, Seyedin SH, Manesh AO (58) | To determine and prioritize the social determinants of health inequality in Iran | A mixed method | Good | Shaping framework for including SDH approach in health equity |
| Beheshtian M, Manesh AO, Bonakdar S, Afzali HM, Larijani B, Hosseini L, et al.(59) | Determining health equity indicators in Iran | A literature review | Satisfactory | “52 indicators have been determined as health equity indicators in five areas including health, social and human development, economic development, physical environment and infrastructure and governance. “ |
| Sadeghipour Roudsari H, Sherafat Kazemzadeh R, Rezaeie M, Derakhshan M.(60) | To assess the knowledge, attitudes and practices of men, Iranians and Afghan refugees, regarding reproductive health | A cross-sectional Study | Satisfactory | “Mean scores for knowledge, attitudes and practices for Iranians were 4.38/30, 13.89/20 and 12.99/31 respectively; for Afghans the scores were 3.79/30, 11.66/20 and 11.88/31.” |
2. Healthcare Utilization: A total of 37 (32%) studies focused on utilization of health services and analyzed the availability, accessibility, and use of health services. For instance, they measured the distribution of health facilities (bed and human resources, etc.,) and access to health care services, which may help improve the distribution policies of health care resources in the country. The results also revealed a meaningful unequal distribution of resources among affluent and deprived areas in Iran and thus the need to redistribute the resources to improve equity in access. Table 3 presents a summary of the objectives and findings of these studies.
Table 3. Summary of articles focusing on equity in healthcare utilization .
| Author(s) | Aims | Study Design | Newcastle-Ottawa Scale** | Main outcome(s) |
| Bidgoli HH, Bogg L, Hasselberg M.(61) | To assess the distribution of pre-hospital trauma care facilities reflect the burden of Road Traffic Injury (RTI) and Mortality (RTM) | Cross-Sectional Ecological Study | Good | Lorenz curves and Gini coefficients |
| Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. (62) | To investigate and decompose the determinants of healthcare utilization (HCU) | Cross-Sectional Population based | Good | Decomposing Inequality |
| Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. (63) | To determine and compare the socioeconomic inequity in HCU by CI and odds ratio (OR) | Cross-Sectional Population based | Good | Concentration Index |
| Noroozi M, Rahimi E, Ghisvand H, Qorbani M, Sharifi H, Noroozi A, et al.(64) | To explore the relative contributions of inequality in utilization of NSPs and to decompose it to its determinants | Cross-Sectional Survey | Good | Decomposing Inequality |
| Davari M, Maracy MR, Aslani A, Bakhshizadeh Z, Khorasani E.(65) | To evaluate the equity in access to pharmaceutical services | Cross-Sectional | Good | Concentration and Lorenz curves. |
| Ramandi SD, Niakan L, Aboutorabi M, Noghabi JJ, Khammarnia M, Sadeghi A. (66) | To determine how doctors, paramedics and hospital beds are distributed in Iran | Trend Analysis | Satisfactory | Gini Coefficient |
| Kiadaliri AA, Najafi B, Haghparast-Bidgoli H.(67) | To evaluate the distribution of need and access to health care services among Iran's rural population | Cross-Sectional Ecological Study | Good | Lorenz Curve, Gini Coefficient, Decile ratio and Index of Dissimilarity |
| Kavosi Z, Mohammadbeigi A, Ramezani-Doroh V, Hatam N, Jafari A, Firoozjahantighi A. (68) | To measure horizontal inequity in access to outpatient services | Cross-Sectional Population based Survey | Good |
Concentration Index Horizontal Inequity Index |
| Karyani AK, Azami SR, Rezaei S, Shaahmadi F, Ghazanfari S. (69) | To investigate the geographical distribution of gynecologists and midwives and to determine their distribution trend | Cross- Sectional | Satisfactory | Gini Coefficient |
| Meshkini AH, Kebriaeezadeh A, Janghorban MR, Keshavarz K, Nikfar S.(70) | To analyze the geographic distribution and accessibility of pharmacies in the municipal territory for both pedestrians and drivers | A cross-sectional geographical based study | Satisfactory | straight-line distance measurements |
| Hajizadeh M, Connelly LB, Butler JR, Khosravi A.(71) | To analyze inequities of health care utilization | A cross-sectional population-based study | Good |
Concentration Index Horizontal Inequity Index |
| Noroozi M, Sharifi H, Noroozi A, Rezaei F, Bazrafshan MR, Armoon B.(72) | To explore the contribution of economic status to inequality in unprotected sex among people who inject drugs (PWID) | A cross-sectional behavioral survey in Tehran | Good | Oaxaca-Blinder Decomposition |
| Geravandi S, Najafi M, Rajaee R, Mahmoudi S, Pakdaman M. (73) | To compare the distribution of burn beds with its disability-adjusted life years (DALY) in Iran | A cross-sectional study | Satisfactory | Gini Coefficient |
| Sefiddashti SE, Arab M, Ghazanfari S, Kazemi Z, Rezaei S, Karyani AK. (74) | To determine the trend of inequality in the allocation of human resources in the health sector | A cross-sectional study | Satisfactory | Gini Coefficient |
| Honarmand R, Mozhdehifard M, Kavosi Z. (75) | To determine distribution of maternal and child health related workforces | A cross-sectional study | Satisfactory | Gini Coefficient |
| MORADI LM, Ramezani M, Naghavi M.(76) | To determine the equality in safe delivery indices, i.e., appropriate place of delivery, type of delivery and skilled attendant for delivery, and their determinants in Iran. | A cross-sectional study | Good | Concentration Index for appropriate place of delivery, normal vaginal delivery and skilled attendant for deliver |
| Meskarpour-Amiri M, Mehdizadeh P, Barouni M, Dopeykar N, Ramezanian M.(77) | To determine the trend of inequality in the distribution of intensive care beds | A cross-sectional study | Satisfactory | Gini Coefficient for ICU and NICU beds |
| Jadidi R, Mohammadbeigi A, Mohammadsalehi N, Ansari H, Ghaderi E.(78) | To evaluate the inequity in timely vaccination with a focus on inequities in timeliness | A historical cohort study | Good | Concentration Index of mother and father’s education for timely vaccination |
| Masoodi M, Rahimzadeh M.(79) | To investigate geographical accessibility of residential areas to health services | A cross-sectional geographical information system | Good | Floating Catchment Area (FCA), minimum distance methods and Response Time (RT) accessibility technique |
| Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. (80) |
To assess the role of economic inequality in the utilization of eye care services, and to identify its determinants |
A cohort study | Good | Oaxaca-Blinder decomposition of ophthalmologist or optometrist Examination. |
| Homaie Rad E, Ghiasi A, Arefnezhad M, Bayati M. (81) | Inequalities between general physicians’ (GP) and specialists’ visits; also, the factors effecting the utilization of visits were determined | A cross-sectional population-based study | Satisfactory | Concentration Index of general practitioners and specialists’ visits. |
| Kazemi Karyani A, Kazemi Z, Shaahmadi F, Arefi Z, Ghazanfari S.(82) | To investigate the inequality and trend of geographic accessibility to Pediatricians | A time trend analysis | Satisfactory | Gini Coefficient and Index of Dissimilarity of accessibility to pediatrics |
| Meskarpour-Amiri M, Dopeykar N, Ameryoun A, Tavana AM. (83) | To examined inequality in geographical distribution of cardiovascular health services | A cross-sectional study | Satisfactory | Gini Coefficient of CCU beds and Cardiologist |
| Mobaraki H, Hassani A, Kashkalani T, Khalilnejad R, Chimeh EE.(84) | To assess distribution of all human resources in public sector of the country | A cross-sectional study | Satisfactory | Gini Coefficient and Rabin hood indexes for human resources distribution |
| Omrani-Khoo H, Lotfi F, Safari H, Jame SZB, Moghri J, Shafii M. (85) | To examine both equality and equity in resources distribution | A cross-sectional study | Good | Gini Coefficient and Rabin hood and Concentration Index of hemodialysis beds |
| Sari AA, Rezaei S, Rad EH, Dehghanian N, Chavehpour Y. (86) | To investigate the disparity in the distribution of health physical resources | A cross-sectional retrospective study | Good | Gini Coefficient, Gaswirth index and Index of Dissimilarity of Health physical resources |
