Abstract
Background
Nephronophthisis (NPHP) is a chronic tubular interstitial disorder that exhibits an autosomal recessive genetic form and causes progressive renal failure in children. Patients with NPHP rarely show urinary abnormalities, edema, or hypertension. Thus, NPHP is often detected only when renal failure becomes advanced. NPHP can be divided into three types based on the age of end-stage renal failure, i.e., infant type (approximately 5 years old), juvenile type (approximately 13–14 years old), and adolescent type (approximately 19 years old). Here, we report a case of NPHP diagnosed by genetic analysis at 26 years of age with atypical histological abnormalities.
Case presentation
A 26-year-old woman showed no growth disorders or urinary abnormalities in annual school physical examinations. However, at a check-up at 26 years old, she exhibited renal dysfunction (eGFR 26 mL/min/1.73 m2). Urine tests indicated low specific gravity of urine, but not proteinuria or microscopic hematuria. Urinary β2-microglobulin was high (805 μg/L), and renal biopsy was performed for definitive diagnosis. Histological findings showed no significant findings in glomeruli. However, moderate fibrosis was observed in the interstitial area, and moderate atrophy was observed in the tubules. There were no significant findings in immunofluorescence analysis, and no electron dense deposits were detected by electron microscopy. Although cyst-like expansion of the tubules was unclear, tubular atrophy was dominantly found in the distal tubule by cytokeratin 7 staining. Genetic analysis of the NPHP1 gene showed complete deletion of this gene, leading to a definitive diagnosis of NPHP.
Conclusions
NPHP is not merely a pediatric disease and is relatively high incidence in patients with adult onset end-stage of renal disease. In this case, typical histological abnormalities, such as cyst-like expansion of the tubular lesion, were not observed, and diagnosis was achieved by genetic analysis of the NPHP1 gene, which is responsible for the onset of NPHP. In patients with renal failure with tubular interstitial disease dominantly in the distal tubules, it is necessary to discriminate NPHP, even in adult cases.
Keywords: Nephronophthisis, Distal tubule, Renal biopsy, End-stage renal failure
Background
Nephronophthisis (NPHP) is a chronic tubular interstitial injuries and is the most common genetic causes of renal failure in children and young adults [1]. The estimated incidence of NPHP is 1:50,000 to 1:70,000 [2, 3], and account for approximately 10 to 15% of end-stage of renal disease (ESRD). Clinical features of NPHP are usually not specific, thus common features of chronic kidney disease (CKD), such as, urinary abnormalities, edema, and hypertension are rarely observed in patients with NPHP. Impairment ability to concentrate urine and retain body fluid induce polyuria, polydipsia, and decreased maximum urine concentration. Several patients with NPHP show extrarenal abnormalities, such as cerebellar ataxia, liver fibrosis, situs inversus, abnormal skeleton and facial features, Senior-Loken syndrome, Cogan syndrome and Joubert syndrome [4, 5].
NPHP is divided into three types based on the onset of ESRD, viz., infant type (approximately 5 years old), juvenile type (approximately 13–14 years old), and adolescent type (approximately 19 years old) [6]. It is not easy to diagnose as NPHP because of lack of specific clinical symptom. Thus, many of patients with NPHP progresses to ESRD in childhood or early adolescence. The diagnosis of NPHP is usually made by genetic analysis, as the findings in renal biopsy are not specific. The histopathology of NPHP is characterized by tubulointerstitial abnormalities, such as tubular atrophy, thickening or thinning of the tubular membrane, interstitial fibrosis and inflammation. However, those pathological phenotypes are not disease specific. Therefore, it is important to perform genetic analysis in suspected NPHP patients. Although NPHP has genetic heterogeneity, the most common NPHP mutation is a homozygous deletion of NPHP1, which is identified in 20% of patients with NPHP harboring NPHP gene mutations [7, 8]. Overall, a greater consideration of the diagnosis of NPHP is necessary to prevent expedited decline of renal function.
