Abstract
Background:
Atypical presentation of coronavirus disease-19 (COVID-19) from classic acute respiratory distress syndrome needs to be extensively evaluated to understand the pathophysiology to optimize the management protocol for severely ill patients to abrogate the terminal event.
Methods:
Autopsy core needle biopsies of lungs were obtained from 12 patients who died with COVID-19. Routine histopathological examination of lung tissue along with immunohistochemical analysis of C4d complement staining was studied. Formalin-fixed paraffin-embedded biopsy material was also subjected to real-time reverse transcription-polymerase chain reaction for severe acute respiratory syndrome – coronavirus (SARS-CoV2) gene.
Results:
In the study, all the deceased patients were symptomatic with two-thirds suffering from isolated SARS-CoV2-related pneumonia while remaining one-third had secondary COVID-19 infection. Histopathological evaluation highlights diffuse alveolar damage as the predominant pattern; however, complement-mediated endothelial injury of septal microvasculature, and microthrombi was also distinctly observed with increased serum levels of D-Dimer and fibrinogen-degradation products. The patients who had extrapulmonary manifestations at the time of presentation also showed pulmonary vascular lesions on histopathologic examination. Our study confirms the presence of coagulopathy and immune-mediated microthrombi in pulmonary septal microvasculature in patients with severe disease.
Conclusion:
The results of our small series of patients highlight the possibility of immune-mediated pulmonary vascular injury and thrombosis which has the potential to evolve into large vessel thrombosis and pulmonary embolism in critically ill patients. Definitive therapeutic management protocol including thromboembolic prophylaxis and development of effective immune-modulatory target could possibly reduce mortality in severely ill patients.
KEY WORDS: COVID-19 pathology, lung biopsy, reverse transcription-polymerase chain reaction
INTRODUCTION
The coronavirus disease-19 (COVID-19), caused by severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), was first reported in early December 2019 (Zhu, 2019).[1] It primarily causes respiratory symptoms but occasionally neurologic, hepatic, and enteric symptoms have also been documented.[2]
The SARS-CoV-2 is an enveloped RNA virus which has four major structural proteins: the spike surface glycoprotein, small envelope protein, matrix protein, and nucleocapsid protein.[3] The pathogenesis of SARS-CoV-2-induced COVID-19 pneumonia is initiated by viral-host cell interaction through binding of spike protein to host receptors through the receptor-binding domains of angiotensin-converting enzyme 2 (ACE2).[4]
The ACE2 protein has been identified and localized in various human organ systems, including respiratory system, gastrointestinal tract, lymph nodes, thymus, bone marrow, spleen, liver, kidney, and brain.[5] Infection with SARS-CoV-2 in humans is associated with a wide spectrum of clinical respiratory syndromes, ranging from mild upper respiratory tract symptoms to progressive life-threatening viral pneumonia.[6] In COVID-19 pneumonia, extensive lung infiltration by macrophages and other immune cells leading to diffuse alveolar damage (DAD) or diffuse interstitial inflammation has been reported.[7] Severe sepsis is due to maladaptive host immune response leading to increased inflammatory markers and ferritin concentrations that result in local activation of pulmonary vascular endothelial cells.[8] The development of hypoxemia, secondary to acute respiratory distress syndrome (ARDS), might also activate the procoagulant coagulation cascade and has been incriminated in endothelial dysfunction as observed beyond the capillary network. Hypoxemia might also play a role in adjacent small pulmonary vascular thrombosis.[9] COVID-19 coagulopathy with significant elevation of D-dimer and fibrin/fibrinogen-degradation products (FDPs) most likely due to profound hyperdrive of inflammatory response, sparing other indices of hemostasis axes, namely prothrombin time, partial thromboplastin time, and platelet counts has been well documented.[10] Moreover, it has been observed that multifold elevation in serum levels of D-dimer is an ominous prognostic indicator mandating the use of anticoagulants in severely afflicted patients.[11]
Three characteristic angiocentric features of COVID-19 that has been reported so far include (i) severe endothelial injury associated with intracellular virus and disrupted endothelial cell membranes, (ii) intravascular thrombosis, microangiopathy, and occlusion of alveolar capillaries in lungs, and (iii) angiogenesis with prominent new vessel growth in the lungs of patients with COVID-19.[9] The present study was designed to examine postmortem histopathological changes within lung tissue of COVID-19-positive patients as confirmed by reverse transcription-polymerase chain reaction (RT-PCR), and the changes were evaluated and correlated in terms of severity of the disease. The postmortem findings were elaborated with the aim to appreciate underlying pathophysiology of disease process inclusive of documenting thromboembolic phenomenon in pulmonary tissue through histopathology, microvascular complement deposition, and presence of viral RNA in the lung tissue by RT-PCR for SARS-CoV-2 that could give potential insight into designing and formulating definitive management protocol. Clinicians world over are gradually developing a consensus on treating all COVID-19 patients admitted to the hospital, with pharmacologic venous thromboembolism prophylaxis, given the high inflammatory state, unless otherwise contraindicated.