| Mohammadbeigi A, Arsangjang S, Mohammadsalehi N, Anbari Z, Ghaderi E. (87) | To estimate the inequity related to the educational level of parents on the access and utilization of oral health care | A cross-sectional study | Good | concentration (C) index of inequity related to the educational level of parents on the access and utilization of oral health care |
| Rad EH, Kavosi Z, Arefnezhad M.(88) | To describe inequality in dental care utilization in Iran | A cross-sectional population-based study | Good | concentration index of dental care utilization in Iran |
| Hatam N, Zakeri M, Sadeghi A, Ramandi SD, Hayati R, Siavashi E.(89) | To assess the distribution of hospital beds in Shiraz in 2014 | A retrospective cross-sectional study | Satisfactory | Gini Coefficient of hospital beds |
| Ameryoun A, Meskarpour-Amiri M, Dezfuli-Nejad ML, Khoddami-Vishteh H, Tofighi S.(90) | to evaluate the inequality of geographical distribution of non-cardiac intensive care beds | A cross-sectional study | Satisfactory | geographical distribution of non-cardiac intensive care beds in Iran using the Gini coefficient |
| Hashemi H, Rezvan F, Fotouhi A, Khabazkhoob M, Gilasi H, Etemad K, et al. (91) | To investigate distribution of the cataract surgical | A cross-sectional study | Satisfactory | Concentration Index of Cataract Surgery per 1 million population |
| Reshadat S, Saedi S, Zangeneh A, Ghasemi S, Gilan N, Karbasi A, et al. (92) | To analyze the spatial accessibility to urban primary-care centers of the population in Kermanshah city, Islamic Republic of Iran | A descriptive-analytical study over 3 time periods | Good | The analysis was based on a standard radius of 750 m distance from health centers, walking speed of 1 m/s and desired access time to health centers of 12.5 mins. |
| Rezaei S, Karyani A, Fallah R, Matin B. (93) | To evaluate inequalities in the geographical distribution of human and physical resources in the health sector | A cross-sectional study | Satisfactory | Gini coefficient for human resources |
| Chavehpour Y, Rashidian A, Raghfar H, Emamgholipour sefiddashti S, Maroofi A.(94) | To assesses the ‘inverse care law’ hypothesis: whether hospitals tended to be built in the relatively better-off areas through the time | A longitudinal time-series study | Good | Gini Coefficient of public and private beds. |
| Nemati R, Seyedin H, Nemati A, Sadeghifar J, Nasiri AB, Mousavi SM, et al. (95) | To examine the disparities in access to health care services | A cross-sectional study | Satisfactory | Scalogram analysis model to access to health care services. |
| Yari A, Nedjat S, Asadi-Lari M, Majdzadeh R (96) | Gaining a deeper understanding of people’s perception on inequality of health and its determinants | A qualitative | Good | “Consensus on social, mental and physical health inequality |
| Mohammadi S, Gargari SS, Fallahian M, Källestål C, Ziaei S, Essén B.(97) | To investigate whether care quality for maternal near miss (MNM) differed between Iranians and Afghans and identify potential preventable attributes of MNM | cross-sectional study | Good | risk of maternal near miss (MNM) and suboptimal care among Afghan rather Iranians |
3. Health Financing:A total of31 (27%) of the studies addressed equity in health financing. The major concern about equitable health financing is inequalities between the poor and the rich. Three main focus areas of equity in health financing are OOP, catastrophic payments (those that exceed a prespecified threshold), and impoverishing payments (those that cause a household to fall below the poverty line). A brief overview of the objectives and results of these studies is presented in Table 4.
Table 4. Summary of articles focusing on equity in health financing .
| Citation | Aims | Study Design | Newcastle-Ottawa Scale** | Summary Results |
| Rezapour A, Arabloo J, Tofighi S, Alipour V, Sepandy M, Mokhtari P, et al.(98) | To determine the equity in health care payments and determining factors among households | A cross-sectional study | Good | Catastrophic and Impoverishing Health care expenditure |
| Rezapour A, Ghaderi H, Azar FE, Larijani B, Gohari MR.(99) | To determine the effects of OOP payment for health care services on households | A cross-sectional study | Good | Concentration Index for capacity to pay and health care payments |
| Zare H, Trujillo AJ, Driessen J, Ghasemi M, Gallego G. (100) | Inequalities assessment of health care expenditures | A longitudinal study | Good | Kakwani Index of health expenditures |
| Davari M, Kheyri M, Nourbakhsh SMK, Khadivi R. (101) | To evaluate households’ health financial protection in different quintiles after implementation of family physician. | A time trend study | Satisfactory | Comparison between different socio-economic group by Chi Square |
| Khammarnia M, Keshtkaran A, Kavosi Z, Hayati R.(102) | To investigate the households' impoverishment due to the healthcare costs | A cross-sectional study | Satisfactory | Health care expenditure impoverishing effect |
| Delavari H, Keshtkaran A, Setoudehzadeh F. (103) | To determine the percentage of households with cancer patients that face catastrophic health expenditures. | A cross-sectional study | Satisfactory | Catastrophic health expenditures. |
| Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. (104) | To assessed change in household catastrophic health care expenditures | A longitudinal population-based study | Good | The proportion of household facing catastrophic health expenditure (CHE) |
| Fazaeli AA, Seyedin H, Moghaddam AV, Delavari A, Salimzadeh H, Varmazyar H, et al.(105) | To present a trend analysis for the indicators related to fairness in healthcare’s financial burden | A time trend study | Satisfactory |
“The percentage of people with Catastrophic Health Expenditure Fairness in Financial Contribution |
| Juyani Y, Hamedi D, Jebeli SSH, Qasham M.(106) | To investigate on what extent Multiple sclerosis patients face catastrophic costs. | A cross-sectional study | Satisfactory | Ratio of catastrophic costs |
| Hajizadeh M, Connelly LB.(107) | To examine the progressivity of health insurance premiums and consumer co-payments | A time trend analysis | Good | Kakwani Progressivity Indices |
| Hajizadeh M, Nghiem HS.(108) | To provide a understanding about the inequality and determinants of the CHE for hospital services | A cross-sectional study | Good | out-of-pocket expenditure (OOPE) and the related catastrophic expenditure (CE) for hospital services |
| Reshadat S, Najafi F, Karami-Matin B, Soofi M, Barfar E, Rajabi-Gilan N, et al. (109) | To measure the financial protection against CHE among hospitalized patients | A cross-sectional study | Satisfactory |
Mean of Out-of-Pocket Payment Catastrophic health Expenditure |
| Ghorbanian A, Rashidian A, Lankarani KB, Kavosi Z. (110) | To estimate the pooled prevalence of CHE in Iran and identifying | A systematic review and meta-analysis | Good | Pooled Prevalence of Catastrophic Health Expenditure |
| Ghoddoosinejad J, Jannati A, Gholipour K, Baghestan EB.(111) | To calculate households encountered with catastrophic healthcare expenditures | A cross-sectional study | Satisfactory | Rate of households encountered to catastrophic health expenditures |
| Mansouri A, Emamian MH, Zeraati H, Hashemi H, Fotouhi A.(112) | To estimate and decompose economic inequality in presenting visual acuity | A cohort study | Good | Concentration Index |
| Kavosi Z, Keshtkaran A, Hayati R, Ravangard R, Khammarnia M. (113) | Investigated the Household Financial Contributions to the health system | A cross-sectional study | Good | Fairness Financial Contribution Index |
| Piroozi B, Moradi G, Nouri B, Bolbanabad AM, Safari H. (114) | Explore the percentage of households facing CHE after the implementation of HSEP | A cross-sectional study | Good | Catastrophic Health Expenditure |
| Rarani MA, Rashidian A, Khosravi A, Arab M, Abbasian E, Morasae EK.(115) | Decompose inequality in neonatal mortality into its contributing factors | A comparative longitudinal study | Good | Inequality in neonatal mortality by normalized Concertation Index |
| Daneshkohan A, Karami M, Najafi F, Matin BK.(116) | To estimate FFCI and quantify extent of catastrophic household heath expenditures | A cross-sectional study | Good | The proportion of households facing catastrophic health expenditures |
| Moghadam MN, Banshi M, Javar MA, Amiresmaili M, Ganjavi S.(117) | Measure percentage of Iranian households exposed to catastrophic health expenditures | A cross-sectional study | Good | Catastrophic Health Expenditure Ratio |
| Abolhallaje M, Hasani S, Bastani P, Ramezanian M, Kazemian M.(118) | To identify measures of fair financing of health services and determinants of fair financing contribution | A cross-sectional study | Satisfactory | Rate for Out of Payments for total health expenditure |