In the current report, we describe a case of NPHP diagnosed by genetic analysis at 26 years of age in a patient with atypical histological abnormalities.
Case presentation
The patient was a 26-year-old Japanese woman who showed no growth disorders or urinary abnormalities at school check-ups. However, during a medical check-up at 26 years of age, she showed renal dysfunction (serum creatinine 2.2 mg/dL). The estimated glomerular filtration rate (eGFR) was 26 mL/min/1.73 m2, and urine tests indicated low specific gravity of urine (1.004); however, proteinuria and microscopic hematuria were not detected. Urinary β2-microglobulin (β2-MG) was high (805 μg/L; Table 1). Analysis of her family history revealed that her father had chronic myelogenous leukemia and her mother had Sjogren’s syndrome and renal dysfunction. At the time of renal biopsy, the patient’s height, weight, and blood pressure were 155.6 cm, 51.4 kg, and 122/91 mmHg, respectively. Physical examination findings were normal. An abdominal computed tomography scan revealed that both kidneys were normal in size. We performed a percutaneous renal biopsy for definitive diagnosis.
Table 1.
Clinical examination at the renal biopsy
| Hematological | Reference values | Blood biochemistry | Reference values | Immunological test | Reference values | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| WBC | 5700 | 3300 ~ 8600 | /μl | TP | 7.0 | 6.6 ~ 8.1 | g/dl | CH50 | 59 | 25.0 ~ 48.0 | U/μl |
| Hb | 10.2 | 11.6 ~ 14.8 | g/dl | Alb | 4.2 | 4.1 ~ 5.1 | g/dl | C3 | 99 | 86 ~ 160 | mg/dl |
| Plt | 28.2 | 15.8 ~ 34.8 | × 104/μl | BUN | 19 | 8.0 ~ 20.0 | mg/dl | C4 | 24 | 17 ~ 45 | mg/dl |
| Cre | 2.03 | 0.46 ~ 0.79 | mg/dl | IgG | 1216 | 870 ~ 1700 | mg/dl | ||||
| Urinalysis | eGFR | 26 | 60~ | mL/min/1.73m2 | IgA | 228 | 110 ~ 410 | mg/dl | |||
| pH | 7.335 | 5.0 ~ 8.0 | Cystatin C | 2.05 | 0.56 ~ 0.87 | mg/dl | IgM | 152 | 33 ~ 190 | mg/dl | |
| Specific gravity | 1.004 | Na | 141 | 138 ~ 145 | mM/l | ANA | <× 40 | ~ 40 | |||
| Protein | < 20 | mg/dl | K | 4.1 | 3.6 ~ 4.8 | mM/l | anti SSA-Ab | 1.9 | ~ 7 | U/ml | |
| RBC | < 1 | /HPF | Cl | 107 | 101 ~ 108 | mM/l | anti SSB-Ab | < 1.0 | ~ 7 | U/ml | |