METHODS
The present observational postmortem lung biopsy study was conducted on 12 COVID-19-positive patients, admitted to S. M. S. Medical College and Attached Hospitals, Jaipur, who had succumbed to the disease process after getting the requisite informed consent from deceased first-degree relative (or legal guardian of the descendent) and observing the stringent stipulations so laid down by Indian Council of Medical Research (ICMR), New Delhi. The study was approved by Institutional Ethics Committee, and ICMR was intimated accordingly. The medical records were deidentified and anonymized, and subsequently, clinical features, radiological investigations, coagulation profile, comorbidities if any, and duration of illness were assessed.
Tissue collection
Autopsy core needle biopsies of lungs were obtained with adequate biosafety measures during the procedure. The tissue so obtained was fixed in 10% neutral-buffered formalin, adequately fixed for 24 h, and then, processed with standard biosafety measures. H and E and trichrome-stained sections were observed independently by two pathologists who were blinded for clinical status of patients. The blocks were then submitted for immunohistochemical study for staining of complement C4d (PathnSitu, C4d, C4D204) in ten cases only as two blocks had insufficient sample. Nonspecific staining noted within the epithelial cells was disregarded while granular/linear staining along the alveolar capillaries and small-to-medium-sized blood vessels was taken as a marker for complement activation. Ten formalin-fixed paraffin-embedded (FFPE) biopsy materials were subjected to molecular testing by RT-PCR for SARS-COV-2.
RNA extraction for reverse transcription-polymerase chain reaction
FFPE tissue blocks were cut into 15 μm sections using microtome and further deparaffinized for RNA extraction using xylene. RNA was extracted by Qiaamp FFPE tissue kit (Qiagen, USA) as per the manufacturer's instructions. RNA quantity was checked using Infinite N200 Pro NanoQuant Spectrophotometer (Tecan, Switzerland) by calculating the ratio of absorbance at 260 and 280 nm. RNA purity was considered adequate when the 260/280 ratio was ≥1.9, as a lower ratio could indicate the presence of proteins, phenol, or other contaminants that typically show strong absorbance at 280 nm.
RESULTS
Clinical and Radiological findings [Table 1]
Table 1.