| Ghiasvand H, Naghdi S, Abolhassani N, Shaarbafchizadeh N, Moghri J.(119) | This study investigated the Iranian rural and urban households’ inequality in payments on food and OOP health expenditures | A cross-sectional time trend study | Good | Concentration Indices for Food and Health Expenditure |
| Ghafoori MH, Ebadifard Azar F, Arab M, Mahmoodi M, Yusef Zadeh N, Rezapour A.(120) | To determine disparities in health expenditures by means of different approaches | A cross-sectional population-based study | Satisfactory |
Fairness in Financial Contribution Concentration Index Catastrophic Health Expenditure |
| Anbari Z, Mohammadbeigi A, Mohammadsalehi N, Ebrazeh A.(121) | Evaluating some health expenditure of inpatient and outpatient care as well as assessing the predictors of catastrophic costs for inpatient care | A cross-sectional study | Good | Catastrophic Costs Ratio |
| Rezapour A, Vahedi S, Khiavi FF, Esmaeilzadeh F, Javan-Noughabi J, Rajabi A.(122) | Analyzing CHE among households with and without chronic NCDs | A cross-sectional study | Satisfactory | The Catastrophic Health Expenditure incidence and intensity in the households with chronic NCDs”. |
| Ghiasvand H, Gorji HA, Maleki M, Hadian M.(13) | To explore the mean of OOP payments among Iranian households for health services and the level of inequality in its distribution | A cross-sectional study | Good |
The Catastrophic Health Expenditure headcount ratio The overshoot of Catastrophic Health Expenditure ratio |
| Rezapour A, Azar FE, Aghdash SA, Tanoomand A, Ahmadzadeh N, Asiabar AS.(123) | To assess the inequality in household's capacity to pay and OOP health care payments | A cross-sectional study | Good | Concentration Index for household's Out-of-Pocket payments |
| Rezapour A, Azar FE, Aghdash SA, Tanoomand A, Shokouh SMH, Yousefzadeh N, et al. (124) | Measuring equity in household’s health care payments according to FFCI and Kakwani indices | A cross-sectional study | Good | “The Fairness in Financial Contribution Index for households in health financing The Kakwani index |
| Ghiasvand H, Sha’baninejad H, Arab M, Rashidian A.(125) | To calculate the proportion of hospitalized patients exposed to catastrophic medical payments | A cross-sectional study | Good | Ratio and likelihood of exposure to Catastrophic Health Expenditure |
| Ibrahimipour H, Maleki M-R, Brown R, Gohari M, Karimi I, Dehnavieh R. (126) | To understand the Iranian health financing system and provide lessons for policy makers about achieving universal coverage | A qualitative study | Good | There are seven major obstacles to universal coverage: unknown insured rate; regressive financing and non-transparent financial flow; fragmented system; non-scientifically designed benefit package; non-health-oriented and expensive payment system; uncontrolled demands; and administrative deficiency”. |
| Naghdi S, Moradi T, Tavangar F, Bahrami G, Shahboulaghi M, Ghiasvand H.(127) | Investigating barriers to develop financial protection as a requirement to achieve universal health coverage | A qualitative study | Satisfactory | “The major themes included the political, social and economic context of the country, the context and structure of healthcare system and dimensions of UHC”. |
Discussion
More than 90% of the final included studies had a cross-sectional design with a quantitative approach, and only 4% were qualitative. Analyzing inequality in the preventive, outpatients, inpatients, diagnostic, and other clinical and medical services constructed about 30% of the studies. The main outcome of interest for Iranian health equity researchers was health resources (human resources, beds, and equipment). There was not any meaningful contribution in analyzing the outside health system contributors to analyzing the health equity.
The findings of our systematic review showed that health equity and its various dimensions were of major research concern in Iran. The included studies mostly assessed the distribution of resources, used macro data (such as the statistical data obtained from the Statistical Center of Iran or the MOHME), and were descriptive. Our review identified 3 main dimensions of equity: health outcomes, utilization, and financing categories. In terms of health outcomes, the studies focused on inequalities in life expectancy; maternal mortality; child mortality; and risk factors, such as diabetes, and obesity; and health indicators, eg, child health, oral health, and specific diseases.Continuous reforms, eg, the expansion of primary health care (PHC) networks, the modified medical education system to respond to increasing demand for expert human resources for health (HRH), and advances in insurance coverage have all contributed to increased life expectancy, decreased mortality, and improved health literacy. However, great challenges still remain, eg, equitable distribution of the health resources, ie, HRH across the country, especially in deprived and marginalized areas, suffer from unfavorable economic conditions (11, 128, 129). Demographic transitions, urbanization, and lifestyle changes have altered the pattern of diseases from communicable to noncommunicable diseases (NCDs), whose risk factors vary, as our included studies revealed, among various socioeconomic groups. Thus, tackling it would require enhancing public health literacy about such risk factors and the ways to prevent them (45, 130, 131). Regarding utilization of health services, inequalities in the distribution of the health resources, for instance, the existing gap in the available health sector resources, eg, access to specialist physicians, and the distribution of hospital beds, particularly intensive care and burn beds, are among major concerns. Despite the continuous efforts to improve the status, including the recent health transformation plan (HTP) that increased total hospital beds in Iran (132, 133), the equitable distribution of secondary care resources still remains a big challenge across the country, particularly the remote and marginalized areas. The latter needs great caution to balance the significant costs to improve access at the price of enhancing fair access (75, 82, 134). As for health financing, the inequality in the distribution of health care costs and households’ high exposure level to significant costs of health care were extensively considered in many studies. We found an unfavorable status of FFCI (concentration, Gini coefficient, and Kakwani) indices and exposure to health catastrophic costs in the course of the past 2 decades in Iran. Despite notable OOP reduction after the HTP implementation, the still high OOP remains a considerable challenge in Iran. Also, citizens in lower socioeconomic quintiles maybe prone to more severe financial hardship due to health expenses, all of which demand greater attention by policymakers in Iran. In particular, insurance policies need serious reforms to cover needed and evidence-informed benefit packages, purchaser-provider split, fact-based premium calculation, and progressive approaches to cover the poor living in rural and deprived areas (110, 135, 136).
Study limitations
Health equity includes a vast range of topics; thus, conducting just a systematic review cannot show the details of the studies. Therefore, it is better to conduct several systematic reviews on the aspect of health equity to achieve better results. We considered all aspects of health equity analysis in Iran, but extracting, summarizing, and reporting the retrieved evidence was a major challenge. Therefore, we have organized our research plan based on the current approaches of World Bank researchers. We used their classification approach for different topics in health equity analysis.
In addition, although primarily we ran search on the published studies in Persian language, based on our initial presumption and then the assessment of the retrieved studies, we decided to ignore them.
Implications for Future Research
We advocate the use of SDH perspective and other factors that affect health, including genetic and biological factors, food and nutrition, environmental and social factors, and even the impact of social and economic macro policies of the governments on health in studying health inequalities. Unless researchers study health inequalities through comprehensive lenses that accommodate social aspects, meaningful tackling
of such inequalities towards sustainable health development might be compromised.