| WBC | < 1 | /HPF | Ca | 8.5 | 8.8 ~ 10.1 | mg/dl | MPO-ANCA | < 1.0 | ~ 3.5 | U/ml | |
| U-NAG | 1.4 | 0.7 ~ 11.2 | μg/l | CRP | < 0.1 | 0.00 ~ 0.14 | mg/dl | PR3-ANCA | < 1.0 | ~ 3.5 | U/ml |
| U-β2MG | 805 | ~ 230 | μg/l | HbA1c | 5.7 | 4.9 ~ 6.0 | % | anti GMB-Ab | < 2.0 | ~ 3 | U/ml |
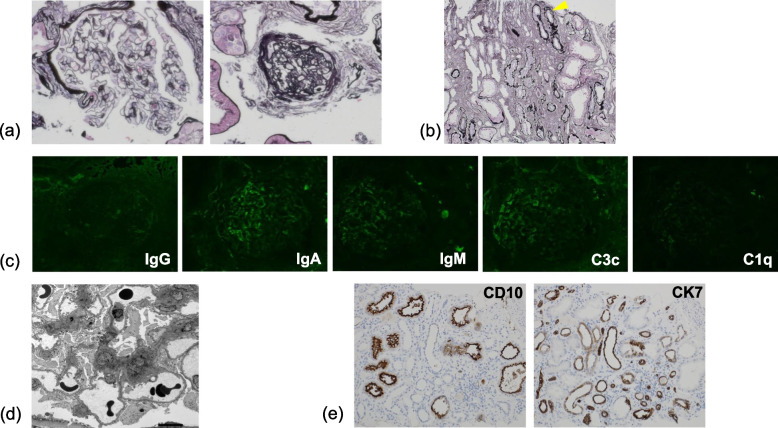
Histological findings showed global sclerotic lesions in approximately half of glomeruli (Fig. 1a). Moderate fibrosis was observed in the interstitial area, and moderate atrophy was observed in the tubules. Irregular splitting of the tubular basement membrane (ISTBM) [9] was also observed in some tubules (Fig. 1b). There were no significant findings in immunofluorescence analysis (Fig. 1c), and no electron dense deposits were detected by electron microscopy (Fig. 1d). Although cyst-like expansion of the tubules was unclear, tubular atrophy was dominantly found in the distal tubules by cytokeratin 7 (CK7) staining (Fig. 1e).
Fig. 1.
Renal biopsy histopathology. a Light microscopic findings indicate global sclerosis in half of the glomeruli. However, the other glomeruli showed minor lesions (periodic acid-silver methenamine stain; original magnification, 200×). b Moderate fibrosis was observed in the interstitial area, and moderate atrophy was observed in the tubules (periodic acid-silver methenamine stain; original magnification, 100×). Irregular splitting TBM was also observed in some tubules (arrowhead). c There were no significant findings in immunofluorescence analysis. d No electron dense deposits were detected by electron microscopy. e Cyst-like expansion of the tubular was unclear. Tubular atrophy was dominantly found in the distal tubule by CK7 staining (original magnification, 100×)
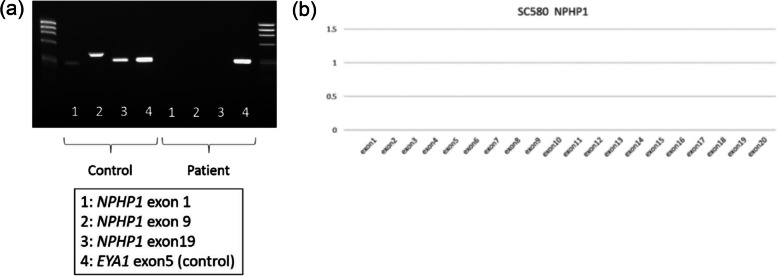
Next, we analyzed the NPHP1 gene, the most common gene responsible for NPHP. No exons of NPHP1 (1, 9, and 19) were amplified (Fig. 2a). Furthermore, multiplex ligation-dependent probe amplification analysis indicated complete deficiency of the NPHP1 gene (Fig. 2b). Based on these results, both alleles of NPHP1 were considered to be deleted in the current case, leading to a diagnosis of a total deletion of NPHP1.
Fig. 2.