Clinical and radiological data of the cases
| Age | Sex | Symptoms | Diagnosis | Comorbidities | Chest radiograph | CT severity score |
|---|---|---|---|---|---|---|
| 78 | Male | Fever, SOB | Pneumonitis with AKI | Coronary artery disease | Bilateral lower zone haziness | Not done |
| 50 | Female | Fever, SOB | Pneumonitis | Hypertension, diabetes mellitus | Bilateral lower zone haziness | Not done |
| 2 | Male | Fever | TAPVC | Congenital heart disease | Cardiomegaly | Not done |
| 70 | Female | Fever, cough | A/H/O of RTA with bilateral pneumonitis | Nil | Bilateral pneumonitis | Not done |
| 35 | Male | Fever, cough, SOB | Pneumonitis | Hypertension | Right lower zone pneumonitis | 22/25 |
| 23 | Male | Fever, pain abdomen | Postoperative gangrenous appendicitis with sepsis | Nil | Normal | Not done |
| 20 | Female | Fever, weakness, back pain | Traumatic compressive myelopathy involving the thoracic vertebra | Nil | Nil | Not done |
| 33 | Male | Cough, fever, SOB | Bilateral pneumonitis | Nil | Bilateral diffuse heterogeneous infiltration | Not done |
| 59 | Female | Cough, fever, SOB | Bilateral pneumonitis | COPD, ILD | Bilateral peripheral homogeneous opacity | Not done |
| 28 | Male | Cough, fever, SOB | Bilateral pneumonitis | Nil | Bilateral diffuse heterogeneous infiltration | 18/25 |
| 75 | Female | Dyspnea | Bilateral pneumonitis | Nil | Bilateral pneumonitis | Not done |
| 60 | Male | Pain abdomen | Intestinal obstruction with septic shock | Nil | Normal | Not done |
CT: Computed tomography, SOB: Shortness of breath, AKI: Acute kidney injury, TAPVC: Total anomalous pulmonary venous circulation, COPD: Chronic obstructive pulmonary disease, ILD: Interstitial lung disease, RTA: Road traffic accident
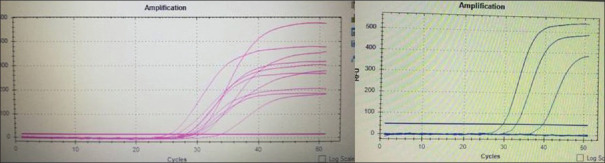
In the present study, all the deceased patients were symptomatic at the time of admission with most common clinical manifestations of fever in 66.66%, shortness of breath in 58.33%, and cough in 33.33%, while few patients had complained of pain abdomen in 16.67% and back pain in 8.33%. Eight patients (66.67%) in the present study population were diagnosed with isolated SARS-CoV-2-related pneumonia while remaining had secondary COVID-19 infection with gastrointestinal complications in two patients, congenital heart disease in one patient and traumatic compressive myelopathy in another. Five patients (41.66%) had underlying comorbid disease of which cardiac disease was found in two patients, hypertension in two patients, and type 2 diabetes mellitus and pulmonary disease in one patient each. The chest radiograph of eight deceased patients 66.67% had documented typical bilateral, peripheral, homogeneous, and lower zone dominant distribution of ground-glass opacities [Figure 1a]. The computed tomography (CT) scan report was available only in two patients and it depicted typical diffuse, bilateral, homogeneous, peripheral predominant ground-glass opacities with a CT severity score of more than 15 on the scoring scale of 25.[12] [Figure 1b].
Figure 1.