Conclusion
This systematic review aimed to shed light on the various factors that contributed to health inequalities in Iran. Many studies approached the issue from the lenses of health system and focused on outcomes, utilization, and financial domains of inequalities as the main challenges to equity. Yet, the literature is tiny to accommodate the social problems that may be the cause of inequality in Iran. For instance, social issues such as unemployment, divorce, child labor, living in slums, and homelessness, which might be the consequences of social inequalities, need to be addressed while analyzing health inequalities in any settings.
In fact, policymakers in Iran need to develop directions in their health equity research priorities toward containing the factors that are not necessarily within the health system. Encouraging interdisciplinary research projects with social scientists is an urgent need.
Conflict of Interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate: IR.TUMS. VCR.REC.1397.230.
Appendix
Search strategy:
• PubMed/MedLine:
(((((((((((((((((((("health"[MeSH Terms] OR "health"[All Fields]) OR ("delivery of health care"[MeSH Terms] OR ("delivery"[All Fields] AND "health"[All Fields] AND "care"[All Fields]) OR "delivery of health care"[All Fields] OR ("health"[All Fields] AND "care"[All Fields]) OR "health care"[All Fields])) OR ("health services"[MeSH Terms] OR ("health"[All Fields] AND "services"[All Fields]) OR "health services"[All Fields])) OR ("health resources"[MeSH Terms] OR ("health"[All Fields] AND "resources"[All Fields]) OR "health resources"[All Fields])) OR (("health"[MeSH Terms] OR "health"[All Fields]) AND outcome[All Fields])) OR (("health"[MeSH Terms] OR "health"[All Fields]) AND consequences[All Fields])) AND equity[All Fields]) OR equality[All Fields]) OR disparity[All Fields]) OR ("socioeconomic factors"[MeSH Terms] OR ("socioeconomic"[All Fields] AND "factors"[All Fields]) OR "socioeconomic factors"[All Fields] OR "inequality"[All Fields])) OR inequity[All Fields]) OR accessibility[All Fields]) OR availability[All Fields]) OR acceptability[All Fields]) OR ("statistics and numerical data"[Subheading] OR ("statistics"[All Fields] AND "numerical"[All Fields] AND "data"[All Fields]) OR "statistics and numerical data"[All Fields] OR "utilization"[All Fields])) OR ("health expenditures"[MeSH Terms] OR ("health"[All Fields] AND "expenditures"[All Fields]) OR "health expenditures"[All Fields] OR "expenditure"[All Fields])) OR ("compensation and redress"[MeSH Terms] OR ("compensation"[All Fields] AND "redress"[All Fields]) OR "compensation and redress"[All Fields] OR "payment"[All Fields])) OR fairness[All Fields]) OR (horizontal[All Fields] AND equity[All Fields])) OR (vertical[All Fields] AND equity[All Fields])) AND ("iran"[MeSH Terms] OR "iran"[All Fields])
• Cochrane Library:
#1 Health
#2 Health Services
# 3 Health Care
#4 Health Outcomes
#5 Health Consequences
#6 Health System
#7 Health Resources
#8 Availability
#9 Accessibility
#10 Utilization
#11 Expenditure
#12 Payments
# 13 Equity
#14 Inequity
# 15 Equality
#16 Inequality
#17 Fairness
#18 Disparity
#19 Acceptability
#20 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7
#21 #8 OR #9 OR #10 OR #11 OR #12
#22 #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19
#23 #20 AND #21 AND #22
Cite this article as: Ghiasvand H, Mohamadi E, Olyaeemanesh A, Kiani MM, Armoon B, Takian A. Health equity in Iran: A systematic review. Med J Islam Repub Iran. 2021 (19 Apr);35:51. https://doi.org/10.47176/mjiri.35.51
Footnotes
Conflicts of Interest: None declared
Funding:This work was funded by the Health Equity Research Centre, Tehran University of Medical Sciences.
References
- 1.Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Health CoSDo. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–9. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 2. Wagstaff A, O'Donnell O, Van Doorslaer E, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation: World Bank Publications; 2007.
- 3.Bleich SN, Jarlenski MP, Bell CN, LaVeist TA. Health inequalities: trends, progress, and policy. Ann Rev Public Health. 2012;33:7–40. doi: 10.1146/annurev-publhealth-031811-124658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bulletin of the World Health Organization. 2000;78(1):19–29. [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MA. Toward a fourth generation of disparities research to achieve health equity. Ann Rev Public Health. 2011;32:399–416. doi: 10.1146/annurev-publhealth-031210-101136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grady SC, McLafferty S. Segregation, Nativity, and Health: Reproductive Health Inequalities for Immigrant and Native-Born Black Women in New York City1. Urban Geogr. 2007;28(4):377–97. [Google Scholar]
- 7. O'Donnell O, Van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data: a guide to techniques and their implementation: The World Bank; 2007.
- 8.Marmot SM. Closing the health gap in a generation: the work of the Commission on Social Determinants of Health and its recommendations. Glob Health Promot. 2009;16(1_suppl):23–7. doi: 10.1177/1757975909103742. [DOI] [PubMed] [Google Scholar]
- 9.Moghaddam AV, Damari B, Alikhani S, Salarianzedeh M, Rostamigooran N, Delavari A. et al. Health in the 5th 5-years Development Plan of Iran: main challenges, general policies and strategies. Iran J Public Health. 2013;42(Supple1):42. [PMC free article] [PubMed] [Google Scholar]
- 10. Motlagh M. Oliaei manesh AR, Beheshtian M. Health and its social determinants Tehran: Health policy council Secretariat of social determinant of health Ministry of Health and Medical Education. 2008.
- 11.Asadi-Lari M, Vaez-Mahdavi MR, Faghihzadeh S, Montazeri A, Farshad AA, Kalantari N. et al. The application of urban health equity assessment and response tool (Urban HEART) in Tehran concepts and framework. Med J Islam Repub Iran. 2010;24(3):175–85. [Google Scholar]
- 12.Rashidian A, Karimi-Shahanjarini A, Khosravi A, Elahi E, Beheshtian M, Shakibazadeh E. et al. Iran's multiple indicator demographic and health survey-2010: Study protocol. Int J Prev Med. 2014;5(5):632. [PMC free article] [PubMed] [Google Scholar]
- 13.Ghiasvand H, Gorji HA, Maleki M, Hadian M. Catastrophic health expenditure among Iranian rural and urban households, 2013-2014. Iran Red Crescent Med J. 2015;17(9) doi: 10.5812/ircmj.30974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 15. cebm. https://www.cebm.net/wp-content/uploads/2019/01/Systematic-Review.pdf 2020.
- 16. cebm. https://www.cebm.net/wp-content/uploads/2019/01/Qualitative-Studies.pdf. 2020.