Genetic analysis of the NPHP1 gene. a No exons from NPHP1 were amplified. b Multiplex ligation-dependent probe amplification analysis indicated complete deficiency of the NPHP1 gene
Discussion and conclusion
NPHP is the most common genetic cause of kidney failure in children and young adults [8, 10], with an estimated incidence of 1:50,000 [11, 12]. NPHP accounts for 6–10% of cases of kidney failure and 15% of renal transplants among children [13, 14]. NPHP has significant genetic heterogeneity, with biallelic pathogenic variants in 20 different genes identified as causative [15] with NPHP1 (20%) being the most common gene [8, 16, 17]. Although NPHP is the most common genetic cause of chronic kidney disease (CKD) in children, its prevalence in the adult population is thought to be low. However, Snoek R, et al. recently reported that the frequency of NPHP in adult onset ESRD is substantially higher than previous report [18]. Genome-wide association study using adult renal transplant recipients from several cohorts revealed median age of adult onset of ESRD was 30, ranged from 18 to 61 years old, in patients with NPHP [18]. Thus, NPHP should be considered as a differential diagnosis in adult patients with unidentified ESRD. With no specific management available, treatment focuses on supportive and preventative strategies to preserve kidney function. However, a greater consideration of the diagnosis of NPHP in adult patients with kidney failure and progressive CKD is required to allow informed prognosis, targeted screening of at-risk family members, and expedited preventative and management strategies of kidney function decline [19, 20].
The findings of this case report emphasize the importance of CD10 and CK7 staining in cases in which the cause of renal dysfunction is unclear. Irregular splitting TBM in tubules is an important finding suggesting autosomal dominant tubulointerstitial kidney disease [9]. In patients with renal failure with tubular interstitial disease dominantly in the distal tubule, it is necessary to discriminate NPHP, even in adult patients. Moreover, it is important to perform genetic testing to obtain a definitive diagnosis, which will enable appropriate genetic counseling and treatment. Further studies are necessary to clarify the mechanisms leading to wide variance in age of disease onset.
In summary, NPHP often progresses to ESRD at an average age of 13–14 years old. However, NPHP is not merely a pediatric disease and is relatively high incidence in patients with adult onset ESRD. Even in cases without typical histological abnormalities, such as cyst-like expansion of tubular lesions, differential diagnosis of NPHP is critical. Thus, wider application of genetic testing is recommended to patients with unidentified ESRD.
Acknowledgements
We would like to express our appreciation to the patient for her permission to publish this case. We also thank Drs. Naoya Morisada and Kazumoto Iijima (Department of Pediatrics, Kobe Graduate School of Medicine) for their voluntary genetic analysis.
Abbreviations
- NPHP
Nephronophthisis
- ESRD
End-stage of renal disease
- eGFR
Estimated glomerular filtration rate
- β2-MG
β2-microglobulin
- TBM
Tubular basement membrane
- CK7
Cytokeratin 7
Authors’ contributions
MA and HS reviewed the patient’s clinical data and wrote the initial draft of the manuscript. AI, MI, DH, HT, and HR assisted in the preparation of the manuscript and contributed to data collection and interpretation. ST analyzed the pathology of the renal biopsy. HS and YS conceived of the case report; carried out analyses of the patient’s clinical course, outcomes, and interpretation of the findings; and provided critical review comments for the manuscript. The authors read and approved the final manuscript.
Funding
This study was supported in part by a Grant-in-Aid for Intractable Renal Diseases Research, Research on rare and intractable diseases, Health and Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare of Japan. The funder supported costs for English proofreading and the fees upon acceptance for publication.