(a) Chest radiograph of 60-year-old male had COVID-19 infection with bilateral, diffuse, homogeneous opacities, peripheral predominant on left side suggestive, for COVID chest X-ray. (b) Coronal section of a 35-year-old male admitted with a chief complaint of fever, cough, SOB, high-resolution computed tomography chest shows diffuse ground-glass opacities with computed tomography severity score 22/25
X-rays and chest CT images are shown in Figure 1a and b, respectively.
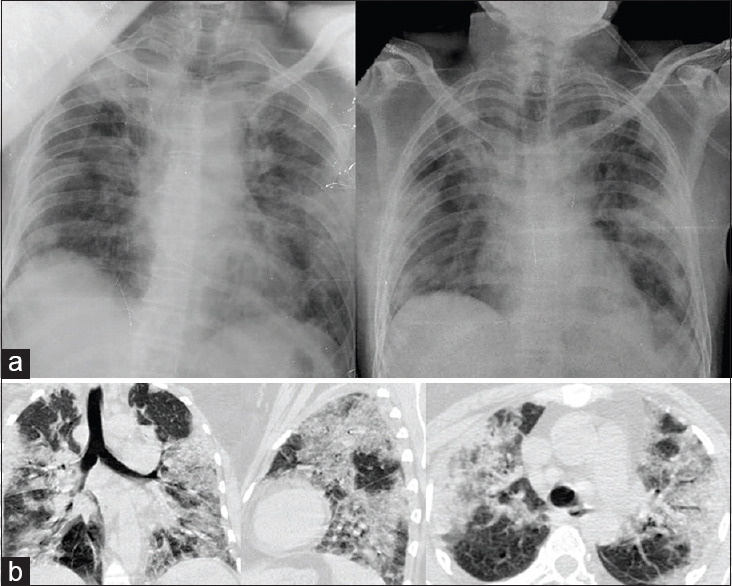
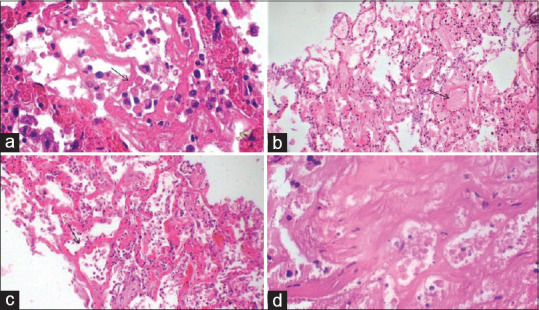
Histopathology findings
The histological changes exhibited DAD with cellular and proteinaceous exudates within the alveolar space [Figure 2b and c], intra-alveolar fibrin deposition with mononuclear infiltration with occasional multinucleated giant cells [Figure 3]. Desquamation of pneumocytes alternating with type II pneumocyte hyperplasia along with hyaline membrane formation was observed [Figure 2a] in 8 cases. However, an organization with interstitial thickening by fibrosis and intra-alveolar fibrous tissue was present in one of these cases. Interstitial mononuclear cells comprising T lymphocytes, plasma cells, and macrophages with septal edema were observed in three cases. A significant finding of septal microvascular injury in the form of endotheliosis, inflammation of vessel wall, thrombosis, and fibrinoid necrosis was observed in 11 of our 12 cases which were highlighted by trichrome stain [Figure 4a, c-f]. Red blood cell (RBC) extravasation was observed in the surrounding septa and alveolar spaces [Figure 4b]. The presence of complement C4d deposition in the vessel wall was observed in 6 out of 10 (60%) cases submitted for IHC [Figure 5].
Figure 2.
Microphotographs H and E stain. (a) Inflammatory alveolar exudates and hyaline membrane formation (×400). (b) Intra-alveolar exudates (×100). (c) Septal widening with intra-alveolar cellular exudate (×100). (d) infarcted lung tissue (×100)
Figure 3.
Microphotographs (a-d × 400) H and E-stained viral cytopathic changes and multinucleated giant cells (a, b and d). Early organization is also noted (c arrow)
Figure 4.
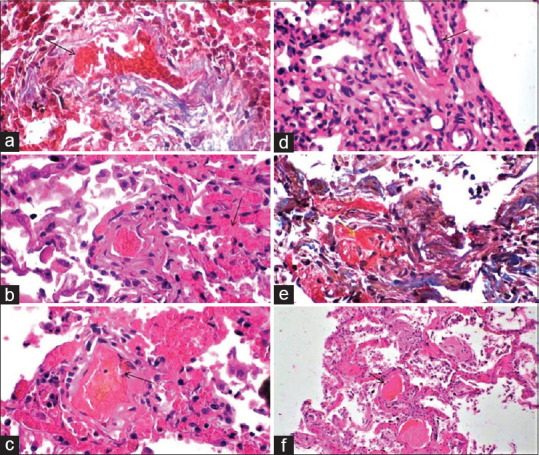
Microphotographs H and E and trichrome stain. (a) Vascular injury highlighted by trichrome stain (×400). (b) Septal widening with RBC extravasation and thickened vessel wall (×400). (c) Fibrin thrombi in alveolar capillary with disruption of the wall (×400). (d) Presence of inflammatory cells in the vessel wall (×400). (e) Fibrinous material in the vessel wall. ( yellow arrow) (×400). (f) Intravascular thrombi in the septal capillaries with perivascular inflammation (×100)
Figure 5.
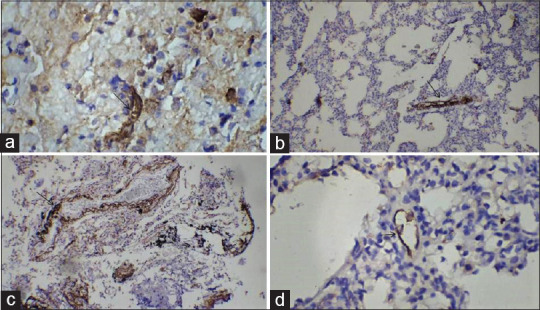
Microphotographs with immunohistochemistry (a and d, ×400) (b and c, ×100) - extensive C4d deposition in the septal microvasculature (arrows)
The postmortem findings of one patient [Case no. 3, Tables 1 and 2], an infant with congenital heart disease (total anomalous pulmonary venous circulation), documented interstitial inflammation along with complement deposition in the septal vessel wall. Another patient had characteristic feature of complete infarction in sampled biopsy tissue with thrombosed vessels and few inflammatory cells [Case no. 12, Tables 1 and 2 and Figure 2d], presumably representing thrombosis in medium size to large blood vessel.