- 17.Emamian MH, Fateh M, Hosseinpoor AR, Alami A, Fotouhi A. Obesity and its socioeconomic determinants in Iran. Econ Hum Biol. 2017;26:144–50. doi: 10.1016/j.ehb.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 18.Farzadi F, Ahmadi B, Shariati B, Alimohamadian M, Mohamad K. Women's health: explaining the trend in gender ratio in Iran over half a century (1956–2006) Public Health. 2010;124(2):86–9. doi: 10.1016/j.puhe.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Gooshki ES, Rezaei R, Wild V. Migrants' Health in Iran from the Perspective of Social Justice: a Systematic Literature Review. Arch Iran Med. 2016;19(10) [PubMed] [Google Scholar]
- 20.Moradi-Lakeh M, Bijari B, Namiranian N, Olyaeemanesh A-R, Khosravi A. Geographical disparities in child mortality in the rural areas of Iran: 16-years trend. J Epidemiol Commun Health. 2013;67(4):346–9. doi: 10.1136/jech-2012-201511. [DOI] [PubMed] [Google Scholar]
- 21.Nedjat S, Hosseinpoor AR, Forouzanfar MH, Golestan B, Majdzadeh R. Decomposing socioeconomic inequality in self-rated health in Tehran. J Epidemiol Commun Health. 2012;66(6):495–500. doi: 10.1136/jech.2010.108977. [DOI] [PubMed] [Google Scholar]
- 22.Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Jafarzadehpur E. et al. Economic inequality in presenting near vision acuity in a middle-aged population: a Blinder–Oaxaca decomposition. Br J Ophthalmol. 2013;97(9):1100–3. doi: 10.1136/bjophthalmol-2013-303249. [DOI] [PubMed] [Google Scholar]
- 23.Morasae EK, Forouzan AS, Majdzadeh R, Asadi-Lari M, Noorbala AA, Hosseinpoor AR. Understanding determinants of socioeconomic inequality in mental health in Iran's capital, Tehran: a concentration index decomposition approach. Int J Equity Health. 2012;11(1):18. doi: 10.1186/1475-9276-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramezani Doroh V, Vahedi S, Arefnezhad M, Kavosi Z, Mohammadbeigi A. Decomposition of health inequality determinants in Shiraz, South-West Iran. J Res Health Sci. 2015;15(3):152–8. [PubMed] [Google Scholar]
- 25.Shahbazi N, Veisani Y, Delpisheh A, Sayehmiri K, Naderi Z, Sohrabnejad A. et al. Relationship between Socioeconomic Status and General Health in the Female-headed Households. J Ilam Uni Med Sci. 2015;23(1):56–62. [Google Scholar]
- 26.Amirian H, Poorolajal J, Roshanaei G, Esmailnasab N, Moradi G. Analyzing socioeconomic related health inequality in mothers and children using the concentration index. Epidemiol Biostat Public Health. 2014;11(3) [Google Scholar]
- 27.Khajavi A, Pishgar F, Dehghani M, Naderimagham S. Socioeconomic inequalities in neonatal and postneonatal mortality: Evidence from rural Iran, 1998–2013. Int J Equity Health. 2017;16(1):83. doi: 10.1186/s12939-017-0570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alizadeh M, Laghousi D. Trend of geographical disparities in child and maternal mortality indicators in Northwest Iran. Soc Determ Health. 2015;1(4):132–40. [Google Scholar]
- 29.Rarani MA, Rashidian A, Arab M, Khosravi A, Abbasian E. Inequality in under-five mortality in Iran: a national and subnational survey data analysis. Glob J Health Sci. 2016;9(3):215. [Google Scholar]
- 30.Kiadaliri AA. Gender and social disparities in esophagus cancer incidence in Iran, 2003-2009: a time trend province-level study. Asian Pac J Cancer Prev. 2014;15(2):623–7. doi: 10.7314/apjcp.2014.15.2.623. [DOI] [PubMed] [Google Scholar]
- 31.Kiadaliri AA, Saadat S, Shahnavazi H, Haghparast-Bidgoli H. Overall, gender and social inequalities in suicide mortality in Iran, 2006–2010: a time trend province-level study. BMJ Open. 2014;4(8):e005227. doi: 10.1136/bmjopen-2014-005227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghorbani Z, Ahmady AE, Ghasemi E, Zwi A. Socioeconomic inequalities in oral health among adults in Tehran, Iran. Commun Dent Health. 2015;32(1):26–31. [PubMed] [Google Scholar]
- 33.Hosseinpoor AR, Mohammad K, Majdzadeh R, Naghavi M, Abolhassani F, Sousa A. et al. Socioeconomic inequality in infant mortality in Iran and across its provinces. Bull World Health Organ. 2005;83(11):837–44. [PMC free article] [PubMed] [Google Scholar]
- 34.Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, Majdzadeh R. et al. Decomposing socioeconomic inequality in infant mortality in Iran. Int J Epidemiol. 2006;35(5):1211–9. doi: 10.1093/ije/dyl164. [DOI] [PubMed] [Google Scholar]
- 35.Almasi-Hashiani A, Sepidarkish M, Safiri S, Morasae EK, Shadi Y, Omani-Samani R. Understanding determinants of unequal distribution of stillbirth in Tehran, Iran: a concentration index decomposition approach. BMJ Open. 2017;7(5):e013644. doi: 10.1136/bmjopen-2016-013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rad EH, Khodaparast M. Inequity in Health Care Financing in Iran: Progressive or Regressive Mechanism? Eurasian J Med. 2016;48(2):112. doi: 10.5152/eurasianjmed.2015.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. Unmet refractive need and its determinants in Shahroud, Iran. Int J Ophthalmol. 2012;32(4):329–36. doi: 10.1007/s10792-012-9567-8. [DOI] [PubMed] [Google Scholar]
- 38.Hosseinkhani Z, Nedjat S, Aflatouni A, Mahram M, Majdzadeh R. Socioeconomic inequality and child maltreatment in Iranian schoolchildren. East Mediterr Health J. 2015;21(11):819. doi: 10.26719/2015.21.11.819. [DOI] [PubMed] [Google Scholar]
- 39.Mansouri A, Rarani MA, Fallahi M, Alvandi I. Irritable bowel syndrome is concentrated in people with higher educations in Iran: an inequality analysis. Epidemiol Health. 2017;39 doi: 10.4178/epih.e2017005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fateh M, Emamian MH, Asgari F, Alami A, Fotouhi A. Socioeconomic inequality in hypertension in Iran. J Hypertens. 2014;32(9):1782–8. doi: 10.1097/HJH.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 41.Moradi G, Ardakani HM, Majdzadeh R, Bidarpour F, Mohammad K, Holakouie-Naieni K. Socioeconomic inequalities in nonuse of seatbelts in cars and helmets on motorcycles among people living in Kurdistan Province, Iran. Iran J Public Health. 2014;43(9):1239. [PMC free article] [PubMed] [Google Scholar]
- 42.Veisani Y, Delpisheh A, Moradi G, Hassanzadeh J, Sayehmiri K. Inequality in addiction and mental disorders in 6818 suicide attempts: determine of positive contribution of determinants by decomposition method. Iran J Public Health. 2017;46(6):796. [PMC free article] [PubMed] [Google Scholar]
- 43.Tourani S, Zarezadeh M, Raadabadi M, Pourshariati F. Association of regional disparity of obstetrics and gynecologic services with children and infants mortality rates: A cross-sectional study. Int J Reprod Biomed. 2017;15(3):147. [PMC free article] [PubMed] [Google Scholar]
- 44.Entezarmahdi R, Majdzadeh R, Foroushani AR, Nasehi M, Lameei A, Naieni KH. Inequality of leprosy disability in Iran, clinical or socio-economic inequality: an extended concentration index decomposition approach. Int J Prev Med. 2014;5(4):414. [PMC free article] [PubMed] [Google Scholar]
- 45.Moradi G, Mohammad K, Majdzadeh R, Ardakani HM, Naieni KH. Socioeconomic inequality of non-communicable risk factors among people living in Kurdistan Province, Islamic Republic of Iran. Int J Prev Med. 2013;4(6):671. [PMC free article] [PubMed] [Google Scholar]