Availability of data and materials
The datasets used in the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Footnotes
The original version of this article was revised: we found that there were misprint in the Figure 2a.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
11/7/2023
A Correction to this paper has been published: 10.1186/s12882-023-03352-6
References
- 1.Wolf MT. Nephronophthisis and related syndromes. Curr Opin Pediatr. 2015;7:201–211. doi: 10.1097/MOP.0000000000000194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Potter DE, et al. Jr treatment of end-stage renal disease in children: a 15-year experience. Kidney Int. 1980;18:103–109. doi: 10.1038/ki.1980.115. [DOI] [PubMed] [Google Scholar]
- 3.Ala-Mello S, et al. Molecular studies in Finnish patients with familial juvenile nephronophthisis exclude a founder effect and support a common mutation causing mechanism. J Med Genet. 1998;35:279–283. doi: 10.1136/jmg.35.4.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsang SH, Aycinena ARP, Sharma T. Ciliopathy: senior-Løken syndrome. Adv Exp Med Biol. 2018;1085:175–178. doi: 10.1007/978-3-319-95046-4_34. [DOI] [PubMed] [Google Scholar]
- 5.Wang SF, et al. Review of ocular manifestations of joubert syndrome. Genes (Basel) 2018;9:605. doi: 10.3390/genes9120605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnan R, Eley L, Sayer JA. Urinary concentration defects and mechanisms underlying nephronophthisis. Kidney Blood Press Res. 2008;31:152–162. doi: 10.1159/000129648. [DOI] [PubMed] [Google Scholar]
- 7.Hildebrandt F, et al. A novel gene encoding an SH3 domain protein is mutated in nephronophthisis type 1. Nat Genet. 1997;17:149–153. doi: 10.1038/ng1097-149. [DOI] [PubMed] [Google Scholar]
- 8.Sugimoto K, et al. Clinical and genetic characteristics of Japanese nephronophthisis patients. Clin Exp Nephrol. 2016;20:637–649. doi: 10.1007/s10157-015-1180-5. [DOI] [PubMed] [Google Scholar]
- 9.Kitamura H. Gene mutation and morphological changes of MCKD and ADTKD. Japanese Soc Nephrol. 2018;60:1239–1243. [Google Scholar]
- 10.Mollet G, et al. The gene mutated in juvenile nephronophthisis type 4 encodes a novel protein that interacts with nephrocystin. Nat Genet. 2002;32:300–305. doi: 10.1038/ng996. [DOI] [PubMed] [Google Scholar]
- 11.Konig J, et al. Phenotypic spectrum of children with nephronophthisis and related ciliopathies. Clin J Am Soc Nephrol. 2017;12:1974–1983. doi: 10.2215/CJN.01280217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hildebrandt F, Zhou W. Nephronophthisis-associated ciliopathies. J Am Soc Nephrol. 2007;18:1855–1871. doi: 10.1681/ASN.2006121344. [DOI] [PubMed] [Google Scholar]
- 13.Mistry K, et al. Novel mutations in NPHP4 in a consanguineous family with histological findings of focal segmental glomerulosclerosis. Am J Kidney Dis. 2007;50:855–864. doi: 10.1053/j.ajkd.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Hoefele J, et al. Mutational analysis of the NPHP4 gene in 250 patients with nephronophthisis. Hum Mutat. 2005;25:411. doi: 10.1002/humu.9326. [DOI] [PubMed] [Google Scholar]
- 15.Hildebrandt F, Attanasio M, Otto E. Nephronophthisis: disease mechanisms of a ciliopathy. J Am Soc Nephrol. 2009;20:23–35. doi: 10.1681/ASN.2008050456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Srivastava S, et al. Many genes-one disease? Genetics of nephronophthisis (NPHP) and NPHP-associated disorders. Front Pediatr. 2017;5:287. doi: 10.3389/fped.2017.00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caridi G, et al. Clinical and molecular heterogeneity of juvenile nephronophthisis in Italy: insights from molecular screening. Am J Kidney Dis. 2000;35:44–51. doi: 10.1016/S0272-6386(00)70300-3. [DOI] [PubMed] [Google Scholar]
- 18.Snoek R, et al. NPHP1 (nephrocystin-1) gene deletions cause adult-onset ESRD. J Am Soc Nephrol. 2018;29:1772–1779. doi: 10.1681/ASN.2017111200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bakkaloglu SA, et al. Diverse phenotypic expression of NPHP4 mutations in four siblings. Turk J Pediatr. 2014;56:423–426. [PMC free article] [PubMed] [Google Scholar]
- 20.Srivastava S, Sayer JA. Nephronophthisis. J Pediatr Genet. 2014;3:103–114. doi: 10.3233/PGE-14086. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used in the current study are available from the corresponding author on reasonable request.