Table 2.
Results of histology and immunohistochemical study along with fibrinogen-degradation products and D Dimer
| Case number | Age | Sex | Histopathological diagnosis | MVI (n=11/12) | C4d staining by IHC (n=6/10) | RT-PCR on FFPE (n=5/10) | FDP µg/ml (0.05.0) | D dimer µg/ml (0.00.50) |
|---|---|---|---|---|---|---|---|---|
| COVID-1 | 78 | Male | Acute exudative pneumonitis with DAD | Positive | Positive | Positive | - | - |
| COVID-2 | 50 | Female | Acute exudative pneumonitis with DAD MVI, fibrinoid necrosis | Positive | Negative | Positive | - | - |
| COVID-3 | 2 months | Male | Interstitial pneumonia with endotheliosis and vasculitis | Positive | Positive | Negative | - | - |
| COVID-4 | 70 | Female | Acute exudative pneumonitis with DAD MVI, fibrinoid necrosis | Positive | Positive | Positive | - | - |
| COVID-5 | 35 | Male | Acute exudative pneumonitis with DAD | Positive | Negative | Negative | - | - |
| COVID-6 | 23 | Male | Interstitial pneumonia with septal vasculitis and endotheliosis | Positive | Positive | Negative | 144.1 | 9.6 |
| COVID-7 | 20 | Female | Acute exudative pneumonitis with DAD with MVI | Positive | Negative | Negative | 115.0 | >20 |
| COVID-8 | 33 | Male | Acute exudative pneumonitis with DAD | Positive | Positive | Negative | - | - |
| COVID-9 | 59 | Female | DAD with organizing pneumonia with MVI | Positive | Negative | Positive | 59.9 | 13.8 |
| COVID-10 | 28 | Male | Interstitial pneumonitis MVT vasculitis endothelial inflammation | Positive | Not done | Not done | - | - |
| COVID-11 | 75 | Female | Acute exudative pneumonitis with DAD and vascular thrombosis | Positive | Positive | Positive | 46.4 | 11.5 |
| COVID-12 | 60 | Male | Lung infarct | Negative | Not done | Not done | 4.0 | 1.20 |
MVI: Microvascular inflammation, FFPE: Formalin-fixed paraffin embedded, IHC: Immunohistochemical, FDP: Fibrinogen-degradation products, RT-PCR: Reverse transcription-polymerase chain reaction, DAD: Diffuse alveolar damage, COVID: Coronavirus disease
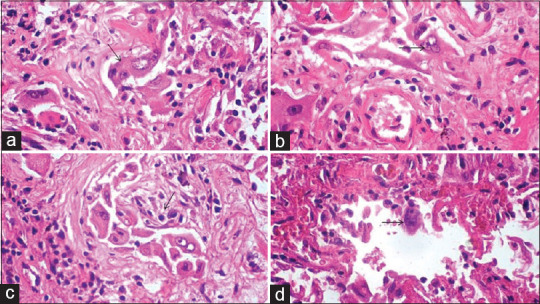
RT-PCR assay for SARS-COV-2 in lung tissue was performed on 10 FFPE tissue blocks. The result was positive in five cases with CT values ranging from ct28 to ct36 [Figure 6].
Figure 6.