- 46.Naghdi S, Ghiasvand H, Zadeh NS, Azami S, Moradi T. Association of health and food expenditures inequality with health outcomes: a case study on Iranian rural households. Iran Red Crescent Med J. 2014;16(3) doi: 10.5812/ircmj.14335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kiadaliri AA. Social disparity in breast and ovarian cancer incidence in iran, 2003-2009: a time trend province-level study. J Breast Cancer. 2013;16(4):372–7. doi: 10.4048/jbc.2013.16.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kia AA, Rezapour A, Khosravi A, Abarghouei VA. Socioeconomic Inequality in Malnutrition in Under-5 Children in Iran: Evidence From the Multiple Indicator Demographic and Health Survey, 2010. J Prev Med Public Health. 2017;50(3):201. doi: 10.3961/jpmph.17.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moradi G, Moinafshar A, Adabi H, Sharafi M, Mostafavi F, Bolbanabad AM. Socioeconomic Inequalities in the Oral Health of People Aged 15-40 Years in Kurdistan, Iran in 2015: A Cross-sectional Study. J prev Med Public Health. 2017;50(5):303. doi: 10.3961/jpmph.17.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kiadaliri AA, Asadi-Lari M, Kalantari N, Jafari M, Mahdavi MRV, Faghihzadeh S. Absolute and relative educational inequalities in obesity among adults in Tehran: Findings from the Urban HEART study-2. Obes Res Clin Pract. 2016;10:S57–S63. doi: 10.1016/j.orcp.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 51.Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. The gap of visual impairment between economic groups in Shahroud, Iran: a Blinder-Oaxaca decomposition. Am J Epidemiol. 2011;173(12):1463–7. doi: 10.1093/aje/kwr050. [DOI] [PubMed] [Google Scholar]
- 52.Hosseini M, Olyaeemanesh A, Ahmadi B, Nedjat S, Farzadi F, Arab M. et al. Gender equity in health: A secondary analysis of data in Iran. Med J Islam Repub Iran. 2016;30:344. [PMC free article] [PubMed] [Google Scholar]
- 53.Emamian MH, Fateh M, Gorgani N, Fotouhi A. Mother's education is the most important factor in socio-economic inequality of child stunting in Iran. Public Health Nutr. 2014;17(9):2010–5. doi: 10.1017/S1368980013002280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Raeisi A, Mehboudi M, Darabi H, Nabipour I, Larijani B, Mehrdad N. et al. Socioeconomic inequality of overweight and obesity of the elderly in Iran: Bushehr Elderly Health (BEH) Program. BMC Public Health. 2017;17(1):72. doi: 10.1186/s12889-016-3912-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Safiri S, Kelishadi R, Heshmat R, Rahimi A, Djalalinia S, Ghasemian A. et al. Socioeconomic inequality in oral health behavior in Iranian children and adolescents by the Oaxaca-Blinder decomposition method: the CASPIAN-IV study. Int J Equity Health. 2016;15(1):143. doi: 10.1186/s12939-016-0423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peykari N, Djalalinia S, Qorbani M, Sobhani S, Farzadfar F, Larijani B. Socioeconomic inequalities and diabetes: A systematic review from Iran. J Diabetes Metab Disord Control. 2015;14(1):8. doi: 10.1186/s40200-015-0135-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ravaghi H, Goshtaei M, Olyaee Manesh A, Abolhassani N, Arabloo J. Stakeholders' perspective on health equity and its indicators in Iran. Med J Islam Repub Iran. 2015;29(1):713–23. [PMC free article] [PubMed] [Google Scholar]
- 58.Zaboli R, Tourani S, Seyedin SH, Manesh AO. Prioritizing the determinants of social-health inequality in Iran: a multiple attribute decision making application. Iran Red Crescent Med J. 2014;16(4) doi: 10.5812/ircmj.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Beheshtian M, Manesh AO, Bonakdar S, Afzali HM, Larijani B, Hosseini L. et al. Intersectoral collaboration to develop health equity indicators in Iran. Iran J Public Health. 2013;42(Supple1):31. [PMC free article] [PubMed] [Google Scholar]
- 60.Sadeghipour Roudsari H, Sherafat Kazemzadeh R, Rezaeie M, Derakhshan M. Reproductive health knowledge, attitudes and practices of Iranian and Afghan men in Tehran province. East Mediterr Health J. 2006;12(6):862–72. [PubMed] [Google Scholar]
- 61.Bidgoli HH, Bogg L, Hasselberg M. Pre-hospital trauma care resources for road traffic injuries in a middle-income country—A province based study on need and access in Iran. Injury. 2011;42(9):879–84. doi: 10.1016/j.injury.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 62.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Decomposition of inequity determinants of healthcare utilization, Iran. Public Health. 2013;127(7):661–7. doi: 10.1016/j.puhe.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 63.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Socioeconomic inequity in health care utilization, Iran. J Epidemiol Glob Health. 2013;3(3):139–46. doi: 10.1016/j.jegh.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Noroozi M, Rahimi E, Ghisvand H, Qorbani M, Sharifi H, Noroozi A. et al. Decomposition of Economic Inequality in Needle and Syringe Programs Utilization to its Determinants among Men Who Inject Drugs in Tehran using Blinder–Oaxaca Decomposition Method. Subst Use Misuse. 2017:1–7. doi: 10.1080/10826084.2017.1400567. [DOI] [PubMed] [Google Scholar]
- 65.Davari M, Maracy MR, Aslani A, Bakhshizadeh Z, Khorasani E. Evaluation of equity in access to pharmaceutical services in selected cites of Isfahan Province, Iran. Journal of Pharmacoeconomics and Pharmaceutical Management. 2017;2(1/2):25–9. [Google Scholar]
- 66.Ramandi SD, Niakan L, Aboutorabi M, Noghabi JJ, Khammarnia M, Sadeghi A. Trend of Inequality in the Distribution of Health Care Resources in Iran. Galen Medical Journal. 2016;5(3):122–30. [Google Scholar]
- 67.Kiadaliri AA, Najafi B, Haghparast-Bidgoli H. Geographic distribution of need and access to health care in rural population: an ecological study in Iran. Int J Equity Health. 2011;10(1):39. doi: 10.1186/1475-9276-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kavosi Z, Mohammadbeigi A, Ramezani-Doroh V, Hatam N, Jafari A, Firoozjahantighi A. Horizontal inequity in access to outpatient services among Shiraz City residents, Iran. J Res Health Sci. 2015;15(1):37–41. [PubMed] [Google Scholar]
- 69.Karyani AK, Azami SR, Rezaei S, Shaahmadi F, Ghazanfari S. Geographical distribution of gynecologists and midwives in Kermanshah province (2008-2013) J Kermanshah Univ Med Sci. 2015;19(5):294–302. [Google Scholar]
- 70.Meshkini AH, Kebriaeezadeh A, Janghorban MR, Keshavarz K, Nikfar S. Assessment of geographic accessibility to pharmacy in Qom, Iran: A geographic information system analysis. Thrita. 2014;3(1) [Google Scholar]
- 71.Hajizadeh M, Connelly LB, Butler JR, Khosravi A. Unmet need and met unneed in health care utilisation in Iran. Int J Soc Econ. 2012;39(6):400–22. [Google Scholar]
- 72.Noroozi M, Sharifi H, Noroozi A, Rezaei F, Bazrafshan MR, Armoon B. Decomposing economic disparities in risky sexual behaviors among people who inject drugs in Tehran: Blinder-Oaxaca decomposition analysis. Epidemiol Health. 2017;39 doi: 10.4178/epih.e2017049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Geravandi S, Najafi M, Rajaee R, Mahmoudi S, Pakdaman M. The assessment of inequality in the geographical distribution of burn beds in Iran. Electron Physician. 2015;7(6):1407. doi: 10.14661/1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sefiddashti SE, Arab M, Ghazanfari S, Kazemi Z, Rezaei S, Karyani AK. Trends of geographic inequalities in the distribution of human resources in healthcare system: the case of Iran. Electron physician. 2016;8(7):2607. doi: 10.19082/2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Honarmand R, Mozhdehifard M, Kavosi Z. Geographic distribution indices of general practitioners, midwives, pediatricians, and gynecologists in the public sector of Iran. Electron Physician. 2017;9(6):4584. doi: 10.19082/4584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moradi LM, Ramezani M, Naghavi M. Equality in safe delivery and its determinants in Iran. Arch Iran Med. 2007;10(4):446–51. [PubMed] [Google Scholar]
- 77.Meskarpour-Amiri M, Mehdizadeh P, Barouni M, Dopeykar N, Ramezanian M. Assessment the trend of inequality in the distribution of intensive care beds in Iran: using GINI index. Glob J Health Sci. 2014;6(6):28. doi: 10.5539/gjhs.v6n6p28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jadidi R, Mohammadbeigi A, Mohammadsalehi N, Ansari H, Ghaderi E. Inequity in timeliness of MMR vaccination in children living in the suburbs of Iranian cities. Int J Biomed Sci. 2015;11(2):93. [PMC free article] [PubMed] [Google Scholar]
- 79.Masoodi M, Rahimzadeh M. Measuring access to urban health services using Geographical Information System (GIS): a case study of health service management in Bandar Abbas, Iran. Int J Health Policy Manag. 2015;4(7):439. doi: 10.15171/ijhpm.2015.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Emamian MH, Zeraati H, Majdzadeh R, Shariati M, Hashemi H, Fotouhi A. Economic inequality in eye care utilization and its determinants: a Blinder–Oaxaca decomposition. Int J Health Policy Manag. 2014;3(6):307. doi: 10.15171/ijhpm.2014.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Homaie Rad E, Ghiasi A, Arefnezhad M, Bayati M. Inequalities of general physicians and specialists visits’ utilization and its determinants in Iran: a population based study. Int J Hum Rights Healthc. 2015;8(3):125–31. [Google Scholar]
- 82.Kazemi Karyani A, Kazemi Z, Shaahmadi F, Arefi Z, Ghazanfari S. Determining inequality and trend of geographic accessibility to pediatricians in Iran: 2007-2013. Int J Pediatr. 2015;3(2.1):51–8. [Google Scholar]
- 83.Meskarpour-Amiri M, Dopeykar N, Ameryoun A, Tavana AM. Assessment inequality in access to public cardiovascular health services in Iran. Med J Islam Repub Iran. 2016;30:420. [PMC free article] [PubMed] [Google Scholar]
- 84.Mobaraki H, Hassani A, Kashkalani T, Khalilnejad R, Chimeh EE. Equality in distribution of human resources: the case of Iran’s Ministry of Health and Medical Education. Iran J Public Health. 2013;42(Supple1):161. [PMC free article] [PubMed] [Google Scholar]
- 85.Omrani-Khoo H, Lotfi F, Safari H, Jame SZB, Moghri J, Shafii M. Equity in distribution of health care resources; assessment of need and access, using three practical indicators. Iran J Public Health. 2013;42(11):1299. [PMC free article] [PubMed] [Google Scholar]
- 86.Sari AA, Rezaei S, Rad EH, Dehghanian N, Chavehpour Y. Regional disparity in physical resources in the health sector in Iran: a comparison of Two time periods. Iran J Public Health. 2015;44(6):848. [PMC free article] [PubMed] [Google Scholar]
- 87.Mohammadbeigi A, Arsangjang S, Mohammadsalehi N, Anbari Z, Ghaderi E. Education-related inequity in access and utilization of oral health care in Iran. J Family Med Prim Care. 2015;4(1):35. doi: 10.4103/2249-4863.152248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rad EH, Kavosi Z, Arefnezhad M. Economic inequalities in dental care utilizations in Iran: Evidence from an urban region. Med J Islam Repub Iran. 2016;30:383. [PMC free article] [PubMed] [Google Scholar]
- 89.Hatam N, Zakeri M, Sadeghi A, Ramandi SD, Hayati R, Siavashi E. Equity analysis of hospital beds distribution in Shiraz, Iran 2014. Med J Islam Repub Iran. 2016;30:393. [PMC free article] [PubMed] [Google Scholar]
- 90.Ameryoun A, Meskarpour-Amiri M, Dezfuli-Nejad ML, Khoddami-Vishteh H, Tofighi S. The assessment of inequality on geographical distribution of Non-cardiac intensive care beds in Iran. Iran J Public Health. 2011;40(2):25. [PMC free article] [PubMed] [Google Scholar]
- 91.Hashemi H, Rezvan F, Fotouhi A, Khabazkhoob M, Gilasi H, Etemad K. et al. Distribution of cataract surgical rate and its economic inequality in Iran. Optom Vis Sci. 2015;92(6):707–13. doi: 10.1097/OPX.0000000000000590. [DOI] [PubMed] [Google Scholar]
- 92.Reshadat S, Saedi S, Zangeneh A, Ghasemi S, Gilan N, Karbasi A. et al. Spatial accessibility of the population to urban health centres in Kermanshah, Islamic Republic of Iran: a geographic information systems analysis. East Mediterr Health J. 2015;21(6):389. doi: 10.26719/2015.21.6.389. [DOI] [PubMed] [Google Scholar]
- 93.Rezaei S, Karyani A, Fallah R, Matin B. Relative inequalities in geographic distribution of health care resources in Kermanshah province, Islamic Republic of Iran. East Mediterr Health J. 2016;22(1):20. [PubMed] [Google Scholar]
- 94.Chavehpour Y, Rashidian A, Raghfar H, Emamgholipour sefiddashti S, Maroofi A. ‘Seeking affluent neighbourhoods?’a time-trend analysis of geographical distribution of hospitals in the Megacity of Tehran. Health Policy Plan. 2017;32(5):669–75. doi: 10.1093/heapol/czw172. [DOI] [PubMed] [Google Scholar]
- 95.Nemati R, Seyedin H, Nemati A, Sadeghifar J, Nasiri AB, Mousavi SM. et al. An analysis of disparities in access to health care in Iran: evidence from Lorestan Province. Glob J Health Sci. 2014;6(5):81. doi: 10.5539/gjhs.v6n5p81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yari A, Nedjat S, Asadi-Lari M, Majdzadeh R. Perceptions about Iranian-Kurds’ ethnic-inequality in health. BMC Int Health Hum Rights. 2017;17(1):24. doi: 10.1186/s12914-017-0133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mohammadi S, Gargari SS, Fallahian M, Källestål C, Ziaei S, Essén B. Afghan migrants face more suboptimal care than natives: a maternal near-miss audit study at university hospitals in Tehran, Iran. BMC Pregnancy Childbirth. 2017;17(1):64. doi: 10.1186/s12884-017-1239-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rezapour A, Arabloo J, Tofighi S, Alipour V, Sepandy M, Mokhtari P. et al. Determining Equity in Household's Health Care Payments in Hamedan Province, Iran. Arch Iran Med. 2016;19(7) [PubMed] [Google Scholar]
- 99.Rezapour A, Ghaderi H, Azar FE, Larijani B, Gohari MR. Effects of health out-of-pocket payment on households in iran; catastrophic and impoverishment: Population based study in Tehran (2012) Life Sci J. 2013;10(3) [Google Scholar]
- 100.Zare H, Trujillo AJ, Driessen J, Ghasemi M, Gallego G. Health inequalities and development plans in Iran; an analysis of the past three decades (1984–2010) Int J Equity Health. 2014;13(1):42. doi: 10.1186/1475-9276-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Davari M, Kheyri M, Nourbakhsh SMK, Khadivi R. Socioeconomic status and catastrophic health expenditure evaluation in IR Iran: A comparative study in 2004 and 2011. Social Determinants of Health. 2015;1(2):48–59. [Google Scholar]
- 102.Khammarnia M, Keshtkaran A, Kavosi Z, Hayati R. The Household Health Spending and Impoverishment: Findings from the Households Survey in Shiraz, Iran. Bangladesh Med Res Counc Bull. 2015;40(2):58–62. doi: 10.3329/bmrcb.v40i2.25184. [DOI] [PubMed] [Google Scholar]
- 103.Delavari H, Keshtkaran A, Setoudehzadeh F. Catastrophic health expenditures and coping strategies in households with cancer patients in Shiraz Namazi hospital. Middle East J Cancer. 2014;5(1):13–22. [Google Scholar]
- 104.Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR. et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613–23. doi: 10.1093/heapol/czs001. [DOI] [PubMed] [Google Scholar]
- 105.Fazaeli AA, Seyedin H, Moghaddam AV, Delavari A, Salimzadeh H, Varmazyar H. et al. Fairness of financial contribution in Iranian health system: Trend analysis of national household income and expenditure, 2003-2010. Glob J Health Sci. 2015;7(5):260. doi: 10.5539/gjhs.v7n5p260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Juyani Y, Hamedi D, Jebeli SSH, Qasham M. Multiple Sclerosis and Catastrophic Health Expenditure in Iran. Glob J Health Sci. 2016;8(9):194. doi: 10.5539/gjhs.v8n9p194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hajizadeh M, Connelly LB. Equity of health care financing in Iran: the effect of extending health insurance to the uninsured. Oxf Dev Stud. 2010;38(4):461–76. [Google Scholar]
- 108.Hajizadeh M, Nghiem HS. Out-of-pocket expenditures for hospital care in Iran: who is at risk of incurring catastrophic payments? Int J Health Econ Manag. 2011;11(4):267. doi: 10.1007/s10754-011-9099-1. [DOI] [PubMed] [Google Scholar]
- 109. Reshadat S, Najafi F, Karami-Matin B, Soofi M, Barfar E, Rajabi-Gilan N, et al. Measuring Financial Protection in Hospitalized Patients after the Health Sector Evolution Plan in Iran. Health Scope. 2017(In Press).