Real-time polymerase chain reaction curves from SARS-CoV2 test samples. Right panel (blue color denotes the positive target gene RDRP) and left panel (pink color denotes the internal control)
DISCUSSION
The clinical manifestations of infection with SARS-CoV-2 are not limited to the respiratory system and are varied with other organ system dysfunctions, namely gastrointestinal complications, liver dysfunction, cardiac manifestations, and neurologic abnormalities.[13] Most of the patients in the present study presented with fever, shortness of breath, and cough at the time of admission and were diagnosed on chest radiograph as SARS-CoV-2-related pneumonia. It has been documented that individuals with coexisting comorbidities such as cardiovascular disease, diabetes mellitus, and obesity are likely to become critically ill.[14] Tian et al. in 2019 reported main pathologic findings from lungs in preliminary studies of COVID-19 pneumonia that was observed to be similar to findings of viral pneumonia and included intra-alveolar edema, hyaline membrane formation, inflammation, and fibrin exudates along with epithelial damage, and diffuse-type II pneumocyte hyperplasia, which are all features of DAD. Viral cytopathic effects in the form of cytolysis and intranuclear cytoplasmic inclusion were documented. There may be superimposed bacterial pneumonia in some patients.[15] In our study, acute exudative pneumonitis with DAD was observed in two-thirds of deceased. Intra-alveolar organization by fibroblastic proliferation and interstitial thickening was observed in one patient.
Three of the sample patient population documented acute interstitial inflammation with minimal alveolar exudates, one of whom was a 2-month-old infant with congenital heart disease (TAPVC). Septal vascular changes of endotheliosis and fibrinoid necrosis of vessel wall with RBC extravasation were observed in all the cases under study. The brunt of injury in these patients was restricted to septal vessels with mild pneumocyte involvement. All of our cases had a significant finding of microvascular injury and thrombosis with vasculopathy, leaving aside one case who had presented with intestinal obstruction and septic shock. The lung biopsy of this case documented the presence of necrotic tissue with inflammatory infiltrate and an area of infarct that could be due to occlusion of blood vessels by thrombus. Studies have suggested that COVID-19 has clinical features distinct from typical ARDS. Severe respiratory distress in this disease manifests by relatively well-preserved lung mechanics, despite the severity of hypoxemia. The pathology in these cases might therefore be expected to differ from the DAD and hyaline membrane formation which are hallmarks of typical ARDS.[16,17] Earlier studies have suggested that tissue injury is not primarily due to viral infection but is a result of overdrive of host immune response that releases excessive cytokines inducing a state of hyper inflammation leading to lung parenchymal damage and endothelial injury subsequent to thrombosis.[18] SARS CoV-2-associated thrombotic microangiopathy may progress to proliferative vasculitis with thrombosis of the arterioles and medium to large artery and veins. The virus is known to activate complement system through lectin pathway initially and then classical and alternate pathway to form the terminal products C5a and C5b-9 causing tissue injury and thrombosis.[19] The presenting pathologic pattern, atypical for classic ARDS, is due to extensive deposition of complements within the lung septal microvasculature leading to membrane attack complex-mediated microvascular endothelial cell injury and subsequent activation of the clotting pathway with fibrin deposition in the wall of blood vessels.[20] A role of complement activation and microvascular thrombosis has been defined in severe cases which is demonstrated by deposition of complement components C5b-9, C4d, and MASP2 by immunohistochemistry.[19] Increased activation of coagulation pathway is further exemplified by elevated D-dimer concentrations at presentation that also happens to be an independent risk factor for death in these patients.[17] Four of deceased patients had extrapulmonary presentations as intestinal obstruction and gangrenous appendicitis with septic shock, congenital heart disease with fever, and traumatic compressive myelopathy. No respiratory symptoms had been documented in these deceased patients with normal chest radiograph except for the infant with congenital heart disease who had cardiomegaly. It had been reported that COVID-19-positive patients develop hypoxemia with sudden deterioration leading to death. The histopathological evaluation of lung biopsy in these patients had documented prominent interstitial inflammation in two cases and early DAD, with hyaline membrane formation in the remaining two. Juxtaposed pulmonary septal vascular involvement was also observed in all four cases with two of them showing deposition of C4d. RT-PCR results on FFPE tissue samples in these four biopsies were negative.
In the study of 12 cases, serum D-dimer and FDP levels were retrieved in five patients, of which four had markedly raised values and two of these had extrapulmonary presentation with subsequent development of hypoxemia.
Biopsy tissue submitted for immunohistochemistry showed extensive C4d deposition localized to inter-alveolar septal capillaries in 6 of 10 cases. All these 6 patients had severe disease presenting morphologically with microvascular injury, fibrinoid necrosis, and inflammation of vessel wall. Severity of the disease was also evident radiologically where all six cases with complement deposition presented with bilateral diffuse pneumonitis.
The presence of viral RNA was documented in 5 of 10 biopsies subjected to RT-PCR assay on FFPE tissue indicative of viral-induced injury.
The results of the study highlight the fact that DAD is the predominant pattern of lung injury in the disease process of COVID-19. Furthermore, the prevalence and severity of endothelial injury of septal microvasculature with microthrombi were also prominently seen. The immune mechanism associated with the disease triggers vascular damage with immune-thrombosis which could be one of contributing factors leading to fatality of the disease. Moreover, increased levels of D-dimer and FDP in serum as observed in our cases are indicative of an impending fulminant smoldering state of hypercoagulability and microangiopathy in critically ill patients.
All hospitalized patients should undergo thromboembolism prophylaxis with an increase in therapeutic anticoagulation in certain clinical situations.[21] Even though there is an associated coagulopathy with COVID-19, bleeding manifestations, even in those with DIC, have not been reported.[22] According to the International Society on Thrombosis and Hemostasis, in patients with markedly raised D-dimers (arbitrarily defined as 3–4-fold increase), hospital admission should be considered even in the absence of other symptoms suggesting disease severity, as this clearly signifies increased thrombin generation.[23] Tang et al. suggest that patients who have documented coagulopathy need to be put on anticoagulation therapy of heparin that could plausibly reduce mortality.[24] Our study also confirms the presence of coagulation disorder presenting as complement-mediated microvascular thrombosis in the biopsy material. Therefore, a 3–4-fold elevation in D-dimer level in a critically ill patient could act as reasonably logical dictate for start of anticoagulation therapeutic intervention immediately.
The main limitation of the present study was nonavailability of radiological and laboratory data in some cases. Furthermore, the sample size is small, and inference cannot be extrapolated and needs to be studied on a larger patient cohort
CONCLUSION
The study provides invaluable insights into mechanism of disease and pathophysiologic role of complement activation, morphologic alterations along with an enhanced propensity for coagulopathy, and thromboembolism in severe COVID 19 disease. Serum levels of D-dimer and FDP need to be closely monitored particularly in patients with 3–4-fold increased levels, which portend ominous levels of thrombin generation in blood.
It is logical to propose and advocate the use of thromboembolic prophylaxis and effective immunomodulatory therapeutic target such as complement and cytokine inhibitors in critically ill patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to acknowledge the multidisciplinary research unit, SMS Medical College, Jaipur (a unit of DHR-ICMR) to provide ecofriendly environment for molecular laboratory work.
REFERENCES
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li F. Structure, function, and evolution of coronavirus spike proteins. Annu Rev Virol. 2016;3:237–61. doi: 10.1146/annurev-virology-110615-042301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–20. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 5.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–7. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franks TJ, Chong PY, Chui P, Galvin JR, Lourens RM, Reid AH, et al. Lung pathology of severe acute respiratory syndrome (SARS): A study of 8 autopsy cases from Singapore. Hum Pathol. 2003;34:743–8. doi: 10.1016/S0046-8177(03)00367-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ten VS, Pinsky DJ. Endothelial response to hypoxia: Physiologic adaptation and pathologic dysfunction. Curr Opin Crit Care. 2002;8:242–50. doi: 10.1097/00075198-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N Engl J Med. 2020;383:120–8. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, et al. Pulmonary embolism in patients with COVID-19: Awareness of an increased prevalence. Circulation. 2020;142:184–6. doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 12.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin Imaging. 2020;66:35–41. doi: 10.1016/j.clinimag.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–14. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “Typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Risitano AM, Mastellos DC, Huber-Lang M, Yancopoulou D, Garlanda C, Ciceri F, et al. Complement as a target in COVID-19? Nat Rev Immunol. 2020;20:343–4. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1–3. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaturvedi S, Braunstein EM, Yuan X, Yu J, Alexander A, Chen H, et al. Complement activity and complement regulatory gene mutations are associated with thrombosis in APS and CAPS. Blood. 2020;135:239–51. doi: 10.1182/blood.2019003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of coronavirus disease 2019. Crit Care Med. 2020;48:1358–64. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–40. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–6. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–7. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]