- 110. Ghorbanian A, Rashidian A, Lankarani KB, Kavosi Z. The Prevalence and Determinants of Catastrophic Health Expenditures in Iran: A Systematic Review and Meta-Analysis. Health Scope. 2017(In Press).
- 111.Ghoddoosinejad J, Jannati A, Gholipour K, Baghestan EB. Households encountering with catastrophic health expenditures in Ferdows, Iran. J Egypt Public Health Assoc. 2014;89(2):81–4. doi: 10.1097/01.EPX.0000451789.21421.61. [DOI] [PubMed] [Google Scholar]
- 112.Mansouri A, Emamian MH, Zeraati H, Hashemi H, Fotouhi A. Economic inequality in presenting vision in Shahroud, Iran: two decomposition methods. Int J Health Policy Manag. 2018;7(1):59. doi: 10.15171/ijhpm.2017.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kavosi Z, Keshtkaran A, Hayati R, Ravangard R, Khammarnia M. Household financial contribution to the health System in Shiraz, Iran in 2012. Int J Health Policy Manag. 2014;3(5):243. doi: 10.15171/ijhpm.2014.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Piroozi B, Moradi G, Nouri B, Bolbanabad AM, Safari H. Catastrophic health expenditure after the implementation of health sector evolution plan: a case study in the west of Iran. Int J Health Policy Manag. 2016;5(7):417. doi: 10.15171/ijhpm.2016.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rarani MA, Rashidian A, Khosravi A, Arab M, Abbasian E, Morasae EK. Changes in socio-economic inequality in neonatal mortality in Iran between 1995-2000 and 2005-2010: an Oaxaca decomposition analysis. Int J Health Policy Manag. 2017;6(4):219. doi: 10.15171/ijhpm.2016.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Daneshkohan A, Karami M, Najafi F, Matin BK. Household catastrophic health expenditure. Iran J Public Health. 2011;40(1):94. [PMC free article] [PubMed] [Google Scholar]
- 117.Moghadam MN, Banshi M, Javar MA, Amiresmaili M, Ganjavi S. Iranian household financial protection against catastrophic health care expenditures. Iran J Public Health. 2012;41(9):62. [PMC free article] [PubMed] [Google Scholar]
- 118.Abolhallaje M, Hasani S, Bastani P, Ramezanian M, Kazemian M. Determinants of catastrophic health expenditure in Iran. Iran J Public Health. 2013;42(Supple1):155. [PMC free article] [PubMed] [Google Scholar]
- 119.Ghiasvand H, Naghdi S, Abolhassani N, Shaarbafchizadeh N, Moghri J. Iranian Households’ Payments on Food and Health Out-of-Pocket Expenditures: Evidence of Inequality. Iran J Public Health. 2015;44(8):1103. [PMC free article] [PubMed] [Google Scholar]
- 120.Ghafoori MH, Ebadifard Azar F, Arab M, Mahmoodi M, Yusef Zadeh N, Rezapour A. Inequality in the Distribution of Health Expenditures in 22 Districts of Tehran. J Commun Health Res. 2014;3(2):132–44. [Google Scholar]
- 121.Anbari Z, Mohammadbeigi A, Mohammadsalehi N, Ebrazeh A. Health expenditure and catastrophic costs for inpatient-and out-patient care in Iran. Int J Prev Med. 2014;5(8):1023. [PMC free article] [PubMed] [Google Scholar]
- 122.Rezapour A, Vahedi S, Khiavi FF, Esmaeilzadeh F, Javan-Noughabi J, Rajabi A. Catastrophic health expenditure of chronic diseases: Evidence from Hamadan, Iran. Int J Prev Med. 2017;8 doi: 10.4103/ijpvm.IJPVM_104_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rezapour A, Azar FE, Aghdash SA, Tanoomand A, Ahmadzadeh N, Asiabar AS. Inequity in household's capacity to pay and health payments in Tehran-Iran-2013. Med J Islam Repub Iran. 2015;29:245. [PMC free article] [PubMed] [Google Scholar]
- 124.Rezapour A, Azar FE, Aghdash SA, Tanoomand A, Shokouh SMH, Yousefzadeh N. et al. Measuring equity in household's health care payments (Tehran-Iran 2013): technical points for health policy decision makers. Med J Islam Repub Iran. 2015;29:246. [PMC free article] [PubMed] [Google Scholar]
- 125.Ghiasvand H, Sha’baninejad H, Arab M, Rashidian A. Hospitalization and catastrophic medical payment: evidence from hospitals located in Tehran. Arch Iran Med. 2014;17(7) [PubMed] [Google Scholar]
- 126.Ibrahimipour H, Maleki M-R, Brown R, Gohari M, Karimi I, Dehnavieh R. A qualitative study of the difficulties in reaching sustainable universal health insurance coverage in Iran. Health policy Plan. 2011;26(6):485–95. doi: 10.1093/heapol/czq084. [DOI] [PubMed] [Google Scholar]
- 127.Naghdi S, Moradi T, Tavangar F, Bahrami G, Shahboulaghi M, Ghiasvand H. The barriers to achieve financial protection in Iranian health system: a qualitative study in a developing country. Ethiop J Health Sci. 2017;27(5):491–500. doi: 10.4314/ejhs.v27i5.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Olyaee MA, Haghdoust AA, Beheshtian M, Tehrani BA, Motlagh M. Progress towards health equity in IR of Iran through last three decades. Iran J Public Health. 2009;38(Supple 1):130–135. [Google Scholar]
- 129.Ravaghi H, Goshtaei M, Manesh AO, Abolhassani N, Arabloo J. Stakeholders' perspective on health equity and its indicators in Iran: a qualitative study. Med J Islam Repub Iran. 2015;29:250. [PMC free article] [PubMed] [Google Scholar]
- 130.Peykari N, Hashemi H, Dinarvand R, Haji-Aghajani M, Malekzadeh R, Sadrolsadat A. et al. National action plan for non-communicable diseases prevention and control in Iran; a response to emerging epidemic. Diabetes Metab Disord. 2017;16(1):3. doi: 10.1186/s40200-017-0288-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Abbasi SH, Sundin Ö, Jalali A, Soares J, Macassa G. Ethnic Differences in the Risk Factors and Severity of Coronary Artery Disease: a Patient-Based Study in Iran. J Racial Ethn Health Disparities. 2017:1–9. doi: 10.1007/s40615-017-0408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Piroozi B, Rashidian A, Takian A, Amerzadeh M, Sakha MA, Faraji O, et al. The impact of health transformation plan on hospitalization rates in Iran: An interrupted time series. Int J Health Plann Manage. 2018. [DOI] [PubMed]
- 133.Mohamadi E, Tabatabaei SM, Olyaeemanesh A, Sagha SF, Zanganeh M, Davari M. et al. Coverage Decision-Making for Orthopedics Interventions in the Health Transformation Program in Iran: A Multiple Criteria Decision Analysis (MCDA) Shiraz E-Medic J. 2016;17(12) [Google Scholar]
- 134.Rezaei S, Bazyar M, Fallah R, Chavehpour Y, Rad EH. Assessment of need and access to physician and hospital beds: a cross sectional province based study in Iran. Shiraz E-Medic J. 2015;16(6) [Google Scholar]
- 135.Aryankhesal A, Etemadi M, Mohseni M, Azami-Aghdash S, Nakhaei M. Catastrophic Health Expenditure in Iran: A Review Article. Iran J Public Health. 2018;47(2):166. [PMC free article] [PubMed] [Google Scholar]
- 136.Takian A, Rashidian A, Doshmangir L. The experience of purchaser–provider split in the implementation of family physician and rural health insurance in Iran: an institutional approach. Health Policy Plan. 2015;30(10):1261–71. doi: 10.1093/heapol/czu135. [DOI] [PubMed] [Google Scholar]


